Key Teaching Points.
-
•
A single spiky component of epicardial local abnormal ventricular activity (LAVA), clearly distinct from local ventricular potentials, was recorded using 2F microelectrodes at the left ventricular summit.
-
•
The distinct spiky element of epicardial LAVA, excluding the nearby ventricular potentials, was identified at the transition point between the distal great cardiac vein and anterior interventricular vein. Its role as the precise focus of the premature ventricular complex (PVC) was confirmed through its electrical characteristics.
-
•
Successful radiofrequency catheter ablation from the left aortic cusp eliminated the spiky component of epicardial LAVA, resulting in subsequent disappearance of PVCs.
Introduction
The left ventricular (LV) summit, the most septal and superior part of the LV outflow tract, is bounded laterally by the great cardiac vein at the location most susceptible to idiopathic premature ventricular complex (PVC), and superiorly and anteriorly by the left main coronary artery bifurcation. Owing to anatomical reasons, namely the presence of epicardium and the surrounding fat pad, it is also a challenging site for catheter ablation.1
A catheter ablation strategy targeting the local abnormal ventricular activity (LAVA) is often useful for ventricular tachyarrhythmias in patients with structural heart diseases. LAVA is a double-component potential that closely follows the ventricular potential during sinus rhythm.2, 3, 4 However, the precise causal relationship between the distinct single spiky component, apart from the surrounding ventricular potential component, which forms a part of epicardial LAVA in the LV summit, and the origin and development of ventricular tachyarrhythmias has not been fully documented.
Case report
A 70-year-old male patient was referred to our hospital for catheter ablation of frequent PVCs. The patient complained of palpitations and chest discomfort for several years. Although he underwent 2 catheter ablation procedures at another hospital, he continued to have PVC symptoms. A resting 12-lead electrocardiogram (ECG) revealed PVCs with sinus rhythm with normal QRS configuration, without ST–T segment abnormalities. Clinical PVCs (QRS duration, 137 ms) exhibited a left bundle branch block and inferior axis pattern with slurring of the R wave in the anterolateral precordial leads. The maximum deflection index in the precordial leads was 0.50, and the Q-wave amplitude ratio of 1.0 in lead aVL/aVR and S-wave amplitude in V1 was 0.8 mV. Based on these parameters, it was considered that this clinical PVC could be ablated from the left coronary cusp (LCC). A 24-hour ambulatory Holter ECG showed 23,276 PVCs per day, representing 24.8% of all cardiac beats in a day. No obvious abnormalities were observed on physical examination, and transthoracic echocardiography revealed no structural heart abnormalities.
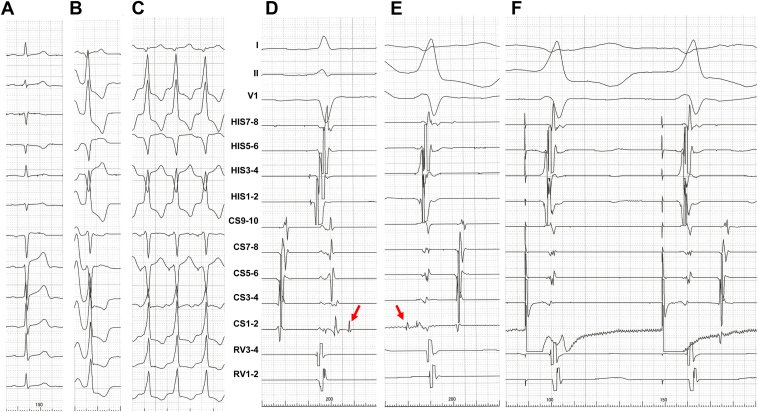
After written informed consent was obtained, electrophysiological analysis and catheter ablation were performed using an impedance-based electroanatomical mapping system (EnSite X; Abbott Medical Japan; Nihon Kohden Co, Ltd, Tokyo, Japan). Multipolar electrode catheters were percutaneously inserted into the left femoral vein and positioned in the His bundle region and right ventricular apex. A 2F microelectrode catheter (EPstarTM Fix; Japan Lifeline, Tokyo, Japan) with a 1.3 mm electrode and a 5 mm interelectrode spacing was inserted to the position of the transition from the distal great cardiac vein (GCV) to the anterior interventricular vein in the coronary sinus (CS 1-2). Distinct spiky late potentials (amplitude 0.56 mV) during the sinus rhythm were observed on CS 1-2; these were clearly separated from the ventricular potential with a distinct single spiky potential 51 ms earlier than the QRS onset of the PVC and a 143 ms delayed late potential from the QRS onset during the sinus rhythm (Figure 1A, 1B, 1D, and 1E). Electrical stimulation from a single spiky potential as the earliest site during PVC was consistent with the QRS complex of clinical PVCs (Figure 1C and 1F) on a 12-lead ECG, with a latency (time interval from electrical stimulus to QRS onset was 51 ms) and almost the same morphology and sequence of ventricular potentials within CS microelectrodes on the intracardiac electrogram. This distinct single spiky potential was considered consistent with a part of an epicardial LAVA.
