Abstract
Objectives
To analyse the content of letters written by female spouse primary caregivers of patients with glioblastoma multiforme (GBM), a devastating and terminal primary brain cancer, and give voice to their experiences for medical providers of patients with GBM.
Design
A qualitative study using reflexive thematic analysis of letters written by female spouses/life partners and primary caregivers of patients with GBM.
Participants
101 current or former female spouse primary caregivers of patients with GBM wrote letters to share with the medical community between July 2019 and August 2019. Inclusion criteria: (1) the primary caregiver who is a spouse of a patient with glioblastoma, (2) be a member of the secret Facebook group, ‘We are the wives of GBM and this is our story’, and (3) completed informed consent for the contents of their letter to be included for primary and secondary data analysis. Participants who wrote letters but did not complete the informed consent were excluded from the study.
Results
Themes from the letters included the patient experiences: (1) medical details of the disease trajectory, (2) interactions of the patient/caregiver dyads with healthcare and (3) the changing patient condition over time. Themes focused on the caregiver experiences: (1) caregiver challenges, (2) caregiver responses and (3) caregiver coping strategies, and description of tangible needs that would help other caregivers in the future. Caregiver needs were highest during the living with disease progression phase. Caregivers wanted more education and to be valued as members of the care team.
Conclusion
Shared decision-making through family-centred care would be beneficial for primary caregivers of patients with GBM. These findings provide opportunities to guide more timely and tailored interventions to provide support and improve care for patient/caregiver dyads to help mitigate the burden of this progressive disease and improve quality of life for caregivers.
Keywords: Clinical Decision-Making, Community-Based Participatory Research, Neurological oncology, Nursing Care, Caregivers, Caregiver Burden
STRENGTHS AND LIMITATIONS OF THIS STUDY.
The qualitative research design provides a voice for female spouse caregivers of patients with glioblastoma to share their experience with the medical community.
The letters highlighted the experiences of patients and caregivers from the caregivers’ perspectives and provided recommendations for healthcare providers to better meet the caregivers’ educational needs and is a strength of this study.
The open-ended instructions of writing a 500-word letter could have been a limitation of the study; however, many letters did not abide by this recommendation and were still included in the analysis regardless of length.
Letters were written by caregivers in different stages of their patient’s disease journey and included information caregivers deemed important; therefore, the type of data collected was difficult to analyse and could be a limitation of the study.
The large sample set (n=101 letters) allowed for some analysis of the frequency of codes and themes used in each letter; however, since each participant’s experience was different, this method of analysis and presentation may not fully reflect the caregivers’ experiences within these topics and is a limitation of the study.
Introduction
Brain tumours are the 3rd most common cancer among patients aged 15–39 years old and the 8th most common cancer in patients 40 years and older.1 Glioblastoma multiforme (GBM) is the most common and deadly brain cancer with an incidence of 3.19 per 100 000; it affects males at nearly double the rate as in females with the median survival of 12–18 months after initial diagnosis.2 Patients with GBM experience a host of irreversible and progressive neuropsychological symptoms including cognitive decline, personality changes, headaches, seizures and focal neurological changes dependent on tumour location.3–6 Although individual outcomes vary, the disease trajectory of GBM involves the acute phase (3–4 months) that represents the initial diagnosis and standard of care (maximal surgical resection followed by concurrent temozolomide and radiation therapy for 6 weeks), living with disease progression phase (the period after the acute phase where patients continue with monthly temozolomide until recurrence), and the end-of-life phase.7
Patients with GBM rely on a caregiver; 67% of the time the caregiver is a spouse and 73% of caregivers are female.8 More than a quarter of brain cancer caregivers report distress or severe distress and often place their needs behind those of their patients leading to psychological, physical and financial burden.8 9 Unlike other cancers, the rapid and irreversible disease progression combined with the cognitive declines of patients with GBM leaves caregivers with unique time-sensitive challenges often not adequately addressed by the medical community.10–13
Caregivers of patients with GBM face many significant challenges related to this progressive and terminal cancer that include feelings of isolation, difficulty managing the symptoms of GBM and a need for increased psychological, physical and daily living needs support.6 11 13 14 The increased caregiver burden is linked to the area of the brain affected by GBM.15 Poor performance status and confusion in the patient negatively affects the quality of life of caregivers.15 16 Importantly, improved GBM survival is linked to family caregivers’ mastery demonstrating the essential role of caregivers for patients with GBM.17
The low incidence of GBM also means that caregivers of patients with GBM may not have access to local support resources. Social media platforms such as Facebook provide patients and caregivers with serious illnesses a place to share experiences and concerns and improve patient and caregiver coping and are a valuable tool to provide insight into identifying unmet needs among caregivers of patients with GBM.18 The purpose of this study was to identify shared experiences among female spouse caregivers of patients with GBM and to identify areas to support future guided interventions.
Methods and data analysis
Study design
The letters written by female spouse caregivers of patients with GBM were analysed using thematic qualitative analysis as described by Braun and Clarke.19–22 The letters were collected to provide information about the unmet needs of these caregivers that could be shared with providers who care for patients with GBM and their families and to give voice to the female partners/spouses of patients with GBM about their unmet needs and concerns (box 1). For this analysis, the researcher’s active role in knowledge production is acknowledged and highlighted.19 In this study, the principal investigator (LAM) and co-author (LD) are members of the Facebook group and have personal experience as caregivers of a spouse with GBM. The other authors included students (DLC, MPC) and an expert in qualitative and caregiving research (BJL).
