Abstract
Introduction
Spinal pain syndromes have a severe impact on the patient's sex life, contributing to a decrease in sexual function and sexual satisfaction. Despite the importance of sexual health on mental and physical wellbeing, sexual health is rarely discussed during consultations.
Research question
The aim of this study is to explore to what extent influencing factors can alter the discussion about sexual health during consultations. More specifically, we will evaluate the influence of healthcare profession, sex of the patient and the surgical approach that is proposed.
Material and methods
An online survey was sent to neurosurgeons, pain physicians and orthopedists in Belgium and The Netherlands in April 2019. Participants were asked about; counseling routine, knowledge, and opinion on sexual health. Answers were scored on a 5-point Likert scale. Independence between the response levels and type of surgery as well as profession were tested.
Results
In total, 350 respondents were approached of whom 57 completed the survey. The majority of respondents (61.4%) indicated that they rarely or never discussed sexual disturbances. Profession and type of surgery had an influence on discussing erectile dysfunction, retrograde ejaculation, and alterations in orgasms. Thirty-five percent of healthcare providers considered it the patient's responsibility to bring up the subject of sexual health.
Discussion and conclusion
Sexual health is rarely addressed by healthcare providers during spinal care. Profession as well as type of surgery seems to play a role on whether sexual health is discussed during consultations.
Keywords: Sexual health, Counseling, Sexual dysfunction, Spine procedures, Patient care
Highlights
-
•
Sexual health is rarely discussed by healthcare providers before spine surgery.
-
•
Healthcare profession and type of surgery influence sexual health discussions.
-
•
Sex differences seem to play a role in discussing sexual health.
1. Introduction
Sexual health has been denoted as a highly important aspect of quality of life (Flynn et al., 2016). High sexual health is associated with mental and physical wellbeing, as well as with relationship satisfaction (Boul, 2007; McCabe et al., 2010; Mitchell et al., 2013). In contrast, low sexual quality of life is associated with depression, instability in intimate relationships and serves as a predisposing factor to subsequent relationship distress (Forbes et al., 2017; Yeh et al., 2006). Despite the lower sexual satisfaction that is often reported by patients who experience poor health, sexual health remains an important factor (Flynn et al., 2016).
Spinal pain syndromes have a severe impact on the patient's sex life (Moscicki et al., 2022), contributing to a decrease in sexual function and sexual satisfaction (Ferrari et al., 2019; Sahin et al., 2022; Łabuz-Roszak et al., 2018). Lumbar disc herniation appears to be associated with sexual dysfunction in up to 77% of patients (Panneerselvam et al., 2022). Sexual function and satisfaction can significantly improve after surgical interventions (Sahin et al., 2022; Holmberg et al., 2021), however sexual function is rarely discussed in a public health context (Mitchell et al., 2013; Mercer et al., 2003). Percentages of up to 81% of patients with chronic low back pain complained of sexual problems, whereas 66% never discussed the subject with their healthcare provider (Bahouq et al., 2013). Despite the scarcity of discussing sexual health, 93% of chronic low back pain patients expressed the need for sexual problem management during consultations for chronic low back pain (Bahouq et al., 2013). According to patients, main barriers to prevent a discussion on sex include the taboo character of the topic and inappropriateness of visit conditions (Bahouq et al., 2013).
When evaluating the opinion of neurosurgeons on discussing sexual health in spinal care, 73% indicated that they (almost) never discussed sexual health with their patients (Korse et al., 2016). The main barriers for not discussing sexual health were patients' old age (42%), lack of knowledge (38%) and lack of patients' initiative to bring up the subject (36%) (Korse et al., 2016). These findings can be generalized towards other pathologies among which brain tumors, whereby 59.1% of the neurosurgeons never discussed sexual health with their patients (Laldjising et al., 2021). A trend was observed of discussing sexual health less with older patients (Laldjising et al., 2021). The most frequent barriers for avoiding discussing sexual health with brain tumor patients were that patients do not express sexual problems spontaneously, insufficient training or knowledge of the neurosurgeon and insufficient time to discuss sexual health (Laldjising et al., 2021).
Specifically for spine surgeries, anterior lumbar interbody fusion procedures and total disc replacements with anterior exposure of the lumbar spine entail a risk of a vascular injury and dysfunction of the sympathetic and parasympathetic nerves due to disturbance of the inferior and superior hypogastric plexus (Wuertz-Kozak et al., 2019). The overall incidence of delayed ejaculation was 0.09%, with the highest rate among ALIF surgeries at 0.13% (Bhambhvani et al., 2022). In males, retrograde ejaculation with consecutive potential infertility is a known complication of the anterior spinal approach with prevalence rates ranging between 0.9% and 6.3% (Comer et al., 2012; Body et al., 2021). Furthermore, a prospective study evaluated complications among which retrograde ejaculation, observable in 12% after degenerative disk disease with radiculopathy and in 29% after failed posterior fusion (Rao et al., 2015). In patients undergoing anterior lumbar spine surgery, difficulties with orgasm were reported in 46% of males versus 17% of females, changes in genital sensation occurred in 32% of males and 17% of females and 78% of females had no difficulty with genital moistness (Fischer et al., 2014). Another study indicated that anterior approaches did not seem to negatively influence sexual and urinary function in females (Wuertz-Kozak et al., 2019). These findings suggest that the considered surgical approach and sex of the patient may play a role in determining the frequency and quality of communication concerning sexual health with patients. Additionally, this study will not only address sexual health in neurosurgeons, but in all healthcare professions involved in the treatment of patients with spinal pain syndromes, i.e. orthopedic surgeons, neurosurgeons and pain physicians. Therefore, the aim of this study is to further explore to what extent influencing factors can alter the discussion about sexual health. More specifically, we will evaluate the influence of healthcare profession, sex of the patient and the surgical approach that is proposed.
