Abstract
Posterior pilon variant ankle fractures (PPVF) are a unique subtype of posterior malleolar fractures which have been a source of controversy and confusion in recent years. There has not been a thorough literature review previously written on the topic. Database searches of PubMed and Embase were conducted from inception until June 2023. The key words included “pilon variant,” “posterior pilon variant,” and “posterior pilon” fractures. Outcomes were evaluated by union time, rates of delayed union, nonunion, malunion, and complication. A total of 15 articles relevant to surgical repair of pilon variant fractures were included in the literature review. The unique mechanism of injury has been reported to involve both rotational and axial forces, leading to involvement of the posterior and medial aspects of the distal tibia. Pilon variant fractures can be suspected by several characteristics on radiographs and have a high confirmation rate via CT images. Multiple systems have been proposed to classify this fracture pattern, but there is no consensus on the ideal classification system. Surgically, direct fixation has shown better short-term clinical outcomes versus indirect fixation or no fixation. PPVF have a distinct fracture pattern involving the posterior and medial columns of the distal tibial plafond, and results from a mechanism intermediate to rotational and axial forces. These fractures are more severe than tri-malleolar fractures due to increased rates of articular impaction and incongruity. Future classification systems should focus on joint surface area and the tibial pilon column involved to avoid confusion with less severe posterior malleolar fractures.
Keywords: Ankle fracture, Posterior malleolar fracture, Pilon variant, Posterior pilon, Posterior pilon variant, Tri-malleolar fracture
1. Introduction
Posterior Pilon variant fractures (PPVF) are a unique type of fracture described in recent medical literature involving the posterior column of the distal tibia at the ankle joint pilon. Few manuscripts have been written describing these fractures, and those published demonstrate inconsistency and confusion surrounding diagnosis, classification, and treatment. In 2001, Karachalios described a tri-malleolar fracture involving two fragments of the posterior malleolus, a posteromedial and posterolateral fragment.1 In 2004, Weber described a similar pattern involving multi-fragmentary fractures of the entire posterior tibial lip, including the posterior colliculus (PC) of the medial malleolus (MM). Of the two major fracture fragments, the posteromedial fragment, involving the posterior colliculus, was always larger than the posterolateral fragment.2 This larger posteromedial fragment compromises the integrity of the posterior aspect of the ankle joint, increasing the risk of posteromedial talar subluxation if not properly treated. Hansen introduced the term “posterior pilon” to describe severe tri-malleolar fractures involving the posterior tibial plafond, noting that they often involve additional bone fragments located deeper than the avulsed posterior fragment.3
The terms “pilon variant,” “posterior pilon,” and “posterior pilon variant” have been used to describe similar fracture patterns of the posterior tibia.4, 5, 6, 7 While some papers use the term pilon fracture to define any fracture of the distal tibial plafond, this paper will only focus on fractures of posterior aspect.8 Currently, there is a lack of consistency regarding what ankle fractures are classified as PPVF, and what classifications separate more and less severe subtypes. This systematic review aims to answer three specific questions: 1) How are PPVF described in current orthopedic literature? 2) What systems are used to classify PPVF? 3) Do newer surgical approaches provide better outcomes than the traditional posterolateral approach?
2. Methods
2.1. Search strategy
A systematic literature review of PPVF was completed on June 15, 2023. The search was conducted through PubMed and Embase, using the following search strategy: (pilon variant) OR (posterior pilon)) AND (fracture). Reference lists of relevant review articles and articles included in this paper were further reviewed for related content. There was no limitation on publishing journal or publication date.
2.2. Study selection
Any articles duplicated between the two databases were removed prior to screening. Studies discussing pilon ankle fractures were screened for PPVF specificity. This included articles discussing classification, mechanism of injury, management, and outcomes. Titles and abstracts were screened for exclusion criteria by 3 independent reviewers (KB, DP, EL). Any disagreements were reviewed collectively, and a final decision was made. Articles passing title and abstract screening were collected as full text PDFs and further screened by the same three reviewers (KB, DP, EL). Cadaveric studies, biomechanical studies, non-clinical studies, and studies not published in English were excluded.
2.3. Data extraction
Data extraction was performed using Microsoft Excel Spreadsheet by 3 reviewers (KB, DP, EL). Data extracted included: Author, sample size, study type, surgical treatment method, mean follow-up, union time, rates of delayed union, nonunion, malunion, complications, and AOFAS score. Outcomes were evaluated by union time, rates of delayed union, nonunion, malunion, complications, and AOFAS score. Time to union and AOFAS scores were analyzed using one-way ANOVA. Complication rates between surgical approaches could not be analyzed using Fisher's exact test due to the small sample size of reported data.
