Abstract
Introduction:
Renal cell carcinoma, a common kidney tumour which is often incidentally discovered on imaging, can manifest with atypical symptoms. Renal cell carcinoma with rhabdoid features is a rare occurrence and even rarer in case of adults. Renal cell carcinoma has the tendency to form thrombus that can migrate to renal vein, inferior vena cava and even right atrium.
Case presentation:
The authors report a case of an 81-year-old male with rhabdoid renal cell carcinoma presenting with persistent cough for 6–7 months. with tumour thrombus extending into the renal vein and hepatic inferior vena cava. The patient was found feeble for the surgery and hence was treated on anticancer drugs pembrolizumab and axitinib.
Conclusion:
Renal cell carcinoma has the tendency to form tumour thrombus in renal vein and inferior vena cava. Prognosis without surgical intervention in these conditions is very poor.
Keywords: Case report, renal cell carcinoma, rhabdoid, thrombosis
Introduction
Highlights
Renal cell carcinoma is often found incidentally and can present with atypical symptoms.
Renal cell carcinoma with rhabdoid features is a rare condition in children and even rarer in adults.
Prevalence of rhabdoid renal cell carcinoma with venous thromboembolism is very rare.
Surgical intervention is the mainstay of treatment of rhabdoid renal cell carcinoma with tumour thrombus. Prognosis without any surgical intervention is very poor.
Renal cell carcinoma (RCC) is the most common kidney tumour accounting for 2% of global cancer death and diagnoses in the world1. With the widespread use of imaging modalities, most notably computed tomography (CT) and ultrasonography, a large proportion of RCC cases are incidentally identified, with only a few cases presenting with the classic triad of flank pain, haematuria and flank mass2. RCC encompasses a diverse group of cancers with the major subtypes being clear cell RCC, papillary RCC and chromophobe RCC. These subtypes can occasionally exhibit more aggressive features, such as sarcomatoid and rhabdoid dedifferentiation3.
RCC with rhabdoid cells is an aggressive form of neoplasm characterized by eccentric nuclei, prominent nucleoli and the presence of paranuclear intracytoplasmic hyaline globules. RCC with rhabdoid features is a rare occurrence. Pure rhabdoid carcinoma is mostly seen in children and accounts for 2% of the paediatric renal tumours and is even rarer in the adult population4,5. RCC is known for its tendency to migrate into the veins and form a thrombus6. Studies have shown that roughly 10% of patients with RCC experience intravascular tumour growth along the renal vein into the inferior vena cava and 1% of all RCC cases exhibit a further extension of thrombus into the right atrium7,8. Here we present a case of rhabdoid RCC with renal vein thrombosis. The case is reported in line with SCARE 2023 guidelines9.
Case presentation
An 81-year-old native American male with a history of heart failure with a reduced ejection fraction of 20%, hypertensive cardiovascular disease, coronary artery disease status post-coronary artery bypass graft (CABG), hyperlipidemia, unstable angina, and hyperplastic polyps had been experiencing a persistent cough for the past 6–7 months, with production of mucoid, non-bloody sputum. It was associated with fatigue, vomiting and loss of appetite leading to significant weight loss. There was no history of fever, pain, haematuria, hematemesis, chest pain, palpitation, dizziness, headache, urinary symptoms or change in bowel habits. The patient was a former smoker and had a smoking history of one pack per day for more than 20 years. The patient has a family history of coronary artery disease but denies family history of cancer and cerebrovascular accident.
Despite multiple specialist consultations, including neurology, ear-nose and throat, gastroenterology, pulmonology and cardiology, the cause of his cough remained elusive. The patient underwent an abdominal CT scan which revealed a large left-sided renal mass suggestive of RCC, measuring 5.7×6.3×5 cm with involvement of left renal vein and hepatic inferior vena cava, extending up to 2.6 cm away from the right atrium. His right kidney was unaffected (Figs. 1–4).
