Abstract
Introduction
The treatment gap for mental health disorders persists in low‐ and middle‐income countries despite overwhelming evidence of the efficacy of task‐sharing mental health interventions. Key barriers in the uptake of these innovations include the absence of policy to support implementation and diverting of staff from usual routines in health systems that are already overstretched. South Africa enjoys a conducive policy environment; however, strategies for operationalizing the policy ideals are lacking. This paper describes the Mental health INTegration Programme (MhINT), which adopted a health system strengthening approach to embed an evidence‐based task‐sharing care package for depression to integrate mental health care into chronic care at primary health care (PHC).
Methods
The MhINT care package consisting of psycho‐education talks, nurse‐led mental health assessment, and a structured psychosocial counselling intervention provided by lay counsellors was implemented in Amajuba district in KwaZulu‐Natal over a 2‐year period. A learning health systems approach was adopted, using continuous quality improvement (CQI) strategies to facilitate embedding of the intervention.
MhINT was implemented along five phases: the project phase wherein teams to drive implementation were formed; the diagnostic phase where routinely collected data were used to identify system barriers to integrated mental health care; the intervention phase consisting of capacity building and using Plan‐Do‐Study‐Act cycles to address implementation barriers and the impact and sustaining improvement phases entailed assessing the impact of the program and initiation of system‐level interventions to sustain and institutionalize successful change ideas.
Results
Integrated planning and monitoring were enabled by including key mental health service indicators in weekly meetings designed to track the performance of noncommunicable diseases and human immunovirus clinical programmes. Lack of standardization in mental health screening prompted the validation of a mental health screening tool and testing feasibility of its use in centralized screening stations. A culture of collaborative problem‐solving was promoted through CQI data‐driven learning sessions. The province‐level screening rate increased by 10%, whilst the district screening rate increased by 7% and new patients initiated to mental health treatment increased by 16%.
Conclusions
The CQI approach holds promise in facilitating the attainment of integrated mental health care in resource‐scarce contexts. A collaborative relationship between researchers and health system stakeholders is an important strategy for facilitating the uptake of evidence‐based innovations. However, the lack of interventions to address healthcare workers' own mental health poses a threat to integrated mental health care at PHC.
Keywords: integrated mental health care, quality improvement, task‐sharing
Abbreviations
- APC
adult primary health care
- BMH
Brief Mental Health Screening Tool
- CMDs
common mental disorders
- CNP
clinical nurse practitioner
- CQI
continuous quality improvement
- DHIS
District Health Information System
- DoH
Department of Health
- EN
enrolled nurse
- KZN
KwaZulu‐Natal
- LHS
learning health system
- LMICs
low‐ and middle‐income countries
- MH
mental health
- MhINT
Mental health INTegration Programme
- NCD
noncommunicable diseases
- NDoH
National Department of Health
- PDSA
Plan‐Do‐Study‐Act
- PHC
primary health care
- PRIME
Programme for Improving Mental Health
- SA
South Africa
1. BACKGROUND
The treatment gap for mental health disorders in South Africa is notably high and estimated to be as high as 92%. 1 Factors that contribute to this crisis are common to those reported in other Low‐ and Middle‐income Countries (LMICs) and these include limited mental health specialists, concentration of mental health services in hospitals, stigma associated with mental health problems, and poor financial investment in mental health services by local governments. 1 , 2 , 3 , 4 Integration of mental health services into primary health care (PHC) through task‐sharing has been presented as a feasible remedy for challenges in mental healthcare access in resource‐scarce contexts, 5 , 6 , 7 especially as it applies to common mental disorders (CMDs) such as anxiety, depression and substance use disorders, which constitute the bulk of the global burden of disease 8 and can be effectively managed out of hospital. 1 , 9 The efficacy of task‐sharing mental health interventions in symptom reduction of CMDs across sub‐Saharan Africa is well‐established, 10 including in South Africa. 11
However, there have been barriers to the uptake of these innovations in LMICs and these include the absence of policy to support implementation, increase in spending, shifting of norms and beliefs about health service provision, and diverting of staff from usual routines in health systems that are already overstretched. 12 , 13 , 14 , 15 , 16 Whilst South Africa has a favorable policy environment for integrated care, it has lacked clear implementation strategies for achieving the policy ideals and this has contributed to the country's challenges in embedding evidence‐based interventions successfully into routine practice. Additionally, prevailing acute shortages in health staff continue to be a barrier to the uptake of some (even cost‐effective) innovations whose efficacy has been established in the country. 1 , 6
These challenges emphasize the need for focusing on health systems strengthening to address contextual barriers to the uptake and sustainability of evidence‐based health innovations. 17
This paper describes the implementation of an intervention called the Mental health INTegration Programme (MhINT), which aimed to introduce an evidence‐based collaborative care package for depression into the PHC platform and simultaneously strengthen the health system to embed the intervention. The MhINT collaborative care package developed and tested through the Programme for Improving Mental health (PRIME), 18 , 19 , 20 consisted of psycho‐education talks to increase mental health literacy; enhanced Adult Primary Health Care (APC) guidelines to strengthen nurse‐led mental health assessment and a structured 8‐session manualized depression and/or chronic medication adherence counselling provided by facility‐based lay counsellors under supervision. 18 It provides lessons on the utilization of data‐driven continuous quality improvement (CQI) strategies to facilitate the uptake of an evidence‐based innovation and foster a learning health system to achieve integrated mental health care in a resource‐scarce context.