Box 1. Letter-writer instructions.
We are compiling letters to give to the medical community expressing the challenges and needs for caregivers dealing with glioblastoma multiforme.
The letters can include recommendations which should consider the criteria below:
The letter should not exceed 500 words.
You could share the challenges you faced.
You can include what you wished you knew going into the care for a person with this disease.
Identify resources you found helpful during your experience.
What you wished you knew before that you learnt after; add anything else you feel may be relevant.
Participants
Participants were recruited from a private Facebook support group called ‘We are the wives of GBM and this is our story’ to write letters to share with the medical community so that providers could gain a better understanding of the reality of the caregiver experience. The Facebook support group is a secret Facebook group where members can only be invited by other ‘friends’; it is not publicly searchable, and all participants in this group identify themselves as female life partners of patients with GBM. As such, it is inferred that all participants writing the letters identify as female spouses (Facebook group size was ~1800 members).23 For participants to be included in the study, they must have been (1) the primary caregiver and spouse of a patient with glioblastoma, (2) be a member of the Facebook group, ‘we are the wives of GBM and this is our story’, and (3) completed informed consent for the contents of their letter to be included for primary and secondary data analysis. Exclusion criteria: participants who did not complete the informed consent. Minimal instruction was provided to the letter writers; however, participants were encouraged to provide recommendations to the medical community (box 1).
Data collection
A total of 120 letters were collected during July and August of 2019; 101 participants completed informed consent. Letters were redacted to remove all identifiable information. Each letter was written by a single individual; four duplicate letters were excluded from analysis resulting in a sample size of 101 letters. The length range was 148–1957 words; the median letter length was 633 words and the mean letter length was 736 words.
Preliminary primary data analysis was performed at the University of Montana; however, the results were not published. LAM brought the redacted dataset to the University of North Carolina Wilmington. Secondary data analysis began in October 2021.
Data analysis
Members of the research team independently familiarised themselves with the data: LAM, LD, MPC and DLC each independently reviewed the entire dataset. Initial systematic coding using NVivo qualitative data management software was performed by two research team members independently (DLC, MPC) with auditing by senior research members (LAM and BJL). Initial themes were identified during research meetings until a final coding structure was determined by group consensus. Codes were placed into themes that were identified in the letters. The research team met weekly to discuss the ongoing analysis and kept an audit trail of memos and methods notes to detail the study findings and revise coding and thematic grouping. Themes were revisited during the group meetings and revised by consensus until seven main themes were identified that encompassed the open coding codes from the letters. Several features of the NVivo software were used to graphically represent the data, including a hierarchy tree map that included nested rectangles of varying sizes that represent the amount of coding within each of the seven themes.
Demographic data were extracted from the letters if provided by the letter writer (table 1). The median age of the primary caregivers was 54 years; the patients described in the letters were all male with a median age of 57 years. Caregivers of patients with GBM were involved in the initial design of the study and recruitment of participants for the study.
Table 1.
Demographic data of female spouse caregivers of patients with glioblastoma
| Participant demographics (n=101 letters) |
Median | Range | Number of letters |
| Female caregiver age at Dx (years) | 54.0 | 30–73 | 73 |
| Widowed (age) | 54.5 | 30–73 | 68 |
| Non-widowed (age) | 50.2 | 38–66 | 14 |
| Age of male pt at Dx | 57.0 | 28–77 | 77 |
| Time since since Dx | |||
| Dx-death (months) | 12.0 | 2–37 | 68 |
| Still alive (months) | 15.5 | 2–48 | 22 |
| Surgical resection craniotomy | 88 | ||
| Inoperable tumour | 13 | ||
| Pt died at home | 33 | ||
| Pt died in a medical facility or residential hospice | 13 |
The letters provided rich data about female spouse primary caregiver experiences. The number of unique codes per letter ranged from 12 to 54. When multiple excerpts fell under the same code (‘references’ to the same code), they were coded separately from each other; the range of references was 18–263 per letter. The median number of codes used per letter was 30 and the median number of code references was 84 per letter.
Patient and public involvement
Participants were involved in the project from its conception. The letters arose from a series of posts and discussions within the Facebook group where members decided something needed to change. The principal investigator (LAM) and co-author (LD) are members of the Facebook group and have personal experience as primary caregivers of spouses with GBM. LD initiated a ‘letter-writing’ campaign within the Facebook group in July 2019. LAM obtained IRB approval and obtained the informed consent of letter writers. LD initially collected letters (n=121); informed consent was provided for 101 letters. Only letters with accompanying informed consent were read and used for data analysis. Preliminary data (PDFs of posters from the American Association of Cancer Researchers meeting April 2023 and the AACR Brain Cancer meeting October 2023) was shared with letter writers from the Facebook group; members of the Facebook group reviewed the material and expressed gratitude for sharing their stories.
