Abstract
Background
Shortage of neurosurgeons in Pakistan, one per 720,000 people, stems from a lack of trainees. Therefore, it is vital to assess the training experience, career opportunities, and satisfaction levels of neurosurgical trainees in Pakistan.
Methods
A nationwide survey was conducted, covering 22 CPSP-accredited neurosurgery training programs in Pakistan. Convenience sampling was utilized with a pilot tested questionnaire and responses were analyzed using STATA 15.
Results
The response rate was 98% (120/122) with 70.8% male and mean age of 30.4 ± 4.1 years. Training programs included teaching courses (79%) and journal club (66%); however, there was a lack of cadaver workshops (14%) and cranial model-based stimulation (22%). 67% of trainees lacked publications in indexed journals. 69% worked 50–100 h weekly, with 62% experiencing burnout due to workload and hours and a third reporting poor work-life balance. Trainees dedicated more to operating rooms (37%, 10–24 h/week) and clinics (34%, 24–48 h/week) compared to study (42%, <5 h/week) and research (64%, <5 h/week). Gender equality was rated poorly by 50%. Disparities emerged in subspecialty exposure, with over half of trainees lacking exposure to deep brain stimulation (67%), and epilepsy (75%). 52.5% of the training institutes did not offer fellowships and 64.1% of trainees planned to pursue fellowships abroad.
Conclusions
Steps need to be taken to improve working hours, gender equity, and increase simulation courses, diversify subspecialty exposure, and promote research initiatives.
Keywords: Neurosurgery, Residency, Surgical training, Developing Country
Abbreviations List
- PGY
Postgraduate year
- CPSP
College of Physicians and Surgeons of Pakistan
- FSPS
Fellow of College of Physicians and Surgeons
- MBBS
Bachelor of Medicine and Bachelor of Surgery
- ICT
Islamabad
- KPK
Khyber Pakhtunkhwa
1. Introduction
The field of neurosurgery has seen monumental growth since the earliest foundations, laid by ancient South America, Egypt and Greece.1 Despite these historic contributions, organized neurosurgery is one of the younger fields of surgery and modern neurosurgery can be credited to Sir William Macewen and others across Europe and the United States who continued to build on his works.1,2 The innovations in robotic surgery, intraoperative imaging, and neuromodulation, have meant the field continues to progress at rates unmatched throughout the history of the field.
Surgeons and their team must have critical knowledge of detail, as well as concentration, precision, and expertise of surgery. Their outpatient facilities and operating rooms must be built on collaboration and must be able to guarantee the availability of life-saving medications, advanced imaging techniques, and the latest surgical equipment. Furthermore, they require comprehensive continuous training to ensure surgeons can make diagnoses and provide care that is updated to recent-most developments in global literature.
Several factors contribute to the limited availability of appropriate neurosurgery training programs in Pakistan. The healthcare expenditure, which includes expenditure on training programs, remains a low priority for the country where only 3.38% of GDP is allocated to healthcare.3 These are concerning low numbers for an LMIC. Furthermore, the lack of qualified trainers and mentors adversely affects the quality of training available to neurosurgery residents. The country has a total of 212 trained neurosurgeons, which averages to about 1 neurosurgeon for every million population.4 This number is significantly lower than numbers seen across many countries.5 The low research output from Pakistan can be seen as evidence of the lack of quality facilities and resident-training structures.6
In Pakistan, the journey to becoming a neurosurgeon is rigorous and demanding. After completing a five-year Bachelor of Medicine and Bachelor of Surgery (MBBS) program, medical graduates embark on a one-year clinical internship or house job in various specialties. Subsequently, those aspiring to become neurosurgeons must complete a set of examinations and secure a highly competitive spot in a direct neurosurgery program or a general surgery residency program, where they can then make the switch to neurosurgery after completing two years of training. A College of Physicians and Surgeons Pakistan (CPSP) recognized fellowship or a university-based master's program are the two available training programs, each extending five to six years.7,8 This prolonged and intensive pathway requires unwavering commitment, dedication, and the pursuit of excellence in a field that demands nothing less.
According to a study from 2021,9 a total of 177 residents are being trained at 22 centers across the country. CPSP has developed a structured neurosurgery program and compiled a curriculum for post-graduate training in Pakistan. The organization also ensures teaching hospitals across the country have established dedicated neurosurgery departments conforming to international standards with state-of-the-art facilities.10 The number of available facilities, however, still fails to cater to the needs of those interested in pursuing neurosurgery. Medical graduates from Pakistan, across many specialties, aim to find training in other countries, particularly the United States and the United Kingdom.11
Constant improvements are crucial for all levels of medical education to keep up with technological advancements and learner needs. Although previous studies have assessed the status of training in Pakistan,12 a comprehensive study exploring main stakeholder recommendations from the trainees and their plans for fellowship has not been explored. It is therefore important to comprehensively explore the current system, to update the literature on the current status before any reforms can be made. The authors thereby felt a need to carry out a large scoping survey of neurosurgery trainees in Pakistan and present this study.
2. Materials and methods
A nationwide survey was conducted over a three-week period from April 1st to April 20th, 2023, among neurosurgery trainees in Pakistan. The study's overarching goal was to evaluate the neurosurgery training experience, encompassing both academic and surgical aspects, and to gauge trainee satisfaction and assess the available career opportunities in the field. Ethical approval for the study was granted by the Ethical Review Committee of Aga Khan University, Pakistan. The survey target population was neurosurgery trainees, including fellows and instructors, from various regions across the country.