2. METHODS
MhINT was implemented in Amajuba District, which is situated in the north‐western corner of KwaZulu‐Natal comprising Newcastle (mostly urban), Emadlangeni (rural), and Dannhauser (peri‐urban) subdistricts. About 91% of the district's population of approximately 565 227 rely solely on the public health system for health services. The district has three hospitals (two in Newcastle and one in Emadlangeni) and specialist psychiatric and psychological services are located in the hospitals in Newcastle subdistrict. PHC services are delivered through 25 fixed PHC facilities, eight mobile clinics, and one Community Health Care Centre located in Dannhauser subdistrict. As per national guidelines, the PHC platform in Amajuba provides both curative and preventive health services at the community level and within PHC facilities. The package of care is inclusive of chronic disease care as well as the management of communicable and noncommunicable diseases across the developmental span. 21 Amajuba District was recommended as an implementation site as it is a National Health Insurance pilot site* and due to it having PHC facilities that meet “Ideal Clinic” status (an indicator of PHC functionality). 22 It was anticipated that innovations developed in the district through MhINT could be spread to other districts in the province and potentially, nationwide. This strategy has often been observed in high‐performing health systems, where a small pilot within the health system is used for experimenting, learning, and modeling new methods for the rest of the health system. 23 The MhINT programme was implemented over a 2‐year period from September 2017 to October 2019.
2.1. Implementation approach
Continuous quality improvement (CQI) strategies were utilized within a Learning Health Systems approach to introduce each component of the MhINT package into the health system as well as tailor, modify, and embed the intervention within the health system. Learning health systems have been defined as those that typically seek to be continuously learning and improving in order to remain efficient and responsive to their goals. 24
In learning health systems, learning occurs both through formal knowledge and skills transfer and through the transference of attitudes, behaviors, and will to generate innovative practices to enable improvement and embedding of health innovations into routine practice. 23 , 24 The team approach is central in this regard and teams are used as vehicles for learning and driving improvement in both clinical and nonclinical processes. 24 The focus of CQI methods on understanding the system and using data to drive change prevents a tendency to blame and facilitates collaboration, and scientific thinking in addressing health system challenges. 25 , 26 Whilst there are multiple strategies within the CQI umbrella, the model of improvement developed by Associates in Process Improvement (API) 27 was adopted for the MhINT Programme due to its versatility and accessibility even without advanced training in QI. 23 Within this model, three key questions are posed in relation to the project, namely What are we trying to accomplish? How will we know if a change is an improvement? And what changes can we make that will result in improvement? These questions guided activities along five implementation phases namely; the project, diagnostic, intervention, impact, and improvement sustainment phases. 28
The project phase entailed building the relationship between the researchers and health system stakeholders and setting project aims. 28 As such, multidisciplinary teams were formed at different levels of the health system leveraging pre‐existing networks to avoid creating new structures. These teams historically lacked representation from mental health and as such, it was novel to have the provincial multidisciplinary team being led by the Mental Health and Substance Abuse Directorate. This team was formed first in order to attain access to the implementing district and ensure project aims were aligned with policy and the Department of Health (DoH)'s strategic objectives for integrated care at PHC.
The district and subdistrict teams were set, and their primary responsibility was to align and enhance the motivations of the human resources in testing and implementing MhINT programme components. 26 Facility‐based teams would be more intimately involved in operational matters, developing and testing change ideas to facilitate integrated mental health care.
In order to set project aims routinely collected Mental Health (MH) service data for Amajuba district collated in the District Health Information System (DHIS) was charted visually by the research team to reflect the KZN province and Amajuba District's performance on key service indicators along the MH treatment cascade. From this, the multidisciplinary teams developed time‐specific, data‐informed project aims, and identified key service indicators that would be monitored throughout the MhINT project. A staggered intervention roll‐out plan was proposed, beginning in Newcastle subdistrict before scaling up to the additional subdistricts at 6 month‐intervals.
During the diagnostic phase, the researchers led by the District Mental Health Coordinator undertook activities to better understand the process of care within PHC and referral pathways for patients with mental health problems. The team began by emulating the patient's journey in PHC facilities in the chronic care stream using a process mapping tool. The process mapping exercise was used to identify, characterize, and document each step of health care, the service provider at each point, treatment tools used, as well as nonclinical processes associated with each clinical activity. 29 In order to be impactful, process mapping must be conducted in an inclusive, nonconfrontational, and nonblaming manner with the spirit of curiosity about the interaction between the human resources, their tools, and patients. 27 , 29 We conducted the exercise in‐person, rather than a desktop review as even seemingly straightforward patient journeys can be complex in practice. 29
Within the intervention phase, different cadres within the health system were provided training in line with their role and function in the MhINT collaborative care package (see Fig. 1). Training was structured and manualized and provided through a train‐the‐trainer cascade model. Data on components of the MhINT programme, that is, training, MH assessment, referral, and initiation to the psychosocial counseling, were documented by project staff. The multidisciplinary teams at all levels were trained on how to conduct root‐cause analysis and develop change ideas as well as how to use the Plan‐Do‐Study‐Act (PDSA) tool to develop a plan of action for testing each change to address implementation bottlenecks. PDSA cycles consist of iterations in: using data to articulate, which processes need to be improved, understanding process bottlenecks through root‐cause analysis, generating and testing change ideas to address the bottlenecks, studying the outcomes of the tests, and providing data to support changes that would likely result in sustained improvements. 27 , 28 The multidisciplinary CQI teams were provided mentorship on the application of CQI principles and tools by MhINT CQI Advisors and Mentors at agreed upon intervals. Learning sessions, which are platforms for reviewing implementation progress, troubleshoot cross‐cutting challenges, and learn additional CQI techniques 30 were scheduled quarterly to promote learning and fast‐track scale up of effective practices.
FIGURE 1.