2. Materials & methods
2.1. Participants
As target population for this online survey, specialized Belgian and Dutch healthcare professionals who were familiar with the treatment of spinal pain syndromes and the surgical options, were selected. Therefore, neurosurgeons, orthopedic surgeons, and pain physicians were invited to take part. The main rationale to distribute the survey among pain physicians is the fact that more and more patients are visiting a pain physician before and after surgery. Ethical approval for this study was obtained by the ethical committee of the UZ Brussel, Belgium (B.U.N. 143201837053) on 20th March 2019.
2.2. Data collection and survey construction
An online survey was sent to the chairs of the Dutch Association for Neurosurgery (NVvN), the Belgian Spine Society (BSS), the Dutch Orthopaedic Association (NOV), the Belgium society of Neurosurgery (BSN) and the Flemish Anesthesiologic Society for Pain Relief (VAVP) for further distribution among their members. Participation was voluntary. Before starting the survey, a privacy disclaimer asked the participants to state that they understood the goal of the study and that they were willing to fill in the survey. The survey was anonymous, and no questions allowed to identify the respondents.
This survey consisted of 28 questions, divided in 5 sections and was constructed by a multidisciplinary team of healthcare providers. Within section 1, general information regarding the respondent's profession was obtained (5 questions). In section 2, the frequency of communication concerning sexual health in spinal patients was questioned with 4 questions. Section 3 elaborated on the frequency of communication before and after spinal surgery for three different surgical procedures: anterior lumbar interbody fusion (ALIF), posterior lumbar interbody fusion (PLIF) and herniated disc surgery (HDS) through 5 questions. In section 4, the frequency of communication about possible consequences of spinal surgery on the patient's sex life was explored through 5 questions. In the final section, healthcare professional's knowledge and opinion on sexual health were explored with 9 questions. The full questionnaire is presented in Supplementary Material I. The questions in this survey were based on previous questionnaires used in the setting of sexual health in spinal care (Bahouq et al., 2013; Korse et al., 2016; Hägg et al., 2006). The complete survey consisted of closed-ended questions, with either dichotomous answer categories (yes/no) or multiple choice answer options on a 5-point Likert scale (never/rarely/sometimes/usually/always). The online survey was available in English and in the official national languages of Belgium and the Netherlands, i.e. Dutch, French, and German. The usability, technical functionality, and logical order of the survey were pilot-tested by 3 people. The survey was designed in LimeSurvey Version 2.00+ (https://www.limesurvey.org/), an open-source survey tool and took a maximum of 10 min to complete.
2.3. Statistical analysis
Data analysis was carried out in R Studio (version 2022.07.2). Descriptive statistics are provided as absolute numbers and frequencies. To evaluate differences in frequency of communication about sexual health between the three types of physicians, observed counts and expected counts under independence were calculated. To test for independence, the likelihood-ratio chi-squared (G2) tests were used.
Both before and after surgery, chi-squared tests were used to determine whether response levels were associated with type of surgery and healthcare professional. Expected and observed cell counts were compared and standardized Pearson residuals were computed to denote the cells with differences. More specifically, these residuals could identify specific cells that have a lack of fit (i.e., a cell-by-cell comparison between the observed and expected counts) and are presented in mosaic plots (Zeileis et al., 2007). A standardized Pearson residuals that exceeds about two or three in absolute value indicates a lack of fit of the null hypothesis of independence in that cell (Agresti, 2002). A similar approach was conducted to evaluate possible consequences of spinal surgery, namely erectile dysfunction, retrograde ejaculation, alterations in orgasms, and disturbed lubrication. P‐values of 0.05 or less were considered statistically significant. Data was used as observed, meaning no imputation strategies were applied. Knowledge and opinions of physicians were described descriptively.
3. Results
3.1. Participants
The healthcare organizations jointly consist of approximately 350 healthcare professionals involved in spinal care. After sending two reminders, there was no response from the Dutch Orthopaedic As-sociation (NOV), the Belgium society of Neurosurgery (BSN). In total 69 persons opened the survey of which 59 effectively started to complete the survey. Two of the remaining 59 respondents were excluded from the survey as candidates did not meet the inclusion criteria (one physiotherapist and one psychologist). Sixteen neurosurgeons, 15 orthopedic surgeons and 26 pain physicians participated in this study. Of the 57 received responses, three physicians (one neurosurgeon and 2 pain physicians) only completed the first section with general information.
Regarding the country where physicians perform their profession, 43 physicians (75.4%) were working in Belgium, 14 (24.6%) in The Netherlands. One person is counted in both countries since this physician practiced in Belgium as well as in The Netherlands. One person is retired, wherefore no country was provided by that physician.
In terms of monthly number of procedures performed by the surgeons (N = 31), 23 surgeons (74.2%) performed more than 10 procedures per month, 6 surgeons (19.3%) performed 6–10 procedures per month and 2 surgeons (6.5%) performed 1–5 procedures per month.
