Abstract
Background and Objectives
Medicaid beneficiaries in many American academic medical centers can receive care in a separate facility than those not covered by Medicaid. We aimed to identify possible disparities in care by evaluating the association between facility type (integrated faculty practice or Medicaid-only outpatient clinic) and telehealth utilization in people with epilepsy.
Methods
We performed retrospective analyses using structured data from the Mount Sinai Health System electronic medical record data from January 2003 to August 2021. We identified people of all ages with epilepsy who were followed by an epileptologist after January 3, 2018, using a validated ICD-9-CM/10-CM coded case definition. We evaluated associations between practice setting and telehealth utilization, an outcome measure that captures the evolving delivery of neurologic care in a post–coronavirus disease 2019 era, using multivariable logistic regression.
Results
We identified 4,586 people with epilepsy seen by an epileptologist, including Medicaid beneficiaries in the Medicaid outpatient clinic (N = 387), Medicaid beneficiaries in the faculty practice after integration (N = 723), and non-Medicaid beneficiaries (N = 3,476). Patients not insured by Medicaid were significantly older (average age 40 years vs 29 in persons seen in Medicaid-only outpatient clinic and 28.5 in persons insured with Medicaid seen in faculty practice [p < 0.0001]). Medicaid beneficiaries were more likely to have drug-resistant epilepsy (DRE), with 51.94% of people seen in Medicaid-only outpatient clinic, 41.63% of Medicaid beneficiaries seen in faculty practice, and 37.2% of non-Medicaid beneficiaries having DRE (p < 0.0001). Medicaid outpatient clinic patients were less likely to have telehealth visits (phone or video); 81.65% of patients in the Medicaid outpatient clinic having no telehealth visits vs 71.78% of Medicaid beneficiaries in the faculty practice and 70.89% of non-Medicaid beneficiaries (p < 0.0001). In an adjusted logistic regression analysis, Medicaid beneficiaries had lower odds (0.61; 95% CI 0.46–0.81) of using teleneurology compared with all patients seen in faculty practice (p = 0.0005).
Discussion
Compared with the Medicaid-only outpatient clinic, we found higher telehealth utilization in the integrated faculty practice with no difference by insurance status (Medicaid vs other). Integrated care may be associated with better health care delivery in people with epilepsy; thus, future research should examine its impact on other epilepsy-related outcomes.
Introduction
Medicaid beneficiaries and socioeconomically disadvantaged persons with epilepsy represent one-third of all people with epilepsy and experience disparities in access to longitudinal care, specialists, timely diagnosis, video-EEG monitoring, and antiseizure medication (ASM).1-6 Nationally, Medicaid coverage is 83.6% non-White (Black, Hispanic, Asian/Native Hawaiian and Pacific Islander, American Indian/Alaska Native, Multiple Races),7 further compounding insurance-related access disparities onto racial and ethnic disparities in care. Non-White people with epilepsy experience higher premature mortality from epilepsy and epilepsy-related causes, increased emergency department utilization, increased hospitalizations, decreased access to epilepsy specialists, underutilization of epilepsy surgery, decreased social support, and poorer patient-provider communication and trust.2,8-13
As expected, the 2010 Affordable Care Act led to overall improvements in access to care and reduction in premature mortality due to Medicaid expansion to uninsured persons.14 However, studies continue to show that across primary and specialty care, Medicaid beneficiaries in the general population still experience lower access to in-network physicians,15 higher wait times,16 and poorer health care outcomes than their non-Medicaid counterparts.17
In New York City, many academic medical centers operate a two-tiered system, offering one practice setting for commercially insured patients (faculty practices) and another for Medicaid insured patients (outpatient clinics).18,19 Black and Hispanic New Yorkers are more likely to be publicly insured or uninsured, thus are substantially affected by insurance-based facility differences.20 In general, practices with a high share of minority patients have been shown to have more chaotic work environments, less access to medical supplies, and spend less time with patients.21 More broadly, people with public insurance report higher rates of insurance-based discrimination, feelings of lack of continuity of care, and lack of confidence in accessing care.22
In 2008, the Bronx Health REACH Coalition filed a civil rights complaint, citing violations in the Hill-Burton Act,23 advocating against separate and unequal practice settings based on insurance status. Studies found that Medicaid-only outpatient clinics are primarily operated by fellows and residents rather than attendings and perform lower on quality metrics relating to continuity of care, timely communication of medical records, and after-hours emergency availability as mandated by the New York State Department of Health.18,20 Two-tiered systems persist across a number of states including in but not limited to New York, Pennsylvania, Virginia, and Texas and across nursing homes nationally.24,25 The reasons for this may be due to insurance status, as in New York, or due to geographic disparities that reflect systemic racism, such as in nursing homes where 80% of Black residents reside in 28% of US nursing homes.25
While the reasons for the fragmentation in care are multifold and have yet to be studied at a hospital level, they can be attributed, in large part, to a consequence of the fragmentation in health care delivery at the nationwide level. One study demonstrated that although 96% of physicians accept new patients, 31% did not accept new Medicaid patients.15 This finding could relate to low Medicaid reimbursement—the same study found that states with increased Medicaid to Medicare fee ratios had increased acceptance of new Medicaid patients.15 Although Medicare fees are also lower than private insurance, only 17% of physicians did not accept new Medicare patients—this is likely due to Medicare fees being higher than Medicaid fees: on average, 28% lower than Medicare reimbursements for all services and 33% lower than Medicare reimbursements for primary care.26,27 In addition, such fragmentation may not exist for Medicare patients as Medicare accounts for a majority of national health care spending—in 2021, it accounted for 26% of spending on hospital care and physician and clinical services.28 Considering the aging population and reliance on Medicare for hospital reimbursements, this population is not carved out into a separate facility as the Medicaid population is. While it is unclear, from a hospital administration perspective, why separating Medicaid patients by facility would improve financials, it is presumable that reimbursement rates are largely involved.