2.4. Quality assessment
To assess the research quality of each included study, a modified version of the Coleman Methodology Score (CMS) was applied by two independent reviewers (EL, JL). The scale consists of ten criteria divided into two parts, which aim to assess the overall quality of research and elimination of bias. Part A assesses study size, mean follow-up, number of surgical procedures per outcome, study design, diagnostic certainty, procedure description, and postoperative rehabilitation description and compliance. Part B assesses outcome criteria, the procedure employed for outcome assessment, and the subject selection process. Scores range from 0 to 100, with a score of 100 representing a study that avoids the influence of chance, bias, and confounding factors.9
3. Results
3.1. Search results
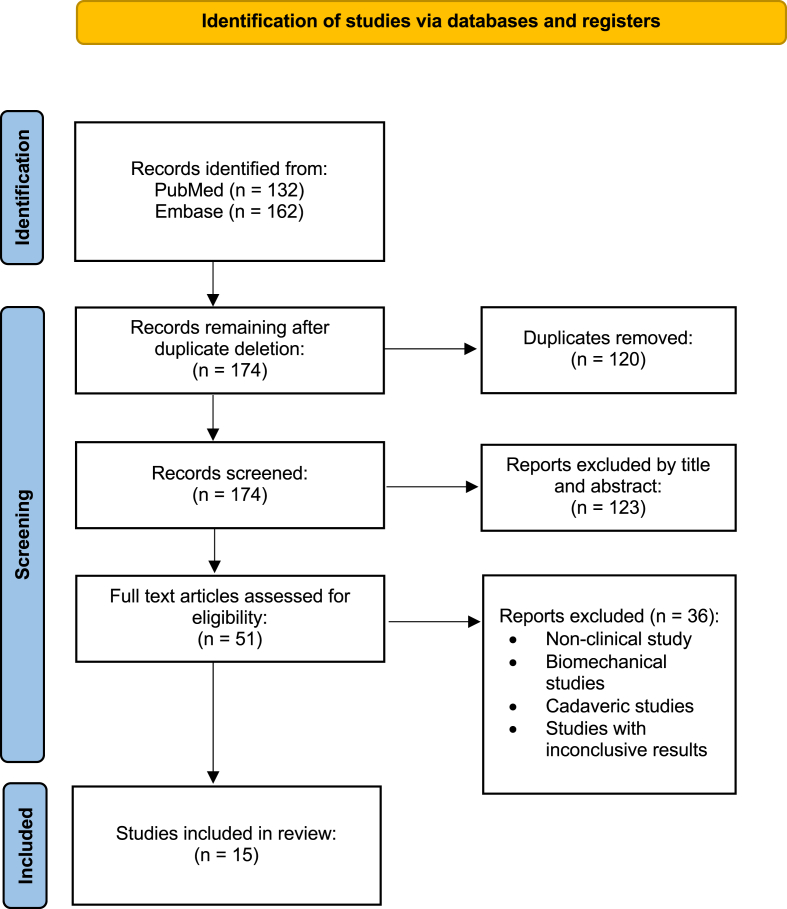
A thorough literature search was conducted on PubMed and Embase, with 294 potentially relevant articles were retrieved. After the removal of duplicates, titles and abstracts were screened for inclusion, with 51 articles collected for full text review. After applying exclusion criteria, 15 articles were included in the current review. The selection process was performed according to “Preferred Reporting Items for Systematic Review and Meta-Analyses” (PRISMA) and a flowchart demonstrating the selection progression is shown in Fig. 1.10
Fig. 1.
Prisma flowchart for systematic review process.
3.2. Study characteristics
15 studies were included in the systematic review. Of the articles included, 13 were retrospective and 2 were prospective. There were 361 total subjects, with 13 studies reporting gender demographics (M: F = 125:197, n = 322). All but two studies reported mean and age range of participants; one study reported only mean age and another study did not report any age demographics. Of those reporting age, the weighted mean age was 48.6 years (Range = 18–88). Thirteen studies reported follow-up information, with a mean follow-up time of 22.3 months (Range = 12–37.1 mo). Surgical approaches and the number of papers investigating each approach were as follows: Posterolateral (PL) alone (n = 9), posteromedial (PM) alone (n = 2), modified posteromedial (MPM) approach (n = 3), combined PM and PL (n = 5), PM and lateral approach (n = 1), posterior arthroscopic-assisted reduction internal fixation (PAARIF) (n = 1), and open fibula fracture line technique (n = 1). The Modified CMS was low across all studies, with an average of 44.9, ranging from 26 to 59 points. A complete summary of study characteristics and outcome metrics collected is shown in Table 1.
Table 1.
Study characteristics.
| Author | Patients | M/F | Treatment method | AOFAS | Mean follow-up (months) | Study type | Modified CMS |
|---|---|---|---|---|---|---|---|
| Weber 20042 | 10 | – | PL/PM | 94.3 | 15.7 | RS | 45 |
| Martin 202011 | 29 | – | PAARIF | 88.1 | 12 | CS | 36 |
| Zhang et al., 201912 | 36 | 18/18 | 1) PL2) PL/PM | 82.5 | 28.2 | RS | 52 |
| Black et al., 202213 | 68 | 17/51 | 1) PM or PL 2) indirect fixation 3) no fixation |
– | >12 | RS | 39 |
| Klammer et al., 201314 | 11 | 2/9 | PL | 82 | 22.7 | RS | 42 |
| Wang et al., 20164 | 16 | 4/12 | Modified PM | 85.6 | 30.1 | PS | 59 |
| Dwivedi et al., 201815 | 13 | 10/3 | PL w/buttress plating | 90.38 | 18.5 | RS | 42 |
| Gao et al., 201916 | 23 | 9/14 | PL | 82.3 | 14.5 | RS | 49 |
| Sukur et al., 201717 | 14 | 8/6 | 1) PL/PM 2) PM/Lateral | 83.7 | 17.1 | RS | 45 |
| Chen et al., 201418 | 10 | 7/3 | 1) PL 2) PL/PM | 87.8 | 36.2 | RS | 47 |
| Amorosa et al., 201019 | 15 | 4/11 | 1) PL 2) PM 3) PL/PM |
– | 37.1 | RS | 42 |
| Lei et al., 201120 | 12 | 5/7 | PL/PM | 85.7 | 18.9 | RS | 50 |
| Chaparro et al., 201921 | 25 | 6/19 | 1) Modified PM 2) PL |
– | 21.7 | CS | 26 |
| Zhang et al., 202222 | 20 | 7/13 | Modified PM | 80.55 | 16.95 | RS | 56 |
| Jiang et al., 202223 | 59 | 28/31 | 1) Open fibula fracture line technique 2) PL |
1) 86.6 2) 82.7 |
– | RS | 44 |
PM = posteromedial, PL = posterolateral, PAARIF = posterior arthroscopic-assisted reduction internal fixation, RS = retrospective study, CS = case series, PS = prospective study.