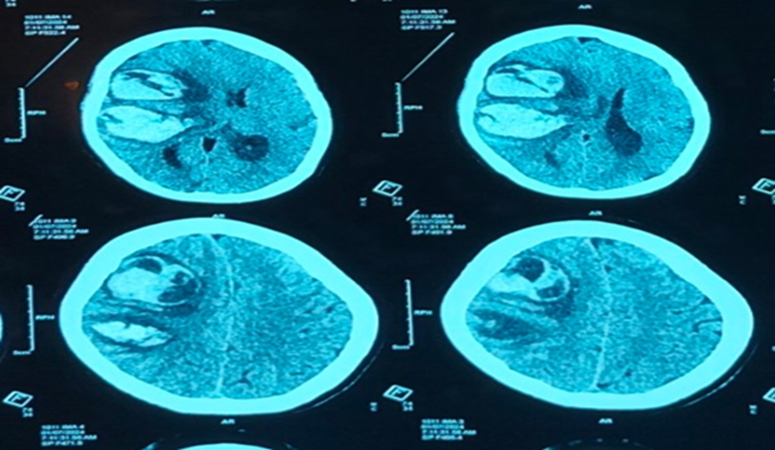
Figure 1.
Computed tomography head suggestive of hyperacute parenchymal lobar haemorrhage showing haematocrit effect and measuring 8 cm3 in right frontal lobe with minimal Perifocal OEdema.
Figure 4.

Computed tomography head of the patient before getting discharged with features suggestive of decompressive craniectomy changes in right fronto parietal area, minimal residual haemorrhage in right frontal lobe with trace oedema without any midline shift.
With this background he presented to our centre. At presentation, the patient was afebrile with pulse rate of 79/min, respiratory rate of 18 breaths per min, blood pressure of 135/79 mm Hg and SpO2 97% in room air. The physical examination was unremarkable. White blood cell (WBC) count was mildly elevated with 11 800/mm3, haemoglobin level was low at 8.9 g/dl with a haematocrit of 27.4% and MCV was 78.4%. His blood tests showed hyponatremia with sodium levels of 128 mmol/l and potassium 4.5 mmol/l. His blood urea nitrogen (BUN) was 17 mg/dl and creatinine was 0.9 mg/dl. Urinalysis showed findings of urinary tract infection (UTI) with a hazy appearance, positive nitrite, leucocyte esterase, elevated WBCs, and trace bacteria. Urine culture found pan-sensitive Escherichia coli.
We performed a MRI of the abdomen which revealed left RCC with tumour thrombus involving the left renal vein and intrahepatic IVC without any intrathoracic extension. The mass extended posteriorly to contact with Gerota’s fascia and involved the left renal collecting system. Needle biopsy of the mass confirmed RCC, clear cell type with areas of high-grade rhabdoid RCC. It was Stage III RCC extending up to hepatic inferior vena cava without any lymph node or distant metastasis. MRI of abdomen revealed the patient had acute renal vein thrombosis. Urine cytology showed no abnormality which further excluded the involvement of urinary tract. The patient was started on a heparin drip for thrombosis and ceftriaxone for UTI. He was evaluated for surgical management but was deemed too weak for surgery and was started on chemotherapy for advanced RCC with Pembrolizumab and Axitinib.
Discussion
In recent years, RCC is often detected incidentally through imaging rather than by the classical triad of haematuria, flank pain and palpable mass, which is seen in only 10% of cases10. In our case also the diagnosis was incidental, and our patient had risk factors such as smoking and hypertension that increased the likelihood of developing RCC. Research has shown that smokers have a 1.38 times higher relative risk of developing RCC compared to non-smokers11. Similarly individuals who have smoked for over 20 years have a 60% higher risk of RCC than those who smoked for less than 20 years12. Hypertension also doubles the risk of developing RCC as compared to normotensive patients13.
Studies have shown that some patients with RCC may experience a chronic cough, which was initially thought to be linked to pulmonary irritation or irritation of the diaphragm by the tumour mass14. However, there have been few cases of chronic cough in RCC patients even when there are no pulmonary metastases15. The most likely cause of this chronic cough in RCC patients is believed to be paraneoplastic syndrome. Prostaglandins, specifically prostaglandin E2 produced from tumour cells, or the immune system can irritate the afferent nerves and start a cough reflex16. In our case, there was no pulmonary metastasis or tumour infiltration in diaphragm suggesting that the persistent cough could potentially be attributed to the prostaglandins produced due to paraneoblastic syndrome.
RCC can continuously grow, penetrate capillary walls, and enter the renal vein, eventually migrating into the inferior vena cava. There are different mechanisms that explains how malignancy can cause venous thromboembolism namely external compression by solid tumours, tumour invasion and malignancy related hypercoagulability17–19. Inflammatory mediators in response to malignancy prompt the activation of coagulation cascade while simultaneously suppressing anticoagulatory pathways. The inhibited removal of fibrin also promotes haemostasis and clotting that ultimately leads to formation of thrombus18.