In 2018, the neurology department at Mount Sinai Hospital adopted New York State Public Health Law Article 28 which among other things achieves integration by incentivizing Medicaid beneficiaries to be seen in faculty practices along with commercially insured patients.29 Ultimately working toward integration of care, Article 28 certification requires facilities to meet a wide range of quality metrics.29 Clinical spaces are incentivized to be certified as Article 28 facilities by 340B billing practices which provide higher reimbursement rates than non-Article 28 facilities.30 In this study, we aimed to quantify disparities in epilepsy care for Medicaid beneficiaries seen in the faculty practice vs the Medicaid-only outpatient clinic. We select an outcome measure that coincides well with our study period, which captures 1 year prior to and 1 year after the onset of the coronavirus disease 2019 (COVID-19) pandemic, and the ongoing acceptability and utilization of telehealth in neurologic care: teleneurology visits.31-33 Our hypothesis was that integration of care would be associated with better access to teleneurology for people living with epilepsy who have Medicaid insurance, with increased visits associated with better care access and delivery for people with epilepsy.
Ethnic and racial minority populations in the United States are heterogeneous and experience culturally and historically unique barriers to care. Although many studies focus specifically on non-Hispanic (NH) Black and Hispanic people, we aim to use inclusive language, acknowledging that non-White people in the United States face racially and ethnically driven structural disparities in care that cannot and should not be homogenized. We acknowledge that multiple marginalized racial and ethnic groups have been understudied in disparities literature, limiting references to data on all groups that may be affected by systemic inequities, but conduct this study with the motivation to advocate for equitable care for all marginalized racial and ethnic groups.
Methods
Study Design, Data Source, and Cohort Identification
We performed a retrospective analysis within a large multicenter New York State health system, the Mount Sinai Health System (MSHS). People with epilepsy were ascertained from the MSHS epilepsy faculty practice, which sees both privately and publicly insured patients under New York Public Health Law Article 28 since 2018, as well as the outpatient epilepsy clinic, which only sees Medicaid beneficiaries. All data were obtained from the Mount Sinai Data Warehouse which holds the MSHS electronic health record, Epic (Epic Systems Corporation, Verona, WI).
Study Cohort Identification
Patients of all ages who met the validated epilepsy case definition between January 2003 and August 2021 were included.34 Persons were defined to have epilepsy if they had either (1) an (ICD-9-CM (345.x [except 345.2 and 345.5]) or ICD-10-CM (G40.x [except G40.xx1]) epilepsy-related code in any diagnostic position) with or without an ASM or (2) an (ICD-9-CM (345.2, 345.3, or 780.3x) or an ICD-10-CM epilepsy or seizure-related codes (G40.xx1, G41.x, or R56.x) in any diagnostic position) with at least 1 ASM. This case definition has been validated in the MSHS with a sensitivity of 95% (CI 93%–97%), specificity of 72% (CI 68%–77%), negative predictive value (NPV) of 92% (CI 89%–95%), and positive predictive value (PPV) of 80% (CI 77%–84%).34 Once patients met the case definition for epilepsy, only those visits in which epilepsy was coded in the primary diagnostic position (e.g., for refills, laboratory test results, follow-ups, or visits to any department) were included. This was to ensure that the main reason for follow-up in the epilepsy practices or clinics was epilepsy. While our outcome was measured starting in 2018, we identified patients starting in 2003 as this is the earliest data available from them Mount Sinai Data Warehouse and electronic medical record (EMR).
Outcomes
The primary outcome was utilization of teleneurology in the epilepsy faculty practice or Medicaid-only outpatient clinic (January 3, 2018–August 3, 2021) for a primary diagnosis of epilepsy, defined as utilization of at least 1 telehealth visit during the study period. Only unique patient visits are represented in either setting (i.e., the same patient was not seen in both settings), as there was no concerted effort to transfer patients between the Medicaid-only outpatient clinic and faculty practice after the adoption of Article 28. Instead, all Medicaid patients seen in the faculty practice after 2018 were new patients, either seen after a direct referral to faculty practice or after being admitted to the hospital without an existing epileptologist, thus later scheduled for follow-up in faculty practice.
Exposures of Interest
The primary variable of interest in this analysis was practice setting (Medicaid-only outpatient clinic vs faculty practice). The primary patient characteristic was insurance status/type (commercially insured, Medicaid, Medicare, self-pay, and other). While all insurance types were included, we were primarily interested in Medicaid beneficiary outcomes by practice setting. Non-Medicaid beneficiaries (commercially insured, Medicare, and other) were used as a comparison group for those persons with Medicaid insurance seen in faculty practice. While the study objective is to observe the impact of integrated practice setting on outcome, not insurance status, we use this comparator to demonstrate the differences in patient characteristics between Medicaid and non-Medicaid patients and show the consistency in teleneurology utilization by practice setting yet across insurance statuses in our logistic regression analysis.
Covariates
Other characteristics included in this study were age, sex, race/ethnicity, marital status, language, smoking status, Charlson Comorbidity Index, and additional neurologic comorbidities associated with epilepsy not included in the above comorbidity indices (e.g., traumatic brain injury, brain tumor, CNS infection, multiple sclerosis). Sex referred to sex assigned at birth and was self-reported as a binary variable (female, male). Race/ethnicity was self-reported and recorded in the EMR as Hispanic, NH White, NH Black, NH Asian, other, or unknown. Comorbidities were defined before and up to data availability for a patient, meaning they could have been defined before the study period of 2018–2021 within a patient's EMR. We adjusted for epilepsy severity (i.e., drug-resistant epilepsy [DRE]) using a validated drug-resistant ICD-9-CM/10-CM–based case definition with sensitivity of 83%, specificity 77%, NPV 93%, and PPV 56%.34
Statistical Analysis
All outcomes and covariates were described using summary statistics: frequencies and percentages for categorical variables and mean and SD or median and range for continuous variables. Chi-squared tests and Wilcoxon rank-sum tests were conducted to compare descriptive statistics. Multivariable logistic regression was conducted to assess the association between telehealth utilization and practice setting, after controlling for covariates.
Standard Protocol Approvals, Registrations, and Patient Consents
The Mount Sinai Hospital Institutional Review Board (IRB) approved the use of patient data and waived the need for individual informed consent under STUDY-18-00778.
Data Availability
Researchers with the appropriate credentials, IRB training, and certification can apply to the senior authors to request access after a data use agreement has been executed with Mount Sinai.
Results
Our sample included 4,586 patients, 387 (8.44%) of whom were Medicaid beneficiaries seen in the Medicaid-only outpatient clinic, 723 (15.77%) of whom were Medicaid beneficiaries seen in the integrated faculty practice, and 3,476 (75.8%) of whom were non-Medicaid beneficiaries seen in the integrated faculty practice. A flowchart of sample allocation is presented in eFigure 1.