Results
Participant demographics
Although the letter writers were not asked to share demographic data, 77 letters detailed the age of their spouse, and 73 letters detailed the age of the caregiver (table 1). All the letters were written by self-described female life partners; two-thirds of the letters were written by self-identified widows (table 1). When describing the end-of-life stage of the patient, the letters indicated 33 patients died at home whereas 13 patients died in a medical facility or in patient hospice (table 1).
Patient experience theme 1: changing patient condition
Most letters included detailed medical information about the changing patient condition. For example, letter RGBM040 provided a very detailed timeline typical of most letters.
11/08/20XX—Grand Mal Seizure at home, ambulance called taken to ER admitted to ICU; 11/09/20XX—Biopsy done, followed by a hemorrhage in the brain and emergency surgery to place a drain to relieve the pressure; 11/10/20XX—Diagnosed GBM 6 cm on the corpus callosum—surgery not an option; 11/27/20XX—Radiation begins—one dose 11/30/20XX—Surgery done to place a shunt and remove the drain—still in ICU; 12/01/20XX—Moved to rehab unit out of ICU 12/15/20XX—released from hospital, regular rehab appointments for physical therapy, occupational and speech; 12/20/20XX—Radiation begins again twice a week 01/05/20XX—Chemo added to radiation treatments 01/24/20XX—MRI—GBM reduced to 4.8 cm (RGBM040).
Although the specific data varied from each letter, nearly every letter included a detailed timeline of the patient’s medical experience, including the changing patient condition (n=99, table 2). The data from timelines helped identify that 88 letters indicated that their spouse received a craniotomy whereas 13 letters detailed their patient had inoperable tumours (table 1).
Table 2.
Themes and codes about the patient experience
| Theme | Code name | Number of letters | Number of codes |
| Changing patient condition | 99 | 422 | |
| Patient completed standard of care (SOC); letter provided details | 60 | 74 | |
| Cognitive behaviour changes | 51 | 61 | |
| Utilisation of external medical support | 50 | 75 | |
| Symptoms prediagnosis | 48 | 53 | |
| Medical complications from treatments | 42 | 59 | |
| SOC side effects | 26 | 28 | |
| Interest in participating in clinical trials | 14 | 20 | |
| Complications from craniotomy | 12 | 13 | |
| SOC delayed | 11 | 14 | |
| Utilisation of complementary-alternative medicine | 10 | 12 | |
| SOC improved symptoms | 7 | 7 | |
| Dignity loss | 6 | 6 | |
| Disease trajectory details | 87 | 446 | |
| Acute phase | 78 | 165 | |
| Living with progressive | 67 | 194 | |
| End of life | 51 | 70 | |
| Post death | 16 | 17 | |
| Interactions with healthcare workers | 67 | 148 | |
| Negative medical care experience | 38 | 56 | |
| Supportive medical team | 26 | 36 | |
| Delayed medical treatment | 17 | 20 | |
| Caregiver as patient advocate | 17 | 19 | |
| False hope | 14 | 15 | |
Patient experience theme: details of the stages of disease trajectory
Caregivers detailed events from each of the stages of the disease progression: the acute stage where the patient first presented with symptoms and whether they had a craniotomy, radiation and temozolomide chemotherapy (table 2). From the initial diagnosis to surgery, there was little time to find or process information leaving caregivers blindsided. Unique among many cancers, decisions are made quickly, and major medical interventions occur within hours to days following the identification of the tumour.
ER visit, MRI noting 30% brain oedema and tumour in left parietal lobe which explained head aches after months of increasing struggle to recognise numbers and letters and word find (RGBM043)
After the initial acute period, patients in this study continued maintenance chemotherapy and eventually presented with worsening symptoms or MRI indications of recurrence. Caregivers expressed how GBM, and its treatments affected their loved ones in less tangible ways. It was common for caregivers to detail how the patient’s declines affected their interactions with the caregiver, family members and other aspects of the patient’s life in unimaginable ways often not recognised by people outside the family unit. Competing demands between caring for a husband in an acute medical emergency and maintaining other family, work and community responsibilities was mentioned frequently in the letters. For example, letter RGBM008 details the frustration on learning about her spouse’s tumour recurrence.
Living through GBM is living a life in limbo. You just wait for a new spot to show then wait to see if it’s tumor or radiation necrosis or something else. Then, you wait to see if there are any options or medications to help. You slowly lose your loved ones daily. They forget your kids’ names, their name, their personality changes, they become strangers. They lose their independence, can no longer work, drive or be left alone. But because they look good everyone thinks everything is just fine and great. (RGBM034)
Many of the letters indicated that hospice was brought in at the end of life, but when the letters discussed hospice, they indicated their patient was on hospice a very short time before dying. The decline was rapid and caregivers were shocked at how quickly things progressed for their patient.