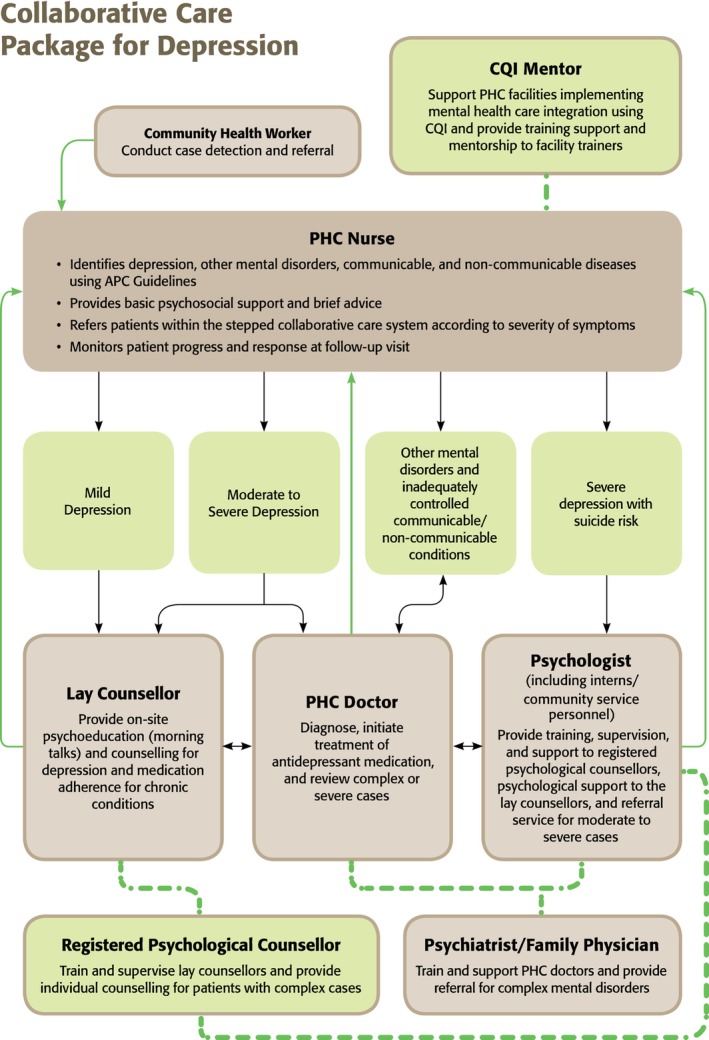
MhINT collaborative care model.
During the impact phase, project data were reviewed against routinely collected DHIS data. The data were interrogated against the project aims and targets set during the project phase.
The sustaining improvement phase entailed formalizing and improving monitoring systems, developing standard operating procedures and guidelines for adopted change ideas, and putting in place mechanisms for promoting improvement over time. 23 , 27
3. RESULTS
3.1. CQI teams and project aims
The multidisciplinary CQI team formed at the provincial level included managers from the noncommunicable disease (NCD) and communicable disease programmes (HIV and AIDS/STI/TB) programmes. This team invited representatives from other DoH units (i.e., PHC directorate, Monitoring and Evaluation) when it was needed. Within the provincial MH directorate, one of the managers assumed the role of being the principal liaison person between the MhINT researchers, National DoH MH directorate, senior provincial management, and district management, and this allowed prompt circulation of project data that had policy implications. The district‐level CQI team was led by the district Director and provided an endorsement of the MhINT programme and implementation of MhINT activities in PHC facilities. The subdistrict and district teams were led by PHC supervisors and PHC operational managers, respectively. Selective members from each team were paired with a MhINT researcher in leading key components of the intervention. It was anticipated that the pairing or twinning of DoH cadre and researcher strategy would enable skill transfer and facilitate institutionalization of the MhINT package beyond the programme's funding cycle.
At provincial‐level MH service, indicators were reviewed alongside dashboard indicators for the HIV and AIDS/STI/TB (HAST) clinical programme to facilitate integrated planning and monitoring of health services from the onset. The gaps in the MH indicator dataset were immediately visible when compared to the robust set of data elements for monitoring the TB/HIV programme, that is, only three MH service delivery indicators were collected and reported at the PHC level (#patients screened, # patients treated, and total MH caseload).
The limited MH dataset was viewed as limited and not conducive to the effective management of the MH programme. Findings from the process mapping exercise revealed the lack of standardization in the MH screening process. MH screening and MH assessment were generally merged and provided only to known mental healthcare users during their routine follow‐up visits with either a clinical nurse practitioner (CNP) referred to as the “Mental Health Champion” or the PHC‐based doctor. This practice deviated from how health services for other chronic diseases were provided, that is, screening provided at a central point (vitals station) by an enrolled nurse (EN) to the whole PHC headcount before patients could undergo assessment and further intervention by a CNP or PHC‐based doctor. Some facilities did not have a standard MH screening tool whilst some had a tool but described it as complex and cumbersome. Where symptoms of a mental disorder were detected, patients were referred to a district hospital regardless of symptom severity. Whilst the “Mental Health Champions” reported providing some counselling to known mental healthcare users; however, they indicated that they did not capture the service in their records as they held the view that MH treatment at PHC entailed only medical interventions. It was reasoned that the conflation of MH screening and assessment as well as the lack of clarity on the definition of “MH treatment” at PHC contributed to data capturing irregularities.
At the initial roll‐out of the MhINT project (September 2017), the provincial MH screening rate was 35%; Amajuba district was at 49%; and the Newcastle subdistrict rate was at 54% The screening rate in one of the targeted facilities in Newcastle subdistrict was well above 100% thus confirming data irregularities. On average, PHC facilities in Amajuba District were treating 14 new MH patients per month. Service data reviewed at baseline were accepted as tentative and not an accurate reflection of MH services provided in the district.
An implementation strategy prioritizing strengthening of the MH screening process first was adopted, anticipating that improvements in screening would affect improvement in the rest of the MH treatment cascade. The provincial team settled on maintaining the MH screening rate of 35% in line with targets set in the ideal clinic realization manual. 22 At the district level, an aim to improve the MH screening rate from 49% to 90% over a period of 12 months was set. This target was in line with the UNAIDS 90‐90‐90 strategy 31 used to monitor the HIV clinical programme performance. The MhINT project would focus on achieving the first 90, that is, providing MH screening services to 90% of the adult PHC headcount.
3.2. Capacity building
All training packages provided an orientation to the MhINT collaborative care package for depression, the referral pathways within the PHC as well as upward referral for specialized care in hospital. A facility‐based APC trainer from each intervention clinic was capacitated to cascade the enhanced mental health APC training. PHC‐based doctors were oriented to the APC guidelines and received a refresher training on the medical management of mental illness at PHC by a psychiatrist who was part of the District Mental Health Specialist team.