Descriptive statistics are presented in Table 1. While the objective of the study was to use practice setting as the exposure, we demonstrate the differences in Medicaid vs non-Medicaid patients across practice settings, showing that there are similarities in patient characteristics of the Medicaid patients that are seen in either the Medicaid-only outpatient clinic or integrated faculty practice. Non-Medicaid beneficiaries were significantly older (average age 40 years) vs an average age of 29 years in the Medicaid-only outpatient clinic and 28.5 in the Medicaid faculty practice (p < 0.0001). Patients in Medicaid-only outpatient clinic and Medicaid beneficiaries in faculty practice were more frequently Hispanic and NH Black (p < 0.0001). In total, 34.63% of patients in the Medicaid-only outpatient clinic were Hispanic vs 30.71% in the Medicaid faculty practice and 16.46% in non-Medicaid faculty practice. Overall, 22.22% of patients in the Medicaid-only outpatient clinic and 23.1% of Medicaid beneficiaries in faculty practice were NH Black compared with 15.3% of non-Medicaid beneficiaries in faculty practice. Patients in the Medicaid-only outpatient clinic were more frequently single (82.17% of patients in the Medicaid-only outpatient clinic were single compared with 76.9% in Medicaid faculty practice and 58.86% in the non-Medicaid faculty practice [p < 0.0001]). Non-Medicaid beneficiaries in faculty practice more frequently spoke English (93.5%) vs 89.41% in the Medicaid-only outpatient clinic and 85.62% in Medicaid faculty practice (p < 0.0001).
Table 1.
Descriptive Characteristics of People With Epilepsy by Practice Setting and Insurance Type
| Total | Outpatient clinic (Medicaid) | Faculty practice (Medicaid) | Faculty practice (non-Medicaid) | p Value | |
| Total, n (%) | 4,586 (100) | 387 (8.44) | 723 (15.77) | 3,476 (75.8) | |
| Age, mean (SD) | 37 (22.2) | 29 (17.2) | 28.5 (18.5) | 40 (22.7) | <0.0001 |
| Sex, % | 0.672 | ||||
| Female | 51.7 | 50.39 | 50.62 | 52.07 | |
| Male | 48.3 | 49.61 | 49.38 | 47.93 | |
| Race/ethnicity, % | <0.0001 | ||||
| Hispanic | 20.24 | 34.63 | 30.71 | 16.46 | |
| Non-Hispanic White | 29.33 | 15.76 | 14.11 | 34 | |
| Non-Hispanic Black | 17.12 | 22.22 | 23.1 | 15.3 | |
| Non-Hispanic Asian | 4.25 | 2.84 | 5.67 | 4.11 | |
| Other | 9.81 | 15.5 | 13.42 | 8.43 | |
| Unknown | 19.25 | 9.04 | 13 | 21.69 | |
| Marital status, % | <0.0001 | ||||
| Married, life partner | 21.06 | 9.82 | 11.2 | 24.37 | |
| Single | 63.67 | 82.17 | 76.9 | 58.86 | |
| Divorced, separated, widowed | 6.26 | 2.84 | 3.73 | 7.16 | |
| Unknown/other | 9.01 | 5.17 | 8.16 | 9.61 | |
| Language, % | <0.0001 | ||||
| English | 91.91 | 89.41 | 85.62 | 93.5 | |
| Spanish | 5.19 | 6.98 | 10.79 | 3.83 | |
| Other | 1.61 | 1.03 | 2.35 | 1.52 | |
| Unknown | 1.29 | 2.58 | 1.24 | 1.15 | |
| Smoking status, % | <0.0001 | ||||
| Current smoker | 6.98 | 9.56 | 10.1 | 6.04 | |
| Former smoker | 14.98 | 9.82 | 9.96 | 16.6 | |
| Never smoker | 60.92 | 61.76 | 66.94 | 59.58 | |
| Never assessed | 10.84 | 15.76 | 7.88 | 10.9 | |
| Unknown | 6.28 | 3.1 | 5.12 | 6.88 | |
| Body mass index, median (IQR) | 25.1 (21.1, 29.6) | 24.8 (21.3, 30.2) | 25 (19.8, 30.2) | 25.1 (21.2, 29.5) | 0.4886 |
| Charlson Comorbidity Index, mean, median (range) | 1.39, 0 (0, 19) | 1.22, 0 (0, 15) | 1.04, 0 (0, 19) | 1.48, 0 (0, 18) | 0.0114 |
| Myocardial infarction | 2.05 | 0.78 | 1.11 | 2.39 | 0.0145 |
| Congestive heart failure | 4.43 | 2.33 | 3.32 | 4.89 | 0.0192 |
| Peripheral vascular disease | 7.26 | 5.94 | 4.56 | 7.97 | 0.0034 |
| Cerebrovascular disease | 14.89 | 11.63 | 10.65 | 16.14 | 0.0001 |
| Dementia | 3.16 | 1.03 | 1.52 | 3.74 | 0.0001 |
| Chronic pulmonary disease | 13.5 | 17.83 | 16.74 | 12.34 | 0.0002 |
| Rheumatic disease | 2.33 | 1.81 | 1.8 | 2.5 | 0.4036 |
| Peptic ulcer disease | 0.85 | 0.26 | 1.24 | 0.83 | 0.2735 |
| Mild liver disease | 4.82 | 6.46 | 4.43 | 4.72 | 0.0076 |
| Diabetes without complications | 9.01 | 7.75 | 6.22 | 9.72 | 0.0002 |
| Diabetes with complications | 4.01 | 2.84 | 1.52 | 4.66 | 0.0011 |
| Paraplegia or hemiplegia | 7.89 | 12.66 | 6.92 | 7.57 | 0.0108 |
| Renal disease | 5.34 | 3.1 | 3.87 | 5.9 | <0.0001 |
| Cancer | 8.13 | 3.62 | 4.29 | 9.44 | <0.0001 |
| Moderate–severe liver disease | 0.68 | 1.03 | 0.69 | 0.63 | 0.5384 |
| Metastatic carcinoma | 2.51 | 1.03 | 1.8 | 2.82 | 0.0397 |
| AIDS | 1.42 | 2.07 | 1.11 | 1.41 | 0.4336 |
| Neuro-related comorbidities, % | |||||
| Drug-resistant epilepsy | 39.14 | 51.94 | 41.63 | 37.2 | <0.0001 |
| Traumatic brain injury | 5.67 | 3.88 | 6.09 | 5.78 | 0.2665 |
| Multiple sclerosis | 3.49 | 1.55 | 1.11 | 4.2 | <0.0001 |
| Brain tumor | 1.68 | 0.52 | 1.38 | 1.87 | 0.11 |
| CNS infection | 1.11 | 0.78 | 1.11 | 1.15 | 0.911 |
Abbreviation: IQR = interquartile range.