Figure 1.
A–C: Twelve-lead electrocardiogram (ECG) during sinus rhythm (A), clinical premature ventricular complex (PVC) (B), and electrical bipolar stimulation from the earliest site of distal bipolar microelectrodes (CS 1-2) with excellent match for the QRS complex of clinical PVCs (C). D–F: Surface ECG (I, II, and V1) and intracardiac electrograms during sinus rhythm (D), clinical PVC (E), and electrical stimulation from CS 1-2 (F). Red arrows indicate a single spiky component of local abnormal ventricular activity, late potential during sinus rhythm (D) and prepotential during clinical PVC (E). CS = coronary sinus; HIS = His bundle electrogram; RV = right ventricular apex.
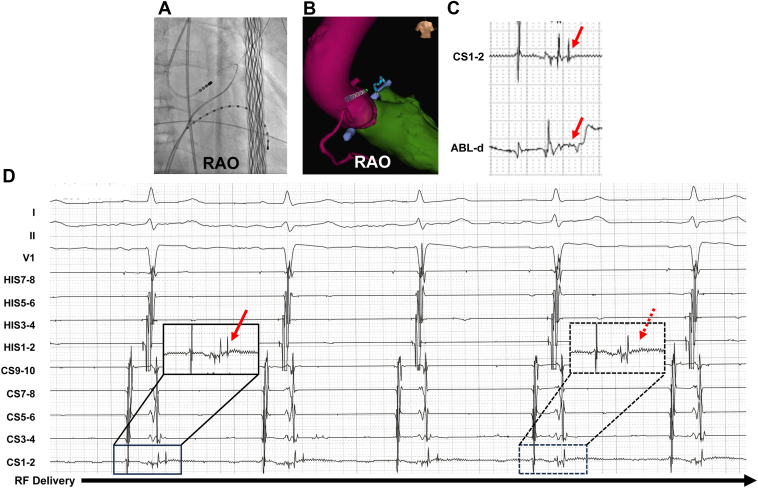
After confirmation that the distinct single spiky component of LAVA on CS 1-2 was the focus of clinical PVC, irrigated radiofrequency ablation catheter (TactiCathTM Contact Force Ablation Catheter; Abbott Medical) was navigated into the LCC using fluoroscopy and an impedance-based electroanatomical mapping system (Figure 2A and 2B). Irrigated radiofrequency energy was applied with an output power of 30 W × 20 g × 30 seconds at a point where the LAVA was clearly recorded in the distal electrodes of the ablation catheter (Figure 2C). Immediately after radiofrequency application, the single spiky component of LAVA in CS 1-2 totally disappeared (Figure 2D). Impedance decreased from 90 Ω to 79 Ω during energy application. Additional applications were delivered in the vicinity of the first radiofrequency application site. The patient has been free of PVCs for 12 months after treatment.
Figure 2.
A: Fluoroscopic image. B: Impedance-based electroanatomical mapping images. C: Intracardiac electrogram at CS 1-2 and ABL-d. The red arrows show the delayed single spiky component of the local abnormal ventricular activity (LAVA) at CS 1-2 and far-field delayed potential of the LAVA at ABL-d during sinus rhythm, respectively. D: Intracardiac electrogram taken immediately after radiofrequency application. The solid and dotted black rectangles indicate the potential of the distal coronary sinus microelectrodes during sinus rhythm and at the 4 beats after radiofrequency (RF) application, respectively. The solid and dotted red arrows indicate the single spiky component of LAVA and its disappearance at the 4 beats after RF application, respectively. ABL-d = distal site of the ablation catheter; HIS = His bundle electrogram; RAO = right anterior oblique 30° view; RV = right ventricular apex.
Discussion
The LV summit constitutes the most superior aspect of LV, and the GCV divides the 2 regions into basal and apical LV summits. Although the basal LV summit is very close to the main trunk of the left coronary artery and epicardial fat, the relationship between the course of the GCV and the left coronary artery varies greatly.5,6 Therefore, the electrodes within the CS cannot always record the accurate origin of a PVC in the LV summit.
