Summary
Background
Prevention and control of non-communicable diseases (NCDs) are prioritized in both the Sustainable Development Goal and the Healthy China 2030 Initiatives. Efforts have been devoted to combating NCDs in China. This study examined changes in NCD trajectory.
Methods
We described and analyzed the trends in prevalence and control of major NCDs including obesity, hypertension, diabetes, and dyslipidemia and examined selected main behavioral risk factors in China by sex, age group, and residence using nationally representative CDC survey data. Data included were from the China Chronic Disease Risk Factor Surveillance (CCDRFS, 2013 and 2018) and China National Nutrition Survey (CNNS, 2002, 2010–2013, 2015, and 2020). Annual and relative changes in rates were used. Rural-urban ratio of related indicators was assessed.
Findings
NCD-attributed deaths increased from 80.0% in 2002 to 86.6% in 2012, and 88.5% in 2019, with cardiovascular diseases, cancer, chronic respiratory diseases, and diabetes accounted for 47.1%, 24.1%, 8.8%, and 2.5% of deaths in 2019, respectively. Prevalence of obesity (7.1%–16.4%), overweight/obesity (29.9%–50.7%), hypertension (18.8%–27.5%), diabetes (2.6%–11.9%), and dyslipidemia (18.6%–35.6%) all increased from 2002 to 2018. These rates increased faster in rural areas than in urban areas. Rates of awareness, treatment and control of hypertension and diabetes increased very slowly from 2012 to 2018. Most rates were between 30 and 40% with the lowest rate of 11% for hypertension control even in 2018. The rates were worse for rural residents compared to urban residents. Furthermore, many modifiable behavioral risk factors showed little improvement and some became worse over time, including smoking, excessive alcohol use, inadequate vegetable/fruit intake, excessive red meat intake, and physical inactivity.
Interpretation
NCD burden in China increased during 2002–2019 despite of the intervention efforts. To reach the global and national targets, China must strengthen its actions, especially in rural areas, including improvement of NCD screening and management and reduction of behavioral risk factors.
Funding
The study was supported in part by research grants of National Key R&D Program of China (2017YFC0907200, 2017YFC0907201), International Collaboration Project from the Chinese Ministry of Science and Technology-Prevention and control of chronic diseases and health promotion (G2021170007L), Natural Scientific Foundation of China (82103846), Key R&D and Transformation Program of Qinghai (2023-QY-204).
Keywords: Non-communicable diseases, Obesity, Hypertension, Diabetes, Dyslipidemia, Prevalence, Control, Behavioral risk factors, Trends
Research in context.
Evidence before this study
In the past decades, China has seen steady increase in NCD burden. Demographic transition towards aging and shifts in lifestyle factors are important drivers of the increase in NCDs. Substantial efforts have been devoted to combating NCDs in China. It is unclear how the NCDs burden has changed, and what the trend would be in the future.
Added value of this study
This study provided updated, most comprehensive, and nationally representative data on NCD trends in China, from modifiable risk factors to the prevalence, control, and ultimate endpoint health outcome of mortality rates. The comparison of the projected prevalence and treatment with the global and national goals also delivered important messages. Notably, residents in rural areas had been and would be increasingly and more adversely affected. These findings provided information much needed for policy development and preparedness to face NCD challenges.
Implications of all the available evidence
The NCD burden in China is high, has increased from 2002 to 2018, and is likely continue to increase in near future. There was no significant improvement in NCD management or behavioral risk factors during the period. China may fail to reach the global and national targets against NCDs unless more effective measures are taken.
Introduction
Prevention and control of the non-communicable diseases (NCDs) are health priorities both globally and in China. The Target 3.4 of the Sustainable Development Goal (SDG) is to reduce the premature NCD mortality by one-third by 2030.1 The World Health Organization (WHO) also released the Global Action Plan 2013–2020 as a road map for the prevention and control of NCDs.2 Cardiovascular diseases, cancer, chronic respiratory diseases, and diabetes are considered the four major NCDs in the WHO NCD framework for prevention and treatment.3
In the past decades, NCD burden increased rapidly in low-and-middle income countries (LMICs) including in China. According to the Global Burden of Disease (GBD) Study, NCDs accounted for 56.8% of total deaths in LMICs in 1990, and it increased to 74.4% in 2019. The disability-adjusted life years (DALYs) attributed to NCDs in LMICs increased from 37.8% to 66.0% during the same period.4 Worldwide, approximately three quarters of all NCD deaths, and 82% of the 16 million people who died prematurely (30–70 years old), occurred in LMICs.5
In China, our previous studies suggested an alarmingly increase in obesity and NCDs from 1992 to 2012.6,7 Demographic transition towards the aging and shifts in lifestyle factors are considered important drivers for the increased NCDs.8 China released The Healthy China Initiatives in 2016. The healthy lifestyle promotion and behavioral changes, which are the most important modifiable determinants of NCDs, are considered key points in the initiatives.9 In the Healthy China Action Plan 2019–2030, 15 special action plans are proposed, of which 14 are closely related to NCD prevention and control.10 In spite of these rigorous efforts, it is unclear whether the trajectory of NCDs has changed in China, and how it will develop in the future.
To gauge the NCD epidemic and control in China, this study described and analyzed the trends in the prevalence and control rates of major NCDs, including obesity, hypertension, diabetes, and dyslipidemia, as well as the key behavioral risk factors using the most updated nationally representative CDC survey data. The research findings will provide essential information for future health policies and intervention programs.
Methods
Data sources
We searched and reviewed all published national survey reports and original studies in academic journals that conducted by the Chinese Diseases Control and Prevention Center (CDC) and contained data related to NCD prevalence and control in China in the past 20 years. PubMed and China National Knowledge Infrastructure databases were searched for studies published from January 2002 to October 2022. Several key terms were used in search, including “China”, “NCDs”, “non communicable diseases”, “overweight”, “obesity”, “hypertension”, “diabetes”, “dyslipidemia”, “mortality”, “prevalence”, “management", etc. Titles and abstracts of relevant reports or studies (391 papers) were examined first, and the full text (114 papers) was obtained and reviewed. The references of important publications were also cross-checked for potential data source. In addition, several studies coming to our attention brought by experts that we consulted were included.
The following inclusion criteria were used for the selection of survey reports and original studies: 1) data collection was conducted by Chinese CDC using nationally representative samples for consistent study design and consistent definition of NCDs, which ensured good comparability of data across years; 2) participants were adults aged 18 years and older; 3) rates of the outcome measures were reported, including the prevalence rates of overweight and obesity, hypertension, diabetes, and dyslipidemia; rates of awareness, treatment and control of hypertension and diabetes, and prevalence rates of modifiable behavioral risk factors; and 4) the data were collected since 2002.
Of the total 391 retrieved documents, 17 original studies11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27 in academic journals and six national reports28, 29, 30, 31, 32, 33 met the inclusion criteria, and were summarized in Supplementary Table S1. A further study of these documents indicated that the 17 original studies published in journals defined the NCDs and behavioral risk factors inconsistently. Considering consistency in definition and comparability across years, we finally included the six national survey reports. The data in these reports were derived from the China Chronic Disease Risk Factor Surveillance (CCDRFS, 2013 and 2018) and China National Nutrition Survey (CNNS, 2002, 2010–2013, 2015, and 2020). Both CCDRFS and CNNS are nationally representative cross-sectional surveys among Chinese residents. Since the consistent study design and consistent definition of NCDs, the data extracted from the six reports were comparable to show the trends. Supplementary Figure S1 is the flowchart of the literature search and study selection.
Data extraction and study quality assessment
A study extraction form was created to extract information on study design, participants, age (years), survey year, diagnosed criteria, and outcomes. For national survey reports, we extracted study institution, type, and coverage additionally. Two investigators assessed the quality of included studies with the National Heart, Lung, and Blood Institute's Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. For the 14 criteria, each was assigned one score if the response was yes, otherwise zero score was assigned. The quality of studies was evaluated according to the sum of score: good, total score ≥7; fair, 4< total score ≤6; poor, total score ≤4. The quality assessment was detailed in Supplementary Table S2 and the PRISMA checklist was provided in Supplementary Table S3.
Study NCD outcomes
The NCD outcomes were pre-determined mainly based on the WHO NCD prevention and control framework, and the targets in the Healthy China Action Plan 2019–2030. The mortality rates of the four major NCDs in the WHO NCD framework were included. Of note, obesity, hypertension, diabetes, and dyslipidemia are identified as NCDs according to the International Classification of Diseases (ICD) from the WHO.34 Meanwhile, the WHO recognized overweight/obesity, raised blood pressure, raised blood glucose and raised cholesterol as the four key metabolic risk factors for NCDs.35 Thus, they can be seen as both NCDs and risk factors of NCDs by themselves depending on the context and the degree of the disorders. In this study, we defined them mainly as NCDs. The definitions were:
-
1)
Overweight was defined as 24≤ BMI <28 kg/m2, and obesity as BMI ≥28 kg/m2, based on the Chinese standard.36,37
-
2)
Hypertension was defined as systolic blood pressure (SBP) ≥140 mmHg and/or diastolic blood pressure (DBP) ≥90 mmHg, and/or those taking antihypertensive drugs within the past two weeks, according to the Chinese criteria.38
-
3)
Diabetes was defined as fasting plasma glucose ≥7.0 mmol/L and/or 2-h plasma glucose after a 75-g oral glucose challenge (OGTT-2h) ≥11.1 mmol/L, and/or had been diagnosed with diabetes by township/community-level or higher-level hospitals, according to the 1999 WHO criteria.39
-
4)
Dyslipidemia was defined as any or combinations of the four types of anormal lipid level, including high cholesterol (high TC), high triglyceride (high TG), high low-density lipoprotein cholesterol (high LDL-C), and low high-density lipoprotein cholesterol (low HDL-C). The respective diagnostic criteria included TC ≥ 6.22 mmol/L, TG ≥ 2.26 mmol/L, LDL-C ≥4.14 mmol/L, HDL-C <1.04 mmol/L.40
We also set the awareness, treatment, and control of hypertension and diabetes as outcomes. They are the monitoring indicators for targets in NCD prevention and control in China and in many other countries.
Selected NCD behavioral risk factors
The four major NCD behavioral risk factors defined by the WHO were used: tobacco use, unhealthy use of alcohol, poor diet, and inadequate physical activity, defined as41:
-
1)
Tobacco use: current smokers as the proxy, which were those who were still smoking at the time of the survey.
-
2)
Unhealthy use of alcohol: excessive drinking as the proxy, which was defined as an average daily alcohol intake of ≥41 g for men, and 21 g for women.
-
3)
Poor diet: inadequate vegetable/fruit intake and excessive red meat intake as proxy. Inadequate vegetable/fruit intake referred to an average daily intake <400 g; excessive red meat intake was regarded as an average daily intake of ≥100 g.
-
4)
Inadequate physical activity was defined as the total activity time in a week <150 min.
Statistical analysis
The rates of NCDs and related risk factors were extracted for all and stratified by sex (men vs. women), residence (urban vs. rural), and age groups (18–44 y, 45–59 y, 60+ y). Annual changes in rates were calculated as the absolute difference in these measures between the last and first year divided by the duration in years. In addition, relative change was used, and it was calculated as the absolute differences divided by the value in the first year. Last, rural-urban difference was assessed using a rural-urban ratio of related indicators.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
Overall, as indicated by the various measures collected in national representative surveys, NCD burden had increased in China during 2002–2018.
NCD mortality
The mortality rate of NCDs increased from 533.0 deaths per 100,000 people in 2012 to 685.0 in 2018. The percentage of deaths caused by NCDs was 80.0% in 2002, 86.6% in 2012 and 88.5% in 2018. Mortality among males was higher than that in females (Table 1). Deaths caused by cardiovascular diseases and cancer increased while chronic respiratory diseases declined.
Table 1.
Trends in NCD mortality rates and proportional mortality from NCDs in China, 2012 to 2018.
| 2012a | 2018a | Annual increase 2012–2018b | Relative increase 2012–2018c (%) | |
|---|---|---|---|---|
| A. Percentage of deaths due to NCDs (%) | 86.6 | 88.5 | 0.32 | 2.19 |
| Cardiovascular diseases | 44.4 | 47.1 | 0.45 | 6.08 |
| Cancer | 23.7 | 24.1 | 0.07 | 1.69 |
| Chronic respiratory diseases | 11.3 | 8.8 | −0.42 | −22.12 |
| Diabetes | – | 2.5 | – | – |
| Other NCDs | – | 6.0 | – | – |
| B. NCDs Mortality rates (/100,000) | ||||
| Overall | 533.0 | 685.0 | 25.33 | 28.52 |
| Men | 611.2 | 775.1 | 27.32 | 26.82 |
| Women | 452.6 | 592.1 | 23.25 | 30.82 |
| Cardiovascular diseases | ||||
| Overall | 271.8 | 364.6 | 15.47 | 34.14 |
| Men | 296.4 | 387.6 | 15.20 | 30.77 |
| Women | 246.4 | 340.8 | 15.73 | 38.31 |
| Cancer | ||||
| Overall | 144.3 | 186.5 | 7.03 | 29.24 |
| Men | 185.2 | 237.7 | 8.75 | 28.35 |
| Women | 102.2 | 133.7 | 5.25 | 30.82 |
| Chronic respiratory diseases | ||||
| Overall | 68.0 | 68.2 | 0.03 | 0.29 |
| Men | 76.7 | 80.0 | 0.55 | 4.30 |
| Women | 59.1 | 55.9 | −0.53 | −5.41 |
| Diabetesd | ||||
| Overall | 15.5 | 18.4 | 0.48 | 18.71 |
| Men | 14.4 | 18.1 | 0.62 | 25.69 |
| Women | 16.7 | 18.8 | 0.35 | 12.57 |
– Missing value.