Charlson Comorbidity Index was highest in non-Medicaid faculty practice (mean 1.48) compared with a mean of 1.22 and 1.04 in the Medicaid-only outpatient clinic and Medicaid faculty practice, respectively (p = 0.0114). There were statistically significant differences for myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, dementia, diabetes with and without complications, renal disease, cancer, metastatic carcinoma, chronic pulmonary disease, mild liver disease, and paraplegia or hemiplegia, as presented in Table 1.
DRE was the most frequent in the Medicaid-only outpatient clinic, with 51.94% of patients in the Medicaid-only outpatient clinic having DRE compared with 41.63% in Medicaid faculty practice and 37.2% in non-Medicaid faculty practice (p < 0.0001). Multiple sclerosis was more common in non-Medicaid faculty practice (4.2%) compared with 1.55% in the Medicaid-only outpatient clinic and 1.11% in Medicaid faculty practice (p < 0.0001).
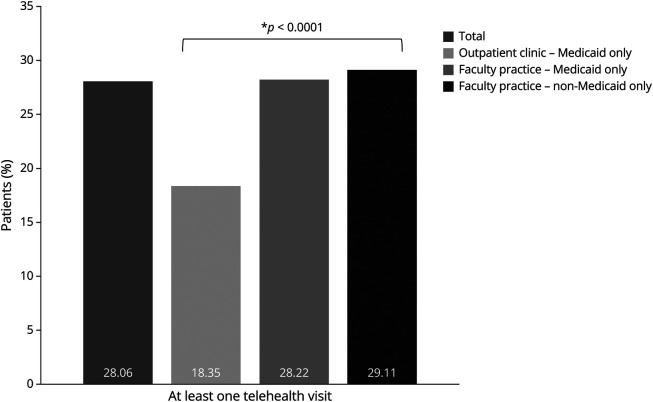
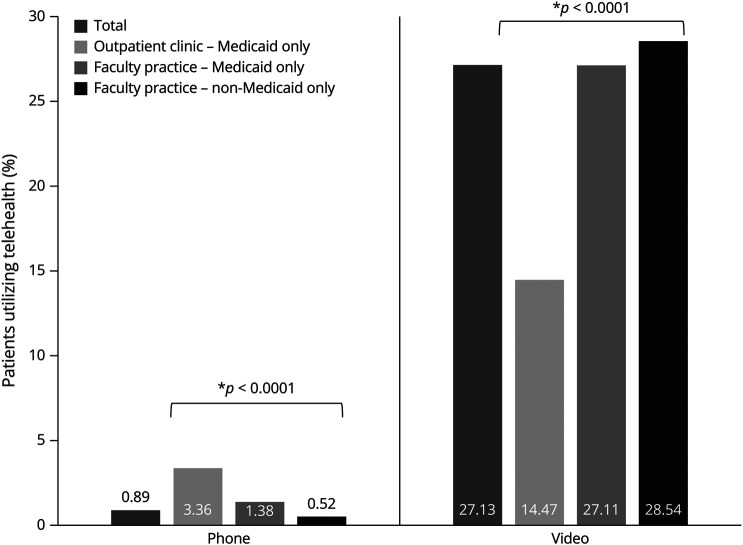
Telehealth utilization is presented in Figure 1. Non-Medicaid beneficiaries in faculty practice had the highest proportion of patients with at least 1 telehealth visit (29.11%) compared with 28.22% in Medicaid faculty practice and 18.35% in the Medicaid-only outpatient clinic (p < 0.0001). As shown in Figure 2, video visits were more frequent in non-Medicaid faculty practice—28.54% of patients using telehealth used video visits compared with 27.11% in Medicaid faculty practice and 14.47% in the Medicaid-only outpatient clinic (p < 0.0001). Phone visits were more frequent in the Medicaid-only outpatient clinic, with 3.36% of patients using telehealth having a phone visit compared with 1.38% in Medicaid faculty practice and 0.52% in non-Medicaid faculty practice (p < 0.0001).
Figure 1. Utilization of Teleneurology by Practice Setting.
Figure 2. Utilization of Teleneurology by Practice Setting and Visit Type.
We conducted a multivariable logistic regression, as presented in Table 2, and controlling for age, sex, race and ethnicity, marital status, language, smoking status, Charlson Comorbidity Index, and additional neuro-related comorbidities. Compared with non-Medicaid patients in the faculty practice, the adjusted odds ratio for telehealth utilization in the Medicaid-only outpatient clinic was 0.61 (p = 0.0005) with a 95% CI of 0.46–0.81. There was no significant difference between odds of teleneurology utilization in Medicaid patients seen in faculty practice when compared with non-Medicaid patients seen in faculty practice, demonstrating the consistency of the facility type as the exposure of interest.
Table 2.