Sample size and population: This sample size was calculated using OpenEpi.13 There are an estimated 22 CPSP accredited neurosurgery training centers with 177 registered neurosurgery residents in training.9 Therefore, with 95% confidence interval and 5% confidence limits, the minimum sample size required was 122 for neurosurgical trainees. Our study achieved a 98.36% response rate from our desired sample size.
Data collection tool: Due to the absence of a previously validated questionnaire suitable for our population, the questionnaire used was self-designed by the research team in close association with faculty with expertise in cross-sectional studies and neurosurgery research team at the section of neurosurgery at the Aga Khan University. The questionnaire underwent a validation process to ensure content validity and reliability. Content validity was confirmed through a panel review of neurosurgeons, while reliability was assessed using test-retest and Cronbach's alpha methods. A pilot study involving ten neurosurgery trainees further refined the questionnaire, with adjustments made to response options to improve clarity. The final questionnaire covered participant demographics, training characteristics in terms of types of engagement in their institute, opportunities for surgical exposure, research and study, training satisfaction, possible barriers and recommendations, and plans for further training.
Sampling and data collection strategy: We utilized the method of non-probability convenience sampling and snowball sampling approaches. Dissemination of the questionnaire was undertaken by an anonymous Google Form survey, which included a consent form explaining the aims and objectives of the study.
Potential participants were sourced through an ambassadorship program created by the research team, which recruited data collectors from all over Pakistan. The ambassadorship program for our study yielded approximately an equal distribution of data collectors from all provinces of Pakistan. Multiple strategies of data collection were used, which included online distribution through social media platforms and a face-to-face approach. Moreover, emails were sent out to neurosurgery residency programs across Pakistan to invite them to our study.
Statistical analysis: Statistical analyses were run using STATA 15. Descriptive statistics were used to report the demographic characteristics found through the study. Normally distributed continuous data was reported as mean ± standard deviation (SD), whereas categorical data was reported as gross numbers and percentages (n; %). Unpaired categorical data was compared using Chi-squared tests. A p-value <0.05 was considered as significant for all analyses.
Ethical considerations: The study received ethical approval from Aga Khan University Ethical Review Committee (AKU-ERC). Participants received a detailed explanation of the study, including its objectives, procedures, and their rights. They were given the chance to seek clarification and were provided with an informed consent form. Participation was entirely voluntary, and participants could withdraw at any point without consequences. To protect their anonymity and confidentiality, no personal identifiers were gathered. Data was securely stored in a password-encrypted file, with access restricted to the principal investigator and co-investigators.
3. Results
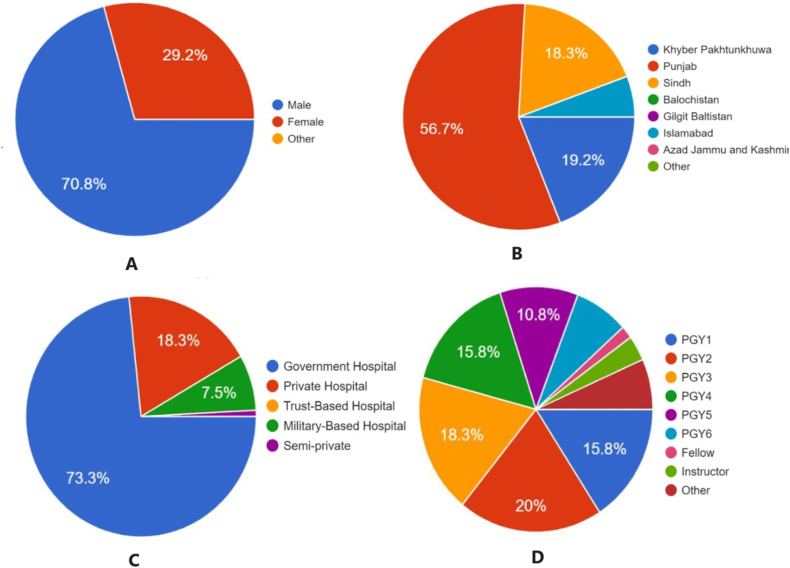
A total of 120 neurosurgery trainees from various training centers across Pakistan- Punjab (56.7%), Sindh (18.3%), Khyber Pakhtunkhwa (19.2%), and the federal capital, Islamabad (5.8%) participated in the survey (Fig. 1B). The mean age of participants was 30.4 ± 4.1 years. Most respondents were male (70.8%) and from Government Hospitals (81.7%), as shown in Fig. 1A and C. Most participants were residents (88.3%), while only 2 participants were fellows, and 4 were instructors, as illustrated in Fig. 1D. 95% of participants had average salaries between 50,000 and 150,000 PKR and more than half had a monthly household income under 150,000 PKR. The sociodemographic characteristics of the participants are summarized in Table 1.
Fig. 1.
A) Distribution of responses by gender as a percentage. B) Regional distribution of responses across Pakistan (%). C) Distribution of responses based on institutional sector (%). D) Responses categorized by year of training. Postgraduate year (PGY).
Table 1.