Data were from the "Report on Nutrition and Chronic Disease Status of Chinese Residents (2015)" and "Report on Nutrition and Chronic Disease Status of Chinese Residents (2020)".
Annual increase was calculated as the absolute difference in these measures between the first and last year divided by the duration in years.
Relative increase was calculated as the absolute difference in these measures between the first and last year divided by the first-year value.
Data were from the reports of “2013 Health Statistics Yearbook in the People's Republic of China” and “2019 Health Statistics Yearbook in the People's Republic of China”, only for urban residents.
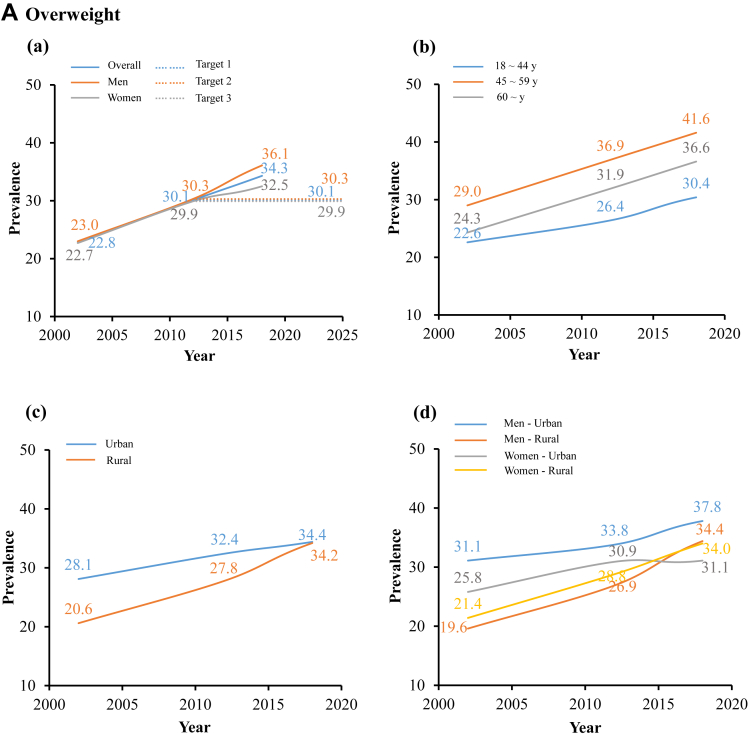
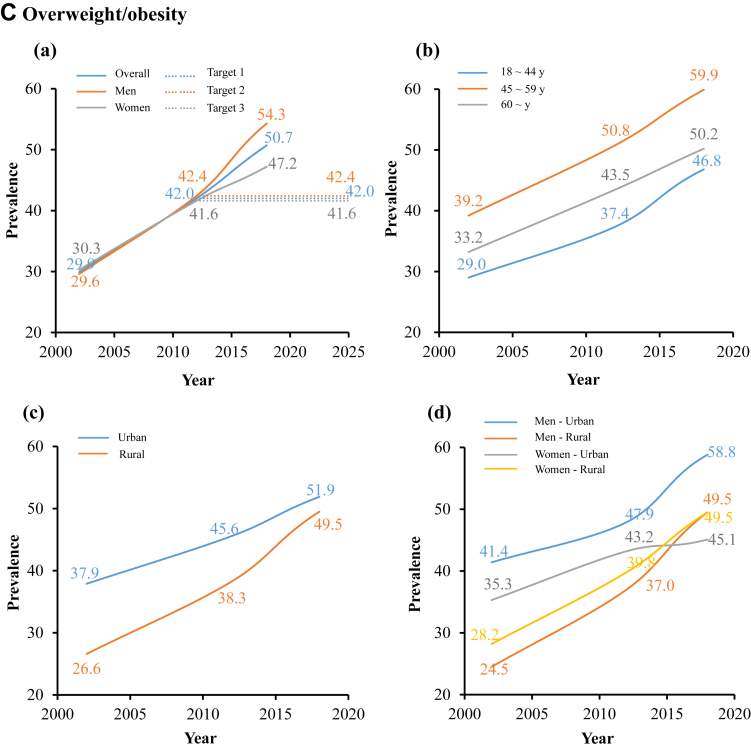
Obesity
From 2002 to 2018, the prevalence of obesity increased from 7.1% to 16.4%. In 2002, the obesity prevalence for men was lower than for women; but this pattern was reversed since 2012 (Fig. 1B a). In 2002, 2012, and 2018, obesity prevalence in the 45–59 y age group was higher than that in the 18–44 y and 60+ y age groups (Fig. 1B b). Prevalence of obesity in urban areas was higher than that in rural areas and the gap narrowed over time (Fig. 1B c). Moreover, the urban men had the highest obesity prevalence (Fig. 1B d). Similar trends were observed for the prevalence of overweight/obesity (ov/ob).
Fig. 1.
Trends in prevalence (%) of overweight and obesity in 2002–2018, adults 18 years and older, China. Overweight was defined as 24.0≤ BMI <28.0 kg/m2; obesity, as BMI ≥28.0 kg/m2. The data published in 2002, 2012 and 2018 were from the "Report on Nutrition and Chronic Diseases of Chinese Residents". The target values in 2030 were derived from the "Global Action Plan for the Prevention and Control of Non-communicable Diseases (2013–2020)” by WHO. Based on the 2013 data, the target is to halt the rise of the prevalence of overweight and obesity.
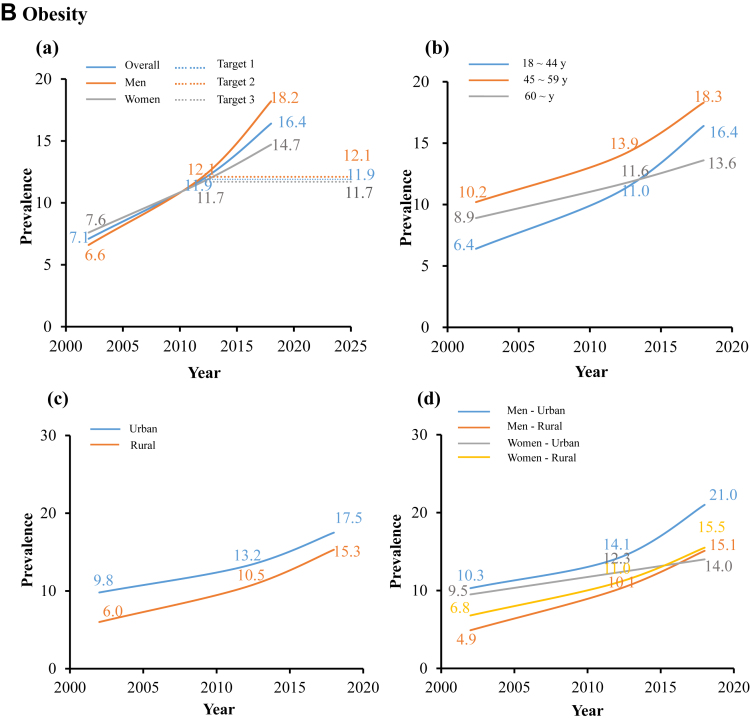
Hypertension
The prevalence of hypertension increased from 18.8% in 2002, to 25.2% in 2012, and further to 27.5% in 2018. The prevalence for men was higher than for women, and the gender-difference doubled from 2002 to 2018 (Fig. 2A a). The prevalence increased with age, and the age-specific prevalence also increased with time (Fig. 2A b). Hypertension was more prevalent in urban areas than in rural areas, except for 2018 (Fig. 2A c).
Fig. 2.
Trends in prevalence (%) of hypertension and diabetes in 2002–2018, adults 18 years and older, China. Hypertension was defined as SBP ≥140 mmHg or DBP ≥90 mmHg or taking antihypertensive drugs within the past two weeks. Diabetes was defined as fasting blood glucose ≥7.0 mmol/L or OGTT-2h ≥ 11.1 mmol/L or had been diagnosed with diabetes by physicians. The data published in 2002, 2012 and 2018 were from the “Report on Nutrition and Chronic Diseases of Chinese Residents”. The target values in 2030 were derived from the “Global Action Plan for the Prevention and Control of Non-communicable Diseases (2013–2020)” by WHO. Based on the 2013 data, the targets are to reduce the prevalence of hypertension by 25% and halt the rise of the prevalence of diabetes, respectively.
Overall, the awareness, treatment and control rates of hypertension increased by 10.8%, 10.2% and 4.9% from 2002 to 2018. The rates of awareness, treatment and control in men were lower than those in women and they were the highest in the 60+ y age group and the lowest in the 18–44 y age group. Also, the awareness, treatment, and control rates of hypertension in urban areas were higher than those in rural areas (Table 2).
Table 2.
Trends in rates (%) of treatment and control of hypertension among Chinese adults during 2002–2018.