Adjusted Logistic Regression Analysis of Teleneurology Utilization
| aOR | 95% CI | p Value | |
| Practice setting | |||
| Outpatient clinic (Medicaid only) | 0.61 | 0.46–0.81 | 0.0005 |
| Faculty practice (Medicaid) | 1.03 | 0.85–1.25 | 0.7757 |
| Faculty practice (non-Medicaid) | Reference | ||
| Age | 1.00 | 1.00–1.00 | 0.9656 |
| Sex | |||
| Female | 1.01 | 0.89–1.16 | 0.8414 |
| Male | Reference | ||
| Race/ethnicity | |||
| Hispanic | 0.944 | 0.775–1.151 | 0.5704 |
| Non-Hispanic Black | 0.803 | 0.659–0.98 | 0.0311 |
| Non-Hispanic Asian | 1.269 | 0.915–1.759 | 0.1532 |
| Other | 0.54 | 0.416–0.701 | <0.0001 |
| Unknown | 0.27 | 0.211–0.347 | <0.0001 |
| Non-Hispanic White | Reference | ||
| Marital status | |||
| Single | 0.59 | 0.49–0.70 | <0.0001 |
| Divorced, separated, widowed | 0.65 | 0.49–0.87 | 0.0039 |
| Unknown/other | 0.68 | 0.50–0.91 | 0.0089 |
| Married, life partner | Reference | ||
| Language | |||
| Spanish | 0.76 | 0.54–1.06 | 0.1023 |
| Other | 0.88 | 0.52–1.50 | 0.6428 |
| Unknown | 0.43 | 0.19–0.98 | 0.0443 |
| English | Reference | ||
| Smoking status | |||
| Current smoker | 0.83 | 0.629–1.095 | 0.1874 |
| Former smoker | 1.139 | 0.936–1.386 | 0.1938 |
| Never assessed | 0.608 | 0.46–0.804 | 0.0005 |
| Unknown | 1.879 | 1.435–2.459 | <0.0001 |
| Never smoker | Reference | ||
| Charlson Comorbidity Index | 0.95 | 0.93–0.98 | 0.0025 |
| Additional neuro-related comorbidities (“no” as reference) | |||
| Drug resistant epilepsy | 1.00 | 0.87–1.16 | 0.9616 |
| Traumatic brain injury | 1.21 | 0.92–1.60 | 0.1799 |
| Multiple sclerosis | 1.16 | 0.81–1.64 | 0.4194 |
| Brain tumor | 1.64 | 1.02–2.64 | 0.0428 |
| CNS infection | 1.44 | 0.80–2.59 | 0.2205 |
Abbreviation: aOR = adjusted odds ratio.
Discussion
Our study found that the integrated faculty practice, which saw both Medicaid and non-Medicaid beneficiaries after 2018, was associated with higher telehealth utilization relative to the Medicaid-only outpatient clinic in people with epilepsy. Although telehealth utilization does not represent 100% of all visits, our study period captures the height of the COVID-19 pandemic when many visits were conducted virtually. We selected teleneurology visits as our primary outcome, rather than in-person visits, considering the impact of COVID-19 on neurologic care and increases in teleneurology utilization both before and after the onset of the pandemic.31-33 Our study period includes 1 year prior to and 1 year after the onset of the COVID-19 pandemic—capturing the onset of the pandemic was not a limitation but rather a strength in the study design allowing for continuity in our utilization metric over time. Our aim was not to do a time series analysis and see effects pre–COVID-19 and post–COVID-19 but rather to analyze telehealth utilization in different types of settings. Thus, in this setting, telehealth utilization can serve as a proxy for overall epilepsy surveillance and follow-up.35-37 Our findings thus highlight the potential benefit of integrated care for overall improved health care delivery in the Medicaid population. In addition, our findings serve to advocate for the benefit of teleneurology care, especially as distance to specialty neurology care can be an important social determinant of health for people with epilepsy.12
We found significant demographic differences by practice setting that are important in the interpretation of our results. For example, patients seen in the faculty practice were significantly older than those in the Medicaid-only outpatient clinic, likely due to the faculty practice seeing Medicare patients in addition to those who are privately insured, signaling a potential difference in age-related comorbidities, and amenability/comfort with telehealth usage.38
Patients seen in the Medicaid-only outpatient clinic more frequently identified as Hispanic, NH Black, and Spanish speaking than in the faculty practice. Medicaid beneficiaries seen in faculty practice had similar proportions of Hispanic and NH Black people and overall, the highest proportion of Spanish speaking people. Studies have shown that Medicaid beneficiaries are majority non-White; thus, systemic racism, institutional policies, and unconscious bias are inextricably compounded on the access disparities faced due to insurance status.39,40
Prior work has shown that Black, Latinx, and non-English speaking low-income patients are less likely to complete a scheduled telehealth visit and more likely to partake in audio-only telehealth than video-enabled telehealth.41 Our study similarly found greater audio-only telehealth utilization in the Medicaid-only outpatient clinic when compared with Medicaid beneficiaries in the faculty practice and non-Medicaid beneficiaries in the faculty practice clinic. Studies have shown that videoconference telehealth visits improve diagnostic accuracy and reduce readmissions in comparison with phone telehealth visits, highlighting potential disparities by practice setting for this patient population.42
Despite an increase in reimbursement for telehealth following the 1135 waivers43 in March 2020 for people with Medicaid,44 barriers to telehealth utilization in Medicaid, non-English speaking, and minority patients persist. For example, decreased digital acumen, need for interpreters, internet availability, time availability, or privacy availability have been shown to be ongoing barriers to telehealth utilization.38,45,46 Our study did not include a qualitative evaluation of telehealth barriers in persons with Medicaid insurance. However, anecdotal discussions with epilepsy attendings have suggested that many patients were not set up for video visits because they did not activate their EMR portal through which video visits are conducted, or there were connectivity issues limiting their ability to complete a video visit. This suggests that equity-based interventions to improve activation of telehealth interfaces, digital literacy, and internet access may be beneficial.
Notably, we found that significantly more people in the Medicaid-only outpatient clinic had DRE (51.94%) when compared with 41.63% in Medicaid beneficiaries seen in the faculty practice and 37.2% of persons not insured with Medicaid in the faculty practice (p < 0.0001). Considering that it is known that Hispanic and NH Black people are less likely to receive epilepsy surgery,8 this finding has potentially important implications for providing equitable, guideline-adherent epilepsy care. DRE is higher in lower socioeconomic groups, but there may be a component of “pseudo” DRE in our population, considering the social and cultural barriers to medication access and adherence.47 If surgery is less accessible to minority patients and patients with lower socioeconomic status, and this group does indeed have a higher frequency of DRE, integration of the Medicaid-only outpatient clinic with the faculty practice may be a helpful step in improving access to epilepsy surgery.