Respondent demographics, Institution sector and province, Year of Training, Monthly Salary, and Household Income.
| Variable | n (%) |
|---|---|
| Age (mean ± SD) | 30.43 ± 4.186 |
| Gender | |
| Female | 35 (29.2) |
| Male | 85 (70.8) |
| Province and Capital | |
| Islamabad | 7 (5.8) |
| KPK | 23 (19.2) |
| Punjab | 68 (56.7) |
| Sindh | 22 (18.3) |
| Institution Sector | |
| Private Hospital | 98 (81.7) |
| Government Hospital | 22 (18.3) |
| Year of Training | |
| PGY1 | 19 (15.8) |
| PGY2 | 24 (20) |
| PGY3 | 22 (18.3) |
| PGY4 | 19 (15.8) |
| PGY5 | 13 (10.8) |
| PGY6 | 9 (7.5) |
| Fellow | 2 (1.7) |
| Instructor | 4 (3.3) |
| Other | 8 (6.7) |
| Monthly Salary (PKR) | |
| <50,000 | 3 (2.5) |
| 50,000–100,000 | 62 (51.7) |
| 100,000–150,000 | 52 (43.3) |
| 150,000–200,000 | 3 (2.5) |
| Monthly Household Income (PKR) | |
| <100,000 | 21 (17.5) |
| 100,000–150,000 | 50 (41.7) |
| 200,000–300,000 | 16 (13.3) |
| 300,000–400,000 | 2 (1.7) |
| 400,000–500,000 | 1 (0.8) |
| >500,000 | 1 (0.8) |
Table 2 shows the reported academic activities of the participants’ training programs. The majority of respondents indicated that their training programs offered teaching courses (79.2%), neurosurgical conferences (81.7%), and educational activities such as morbidity and mortality meetings (84.2%) and journal clubs (66.7%). However, opportunities such as cadaver workshops (14.2%), augmented/virtual reality simulations (9.2%), and didactic lectures (38.3%) were reported less frequently. The availability of a regular evaluation system for trainees was reported by 50.8% of respondents, while 47.5% reported the presence of fellowship training opportunities in their hospitals.
Table 2.
Training Program Characteristics in terms of Learning Modalities.
| Yes [n (%)] | No [n (%)] | |
|---|---|---|
| Courses and Workshops | ||
| Teaching Courses | 95(79.2) | 25(20.8) |
| Cadaver Workshops | 17(14.2) | 103(85.8) |
| Neurosurgical Conferences | 98(81.7) | 22(18.3) |
| Live Surgery Workshops | 62(51.7) | 58(48.3) |
| Cranial model-based simulation | 27(22.5) | 93(77.5) |
| Spinal Model-based simulation | 28(23.3) | 92(76.7) |
| Augmented/Virtual Reality simulation | 11(9.2) | 109(90.8) |
| Educational Activities | ||
| Morbidity and Mortality Meetings | 101(84.2) | 19(15.8) |
| Tumor Board Meetings | 77(64.2) | 43(35.8) |
| Journal Club | 80(66.7) | 40(33.3) |
| Case Based sessions | 93(77.5) | 27(22.5) |
| Seminar | 87(72.5) | 33(27.5) |
| Pre-operative discussion | 91(75.8) | 29(24.2) |
| Didactic Lecture | 46(38.3) | 74(61.7) |
| Radiology Discussion and Interpretation | 92(76.7) | 28(23.3) |
Significant associations were observed in the availability of spinal model-based simulations (p = 0.007) and cranial model-based simulations (p = 0.001), as participants from private hospital training programs reported higher prevalence of simulation-based training. On the contrary, a higher prevalence of live surgery workshops (p = 0.039) was reported by respondents from public hospitals than private hospitals.
Our findings showed significant associations between availability of training program characteristics and the province of training. A greater proportion of trainees from KPK and Punjab have radiology discussions (p = 0.008) and preoperative discussions (p = 0.043), compared to Islamabad and Sindh. While more seminars occur according to trainees in Sindh (86.4%) and Punjab (76.5%). Significant differences were also observed between provinces for journal club (p = 0.015), cranial-based simulations (p = 0.046), live surgery workshops (p = 0.002) and neurosurgical conferences (0.024).
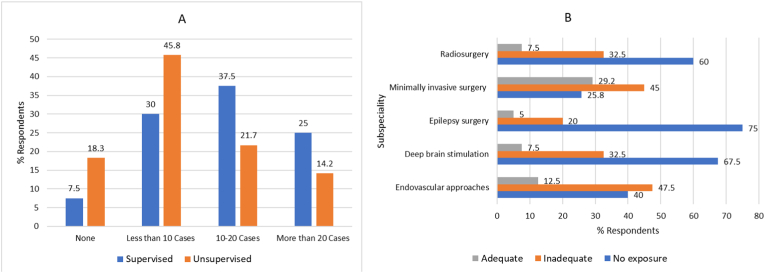
Our study also explored the trainees’ hands-on surgical exposure during training. Most trainees reported to have unsupervised exposure of less than 10 cases (45.8%) and supervised exposure of 10–20 cases (37.5%). However, exposure to subspecialties was reported as inadequate or absent in several areas, including endovascular approaches (87.5%), deep brain stimulation (>90%), epilepsy surgery (95%), minimally invasive surgery (60.8%), and radiosurgery (92.5%). Surgical exposure is depicted in Fig. 2.
Fig. 2.