LAVA are high-frequency sharp signals that represent near-field signals of slowly conducting tissue, and hence, potential VT circuits; they are therapeutic targets, and their elimination via ablation is effective for the treatment of ventricular arrhythmias in patients with structural heart diseases.2, 3, 4
In this case, a distinct single spiky component of epicardial LAVA was recorded at the transition from the distal GCV to anterior interventricular vein within the CS, as a late potential during sinus rhythm and prepotential during PVC. Local bipolar electrical stimulation from CS 1-2 in the 2F microelectrode only captured the spiky component of the LAVA, without capturing the neighboring ventricular tissue, resulting in excellent pace mapping on 12-lead ECG. The latency (time interval from electrical stimulation to QRS onset) was consistent with the time from spiky potential to QRS onset of PVC. Furthermore, morphology and sequence of ventricular potentials within the CS were almost the same during CS 1-2 pacing and clinical PVC. Accordingly, this distinct single spiky component of epicardial LAVA was confirmed as an accurate focus potential of clinical PVC and led us to delivering radiofrequency energy from the LCC, as the closest site on the endocardial side where the far-field spiky potential of epicardial LAVA could be recorded and was successfully eliminated as a consequence.
To the best of our knowledge, there are no previous reports of a single spiky component of LAVA alone, excluding neighboring ventricular signals, which clearly and strictly demonstrates an accurate PVC focus owing to its electrical behavior. We speculate that this type of spiky component of LAVA regularly synchronizes with the preceding prepotential during PVC, and the following late potential during sinus rhythm might originate from the periphery of the cardiac conduction system and extend to the epicardial side, similar to Purkinje fibers.7
Acknowledgments
Funding Sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosures
The Endowed Department of Advanced Therapeutics for Cardiovascular Disease (Drs Ogawa and Tashiro), Fukuoka University, is supported by Abbott Japan LLC, Biotronik Medical Japan, Boston Scientific Japan, Fukuda Denshi, and Japan Lifeline Co, Ltd. The other authors have nothing to disclose.
References
- 1.Yamada T., Yoshida N., Doppalapudi H., Litovsky S.H., McElderry H.T., Kay G.N. Efficacy of an anatomical approach in radiofrequency catheter ablation of idiopathic ventricular arrhythmias originating from the left ventricular outflow tract. Circ Arrhythm Electrophysiol. 2017;10 doi: 10.1161/CIRCEP.116.004959. [DOI] [PubMed] [Google Scholar]
- 2.Jais P., Maury P., Khairy P., et al. Elimination of local abnormal ventricular activities: a new end point for substrate modification in patients with scar-related ventricular tachycardia. Circulation. 2012;125:2184–2196. doi: 10.1161/CIRCULATIONAHA.111.043216. [DOI] [PubMed] [Google Scholar]
- 3.Komatsu Y., Daly M., Sacher F., et al. Electrophysiologic characterization of local abnormal ventricular activities in postinfarction ventricular tachycardia with respect to their anatomic location. Heart Rhythm. 2013;10:1630–1637. doi: 10.1016/j.hrthm.2013.08.031. [DOI] [PubMed] [Google Scholar]
- 4.Komatsu Y., Daly M., Sacher F., et al. Endocardial ablation to eliminate epicardial arrhythmia substrate in scar-related ventricular tachycardia. J Am Coll Cardiol. 2014;63:1416–1426. doi: 10.1016/j.jacc.2013.10.087. [DOI] [PubMed] [Google Scholar]
- 5.Santangeli P., Marchlinski F.E., Zado E.S., et al. Percutaneous epicardial ablation of ventricular arrhythmias arising from the left ventricular summit: outcomes and electrocardiogram correlates of success. Circ Arrhythm Electrophysiol. 2015;8:337–343. doi: 10.1161/CIRCEP.114.002377. [DOI] [PubMed] [Google Scholar]
- 6.Bales G.S. Great cardiac vein variations. Clin Anat. 2004;17:436–443. doi: 10.1002/ca.10248. [DOI] [PubMed] [Google Scholar]
- 7.Sung R.K., Boyden P.A., Scheinman M. Cellular physiology and clinical manifestations of fascicular arrhythmias in normal hearts. JACC Clin Electrophysiol. 2017;3:1343–1355. doi: 10.1016/j.jacep.2017.07.011. [DOI] [PubMed] [Google Scholar]