One review48 characterized barriers to epilepsy surgery with the acronym “FACETS,” describing “fear of treatment, access to care, communication barriers, education, trust between patient and physician, and social support.” In considering the imperative to increase access to epilepsy surgery, it may not be sufficient to only increase referrals to epilepsy surgery for minority patients. It is also important to consider additional determinants of these disparities, for example, how cultural misconceptions can inform fear and how a language barrier and use of an interpreter can decrease conversation and decision-making time with physicians.48
Among this study's strengths is that there is a scarcity of studies quantifying the association between segregation of care and access to care in epilepsy. However, our study also has several limitations. First, the study was retrospective; thus, disparities in telehealth outcomes cannot be causally attributed to practice setting. Furthermore, we used ICD-9-CM/10-CM codes to identify those with epilepsy and DRE which could be associated with misclassification of cases. However, we used a case definition validated in our EMR for both epilepsy and DRE, and we believe that this type of misclassification would be nondifferential between groups. This study was also conducted in a single health system which could limit generalizability; however, the MSHS catchment is particularly diverse, capturing a population that is at least 51% non-White. In addition, the MSHS catchment which includes New York City and parts of New Jersey, Connecticut, and New York State is very socioeconomically, racially, ethnically, and linguistically diverse, capturing a wide range of patient experiences in accessing care. We also acknowledge that our discussion of racial/ethnic minorities is data-limited to self-identified race/ethnicity in the EMR. The only racial/ethnic minority group other than Hispanic and NH Black is NH Asian, which comprises only 4.25% of our study population. We also include individuals with a race/ethnicity of “other” and “unknown” and acknowledge the diverse experiences of individuals of unknown heritage or multiracial backgrounds. We acknowledge that non-White and/or minority racial/ethnic groups covered by Medicaid may experience structurally driven disparities in access to care, though are limited in commenting on the unique disparities of these groups given the limited population size in our data set and demographic. While aiming to advocate for equitable access to care for all racial/ethnic minority groups, we further acknowledge and emphasize that the experiences of all such groups are not homogeneous and encourage future studies to focus specifically on racial and ethnic minority groups that are often underdiscussed in the literature.
New York City is also unique in its proximity to other hospitals and concentration of medical specialists such as epileptologists. Given the location of patients included in this study in New York City, it is possible that health care services could have been sought outside the MSHS, and thus, not able to be captured by our data. Our study also lacked a qualitative component addressing the reasons for the differences in practice setting with regard to patient satisfaction, staff differences, and resource disparities, among other quality of care measures, which will be important avenues for future work. In addition, we determined that new patients are more likely to first establish care in person rather than through telehealth, somewhat limiting the use of our outcome. However, we also noted that despite there being a higher proportion of new Medicaid patients in the faculty practice when compared with the Medicaid-only outpatient clinic, there was still higher telehealth utilization in the integrated faculty practice, strengthening our overall finding. Finally, EMR data do not allow for us to measure potentially important confounders such as social support and internet/device availability that could affect the patient experience in using health care services.
Despite these limitations, our study shows some potential benefits of Medicaid practice integration for people with epilepsy. We show that telehealth utilization is higher in integrated care settings which may in turn lead to improvement in other health outcomes. Our results suggest that institutions should be further encouraged to adopt integrated practices that can treat both Medicaid and non-Medicaid beneficiaries. Our findings also suggest that health care financing may perpetuate structural racism when an insurance status designed for lower-income adults lacks reimbursement, coverage, or equitable value-based incentives.25 Advocacy for integrated care is thus advocacy for equitable care for all people with epilepsy.
Glossary
- ASM
antiseizure medication
- COVID-19
coronavirus disease 2019
- DRE
drug-resistant epilepsy
- EMR
electronic medical record
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- ICD-10-CM
International Classification of Diseases, Tenth Revision, Clinical Modification
- IRB
institutional review board
- MSHS
Mount Sinai Health System
- NH
non-Hispanic
- NPV
negative predictive value
- PPV
positive predictive value
Appendix. Authors
| Name | Location | Contribution |
| Evelyn Gotlieb, BS | Icahn School of Medicine at Mount Sinai, New York, NY | Drafting/revision of the manuscript for content, including medical writing for content; study concept or design; analysis or interpretation of data |
| Parul Agarwal, PhD | Department of Population Health Science and Policy and Institute for Healthcare Delivery Science, Icahn School of Medicine at Mount Sinai, New York, NY | Drafting/revision of the manuscript for content, including medical writing for content; major role in the acquisition of data; study concept or design; analysis or interpretation of data |
| Leah J. Blank, MD, MPH | Departments of Neurology, Population Health Science, and Policy and Institute for Healthcare Delivery Science, Icahn School of Medicine at Mount Sinai, New York, NY | Drafting/revision of the manuscript for content, including medical writing for content; study concept or design; analysis or interpretation of data |
| Churl-Su Kwon, MD, MPH | Departments of Neurology, Neurosurgery, Epidemiology, and the Gertrude H. Sergievsky Center, Columbia University, New York, NY | Drafting/revision of the manuscript for content, including medical writing for content; analysis or interpretation of data |
| Maria Muxfeldt, MD | Department of Neurology, Icahn School of Medicine at Mount Sinai, New York, NY | Drafting/revision of the manuscript for content, including medical writing for content; analysis or interpretation of data |
| James J. Young, MD, PhD | Department of Neurology, Icahn School of Medicine at Mount Sinai, New York, NY | Drafting/revision of the manuscript for content, including medical writing for content |
| Nathalie Jette, MD, MSc, FRCPC | Departments of Neurology, Population Health Science, and Policy and Institute for Healthcare Delivery Science, Icahn School of Medicine at Mount Sinai, New York, NY; Department of Clinical Neurosciences, University of Calgary, Alberta, Canada | Drafting/revision of the manuscript for content, including medical writing for content; major role in the acquisition of data; study concept or design; analysis or interpretation of data |
Study Funding
This project was supported by the Mount Sinai Data Warehouse. This project was also funded by The Mount Sinai Research Office Patricia S. Levinson Fellowship for Community Oriented Research and Service Award.
Disclosure
E. Gotlieb and P. Agarwal report no disclosures relevant to the manuscript. L.J. Blank received research support from the American Epilepsy Society, Epilepsy Foundation, NORSE Institute, the Mount Sinai Claude D Pepper Older American Independence Center (5P30AG028741-11), and the Icahn School of Medicine Department of Neurology for work unrelated to this manuscript. C.-S. Kwon, M. Muxfeldt, and J. Young report no disclosures relevant to the manuscript. N. Jette received grant funding paid to her institution from the National Institute of Neurological Disorders and Stroke (NIH U24NS107201, NIH IU54NS100064, and NIH U24NS113849), the American Epilepsy Society and the NORSE Institute for work unrelated this manuscript. She receives an honorarium for her work as an Associate Editor of Epilepsia. Go to Neurology.org/N for full disclosures.