Permission from provincial and district management was provided to recruit and train lay counsellors from a pool of HIV counsellors who had at least 10 years' experience, had an interest in mental health, and were not committed to any other skill development programme offered by the DoH. It was proposed that their role would be diversified, and the psychosocial counselling sessions would be counted in their daily counselling targets for the HAST programme. Each intervention clinic had one trained lay counsellor except one high‐volume clinic, which had two. Lay counsellors received supervision from a MhINT‐registered psychological counsellor (individually once a week and in a group once a month).
In vivo supervision using a fidelity scale was utilized in the one‐on‐one support and group supervision focused on providing emotional support, collecting treatment data, and identifying successes and bottlenecks related to providing the psychosocial intervention.
3.3. Change ideas to improve MH screening services
In order to improve mental health screening services, a change idea to introduce a simpler mental health screening tool with clear instructions for administration and scoring was proposed. A seven‐item Brief Mental Health (BMH) tool comprising internationally validated measures namely the Alcohol Use Disorders Identification Test (AUD‐C), Patient Health Questionnaire (PHQ‐2), and Generalized Anxiety Disorder (GAD‐2) was translated into the local language and validated. 32 An important finding from the validation study was that the BMH was not only effective in identifying individuals with symptoms of the screened CMDs but also identified a majority of those who did not have symptoms thus reducing the potential for overburdening nurses with false positives. 32 A PDSA Cycle to introduce the validated BHM tool as part of routine care entailed testing the use of the tool in 13 intervention clinics in Newcastle subdistrict. Each facility was provided 10 copies of the BMH tool to administer to patients over 5 days. Teams met to reflect on their own and patient's experience of the tool; its utility and feasibility of it being integrated within screening services conducted in the vital signs station. Concerns about administration time were raised as some patients began describing their emotional distress to ENAs who reported being ill‐equipped to intervene. Additional concerns were raised about the lack of privacy in vitals' stations, which typically accommodated two patients at a time for routine screening services.
Some clinicians indicated the tool triggered their own emotional distress and admitted to also needing psychological support.
However, the overall feedback on the tool was mostly positive with clinicians describing it as short and user‐friendly. Feedback from patients was also positive and some facilities observed patients sharing their experience with other healthcare users who subsequently asked to receive the MH screening service. Continued use of the BHM as part of routine care was therefore adopted. To improve monitoring of the MH screening service, HIV and NCD Clinical programme managers authorized weekly review of MH screening data during nerve centre meetings. Nerve centre meetings were formed to operationalize the country's integrated chronic disease model and curb the HIV epidemic. 21 They are typically attended by PHC supervisors, PHC operational managers, and Facility Information officers to closely monitor the performance of HIV, TB, and noncommunicable diseases at district and subdistrict level to identify facilities that perform well, share best practice, identify facilities that require support, and develop corrective actions. 21 It was anticipated that including MH indicators in nerve centre meetings would facilitate integrated care and integrated approach to monitoring and improving clinical services at PHC. CQI workshops targeting nonclinical staff (data capturers, facility information officers, and district information officers) provided clarification on the definitions of MH data indicators (i.e., MH treatment includes psychosocial counselling as well).
3.4. Change ideas to improve MH Assessment and referrals to lay counsellors
Bottlenecks in the cascading of the APC training resulted in limited capacitation of all CNPs leaving the responsibility of conducting MH assessments solely to the APC trainers who were in most instances the “Mental Health Champion” in their facilities. The “champion” model was viewed as a barrier to integrated care it and was noted that referrals to the psychosocial service declined when the Mental Health Champion was not on duty.
To address this bottleneck, MhINT APC trainers supported the District Training coordinators to expedite capacitation in mental health assessment by providing training to CNPs directly as opposed to waiting for facility‐based APC trainers to cascade the training.
A pattern was noted whereby CNPs referred patients for adherence counselling more readily than for depression counselling despite the MH screening and/or assessment outcome. Unlike the psychosocial counselling intervention, medication adherence support was already part of the scope of practice of HIV counsellors prior to the MhINT programme. The low depression counselling referrals appeared to be indicative of a lack of trust in lay counsellors' capacity to provide a service perceived as being clinical and reserved for mental health specialists. Some of the change ideas introduced to engender trust included orienting CNPs to the content and structure of the depression counselling sessions and inviting patients who had received the intervention to provide feedback on their experiences. Other challenges to the uptake of the counselling intervention included competing responsibilities for lay counsellors linked to the HAST programme, poor access to telephones to reschedule appointments, as well as lack of tools for identifying and tracing MH care users lost to care in communities.
3.5. Cross‐cutting implementation bottlenecks and system‐wide improvement ideas
Learning sessions provided a platform for comprehensive interrogation of cross‐cutting implementation bottlenecks and collaborative problem‐solving between members of the CQI teams and facility‐based implementers. Data obtained from the DHIS were presented as pareto charts and run charts alongside MhINT project data and substantiated with narrative reports from each facility. Root‐cause analyses of cross‐cutting bottlenecks were undertaken, and improvement change ideas were generated (see Table 1).
TABLE 1.
