ABSTRACT
The novel coronavirus (COVID-19) has inundated the whole world by causing severe acute respiratory syndrome in humans, thus posing serious public health concerns. The oral and olfactory systems are significantly impacted by the COVID-19 condition, in addition to the respiratory and digestive systems. Oral symptoms of COVID-19 can be caused by a loss in oral hygiene, immune system suppression, a decline in general health, and candidiasis due to prolonged antibiotic use. Because many aerosols and droplets are produced during various dental operations, dental professionals and dentists are at a significant risk of contracting the COVID-19 infection. Few precautionary measures include performing a pre-appointment health screening for all patients, performing aerosol-producing procedures in a designated space or operatory, using proper personal protective equipment and disinfecting the operatory between patients, and limiting the number of dental procedures at one time. Against this background, the purposes of this article are to explore the oral presentations of COVID-19 infection and to emphasize the hazards to dental professionals during COVID-19 pandemic. Additionally, few preventive measures are also highlighted.
KEYWORDS: COVID-19, dentist, infection, pandemic
INTRODUCTION
The coronavirus family is the largest group of single-stranded, non-segmented, and enveloped RNA viruses. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a strain of coronavirus that is responsible for novel coronavirus infection (COVID-19). WHO classified the COVID-19 illness as a worldwide pandemic on January 30, 2020. Although symptomatic COVID-19 patients are the main source of transmission for this illness, recent research has shown that asymptomatic patients, stealth carriers, and people who are still in the incubation period can also carry this infection.[1]
The COVID-19 infection has been associated with the oral cavity because of the identification of human angiotensin-converting enzyme-2 (ACE-2) receptor and transmembrane serine protease 2 in the epithelial cells of salivary glands and the oral mucosa.[2] The purposes of this article are to explore the oral presentations of COVID-19 infection and to emphasize the hazards to dental professionals during the COVID-19 pandemic. Additionally, few preventive measures are also highlighted.
The following are some briefly discussed oral manifestations of COVID-19:
1. Taste impairment
Ageusia, dysgeusia, and hypogeusia are the reported gustatory changes that have been linked with COVID-19.[11] As stated earlier, it has been reported that when the SARS-CoV-2 attaches to ACE-2 receptors, it directly damages the oral and nasal epithelium, thus resulting in gustatory and olfactory disorders.[3]
2. Mucormycosis
A rare but dangerous fungal infection known as mucormycosis is caused by a class of molds known as mucormycetes. People with compromised immune systems are more susceptible to mucormycosis and the infection usually affects the sinuses, brain, or lungs.[4]
3. Vesicobullous lesions
Infections with COVID-19 primarily cause vesicobullous lesions on the tongue and palate. Vesicobullous lesions include blisters, petechiae, erythematous lesions, and lesions that resemble erythema multiforme.[5]
4. Ulcer and erosion
The tongue, hard palate, and labial mucosa are the most typical sites for the development of ulcerative and erosive lesions, which are painful lesions. Thrombotic vasculopathy, vasculitis, and drug eruption consequent to COVID-19 infection are theorized as the causes of ulcers and erosions.[6]
5. Gingival changes
The correlation between COVID-19 infection and gingival abnormalities, including desquamative gingivitis, necrotic interdental papillae, and gingival hemorrhage, has been documented in numerous investigations.[7]
6. Dry mouth
COVID-19 patients have also reported dry mouth as a common symptom.[7]
The following section highlights the risk faced by dental professional during the COVID-19 pandemic.
1. Dental practice
Dental offices have suffered greatly as a result of the COVID-19 outbreak. Dentists and dental employees run a high risk of contracting airborne diseases like COVID-19. When a dentist inhales aerosols and droplets from an infected person or directly contacts contaminated tools or surfaces, they are at risk of contracting COVID-19. The patients seeking dental care are also at high risk of getting COVID-19 infections. For example, when dental equipment is used in a patient’s oral cavity, a significant number of aerosols and droplets mix with the patient’s blood or saliva.[8]
Figure 1 illustrates the transmission of COVID-19 in a dental sitting.[8]
Figure 1.