Surgical exposure of trainees (A) Based on number of cases divided between supervised and unsupervised and (B) Based on subspeciality.
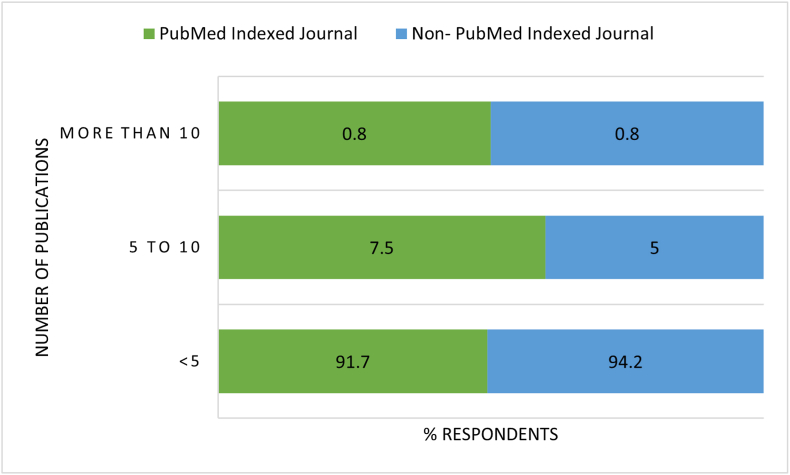
Over 90% of the participants had little to no research publications with 24.2% and 40% of respondents having under 5 neurosurgery publications, PubMed Indexed and Non-Indexed, respectively. 67.5% reported no PubMed indexed publications while 54.2% further reported zero non-PubMed indexed publications. Only one respondent had more than 10 publications, both indexed and non-indexed. Fig. 3 depicts the publication output of trainees in our study.
Fig. 3.
Research publications of respondents divided between indexing.
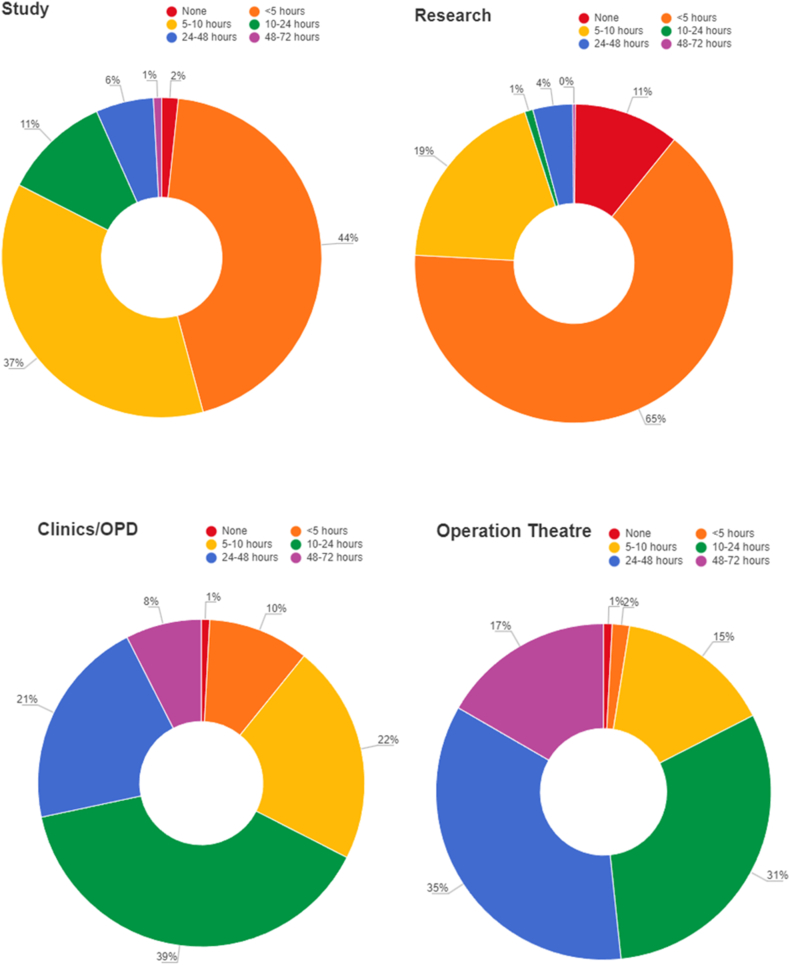
A predominant portion of the trainees allocated a higher amount of weekly hours to surgical activities within operating rooms (35% for 24–48 h/week and 31% for 10–24 h/week) and clinical duties (39% for 10–24 h/week and 21% for 24–48 h/week) in comparison to their engagement in academic activities, including research (4% for 24–48 h/week and 1% for 10–24 h/week) and study (6% for 24–48 h/week and 11% for 10–24 h/week), as depicted in Fig. 4.
Fig. 4.
Graphs showing time allotment to various activities during training.