| 2002a |
2012b |
2018–2019b |
Annual increase 2002–2018c |
2030 |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | Urban | Rural | Ratiod | Overall | Urban | Rural | Ratiod | Overall | Urban | Rural | Ratiod | Overall | Urban | Rural | Target valuee | |
| Awareness | ||||||||||||||||
| Overall | 30.2 | 41.1 | 22.5 | 1.83 | 38.2 | 41.2 | 34.6 | 1.19 | 41.0 | 43.1 | 39.0 | 1.11 | 0.68 | 0.13 | 1.03 | 65.0 |
| 18–44 y | 13.6 | 17.8 | 11.6 | 1.53 | 18.4 | 19.7 | 17.0 | 1.16 | 22.3 | 23.5 | 20.9 | 1.12 | 0.54 | 0.36 | 0.58 | |
| 45–59 y | 31.0 | 40.8 | 25.1 | 1.63 | 40.6 | 42.9 | 37.7 | 1.14 | 42.6 | 46.3 | 39.2 | 1.18 | 0.73 | 0.34 | 0.88 | |
| 60 y∼ | 37.6 | 48.5 | 26.8 | 1.81 | 48.5 | 52.9 | 43.5 | 1.22 | 53.4 | 58.1 | 49.7 | 1.17 | 0.99 | 0.60 | 1.43 | |
| Men | ||||||||||||||||
| Overall | 27.2 | 37.9 | 19.5 | 1.94 | 34.0 | 37.0 | 30.4 | 1.22 | 36.9 | 39.1 | 34.6 | 1.13 | 0.61 | 0.08 | 0.94 | 65.0 |
| 18–44 y | 11.1 | 16.3 | 8.4 | 1.94 | 16.2 | 17.3 | 14.9 | 1.16 | 21.6 | 21.8 | 21.3 | 1.02 | 0.66 | 0.34 | 0.81 | |
| 45–59 y | 26.8 | 36.5 | 20.9 | 1.75 | 37.5 | 41.2 | 32.4 | 1.27 | 40.1 | 44.6 | 35.6 | 1.25 | 0.83 | 0.51 | 0.92 | |
| 60 y∼ | 36.8 | 47.5 | 26.3 | 1.81 | 47.1 | 50.9 | 43.0 | 1.18 | 50.3 | 56.8 | 45.0 | 1.26 | 0.84 | 0.58 | 1.17 | |
| Women | ||||||||||||||||
| Overall | 33.1 | 44.1 | 25.3 | 1.74 | 43.1 | 46.2 | 39.5 | 1.17 | 46.2 | 48.9 | 44.0 | 1.11 | 0.82 | 0.30 | 1.17 | 65.0 |
| 18–44 y | 16.8 | 20.2 | 15.4 | 1.31 | 23.3 | 25.3 | 21.3 | 1.19 | 24.1 | 28.2 | 20.1 | 1.40 | 0.46 | 0.50 | 0.29 | |
| 45–59 y | 34.4 | 44.3 | 28.4 | 1.56 | 44.1 | 44.9 | 43.1 | 1.04 | 45.5 | 48.6 | 43.1 | 1.13 | 0.69 | 0.27 | 0.92 | |
| 60 y∼ | 38.4 | 49.5 | 27.2 | 1.82 | 49.7 | 54.7 | 43.9 | 1.25 | 56.2 | 59.3 | 53.8 | 1.10 | 1.11 | 0.61 | 1.66 | |
| Treatment | ||||||||||||||||
| Overall | 24.7 | 35.1 | 17.4 | 2.02 | 32.8 | 36.0 | 29.0 | 1.24 | 34.9 | 37.5 | 32.4 | 1.16 | 0.64 | 0.15 | 0.94 | Rising |
| 18–44 y | 9.1 | 11.8 | 7.9 | 1.49 | 13.9 | 15.1 | 12.5 | 1.21 | 16.6 | 17.7 | 15.2 | 1.16 | 0.47 | 0.37 | 0.46 | |
| 45–59 y | 25.0 | 34.1 | 19.4 | 1.76 | 34.3 | 36.6 | 31.2 | 1.17 | 36.1 | 40.3 | 32.3 | 1.25 | 0.69 | 0.39 | 0.81 | |
| 60 y∼ | 32.2 | 43.1 | 21.3 | 2.02 | 43.5 | 48.5 | 37.9 | 1.28 | 47.3 | 53.1 | 42.7 | 1.24 | 0.94 | 0.63 | 1.34 | |
| Men | ||||||||||||||||
| Overall | 21.6 | 31.2 | 14.7 | 2.12 | 28.4 | 31.4 | 24.7 | 1.27 | 30.8 | 33.5 | 27.9 | 1.20 | 0.58 | 0.14 | 0.83 | Rising |
| 18–44 y | 6.9 | 9.7 | 5.4 | 1.80 | 11.8 | 13.1 | 10.4 | 1.26 | 16.1 | 16.5 | 15.6 | 1.06 | 0.58 | 0.43 | 0.64 | |
| 45–59 y | 20.6 | 28.6 | 15.7 | 1.82 | 30.8 | 34.2 | 26.0 | 1.32 | 33.8 | 38.8 | 28.8 | 1.35 | 0.83 | 0.64 | 0.82 | |
| 60 y∼ | 31.0 | 41.5 | 20.7 | 2.00 | 41.5 | 45.8 | 36.9 | 1.24 | 43.5 | 51.2 | 37.4 | 1.37 | 0.78 | 0.61 | 1.04 | |
| Women | ||||||||||||||||
| Overall | 27.7 | 38.8 | 19.8 | 1.96 | 38.0 | 41.5 | 33.9 | 1.22 | 40.1 | 43.3 | 37.5 | 1.15 | 0.78 | 0.28 | 1.11 | Rising |
| 18–44 y | 12.0 | 15.0 | 10.8 | 1.39 | 18.4 | 19.9 | 16.9 | 1.18 | 17.8 | 21.1 | 14.5 | 1.46 | 0.36 | 0.38 | 0.23 | |
| 45–59 y | 28.5 | 38.5 | 22.3 | 1.73 | 38.1 | 39.4 | 36.5 | 1.08 | 38.8 | 42.2 | 36.0 | 1.17 | 0.64 | 0.23 | 0.86 | |
| 60 y∼ | 33.3 | 44.7 | 21.9 | 2.04 | 45.3 | 50.8 | 38.8 | 1.31 | 50.6 | 54.9 | 47.3 | 1.16 | 1.08 | 0.64 | 1.59 | |
| Control | ||||||||||||||||
| Overall | 6.1 | 9.7 | 3.5 | 2.77 | 10.4 | 12.5 | 8.0 | 1.56 | 11.0 | 13.6 | 8.5 | 1.60 | 0.31 | 0.24 | 0.31 | Rising |
| 18–44 y | 2.7 | 4.2 | 2.1 | 2.00 | 4.7 | 5.2 | 4.1 | 1.27 | 4.6 | 5.5 | 3.6 | 1.53 | 0.12 | 0.08 | 0.09 | |
| 45–59 y | 6.2 | 10.0 | 3.8 | 2.63 | 11.4 | 13.8 | 8.2 | 1.68 | 12.2 | 16.0 | 8.7 | 1.84 | 0.38 | 0.38 | 0.31 | |
| 60 y∼ | 7.6 | 11.3 | 3.9 | 2.90 | 13.1 | 15.5 | 10.4 | 1.49 | 14.6 | 18.7 | 11.3 | 1.65 | 0.44 | 0.46 | 0.46 | |
| Men | ||||||||||||||||
| Overall | 5.6 | 8.8 | 3.3 | 2.67 | 9.7 | 11.8 | 7.2 | 1.64 | 9.8 | 12.2 | 7.3 | 1.67 | 0.26 | 0.21 | 0.25 | Rising |
| 18–44 y | 1.9 | 2.7 | 1.5 | 1.80 | 4.1 | 4.9 | 3.1 | 1.58 | 4.3 | 4.9 | 3.3 | 1.48 | 0.15 | 0.14 | 0.11 | |
| 45–59 y | 5.3 | 8.2 | 3.6 | 2.28 | 11.0 | 13.6 | 7.4 | 1.84 | 11.6 | 15.3 | 7.7 | 1.99 | 0.39 | 0.44 | 0.26 | |
| 60 y∼ | 7.8 | 11.6 | 4.3 | 2.70 | 13.6 | 16.1 | 10.9 | 1.48 | 14.1 | 18.8 | 10.2 | 1.84 | 0.39 | 0.45 | 0.37 | |
| Women | ||||||||||||||||
| Overall | 6.5 | 10.6 | 3.6 | 2.94 | 11.3 | 13.3 | 8.9 | 1.49 | 12.5 | 15.6 | 9.9 | 1.58 | 0.38 | 0.31 | 0.39 | Rising |
| 18–44 y | 3.8 | 6.5 | 2.8 | 2.32 | 6.0 | 5.9 | 6.2 | 0.95 | 5.5 | 6.9 | 4.1 | 1.68 | 0.11 | 0.03 | 0.08 | |
| 45–59 y | 6.8 | 11.4 | 4.0 | 2.85 | 11.8 | 14.1 | 9.1 | 1.55 | 13.0 | 17.0 | 9.8 | 1.73 | 0.39 | 0.35 | 0.36 | |
| 60 y∼ | 7.3 | 11.0 | 3.6 | 3.06 | 12.7 | 15.0 | 9.9 | 1.52 | 15.0 | 18.7 | 12.2 | 1.53 | 0.48 | 0.48 | 0.54 | |
Hypertension was defined as SBP ≥140 mmHg or DBP ≥90 mmHg or taking antihypertensive drugs within the past two weeks. Treatment rate: the proportion of hypertensive patients who took antihypertensive drugs in the past two weeks to the total number of hypertensive patients. Control rate: the proportion of hypertensive patients whose blood pressure levels were controlled below 140/90 mmHg through treatment to the total number of hypertensive patients.
Data were from "Report on Nutrition and Chronic Disease Status of Chinese Residents (2015)".
Data were from "Report on Nutrition and Chronic Disease Status of Chinese Residents (2020)".
Annual increase was calculated as the absolute difference in these measures between the first and last year divided by the duration in years.
Ratio = Urban value/Rural value.
The 2030 target values were derived from the “Healthy China Action Plan 2019–2030”. The awareness rate had a specific target value of 65%, whilst the treatment and control rates had only an ambiguous target of continuously rising rates, without a specific target value. China would fail to reach its target in awareness rate based on the observed slow improvement.
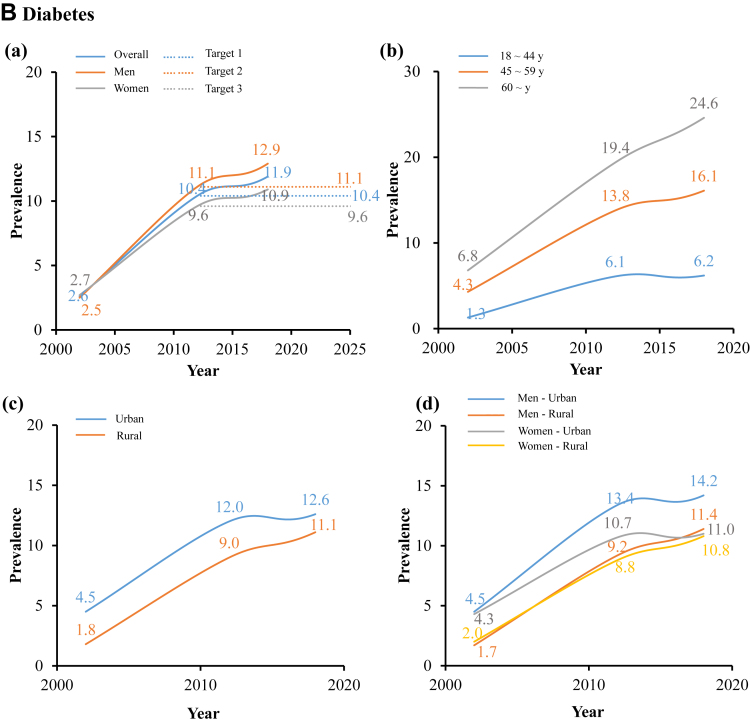
Diabetes
The prevalence of diabetes increased from 2.6% in 2002 to 11.9% in 2018. Prevalence of diabetes in men was lower than that in women in 2002, yet the condition reversed in 2013 and 2018 (Fig. 2B a). Compared with younger people, older adults had higher diabetes prevalence and faster growth rate (Fig. 2B b). The prevalence in urban areas was higher than that in rural areas while the difference was decreasing with time (Fig. 2B c).
The rates of awareness, treatment, and control of diabetes were on the rise in the past two decades, but remained very low in 2018. Men had a lower rate of management than women. For both men and women, the 60+ y age group had the highest diabetes awareness and treatment rate, followed by 45–59 y and 18–44 y age groups. Awareness and treatment rates of diabetes in urban areas were higher than rural areas in all 18–44 y, 45–59 y, and 60+ y age groups (Table 3).
Table 3.
Trends in rates (%) of treatment and control of diabetes among Chinese adults during 2012–2018.