November 20XX—In home hospice December 20XX—awaiting the inevitable December 16th 20XX—… birthday December 23rd 20XX—death (RGBM028)
I was not prepared to see how fast [he] went downhill. Within 2 weeks he was completely bedridden. 2 weeks after that he was gone. It was extremely hard as a caregiver and wife. It was my responsibility, but no one explained what a toll it would be. (RGBM085)
Patient experience theme: interactions with healthcare workers
Letters described the roles of different members of the healthcare team: neurosurgeons, radiation oncologists, oncologists, neuro-oncologists (not all letters writers had a neuro-oncologist) and to a lesser degree, palliative medicine, social workers and nurses (including hospice and rehab nurses). The letters detailed some of the communication with medical providers; 38 letters reflected negative experiences with their care team whereas 26 letters reported positive experiences (table 2). One common issue was that some members of the healthcare team side-stepped conversations about known issues of disease progression or even provided false hope regarding GBM outcomes and treatment options. Many letters described how different providers of the healthcare team did not work well together for the benefit of the patient and their caregiver leading to negative medical care experiences.
This siloed approach left caregivers grossly unprepared emotionally and shocked when ‘known’ outcomes from certain members of the medical community were finally shared with primary caregivers. There were several instances where caregivers reported a general lack of understanding by healthcare workers regarding the memory and cognitive deficits their patient experienced. Caregivers wanted to be more involved in the care team, particularly regarding reporting their patient’s condition and in advocating for their patient’s needs. Caregivers felt unheard by healthcare workers and felt they needed to be listened to more and have their needs and concerns addressed.
The reality is the brain does not work. The patient’s understanding is gone. Asking the GBM patient if they are okay is like asking a newborn how old they are. They can’t provide you with the information. (RGBM062)
As his caregiver, I had to act as his advocate. assisting. [He] never understood money or time after his craniotomy. He understood his treatment plans, but only if described in simplified terms and in small chunks of information. He never wrote again. I had to advocate for proper care (i.e.: insisting on him getting a MRI) (RGBM 063).
These types of interactions with the healthcare team members left caregivers feeling frustrated, unprepared and undervalued by members of the healthcare team.
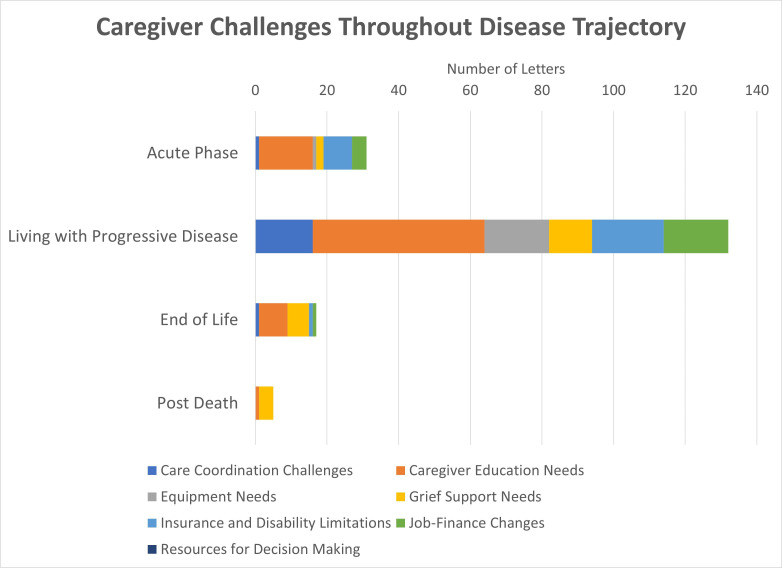
Caregiver experience theme: caregiver challenges
Codes associated with caregiver challenges appeared in 81 letters (table 3). The letters reported feeling unsupported by the medical community, appearing in 43 letters, feeling unprepared for the sudden life changes (28 letters), experienced competing demands of caring for their patient and children or elderly parents (24 letters) and highlighted relationship strains with their spouse (24 letters) (table 3). The sudden life changes and being unprepared for those changes were highest during the acute phase of the disease progression (figure 1). Relationship strains, feeling unsupported by the medical community, and competing demands of caregivers in caring for children or elderly parents were highest during the disease progression phase (figure 1).
Table 3.
Themes and codes about the caregiver experience
| Theme | Code name | Number of letters | Number of codes |
| Caregiver challenges | 81 | 224 | |
| Feels unsupported | 43 | 57 | |
| Sudden life change | 28 | 34 | |
| Unprepared for changes | 26 | 31 | |
| Competing demands (children/parents) | 24 | 38 | |
| Relationship strains | 24 | 30 | |
| No GBM knowledge | 17 | 18 | |
| Underestimating care burden | 11 | 14 | |
| Caregiver responses | 77 | 223 | |
| Exhausted/overwhelmed | 41 | 55 | |
| Lack of control | 35 | 53 | |
| Agony | 31 | 32 | |
| Post-traumatic stress disorder | 21 | 26 | |
| Disappointment | 18 | 22 | |
| Fear | 16 | 20 | |
| Regret | 9 | 9 | |
| Coping strategies for caregivers | 86 | 203 | |
| Mission to raise awareness | 54 | 67 | |
| Family, friends, and pets | 35 | 43 | |
| GBM spouse support | 27 | 29 | |
| Faith, hope and strength | 18 | 32 | |
| Preparing for end of life | 14 | 17 | |
| Fulfilling wishes | 7 | 10 | |
| Family medical leave—employer disability | 5 | 6 | |
| Tangible needs for caregivers | 92 | 355 | |
| Caregiver education needs | 66 | 135 | |
| Insurance and disability limitations | 47 | 73 | |
| Job-finance changes | 35 | 46 | |
| Care coordination challenges | 30 | 37 | |
| Grief support needs | 29 | 36 | |
| Equipment needs | 23 | 28 | |
GBM, glioblastoma multiforme.