3.3. Mechanism of injury
Mechanisms leading to PPVF included motor vehicle accidents, falls from a height, and falls on ground level/while walking.4,12,15-19The mechanism is a combination of low energy torsion and high energy compression, believed to result from external rotation and abduction of a plantarflexed foot with a loaded talus.24 PPVF fractures can present similarly to rotational fractures described by the Lauge Hansen classification, but unlike rotational tri-malleolar ankle injuries, the PPVF fracture lines extend proximally and medially, through the medial malleolus. Furthermore, fractures commonly occur in the coronal plane, unlike traditional high energy pilon fractures that typically split in the sagittal plane.4 This combined injury mechanism can lead to large, comminuted and/or impacted posterior malleolar fragments that are unique to PPVF.4,18,25
When assessing fracture morphology and mechanism of injury, fractures with a larger posteromedial fragment are typically severe and result in articular impaction of the tibial aspect of the ankle joint. PPVF are highly associated with the supination external rotation (SER) mechanism of injury while traditional avulsion posterior malleolar fractures (PMF) correlate with a pronation external rotation (PER) mechanism. Note, however, neither fracture pattern is exclusive to one mechanism of injury.26 The lack of an exclusive correlation between mechanism and morphology emphasizes the importance of advanced imaging, such as computed tomography (CT) when diagnosing moderate to severe ankle injuries and planning surgical management.4
3.4. Diagnosis and morphology
Several radiographic imaging signs have been described that can assist in making a diagnosis of PPVF. The double contour sign, which can be seen on anterior posterior (AP) radiographs, is defined as a double contour line on the medial aspect of the radiograph superior to the medial malleolus and produced by dislocation of the medial ankle fracture fragment. This pattern is highly associated with PPVF, seen in all but one case studied by Weber et al.2 When using this sign combined with the presence of a sagittal split of the posterior malleolus to diagnosis a posterior pilon variant, one study found up to 20% of operative ankle fractures could be classified as pilon variants using preoperative radiographs, and 40% of fractures with a PMF are actually posterior pilon variants.6 This is the highest reported rate of PPVF to date, more than double the 8% incidence reported by Weber in 2004.2 A double joint line on lateral radiographs has also been used to make a diagnosis, resulting from the proximal displacement of the posterior bone fragment in fractures involving the entire width of the posterior tibial column.2,4,6,14
While plain radiographs can be utilized to identify fractures that are potentially PPVF, CT examination is the preferred imaging modality for definitive diagnosis and preoperative surgical planning. The three-dimensional aspect of CT provides more information regarding complex ankle injuries that can be used to differentiate PPVF from PMF, including fracture line orientation and the amount of the tibial surface involved. When compared to PMF on CT, PPVF have a significantly greater angle between the major fracture line and the intermalleolar axis, involve a greater proportion of the weightbearing surface of the tibia, and involve a greater proportion of the cross-sectional area of the distal tibia on axial CT images.4,24
3.5. Classification systems
Six fracture classification systems were used across 9 papers, including the AO Foundation/Orthopaedic Trauma Association (AO/OTA) (n = 5), Klammer (n = 4), Lauge Hansen (n = 2), Lei (n = 2), Zhang (n = 1), and Yu fracture classification systems (n = 1) (Table 2). A written summary and explanation of each classification system is provided in Table 3, excluding the AO/OTA and Lauge Hansen systems. These systems have been well described in previous literature and are not specific to PPVF. The AO/OTA 44 subgroup is for malleolar ankle fractures, with major divisions within this subgroup based on the location of the fibular fracture relative to the tibiofibular syndesmosis. The only subgroup that specifically mentions a PMF is the 44C2.3, described as a “supra-syndesmotic fibula fracture with medial and posterior malleolus tibia fracture.”27 Within the Lauge Hansen classification system, SER, PER, and pronation abduction (PAB) all can result in PMF if the mechanism is severe enough; however, these subgroups do not always result in a PPVF, and therefore more specific classification systems based on morphology rather than mechanism should be used.28
Table 2.
Classification systems utilized in included papers.
| Author | Classification system | Classification subgroup | Total cases reported |
|---|---|---|---|
| 1.Weber | AO/OTA | 44B3.2 | 7 |
| 44C2.3 | 3 | ||
| 3.Zhang | Yu | II | 1 |
| IIa | 9 | ||
| IIb | 6 | ||
| III | 9 | ||
| Klammer | I | 12 | |
| II | 14 | ||
| III | 10 | ||
| Zhang | I | 12 | |
| IIa | 10 | ||
| IIb | 4 | ||
| IIIa | 6 | ||
| IIIb | 4 | ||
| 5.Klammer | Klammer | I | 1 |
| II | 2 | ||
| III | 8 | ||
| 6.Wang | AO/OTA | 44-B3.2 | 12* |
| 44-C2.3 | 4* | ||
| Lauge Hansen | SER | 12* | |
| PER | 4* | ||
| 8.Gao | Klammer | I | 5 |
| II | 10 | ||
| III | 8 | ||
| AO/OTA | B3 | 5 | |
| C1 | 4 | ||
| C2 | 6 | ||
| C3 | 7 | ||
| 9.sukur | Lei | Type 1 | 8 |
| Type 2 | 6 | ||
| 12.Lei | AO/OTA | 44-B3.2 | 5 |
| 44-C2.3 | 7 | ||
| Lei | Type 1 | 7 | |
| Type 2 | 5 | ||
| 13.Chaparro | Lauge Hansen | SER | 18* |
| PER | 4 | ||
| PAB | 3* | ||
| AO/OTA | 44-B | 18* | |
| 44-C | 3* | ||
| 14.Zhang | Klammer | III | 20 |
Abbreviations: SER; supination external rotation, PER; pronation external rotation, PAD; pronation abduction.
Note: * indicates cases where two classification systems were used to describe the same group of fractures (i.e., Wang considered AO/OTA 44-B3.2 the same fracture as Lauge Hansen SER).
Table 3.
Description of Classification systems.
| Classification system | Year | Subgroup | Explanation | Notes |
|---|---|---|---|---|
| Lei | 2011 | Type I | Spiral fibular fracture, shear fracture of PC from MM and PL malleolar fragment | Tri-malleolar fracture |
| Type II | PM fragment, with transverse fracture anteriorly and coronal fracture posteriorly | P.Mal and MM in one fragment | ||
| Klammer | 2013 | Type I | Single medial P.Mal. Fragment | address through PL approach alone |
| Type II | P.Mal. Fragment split into PM and PL fragment | add medial or PM approach | ||
| Type III | P.Mal fracture line exits anterior to the PC of MM with additional anteromedial fragment | medial approach required for reduction of anteromedial fragment | ||
| Yua | 2015 | Type I | PL avulsion fracture with a large Volkmann fragment | |
| (from Zhang, article in Chinese) | Type II | single posterior fragment with fracture line extending toward the posterior MM | ||
| Type III | Fracture dividing P.Mal. into PM and PL fragments | |||
| Zhang | 2019 | Type I | P.Mal. is a single complete fragment | |
| Type IIa | P.Mal. split into PM and PL fragment | |||
| Type IIb | P.Mal. Is a comminuted fracture | |||
| Type IIIa | P.Mal fracture line travels through AC of MM, but AC and PC are one fragment | |||
| Type IIIb | P.Mal fracture line travels through intercollicular groove of MM, AC and PC individual fragments |
Abbreviations: PC = posterior colliculus; AC = anterior colliculus; MM = medial malleolus; PL = posterolateral; PM = posteromedial; P.Mal = posterior malleolus.