3.2. Communication concerning sexual disturbances
The majority of respondents (61.4%) indicated that they rarely or never talked to their patients about sexual disturbances. Only a minority (14%) effectively discussed sexual disturbances on a regular basis (usually or always) with their patients. More specific topic of sexual health namely sexual satisfaction, painful intercourse positions and a decrease in libido were even less frequently discussed (Table 1).
Table 1.
Frequency of communication concerning sexual health on a 5-point Likert scale. The most frequently responded answer is underlined.
| Never | Rarely | Sometimes | Usually | Always | Missing | |
|---|---|---|---|---|---|---|
| Sexual disturbances | 10 (17.5%) | 25 (43.9%) | 11 (19.3%) | 6 (10.5%) | 2 (3.5%) | 3 (5.3%) |
| Decrease in sexual satisfaction | 29 (50.9%) | 11 (19.3%) | 9 (15.8%) | 4 (7.0%) | 1 (1.8%) | 3 (5.3%) |
| Painful intercourse positions | 40 (70.2%) | 10 (17.5%) | 3 (5.3%) | 0 (0%) | 0 (0%) | 4 (7.0%) |
| Decrease in libido | 22 (38.6%) | 13 (22.8%) | 11 (19.3%) | 6 (10.5%) | 0 (0%) | 5 (8.8%) |
The null hypothesis of independence between profession and response levels could not be rejected for frequency in communication about sexual disturbances (χ2 = 4.78, p = 0.78), sexual satisfaction (χ2 = 11.87, p = 0.16), painful intercourse positions (χ2 = 8.05, p = 0.43), or libido (χ2 = 11.11, p = 0.19).
3.3. Communication about sexual functionality and sexual satisfaction before and after surgery
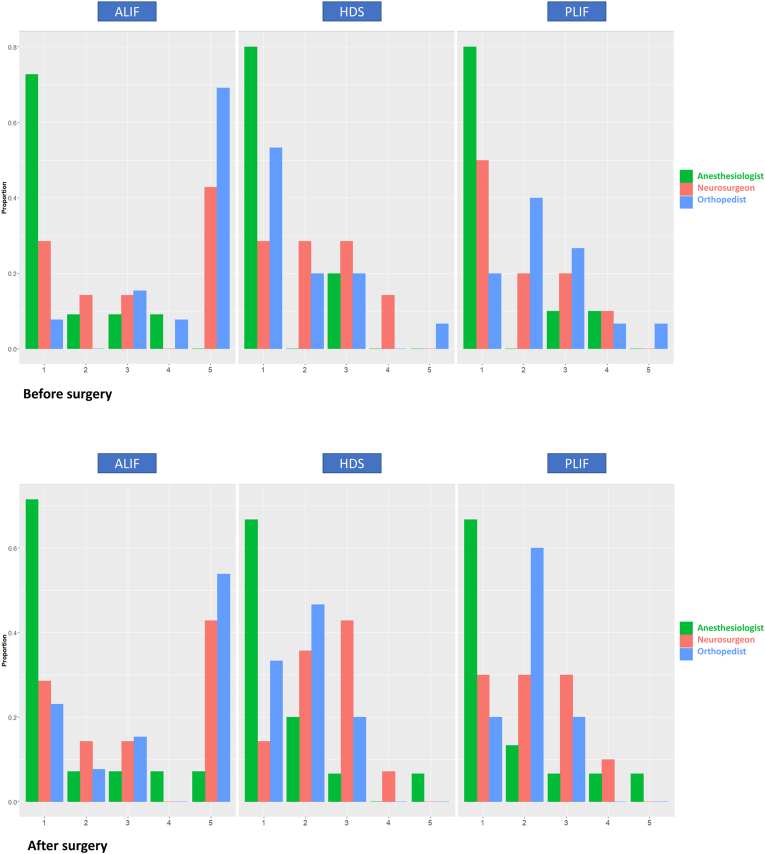
The proportion of response levels per professional and type of surgery for sexual functionality is presented in Fig. 1. Before surgery, we could reject the null hypothesis of independence between type of surgery and response levels (χ2 = 26.17, df = 8, p < 0.001), and between profession and response levels (χ2 = 26.36, df = 8, p < 0.001) for sexual functionality. Standardized residuals indicated that there were more pain physicians who never asked about sexual functionality before surgery than expected (under the null hypothesis of independence). Additionally, more orthopedists always questioned this topic before surgery. For ALIF procedures, more physicians discussed sexual functionality before surgery than expected under independence (Fig. 2).
Fig. 1.
Bar plots of the proportion of response levels for sexual functionality, separated by type of surgery and profession of healthcare providers. Physicians could give a rating on a 5-point Likert scale with the following options: (1) never; (2) rarely; (3) sometimes; (4) usually; (5) always. Pain physicians are indicated in green, neurosurgeons in red and orthopedists in blue. The upper row presents the frequency of asking patients about sexual functionality before surgery, and the lower row the same question after surgery. Abbreviations. ALIF: anterior lumbar interbody fusion procedures; DHS: herniated disc surgery; PLIF: posterior lumbar interbody fusion (PLIF). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
Fig. 2.