A study including 784 patients with tumour thrombus in the inferior vena cava found that 98% of these cases were associated with RCC20. The majority of the RCC with tumour thrombus are typically clear cell type. In a study conducted in China among the patients with concurrent RCC and renal vein thrombosis, only 6.4% of the cases showed rhabdoid differentiation21. There is no prior literature that provides us information on the prevalence of either unilateral or bilateral renal vein thrombosis specifically in rhabdoid RCC.
Regarding the prognostic value of the presence and extent of tumour thrombus in RCC patients, studies have produced conflicting results22–24. However, tumour thrombus is generally associated with larger tumours, higher tumour grades and stages as well as distant metastases. This aggressive biological behaviour of the tumour is suggested to have a significant impact on prognosis25. Individuals with RCC and residual tumour thrombus have a seven-fold higher risk of developing venous thromboembolism compared to those whose tumour thrombus is completely removed. Moreover, they are eight times more likely to experience venous thromboembolism than individuals who have never had a tumour thrombus. The heightened risk may be attributed to the fact that residual tumour can disrupt the vascular integrity and disturb venous blood flow, increasing the likelihood of venous thromboembolism26.
Imaging is crucial for differentiating between acute and chronic renal vein thrombosis. In ultrasound, acute thrombosis is characterized by distension due to hyperechoic thrombus and partial or no compressibility without collaterals. Chronic thrombosis presents with an incompressible, narrow and irregular vein showing echogenic thrombus adhering to the venous walls with development of collaterals. MRI typically reveals irregular wall thickening with collaterals and diminished lumen, primarily observed in in chronic renal vein thrombosis27.
Preoperative CT is done to assess the primary tumour. MRI is done to accurately delineate the level or extent of thrombus in cases where CT detects tumour thrombus28. RCC with rhabdoid features, classified as Grade 4 according to the International Society of Urological Pathology, is in itself an independent risk factor for poor prognosis4,29. Surgery is the treatment of choice in patients with RCC and IVC thrombus and the absence of any surgical intervention further worsens the prognosis as the median survival time in these patients is only 5.1 months30.
The surgical procedure depends on the size, location, length, and degree of obstruction of the tumour thrombus in the renal vein and inferior vena cava. Radical nephrectomy along with caval thrombectomy is the surgery of choice in cases of inferior vena cava thrombus in patients with RCC31. Traditionally, a thoracoabdominal incision was the preferred approach for the surgery. However, the abdominal trans-diaphragmatic approach to intrapericardial inferior vena cava and the advantages of optimal exposure of the surgical field with a chevron incision has led to these methods becoming more widely adopted in cases when thrombus is infra-diaphragmatic. Midline sternotomy combined with abdominal incision is given in cases where the thrombus is supradiaphragmatic32,33.
Although surgery is the cornerstone of treatment in RCC with tumour thrombus, the use of antitumor agents and anticoagulants is also important. Traditionally, sunitinib was the anticancer of choice but a randomized controlled trial found that pembrolizumab and axitinib resulted in significantly longer overall survival and progression-free survival34. Risk of tumour embolization in patients with tumour thrombus is only 1.5% but increases when tumour thrombus is in the IVC or beyond. Anticoagulant is used to prevent further progression and embolization of the thrombus35. Low molecular weight heparin has been proven to reduce the risk of recurrent venous thromboembolic events without increasing the risk of bleeding36.
Conclusion
RCC is often discovered by chance on imaging and may manifest as a chronic cough. RCC has the tendency to invade renal veins increasing the risk of developing a tumour thrombus in the renal vein, which can extend into the inferior vena cava. Surgical treatment is crucial for managing this condition and the prognosis for RCC with inferior vena cava thrombus without any surgical intervention is poor.
Patient perspective
Patient knows about the condition and knows why he couldn’t get the surgery and had to undergo medical treatment. He hopes that sharing his experiences can help healthcare professionals better manage similar cases.
Figure 2.
Computed tomography head suggestive of two large epicentres of acute parenchymal haemorrhage measuring 41 cm3 in right frontal lobe and 32 cm3 posterior to it in right temporo parietal lobe with perifocal hypoattenuation.
Figure 3.