Transmission of coronavirus in a dental setting
The COVID-19 has had a major effect on dentistry practices. Many practices have temporarily closed as a result of the pandemic, which has created an income loss and service disruption. New regulations and safety procedures must be followed in order for practices to continue operating present difficulties for many of them as well.[8] The need for practices to maintain their financial stability is further highlighted by the rise in the price of supplies and personal protective equipment. Not only physical and financial issues, but also anxiety and burnout among healthcare personnel have grown that could be due to the increased risk of COVID-19 infection, sleep deprivation brought on by work demands, and family obligations.[8]
2. Academics
The COVID-19 pandemic has made academics, including students and teachers working in the field of dentistry, subjected to an increased risk anxiety, depression, and stress. These high levels of stress have triggered the need for the implementation and development of psychological support measures among dental professionals.[9]
3. Dental research
The research conducted in the dental field has also been negatively impacted by the COVID-19 outbreak. Due to the pandemic’s restrictions on patient access to dental care, new research could not be implemented as planned and the outcomes of clinical trials were compromised.[9]
In the following section, some precautionary measures regarding COVID-19 are briefly discussed.
1. Evaluation of patients in the waiting room
The waiting areas in a dental office should have adequate ventilation. Patients’ temperatures should be taken. A minimum of 6 ft social distancing should be followed between patients.[10]
2. Personal protection measurement
It is always recommended to use personal protection equipment (like the use of face masks, protective outwear, gloves, and protective face shields and googles) in a dental setting to avoid the risk of COVID-19 infection.[10]
3. Hand hygiene
Both hand washing with water and soap for 20 s and hand disinfection with alcohol-based solutions are acceptable hand hygiene practices for dental practitioners.[10]
4. Surface disinfection
Every surface in a dental office, including doorknobs, drawer handles, dental chair, and so on, needs to be thoroughly cleaned with 70% ethanol before use.[10]
5. Mouth-rinsing before dental treatments
Mouth rinses and mouthwash solution that contain hydrogen peroxide can help prevent the COVID-19 infection because the virus is sensitive to oxidation.[10]
Figure 2 shows a protocol of screening and managing COVID-19 patients.[11]
Figure 2.
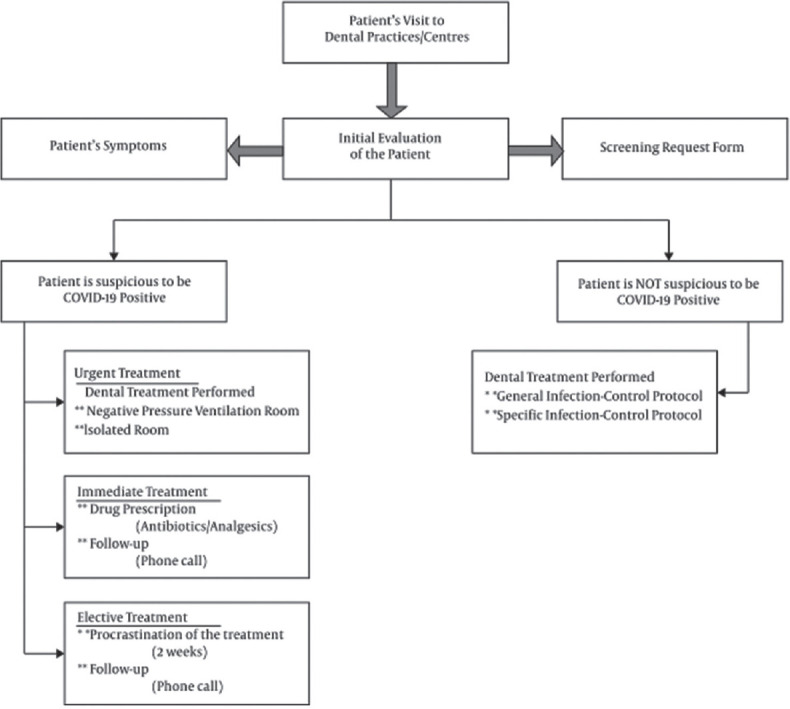
Dental treatment protocols after the COVID-19 outbreak
CONCLUSION