The original Yu et al. paper was published in Chinese; therefore, the description of the classification system was gathered from Zhang et al., 2019.
The remaining four classification systems (Lei, Klammer, Yu, and Zhang) showed high levels of redundancy in their subclassifications.12,14,20,22 A summary of each classification system and their respective subclassifications are listed below (Table 3). Criteria used to differentiate subclassifications were the location of fracture fragments, the malleolus involved in the fragment, the direction of the major fracture lines, and the number of fracture fragments. The current authors have chosen to summarize the various subclassifications from all four articles from least to most severe injury.
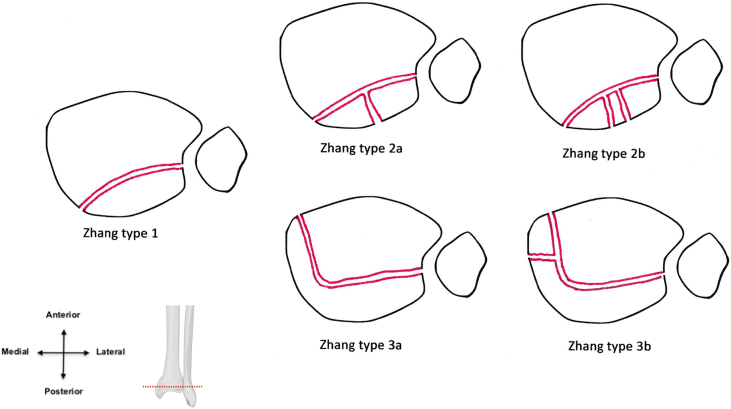
The smallest fracture pattern described was confined to the Volkmann fragment, classified by Yu as a type 1 fracture. This fracture pattern results from a torsional force applied to the posterior inferior tibiofibular ligament (PITFL).12 Multiple authors defined a single, large, posterior malleolar fragment, including the Klammer type 1, Zhang type 1, and Yu type 2 (Fig. 2A). If the posterior malleolar fragment split into two fragments (posterolateral and posteromedial), it is classified as a Klammer type 2, Yu type 3, or a Zhang type 2a. Lei type 1 has a similar fracture pattern but specifies that the posteromedial fragment contained the PC of the MM (Fig. 2B). A comminuted fracture of only the posterior malleolus (i.e., three or more fragments), it was classified as a Zhang type 2b (Fig. 2C). When the fracture lines exited anterior to the anterior colliculus (AC), resulting in a single fragment containing the entire posterior malleolus and the MM, Lei defined it as a type 2 and Zhang as a type 3a (Fig. 2D). Type 3b from Zhang adds in a second fracture line separating the two colliculi of MM, creating a large posterior fragment, composed of the posterior malleolus and the PC of the MM, and an anterior fragment containing the AC.12 This pattern resembles Klammer type 3 which describes a large anteromedial fragment plus a large posterior fragment (Fig. 2E).14 The classification system published by Zhang is the most comprehensive of those described in Table 3.
Fig. 2.
A cross-sectional representation of the Zhang et al Classification System (Zhang et al. Medicine (2019) 98:3). The illustrations are a cross section of the distal aspect of the right tibia and fibula. Orientation and location of cross section are indicated in the lower left corner. Zhang type 1, 2a, and 2b are fractures involving only the posterior malleolus, with more severe subtypes indicating a greater degree of fragmentation. Type 3a involves a single fracture fragment that exits from the anteromedial aspect of the tibia, anterior to the anterior colliculus of the medial malleolus. Type 3b is the most severe, with an additional fracture line through the intercollicular groove, separating the anterior colliculus of the medial malleolus from the posterior fragment that is composed of the posterior malleolus and the posterior colliculus of the medial malleolus. Reference illustration indicating the level of the cross section created with BioRender.com.
3.6. Surgical management outcomes and approaches
Eight surgical approaches were described, with an average follow-up time of 22.3 months. The most used approach was the traditional posterolateral (PL) (n = 9), with combined posterolateral/posteromedial (PL/PM), modified posteromedial (MPM), and posteromedial (PM) alone following in order of frequency of use. All other surgical approaches used were only investigated by a single publication (Table 1). Twelve papers reported average AOFAS scores following surgery, but only 6 of those papers reported AOFAS score for each individual included in the study.2,4,12,14,15,22 Of these papers, Zhang et al. had the largest sample size (n = 36), however, the focus of the paper was classification of PPVF rather than outcomes, and therefore specific surgical approach for each patient was not described, and therefore could not be used to compare treatment outcomes between approaches.12
Of the papers reporting individual patient data, two used a PL approach (n = 20), two used a modified PM (n = 34), and one used a combined PL/PM approach (n = 10). The mean AOFAS score at follow-up was 87.3 for the PL approach, 82.6 for the PM approach, and 94.3 for the PL/PM approach (Table 4). Notably, Klammer et al. reported one outlier (AOFAS = 29) who developed complex regional pain syndrome following surgery, resulting in an abnormally low AOFAS. Removal of this patient improves the mean score for the PL approach to 90.4 (Table 4). One way ANOVA demonstrated a significant difference in the AOFAS scores between the three surgical approaches, both with and without the outlier described above. A combined PM/PL approach demonstrated the best outcomes (p < 0.01). One paper compared the open fibula fracture line technique to the PL approach and found the open fibula fracture line group had significantly better AOFAS scores than the PL group (86.6 ± 7.1 vs. 82.7 ± 6.9, p = 0.037) (Table 4).23
Table 4.