Mosaic plots with a cell-by-cell comparison of the observed and expected counts, calculated on standardized Pearson residuals. A standardized Pearson residuals that exceeds about two or three in absolute value indicates a lack of fit of the null hypothesis of independence in that specific cell. Blue colors indicate a higher observed count than expected; red colors indicate a lower observed count than expected under the null hypothesis of independence. Abbreviations. ALIF: anterior lumbar interbody fusion procedures; anes: pain physicians; DHS: herniated disc surgery; neur: neurosurgeons; orth: orthopedists; PLIF: posterior lumbar interbody fusion (PLIF). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
After surgery, the null hypothesis of independence was rejected between profession and response levels (χ2 = 29.48, df = 8, p < 0.001) as well as between type of surgery and response levels (χ2 = 27.57, df = 8, p < 0.001). After surgery, there were more pain physicians who never asked about sexual functionality than expected under independence. Standardized residuals indicated that for ALIF procedures, less physicians rarely discussed sexual functionality than expected, while more physicians always discussed this after ALIF (Fig. 2).
In terms of sexual satisfaction, before surgery, we could not reject the null hypothesis of independence between profession and response levels (χ2 = 13.06, df = 8, p = 0.11), nor between type of surgery and response levels (χ2 = 4.06, df = 8, p = 0.85). After surgery, the null hypothesis of independence between response levels and profession (χ2 = 12.58, df = 8, p = 0.13) and type of surgery (χ2 = 8.70, df = 8, p = 0.37) could not be rejected.
3.4. Communication regarding possible consequences of spinal surgery
In Table 2, the frequency of discussing possible consequences of spinal surgery are presented. Percentages of never discussing consequences range from 26.3% to 59.6% for male patients and from 42.1% to 66.7% for female patients. For erectile dysfunction, the null hypothesis of independence was rejected between profession and response levels (χ2 = 19.97, df = 8, p = 0.01) and between type of surgery and response levels (χ2 = 19.15, df = 8, p = 0.01). More neurosurgeons sometimes evaluated erectile dysfunction than expected. For ALIF procedures, more physicians always asked about erectile dysfunction than expected under independence.
Table 2.
Frequency of discussing potential consequences, namely erectile dysfunctions, retrograde ejaculation, alterations in orgasm and disturbed lubrication after different type of surgeries.
| Never | Rarely | Sometimes | Usually | Always | Missing value | |
|---|---|---|---|---|---|---|
| Discussions with male patients | ||||||
| Erectile dysfunction after ALIF | 15 (26.3%) | 3 (5.3%) | 4 (7.0%) | 3 (5.3%) | 12 (21.1%) | 20 (35.1%) |
| Erectile dysfunction after PLIF | 23 (40.4%) | 7 (12.3%) | 7 (12.3%) | 2 (3.5%) | 2 (3.5%) | 16 (28.0%) |
| Erectile dysfunction after HDS | 24 (42.1%) | 8 (14.0%) | 8 (14.0%) | 2 (3.5%) | 2 (3.5%) | 13 (22.8%) |
| Retrograde ejaculation after ALIF | 19 (33.3%) | 4 (7.0%) | 2 (3.5%) | 2 (3.5%) | 9 (15.8%) | 21 (36.8%) |
| Retrograde ejaculation after PLIF | 32 (56.1%) | 7 (12.3%) | 2 (3.5%) | 0 (0%) | 0 (0%) | 16 (28.0%) |
| Retrograde ejaculation after HDS | 34 (59.6%) | 9 (15.8%) | 1 (1.8%) | 0 (0%) | 0 (0%) | 13 (22.8%) |
| Discussions with female patients | ||||||
| Abnormal orgasms after ALIF | 24 (42.1%) | 2 (3.5%) | 5 (8.8%) | 1 (1.8%) | 4 (7.0%) | 21 (36.8%) |
| Abnormal orgasms after PLIF | 32 (56.1%) | 6 (10.5%) | 2 (3.5%) | 1 (1.8%) | 0 (0%) | 16 (28.0%) |
| Abnormal orgasms after HDS | 34 (59.6%) | 8 (14.0%) | 2 (3.5%) | 0 (0%) | 0 (0%) | 13 (22.8%) |
| Disturbed lubrification after ALIF | 27 (47.4%) | 3 (5.3%) | 1 (1.8%) | 1 (1.8%) | 4 (7.0%) | 21 (36.8%) |
| Disturbed lubrification after PLIF | 34 (59.6%) | 4 (7.0%) | 2 (3.5%) | 0 (0%) | 0 (0%) | 17 (29.8%) |
| Disturbed lubrification after HDS | 38 (66.7%) | 3 (5.3%) | 2 (3.5%) | 0 (0%) | 0 (0%) | 14 (24.6%) |
When exploring retrograde ejaculation, the null hypothesis of independence was rejected between profession and response levels (χ2 = 22.56, df = 8, p = 0.004) and between type of surgery and response levels (χ2 = 29.86, df = 8, p < 0.001). For ALIF procedures, more physicians always asked about retrograde ejaculation than expected under independence.
The frequency of sometimes asking about alterations in orgasm as orthopedist was higher than expected. For ALIF procedures, alterations in orgasm was a fixed component (i.e., always discussed) of the consultation more than expected. Independence was rejected between type of surgery and response levels (χ2 = 16.36, df = 8, p = 0.04) as well as between profession and response levels (χ2 = 25.05, df = 8, p = 0.001).
For disturbed lubrication, the null hypothesis of independence could not be rejected between profession and response levels (χ2 = 12.13, df = 8, p = 0.14), nor between type of surgery and response levels (χ2 = 12.45, df = 8, p = 0.13).