| 2012a |
2018–2019a |
Annual increase 2012–2018b |
2030 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | Urban | Rural | Ratioc | Overall | Urban | Rural | Ratioc | Overall | Urban | Rural | Target valued | |
| Awareness | ||||||||||||
| Overall | 36.1 | 45.2 | 30.1 | 1.50 | 38.0 | 41.3 | 33.9 | 1.22 | 0.32 | −0.65 | 0.63 | 60.0 |
| 18–44 y | 27.7 | 36.6 | 22.9 | 1.60 | 23.4 | 25.3 | 20.3 | 1.25 | −0.72 | −1.88 | −0.43 | |
| 45–59 y | 37.8 | 44.9 | 32.5 | 1.38 | 41.5 | 45.6 | 36.7 | 1.24 | 0.62 | 0.12 | 0.70 | |
| 60 y∼ | 42.3 | 52.3 | 35.2 | 1.49 | 46.8 | 52.9 | 40.5 | 1.31 | 0.75 | 0.10 | 0.88 | |
| Men | ||||||||||||
| Overall | 35.3 | 44.9 | 28.7 | 1.56 | 33.6 | 37.6 | 28.3 | 1.33 | −0.28 | −1.22 | −0.07 | 60.0 |
| 18–44 y | 29.1 | 37.7 | 24.3 | 1.55 | 19.8 | 21.5 | 17.0 | 1.26 | −1.55 | −2.70 | −1.22 | |
| 45–59 y | 37.1 | 45.1 | 30.6 | 1.47 | 38.9 | 43.9 | 32.2 | 1.36 | 0.30 | −0.20 | 0.27 | |
| 60 y∼ | 40.5 | 52.1 | 32.2 | 1.62 | 42.4 | 49.8 | 34.0 | 1.46 | 0.32 | −0.38 | 0.30 | |
| Women | ||||||||||||
| Overall | 37.2 | 45.6 | 31.8 | 1.43 | 43.1 | 46.1 | 39.8 | 1.16 | 0.98 | 0.08 | 1.33 | 60.0 |
| 18–44 y | 25.5 | 34.7 | 20.7 | 1.68 | 28.8 | 31.2 | 25.1 | 1.24 | 0.55 | −0.58 | 0.73 | |
| 45–59 y | 38.7 | 44.7 | 34.7 | 1.29 | 44.9 | 48.2 | 41.6 | 1.16 | 1.03 | 0.58 | 1.15 | |
| 60 y∼ | 43.8 | 52.5 | 37.7 | 1.39 | 50.7 | 55.7 | 45.7 | 1.22 | 1.15 | 0.53 | 1.33 | |
| Treatment | ||||||||||||
| Overall | 33.4 | 41.8 | 27.9 | 1.50 | 34.1 | 37.5 | 29.9 | 1.25 | 0.12 | −0.72 | 0.33 | Rising |
| 18–44 y | 24.9 | 32.7 | 20.6 | 1.59 | 20.1 | 21.6 | 17.8 | 1.21 | −0.80 | −1.85 | −0.47 | |
| 45–59 y | 35.2 | 41.7 | 30.3 | 1.38 | 37.4 | 41.5 | 32.5 | 1.28 | 0.37 | −0.03 | 0.37 | |
| 60 y∼ | 39.6 | 49.0 | 32.8 | 1.49 | 42.5 | 49.1 | 35.5 | 1.38 | 0.48 | 0.02 | 0.45 | |
| Men | ||||||||||||
| Overall | 32.5 | 40.8 | 26.8 | 1.52 | 30.0 | 34.2 | 24.4 | 1.40 | −0.42 | −1.10 | −0.40 | Rising |
| 18–44 y | 26.2 | 33.8 | 22.0 | 1.54 | 17.6 | 19.3 | 14.8 | 1.30 | −1.43 | −2.42 | −1.20 | |
| 45–59 y | 34.2 | 41.2 | 28.6 | 1.44 | 34.6 | 39.5 | 27.9 | 1.42 | 0.07 | −0.28 | −0.12 | |
| 60 y∼ | 37.9 | 47.6 | 31.0 | 1.54 | 38.1 | 46.3 | 28.9 | 1.60 | 0.03 | −0.22 | −0.35 | |
| Women | ||||||||||||
| Overall | 34.6 | 43.0 | 29.1 | 1.48 | 38.8 | 41.7 | 35.7 | 1.17 | 0.70 | −0.22 | 1.10 | Rising |
| 18–44 y | 22.7 | 31.0 | 18.4 | 1.68 | 23.9 | 25.2 | 22.1 | 1.14 | 0.20 | −0.97 | 0.62 | |
| 45–59 y | 36.4 | 42.5 | 32.4 | 1.31 | 41.1 | 44.6 | 37.6 | 1.19 | 0.78 | 0.35 | 0.87 | |
| 60 y∼ | 40.9 | 50.2 | 34.4 | 1.46 | 46.3 | 51.7 | 40.9 | 1.26 | 0.90 | 0.25 | 1.08 | |
| Control | ||||||||||||
| Overall | 30.6 | 30.5 | 30.7 | 0.99 | 33.1 | 33.5 | 32.5 | 1.03 | 0.42 | 0.50 | 0.30 | Rising |
| 18–44 y | 27.1 | 26.5 | 27.4 | 0.97 | 32.9 | 35.0 | 29.5 | 1.19 | 0.97 | 1.42 | 0.35 | |
| 45–59 y | 27.8 | 28.1 | 27.5 | 1.02 | 29.1 | 29.6 | 28.4 | 1.04 | 0.22 | 0.25 | 0.15 | |
| 60 y∼ | 37.1 | 36.5 | 37.6 | 0.97 | 37.3 | 36.0 | 38.5 | 0.94 | 0.03 | −0.08 | 0.15 | |
| Men | ||||||||||||
| Overall | 28.9 | 28.5 | 29.2 | 0.98 | 31.5 | 31.3 | 31.6 | 0.99 | 0.43 | 0.47 | 0.40 | Rising |
| 18–44 y | 24.5 | 24.3 | 24.6 | 0.99 | 30.8 | 32.1 | 28.8 | 1.11 | 1.05 | 1.30 | 0.70 | |
| 45–59 y | 27.8 | 27.2 | 28.3 | 0.96 | 27.7 | 28.1 | 27.3 | 1.03 | −0.02 | 0.15 | −0.17 | |
| 60 y∼ | 36.0 | 35.0 | 36.7 | 0.95 | 36.7 | 34.7 | 39.0 | 0.89 | 0.12 | −0.05 | 0.38 | |
| Women | ||||||||||||
| Overall | 32.6 | 36.0 | 32.4 | 1.11 | 35.0 | 36.4 | 33.5 | 1.09 | 0.40 | 0.07 | 0.18 | Rising |
| 18–44 y | 31.2 | 28.6 | 31.7 | 0.90 | 36.0 | 39.7 | 30.6 | 1.30 | 0.80 | 1.85 | −0.18 | |
| 45–59 y | 27.7 | 33.4 | 26.6 | 1.26 | 30.8 | 32.1 | 29.5 | 1.09 | 0.52 | −0.22 | 0.48 | |
| 60 y∼ | 38.1 | 42.0 | 38.3 | 1.10 | 37.7 | 37.3 | 38.2 | 0.98 | −0.07 | −0.78 | −0.02 | |
Diabetes was defined as fasting blood glucose ≥7.0 mmol/L or OGTT-2h ≥11.1 mmol/L or had been diagnosed with diabetes by township/community level or above hospitals. Treatment rate: the proportion of diabetic patients who took lifestyle interventions or medication to the total number of diabetic patients. Control rate: the proportion of diabetic patients whose fasting blood glucose was controlled at or below 7.0 mmol/L to the total number of diabetic patients.
Data were from "Report on Nutrition and Chronic Disease Status of Chinese Residents (2020)".
Annual increase was calculated as the absolute difference in these measures between the first and last year divided by the duration in years.
Ratio = Urban value/Rural value.
The 2030 target values were derived from the “Healthy China Action Plan 2019–2030”. The awareness rate had a specific target value of 60%, whilst the treatment and control rates had only an ambiguous target of continuously rising rates, without a specific target value. China would fail to reach its target in awareness rate based on the observed slow improvement.
Dyslipidemia
The prevalence rates of dyslipidemia were 18.6%, 40.4%, 35.6% in 2002, 2012 and 2018, respectively. The prevalence rates of high TC, high TG and high LDL-C raised from 2.9%, 11.9% and 2.5% in 2002 to 8.2%, 18.4% and 8.0% in 2018, respectively. Compared to women, men had higher prevalence rates of dyslipidemia, high TG and low HDL-C. Prevalence of high TC and high LDL-C increased with age. Dyslipidemia and high TG prevalence only rose with age in women (Table 4).
Table 4.
Trends in prevalence (%) of dyslipidemia among Chinese adults during 2002–2018.
| 2002a |
2012b |
2018–2019c |
Annual increase 2002–2018d |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | Urban | Rural | Ratioe | Overall | Urban | Rural | Ratioe | Overall | Urban | Rural | Ratioe | Overall | Urban | Rural | |
| Dyslipidemia | |||||||||||||||
| Overall | 18.6 | 21.0 | 17.7 | 1.19 | 40.4 | 39.9 | 40.8 | 0.98 | 35.6 | 36.5 | 34.6 | 1.05 | 1.06 | 0.97 | 1.06 |
| 18–44 y | 17.0 | 17.8 | 16.6 | 1.07 | 38.9 | 37.4 | 40.3 | 0.93 | 33.2 | 33.6 | 32.7 | 1.03 | 1.01 | 0.99 | 1.01 |
| 45–59 y | 22.9 | 29.0 | 20.6 | 1.41 | 43.3 | 43.7 | 42.9 | 1.02 | 40.3 | 42.1 | 38.6 | 1.09 | 1.09 | 0.82 | 1.13 |
| 60 y∼ | 23.4 | 30.5 | 20.8 | 1.47 | 40.8 | 41.8 | 39.6 | 1.06 | 36.4 | 39.2 | 34.2 | 1.15 | 0.81 | 0.54 | 0.84 |
| Men | |||||||||||||||
| Overall | 22.2 | 27.2 | 20.1 | 1.35 | 47.0 | 48.4 | 45.7 | 1.06 | 44.1 | 47.3 | 40.7 | 1.16 | 1.37 | 1.26 | 1.29 |
| 18–44 y | 23.3 | 27.4 | 21.5 | 1.27 | 48.6 | 49.5 | 47.9 | 1.03 | 46.3 | 48.5 | 43.6 | 1.11 | 1.44 | 1.32 | 1.38 |
| 45–59 y | 23.9 | 32.3 | 20.7 | 1.56 | 47.8 | 50.1 | 45.1 | 1.11 | 46.0 | 49.5 | 42.6 | 1.16 | 1.38 | 1.08 | 1.37 |
| 60 y∼ | 23.4 | 30.5 | 20.8 | 1.47 | 39.8 | 41.6 | 37.8 | 1.10 | 33.6 | 37.9 | 30.2 | 1.25 | 0.64 | 0.46 | 0.59 |
| Women | |||||||||||||||
| Overall | 15.9 | 16.3 | 15.7 | 1.04 | 33.5 | 31.3 | 35.7 | 0.88 | 27.1 | 25.7 | 28.6 | 0.90 | 0.70 | 0.59 | 0.81 |
| 18–44 y | 11.6 | 10.0 | 12.4 | 0.81 | 28.7 | 24.9 | 32.2 | 0.77 | 20.1 | 18.6 | 21.9 | 0.85 | 0.53 | 0.54 | 0.59 |
| 45–59 y | 22.1 | 26.3 | 20.4 | 1.29 | 38.7 | 37.1 | 40.6 | 0.91 | 34.6 | 34.6 | 34.7 | 1.00 | 0.78 | 0.52 | 0.89 |
| 60 y∼ | 26.4 | 33.5 | 23.8 | 1.41 | 41.7 | 42.0 | 41.4 | 1.01 | 39.1 | 40.4 | 38.1 | 1.06 | 0.79 | 0.43 | 0.89 |
| High cholesterol | |||||||||||||||
| Overall | 2.9 | 4.1 | 2.4 | 1.71 | 4.9 | 5.6 | 4.3 | 1.30 | 8.2 | 8.1 | 8.3 | 0.98 | 0.33 | 0.25 | 0.37 |
| 18–44 y | 1.8 | 2.1 | 1.6 | 1.31 | 2.9 | 2.9 | 2.8 | 1.04 | 5.5 | 5.8 | 5.1 | 1.14 | 0.23 | 0.23 | 0.22 |
| 45–59 y | 4.7 | 7.0 | 3.9 | 1.79 | 7.1 | 8.0 | 6.1 | 1.31 | 11.2 | 11.1 | 11.4 | 0.97 | 0.41 | 0.26 | 0.47 |
| 60 y∼ | 6.1 | 10.6 | 4.5 | 2.36 | 8.6 | 9.9 | 7.3 | 1.36 | 12.7 | 12.7 | 12.7 | 1.00 | 0.41 | 0.13 | 0.51 |
| Men | |||||||||||||||
| Overall | 2.7 | 3.7 | 2.3 | 1.61 | 4.7 | 5.1 | 4.3 | 1.19 | 8.4 | 8.6 | 8.2 | 1.05 | 0.36 | 0.31 | 0.37 |
| 18–44 y | 2.3 | 2.7 | 2.2 | 1.23 | 3.9 | 4.1 | 3.7 | 1.11 | 7.2 | 7.8 | 6.5 | 1.20 | 0.31 | 0.32 | 0.27 |
| 45–59 y | 4.0 | 6.0 | 3.2 | 1.88 | 6.2 | 6.7 | 5.7 | 1.18 | 10.8 | 10.4 | 11.2 | 0.93 | 0.43 | 0.28 | 0.50 |
| 60 y∼ | 4.0 | 7.0 | 2.9 | 2.41 | 5.3 | 5.8 | 4.7 | 1.23 | 8.7 | 8.9 | 8.5 | 1.05 | 0.29 | 0.12 | 0.35 |