One-way ANOVA of AOFAS scores for Pooled Patient Data.
| Author | Surgical Approach | sample size | Mean AOFAS | Variance |
|---|---|---|---|---|
| Klammer et al., 2013 | posterolateral approach | 7 | 81.57 | 650.29 |
| Klammer et al., 2013 | posterolateral approach | 6 | 90.33 | 135.47 |
| (without outlier) | ||||
| Dwivedi et al., 2018 | Posterolateral approach with buttress plating | 13 | 90.38 | 38.42 |
| Wang et al., 2016 | Modified posteromedial approach | 14 | 85.57 | 45.65 |
| Zhang et al., 2022 | Modified posteromedial approach | 20 | 80.55 | 17.63 |
| Weber 2004 | Posterolateral + Posteromedial approach | 10 | 94.3 | 40.46 |
| Surgical approach (pooled) | sample size | mean AOFAS | variance | |
| PM/PL | 10 | 94.3 | 40.46 | p = 0.007 |
| PL | 20 | 87.3 | 248.22 | |
| Modified PM | 34 | 82.62 | 34.43 | |
| Surgical approach (pooled) w/o Klammer outlier | sample size | mean AOFAS | variance | |
| PM/PL | 10 | 94.3 | 40.46 | p = 2.86E-06 |
| PL | 19 | 90.37 | 63.25 | |
| Modified PM | 34 | 82.62 | 34.43 |
When comparing time to union, Black et al. found a significantly shorter time to union with either direct (85.1 days) or indirect fixation (74 days) when compared to no fixation (174.3 days), but no significant difference existed between direct and indirect fixation. Furthermore, the PM approach showed significantly shorter time to union compared to the PL approach, 63 and 124.8 days (about 4 months) respectively.13
4. Complications
Complications encountered after surgical repair of PPVF varied across the included studies, with eleven studies reporting 51 complications. Ten studies reported frequencies of individual complications and one study reported percentages of complications, rather than frequencies.13 Postoperative complications included soft tissue complications (impaired wound healing/infection), localized pain, neurovascular complications, postoperative arthritis, bone, or joint deformities (exostosis/impingement), malunion/disunion, and hardware failure (Table 5). One study investigating posterior arthroscopic-assisted reductio with internal fixation (PAARIF) had 1/29 cases converted to traditional open reduction internal fixation treatment after inability to achieve adequate reduction.11 Direct fixation of PPVF was found to have significantly fewer soft tissue complications when compared to both indirect fixation and no fixation (5.9% vs. 33.3% and 28.6%, respectively). There was no significant difference in complications when comparing posteromedial approach to posterolateral approach within the direct fixation group.13 Jiang et al. found no difference in complications between open fibula fracture line group and the traditional posterolateral group.23
Table 5.
Surgical complications.
| Author | Surgical approach (if reported) | Complication | Category | Cases | Percentage of cases | Intervention | Notes |
|---|---|---|---|---|---|---|---|
| Martin | PAARIF | Unable to reduce fragment with PAARIF approach | intraoperative | 1 | 3.40% | conversion to open PL approach | |
| PAARIF | Hardware misplaced through fibular incisura | hardware failure | 1 | 3.40% | removal at 12 weeks | ||
| Zhang | – | Posterior tibial tendon irritation | pain | 6 | 16.70% | plate removal | |
| – | traumatic arthritis | arthritis | 1 | 2.80% | debridement | ||
| – | postoperative pain | pain | 1 | 2.80% | NSAIDS | ||
| Black | indirect | soft tissue | soft tissue complication | – | 33.30% | – | |
| no fixation | soft tissue | soft tissue complication | – | 28.60% | – | ||
| Direct fixation | soft tissue | soft tissue complication | – | 5.90% | – | ||
| Klammer | PL | localized pain | pain | 2 | 18.20% | medial hardware/osteophyte removal | |
| PL | sural neuritis | neurovascular | 1 | 9.10% | nerve decompression | Complex regional pain syndrome | |
| PL | fibular exostosis | bone/joint deformity | 1 | 9.10% | exostectomy/drilling of talar chondral defect | ||
| PL | anterior ankle impingement | bone/joint deformity | 1 | 9.10% | arthroscopy and debridement | Complex regional pain syndrome | |
| PL | ankle misalignment | bone/joint deformity | 1 | 9.10% | Achilles tendon lengthening with joint debridement | ||
| PL | deep wound infection following syndesmotic hardware removal | soft tissue complication | 1 | 9.10% | two rounds irrigation and debridement | ||
| Dwivedi | PL with buttress plate | superficial wound infection | soft tissue complication | 1 | 7.70% | antibiotics | |
| Gao | PL | persistent pain | pain | 3 | 13.00% | internal fixation removed | |
| PL | superficial wound infection | soft tissue complication | 1 | 4.30% | antibiotics | ||
| PL | numbness near incision and dorsum of foot | pain | 1 | 4.30% | subsided over 4 months with neurotrophic agent | attributed to retractors during surgery | |
| Amorosa | – | nonunion of medial malleolus | nonunion/malunion | 1 | 6.70% | repeat fixation with bone grafting | patient noncompliant, weight bearing within 1 week. |
| – | posterior tibial tendon irritation | pain | 1 | 6.70% | implant removed | ||
| – | peroneal tendon irritation | pain | 1 | 6.70% | implant removed | ||
| Lei | PM/PL | ankle stiffness and pain at 6 months | pain | 1 | 8.30% | noncompliance of rehabilitation | |
| PM/PL | lateral ankle pain | pain | 1 | 8.30% | hardware removal | ||
| PM/PL | irritation of extensor digitorum longus | pain | 1 | 8.30% | hardware removal | ||
| Chaparro | – | superficial wound infection | soft tissue complication | 2 | 8.00% | antibiotics | |
| – | osteoarthritis | arthritis | 2 | 8.00% | 1 arthrodesis | ||
| – | posterior pilon nonunion | nonunion/malunion | 2 | 8.00% | 1 revision, 1 arthrodesis (same osteoarthritis patient) | ||
| – | syndesmotic malreduction | nonunion/malunion | 1 | 4.00% | syndesmotic fusion | ||
| – | CRPS | pain | 1 | 4.00% | |||
| Zhang | MPM | infection | soft tissue complication | 1 | 5.00% | debridement and antibiotics | diabetic, poor management of blood glucose |
| MPM | screw loosening | hardware failure | 1 | 5.00% | refixation of screw | ||
| Jiang | OFFL | vascular nerve injury | neurovascular | 2 | 3.40% | ||
| OFFL | soft tissue complication | soft tissue complication | 2 | 3.40% | |||
| OFFL | postoperative pain | pain | 1 | 1.70% | |||
| PL | vascular nerve injury | neurovascular | 3 | 5.10% | |||
| PL | soft tissue complication | soft tissue complication | 2 | 3.40% | |||
| PL | postoperative pain | pain | 2 | 3.40% |
PM = posteromedial, PL = posterolateral, PAARIF = posterior arthroscopic-assisted reduction internal fixation, OFFL = open fibular fracture line. Percentages reported relative to sample size of published article.