Figure 1.
Caregiver challenges throughout the disease trajectory. GBM, glioblastoma multiforme.
This lack of support resulted in caregivers feeling exhausted and overwhelmed (41 letters) feeling a lack of control (35 letters) and showed an expression of agony (31 letters). Some letters mentioned they had been diagnosed with post-traumatic stress disorder attributed to their caregiving journey (n=21 letters) (table 3).
Caretaking my husband through his GBM journey was the hardest thing I’ve ever done. It was exhausting, overwhelming, my daughter and I got sick (no doubt from stress). We underestimated the effects of the tumor on faulty decision-making. It was excruciating watching [my husband’s] quickly weakening condition, difficulty speaking, word retrieval issues, frustration. (RGBM001)
These caregiver responses resulted in physical and mental declines among caregivers that might have been mitigated by better communication and support during the disease journey.
I was the one who brought up palliative care. I brought up hospice. I don’t understand why we were not more leveled with. We were told early on in this nightmare that “some patients don’t want to know all the information”, but we assured our team that we are people who DO want to know. Be square with us. Lay the cards on the table, with nothing held back. When I would bring up questions, we were often giving a gentle shrug and a “time will tell” kind of response.” (RGBM009)
Caregiver experience theme: coping strategies
As they transitioned through the initial role change, the wife caregivers implemented various coping strategies to manage the new stresses in their lives. They became hypervigilant and began researching the disease on their own to make sense of what to expect and to determine scenarios within their control, and then developed a care plan to address the situations. A common sentiment shared by caregivers in the dataset was gratitude for the online Facebook support group. The group was a safe, neutral and non-judgmental place where caregivers shared their struggles and received invaluable support and advice from fellow women with shared experiences. The support group was beneficial for caregivers who may have experienced anticipatory grief when facing a terminal diagnosis of a close person. The support group also became a clearing house for educational information not provided directly by members of the care team.
The only source of comfort, help, and information is the Wives of GBM Facebook page. These ladies are incredibly supportive and helpful. They will answer anything any time, day or night. (RGBM041)
Caregivers chose to find joyful moments with their spouses on the last stretch of life and chose to live in the moment, enjoying present moments, fulfilling life wishes and organising special life events for their spouse. Spiritual connection and prayers are common activities enabling the caregivers to maintain hope during stressful times.
I had hope, a powerful healing agent during what was in reality, a terminal illness (RGBM002).
In addition to implementing coping strategies, the caregivers harnessed available social and community services to manage their tasks. Family, friends and community members became involved to help the caregivers with house chores like grocery shopping and transportation. These positive caregiving experiences fostered resilience.
Had it not been for friends and family, I wouldn’t have been able to even get [him] to his appointments (RGBM004).
Caregiver experience theme: tangible unmet needs
Of the 101 letters, 92 letters expressed tangible needs of caregivers that could be better met by the medical community with the highest need in the areas of education (66 letters) assistance with insurance and disability issues (47 letters), help navigating job changes (job loss of the patient) and ensuring financial hardships (35 letters,) and additional needs for better care coordination, grief support and medical equipment (table 3). Caregiver needs were highest during the ‘living with progressive disease’ phase (figure 2). These needs were prevalent regardless of medical training or self-described socioeconomic status.
Figure 2.
Tangible needs throughout the disease trajectory.
[We paid for homecare] about 40 hours/week or $3500/month. This leaves 168 hours per week that I am [his] caretaker. I am quite overwhelmed and exhausted by now 4.5 years in…My health is taking quite a toll.” (RGBM032)
I was exhausted. I am still exhausted. Almost 5 months later [after he died]. I am an RN X 30 years and I am still traumatized by caring for my husband. (RGBM034.)
Caregivers consistently expressed how better education would have increased the quality of life of the patient and their family caregivers. Caregivers wanted to be included in medical decision-making and treated as part of the medical team.
I believe that the caregiver should be considered a part of the team from the onset. The voice of the caregiver needs to be heard and validated. (RGBM061)
My husband was in the hospital after his first surgery for three short days. I had no preparation or training for what I was about to take on. I am not a nurse; I don’t even work in the medical profession. After we came home my husband … needed 24-hour care. (RGBM003)
I feel that the medical community could have done a better job at making us aware of and equipping us for the devastating stages of decline that were likely going to unfold over just a few months. It would have been horrifying to hear, yet helpful so that our family could have been somewhat prepared. (RGBM025). The equipment we would eventually need, was never told to us. With the exception of the walker and the gait belt that we got when we left the rehab, the rest of the equipment was bought on an as needed basis. From wheelchair, hospital bed, commode. (RGBM055)
Several caregivers discussed the need for better financial support. Although GBM is part of the compassionate allowance for Social Security Disability Insurance (SSDI) in the USA, many patients were the primary financial providers for their family and when they were diagnosed with GBM they had to stop working. Families suffered financial setbacks and difficulty navigating insurance changes. In families where both spouses/partners were working, the caregiver also often had to use job protections of Family Medical Leave Act which may have been unpaid. A wait time of 6 months for SSDI and 2 years for Medicare do not align with the current life expectancy of a GBM patient.