3.5. Knowledge and opinion
In total, 77.2% (44/57) of the physicians was aware of the potential negative effects of spinal surgery on sexual health, while 47.4% (27/57) has knowledge about the potential positive effects of spinal surgery on this factor. Twelve physicians (21.1%) indicated that they have knowledge about recommended intercourse positions to avoid pain in lower back pain patients, of whom 2/12 never gave this advice to patients, 8/12 rarely and 2/12 sometimes. Sixty-one percent of physicians did not know a sexologist in the neighborhood, 24.5% knew a sexologist and 14% did not answered this question. Of the physicians who knew a sexologist, only 28.5% sometimes referred to those healthcare providers. Twenty physicians (35.1%) are convinced that patients have the responsibility to address the topic of sexual problems, while 24 (42.1%) physicians do not support this statement. Systematically evaluating sexual health in patients with spinal pain should not be conducted as a standard routine according to 47.36% of the physicians (compared to 31.6% who supports this approach). Most healthcare providers (n = 41, 71.9%) found that more attention should be paid to the sexual counseling in spinal patients during their professional training.
4. Discussion
This survey demonstrated that sexual counseling by healthcare providers only occurs in a minority of spinal patients who are eligible for spine surgery. Of the 57 participants, more than half (61.4%) of the physicians rarely or never discuss sexual concerns with their patients, and a minority (14%) effectively discussed sexual health on a regular basis. Communication on sexual disturbances was independent of profession, meaning that no differences were found between orthopedic surgeons, neurosurgeons and pain management physicians. Several studies showed that sexual activity is severely impacted in spinal patients (Pakpour et al., 2015; Ambler et al., 2001; Maigne and Chatellier, 2001), which in turn negatively influences quality of life (Stephenson et al., 2015). In addition, spinal surgery can induce a positive as well as a negative effect on the patient's sex life (Hägg et al., 2006; Akbaş et al., 2010), an aspect that merits counseling as well. In general, our study confirmed the findings of Korse et al. (2016) where it was revealed that 73% of the neurosurgeons (almost) never discussed sexual health with their patients. Presumably, this may be explained by the lack of training or the taboo character of the topic in spinal care (Bahouq et al., 2013; Korse et al., 2016). In other disciplines, however, sexual health is often discussed. A recent study revealed that after pelvic reconstructive surgery, nearly all surgeons included counseling on the safety of intercourse and reassurance that intercourse would not harm the surgical repair (Caldwell et al., 2023). Qualitative research revealed that specific suggestions were provided among which advice concerning different positions, use of lubrication, vaginal estrogen use, specific products/vendors, alternatives to (vaginal) intercourse, and the importance of foreplay (Caldwell et al., 2023).
With respect to sexual functionality, there were more pain physicians who never asked about sexual functionality than expected. This finding may be explained by the type of profession of pain physicians, with a more consulting function (Verma et al., 2015) compared to the surgical disciplines and the fact that they do not perform the procedures themselves. Additionally, more orthopedists always discussed sexual functionality before surgery, which could be a reflection of the type of procedures they perform, since orthopedic surgeons are more exposed to instrumentation and osseous fixation techniques during their residency training (Prabhakar et al., 2020). For ALIF procedures, more physicians discussed sexual functionality (both before and after surgery), presumably due to the higher risk of dysfunctions for sexual functioning with ALIF procedures (Bhambhvani et al., 2022).
Our survey showed that counseling about sexual health related consequences, namely erectile dysfunction, retrograde ejaculation, and alterations in orgasms depended on the surgical procedure that is proposed, except for disturbed lubrication. In patients who underwent an ALIF, physicians more often always discussed erectile dysfunction, retrograde ejaculation, and alterations in orgasms with their patients after surgery. These findings could imply that surgery-related sexual problems are underreported in the setting of PLIF or HDS. In terms of clinical outcome, there is no generally accepted superior approach to perform a lumbar interbody fusion procedure yet (Mobbs et al., 2015). The choice of the procedure might be influenced by the perception that previously mentioned consequences are unique to anterior approaches (Comer et al., 2012; Body et al., 2021; Malham et al., 2014). Nevertheless, it was recently revealed that type of spine surgery is not a predictor of developing delayed ejaculation in multivariable regression (Bhambhvani et al., 2022). However, if sexual complications could be underreported in posterior approaches due to a lack of communication, this may have a major impact on surgical decision-making.
Another important observation of this study is that retrograde ejaculation and erectile dysfunction in males were more frequently discussed than alterations in orgasms and disturbed lubrication in females. These findings illustrate that there is a disparity between sex in the assessment of sexual problems in spinal patients. Korse et al. previously already found that sexual health was discussed significantly more often with male compared to female patients, regardless of the sex of the physician (Korse et al., 2016). However, no comparison was included for communication about possible consequences of spinal surgery solely affecting males and females, whereby the current study provides more details about the inequality of sexual counseling based on the patient's sex. It is important that healthcare providers are aware of this sex bias. Especially since it has been denoted that patients find it easier to discuss sexual concerns with physicians of the same gender (Ryan et al., 2018). A more in depth insight may ultimately lead to a uniform treatment of male and female patients with standardized guidelines for sexual activity and sexual counseling following spinal surgery, which are currently still lacking (Thomas et al., 2019).
The majority of respondents (77.2%) was aware of a potential negative impact of spinal surgery on the patient's sex life. However, only 47.4% of the respondents knew about its potential benefits. It is therefore important to spread awareness that sexual health can be improved by spinal surgery (Sahin et al., 2022; Holmberg et al., 2021). The fact that surgery can improve the patient's sex life (Berg et al., 2009) might help to identify candidates for surgery. However, before considering pre-existing sexual problems as a parameter for surgical decision-making, physicians are encouraged to start discussing sexual health and the related problems with their patients.