Examples of some cross‐cutting implementation bottlenecks and change ideas.
| Theme | Bottlenecks | Impact of bottleneck | Change ideas proposed at 6 mo of intervention | Status/outcome of change idea at end of project |
|---|---|---|---|---|
| MH service data management | Patient files not having space for recording MH screening service and outcomes | Duplication of service when patient is seen by a CNP and double capturing in tick registered | ENA to note positive MH screening outcome in the “management” section of the patient file and attach BMH as source document | Adopted. Recording procedure added in a MH screening SOP developed by the provincial team |
| DoH only permits clinicians registered with a recognized professional body to write in patient files | Lay counsellors unable to document services rendered resulting in discrepancy between data on DHIS and project data | Permission granted for MhINT trained counsellors to confirm document date and session completed in patient file | Abandoned. Monthly counselling statistics were submitted to the district information officer to reconcile DHIS data and project data. Lay counsellor records kept as source documents | |
| Lack of clarity about MH indicator definitions and data flow of MH services rendered at PHC | Facility‐based data capturers omitting MH data from weekly summaries |
CQI workshop provided to targeting non‐clinical staff to clarify MH data indicator definitions (ie, psychosocial counselling is also defined as MH treatment at PHC) MhINT CQI data mentor deployed to coach data capturers on verifying provision of MH services rendered using appropriate source documents Proposal to expand the MH dataset to better reflect the steps in the MH treatment cascade |
Mentorship on data management continued to be provided by PHC supervisors during subdistrict nerve centre meetings MH presumptive indicator added as a key dashboard indicator for the MH programme in the provincial indicator dataset (PIDS). |
|
| Provision of MH services and tracing patients lost to follow‐up |
Psycho‐education morning talks not provided routinely and lay counsellors unable to initiate referred patients to the psychosocial intervention timeously due to having other responsibilities linked to the HAST programme
|
Patients uninformed about MH services provided within the PHC Long waiting times for referred patients, at times resulting in patients not taking up the counselling service Patients not returning for follow‐up appointments with lay counsellors |
Training more than one lay counsellor per facility Patients with missed appointments added to the list of defaulters to be traced by PHC outreach tracer teams |
Adopted. Some facilities excused MhINT trained lay counsellors from their other responsibilities so that they only attended to patients referred for depression and adherence counselling A process of upskilling HIV counsellors and career pathing them to become Social Auxiliary workers was initiated in the province when the MhINT program ended. Content from the MhINT psychosocial counselling training package was submitted to be part of the curriculum for social auxiliary workers in order to institutionalize the psychosocial intervention |
| Mental health of healthcare workers | The intensive focus on MH services increased HCW awareness of their own poor mental health | Decreased motivation in participating in MhINT activities | District team requested the MhINT researchers to develop an intervention to strengthen the employee assistance programme to address the MH needs of healthcare workers | Tentative. Initial engagements between MhINT researchers and EAP practitioners were undertaken. Additional funding required to develop an intervention for healthcare workers providing MH services at PHC |
3.6. Project impact and strategies to sustain improvements
Context‐appropriate modifications were made when the intervention was scaled up to the more rural subdistricts Dannhauser and Emadlangeni. These included providing MH psycho‐education talks and MH screening services as part of the outreach service through mobile clinics. Additionally, the two subdistricts opted to have ENs trained to provide the psychosocial counselling instead of HIV counsellors in order to circumvent the bottleneck of HIV counsellors not being able to capture MH services rendered in patient files (see Table 1). To sustain the improvements to the MH screening process, the provincial MH and substance abuse directorate officially adopted the BMH as the MH screening tool for use at PHC and developed standard operating procedures (SOP) for its use. A policy brief 33 detailing the validation of the BMH tool and its utility was shared with the MH and Substance Abuse Directorate at national level with recommendations for its use in PHC facilities across the country. A data indicator to capture the screening outcome (MH presumptive) was submitted for inclusion in the provincial indicator dataset for MH services to facilitate a more meaningful analysis of MH treatment data.
At the end of the 24‐month MhINT programme implementation period, improvements in performance were noted across the three MH service indicators. At the provincial level, the MH screening rate increased from 35% to 45%. Whilst the district did not meet the 90% target set in their aim statement, their performance, an improvement in the MH screening rate from 49% to 56%, remained substantially higher than the minimum prescribed Ideal Clinic screening target of 35%. 22 At subdistrict level (Newcastle), the MH screening rate improved from 54% to 56%. Screening rates in the intervention clinics improved by between 5% and 20%, but 2 clinics experienced a decline (see Table 2).
TABLE 2.
Mental disorder screening rate—Newcastle Subdistrict.
| Clinic | Quarter 4 (2016/2017) | Quarter 2 (2018/2019) | Improvement (%) |
|---|---|---|---|
| Clinic 1 | 143% | 96% | ‐ (47%) |
| Clinic 2 | 90% | 95% | 5% |
| Clinic 3 | 88% | 83% | ‐ (5%) |
| Clinic 4 | 75% | 95% | 20% |
| Clinic 5 | 63% | 68% | 5% |
| Clinic 6 | 49% | 68% | 19% |
| Clinic 7 | 46% | 54% | 8% |
| Clinic 8 | 34% | 22% | ‐ (12%) |
| Clinic 9 | 32% | 40% | 8% |
| Clinic 10 | 28% | 44% | 16% |
| Clinic 11 | 26% | 48% | 22% |
| Clinic 12 | 19% | 38% | 19% |
| Clinic 13 | 5% | 18% | 13% |
Note: Data accessed with permission from KZN DoH from the District Health Information System in October 2019.
Reduction in data irregularities suggested improved data management processes. Project data revealed that 4469 referrals were received for counselling services across the 31 facilities in the district. Of these, 2080 were for depression counselling and that translated to an average of 87 new MH patients per month in comparison to the 14 new MH patients at baseline. This translates to an improvement of about 16%. The DHIS system, however, only reflected a monthly average of 39 new MH cases at the MhINT programme end‐line, highlighting the need to further strengthen capturing of MH services data. More than 80% of the 2389 patients that were referred for chronic medication adherence counselling were on the HIV Anti Retro Viral Treatment programme.
4. DISCUSSION
Historically, strategies to facilitate the uptake of task‐sharing mental health interventions by healthcare workers have focused on governance, capacity building, and providing clear service guidelines to Reference 34. Whilst these are important, the MhINT programme demonstrated that a collaborative alliance between researchers and DoH stakeholders is as, if not more, an impactful strategy for advancing efforts for embedding evidence‐based health innovations.