The widespread pandemic of the COVID-19 disease has posed serious health threats to the health and well-being of humans, among which dental professionals are on the top of the list. Due to the potential for the formation of aerosols and the nature of dental procedures, dentistry is one of the most dangerous professions in the world. COVID-19 has a variety of oral symptoms that can be moderate or severe. All dental employees, including students, researchers, dentists, and nurses, should adhere to preventive measures to lessen the risk of COVID-19 infections in the future.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Jin Y, Yang H, Ji W, Wu W, Chen S, Zhang W, et al. Virology, epidemiology, pathogenesis, and control of COVID-19. Viruses. 2020;12:372. doi: 10.3390/v12040372. doi:10.3390/v12040372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xu H, Zhong L, Deng J, Peng J, Dan H, Zeng X, et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020;12:8. doi: 10.1038/s41368-020-0074-x. doi:10.1038/s41368-020-0074-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mahmoud MM, Abuohashish HM, Khairy DA, Bugshan AS, Khan AM, Moothedath MM. Pathogenesis of dysgeusia in COVID-19 patients: A scoping review. Eur Rev Med Pharmacol Sci. 2021;25:1114–34. doi: 10.26355/eurrev_202101_24683. doi:10.26355/eurrev_202101_24683. [DOI] [PubMed] [Google Scholar]
- 4.Liu L, Wei Q, Alvarez X, Wang H, Du Y, Zhu H, et al. Epithelial cells lining salivary gland ducts are early target cells of severe acute respiratory syndrome coronavirus infection in the upper respiratory tracts of rhesus macaques. J Virol. 2011;85:4025–30. doi: 10.1128/JVI.02292-10. doi:10.1128/JVI.02292-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wollina U, Karadağ AS, Rowland-Payne C, Chiriac A, Lotti T. Cutaneous signs in COVID-19 patients: A review. Dermatol Ther. 2020;33:e13549. doi: 10.1111/dth.13549. doi:10.1111/dth.13549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh C, Tay J, Shoqirat N. Skin and mucosal damage in patients diagnosed with COVID-19: A case report. J Wound Ostomy Continence Nurs. 2020;47:435–8. doi: 10.1097/WON.0000000000000690. doi:10.1097/WON.0000000000000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Favia G, Tempesta A, Barile G, Brienza N, Capodiferro S, Vestito MC, et al. COVID-19 symptomatic patients with oral lesions: Clinical and histopathological study on 123 cases of the University Hospital Policlinic of Bari with a purpose of a new classification. J Clin Med. 2021;10:757. doi: 10.3390/jcm10040757. doi:10.3390/jcm10040757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Amante LFLS, Afonso JTM, Skrupskelyte G. Dentistry and the COVID-19 outbreak. Int Dent J. 2021;71:358–68. doi: 10.1016/j.identj.2020.12.010. doi:10.1016/j.identj.2020.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chaudhary FA, Fazal A, Ahmad B, Khattak O, Hyder M, Javaid MM, et al. The impact of COVID-19 pandemic on the psychological health and dental practice of oral healthcare workers: A scoping review. Risk Manag Healthc Policy. 2022;15:1421–31. doi: 10.2147/RMHP.S370125. doi:10.2147/RMHP. S370125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goriuc A, Sandu D, Tatarciuc M, Luchian I. The impact of the COVID-19 pandemic on dentistry and dental education: A narrative review. Int J Environ Res Public Health. 2022;19:2537. doi: 10.3390/ijerph19052537. doi:10.3390/ijerph19052537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shamszadeh S, Parhizkar A, Mardani M, Asgary S. Dental considerations after the outbreak of 2019 novel coronavirus disease: A review of literature. Arch Clin Infect Dis. 2020;15:e103257. https://doi.org/10.5812/archcid.103257. [Google Scholar]