| Women | |||||||||||||||
| Overall | 3.2 | 4.6 | 2.6 | 1.77 | 5.1 | 6.0 | 4.2 | 1.43 | 8.0 | 7.6 | 8.5 | 0.89 | 0.30 | 0.19 | 0.37 |
| 18–44 y | 1.3 | 1.7 | 1.2 | 1.42 | 1.8 | 1.8 | 1.9 | 0.95 | 3.8 | 3.8 | 3.8 | 1.00 | 0.16 | 0.13 | 0.16 |
| 45–59 y | 5.4 | 7.9 | 4.5 | 1.76 | 8.1 | 9.4 | 6.5 | 1.45 | 11.7 | 11.8 | 11.6 | 1.02 | 0.39 | 0.24 | 0.44 |
| 60 y∼ | 8.3 | 14.2 | 6.2 | 2.29 | 11.8 | 13.8 | 9.7 | 1.42 | 16.6 | 16.3 | 16.8 | 0.97 | 0.52 | 0.13 | 0.66 |
| High triglyceride | |||||||||||||||
| Overall | 11.9 | 14.2 | 10.9 | 1.30 | 13.1 | 14.1 | 12.2 | 1.16 | 18.4 | 18.8 | 17.9 | 1.05 | 0.41 | 0.29 | 0.44 |
| 18–44 y | 10.9 | 12.3 | 10.3 | 1.19 | 11.8 | 12.6 | 11.2 | 1.13 | 17.1 | 17.3 | 16.8 | 1.03 | 0.39 | 0.31 | 0.41 |
| 45–59 y | 15.7 | 20.4 | 13.9 | 1.47 | 16.5 | 17.6 | 15.0 | 1.17 | 22.0 | 23.0 | 21.1 | 1.09 | 0.39 | 0.16 | 0.45 |
| 60 y∼ | 14.8 | 20.5 | 12.6 | 1.63 | 12.4 | 13.4 | 11.4 | 1.18 | 17.1 | 18.2 | 16.3 | 1.12 | 0.14 | −0.14 | 0.23 |
| Men | |||||||||||||||
| Overall | 14.5 | 19.6 | 12.4 | 1.58 | 16.7 | 18.4 | 14.5 | 1.27 | 23.6 | 25.6 | 21.4 | 1.20 | 0.57 | 0.38 | 0.56 |
| 18–44 y | 16.0 | 20.4 | 14.0 | 1.46 | 17.2 | 19.1 | 15.5 | 1.23 | 25.6 | 27.0 | 23.8 | 1.13 | 0.60 | 0.41 | 0.61 |
| 45–59 y | 16.1 | 23.7 | 13.2 | 1.80 | 18.8 | 21.3 | 15.7 | 1.36 | 25.5 | 27.9 | 23.1 | 1.21 | 0.59 | 0.26 | 0.62 |
| 60 y∼ | 11.8 | 18.3 | 9.4 | 1.95 | 9.7 | 10.4 | 8.9 | 1.17 | 13.9 | 15.4 | 12.7 | 1.21 | 0.13 | −0.18 | 0.21 |
| Women | |||||||||||||||
| Overall | 9.9 | 10.1 | 9.8 | 1.03 | 9.8 | 9.8 | 9.7 | 1.01 | 13.2 | 12.0 | 14.4 | 0.83 | 0.21 | 0.12 | 0.29 |
| 18–44 y | 6.6 | 5.6 | 7.0 | 0.80 | 6.2 | 5.7 | 6.6 | 0.86 | 8.6 | 7.5 | 9.9 | 0.76 | 0.13 | 0.12 | 0.18 |
| 45–59 y | 15.5 | 17.8 | 14.6 | 1.22 | 14.0 | 13.7 | 14.3 | 0.96 | 18.5 | 17.9 | 19.0 | 0.94 | 0.19 | 0.01 | 0.28 |
| 60 y∼ | 17.7 | 22.8 | 15.8 | 1.44 | 15.0 | 16.1 | 13.9 | 1.16 | 20.3 | 20.8 | 19.8 | 1.05 | 0.16 | −0.13 | 0.25 |
| Low HDL-C | |||||||||||||||
| Overall | 7.4 | 7.1 | 7.5 | 0.95 | 33.9 | 32.8 | 35.0 | 0.94 | 20.9 | 22.3 | 19.4 | 1.15 | 0.84 | 0.95 | 0.74 |
| 18–44 y | 7.3 | 6.6 | 7.6 | 0.87 | 34.4 | 32.9 | 35.8 | 0.92 | 22.4 | 23.1 | 21.6 | 1.07 | 0.94 | 1.03 | 0.88 |
| 45–59 y | 7.2 | 7.9 | 6.9 | 1.14 | 34.2 | 33.4 | 35.1 | 0.95 | 20.6 | 22.4 | 18.9 | 1.19 | 0.84 | 0.91 | 0.75 |
| 60 y∼ | 7.0 | 6.7 | 7.1 | 0.94 | 31.4 | 31.5 | 31.4 | 1.00 | 16.4 | 19.1 | 14.2 | 1.35 | 0.59 | 0.78 | 0.44 |
| Men | |||||||||||||||
| Overall | 9.3 | 10.0 | 9.0 | 1.11 | 40.4 | 41.1 | 39.7 | 1.04 | 28.9 | 32.0 | 25.4 | 1.26 | 1.23 | 1.38 | 1.03 |
| 18–44 y | 9.7 | 10.2 | 9.4 | 1.09 | 42.7 | 43.0 | 42.4 | 1.01 | 32.6 | 34.8 | 29.8 | 1.17 | 1.43 | 1.54 | 1.28 |
| 45–59 y | 8.9 | 11.1 | 8.1 | 1.37 | 39.3 | 40.7 | 37.6 | 1.08 | 27.1 | 30.4 | 23.8 | 1.28 | 1.14 | 1.21 | 0.98 |
| 60 y∼ | 8.3 | 8.6 | 8.3 | 1.04 | 33.9 | 35.5 | 32.2 | 1.10 | 18.9 | 23.0 | 15.7 | 1.46 | 0.66 | 0.90 | 0.46 |
| Women | |||||||||||||||
| Overall | 5.4 | 4.3 | 5.9 | 0.73 | 27.1 | 24.3 | 30.0 | 0.81 | 13.0 | 12.6 | 13.5 | 0.93 | 0.48 | 0.52 | 0.48 |
| 18–44 y | 5.2 | 3.7 | 5.9 | 0.63 | 25.7 | 22.3 | 28.8 | 0.77 | 12.3 | 11.4 | 13.4 | 0.85 | 0.44 | 0.48 | 0.47 |
| 45–59 y | 5.8 | 5.3 | 5.9 | 0.90 | 28.9 | 25.9 | 32.5 | 0.80 | 14.1 | 14.2 | 14.0 | 1.01 | 0.52 | 0.56 | 0.51 |
| 60 y∼ | 5.7 | 4.9 | 6.0 | 0.82 | 29.1 | 27.7 | 30.5 | 0.91 | 13.9 | 15.3 | 12.8 | 1.20 | 0.51 | 0.65 | 0.43 |
| High LDL-C | |||||||||||||||
| Overall | 2.5 | 3.6 | 2.0 | 1.80 | 4.8 | 5.5 | 4.2 | 1.31 | 8.0 | 8.3 | 7.7 | 1.08 | 0.34 | 0.29 | 0.36 |
| 18–44 y | 1.3 | 1.8 | 1.1 | 1.64 | 2.7 | 2.8 | 2.7 | 1.04 | 5.5 | 6.1 | 4.7 | 1.30 | 0.26 | 0.27 | 0.23 |
| 45–59 y | 4.1 | 6.3 | 3.2 | 1.97 | 6.9 | 7.8 | 5.9 | 1.32 | 10.6 | 10.9 | 10.4 | 1.05 | 0.41 | 0.29 | 0.45 |
| 60 y∼ | 5.5 | 9.5 | 4.1 | 2.32 | 8.8 | 10.2 | 7.3 | 1.40 | 12.4 | 13.1 | 11.9 | 1.10 | 0.43 | 0.23 | 0.49 |
| Men | |||||||||||||||
| Overall | 2.3 | 3.3 | 1.9 | 1.74 | 4.6 | 5.0 | 4.1 | 1.22 | 8.1 | 8.7 | 7.6 | 1.14 | 0.36 | 0.34 | 0.36 |
| 18–44 y | 1.6 | 2.1 | 1.4 | 1.50 | 3.6 | 3.8 | 3.4 | 1.12 | 7.1 | 8.0 | 6.0 | 1.33 | 0.34 | 0.37 | 0.29 |
| 45–59 y | 3.4 | 5.3 | 2.7 | 1.96 | 5.9 | 6.4 | 5.3 | 1.21 | 9.8 | 9.7 | 9.9 | 0.98 | 0.40 | 0.28 | 0.45 |
| 60 y∼ | 4.0 | 7.1 | 2.9 | 2.45 | 6.0 | 6.7 | 5.2 | 1.29 | 9.2 | 10.0 | 8.6 | 1.16 | 0.33 | 0.18 | 0.36 |
| Women | |||||||||||||||
| Overall | 2.6 | 4.0 | 2.1 | 1.90 | 5.1 | 5.9 | 4.3 | 1.37 | 7.8 | 7.9 | 7.8 | 1.01 | 0.33 | 0.24 | 0.36 |
| 18–44 y | 1.1 | 1.5 | 0.9 | 1.67 | 1.9 | 1.8 | 2.0 | 0.90 | 3.9 | 4.2 | 3.5 | 1.20 | 0.18 | 0.17 | 0.16 |
| 45–59 y | 4.7 | 7.0 | 3.8 | 1.84 | 8.0 | 9.2 | 6.5 | 1.42 | 11.5 | 12.2 | 10.9 | 1.12 | 0.43 | 0.33 | 0.44 |
| 60 y∼ | 7.1 | 11.9 | 5.3 | 2.25 | 11.5 | 13.5 | 9.4 | 1.44 | 15.5 | 16.1 | 15.0 | 1.07 | 0.53 | 0.26 | 1.61 |
Dyslipidemia was defined as any combination of high cholesterol, high triglyceride, low HDL-C, and high LDL-C. High cholesterol: the serum cholesterol level ≥6.22 mmol/L. High triglyceride: the serum triglyceride level ≥2.26 mmol/L. Low HDL-C: the serum HDL-C level <1.04 mmol/L. High LDL-C: the serum LDL-C level ≥4.14 mmol/L.
Data were from "Comprehensive Report on the Survey of Nutrition and Health Status of Chinese Residents 2002" and "Comprehensive Report on the Monitoring of Nutrition and Health Status of Chinese Residents 2010–2013".
Data were from "Comprehensive Report on the Monitoring of Nutrition and Health Status of Chinese Residents 2010–2013", "Report on Nutrition and Chronic Disease Status of Chinese Residents (2015)", and "Report on Nutrition and Chronic Disease Status of Chinese Residents (2020)".
Data were from "Report on Nutrition and Chronic Disease Status of Chinese Residents (2020)".
Annual increase was calculated as the absolute difference in these measures between the first and last year divided by the duration in years.
Ratio = Urban value/Rural value.
Differences across groups
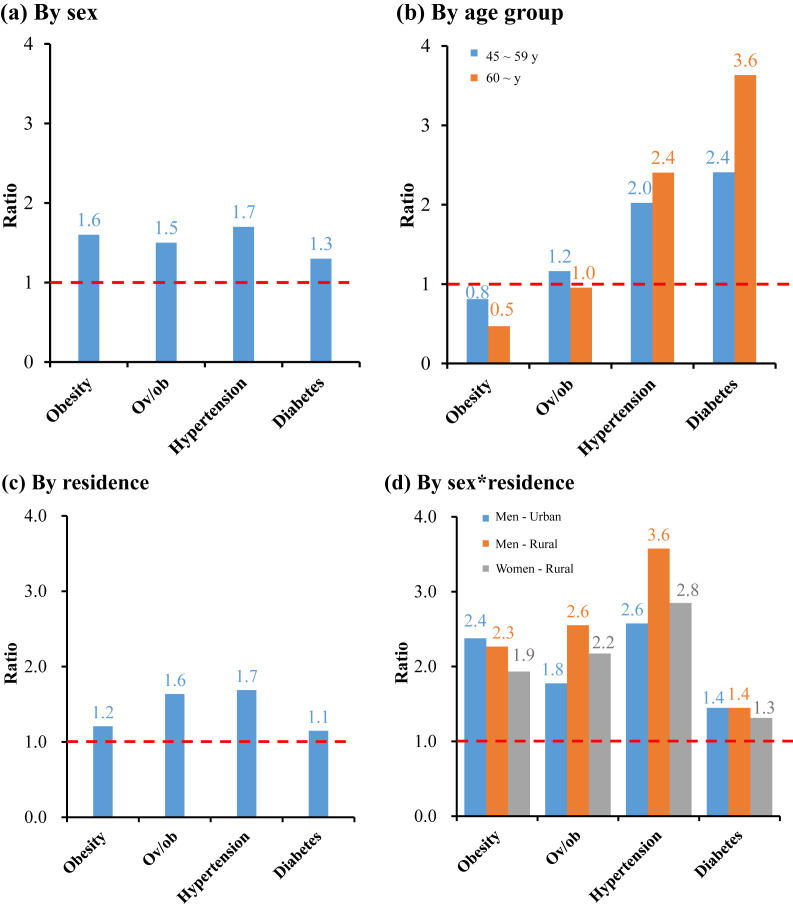
We further compared the increasing rates in prevalence of obesity, hypertension and diabetes by sex, age group, residence and the combination of sex and residence during 2002–2018 (Fig. 3). Men and rural residents had higher increasing rates in prevalence in all the three conditions than their counterparts, women and urban residents, respectively. In addition, urban women had the lowest increasing rates in all the conditions, while rural men had the highest increasing rate in hypertension, and urban men had the highest increasing rate in obesity.
Fig. 3.
Disparities (ratios) in increasing rates in prevalence (%) of obesity, hypertension and diabetes in 2002–2018. ov/ob = overweight and obesity. (a) Ref = Women; (b) Ref = 18–44 y; (c) Ref = Urban; (d) Ref = Women Urban. Ratio = Annual change/Annual change (ref). Annual change was calculated as the absolute difference in these measures between the first and last year divided by the duration in years. The red dotted line represented a ratio value of 1.
Behavioral risk factors
Over time, there were some improvements, but some became worse in these examined NCD behavioral risk factors. The current smoking rate slightly declined from 27.3% in 2013 to 26.2% in 2018. Men and rural residents had higher smoking rates than their counterparts, women and urban residents. Smoking rate also varied by age, with the highest rate among the 45–59 y age group. The rate of excessive drinking also displayed a decreasing trend from 2013 to 2018 with higher rate in men than in women. In 2013, 44–59 y age group had the highest excessive drinking rate, while in 2018, 60+ y age group peaked. The rates of inadequate vegetable/fruit intake declined, with slightly higher rate in men than women, and the highest rate for the 60+ y age group and the lowest in the 18–44 y age group.
Of concern, the rate of excessive red meat intake increased from 32.5% in 2013 to 42.0% in 2018 and declined with age. The rate of physical inactivity increased over time, with higher rate in men than in women and the lowest rate in 44–59 y age group (Table 5).
Table 5.