Computed tomography head post right fronto parieto temporal decompressive craniectomy and evacuation of right fronto parietal haemorrhage with features suggestive of mild dural Bulge, minimal residual haemorrhage anteriorly, perifocal oedema, midline shift measuring 5 mm with minimal surrounding oedema.
Ethical approval
None.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Source of funding
No funding was received for the study.
Author contribution
M.K., H.B., P.S. and A.K. wrote the original manuscript, reviewed, and edited the original manuscript. M.K., H.B., P.S., A.K., M.W., D.K., S.K., and S.G. reviewed and edited the original manuscript.
Conflicts of interest disclosure
None.
Research registration unique identifying number (UIN)
None.
Guarantor
Dr Manish K.C.
Data availability statement
All the required information is in manuscript itself.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Contributor Information
Manish KC, Email: manishkc496@gmail.com.
Himal Bikram Bhattarai, Email: himalbikrambhattarai@gmail.com.
Pratik Subedi, Email: subedipratik03@gmail.com.
Ashutosh Kashyap, Email: ashtuosh7kashyap@gmail.com.
Manish Wadhwa, Email: manishwadwa@gmail.com.
Dania Kaur, Email: kaurdania@gmail.com.
Sabina Koirala, Email: sabinakoirala33@gmail.com.
Swotantra Gautam, Email: bpkihs.gautam@gmail.com.
References
- 1.Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394–424. [DOI] [PubMed] [Google Scholar]
- 2.Escudier B, Porta C, Schmidinger M, et al. Renal cell carcinoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2016;27(suppl 5):v58–v68. [DOI] [PubMed] [Google Scholar]
- 3.Hsieh JJ, Purdue MP, Signoretti S, et al. Renal cell carcinoma. Nat Rev Dis Primers 2017;3:17009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gökden N, Nappi O, Swanson PE, et al. Renal cell carcinoma with rhabdoid features. Am J Surg Pathol 2000;24:1329–1338. [DOI] [PubMed] [Google Scholar]
- 5.Zderic SA. Renal and adrenal tumors in children. Urol Clin North Am 2004;31:607–617; xi. [DOI] [PubMed] [Google Scholar]
- 6.Reese AC, Whitson JM, Meng MV. Natural history of untreated renal cell carcinoma with venous tumor thrombus. Urol Oncol 2013;31:1305–1309. [DOI] [PubMed] [Google Scholar]
- 7.Schimmer C, Hillig F, Riedmiller H, et al. Surgical treatment of renal cell carcinoma with intravascular extension. Interact CardioVasc Thorac Surg 2004;3:395–397. [DOI] [PubMed] [Google Scholar]
- 8.Quencer KB, Friedman T, Sheth R, et al. Tumor thrombus: incidence, imaging, prognosis and treatment. Cardiovasc Diagn Ther 2017;7(Suppl 3):S165–S177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sohrabi C, Mathew G, Maria N, et al. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg 2023;109:1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Padala SA, Barsouk A, Thandra KC, et al. Epidemiology of renal cell carcinoma. World J Oncol 2020;11:79–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hunt JD, van der Hel OL, McMillan GP, et al. Renal cell carcinoma in relation to cigarette smoking: meta-analysis of 24 studies. Int J Cancer 2005;114:101–108. [DOI] [PubMed] [Google Scholar]
- 12.Theis RP, Dolwick Grieb SM, Burr D, et al. Smoking, environmental tobacco smoke, and risk of renal cell cancer: a population-based case-control study. BMC Cancer 2008;8:387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Colt JS, Schwartz K, Graubard BI, et al. Hypertension and risk of renal cell carcinoma among White and Black Americans. Epidemiology 2011;22:797–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Melicow MM, Uson AC. NONUROLOGIC SYMPTOMS IN PATIENTS WITH RENAL CANCER. J Am Med Assoc 1960;172:146–151. [Google Scholar]
- 15.Patel VR, Morganstern BA, Kavoussi LR. Persistent cough as a paraneoplastic presenting symptom in six patients with renal cell carcinoma. Asian J Urol 2017;4:10–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maher SA, Birrell MA, Belvisi MG. Prostaglandin E2 mediates cough via the EP3 receptor. Am J Respir Crit Care Med 2009;180:923–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Falanga A, Marchetti M, Russo L. The mechanisms of cancer-associated thrombosis. Thromb Res 2015;135:S8–S11. [DOI] [PubMed] [Google Scholar]