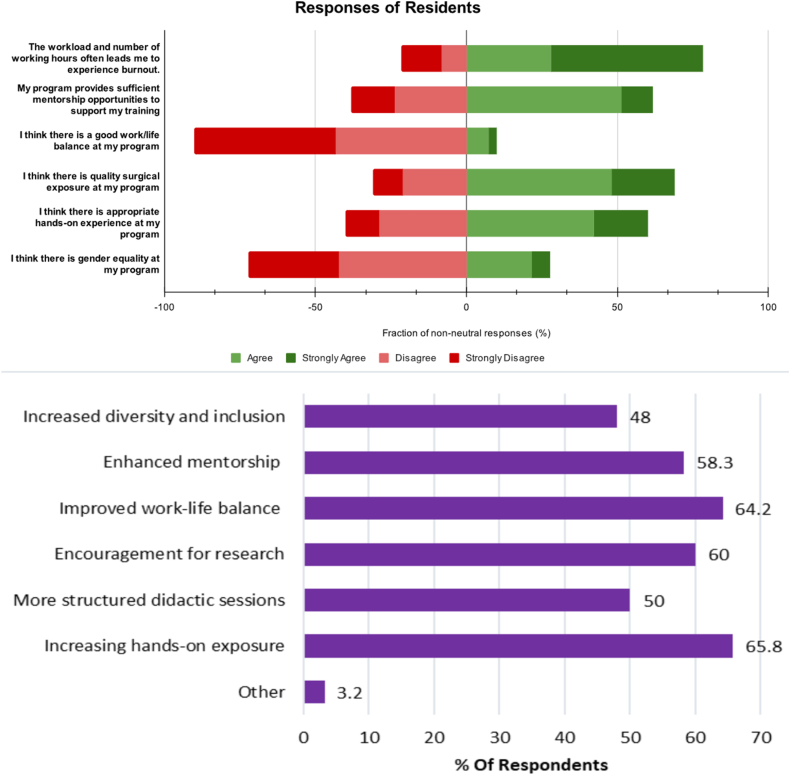
Fig. 5 portrays trainee responses, collected on a Likert scale, of their perceptions about various aspects, particularly major barriers encountered during neurosurgery training and their suggested improvements. Majorities shared opinions that their programs had poor work-life balance leading to burnout, and poor gender equality. Additionally, the proposed improvements to training programs by trainees included improvements in work-life balance (64%), fostering research and innovation (60%), augmenting mentorship of trainees (58.3%), improving hands-on surgical exposure (65.8%), and promoting diversity and inclusion within the training program (40%).
Fig. 5.
Top- Likert Scale responses to barriers in training. Bottom- Suggested improvements by trainees.
Plans for fellowship were also assessed through our study (Table 3). We found 52.5% of the respondents reported that their hospital did not offer fellowship in neurosurgery. Moreover, out of the trainees, 60% intend to pursue further training abroad, with 44% pursuing fellowships in the United Kingdom and Ireland, 18.3% in the USA, and 34.2% planning to stay in Pakistan. In terms of subspecialty preferences, the majority expressed interest in neuro-oncology (20%), followed by neurotrauma and critical care (14.2%), endovascular (13.3%), and pediatrics (12.5%).
Table 3.
Future plans for fellowship in terms of subspecialty and location for further training.
| In which subspeciality are you planning to pursue a fellowship? | |
|---|---|
| Specialty | n (%) |
| Cerebrovascular Endovascular/Interventional at Neuroradiology Functional and Epilepsy Neuro-trauma and Critical Care Neuro-oncology Pediatrics Peripheral Nerve Radiosurgery Skull base/Complex Cranial Spine None |
12(10) 15(12.5) 3(2.5) 17(14.5) 15(12.5) 9(7.5) 7(5.8) 4(3.3) 13(10.8) 24(20) 9(7.5) |
| Where do you plan to pursue your fellowship? | |
| Australia Germany Pakistan UK/Ireland USA None |
1(0.8) 1(0.8) 41(34.2) 53(44.2) 22(18.3) 2(1.7) |
4. Discussion
Our nationwide study provides an assessment of neurosurgery training program characteristics and deficiencies and goes on further to gauge trainee recommendations and plans beyond post-graduate education. Our study finds that training programs vary greatly in terms of the opportunities and experiences offered to neurosurgery trainees. However, the availability of teaching courses, neurosurgical conferences, and educational activities such as morbidity and mortality meetings and journal clubs are promising, indicating efforts to provide a well-rounded training experience. Despite availability of such programs, our study finds disparities between sectors and provinces, thereby calling for efforts to standardize post-graduate training throughout Pakistan.
Our study finds the majority of trainees to come from above households with a monthly income of greater than PKR 100,000. Comparing this with the median household income in Pakistan of PKR 41,545, most trainees for neurosurgery come from higher income households, shedding light into socioeconomic barriers to specialization in the resource-limited setting of Pakistan. This serves to exemplify previous evidence which shows that socioeconomically disadvantaged students tend to experiment less with their career choices.14 Therefore, to make neurosurgery a more accessible field to practice in limited resource nations, one must reduce the challenges of a trainee.
With a majority of participants reporting gender inequality in their programs and a male predominance of neurosurgery trainees, our findings relate to previous studies.9,15 This disparity can be attributed to a complex interplay of various factors, many of which are deeply rooted in societal and historical contexts.16 Historical gender stereotypes and bias, where women are expected to leave careers on hold for matters such as the birth and upbringing of offspring have a two-fold effect as they discourage women from pursuing careers like neurosurgery, and also some program directors are less likely to consider a woman due to the fear of societal norms pressuring them to prioritize family over a career. These factors, coupled with the pre-existing lack of female mentors17 in the field, could explain the disparity in the number of female to male trainees. The poor work-life balance and cases of discrimination and harassment18,19 have all been described as factors dissuading women from surgical fields.