Prevalence (%) of NCD-related behavioral risk factors among Chinese adults during 2013–2018.
| 2013a |
2018a |
Annual increase 2013–2018b |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | Urban | Rural | Ratioc | Overall | Urban | Rural | Ratioc | Overall | Urban | Rural | |
| Current smokers | |||||||||||
| Overall | 27.3 | 25.1 | 29.2 | 0.86 | 26.2 | 24.3 | 28.2 | 0.86 | −0.22 | −0.16 | −0.20 |
| 18–44 y | 26.5 | 24.2 | 28.4 | 0.85 | 25.5 | 23.3 | 28.1 | 0.83 | −0.20 | −0.18 | −0.06 |
| 45–59 y | 31.0 | 29.6 | 32.1 | 0.92 | 29.3 | 28.7 | 29.8 | 0.96 | −0.34 | −0.18 | −0.46 |
| 60 y∼ | 24.7 | 21.0 | 27.4 | 0.77 | 24.2 | 21.4 | 26.4 | 0.81 | −0.10 | 0.08 | −0.20 |
| Men | |||||||||||
| Overall | 51.8 | 48.3 | 54.7 | 0.88 | 50.0 | 46.5 | 53.9 | 0.86 | −0.36 | −0.36 | −0.16 |
| 18–44 y | 50.9 | 47.0 | 54.2 | 0.87 | 48.9 | 44.6 | 54.3 | 0.82 | −0.40 | −0.48 | 0.02 |
| 45–59 y | 58.2 | 56.2 | 59.8 | 0.94 | 55.5 | 54.6 | 56.4 | 0.97 | −0.54 | −0.32 | −0.68 |
| 60 y∼ | 45.4 | 40.4 | 49.1 | 0.82 | 45.5 | 40.9 | 49.1 | 0.83 | 0.02 | 0.10 | 0.00 |
| Women | |||||||||||
| Overall | 2.3 | 2.1 | 2.4 | 0.88 | 2.1 | 1.8 | 2.4 | 0.75 | −0.04 | −0.06 | 0.00 |
| 18–44 y | 1.3 | 1.5 | 1.1 | 1.36 | 1.4 | 1.5 | 1.4 | 1.07 | 0.02 | 0.00 | 0.06 |
| 45–59 y | 2.8 | 2.8 | 2.8 | 1.00 | 2.4 | 2.0 | 2.8 | 0.71 | −0.08 | −0.16 | 0.00 |
| 60 y∼ | 4.7 | 3.3 | 5.8 | 0.57 | 3.7 | 2.9 | 4.4 | 0.66 | −0.20 | −0.08 | −0.28 |
| Excessive drinking | |||||||||||
| Overall | 16.0 | 13.8 | 18.1 | 0.76 | 14.3 | 11.9 | 17.2 | 0.69 | −0.34 | −0.38 | −0.18 |
| 18–44 y | 11.8 | 10.3 | 13.2 | 0.78 | 9.3 | 8.3 | 10.6 | 0.78 | −0.50 | −0.40 | −0.52 |
| 45–59 y | 23.0 | 20.2 | 25.6 | 0.79 | 20.9 | 17.5 | 24.5 | 0.71 | −0.42 | −0.54 | −0.22 |
| 60 y∼ | 21.5 | 18.2 | 24.2 | 0.75 | 24.5 | 19.9 | 28.4 | 0.70 | 0.60 | 0.34 | 0.84 |
| Men | |||||||||||
| Overall | 18.9 | 16.9 | 19.7 | 0.86 | 17.6 | 15.1 | 20.5 | 0.74 | −0.26 | −0.36 | 0.16 |
| 18–44 y | 14.1 | 12.8 | 15.3 | 0.84 | 11.6 | 10.5 | 12.8 | 0.82 | −0.50 | −0.46 | −0.50 |
| 45–59 y | 26.9 | 24.3 | 29.2 | 0.83 | 25.6 | 22.0 | 29.3 | 0.75 | −0.26 | −0.46 | 0.02 |
| 60 y∼ | 24.7 | 21.7 | 27.1 | 0.80 | 28.7 | 24.3 | 32.5 | 0.75 | 0.80 | 0.52 | 1.08 |
| Women | |||||||||||
| Overall | 4.7 | 4.1 | 5.6 | 0.73 | 3.7 | 3.1 | 4.7 | 0.66 | −0.20 | −0.20 | −0.18 |
| 18–44 y | 3.3 | 3.4 | 3.1 | 1.10 | 2.4 | 2.5 | 2.2 | 1.14 | −0.18 | −0.18 | −0.18 |
| 45–59 y | 6.4 | 5.3 | 7.8 | 0.68 | 4.5 | 3.7 | 5.7 | 0.65 | −0.38 | −0.32 | −0.42 |
| 60 y∼ | 8.9 | 6.3 | 11.5 | 0.55 | 9.1 | 5.3 | 12.8 | 0.41 | 0.04 | −0.20 | 0.26 |
| Inadequate vegetable/fruit intake | |||||||||||
| Overall | 46.8 | 44.0 | 49.2 | 0.89 | 44.7 | 38.7 | 51.2 | 0.76 | −0.42 | −1.06 | 0.40 |
| 18–44 y | 44.7 | 42.6 | 46.6 | 0.91 | 43.3 | 38.6 | 49.1 | 0.79 | −0.28 | −0.80 | 0.50 |
| 45–59 y | 46.5 | 44.2 | 48.4 | 0.91 | 43.6 | 36.8 | 50.0 | 0.74 | −0.58 | −1.48 | 0.32 |
| 60 y∼ | 54.5 | 49.1 | 58.6 | 0.84 | 51.1 | 41.8 | 58.4 | 0.72 | −0.68 | −1.46 | −0.04 |
| Men | |||||||||||
| Overall | 47.2 | 45.5 | 48.5 | 0.94 | 45.8 | 40.8 | 51.1 | 0.80 | −0.28 | −0.94 | 0.52 |
| 18–44 y | 45.6 | 44.4 | 46.6 | 0.95 | 45.4 | 41.5 | 50.1 | 0.83 | −0.04 | −0.58 | 0.70 |
| 45–59 y | 47.1 | 46.2 | 47.9 | 0.96 | 44.5 | 39.0 | 49.7 | 0.78 | −0.52 | −1.44 | 0.36 |
| 60 y∼ | 52.7 | 48.3 | 56.0 | 0.86 | 49.3 | 40.6 | 56.1 | 0.72 | −0.68 | −1.54 | 0.02 |
| Women | |||||||||||
| Overall | 46.5 | 42.6 | 49.8 | 0.86 | 43.6 | 36.5 | 51.2 | 0.71 | −0.58 | −1.22 | 0.28 |
| 18–44 y | 43.8 | 40.7 | 46.5 | 0.88 | 41.3 | 35.6 | 48.2 | 0.74 | −0.50 | −1.02 | 0.34 |
| 45–59 y | 45.8 | 42.2 | 49.0 | 0.86 | 42.6 | 34.6 | 50.3 | 0.69 | −0.64 | −1.52 | 0.26 |
| 60 y∼ | 56.1 | 49.7 | 61.2 | 0.81 | 52.8 | 43.0 | 60.6 | 0.71 | −0.66 | −1.34 | −0.12 |
| Excessive red meat intake | |||||||||||
| Overall | 32.5 | 34.5 | 30.9 | 1.12 | 42.0 | 48.0 | 35.7 | 1.34 | 1.90 | 2.70 | 0.96 |
| 18–44 y | 36.1 | 37.9 | 34.6 | 1.10 | 47.8 | 53.7 | 40.6 | 1.32 | 2.34 | 3.16 | 1.20 |
| 45–59 y | 31.0 | 32.4 | 30.0 | 1.08 | 37.7 | 41.9 | 33.6 | 1.25 | 1.34 | 1.90 | 0.72 |
| 60 y∼ | 22.5 | 25.2 | 20.5 | 1.23 | 28.7 | 33.5 | 24.9 | 1.35 | 1.24 | 1.66 | 0.88 |
| Men | |||||||||||
| Overall | 38.2 | 39.7 | 37.0 | 1.07 | 49.3 | 55.8 | 42.4 | 1.32 | 2.22 | 3.22 | 1.08 |
| 18–44 y | 42.2 | 43.4 | 41.2 | 1.05 | 55.8 | 62.3 | 47.9 | 1.30 | 2.72 | 3.78 | 1.34 |
| 45–59 y | 36.7 | 37.5 | 36.0 | 1.04 | 44.5 | 48.8 | 40.3 | 1.21 | 1.56 | 2.26 | 0.86 |
| 60 y∼ | 26.4 | 29.1 | 24.5 | 1.19 | 33.7 | 38.8 | 29.7 | 1.31 | 1.46 | 1.94 | 1.04 |
| Women | |||||||||||
| Overall | 26.8 | 29.3 | 24.6 | 1.19 | 34.7 | 40.1 | 28.9 | 1.39 | 1.58 | 2.16 | 0.86 |
| 18–44 y | 29.9 | 32.4 | 27.6 | 1.17 | 39.7 | 45.0 | 33.1 | 1.36 | 1.96 | 2.52 | 1.10 |
| 45–59 y | 25.2 | 27.1 | 23.5 | 1.15 | 30.7 | 34.8 | 26.8 | 1.30 | 1.10 | 1.54 | 0.66 |
| 60 y∼ | 18.8 | 21.6 | 16.6 | 1.30 | 24.0 | 28.5 | 20.4 | 1.40 | 1.04 | 1.38 | 0.76 |
| Inadequate physical activity | |||||||||||
| Overall | 16.3 | 17.6 | 15.2 | 1.16 | 22.3 | 22.0 | 22.6 | 0.97 | 1.20 | 0.88 | 1.48 |
| 18–44 y | 16.9 | 19.4 | 14.7 | 1.32 | 23.9 | 24.0 | 23.7 | 1.01 | 1.40 | 0.92 | 1.80 |
| 45–59 y | 12.2 | 13.5 | 11.1 | 1.22 | 18.2 | 18.1 | 18.2 | 0.99 | 1.20 | 0.92 | 1.42 |
| 60 y∼ | 20.2 | 17.4 | 22.3 | 0.78 | 23.1 | 20.1 | 25.6 | 0.79 | 0.58 | 0.54 | 0.66 |
| Men | |||||||||||
| Overall | 18.2 | 20.6 | 16.1 | 1.28 | 24.4 | 24.3 | 24.6 | 0.99 | 1.24 | 0.74 | 1.70 |
| 18–44 y | 18.9 | 22.5 | 15.9 | 1.42 | 26.2 | 26.1 | 26.2 | 1.00 | 1.46 | 0.72 | 2.06 |
| 45–59 y | 15.1 | 17.8 | 12.9 | 1.38 | 21.1 | 21.4 | 20.7 | 1.03 | 1.20 | 0.72 | 1.56 |
| 60 y∼ | 20.3 | 18.1 | 21.9 | 0.83 | 23.5 | 21.2 | 25.2 | 0.84 | 0.64 | 0.62 | 0.66 |
| Women | |||||||||||
| Overall | 14.3 | 14.5 | 14.1 | 1.03 | 20.2 | 19.8 | 20.7 | 0.96 | 1.18 | 1.06 | 1.32 |
| 18–44 y | 14.8 | 16.2 | 13.6 | 1.19 | 21.6 | 21.9 | 21.2 | 1.03 | 1.36 | 1.14 | 1.52 |
| 45–59 y | 9.2 | 9.1 | 9.3 | 0.98 | 15.2 | 14.8 | 15.7 | 0.94 | 1.20 | 1.14 | 1.28 |
| 60 y∼ | 20.1 | 16.7 | 22.7 | 0.74 | 22.8 | 18.9 | 25.9 | 0.73 | 0.54 | 0.44 | 0.64 |
Current smokers were those who were still smoking at the time of the survey. Excessive drinking referred to the drinking behavior of male drinkers with an average daily alcohol intake of greater than or equal to 41 g, and female drinkers with an average daily alcohol intake of greater than or equal to 21 g. Inadequate vegetable/fruit intake referred to an average daily intake of vegetables and fruits of less than 400 g. Excessive red meat intake was regarded as an average daily intake of red meat of 100 g or more. Inadequate physical activity meant the total weekly activity time was less than 150 min.
Data were from the "Report on Chronic Disease Risk Factor Surveillance in China" in 2013 and 2018, respectively.
Annual increase was calculated as the absolute difference in these measures between the first and last year divided by the duration in years.
Ratio = Urban value/Rural value.
Discussion
This study provided the most updated, comprehensive, and nationally representative picture of NCD trends in China, from the upstream modifiable risk factors to the downstream endpoint health outcome of mortality rates. NCD has become a serious public health problem in China given the high prevalence and low rates of awareness, treatment and control. Some groups are affected more than the others. There are signs that the situation may become worse in the future considering the worsening of some lifestyle risk factors such as unhealthy diet and lack of physical activity.
Moreover, our published projected analysis showed that the prevalence of overweight/obesity, hypertension and diabetes in China in 2030 might reach 70.5%, 35.4%, and 18.5%, respectively, if China cannot take more vigorous effective actions to fight the growing NCD epidemic.42 The increased NCD burden in China is resulted from the changes in demographic, socioeconomic, behavioral and environmental factors. These findings will facilitate policy development and preparedness for future NCD challenges. China needs to take urgent and effective actions and the whole society needs to give adequate attention to fighting the NCD epidemic, especially in the post COVID-19 pandemic era.