5. Discussion
PPVF are under-researched in foot and ankle orthopedics. This pattern was at first thought to be rare, but as awareness grows around the topic, reported incidence is rising. The current authors believe this is why some reports of PPVF patterns among operative ankle fractures have been as high as 20%.6 By reviewing available literature, the current authors developed a better understanding of the characteristics, management, and outcomes of PPVF. Still, the inherent complexity and diversity of ankle fractures makes identification and treatment difficult, even for highly trained surgeons.29, 30, 31 PPVF involves both the medial malleoli and the posterior aspect of the tibial plafond, leading to worse outcomes as the degree of incongruity, cartilage involvement, and articular impaction increase.8,21,32 Failure to fixate PPVF has been associated with healing times more than double that of direct or indirect fixation.13 Thus, properly differentiating PPVF from other fractures that may require conservative management is imperative.
Previously published data shows that the mechanism of injury for PPVF is similar to that of rotational ankle fractures but with the addition of mild to moderate axial forces complicating the fracture pattern.2,29,30 SER and PER mechanisms, as described in the Lauge Hansen classification system, are most associated with PPVF.4,6,18,21,25 The overlap in mechanism between PMF and PPVF is a clear example of why a thorough diagnostic workup is required. PPVF do not typically present with the high energy axial forces associated with traditional pilon fractures, however, they can create similar challenges in surgical fixation and recovery. Classification of ankle fractures based on mechanism increases the risk of misdiagnosis, and more specific criteria are needed that utilize advanced imaging modalities. While x-ray imaging is the most readily available modality for imaging potentially fractured ankles, morphology of PMF and PPVF can appear similar on plain radiographs, making proper diagnosis challenging.13,19,24,33 CT has been shown to be the most reliable modality for differentiating PPVF from PMF, as imaging characteristics can appear similar when using plain radiographs alone.5,17,34,35
Currently, no single classification system sufficiently describes PPVF while also differentiating them from other ankle fractures, such as high impact pilon fractures and rotational tri-malleolar fractures. The system proposed by Zhang et al. is the most comprehensive to date, but does not address the degree of impaction, discontinuity, or joint surface area involved, three factors that impact outcomes in complex ankle fractures.12,29 Furthermore, types 1 and 2 of the Zhang classification system are similar to PMF patterns described in related literature.12 The current authors believe a true PPVF involves both the posterior and medial aspect of the tibial plafond, also referred to as the posterior and medial columns.7 A four-column theory has been used to describe high energy pilon ankle fractures, with an anterior and posterior column divided by the intermalleolar line, a medial column including the medial weight bearing tibial plafond plus the medial malleolus, and a lateral column comprised of the distal fibula plus the fibular groove.36 This system could potentially be integrated into PPVF descriptions used currently, as most focus on the orientation of major fracture lines. By utilizing the four-column theory, an emphasis is put on the pilon nature of PPVF, potentially reducing the confusion between PPVF and malleolar fractures. The joint surface area involved in the fracture is another potential method for differentiating PPVF from PMF, as PPVF are associated with larger posteromedial fragments and a greater degree of articular involvement.4,25
Surgical repair of the PM fragment of PPVF poses additional challenges due to the anatomical structure found within the tarsal tunnel of the posteromedial ankle. The vasculature and nerves running through the tarsal tunnel are essential for perfusion and function of the intrinsic flexor muscles of the foot making this approach especially difficult.37, 38, 39 The branching pattern of the tibial nerve can vary between patients, further adding to the complexity of this surgery.40 The tendon of the tibialis posterior is the deepest of these structures, and damage to it is the most common cause of acquired flat foot.41
Review of literature found no clear consensus regarding the preferred surgical management strategy for PPVF due to the limited amount of data. Of the eight surgical approaches identified for the management of PPVF, a combined PM/PL approach demonstrated the most favorable outcomes.2 By using two incisions to approach the posterior tibia, both the PM and PL fragments can be visualized and aid in adequate reduction. The current authors believe some medial approach is required for management of true PPVF, as failure to achieve anatomical reduction and fixation may lead to instability of the talus in the PM direction, leading to increased morbidity.2 In cases where a PM fragment is not involved, lateral approaches, either through a PL incision or the fibular fracture incision (which commonly coexists with PPVF), can be utilized.
A major limitation of the current review is the inherent risk of bias of the studies included. As noted by the modified CMS, the considerable risk of bias is primarily due to small sample sizes, retrospective nature of most of the articles, and limited reporting of pertinent experimental data. Despite most articles having sample sizes less than 40, only 5/15 reported data for each participant in the study. Without individual scores, data could not be pooled for meta-analysis. Many studies did not provide thorough descriptions of research methods and inclusion criteria, limiting the conclusions that could be drawn. Future research is needed to clarify diagnostic criteria and classification of PPVF. Through clearer methods of description and diagnosis, more meaningful data can be gathered regarding the appropriate management of PPVF, pre-, peri-, and post-operatively, leading to improvements in patient outcomes.
6. Conclusion
PPVF are a unique and more severe subtype of rotational PMF described in recent medical literature with a distinct fracture pattern involving the posterior and medial malleoli. Several characteristics on radiographs can assist in identifying this fracture pattern, with CT scans being most effective in confirming diagnoses. There is a lack of consensus regarding both the classification system and treatment strategy that should be used with pilon variant fractures. Direct fixation has demonstrated promising short-term outcomes and failure to fixate leading to significantly worse outcomes; however, there have been an insufficient number of studies to form a strong conclusion regarding the most effective surgical approach. Future randomized prospective studies should be employed to assess longer-term outcomes for patients who were managed using various surgical approaches, as this data will be critical in evaluating the ideal management of pilon variant fractures.
Funding
No.
Declaration of patient Consent form
N/A.
Ethical statement
We confirm that this manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. We further confirm that the order of authors listed in the manuscript has been approved by all of us. This manuscript has not been submitted elsewhere. We appreciate that this respected journal has an excellent process of review and decision. Thank you for your time and please feel free to contact me if there are any further questions.