The study observed associations between training program characteristics and sector of hospital, and province. Public sector trainees from Islamabad reported lowest program characteristics such as simulation models, seminars, and discussions, closely followed by trainees from KPK, which is likely due to the geographical contrast from the plains of Sindh and Punjab, making them comparatively less accessible. Additionally, these institutes are younger than those in Sindh and Punjab and hence lag in the presence of infrastructure. The other finding is in congruence to a previous study from Pakistan,9 which details the differences between public and private hospital training in Pakistan and how the public sector training lags behind the private sector. These differences underscore the need for targeted interventions to address variations in training experiences. They also call attention from policymakers and training institutions to these disparities in resources and training quality, to help improve overall neurosurgical training in Pakistan.
The limited availability of certain opportunities like cadaver workshops and advanced simulations raises concerns about the practical exposure of trainees to complex surgical techniques. Ali et al12 also outlined similar limitations in training where a quarter of residents did not participate in any hands-on workshop during their entire. A possible reason for this is the financial expense as these labs can be costly to set up, with some requiring capital investments, upwards of millions of dollars.20 Though some models have seen success setting up labs with a fraction of the investment, these can still be a challenge for economies like Pakistan.21 These models have used existing university infrastructure, such as forensic labs, which are not always available in Pakistan. Centers have been able to establish skills and cadaver labs despite financial constraints with the help of monetary donations from faculty and other institutions, as well as seeking decommissioned, yet functioning equipment from within and outside the center.22, 23, 24 The impact of setting up these labs is undeniable in training, and institutional partnerships such as sharing the center for elective rotations can further enhance its role in improving training across the country.25
The research experience of participants, as evidenced by self-reported publication records, suggests the need for fostering a research culture within the neurosurgery community. Our findings are in agreement with previous studies, that have also reported an underdeveloped research atmosphere in Pakistan,6 where the commonly reported barriers to research have been poor research infrastructure and funding, as well as time constraints.26 Despite CPSP's mandatory dissertation for surgical training certification eligibility, the country's post-graduate research output has been dismal.27 Greater emphasis on research mentorship and support can contribute to improving the research output of trainees and enhancing the overall quality of neurosurgery training programs.28,29 There have been efforts to encourage a lifestyle of research, where online modalities have been used to cater to the wide geographical areas of Pakistan.27
The exposure to subspecialties and hands-on surgical experience reported by participants emphasizes the need for a well-structured training curriculum that provides diverse and comprehensive exposure to various aspects of neurosurgery. The variations in exposure reported by different respondents also point to potential areas of action for CPSP to ensure a standardized training experience for all trainees across Pakistan. A solution could be the sharing of resources across institutes, within Pakistan, where trainees of one hospital can pursue rotations at other centers which may have higher loads of subspecialty surgeries. Additionally, the participants’ attitude to pursuing fellowships outside Pakistan can help train surgeons in the underserved subspecialties in Pakistan, however, this carries the risk of contributing to the brain drain of young doctors from countries like Pakistan.30 Brain drain is a problem faced by several LMICs, and learning from their experiences, emphasis on improvement of training programs goes a long way.31 Therefore, if similar recognition and career development opportunities are provided, brain drain could be reduced.
We found a high ratio of individuals being satisfied with the mentorship available at their institute. Despite the lack of formal mentorship programs,32 this statistic provides insight into the informal mentorship available to neurosurgery trainees in Pakistan. However, this number may conceal findings about women and religious/ethnic minorities being deprived of quality mentorship.17,33
A high prevalence of burnout due to workload and working hours was reported in our survey. This has been commonly highlighted in literature as a concern for residents’ physical and mental health, especially for surgical specialty trainees.34 Burnout has been indicated as a cause of increased incidence of suicidal ideation, depressive symptoms, and cardiovascular disease.35 This finding of our study demands attention to investigate stressors for residents, and to find strategies to reduce workload and stress.
The recommendations generated from our study can be used to enhance programs, thereby supporting best practices and the highest caliber of graduates by standardizing training even more. For the training to advance and stay up to date with global standards, the programs must be standardized both locally and through collaboration with foreign counterparts.36 Partnerships within the country, particularly are not to be taken lightly, such as between the public and private sector can be beneficial, with the example of Khyber Pakhtunkhwa province, where both treatment and educational programs are being developed as joint ventures.37 All this should be undertaken with a multi-disciplinary effort in mind, which can be crucial in reducing disparities, where neurosurgery workforce shortages are prevalent.38
Limitations: It is important to acknowledge the limitations of this study. The self-reported nature of the data might introduce bias, and the cross-sectional design prevents the establishment of causal relationships. Additionally, the relatively small sample size and selection bias of sampling could limit the generalizability of our findings. Efforts were made to mitigate this bias through anonymous survey distribution and rigorous data analysis. However, it is important to acknowledge these limitations when interpreting the results.
5. Conclusion
Despite challenges stemming from economic constraints, political instability, and limited resources, there remains a strong interest among neurosurgery trainees in pursuing careers in the field. While training programs in Pakistan exhibit strengths, such as offering educational activities and conferences, there is room for improvement in terms of practical exposure, research mentorship, and standardized training experiences. Addressing the identified gaps and disparities can contribute to producing well-trained neurosurgeons who are equipped to address the complex healthcare needs of the population.