This study examined the trends in NCDs and related behavioral risk factors in mainland China from 2002 to 2019. It showed the mortality rates of NCDs overall and proportional mortality of NCDs had increased. The prevalence of major NCDs (e.g., obesity, hypertension, and diabetes) was high and had increased, and will likely continue to increase. However, the rates of awareness, treatment and control of hypertension and diabetes were fluctuated at very low levels (ranging from 10 to 40%) with limited improvements over time. Some lifestyle risk factors even worsened. Notably, there were also age- and gender differences in NCDs and behavioral risk factors. Further, residents in rural areas had been increasingly affected. Specifically, the increasing rates in the prevalence of obesity, hypertension and diabetes among rural residents were higher than in urban residents. Moreover, rural residents had higher rates in four of the five behavioral risk factors than urban residents did. These findings suggested the high burden of NCDs and challenges in coping with NCDs in China.
The potential reasons for the increased NCD burden in China may be attributed to many complex social, environmental, and individual factors as well as their interactions. Some related contexts were described blow.
Typical social factors included the increased life expectancy, aging population, urbanization and the disease spectrum shifting from communicable diseases to NCDs,29,43 which could also be found in the developing regions worldwide.44,45 The most recent study showed life expectancy at birth in China was projected to increase to 81.3 years in 2035, compared to 77.7 years in 2019.46 In parallel, the number of population aged 60 years or older in China will increase from 254 million in 2019 to 402 million by 2040, making up about 28% of the total population.43 The rapid increasing percentage of urban population (36% in 2000 to 63% in 2021) also brought nutrition transition, decreased physical activity, and subsequent epidemiological transition from communicable diseases to NCDs.47
The environmental factors included the obesogenic environment, air pollution, and general low health literacy level, etc.32 A recent systematic review classified obesogenic environment as built environmental factors, e.g., land-use mix, access to green space, public transport, bike lanes, sidewalks, etc., and food environmental factors, e.g., access to convenience stores, supermarkets, grocery stores, and fruit and vegetable markets.48 A common view to the most important factors of obesogenic environment includes stress, lifestyle, and urban design, framed in a food system which contributes to intakes of hypercaloric diets. Air pollution, as the 5th major risk factor for NCDs in the WHO framework, may interfere with metabolic processes that regulate lipid accumulation and increase body adiposity.49 The health literacy rate in mainland China increased from 6.5% in 2010 to 23.2% in 2020.50 Even in developed megacities in China, the rates were still very low in 2020 (36.4% in Beijing and 35.6% in Shanghai, respectively).51,52
The individual factors included prevalent behavioral risk factors, such as unhealthy diets and inadequate physical activity. These modifiable behavioral risk factors shall be the focus of intervention.
Other nationally representative studies showed overall consistent results in the rates of awareness, treatment and control of hypertension and diabetes among Chinese adults.16, 17, 18, 19, 20,53 Surprisingly, the awareness and treatment rates of diabetes decreased among young adults (18–44 y) particularly in the urban areas, which indicated the rapid increase in the number of undiagnosed diabetes in this population. A recently published study showed modest improvements in the rates of awareness, treatment and control of hypertension from 2004 to 2018, but they remained low in 2018.53 A recently released clinical practice guidelines for the management of hypertension in China reduced the blood pressure cut-off values for hypertension diagnosis to 130/80 mmHg, but it was not supported in China. This suggested change may increase the hypertension prevalence among adults up to 46.4%, and the number of hypertension patients to 490 million in China.54
The continuously increased prevalence and stagnated management rates of these NCDs showed a challenging situation in the prevention and control of NCD in China. The projected prevalence of obesity, hypertension, and diabetes, and NCD management rates in 2030, were also not optimistic to reach the global or national goals.2,10 Further, the rural areas were increasingly affected, the reasons for which were worthwhile to be explored further.
Another important finding was that men and rural residents had higher increasing rates in prevalence in obesity, hypertension and diabetes than their counterparts, women and urban residents, respectively, and urban women had the lowest increasing rates in all the conditions. Potential explanations were that urban residents had higher socioeconomic status than rural residents and women cared more about their health status than men. This was consistent with the higher awareness, treatment and control rates of hypertension and diabetes among urban residents and women, compared to their counterparts. This finding identified the rural residents and men as the high-risk population group which needs special focused attention and intensive intervention.
To tackle these challenges, vigorous multilevel efforts are needed to strengthen the current policy and practical measures targeting the major behavioral risk factors of NCDs. A supportive, integrated and coordinated policy system covering health, civil affairs, education, and economic factors is needed, but this is inadequate in China. At a practical level, how to transform the policy to effective intervention measures, is a big research question as well as an implementation challenge given the limited resources. Policy evaluation studies, which are not common cases in China, need to be supported and promoted.55 Altogether, big challenges existed in combating NCDs in China, and more rigorous and effective interventions are required.
Findings from health economics studies indicate that promoting healthy lifestyle is the most cost-effective investment.56 Unhealthy diets and tobacco use are considered the top two preventable behavioral risk factors for deaths.4 However, the health-related behavioral risk factors declined rather slowly and a few even increased over time in China, as revealed in this study. Specifically, more than 50% of Chinese men were current smokers, an increasing percentage of adults had inadequate physical activity, and almost half of Chinese adults had low fruit/vegetable intake and high red meat intake (two indicators of an unhealthy diet). All these behavioral risk factors, together with the increased prevalence and poor management of NCDs, had indicated the cardiovascular disease crisis and increased burden of other related NCDs in China. Of concerns, among all the five behavioral risk factors included in this study, rural residents had higher prevalence than their urban counterparts in four. More efforts should be devoted to rural areas to promote healthy lifestyle there.
The Chinese government has made tremendous efforts to promote health equity in recent years. The Health Aid Program for Poverty Alleviation in 2015–2020 has helped more than 20 million disadvantage rural populations to combat against critical illnesses and long-term NCDs. Because of the program, by the end of 2019, more than 99.99% of the rural poor had been covered by the medical insurance system, and the number of people who had fallen into poverty due to illness or returned to poverty had been significantly reduced.57 The systematic integration of the routine medical insurance mechanism and the target financial aid program has successfully blocked the vicious cycle of diseases (mostly NCDs) and poverty.58 For the next step, the Chinese government has prioritized promoting healthy lifestyle and preventing diseases, to increase the life quality and decrease medical costs among rural residents.59,60
In addition to the government commitment, practical, effective, and scalable intervention models are essential to decrease the health disparity, given the resource constraints in rural areas. Difficulties in access to quality health care is one of the key barriers.61 Consolidating the primary health care and promoting the integration of prevention and treatment of NCDs in rural areas is perhaps the solution. A recent published hypertension intervention study in rural China through village doctors provided a feasible, effective, and sustainable intervention model, which may be scaled up to other NCD interventions.62
Studies on the economic costs of NCDs are crucial for policy priority. However, such studies in LMICs including China are very limited.63 Our projection analysis shows that overweight and obesity in China will cost the country 418 billion Chinese Yuan (around US $61 billion) and be attributable to 21.5% of total medical costs.56 A multi-nation comparison study showed that households with NCD patients in China had much higher absolute risk of catastrophic spending compared with non NCDs.64 Further, urban-rural disparities also existed in economic burden of NCDs. Rural households with NCD patients had higher risk of incurring catastrophic health expenditure and heavier economic burden of diseases.65
Despite of its strengths, this study has limitations. Besides the morbidity indicator “prevalence” used in this study, the comprehensive and specific morbidity indicators are not available, which prevents us from demonstrating the quality of life and healthy lifetime among Chinese residents in an aging society. Currently, China adapted such indicators mainly from the Global Burden of Disease (GBD) Project. There is discussion whether and to what extent the weights adapted from the GBD Project fit China's condition.66 Despite the limitation, the indicators used in this study are better than arbitrary and have provided the best available data regarding NCDs and behavioral risk factors in China.
For future NCD prevention and control in China, we recommend: 1) engage all stakeholders in the society and build a supportive environment to help achieve the targets of NCD control; 2) strengthen the standardized management of NCD patients to decrease the NCD related morbidity, and increase the quality and healthy life of NCD patients; 3) integrate public health and clinical services to achieve the whole-chain NCD management covering both prevention and treatment; 4) enhance high-quality training for primary health care personnel, a critical solution to the NCD disparity in China; 5) enhance development and applications of innovative approaches and programs, e.g., those based on new technologies such as digital health approaches; and 6) make more efforts to support the vulnerable population groups such as those with low socioeconomic status and those living in areas with limited resources.56,67, 68, 69
In addition, more future research is needed in the following areas: 1) economic costs of NCDs and related risk factors in China shall be investigated for policy development; 2) more context adapted intervention studies are needed to develop interventions that are feasible, scalable, cost-effective, and sustainable, particularly those for improving the awareness, treatment and control of NCDs and those that support the disadvantaged populations; and 3) studies that evaluate the impact of related health policies and intervention programs.
In conclusion, the mortality and prevalence of major NCDs in China were high and increased from 2002 to 2018. There was no significant improvement in the NCD management and behavioral risk factors. The rates of awareness, treatment and control of some common NCDs like hypertension and diabetes were low, while the situation in some population groups was worse. More vigorous effective measures against NCDs are required timely to achieve the WHO and national Healthy China 2030 targets.
Contributors
YFW and WP conceptualized the research idea and made the research plan. SC and TW conducted literature review, data collection, and data analysis. WP and SC wrote the initial draft of the manuscript. YFW, XC, YM, XS, YGW, and GD revised the manuscript critically. All authors approved the final manuscript for submission. YFW provided administration support.
Data sharing statement
Data used in this study were available from the correspondence author.
Declaration of interests
We declare no competing interests.
Acknowledgements
This study was funded in part by the National Key R&D Program of China (2017YFC0907200, 2017YFC0907201), International Collaboration Project from the Chinese Ministry of Science and Technology-Prevention and control of chronic diseases and health promotion (G2021170007L), Natural Scientific Foundation of China (82103846), Key R&D and Transformation Program of Qinghai (2023-QY-204).
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2023.100809.