References
- 1.Bensken WP, Navale SM, Andrew AS, Jobst BC, Sajatovic M, Koroukian SM. Delays and disparities in diagnosis for adults with epilepsy: findings from U.S. Medicaid data. Epilepsy Res. 2020;166:106406. doi: 10.1016/j.eplepsyres.2020.106406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kelvin EA, Hesdorffer DC, Bagiella E, et al. Prevalence of self-reported epilepsy in a multiracial and multiethnic community in New York City. Epilepsy Res. 2007;77(2-3):141-150. doi: 10.1016/j.eplepsyres.2007.09.012 [DOI] [PubMed] [Google Scholar]
- 3.Schiltz NK, Koroukian SM, Singer ME, Love TE, Kaiboriboon K. Disparities in access to specialized epilepsy care. Epilepsy Res. 2013;107(1-2):172-180. doi: 10.1016/j.eplepsyres.2013.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sirven J, Sprout GT, Speer M, et al. The influence of social determinants of health on epilepsy treatment delays in an Arizona Medicaid population. Epilepsy Behav. 2022;126:108473. doi: 10.1016/j.yebeh.2021.108473 [DOI] [PubMed] [Google Scholar]
- 5.Thurman DJ, Kobau R, Luo YH, Helmers SL, Zack MM. Health-care access among adults with epilepsy: the U.S. National Health Interview Survey, 2010 and 2013. Epilepsy Behav. 2016;55:184-188. doi: 10.1016/j.yebeh.2015.10.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hamade YJ, Palzer EF, Helgeson ES, Hanson JT, Walczak TS, McGovern RA. Persistent racial and ethnic disparities as a potential source of epilepsy surgery underutilization: analysis of large national datasets from 2006-2016. Epilepsy Res. 2021;176:106725. doi: 10.1016/j.eplepsyres.2021.106725 [DOI] [PubMed] [Google Scholar]
- 7.Kaiser Family Foundation. Medicaid Coverage Rates for the Nonelderly by Race/Ethnicity. 2022. Accessed March 26, 2024. https://www.kff.org/medicaid/state-indicator/nonelderly-medicaid-rate-by-raceethnicity/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D [Google Scholar]
- 8.Szaflarski M, Szaflarski JP, Privitera MD, Ficker DM, Horner RD. Racial/ethnic disparities in the treatment of epilepsy: what do we know? What do we need to know? Epilepsy Behav. 2006;9(2):243-264. doi: 10.1016/j.yebeh.2006.05.011 [DOI] [PubMed] [Google Scholar]
- 9.Burneo JG, Black L, Knowlton RC, Faught E, Morawetz R, Kuzniecky RI. Racial disparities in the use of surgical treatment for intractable temporal lobe epilepsy. Neurology. 2005;64(1):50-54. doi: 10.1212/01.WNL.0000150829.89586.25 [DOI] [PubMed] [Google Scholar]
- 10.Begley CE, Basu R, Reynolds T, et al. Sociodemographic disparities in epilepsy care: results from the Houston/New York City health care use and outcomes study. Epilepsia. 2009;50(5):1040-1050. doi: 10.1111/j.1528-1167.2008.01898.x [DOI] [PubMed] [Google Scholar]
- 11.Burneo JG, Jette N, Theodore W, et al. Disparities in epilepsy: report of a systematic review by the North American Commission of the International League Against Epilepsy. Epilepsia. 2009;50(10):2285-2295. doi: 10.1111/j.1528-1167.2009.02282.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Szaflarski M. Social determinants of health in epilepsy. Epilepsy Behav. 2014;41:283-289. doi: 10.1016/j.yebeh.2014.06.013 [DOI] [PubMed] [Google Scholar]
- 13.Kaiboriboon K, Schiltz NK, Bakaki PM, Lhatoo SD, Koroukian SM. Premature mortality in poor health and low income adults with epilepsy. Epilepsia. 2014;55(11):1781-1788. doi: 10.1111/epi.12789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sommers BD, Baicker K, Epstein AM. Mortality and access to care among adults after state Medicaid expansions. N Engl J Med. 2012;367(11):1025-1034. doi: 10.1056/NEJMsa1202099 [DOI] [PubMed] [Google Scholar]
- 15.Decker SL. In 2011 nearly one-third of physicians said they would not accept new Medicaid patients, but rising fees may help. Health Aff (Millwood). 2012;31(8):1673-1679. doi: 10.1377/hlthaff.2012.0294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gotlieb EG, Rhodes KV, Candon MK. Disparities in primary care wait times in Medicaid versus commercial insurance. J Am Board Fam Med. 2021;34(3):571-578. doi: 10.3122/jabfm.2021.03.200496 [DOI] [PubMed] [Google Scholar]
- 17.Koroukian SM, Bakaki PM, Raghavan D. Survival disparities by Medicaid status: an analysis of 8 cancers. Cancer. 2012;118(17):4271-4279. doi: 10.1002/cncr.27380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Golub M, Calman N, Ruddock C, et al. A community mobilizes to end medical apartheid. Prog Community Health Partnersh. 2011;5(3):317-325. doi: 10.1353/cpr.2011.0041 [DOI] [PubMed] [Google Scholar]
- 19.Calman N, Ruddock C, Golub M, Le L. Separate and Unequal: Medical Apartheid in New York City. 2005. Accessed January 13, 2024. latinoshe.org/pdf/MedicalApartheidNYC.pdf. [Google Scholar]
- 20.Calman NS, Golub M, Ruddock C, Le L, Hauser D; Action Committee of the Bronx Health REACH Coalition. Separate and unequal care in New York City. J Health Care Law Policy. 2006;9(1):105-120. [PubMed] [Google Scholar]
- 21.Varkey AB, Manwell LB, Williams ES, et al. Separate and unequal: clinics where minority and nonminority patients receive primary care. Arch Intern Med. 2009;169(3):243-250. doi: 10.1001/archinternmed.2008.559 [DOI] [PubMed] [Google Scholar]
- 22.Han XX, Call KT, Pintor JK, Alarcon-Espinoza G, Simon AB. Reports of insurance-based discrimination in health care and its association with access to care. Am J Public Health. 2015;105(suppl 3):S517-S525. doi: 10.2105/Ajph.2015.302668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.42 U.S.C. §291 et seq.