Supplementary Note
The questionnaire is available from the corresponding author on reasonable request.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Muhammad Shakir: Writing – review & editing, Supervision, Project administration, Methodology, Conceptualization. Hammad Atif Irshad: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision. Aly Hamza Khowaja: Writing – review & editing, Supervision, Project administration, Methodology, Conceptualization. Ahmed Altaf: Writing – review & editing, Writing – original draft, Investigation, Data curation. Syed Ather Enam: Writing – review & editing, Supervision, Project administration, Conceptualization.
Declaration of competing interest
The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article.
Acknowledgements
The authors express their gratitude to the Neurosciences Interest Group (NSIG) at the Aga Khan University and all data collectors for their support in disseminating our questionnaire.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.wnsx.2024.100346.
Appendix A. Supplementary data
The following is the Supplementary data to this article.
References
- 1.James C.D. Sir William Macewen. Proc R Soc Med. 1974;67(4):237–242. doi: 10.1177/003591577406700401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang X. [History of world neurosurgery] Zhonghua Yi Shi Za Zhi. 2017;47(3):160–164. doi: 10.3760/cma.j.issn.0255-7053.2017.03.006. [DOI] [PubMed] [Google Scholar]
- 3.Current health expenditure (% of GDP) - Pakistan | Data. Accessed September 8, 2023. https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS?locations=PK.
- 4.Kato Y., Liew B.S., Sufianov A.A., et al. Review of global neurosurgery education: horizon of neurosurgery in the developing countries. Chinese neurosurgical journal. 2020;6(3):178–190. doi: 10.1186/s41016-020-00194-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mukhopadhyay S., Punchak M., Rattani A., et al. The global neurosurgical workforce: a mixed-methods assessment of density and growth. J Neurosurg. 2019;130(4):1142–1148. doi: 10.3171/2018.10.JNS171723. [DOI] [PubMed] [Google Scholar]
- 6.Shamim M.S., Enam S.A., Kazim S.F. Neurosurgical research in Pakistan: Trends of publication and quality of evidence. Clin Neurol Neurosurg. 2011;113(2):107–110. doi: 10.1016/j.clineuro.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 7.shahzadshams. Training Programs - Best Neurosurgeon in Pakistan. Prof. Shahzad Shams. Published April 9, 2018. Accessed September 8, 2023. http://shahzadshams.com/training-programs.
- 8.University TAK. Residency-Neurosurgery | MC, Pakistan | The Aga Khan University. Accessed September 8, 2023. https://www.aku.edu/mcpk/residency/Pages/neurosurgery.aspx.
- 9.Ali N.U.A., Ali S., Sharif S., Amin F. Benchmarking of neurosurgery training in Pakistan. Asian Journal of Neurosurgery. 2021;16(2):300–306. doi: 10.4103/ajns.AJNS_426_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.College of Physicians and Surgeons Pakistan. Accessed September 8, 2023. https://www.cpsp.edu.pk/.
- 11.Imran N., Azeem Z., Haider, Amjad N., Bhatti M.R. Brain drain: post graduation migration intentions and the influencing factors among medical graduates from Lahore, Pakistan. BMC Res Notes. 2011;4(1):1–5. doi: 10.1186/1756-0500-4-417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.ain Ali N ul, Shaikh Y., Sharif S., Amin F. The challenges in neurosurgery training in a third world country. World Neurosurgery. 2021;152:19–23. doi: 10.1016/j.wneu.2021.04.118. [DOI] [PubMed] [Google Scholar]
- 13.Dean A.G. 2010. OpenEpi: Open Source Epidemiologic Statistics for Public Health. version 2.3. 1. Published online. [Google Scholar]
- 14.Peng M.Y.P., Yue X. Enhancing career Decision status of socioeconomically disadvantaged students through learning engagement: perspective of SOR model. Front Psychol. 2022;13 doi: 10.3389/fpsyg.2022.778928. https://www.frontiersin.org/articles/10.3389/fpsyg.2022.778928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shamim M.S., Tahir M.Z., Godil S.S., Kumar R., Siddiqui A.A. A critical analysis of the current state of neurosurgery training in Pakistan. Surg Neurol Int. 2011;2 doi: 10.4103/2152-7806.91138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Inam H., Janjua M., Martins R.S., et al. Cultural barriers for women in surgery: how Thick is the Glass Ceiling? An analysis from a low middle-income country. World J Surg. 2020;44(9):2870–2878. doi: 10.1007/s00268-020-05544-9. [DOI] [PubMed] [Google Scholar]
- 17.Mahendran G.N., Walker E.R., Bennett M., Chen A.Y. Qualitative study of mentorship for women and minorities in surgery. J Am Coll Surg. 2022;234(3):253–261. doi: 10.1097/XCS.0000000000000059. [DOI] [PubMed] [Google Scholar]