Bahouq et al. showed that most patients with chronic low back pain are willing to talk to their physician about their sex life (Bahouq et al., 2013). However, most patients expect the physician to initiate this topic (Meystre-Agustoni et al., 2011; Metz et al., 1990). However, 35.1% of the healthcare providers surveyed, believed it is the patient's responsibility to initiate that conversation. The discrepancy in the sense of responsibility is of interest and could be the subject of future research. Also more in depth interviews for each specialty separately could be very interesting, to gain better insights in the decision-making process about why/when sexual health is discussed. Campaigns could be developed to raise awareness of the high importance of sexual health for quality of life and the patient's desire to discuss sexual problems.
The fact that the vast majority of physicians (71.9%) agreed to the statement that more attention should be paid to the sexual health of spinal patients during the education of young healthcare professionals, indicates that physicians are willing to accept an advanced training as part of their further education. Previous studies have identified a lack of knowledge and personal discomfort as two of the main barriers preventing an open discussion on sexual health (Korse et al., 2016; Rosen et al., 2006). However, both items can be improved by dedicated training. Rosen et al. showed that after a half-day workshop, participants were already more comfortable with the topic and that they were more inclined to address sexual issues in the future (Rosen et al., 2006). As such, training in communication about sexual problems should probably be integrated in the curriculum of healthcare providers. Creating more awareness about sexual functioning and spinal surgery, properly training healthcare providers on sexual health education and exploring the concrete information that patients aim to receive, may be the first steps before practice guidelines can be provided about what type of information should exactly be provided to patients during consultations.
Despite the further elaboration on sexual health in relation to spine care, one of the main limitations is the small sample size and low response rate. The survey was distributed through the chairs of the different organizations, whereafter they were distributed to the members of each organization. Therefore, it is impossible to estimate the true response rate on this survey, potentially jeopardizing the overall generalizability of the results. Moreover, we cannot exclude a selection bias as physicians interested in the topic of sexual health could have responded more often than others, resulting in an overestimation of discussing sexual health amongst healthcare professionals. Furthermore, our study could be culturally biased since only orthopedic surgeons, neurosurgeons and pain management specialists practicing in Belgium and The Netherlands were surveyed. Since we believe communication on sexual health is strongly influenced by socio-cultural factors (Dialmy, 2010), future research is needed to extend knowledge to other cultures and countries.
5. Conclusion
Overall, neurosurgeons, orthopedic surgeons, and pain specialists rarely addressed sexual problems in patients with spinal pain. The frequency of discussing potential consequences on sexual health are less often conducted in females compared to males. Sexual health counseling should be provided to all patients eligible for spine surgery, regardless of their sex, type of proposed surgery and the physician they are consulting. To improve communication around sexual health, advanced training for healthcare professionals is needed.
Author contributions
Conceptualization, David van Schaik, Lisa Goudman.
Methodology, David van Schaik, Lisa Goudman, Maarten Moens.
Formal analysis, David van Schaik, Lisa Goudman.
Investigation, David van Schaik, Tjeerd Jager.
Writing- original draft preparation, David van Schaik, Lisa Goudman, Tjeerd Jager.
Writing-review and editing: all authors.
Visualization, Lisa Goudman.
Supervisison, Thierry Scheerlinck, Maarten Moens.
All Authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional review board statement
This study was approved by the Institutional Ethics Committee of UZ Brussel, Belgium (B.U.N. 143201837053) on 20th March 2019.
Declaration of competing interest
Goudman is a postdoctoral research fellow funded by the Research Foundation Flanders (FWO), Belgium (project number 12 ZF622N). Maarten Moens has received speaker fees from Medtronic and Nevro, outside the submitted work. STIMULUS received research grants from Medtronic. There are no other conflicts of interests to declare.
Acknowledgements
The authors would like to thank Jannik Heemann for his help with conducting the study.