CRediT authorship contribution statement
Eric M. Lassiter: Data curation, Formal analysis, and interpretation, Writing – original draft, Writing – review & editing. Kevin J. Brown: Data curation, Formal analysis, and interpretation, Writing – original draft, Writing – review & editing. Devon Patel: Data curation, Formal analysis, and interpretation, Writing – original draft. Addison Sparks: Data curation, Formal analysis, and interpretation, Writing – original draft. Jiayong Liu: Conceptualization, Methodology, Software, Formal analysis, and interpretation, Writing – review & editing, Supervision. Osama Elattar: Visualization, Investigation, Software, Formal analysis, and interpretation, Validation, Writing – review & editing, Supervision.
Acknowledgement
Not Applicable.
References
- 1.Karachalios T., Roidis N., Karoutis D., Bargiotas K., Karachalios G.G. Trimalleolar fracture with a double fragment of the posterior malleolus: a case report and modified operative approach to internal fixation. Foot Ankle Int. Feb 2001;22(2):144–149. doi: 10.1177/107110070102200211. [DOI] [PubMed] [Google Scholar]
- 2.Weber M. Trimalleolar fractures with impaction of the posteromedial tibial plafond: implications for talar stability. Foot Ankle Int. Oct 2004;25(10):716–727. doi: 10.1177/107110070402501005. [DOI] [PubMed] [Google Scholar]
- 3.Hansen S.T. Lippincott Williams & Wilkins; 2000. Functional Reconstruction of the Foot and Ankle; p. 525. [Google Scholar]
- 4.Wang Y., Wang J., Luo C.F. Modified posteromedial approach for treatment of posterior pilon variant fracture. BMC Musculoskelet Disord. Aug 5 2016;17:328. doi: 10.1186/s12891-016-1182-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lou Z., Wang Z., Liu C., Tang X. Outcomes of tibial pilon fracture fixation based on four-column theory. Injury. Apr 2023;54(Suppl 2):S36–s42. doi: 10.1016/j.injury.2022.08.017. [DOI] [PubMed] [Google Scholar]
- 6.Switaj P.J., Weatherford B., Fuchs D., Rosenthal B., Pang E., Kadakia A.R. Evaluation of posterior malleolar fractures and the posterior pilon variant in operatively treated ankle fractures. Foot Ankle Int. Sep 2014;35(9):886–895. doi: 10.1177/1071100714537630. [DOI] [PubMed] [Google Scholar]
- 7.Cole P.A., Mehrle R.K., Bhandari M., Zlowodzki M. The pilon map: fracture lines and comminution zones in OTA/AO type 43C3 pilon fractures. J Orthop Trauma. Jul 2013;27(7):e152–e156. doi: 10.1097/BOT.0b013e318288a7e9. [DOI] [PubMed] [Google Scholar]
- 8.Jo S., Tilan J., McAndrew C., Miller A.N. Poor outcomes after anterior impaction pilon fractures. J Am Acad Orthop Surg. Jan 1 2022;30(1):19–26. doi: 10.5435/jaaos-d-20-01329. [DOI] [PubMed] [Google Scholar]
- 9.Coleman B.D., Khan K.M., Maffulli N., Cook J.L., Wark J.D. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports. Feb 2000;10(1):2–11. doi: 10.1034/j.1600-0838.2000.010001002.x. [DOI] [PubMed] [Google Scholar]
- 10.Page M.J., McKenzie J.E., Bossuyt P.M., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj. Mar 29 2021 doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martin K.D. Posterior arthroscopic reduction and internal fixation for treatment of posterior malleolus fractures. Foot Ankle Int. 2020;41(1):115–120. doi: 10.1177/1071100719891978. [DOI] [PubMed] [Google Scholar]
- 12.Zhang J., Wang H., Pen C., et al. Characteristics and proposed classification system of posterior pilon fractures. Medicine. 2019;98(3) doi: 10.1097/MD.0000000000014133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Black A.T., Stowers J.M., Tran S., Mata K., Sherman A.E., RahnamaVaghef A. Clinical outcomes for pilon variant posterior malleolar fractures: a Multicenter retrospective analysis. J Foot Ankle Surg. Nov-Dec 2022;61(6):1303–1307. doi: 10.1053/j.jfas.2022.04.007. [DOI] [PubMed] [Google Scholar]
- 14.Klammer G., Kadakia A.R., Joos D.A., Seybold J.D., Espinosa N. Posterior pilon fractures: a retrospective case series and proposed classification system. Foot Ankle Int. Feb 2013;34(2):189–199. doi: 10.1177/1071100712469334. [DOI] [PubMed] [Google Scholar]
- 15.Dwivedi A.K., Dwivedi S.S., Zhenhong S., et al. Open reduction and internal fixation (ORIF) of posterior pilon variant fractures with buttress plate through posterolateral approach. International Journal of Contemporary Medical Research [IJCMR] 2018 [Google Scholar]
- 16.Gao M., Liu N., Cheng Y., Shi W., Yang H. Treatment outcomes of the posterolateral approach of plate fixation for posterior pilon fractures. Exp Ther Med. May 2019;17(5):4267–4272. doi: 10.3892/etm.2019.7458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sukur E., Akman Y.E., Gokcen H.B., Ozyurek E.C., Senel A., Ozturkmen Y. Open reduction in pilon variant posterior malleolar fractures: Radiological and clinical evaluation. Orthop Traumatol Surg Res. Sep 2017;103(5):703–707. doi: 10.1016/j.otsr.2017.05.012. [DOI] [PubMed] [Google Scholar]
- 18.Chen D.W., Li B., Aubeeluck A., Yang Y.F., Zhou J.Q., Yu G.R. Open reduction and internal fixation of posterior pilon fractures with buttress plate. Acta Ortop Bras. 2014;22(1):48–53. doi: 10.1590/s1413-78522014000100009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Amorosa L.F., Brown G.D., Greisberg J. A surgical approach to posterior pilon fractures. J Orthop Trauma. Mar 2010;24(3):188–193. doi: 10.1097/BOT.0b013e3181b91927. [DOI] [PubMed] [Google Scholar]
- 20.Wang L., Shi Z.M., Zhang C.Q., Zeng B.F. Trimalleolar fracture with involvement of the entire posterior plafond. Foot Ankle Int. Aug 2011;32(8):774–781. doi: 10.3113/fai.2011.0774. [DOI] [PubMed] [Google Scholar]