- 18.Schlick C.J.R., Ellis R.J., Etkin C.D., et al. Experiences of gender discrimination and sexual harassment among residents in general surgery programs across the US. JAMA surgery. 2021;156(10):942–952. doi: 10.1001/jamasurg.2021.3195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ferrari L., Mari V., Parini S., et al. Discrimination toward women in surgery: a systematic scoping review. Ann Surg. 2022;276(1):1–8. doi: 10.1097/SLA.0000000000005435. [DOI] [PubMed] [Google Scholar]
- 20.Greene J.R.T. Design and development of a new facility for teaching and research in clinical anatomy. Anat Sci Educ. 2009;2(1):34–40. doi: 10.1002/ase.70. [DOI] [PubMed] [Google Scholar]
- 21.Signorelli F., Stumpo V., Della Pepa G.M., et al. Step-up establishment of neurosurgical laboratory Starting with limited resources—Tips and Tricks. World neurosurgery. 2019;126:83–89. doi: 10.1016/j.wneu.2019.02.034. [DOI] [PubMed] [Google Scholar]
- 22.Del Valle M.M., De Jesus O., Vicenty-Padilla J.C., Matos A., Inserni J. Development of a neurosurgical cadaver laboratory despite limited resources. Puert Rico Health Sci J. 2022;41(3):153–156. [PMC free article] [PubMed] [Google Scholar]
- 23.Liu J.K., Kshettry V.R., Recinos P.F., Kamian K., Schlenk R.P., Benzel E.C. Establishing a surgical skills laboratory and dissection curriculum for neurosurgical residency training. J Neurosurg. 2015;123(5):1331–1338. doi: 10.3171/2014.11.JNS14902. [DOI] [PubMed] [Google Scholar]
- 24.Fuller A., Tran T., Muhumuza M., Haglund M.M. Building neurosurgical capacity in low and middle income countries. Eneurologicalsci. 2016;3:1–6. doi: 10.1016/j.ensci.2015.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hoz S.S., Al-Sharshahi Z.F., Esene I.N., et al. More laboratory simulations—fewer brain complications: prospects from the first neurosurgery laboratory in Iraq. World Neurosurgery. 2022;157:30–34. doi: 10.1016/j.wneu.2021.09.087. [DOI] [PubMed] [Google Scholar]
- 26.Khan H., Khan S., Iqbal A. Knowledge, attitudes and practices around health research: the perspective of physicians-in-training in Pakistan. BMC Med Educ. 2009;9:1–8. doi: 10.1186/1472-6920-9-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Martins R.S., Ukrani R.D., Raza Raja M.H., et al. Peer-taught virtual research workshops for surgical residents: Protocol for a novel and sustainable solution to improving surgical research in Pakistan. JPMA The Journal of the Pakistan Medical Association. 2021;71(1):S130. Suppl 1. [PubMed] [Google Scholar]
- 28.Reulen H.J. The role of research in the training of residents. Eur Surg Res. 2002;34(1–2):13–17. doi: 10.1159/000048881. [DOI] [PubMed] [Google Scholar]
- 29.Zafar S.N., McQueen K.K. Surgery, public health, and Pakistan. World J Surg. 2011;35:2625–2634. doi: 10.1007/s00268-011-1304-3. [DOI] [PubMed] [Google Scholar]
- 30.Adovor E., Czaika M., Docquier F., Moullan Y. Medical brain drain: how many, where and why? J Health Econ. 2021;76 doi: 10.1016/j.jhealeco.2020.102409. [DOI] [PubMed] [Google Scholar]
- 31.Lund-Johansen M., Dahl J.W., Eilertsen G.M., Wester K. Tidsskrift for Den norske legeforening; 2017. Establishment of Neurosurgery Training in Ethiopia. Published online. [DOI] [PubMed] [Google Scholar]
- 32.Begum S., Khan M.R., Safa M. 2021. Mentorship in Surgical Training: Where Do We Stand? Published Online. [PubMed] [Google Scholar]
- 33.Abdou S.A., Sharif-Askary B., Sayyed A.A., et al. Can mentorship Shatter the Glass Ceiling in academic Microsurgery? A national survey of Microsurgery fellowship-trained women in academia. Plast Reconstr Surg. 2023:10–1097. doi: 10.1097/PRS.0000000000010570. Published online. [DOI] [PubMed] [Google Scholar]
- 34.Rodrigues H., Cobucci R., Oliveira A., et al. Burnout syndrome among medical residents: a systematic review and meta-analysis. PLoS One. 2018;13(11) doi: 10.1371/journal.pone.0206840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nene Y., Tadi P. StatPearls. StatPearls Publishing. 2023. Resident burnout.http://www.ncbi.nlm.nih.gov/books/NBK553176/ [PubMed] [Google Scholar]
- 36.Ormond D.R., Kahamba J., Lillehei K.O., Rutabasibwa N. Overcoming barriers to neurosurgical training in Tanzania: international exchange, curriculum development, and novel methods of resource utilization and subspecialty development. Neurosurg Focus. 2018;45(4):E6. doi: 10.3171/2018.7.FOCUS18239. [DOI] [PubMed] [Google Scholar]
- 37.Khan T., Wahjoepramono E., Wahjoepramono P., Andrews R. Private healthcare initiatives in developing countries–Building sustainable neurosurgery in Indonesia and Pakistan. Brain and Spine. 2023;3 doi: 10.1016/j.bas.2023.101729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wicaksono A.S., Tamba D.A., Sudiharto P., et al. Neurosurgery residency program in Yogyakarta, Indonesia: improving neurosurgical care distribution to reduce inequality. Neurosurgical Focus FOC. 2020;48(3):E5. doi: 10.3171/2019.12.FOCUS19831. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.