The MhINT program demonstrated that the alliance between researchers and health system stakeholders requires nurturing, monitoring, and continuous (re) alignment of the interests of all involved stakeholders 35 if the implementation is to succeed. As researchers, we had to balance being flexible and responsive to the implementation environment, maintaining diplomacy whilst also insisting on fidelity of the intervention. 13 This seemed to affect mutual respect and trust in the scientific methods used in implementation.
The collaborative and trusting relationship between the researchers and the DoH implementers also seemed to absorb threats to the success of the intervention such as staff turnover and retirements. The functionality of the collaborative learning networks/ teams, having supportive leadership, funding, as well as the programme alignment with the broader policy environment 36 were key contributing factors to the gains achieved by the MhINT programme.
At the policy level, the MhINT care package was aligned with the strategic imperatives of the DoH and operationalized aspirations of the MHPF 2013‐2020 for integrated mental health care. MhINT was also aligned with the country's PHC Re‐engineering strategy emphasizing increasing access to comprehensive health services and improving the quality of care on the PHC platform. 37 As such, the MhINT programme emphasized the importance of having ideological support at all levels of governance as this enables multidisciplinary engagements, which are necessary for affecting sustainable health systems transformations. 38 , 39
Using CQI as an implementation vehicle also provided some important insights. Whilst CQI strategies have been widely used to transform health systems and facilitate collaborative learning and adoption of evidence‐based practice 40 there were limited examples of its use in improving both planning and provision of mental healthcare services in the SA context. CQI fosters a continuous learning culture that forefronts collaboration and adaptability through feedback loops, which is a central tenet of a learning health system. 25 It can provide a structured approach and its data‐focused stance was able to highlight that improvement of data management systems for mental health services is also critical to the project of achieving integrated mental health care.
Application of CQI methods, however, can be messy, iterative, and uncertain and can provoke tensions, anxiety, and conflict before the desired transformation is achieved. 39 In already strained health systems like in SA, the often‐mixed results from attempted PDSAs can contribute to healthcare worker disengagement, particularly where the benefits of health innovations are not instantly evident. 13 , 38 For MH services this threat is probably more significant given that the effect of psychological interventions is not always instant and healthcare workers hold a perception that mental health care is an “add‐on” to the “legitimate” workload, particularly at PHC where the impact of staff shortages is acutely felt. 41 Systematic barriers such as the absence of psychological tools for providing MH care at PHC and unclear monitoring and evaluation guidelines for MH services rendered can serve to reinforce the perception of “illegitimacy” of MH care. These barriers are also reflective of disconnection between policy and practice, which contributes to confusion at the service level.
As part of the MhINT programme, CQI techniques were intentionally used to raise awareness of this disconnect and thus enabled healthcare workers to assume the role of the active facilitator of change 42 and develop innovative ideas to tailor the MhINT intervention to their context. The MhINT programme thus highlighted that whilst mentorship is an important strategy for embedding new innovations in the health system; it must be a type of mentorship that is containing, is responsive to healthcare worker anxieties, and is system‐focused rather than clinical skills‐focused. 43 This type of mentorship has been referred to as supportive supervision, and it demands a specialized skillset that would need to be groomed in leaders within the South African health system 37 as it can strengthen relationships within the system, reinforce evidence‐based problem‐solving and maximize resource allocation. 44
Lastly, staff in intervention clinics repeatedly reported that providing mental health services was strenuous and triggered emotional responses not otherwise experienced when treating other chronic conditions. This accentuated the need for focusing on health workers' own emotional health and well‐being as a strategy for facilitating the uptake of task‐sharing mental health interventions. The emotional strain associated with mental health services may be implicit in the often reported “reluctance” of healthcare workers to provide mental health care at PHC. 45 As such implementers of health systems strengthening interventions should be sensitive to the inevitability of mental health services triggering emotional symptoms in healthcare workers and the impact this may have on their willingness to provide such services if they are not cared for.
5. LIMITATIONS
The MhINT programme was implemented over a short implementation period in one of the smallest districts in KZN, which is relatively well‐resourced. Expanding the intervention to larger, more rural contexts with fewer resources over a longer period would undoubtedly allow for more learning and allow for a more comprehensive analysis of the impact of the intervention over time.
6. CONCLUSIONS
This paper described the implementation of an evidence‐based care package for depression to achieve integrated mental health services at PHC. CQI strategies were employed to identify system barriers to the uptake of the innovation and address them utilizing PDSA cycles to facilitate the uptake of the innovation.
Integrated planning and monitoring of the MH programme with the HIV and NCD Programmes shone a spotlight on the need to expand MH indicators in order to improve the monitoring of the MH services. The introduction of a validated MH screening tool into the treatment pathway enabled the health system to clarify guidelines on MH screening and contributed to an improvement in the MH screening rate by 7% at the district level and 10% at the provincial level. Access to mental health services at PHC increased by 16% without adding additional human resources to the health system. The programme, however, revealed that not addressing the mental health of healthcare workers could jeopardize the sustenance of the gains that were achieved. 46 Interventions to care for the caregiver are therefore critical to the integrated mental healthcare agenda along containing, system‐focused and data‐driven mentorship and support. 47 The MhINT programme appears to have the prospects of effecting change and provides an accessible model aligned with policy ideals.
AUTHOR CONTRIBUTIONS
Inge Petersen and Deepa Rao were principal investigators on the study and Arvin Bhana was co‐investigator. The paper was drafted by Sithabisile Gugulethu Gigaba, and all authors commented and provided input. Zamasomi Luvuno, Inge Petersen, and Andre Janse van Rensburg contributed to the methodology. Arvin Bhana and Londiwe Mthethwa contributed to interpretation and writing up of results. Nikiwe Hongo helped conceptualize and participated in the study as a Department of Health representative. [Correction added on 25 October 2023, after first online publication: The preceeding sentence was added.] Inge Petersen was the mentoring author. All authors read and approved the final manuscript.