There is a two year waiting period from date of disability to become eligible for Medicare. Most GBM patients don’t have two years to live, as the median life expectancy for a GBM patient is 14 months. There is inconsistency in how Medicare eligibility is determined based on the type of disability. (RGBM018)
Discussion
Caregiving for a patient with GBM is unique among other medical conditions affecting the brain due to the rapid and irreversible disease progression, focal neurological issues and poor performance status related to the area of the brain affected by GBM.10–12 14–16 It is well documented that patients with brain tumours self-reported subjective cognitive functioning does not align with objective cognitive function.24 25 In spite of patient cognitive decline, the caregivers in this study suggest that many of the medical providers relied heavily on patient self-report where treatment decisions and prognosis were discussed with the patient only.26 For patients with cognitive decline and for those who need assistance from a family caregiver, including the family caregiver in care conversations, decision-making is critical to providing high-quality care. For example, the caregivers in this study described meticulous record-keeping regarding the patient’s medical needs and interactions with healthcare providers. They were able to capture the details of the disease trajectory, the patient’s subjective experiences and symptoms, as well as their experiences; all of which are important for making decisions throughout the progression of the illness.
Caregivers felt as if they were not included or had a very limited role in receiving the information and education required to participate in medical decision-making and to prepare for the future with a progressive and terminal diagnosis. Furthermore, this lack of education and inclusion in medical decision-making affected the quality of life of both caregivers and the patients. Patients with gliomas have cognitive, emotional and behavioural needs throughout the disease trajectory that are largely unmet leading to lower quality of life for patients.27 Similarly, caregiver quality of life is associated with increased symptoms of patients with GBM.15 Meeting the emotional and practical needs of primary caregivers of patients with GBM is especially important since feeling in control of the care situation reduces distress reported by the caregiver and improves survival of patients with cancers such as GBM.17
Caregivers indicated that they felt undervalued as members of the care team. The need to support family caregivers’ ability to manage the medical symptoms of their patient with cancer, obtaining help with daily tasks and providing psychological support has been well documented.28 Even without the complexities of brain-involved cancers, high-quality communication between providers and cancer survivors is still lacking during the different phases of the disease.29 Over half of the letters that discussed communication style with healthcare providers described negative experiences known to increase caregiver distress and worsened patient outcomes. Incorporating the primary caregiver in the care team throughout the illness trajectory can provide valuable insight on the health status and functioning of the patient with GBM, yet these caregivers indicated they felt marginalised and were undervalued as members of the care team. Shared decision-making, defined as a collaborative process that involves patients, caregivers and healthcare practitioners in discussing and understanding the risks and benefits to treatment decisions while also accounting for patient values, life situation and desires, is essential for patient-reported quality of life for patients with GBM.30 31
Using a family-centred approach can help to achieve these goals and is important to addressing the needs of the patient and the family.32–34 Family-centred care (FCC) is an approach where ‘2 or more persons who are related in any way’35 are included in care discussions, given opportunities to discuss concerns and are involved in medical decision-making.33 There are five principles FCC: (1) HCPs and family discuss information openly, (2) all perspectives are welcome including cultural and religious practices, (3) respect and empowerment of families with negotiation around roles and decisions from all parties involved in the care including HCPs, (4) collaborative decision-making where all parties have input, and (5) implementation of family-centred policies in healthcare systems.34 36 Not only does this model include the spouse primary caregivers of patients with serious disease,32 but also it highlights the eventual reliance of the patient with GBM on their family caregivers.
Our data demonstrate that the need for better education, communication and support persists throughout the disease trajectory, with the highest need during the ‘living with disease progression’ phase, where patient encounters with the medical community tend to decrease (once per month for SOC chemotherapy) in comparison to the nearly daily encounters during the acute phase. The WHO and Healthy People 2030 prioritised increased quality of life in patients with cancer and identified improving social support as important health determinants.37–39 Positive social and health outcomes from caregivers’ experiences in other diseases provide insight and potential interventions for caregivers of patients with GBM. The poor performance status of patients with GBM greatly impacts caregiver burden across functional areas.15 16
Importantly, the observational study design and qualitative data included many important limitations. All participants in our study had internet access since they were recruited to participate through a private Facebook support group. The letter-writing instructions were minimal with the intention of providing caregivers the opportunity to share what they felt was important. Their letters were not an exhaustive list of experiences and concerns. Letters that failed to mention topics did not mean they were not important or worthy of discussion. Semiquantitative analysis of the number of codes per letter and the number of letters that were coded in a particular way provided a portion of the experience of caregivers of patients with GBM; however, the experience of each caregiver is that of their own and should be valued as such. The self-disclosed demographic data of participants is similar to other published studies,9 10 13 indicating this sample to be similar of female primary caregivers of patients in the USA with GBM. From this study, we know that all the caregivers defined themselves as female spouse or life partners; these primary caregivers were the patient’s family. Due to their intimate involvement with the patient and with the care experience, they wanted to be included and heard as members of the care team for their patient. Future studies are underway to receive quantitative feedback from former and current caregivers regarding their experiences and recommendations for improvement.