- 24.Gee GC, Ford CL. Structural racism and health inequities: old issues, new directions. Du Bois Rev. 2011;8(1):115-132. doi: 10.1017/S1742058X11000130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yearby R, Clark B, Figueroa JF. Structural racism in historical and modern US health care policy. Health Aff (Millwood). 2022;41(2):187-194. doi: 10.1377/hlthaff.2021.01466 [DOI] [PubMed] [Google Scholar]
- 26.Decker SL. In 2011 nearly one-third of physicians said they would not accept new Medicaid patients, but rising fees may help. Health Aff (Millwood). 2012;31(8):1673-1679. doi: 10.1377/hlthaff.2012.0294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.KFF.org. Medicaid-to-Medicare Fee Index. Accessed January 13, 2024. kff.org/medicaid/state-indicator/medicaid-to-medicare-fee-index/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. [Google Scholar]
- 28.Cubanski J and Neuman T. What to Know about Medicare Spending and Financing. January 19, 2023. Accessed March 26, 2024. https://www.kff.org/medicare/issue-brief/what-to-know-about-medicare-spending-and-financing/. [Google Scholar]
- 29.Senate TNYS. Section 2800. In: Senate TNYS, editor. Section 2800–Section 2818. The Laws of New York: Consoidated Laws of New York; 2014. [Google Scholar]
- 30.NACHC. 2nd Edition NACHC 340B Manual 2018. Accessed January 13, 2024. nachc.org/wp-content/uploads/2018/09/Medicaid-chapter-from-NACHC-340B-Manual.pdf. [Google Scholar]
- 31.Hatcher-Martin JM, Adams JL, Anderson ER, et al. Telemedicine in neurology: telemedicine work group of the American Academy of Neurology update. Neurology. 2020;94(1):30-38. doi: 10.1212/WNL.0000000000008708 [DOI] [PubMed] [Google Scholar]
- 32.Hatcher-Martin JM, Busis NA, Cohen BH, et al. American Academy of Neurology telehealth position statement. Neurology. 2021;97(7):334-339. doi: 10.1212/WNL.0000000000012185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ahrens SM, Ostendorf AP, Lado FA, et al. Impact of the COVID-19 pandemic on epilepsy center practice in the United States. Neurology. 2022;98(19):e1893-e1901. doi: 10.1212/WNL.0000000000200285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lemus HN, Tai HH, Iin JY, et al. Development and Validation of ICD-10-CM Based Algorithms to Identify Epilepsy in Electronic Health Records. American Epilepsy Society Abstracts; 2021. Accessed January 13, 2024. cms.aesnet.org/abstractslisting/development-and-validation-of-icd-10-cm-based-algorithms-to-identify-epilepsy-in-electronic-health-records. [Google Scholar]
- 35.Domingues RB, Mantese CE, Aquino EDS, Fantini F, Prado GFD, Nitrini R. Telemedicine in neurology: current evidence. Arq Neuropsiquiatr. 2020;78(12):818-826. doi: 10.1590/0004-282x20200131 [DOI] [PubMed] [Google Scholar]
- 36.Bahrani K, Singh MB, Bhatia R, et al. Telephonic review for outpatients with epilepsy: a prospective randomized, parallel group study. Seizure. 2017;53:55-61. doi: 10.1016/j.seizure.2017.11.003 [DOI] [PubMed] [Google Scholar]
- 37.Rasmusson KA, Hartshorn JC. A comparison of epilepsy patients in a traditional ambulatory clinic and a telemedicine clinic. Epilepsia. 2005;46(5):767-770. doi: 10.1111/j.1528-1167.2005.44804.x [DOI] [PubMed] [Google Scholar]
- 38.Sachs JW, Graven P, Gold JA, Kassakian SZ. Disparities in telephone and video telehealth engagement during the COVID-19 pandemic. JAMIA Open. 2021;4(3):ooab056. doi: 10.1093/jamiaopen/ooab056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Williams DR, Rucker TD. Understanding and addressing racial disparities in health care. Health Care Financ Rev. 2000;21(4):75-90. [PMC free article] [PubMed] [Google Scholar]
- 40.Feagin J, Bennefield Z. Systemic racism and U.S. health care. Soc Sci Med. 2014;103:7-14. doi: 10.1016/j.socscimed.2013.09.006 [DOI] [PubMed] [Google Scholar]
- 41.Lau KHV, Anand P, Ramirez A, Phicil S. Disparities in telehealth use during the COVID-19 pandemic. J Immigr Minor Health. 2022;24(6):1590-1593. doi: 10.1007/s10903-022-01381-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rush KL, Howlett L, Munro A, Burton L. Videoconference compared to telephone in healthcare delivery: a systematic review. Int J Med Inform. 2018;118:44-53. doi: 10.1016/j.ijmedinf.2018.07.007 [DOI] [PubMed] [Google Scholar]
- 43.Centers for Medicare & Medicaid Services. Medicare telemedicine health care provider fact sheet. 2020. Accessed June 30, 2020. cms.gov/newsroom/fact-sheets/medicare-telemedicinehealth-care-provider-fact-sheet.
- 44.Chu RC, Peters C, De Lew N, Sommers BD. State Medicaid Telehealth Policies Before and During the COVID-19 Public Health Emergency. Office of the Assistant Secretary for Planning and Evaluation; 2021. [Google Scholar]
- 45.Nouri S, Khoong EC, Lyles CR, Karliner L. Addressing equity in telemedicine for chronic disease management during the Covid-19 pandemic. NEJM Catal Innov Care Deliv. 2020;1(3):13. [Google Scholar]
- 46.Perrin PB, Rybarczyk BD, Pierce BS, Jones HA, Shaffer C, Islam L. Rapid telepsychology deployment during the COVID-19 pandemic: a special issue commentary and lessons from primary care psychology training. J Clin Psychol. 2020;76(6):1173-1185. doi: 10.1002/jclp.22969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bensken WP, Fernandez Baca Vaca G, Alberti PM, et al. Racial and ethnic differences in antiseizure medications among people with epilepsy on Medicaid: a case of potential inequities. Neurol Clin Pract. 2023;13(1):e200101. doi: 10.1212/CPJ.0000000000200101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nathan CL, Gutierrez C. FACETS of health disparities in epilepsy surgery and gaps that need to be addressed. Neurol Clin Pract. 2018;8(4):340-345. doi: 10.1212/CPJ.0000000000000490 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Researchers with the appropriate credentials, IRB training, and certification can apply to the senior authors to request access after a data use agreement has been executed with Mount Sinai.