FUNDING INFORMATION
The Mental Health Integration Programme (MhINT) and corresponding materials were funded by the Cooperative Agreement 1U2GGH001197 from the United States Centers for Disease Control and Prevention (CDC) in support of the President's Emergency Plan for AIDS Relief (PEPFAR). The views expressed in this article do not necessarily represent the views of CDC or the US Government.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ACKNOWLEDGMENTS
The authors hereby express gratitude to collaborators from University of KwaZulu‐Natal Centre for Rural Health, the Department of Global Health of the University of Washington, International Training and Education Center for Health South Africa, University of Cape Town's Knowledge Translation Unit, the Alan J Flisher Centre for Public Mental Health of the University of Cape Town, and the Department of Health in South Africa.
Gigaba SG, Luvuno Z, Bhana A, et al. Collaborative implementation of an evidence‐based package of integrated primary mental healthcare using quality improvement within a learning health systems approach: Lessons from the Mental health INTegration programme in South Africa. Learn Health Sys. 2024;8(2):e10389. doi: 10.1002/lrh2.10389
[Correction added on 25 October 2023, after first online publication: Nikiwe Hongo was added to the author list.]
Footnotes
NHI pilot sites have been identified by the SA Health systems to test some aspects of district health systems and determine how reforms under the NHI could be implemented. Piloting interventions prioritise reforms and interventions that promote greater equity, efficiency, effectiveness and participation (Section 27 Policy Brief, 2013).
REFERENCES
- 1. Docrat S, Besada D, Cleary S, Daviaud E, Lund C. Mental health system costs, resources and constraints in South Africa: a national survey. Health Policy Plan. 2019;34(9):706‐719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Votruba N, Eaton J, Prince M, Thornicroft G. The importance of global mental health for the Sustainable Development Goals. J Ment Health. 2014;23(6):283‐286. [DOI] [PubMed] [Google Scholar]
- 3. Semrau M, Evans‐Lacko S, Koschorke M, Ashenafi L, Thornicroft G. Stigma and discrimination related to mental illness in low‐ and middle‐income countries. Epidemiol Psychiatr Sci. 2015;24(5):382‐394. doi: 10.1017/S2045796015000359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Patterson JE, Edwards TM, Vakili S. Global mental health: a call for increased awareness and action for family therapists. Fam Process. 2018;57(1):70‐82. doi: 10.1111/famp.12281 [DOI] [PubMed] [Google Scholar]
- 5. Patel V, Saxena S, Lund C, et al. The Lancet Commission on global mental health and sustainable development. Lancet (London, England). 2018;392(10157):1553‐1598. doi: 10.1016/S0140-6736(18)31612-X [DOI] [PubMed] [Google Scholar]
- 6. Schneider M, Baron E, Breuer E, et al. Integrating mental health into South Africa's health system: current status and way forward. S Afr Health Rev. 2016;2016(1):153‐163. [Google Scholar]
- 7. Kohrt BA, Mendenhall E, eds. Global Mental Health: Anthropological Perspectives. New York, NY: Routledge (Taylor & Francis); 2016. [Google Scholar]
- 8. Rehm J, Shield KD. Global burden of disease and the impact of mental and addictive disorders. Curr Psychiatry Rep. 2019;21:10. doi: 10.1007/s11920-019-0997-0 [DOI] [PubMed] [Google Scholar]
- 9. Petersen I, Lund C. Mental health service delivery in South Africa from 2000 to 2010: one step forward, one step back. S Afr Med J. 2011;101(10):751‐757. [PubMed] [Google Scholar]
- 10. Galvin M, Byansi W. A systematic review of task shifting for mental health in sub‐Saharan Africa. Int J Mental Health. 2020;49(4):336‐360. [Google Scholar]
- 11. Spedding MF, Stein DJ, Sorsdahl K. Task‐shifting psychosocial interventions in public mental health: a review of the evidence in the South African context. S Afr Health Rev. 2014;2014(1):73‐87. [Google Scholar]
- 12. Deane FP, Crowe TP, King R, Kavanagh DJ, Oades LG. Challenges in implementing evidence‐based practice into mental health services. Aust Health Rev. 2006;30(3):305‐309. [DOI] [PubMed] [Google Scholar]
- 13. Murray LK, Tol W, Jordans M, et al. Dissemination and implementation of evidence based, mental health interventions in post conflict, low resource settings. Intervention (Amstelveen, Netherlands). 2014;12(Suppl 1):94‐112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wakida EK, Talib ZM, Akena D, et al. Barriers and facilitators to the integration of mental health services into primary health care: a systematic review. Syst Rev. 2018;7(1):1‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Petersen I, van Rensburg AJ, Kigozi F, et al. Scaling up integrated primary mental health in six low‐and middle‐income countries: obstacles, synergies and implications for systems reform. BJPSych Open. 2019;5:e69. doi: 10.1192/bjo.2019.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Votruba N, Grant J, Thornicroft G. The EVITA framework for evidence‐based mental health policy agenda setting in low‐ and middle‐income countries. Health Policy Plan. 2020;35(4):424‐439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Semrau M, Evans‐Lacko S, Alem A, et al. Strengthening mental health systems in low‐ and middle‐income countries: the Emerald programme. BMC Med. 2015;13:79. doi: 10.1186/s12916-015-0309-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Petersen I, Selohilwe O, Georgeu‐Pepper D, et al. A collaborative care package for depression comorbid with chronic physical conditions in South Africa. BMC Health Serv Res. 2022;22(1):1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Petersen I, Fairall L, Zani B, et al. Effectiveness of a task‐sharing collaborative care model for identification and management of depressive symptoms in clients with hypertension attending public sector primary care clinics in South Africa: pragmatic parallel cluster randomised controlled trial. J Affect Disord. 2021;282:112‐121. [DOI] [PubMed] [Google Scholar]
- 20. Petersen I, Bhana A, Fairall L, et al. Evaluation of a collaborative care model for integrated primary care of common mental disorders comorbid with chronic conditions in South Africa. BMC Psychiatry. 2019;19:1‐11. doi: 10.1186/s12888-019-2081-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mahomed OH, Asmall S, Freeman M. An integrated chronic disease management model: a diagonal approach to health system strengthening in South Africa. J Health Care Poor Underserved. 2014;25(4):1723‐1729. [DOI] [PubMed] [Google Scholar]
- 22. South African National Department of Health . Ideal Clinic South Africa: Ideal Clinic version 16. https://www.kznhealth.gov.za/family/Ideal-Clinic-Manual-Oct2015.pdf [Internet]. Accessed November 2022.