- 21.Chaparro F., Ahumada X., Urbina C., et al. Posterior pilon fracture: Epidemiology and surgical technique. Injury. 2019/12/01/2019;50(12):2312–2317. doi: 10.1016/j.injury.2019.10.007. [DOI] [PubMed] [Google Scholar]
- 22.Zhang Z.-C., He W.-B., Lin H. Analysis of the efficacy of a modified posteromedial approach for Klammer III posterior Pilon fractures. Chin J Traumatol. 2022/03/01/2022;25(2):83–89. doi: 10.1016/j.cjtee.2022.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jiang Z., Zhang C., Qin J.-J., Wang G.-D., Wang H.-S. Posterior pilon fracture treated by opening the fibula fracture gap. J Orthop Surg Res. 2022/04/07 2022;17(1):214. doi: 10.1186/s13018-022-03106-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang J., Wang X., Xie L., Zheng W., Chen H., Cai L. Comparison of radiographs and CT features between posterior Pilon fracture and posterior malleolus fracture: a retrospective cohort study. The British Journal of Radiology. 2020/06/01 2020;93(1110) doi: 10.1259/bjr.20191030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang C., Chen C., Zhou Y., Pan Z.E. Morphological study of CT image of posterior pilon variant fracture and its possible clinical significance. Arch Orthop Trauma Surg. Mar 2023;143(3):1203–1215. doi: 10.1007/s00402-021-04224-0. [DOI] [PubMed] [Google Scholar]
- 26.Mason L.W., Marlow W.J., Widnall J., Molloy A.P. Pathoanatomy and associated injuries of posterior malleolus fracture of the ankle. Foot Ankle Int. Nov 2017;38(11):1229–1235. doi: 10.1177/1071100717719533. [DOI] [PubMed] [Google Scholar]
- 27.Meinberg E.G., Agel J., Roberts C.S., Karam M.D., Kellam J.F. Fracture and dislocation classification Compendium—2018. J Orthop Trauma. 2018;32 doi: 10.1097/BOT.0000000000001063. [DOI] [PubMed] [Google Scholar]
- 28.Lauge-Hansen N. Fractures of the ankle. II. Combined experimental-surgical and experimental-roentgenologic investigations. Arch Surg. May 1950;60(5):957–985. [PubMed] [Google Scholar]
- 29.Sultan F., Zheng X., Pan Z., Zheng Q., Li H., Wang J. Characteristics of intercalary fragment in posterior malleolus fractures. Foot Ankle Surg. 2020/04/01/2020;26(3):289–294. doi: 10.1016/j.fas.2019.03.011. [DOI] [PubMed] [Google Scholar]
- 30.Yi Y., Chun D.-I., Won S.H., Park S., Lee S., Cho J. Morphological characteristics of the posterior malleolar fragment according to ankle fracture patterns: a computed tomography-based study. BMC Muscoskel Disord. 2018/02/13 2018;19(1):51. doi: 10.1186/s12891-018-1974-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Keiler A., Riechelmann F., Thöni M., Brunner A., Ulmar B. Three-dimensional computed tomography reconstruction improves the reliability of tibial pilon fracture classification and preoperative surgical planning. Arch Orthop Trauma Surg. 2020/02/01 2020;140(2):187–195. doi: 10.1007/s00402-019-03259-8. [DOI] [PubMed] [Google Scholar]
- 32.Langenhuijsen J.F., Heetveld M.J., Ultee J.M., Steller E.P., Butzelaar R.M.J.M. Results of ankle fractures with involvement of the posterior tibial Margin. J Trauma Acute Care Surg. 2002;53(1):55–60. doi: 10.1097/00005373-200207000-00012. [DOI] [PubMed] [Google Scholar]
- 33.Gardner M.J., Streubel P.N., McCormick J.J., Klein S.E., Johnson J.E., Ricci W.M. Surgeon Practices regarding operative treatment of posterior malleolus fractures. Foot Ankle Int. 2011/04/01 2011;32(4):385–393. doi: 10.3113/FAI.2011.0385. [DOI] [PubMed] [Google Scholar]
- 34.Donohoe S., Alluri R.K., Hill J.R., Fleming M., Tan E., Marecek G. Impact of computed tomography on operative planning for ankle fractures involving the posterior malleolus. Foot Ankle Int. Dec 2017;38(12):1337–1342. doi: 10.1177/1071100717731568. [DOI] [PubMed] [Google Scholar]
- 35.Stringfellow T.D., Walters S.T., Nash W., Ahluwalia R. Management of posterior malleolus fractures: a multicentre cohort study in the United Kingdom. Foot Ankle Surg. Aug 2021;27(6):629–635. doi: 10.1016/j.fas.2020.08.003. [DOI] [PubMed] [Google Scholar]
- 36.Tang X., Tang P.F., Wang M.Y., et al. Pilon fractures: a new classification and therapeutic strategies. Chin Med J (Engl) Jul 2012;125(14):2487–2492. [PubMed] [Google Scholar]
- 37.Fortier L.M., Leethy K.N., Smith M., et al. An Update on posterior tarsal tunnel syndrome. Orthop Rev. 2022;14(4) doi: 10.52965/001c.35444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rodríguez-Merchán E.C., Moracia-Ochagavía I. Tarsal tunnel syndrome: current rationale, indications and results. EFORT Open Rev. Dec 10 2021;6(12):1140–1147. doi: 10.1302/2058-5241.6.210031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Torres A.L., Ferreira M.C. Study of the anatomy of the tibial nerve and its branches in the distal medial leg. Acta Ortop Bras. 2012;20(3):157–164. doi: 10.1590/s1413-78522012000300005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moroni S., Zwierzina M., Starke V., Moriggl B., Montesi F., Konschake M. Clinical-anatomic mapping of the tarsal tunnel with regard to Baxter's neuropathy in recalcitrant heel pain syndrome: part I. Surg Radiol Anat. Jan 2019;41(1):29–41. doi: 10.1007/s00276-018-2124-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hung C.Y., Chang K.V., Mezian K., et al. Advanced ankle and foot Sonoanatomy: imaging beyond the Basics. Diagnostics. Mar 14 2020;10(3) doi: 10.3390/diagnostics10030160. [DOI] [PMC free article] [PubMed] [Google Scholar]