Appendix A. Supplementary data
References
- 1.United Nations Transforming our world: the 2030 agenda for sustainable development. 2015. https://sdgs.un.org/sites/default/files/publications/21252030%20Agenda%20for%20Sustainable%20Development%20web.pdf
- 2.World Health Organization Global action plan for the prevention and control of noncommunicable diseases 2013-2020. 2013. https://www.who.int/publications/i/item/9789241506236
- 3.World Health Organization Noncommunicable diseases 2022. 2022. https://www.who.int/health-topics/noncommunicable-diseases#tab=tab_1
- 4.The Institute for Health Metrics and Evaluation Global burden of disease. 2019. https://vizhub.healthdata.org/gbd-results/
- 5.World Health Organization WHO Director-General’s opening remarks at first annual gathering of the global group of Heads of State and government group for the prevention and control of noncommunicable diseases. 2022. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-first-annual-gathering-of-the-global-group-of-heads-of-state-and-government-group-for-the-prevention-and-control-of-noncommunicable-diseases---21-september-2022
- 6.Wang Y., Mi J., Shan X., et al. Is China facing an obesity epidemic and the consequences? The trends in obesity and chronic disease in China. Int J Obes. 2007;31(1):177–188. doi: 10.1038/sj.ijo.0803354. [DOI] [PubMed] [Google Scholar]
- 7.Wang Y., Wang L., Qu W. New national data show alarming increase in obesity and noncommunicable chronic diseases in China. Eur J Clin Nutr. 2017;71(1):149–150. doi: 10.1038/ejcn.2016.171. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization Technical Report Series Diet . WHO; Geneva: 2003. Nutrition and the prevention of chronic diseases. [PubMed] [Google Scholar]
- 9.The State Council, The Central Committee of China . The State Council, the Central Committee of China; Beijing: 2016. Plan outline for healthy China 2030. [Google Scholar]
- 10.People's Central Government of the People's Republic of China . Government of China; Beijing: 2019. Healthy China action plan (2019–2030) [Google Scholar]
- 11.Li X., Jiang Y., Hu N., et al. Prevalence and characteristic of overweight and obesity among adults in China, 2010. Zhonghua Yufang Yixue Zazhi. 2012;46(8):683–686. [PubMed] [Google Scholar]
- 12.Zhang M., Jiang Y., Li Y., et al. Prevalence of overweight and obesity among Chinese elderly aged 60 and above in 2010. Zhonghua Liu Xing Bing Xue Za Zhi. 2014;35(4):365–369. [PubMed] [Google Scholar]
- 13.Wang L., Zhou B., Zhao Z., et al. Body-mass index and obesity in urban and rural China: findings from consecutive nationally representative surveys during 2004-18. Lancet. 2021;398(10294):53–63. doi: 10.1016/S0140-6736(21)00798-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li Y., Wang L., Jiang Y., et al. Prevalence of hypertension among Chinese adults in 2010. Zhonghua Yufang Yixue Zazhi. 2012;46(5):409–413. [PubMed] [Google Scholar]
- 15.Zhao L., Yang D., Fu P., et al. Prevalence of hypertension among 18 years old and over adults in 2010-2012 in China: based on the value of mercury sphygmomanometer and converted electronic sphygmomanometer. Wei Sheng Yan Jiu. 2018;47(1):7–12. [PubMed] [Google Scholar]
- 16.Li Y., Yang L., Wang L., et al. Burden of hypertension in China: a nationally representative survey of 174,621 adults. Int J Cardiol. 2017;227:516–523. doi: 10.1016/j.ijcard.2016.10.110. [DOI] [PubMed] [Google Scholar]
- 17.Wang W., Zhang M., Xu C., et al. Hypertension prevalence, awareness, treatment, and control and their associated socioeconomic factors in China: a spatial analysis of a national representative survey. Biomed Environ Sci. 2021;34(12):937–951. doi: 10.3967/bes2021.130. [DOI] [PubMed] [Google Scholar]
- 18.Zhang M., Wu J., Zhang X., et al. Prevalence and control of hypertension in adults in China, 2018. Zhonghua Liu Xing Bing Xue Za Zhi. 2021;42(10):1780–1789. doi: 10.3760/cma.j.cn112338-20210508-00379. [DOI] [PubMed] [Google Scholar]
- 19.Wang L., Gao P., Zhang M., et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA. 2017;317(24):2515–2523. doi: 10.1001/jama.2017.7596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang L., Peng W., Zhao Z., et al. Prevalence and treatment of diabetes in China, 2013-2018. JAMA. 2021;326(24):2498–2506. doi: 10.1001/jama.2021.22208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhao W., Zhang J., You Y., et al. Epidemiologic characteristics of dyslipidemia in people aged 18 years and over in China. Zhonghua Yufang Yixue Zazhi. 2005;39(5):306–310. [PubMed] [Google Scholar]
- 22.Song P., Man Q., Li H., et al. Trends in lipids level and dyslipidemia among Chinese adults, 2002-2015. Biomed Environ Sci. 2019;32(8):559–570. doi: 10.3967/bes2019.074. [DOI] [PubMed] [Google Scholar]
- 23.Zhang M., Deng Q., Wang L., et al. Prevalence of dyslipidemia and achievement of low-density lipoprotein cholesterol targets in Chinese adults: a nationally representative survey of 163,641 adults. Int J Cardiol. 2018;260:196–203. doi: 10.1016/j.ijcard.2017.12.069. [DOI] [PubMed] [Google Scholar]
- 24.Li Y., Wang L., Jiang Y., et al. Risk factors for noncommunicable chronic diseases in women in China: surveillance efforts. Bull World Health Organ. 2013;91(9):650–660. doi: 10.2471/BLT.13.117549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shang J., Zhang M., Zhao Z., et al. Relations between cigarette smoking and chronic diseases of Chinese adults in 2013. Zhonghua Liu Xing Bing Xue Za Zhi. 2018;39(4):433–438. doi: 10.3760/cma.j.issn.0254-6450.2018.04.009. [DOI] [PubMed] [Google Scholar]
- 26.Zhang M., Yang L., Wang L., et al. Trends in smoking prevalence in urban and rural China, 2007 to 2018: findings from 5 consecutive nationally representative cross-sectional surveys. PLoS Med. 2022;19(8):e1004064. doi: 10.1371/journal.pmed.1004064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ren X., Yu S., Wang L., et al. The analysis of stroke death attributed to smoking in 2018 of China. Chin J Cardiovasc Med. 2021;29(2):81–84. [Google Scholar]
- 28.National Center for Chronic and Noncommunicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention . Military Medicine Press; Beijing: 2016. Report on chronic disease risk factor surveillance in China 2013. [Google Scholar]
- 29.National Center for Chronic and Noncommunicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention . People’s Health Publishing House; Beijing: 2021. Report on chronic disease risk factor surveillance in China 2018. [Google Scholar]
- 30.Disease Prevention and Control Bureau of the National Health Commission . People’s Health Publishing House; Beijing: 2015. Report on nutrition and chronic disease status of Chinese residents (2015) [Google Scholar]
- 31.Disease Prevention and Control Bureau of the National Health Commission . Peking University Medical Press; Beijing: 2015. Comprehensive report on the monitoring of nutrition and health status of Chinese residents 2010-2013. [Google Scholar]
- 32.Disease Prevention and Control Bureau of the National Health Commission . People’s Health Publishing House; Beijing: 2022. Report on nutrition and chronic disease status of Chinese residents (2020) [Google Scholar]
- 33.Wang L. People’s Health Publishing House; Beijing: 2005. Comprehensive report on the survey of nutrition and health status of Chinese residents 2002. [Google Scholar]
- 34.World Health Organization International statistical classification of diseases and related health problems (ICD) 2022. https://www.who.int/standards/classifications/classification-of-diseases
- 35.World Health Organization Noncommunicable diseases key facts 2022. 2022. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
- 36.China Center for Chronic Non communicable Disease Control and Prevention Criteria of weight for adults (WS/T 428-2013) 2013. http://www.nhc.gov.cn/wjw/yingyang/201308/a233d450fdbc47c5ad4f08b7e394d1e8.shtml
- 37.Zhou B., Cooperative Meta-Analysis Group of the Working Group on Obesity in China Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults—study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. 2002;15(1):83–96. [PubMed] [Google Scholar]
- 38.China Hypertension Prevention and Control Guidelines Revision Committee Chinese hypertension prevention and control guidelines (2018 revised edition) Chin J Cardiovasc Med. 2019;24(1):24–56. [Google Scholar]
- 39.World Health Organization Diagnosis criteria for diabetes. 1999. https://apps.who.int/iris/handle/10665/66040
- 40.China Joint Committee on the Formulation of Guidelines for the Prevention and Treatment of Adult Dyslipidemia Guidelines for the prevention and treatment of dyslipidemia in Chinese adults (2007) Chin J Cardiovasc Med. 2007;35(5):390–420. [Google Scholar]
- 41.World Health Organization Global comprehensive surveillance framework (with indicators) and voluntary targets for the prevention and control of non-communicable diseases (2013-2025) 2012. https://www.who.int/publications/i/item/ncd-surveillance-global-monitoring-framework
- 42.Sun X., Yan A.F., Shi Z., et al. Health consequences of obesity and projected future obesity health burden in China. Obesity. 2022;30(9):1724–1751. doi: 10.1002/oby.23472. [DOI] [PubMed] [Google Scholar]
- 43.Chen X., Giles J., Yao Y., et al. The path to healthy ageing in China: a Peking University-Lancet Commission. Lancet. 2022;400(10367):1967–2006. doi: 10.1016/S0140-6736(22)01546-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bigna J., Noubiap J. The rising burden of non-communicable diseases in sub-Saharan Africa. Lancet Glob Health. 2019;7(10):e1295–e1296. doi: 10.1016/S2214-109X(19)30370-5. [DOI] [PubMed] [Google Scholar]
- 45.Gouda H., Charlson F., Sorsdahl K., et al. Burden of non-communicable diseases in sub-Saharan Africa, 1990-2017: results from the global burden of disease study 2017. Lancet Glob Health. 2019;7(10):e1375–e1387. doi: 10.1016/S2214-109X(19)30374-2. [DOI] [PubMed] [Google Scholar]
- 46.Bai R., Liu Y., Zhang L., et al. Projections of future life expectancy in China up to 2035: a modelling study. Lancet Public Health. 2022 doi: 10.1016/S2468-2667(22)00338-3. S2468–S2667(22)00338-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.The World Bank Urban population (% of total population) 2022. https://data.worldbank.org/indicator/SP.URB.TOTL.IN.ZS?locations=CN.html
- 48.Jia P., Shi Y., Jiang Q., et al. Environmental determinants of childhood obesity: a meta-analysis. The Lancet Glob Health. 2023;11(Suppl 1):S7. doi: 10.1016/S2214-109X(23)00092-X. [DOI] [PubMed] [Google Scholar]
- 49.Martínez-Esquivel A., Trujillo-Silva D.J., Cilia-López V.G. Impact of environmental pollution on the obesogenic environment. Nutr Rev. 2022;80(7):1787–1799. doi: 10.1093/nutrit/nuac003. [DOI] [PubMed] [Google Scholar]
- 50.The Central People’s Government of the People’s Republic of China National health literacy level of residents in 2020. 2021. http://www.gov.cn/xinwen/2021-04/01/content_5597287.html
- 51.Beijing Municipal Health Commission The health literacy level of Beijing residents will reach 36.4% by 2020. 2021. http://wjw.beijing.gov.cn/wjwh/ztzl/awjk/awjkjkbj/202112/t20211217_2564085.html
- 52.Shanghai Health Promotion Commission Office, Shanghai Health Promotion Center 2020 press conference on health literacy monitoring of Shanghai residents. 2021. https://www.cnr.cn/shanghai/tt/20210301/t20210301_525424722.shtml
- 53.Zhang M., Shi Y., Zhou B., et al. Prevalence, awareness, treatment, and control of hypertension in China, 2004-18: findings from six rounds of a national survey. BMJ. 2023;380:e071952. doi: 10.1136/bmj-2022-071952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.National Center for Cardiovascular Diseases, Chinese Medical Doctor Association, Hypertension Committee of the Chinese Medical Doctor Association, et al. Clinical practice guidelines for the management of hypertension in China. Chin J Cardiovasc Med. 2022;50(11):1050–1095. [Google Scholar]
- 55.Wang Y., Zhao L., Gao L., et al. Health policy and public health implications of obesity in China. Lancet Diabetes Endocrinol. 2021;9(7):446–461. doi: 10.1016/S2213-8587(21)00118-2. [DOI] [PubMed] [Google Scholar]
- 56.World Health Organization Saving lives, spending less: a strategic response to noncommunicable diseases 2018. 2018. https://www.who.int/publications/i/item/WHO-NMH-NVI-18.8
- 57.National Rural Revitalization Administration Health aid program for poverty alleviation. 2020. http://fpzg.cpad.gov.cn/429463/430986/431000/index.html
- 58.The State Council, the Central Committee of China The "fourteenth five-year plan" national medical security plan. 2021. http://www.gov.cn/zhengce/content/2021-09/29/content_5639967.htm
- 59.Shanghai Academy of Social Sciences, China Financial Information Center, Ping An 2018-2020 rural health poverty alleviation report. 2021. http://health.people.com.cn/n1/2021/0330/c14739-32064430.html
- 60.National Health Commission The National Health Commission held a press conference on the achievements of health poverty alleviation since the 18th National Congress of the Communist Party of China and the progress of effective connection with rural revitalization. 2022. http://www.china.com.cn/zhibo/content_78233447.htm
- 61.Wang M., Fang H., Bishwajit G., et al. Evaluation of rural primary health care in Western China: a cross-sectional study. Int J Environ Res Publ Health. 2015;12(11):13843–13860. doi: 10.3390/ijerph121113843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sun Y., Mu J., Wang D., et al. A village doctor-led multifaceted intervention for blood pressure control in rural China: an open, cluster randomised trial. Lancet. 2022;399(10339):1964–1975. doi: 10.1016/S0140-6736(22)00325-7. [DOI] [PubMed] [Google Scholar]
- 63.Kazibwe J., Tran P., Annerstedt K. The household financial burden of non-communicable diseases in low- and middle-income countries: a systematic review. Health Res Pol Syst. 2021;19(1):96. doi: 10.1186/s12961-021-00732-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Murphy A., Palafox B., Walli-Attaei M., et al. The household economic burden of non-communicable diseases in 18 countries. BMJ Glob Health. 2020;5(2) doi: 10.1136/bmjgh-2019-002040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fu X., Sun Q., Sun C., et al. Urban-rural differences in catastrophic health expenditure among households with chronic non-communicable disease patients: evidence from China family panel studies. BMC Publ Health. 2021;21(1):874. doi: 10.1186/s12889-021-10887-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Liu X., Wang F., Yu C., et al. Eliciting national and subnational sets of disability weights in mainland China: findings from the Chinese disability weight measurement study. Lancet Reg Health West Pac. 2022;26:100520. doi: 10.1016/j.lanwpc.2022.100520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yip W., Fu H., Chen A., et al. 10 years of health-care reform in China: progress and gaps in Universal Health Coverage. Lancet. 2019;394(10204):1192–1204. doi: 10.1016/S0140-6736(19)32136-1. [DOI] [PubMed] [Google Scholar]
- 68.Wang L., Wang Z., Ma Q., et al. The development and reform of public health in China from 1949 to 2019. Glob Health. 2019;15(1):45. doi: 10.1186/s12992-019-0486-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wang Y., Min J., Khuri J., et al. Effectiveness of mobile health interventions on diabetes and obesity treatment and management: systematic review of systematic reviews. JMIR Mhealth Uhealth. 2020;8(4):e15400. doi: 10.2196/15400. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.