Supplementary Material
Acknowledgments
We thank the current and former primary caregivers of patients with glioblastoma for sharing their stories.
Footnotes
Contributors: In this study, the principal investigator (LAM) is a member of the Facebook group and has personal experience as a caregiver of a spouse with GBM. LD is a member of the Facebook group and collected letters from caregivers. LD redacted files and collected informed consent from letter writers. The other authors included students (DLC, MPC, LD) and an expert in qualitative and caregiving research (BL). All members of the research team independently familiarised themselves with the data. Initial systematic coding using NVivo qualitative data management software was performed by two research team members independently (DLC, MPC) with auditing by senior research members (LAM and BL). DLC, MPC and LAM wrote the manuscript. LAM and BL edited the manuscript.
Funding: A portion of the work in this study was funded by a UNCW Corbett Trust Grant.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request. The dataset is available upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The collection of the letters and informed consent was approved by the University of Montana (IRB 224-19). The University of North Carolina Wilmington IRB reviewed the study and provided an exemption (IRB 22-0103) for secondary data analysis on the redacted letters dataset. Participants gave informed consent to participate in the study before taking part.
References
- 1. Ostrom QT, Cioffi G, Gittleman H, et al. CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2012-2016. Neuro Oncol 2019;21:v1–100. 10.1093/neuonc/noz150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Thakkar JP, Dolecek TA, Horbinski C, et al. Epidemiologic and molecular prognostic review of glioblastoma. Cancer Epidemiol Biomarkers Prev 2014;23:1985–96. 10.1158/1055-9965.EPI-14-0275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Oberheim Bush NA, Hervey-Jumper SL, Berger MS. Management of glioblastoma, present and future. World Neurosurg 2019;131:328–38. 10.1016/j.wneu.2019.07.044 [DOI] [PubMed] [Google Scholar]
- 4. Niki C, Kumada T, Maruyama T, et al. Primary cognitive factors impaired after glioma surgery and associated brain regions. Behav Neurol 2020;2020:7941689. 10.1155/2020/7941689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bergo E, Lombardi G, Guglieri I, et al. Neurocognitive functions and health-related quality of life in glioblastoma patients: a concise review of the literature. Eur J Cancer Care 2019;28:e12410. 10.1111/ecc.12410 [DOI] [PubMed] [Google Scholar]
- 6. Collins A, Lethborg C, Brand C, et al. The challenges and suffering of caring for people with primary malignant glioma: qualitative perspectives on improving current supportive and palliative care practices. BMJ Support Palliat Care 2014;4:68–76. 10.1136/bmjspcare-2012-000419 [DOI] [PubMed] [Google Scholar]
- 7. Catt S, Chalmers A, Fallowfield L. Psychosocial and supportive-care needs in high-grade glioma. Lancet Oncol 2008;9:884–91. 10.1016/S1470-2045(08)70230-4 [DOI] [PubMed] [Google Scholar]
- 8. Russell B, Collins A, Dowling A, et al. Predicting distress among people who care for patients living longer with high-grade malignant glioma. Support Care Cancer 2016;24:43–51. 10.1007/s00520-015-2739-0 [DOI] [PubMed] [Google Scholar]
- 9. Schubart JR, Kinzie MB, Farace E. Caring for the brain tumor patient: family caregiver burden and unmet needs. Neuro Oncol 2008;10:61–72. 10.1215/15228517-2007-040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. McConigley R, Halkett G, Lobb E, et al. Caring for someone with high-grade glioma: a time of rapid change for caregivers. Palliat Med 2010;24:473–9. 10.1177/0269216309360118 [DOI] [PubMed] [Google Scholar]
- 11. Boele FW, Klein M, Reijneveld JC, et al. Symptom management and quality of life in glioma patients. CNS Oncol 2014;3:37–47. 10.2217/cns.13.65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Seekatz B, Lukasczik M, Löhr M, et al. Screening for symptom burden and supportive needs of patients with glioblastoma and brain metastases and their caregivers in relation to their use of specialized palliative care. Support Care Cancer 2017;25:2761–70. 10.1007/s00520-017-3687-7 [DOI] [PubMed] [Google Scholar]
- 13. Renovanz M, Hechtner M, Janko M, et al. Factors associated with supportive care needs in glioma patients in the neuro-oncological outpatient setting. J Neurooncol 2017;133:653–62. 10.1007/s11060-017-2484-y [DOI] [PubMed] [Google Scholar]