Handling Editor: Prof F Kandziora
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bas.2024.102776.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Agresti A. second ed. ed. John Wiley & Sons Inc; New York: 2002. Categorical Data Analysis. [Google Scholar]
- Akbaş N.B., Dalbayrak S., Külcü D.G., Yilmaz M., Yilmaz T., Naderi S. Assessment of sexual dysfunction before and after surgery for lumbar disc herniation. J. Neurosurg. Spine. 2010;13:581–586. doi: 10.3171/2010.5.Spine09906. [DOI] [PubMed] [Google Scholar]
- Ambler N., Williams A.C., Hill P., Gunary R., Cratchley G. Sexual difficulties of chronic pain patients. Clin. J. Pain. 2001;17:138–145. doi: 10.1097/00002508-200106000-00006. [DOI] [PubMed] [Google Scholar]
- Bahouq H., Allali F., Rkain H., Hajjaj-Hassouni N. Discussing sexual concerns with chronic low back pain patients: barriers and patients' expectations. Clin. Rheumatol. 2013;32:1487–1492. doi: 10.1007/s10067-013-2299-y. [DOI] [PubMed] [Google Scholar]
- Berg S., Fritzell P., Tropp H. Sex life and sexual function in men and women before and after total disc replacement compared with posterior lumbar fusion. Spine J. 2009;9:987–994. doi: 10.1016/j.spinee.2009.08.454. [DOI] [PubMed] [Google Scholar]
- Bhambhvani H.P., Kasman A.M., Zhang C.A., Hu S.S., Eisenberg M.L. Delayed ejaculation after lumbar spine surgery: a claims database analysis. Global Spine J. 2022;12:663–667. doi: 10.1177/2192568220962435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Body A.M., Plummer Z.J., Krueger B.M., Virojanapa J., Nasser R., Cheng J.S., Prestigiacomo C.J. Retrograde ejaculation following anterior lumbar surgery: a systematic review and pooled analysis. J. Neurosurg. Spine. 2021;35:427–436. doi: 10.3171/2020.12.SPINE201101. [DOI] [PubMed] [Google Scholar]
- Boul L. Sexual function and relationship satisfaction: an investigation into men's attitudes and perceptions. Sex. Relatsh. Ther. 2007;22:209–220. [Google Scholar]
- Caldwell L., Kim-Fine S., Antosh D.D., Husk K., Meriwether K.V., Long J.B., Heisler C.A., Hudson P.L., Lozo S., Iyer S., et al. Surgeon counseling regarding return to sexual activity after pelvic reconstructive surgery. Urogynecology. 2023 doi: 10.1097/SPV.0000000000001338. 10.1097/SPV.0000000000001338. [DOI] [PubMed] [Google Scholar]
- Comer G.C., Smith M.W., Hurwitz E.L., Mitsunaga K.A., Kessler R., Carragee E.J. Retrograde ejaculation after anterior lumbar interbody fusion with and without bone morphogenetic protein-2 augmentation: a 10-year cohort controlled study. Spine J. 2012;12:881–890. doi: 10.1016/j.spinee.2012.09.040. [DOI] [PubMed] [Google Scholar]
- Dialmy A. Sexuality and islam. Eur. J. Contracept. Reprod. Health Care. 2010;15:160–168. doi: 10.3109/13625181003793339. [DOI] [PubMed] [Google Scholar]
- Ferrari S., Vanti C., Frigau L., Guccione A.A., Mola F., Ruggeri M., Pillastrini P., Monticone M. Sexual disability in patients with chronic non-specific low back pain-a multicenter retrospective analysis. J. Phys. Ther. Sci. 2019;31:360–365. doi: 10.1589/jpts.31.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer C.R., Braaksma B., Peters A., Weinreb J.H., Nalbandian M., Spivak J.M., Petrizzo A. Outcomes and complications of the midline anterior approach 3 years after lumbar spine surgery. Adv. Orthop. 2014;2014 doi: 10.1155/2014/142604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flynn K.E., Lin L., Bruner D.W., Cyranowski J.M., Hahn E.A., Jeffery D.D., Reese J.B., Reeve B.B., Shelby R.A., Weinfurt K.P. Sexual satisfaction and the importance of sexual health to quality of life throughout the life course of U.S. Adults. J. Sex. Med. 2016;13:1642–1650. doi: 10.1016/j.jsxm.2016.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes M.K., Eaton N.R., Krueger R.F. Sexual quality of life and aging: a prospective study of a nationally representative sample. J. Sex. Res. 2017;54:137–148. doi: 10.1080/00224499.2016.1233315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hägg O., Fritzell P., Nordwall A. Sexual function in men and women after anterior surgery for chronic low back pain. Eur. Spine J. 2006;15:677–682. doi: 10.1007/s00586-005-1017-0. official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmberg S.T., Vangen-Lønne V., Gulati A.M., Nygaard Ø P., Solberg T.K., Salvesen Ø O., Gulati S. Pain during sex before and after decompressive surgery for lumbar spinal stenosis: a multicenter observational study. Spine. 2021;46:1354–1361. doi: 10.1097/brs.0000000000004008. [DOI] [PubMed] [Google Scholar]
- Korse N.S., Nicolai M.P., Both S., Vleggeert-Lankamp C.L., Elzevier H.W. Discussing sexual health in spinal care. Eur. Spine J. 2016;25:766–773. doi: 10.1007/s00586-015-3991-1. official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. [DOI] [PubMed] [Google Scholar]
- Łabuz-Roszak B., Babińska A., Skupiński J., Czech E., Szczygieł J., Wawrzynek W. [Sexual quality of life in patients with low back pain and the radiological changes evaluated in magnetic resonance] Wiad. Lek. 2018;71:1039–1045. [PubMed] [Google Scholar]
- Laldjising E., Sekercan A., Gadjradj P.S. Neurosurgeons' opinions on discussing sexual health among brain tumor patients: room for improvement? J. Clin. Neurosci. 2021;94:292–297. doi: 10.1016/j.jocn.2021.10.040. [DOI] [PubMed] [Google Scholar]
- Maigne J.Y., Chatellier G. Assessment of sexual activity in patients with back pain compared with patients with neck pain. Clin. Orthop. Relat. Res. 2001:82–87. doi: 10.1097/00003086-200104000-00014. 10.1097/00003086-200104000-00014. [DOI] [PubMed] [Google Scholar]