- 18.Olson MC, Lubner MG, Menias CO, et al. Venous thrombosis and hypercoagulability in the abdomen and pelvis: causes and imaging findings. RadioGraphics 2020;40:190097. [DOI] [PubMed] [Google Scholar]
- 19.Elajami MK, Mansour E, Bahmad HF, et al. Renal cell carcinoma presenting as syncope due to saddle pulmonary tumor embolism. Diseases 2022;10:119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Protopapas AD, Ashrafian H, Athanasiou T. Tumour thrombi in the suprahepatic inferior vena cava: the cardiothoracic surgeons’ view. Int Scholar Res Notices 2013;2013:e546709. [Google Scholar]
- 21.Yang B, Xia H, Xu C, et al. Impact of sarcomatoid differentiation and rhabdoid differentiation on prognosis for renal cell carcinoma with vena caval tumour thrombus treated surgically. BMC Urol 2020;20:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Skinner DG, Pritchett TR, Lieskovsky G, et al. Vena caval involvement by renal cell carcinoma. Surgical resection provides meaningful long-term survival. Ann Surg 1989;210:387–392; discussion 392-394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hatcher PA, Anderson EE, Paulson DF, et al. Surgical management and prognosis of renal cell carcinoma invading the vena cava. J Urol 1991;145:20–23; discussion 23-24. [DOI] [PubMed] [Google Scholar]
- 24.Moinzadeh A, Libertino JA. Prognostic significance of tumor thrombus level in patients with renal cell carcinoma and venous tumor thrombus extension. Is all T3b the same? J Urol 2004;171(2 Pt 1):598–601. [DOI] [PubMed] [Google Scholar]
- 25.Zisman A, Wieder JA, Pantuck AJ, et al. Renal cell carcinoma with tumor thrombus extension: biology, role of nephrectomy and response to immunotherapy. J Urol 2003;169:909–916. [DOI] [PubMed] [Google Scholar]
- 26.Ihaddadene R, Yokom DW, Le Gal G, et al. The risk of venous thromboembolism in renal cell carcinoma patients with residual tumor thrombus. J Thromb Haemostasis 2014;12:855–859. [DOI] [PubMed] [Google Scholar]
- 27.Karande GY, Hedgire SS, Sanchez Y, et al. Advanced imaging in acute and chronic deep vein thrombosis. Cardiovasc Diagn Ther 2016;6:493–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hallscheidt PJ, Fink C, Haferkamp A, et al. Preoperative staging of renal cell carcinoma with inferior vena cava thrombus using multidetector CT and MRI: prospective study with histopathological correlation. J Comput Assist Tomogr 2005;29:64–68. [DOI] [PubMed] [Google Scholar]
- 29.Delahunt B, Cheville JC, Martignoni G, et al. The International Society of Urological Pathology (ISUP) grading system for renal cell carcinoma and other prognostic parameters. Am J Surg Pathol 2013;37:1490–1504. [DOI] [PubMed] [Google Scholar]
- 30.Hatakeyama S, Yoneyama T, Hamano I, et al. Prognostic benefit of surgical management in renal cell carcinoma patients with thrombus extending to the renal vein and inferior vena cava: 17-year experience at a single center. BMC Urol 2013;13:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Psutka SP, Leibovich BC. Management of inferior vena cava tumor thrombus in locally advanced renal cell carcinoma. Ther Adv Urol 2015;7:216–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Belgrano E, Trombetta C, Liguori G, et al. Intrahepatic tumor thrombectomy through an abdominal diaphragmatic approach. J Urol 1997;158:2233–2234. [DOI] [PubMed] [Google Scholar]
- 33.Vaidya A, Ciancio G, Soloway M. Surgical techniques for treating a renal neoplasm invading the inferior vena cava. J Urol 2003;169:435–444. [DOI] [PubMed] [Google Scholar]
- 34.Rini BI, Plimack ER, Stus V, et al. Pembrolizumab plus Axitinib versus Sunitinib for advanced renal-cell carcinoma. New Engl J Med 2019;380:1116–1127. [DOI] [PubMed] [Google Scholar]
- 35.Kaptein FHJ, van der HT, Braken SJE, et al. Prevalence, treatment, and prognosis of tumor thrombi in renal cell carcinoma. JACC CardioOncol 2022;4:522–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee AYY. Anticoagulation in the treatment of established venous thromboembolism in patients with cancer. J Clin Oncol 2009;27:4895–4901. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the required information is in manuscript itself.