- 14. Renovanz M, Maurer D, Lahr H, et al. Supportive care needs in glioma patients and their caregivers in clinical practice: results of a multicenter cross-sectional study. Front Neurol 2018;9:763. 10.3389/fneur.2018.00763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Au TH, Willis C, Reblin M, et al. Caregiver burden by treatment and clinical characteristics of patients with glioblastoma. Support Care Cancer 2022;30:1365–75. 10.1007/s00520-021-06514-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Au TH, Willis C, Reblin M, et al. Correction to: caregiver burden by treatment and clinical characteristics of patients with glioblastoma. Support Care Cancer 2022;30:1377–78. 10.1007/s00520-021-06691-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Boele FW, Given CW, Given BA, et al. Family caregivers' level of mastery predicts survival of patients with glioblastoma: a preliminary report. Cancer 2017;123:832–40. 10.1002/cncr.30428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gage-Bouchard EA, LaValley S, Mollica M, et al. Cancer communication on social media: examining how cancer caregivers use Facebook for cancer-related communication. Cancer Nurs 2017;40:332–8. 10.1097/NCC.0000000000000418 [DOI] [PubMed] [Google Scholar]
- 19. Braun V, Clarke V. Novel insights into patients' life-worlds: the value of qualitative research. Lancet Psychiatry 2019;6:720–1. 10.1016/S2215-0366(19)30296-2 [DOI] [PubMed] [Google Scholar]
- 20. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 21. Braun V, Clarke V, Hayfield N. 'A starting point for your journey, not a map': Nikki Hayfield in conversation with virginia braun and cictoria clarke about thematic analysis. Qual Res Psychol 2022;19:424–45. 10.1080/14780887.2019.1670765 [DOI] [Google Scholar]
- 22. Braun V, Clarke V, Cooper H. APA handbook of research methods in psychology. In: Cooper H, eds. Thematic analysis, 2012: 2. 10.1037/13620-000 [DOI] [Google Scholar]
- 23. We are the wives of GBM and this is our story. Secret Facebook group: Facebook; 2015. [Google Scholar]
- 24. Pranckeviciene A, Deltuva VP, Tamasauskas A, et al. Association between psychological distress, subjective cognitive complaints and objective neuropsychological functioning in brain tumor patients. Clin Neurol Neurosurg 2017;163:18–23. 10.1016/j.clineuro.2017.10.007 [DOI] [PubMed] [Google Scholar]
- 25. Nicol C, Ownsworth T, Cubis L, et al. Subjective cognitive functioning and associations with psychological distress in adult brain tumour survivors. J Cancer Surviv 2019;13:653–62. 10.1007/s11764-019-00784-8 [DOI] [PubMed] [Google Scholar]
- 26. Tzelepis F, Sanson-Fisher RW, Zucca AC, et al. Measuring the quality of patient-centered care: why patient-reported measures are critical to reliable assessment. Patient Prefer Adherence 2015;9:831–5. 10.2147/PPA.S81975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sagberg LM, Iversen DH, Fyllingen EH, et al. Brain Atlas for assessing the impact of tumor location on perioperative quality of life in patients with high-grade glioma: a prospective population-based cohort study. Neuroimage Clin 2019;21:101658. 10.1016/j.nicl.2019.101658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kim Y, Carver CS. Recognizing the value and needs of the caregiver in oncology. Curr Opin Support Palliat Care 2012;6:280–8. 10.1097/SPC.0b013e3283526999 [DOI] [PubMed] [Google Scholar]
- 29. Chawla N, Blanch-Hartigan D, Virgo KS, et al. Quality of patient-provider communication among cancer survivors: findings from a nationally representative sample. J Oncol Pract 2016;12:e964–73. 10.1200/JOP.2015.006999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Makoul G, Clayman ML. An integrative model of shared decision making in medical encounters. Patient Educ Couns 2006;60:301–12. 10.1016/j.pec.2005.06.010 [DOI] [PubMed] [Google Scholar]
- 31. Musella A, DeVitto R, Anthony M, et al. The importance of shared decision-making for patients with glioblastoma. Patient Prefer Adherence 2021;15:2009–16. 10.2147/PPA.S314792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Creasy KR, Lutz BJ, Young ME, et al. Clinical implications of family-centered care in stroke rehabilitation. Rehabil Nurs 2015;40:349–59. 10.1002/rnj.188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Clay AM, Parsh B. Patient- and family-centered care: it’s not just for pediatrics anymore. AMA J Ethics 2016;18:40–4. 10.1001/journalofethics.2016.18.1.medu3-1601 [DOI] [PubMed] [Google Scholar]
- 34. Davidson JE, Aslakson RA, Long AC, et al. Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med 2017;45:103–28. 10.1097/CCM.0000000000002169 [DOI] [PubMed] [Google Scholar]
- 35. Patient- and family-centered care defined. n.d. Available: https://www.ipfcc.org/bestpractices/sustainable-partnerships/background/pfcc-defined.html
- 36. Schwartz AC, Dunn SE, Simon HFM, et al. Making family-centered care for adults in the ICU a reality. Front Psychiatry 2022;13:837708. 10.3389/fpsyt.2022.837708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Services UDoHaH . Healthy people 2030: increase quality of life for cancer survivors. In: Healthy People 2030. Edited by promotion OoDPaH. Office of the Assistant Secretary for Health, Office of the Secretary, U.S. Department of Health and Human Services, 2020. [Google Scholar]
- 38. Services USDoHaH . Healthy people 2030: social determinants of health. In: Edited by services USDoHaH. Office of Disease Prevention and Health Promotion, 2020. [Google Scholar]
- 39. Determinants of health. n.d. Available: https://www.who.int/news-room/q-a-detail/determinants-of-health
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request. The dataset is available upon reasonable request.