- 23. Silver SA, McQuillan R, Harel Z, et al. How to sustain change and support continuous quality improvement. Clin J Am Soc Nephrol. 2016;11(5):916‐924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Faden RR, Kass NE, Goodman SN, Pronovost P, Tunis S, Beauchamp TL. An ethics framework for a learning health care system: a departure from traditional research ethics and clinical ethics. Hastings Cent Rep. 2013;43(s1):S16‐S27. [DOI] [PubMed] [Google Scholar]
- 25. McGinnis JM, Stuckhardt L, Saunders R, Smith M, eds. Best Care at Lower Cost: the Path to Continuously Learning Health Care in America. Washington DC: National Academies Press; 2013. [PubMed] [Google Scholar]
- 26. Hilton K, Anderson A. IHI Psychology of Change Framework to Advance and Sustain Improvement. Boston, MA: Institute for Healthcare Improvement; 2018. ihi.org [Google Scholar]
- 27. Langley GL, Moen R, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. 2nd ed. San Francisco, CA: Jossey‐Bass Publishers; 2009. [Google Scholar]
- 28. NSW Department of Health . Easy Guide to Clinical Practice Improvement. www.health.nsw.gov.au/quality/pdf/cpi_easyguide.pdf. 2002.
- 29. Trebble TM, Hansi N, Hydes T, Smith MA, Baker M. Process mapping the clients journey: an introduction. BMJ. 2010;341:c4078. doi: 10.1136/bmj.c4078 [DOI] [PubMed] [Google Scholar]
- 30. Gotham HJ, Paris M, Hoge MA. Learning collaboratives: a strategy for quality improvement and implementation in behavioral health. J Behav Health Serv Res. 2022;50:263‐278. doi: 10.1007/s11414-022-09826-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.90–90–90—An ambitious treatment target to help end the AIDS epidemic. UNAIDS [Internet]. http://www.unaids.org/en/resources/documents/2014/90-90-90. Accessed November 2022.
- 32. Bhana A, Mntambo N, Gigaba SG, et al. Validation of a brief mental health screening tool for common mental disorders in primary healthcare. S Afr Med J. 2019;109(4):278‐283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bhana A, Mntambo N, Gigaba SG, et al. Validation of the Brief Mental Health Screening Tool (BMH). Policy Brief 17; August 2018.
- 34. Marais DL, Petersen I. Health system governance to support integrated mental health care in South Africa: challenges and opportunities. Int J Mental Health Syst. 2015;9:1‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Geboers HJ, Grol RP, van den Bosch WJ, et al. A model for continuous quality improvement in small scale practices. Qual Health Care. 1999;8(1):43‐48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Zamboni K, Baker U, Tyagi M, Schellenberg J, Hill Z, Hanson C. How and under what circumstances do quality improvement collaboratives lead to better outcomes? A systematic review. Implement Sci. 2020;15:1‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mckenzie A, Schneider H, Schaay N, Scott V, Sanders D. Primary Health Care in South Africa: Case Study prepared for the PRIMASYS (Primary Care Systems Profile and Performance) initiative of the Alliance for Health Policy and Systems Research and World Health Organization; 2016.
- 38. Travis P, Bennett S, Haines A, et al. Overcoming health‐systems constraints to achieve the Millennium Development Goals. Lancet. 2004;364(9437):900‐906. [DOI] [PubMed] [Google Scholar]
- 39. Gardner KL, Dowden M, Togni S, Bailie R. Understanding uptake of continuous quality improvement in Indigenous primary health care: lessons from a multi‐site case study of the Audit and Best Practice for Chronic Disease project. Implement Sci. 2010;5(1):1‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Rohweder C, Wangen M, Black M, et al. Understanding quality improvement collaboratives through an implementation science lens. Prev Med. 2019;129:105859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Lund C, De Silva M, Plagerson S, et al. Poverty and mental disorders: breaking the cycle in low‐income and middle‐income countries. Lancet. 2011;378(9801):1502‐1514. [DOI] [PubMed] [Google Scholar]
- 42. Harvey G, Lynch E. Enabling continuous quality improvement in practice: the role and contribution of facilitation. Front Public Health. 2017;5:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hill JE, Stephani AM, Sapple P, Clegg AJ. The effectiveness of continuous quality improvement for developing professional practice and improving health care outcomes: a systematic review. Implemen Sci. 2020;15(1):1‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Bailey C, Blake C, Schriver M, Cubaka VK, Thomas T, Hilber AM. A systematic review of supportive supervision as a strategy to improve primary healthcare services in Sub‐Saharan Africa. Int J Gynecol Obstet. 2016;132(1):117‐125. [DOI] [PubMed] [Google Scholar]
- 45. Kemp CG, Mntambo N, Weiner BJ, et al. Pushing the bench: a mixed methods study of barriers to and facilitators of identification and referral into depression care by professional nurses in KwaZulu‐Natal, South Africa. SSM‐Mental Health. 2021;1:100009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Maphumulo WT, Bhengu BR. Challenges of quality improvement in the healthcare of South Africa post‐apartheid: a critical review. Curationis. 2019;42(1):1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Kilbourne AM, Goodrich DE, Miake‐Lye I, Braganza MZ, Bowersox NW. Quality enhancement research initiative implementation roadmap: toward sustainability of evidence‐based practices in a learning health system. Med Care. 2019;57(10 Suppl 3):S286‐S293. [DOI] [PMC free article] [PubMed] [Google Scholar]