- Malham G.M., Parker R.M., Ellis N.J., Blecher C.M., Chow F.Y., Claydon M.H. Anterior lumbar interbody fusion using recombinant human bone morphogenetic protein-2: a prospective study of complications. J. Neurosurg. Spine. 2014;21:851–860. doi: 10.3171/2014.8.Spine13524. [DOI] [PubMed] [Google Scholar]
- McCabe M., Althof S.E., Assalian P., Chevret-Measson M., Leiblum S.R., Simonelli C., Wylie K. Psychological and interpersonal dimensions of sexual function and dysfunction. J. Sex. Med. 2010;7:327–336. doi: 10.1111/j.1743-6109.2009.01618.x. [DOI] [PubMed] [Google Scholar]
- Mercer C.H., Fenton K.A., Johnson A.M., Wellings K., Macdowall W., McManus S., Nanchahal K., Erens B. Sexual function problems and help seeking behaviour in Britain: national probability sample survey. BMJ. 2003;327:426–427. doi: 10.1136/bmj.327.7412.426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metz M.E., Seifert M.H., Jr. Men's expectations of physicians in sexual health concerns. J. Sex Marital Ther. 1990;16:79–88. doi: 10.1080/00926239008405254. [DOI] [PubMed] [Google Scholar]
- Meystre-Agustoni G., Jeannin A., de Heller K., Pécoud A., Bodenmann P., Dubois-Arber F. Talking about sexuality with the physician: are patients receiving what they wish? Swiss Med. Wkly. 2011;141 doi: 10.4414/smw.2011.13178. [DOI] [PubMed] [Google Scholar]
- Mitchell K.R., Mercer C.H., Ploubidis G.B., Jones K.G., Datta J., Field N., Copas A.J., Tanton C., Erens B., Sonnenberg P., et al. Sexual function in Britain: findings from the third national survey of sexual attitudes and lifestyles (Natsal-3) Lancet. 2013;382:1817–1829. doi: 10.1016/s0140-6736(13)62366-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mobbs R.J., Phan K., Malham G., Seex K., Rao P.J. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. Journal of spine surgery (Hong Kong) 2015;1:2–18. doi: 10.3978/j.issn.2414-469X.2015.10.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moscicki P., Bachmann G.A. Characterization of female sexual dysfunction associated with spinal pathology and surgery. Sex Med Rev. 2022;10:493–498. doi: 10.1016/j.sxmr.2022.01.003. [DOI] [PubMed] [Google Scholar]
- Pakpour A.H., Nikoobakht M., Campbell P. Association of pain and depression in those with chronic low back pain: the mediation effect of patient sexual functioning. Clin. J. Pain. 2015;31:44–51. doi: 10.1097/ajp.0000000000000076. [DOI] [PubMed] [Google Scholar]
- Panneerselvam K., Kanna R.M., Shetty A.P., Rajasekaran S. Impact of acute lumbar disk herniation on sexual function in male patients. Asian Spine J. 2022;16:510–518. doi: 10.31616/asj.2021.0083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prabhakar G., Kusnezov N., Dunn J., Cleveland A., Herzog J. Orthopaedics and neurosurgery: is there a difference in surgical outcomes following anterior cervical spinal fusion? J. Orthop. 2020;21:278–282. doi: 10.1016/j.jor.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao P.J., Loganathan A., Yeung V., Mobbs R.J. Outcomes of anterior lumbar interbody fusion surgery based on indication: a prospective study. Neurosurgery. 2015;76:7–23. doi: 10.1227/neu.0000000000000561. discussion 23-24. [DOI] [PubMed] [Google Scholar]
- Rosen R., Kountz D., Post-Zwicker T., Leiblum S., Wiegel M. Sexual communication skills in residency training: the Robert Wood Johnson model. J. Sex. Med. 2006;3:37–46. doi: 10.1111/j.1743-6109.2005.00135.x. [DOI] [PubMed] [Google Scholar]
- Ryan K.L., Arbuckle-Bernstein V., Smith G., Phillips J. Let's talk about sex: a survey of patients' preferences when addressing sexual health concerns in a family medicine residency program office. PRiMER. 2018;2:23. doi: 10.22454/PRiMER.2018.728252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahin C.U., Aydin M., Kalkisim S., Sahin H., Arslan F.C. Comparison of preoperative and postoperative sexual dysfunction in male patients with lumbar disc herniation. Turk. Neurosurg. 2022;32:442–448. doi: 10.5137/1019-5149.Jtn.35810-21.2. [DOI] [PubMed] [Google Scholar]
- Stephenson K.R., Meston C.M. The conditional importance of sex: exploring the association between sexual well-being and life satisfaction. J. Sex Marital Ther. 2015;41:25–38. doi: 10.1080/0092623x.2013.811450. [DOI] [PubMed] [Google Scholar]
- Thomas C.M., Levene H.B. Lack of current recommendations for resuming sexual activity following spinal surgery. Asian Spine J. 2019;13:515–518. doi: 10.31616/asj.2018.0106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verma R., Mohan B., Attri J.P., Chatrath V., Bala A., Singh M. Anesthesiologist: the silent force behind the scene. Anesth. Essays Res. 2015;9:293–297. doi: 10.4103/0259-1162.159775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wuertz-Kozak K., Bleisch D., Nadi N., Prömmel P., Hitzl W., Kessler T.M.M., Gautschi O.P., Hausmann O.N. Sexual and urinary function following anterior lumbar surgery in females. Neurourol. Urodyn. 2019;38:632–636. doi: 10.1002/nau.23874. [DOI] [PubMed] [Google Scholar]
- Yeh H.C., Lorenz F.O., Wickrama K.A., Conger R.D., Elder G.H., Jr. Relationships among sexual satisfaction, marital quality, and marital instability at midlife. J. Fam. Psychol. 2006;20:339–343. doi: 10.1037/0893-3200.20.2.339. [DOI] [PubMed] [Google Scholar]
- Zeileis A., Meyer D., Hornik K. Residual-based shadings for visualizing (conditional) independence. J. Comput. Graph Stat. 2007;16:507–525. doi: 10.1198/106186007x237856. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.