Introduction
Minimally invasive surgical (MIS) procedures are becoming increasingly popular in foot and ankle surgery. Several benefits of MIS procedures have been reported in the literature including decreased postoperative pain, shorter recovery times, and lower need for postoperative narcotics.10,11,33,53,71,72 Specifically regarding Haglund deformity (HD) and insertional Achilles tendinopathy (IAT), MIS techniques have been increasingly used over the last decade.
Traditional open procedures for HD and IAT have relatively good outcomes; however, longer recoveries combined with complications such as wound issues and infections have resulted in the expansion of MIS approaches to treat these pathologies. Although the first generation of MIS techniques involved endoscopic surgery,5,11,13-15,17,18,24,27,33,35,50,53-55,70,73,74 percutaneous approaches are now gaining momentum. The current work reviews these techniques including endoscopic calcaneoplasty (Haglund resection), percutaneous Haglund resection, and percutaneous Zadek (dorsal closing wedge) calcaneal osteotomy.
Background
It has been estimated that 6% of the general population will at some point be affected by Achilles tendon pain, with 33% of cases due to IAT. 9 Although they may be considered and treated as distinct pathologies, IAT and HD intersect in patients with Haglund syndrome (HS). HS is one of the most common causes of retrocalcaneal pain addressed by foot and ankle surgeons and is estimated to affect 25% of patients who present with IAT.48,61,75 HD can mechanically irritate the Achilles tendon, resulting in a retrocalcaneal bursitis and worsened IAT, completing the Haglund Syndrome triad.9,61
Conventional approaches to IAT and HD begin with nonoperative therapy, although failure rates have been reported to be as high as 40%. 42 Patients who have persistent symptoms after 3-6 months of nonoperative treatment are potential candidates for surgical intervention.
Historically, the traditional surgical approach for HD and IAT has been an open Achilles tendon–splitting procedure. The Achilles tendon is split midline or slightly off midline, the tendinopathy and intratendinous calcifications are debrided, any HD (posterosuperior prominence) is resected, and the Achilles tendon is reattached. Although this procedure is considered an effective approach to HD and IAT correction, multiple complications have been described, including impaired wound healing, sural nerve injury, wound tenderness, shoe wear irritation, infection, pain, prolonged recovery time, and skin sensitivity.11,13,18,25,33,50,53,56,59,71 This has led many to adopt minimally invasive approaches to treat HD and IAT. Those in support of MIS approaches cite less pain, better outcomes, quicker return to activity, and increased patient satisfaction.2,10,11,33,37,38,53,71
Presentation
History
Patients with HD and IAT typically present with retrocalcaneal pain including pain at or near the Achilles tendon insertion, often exacerbated by shoes and activity. As the disease progresses, the pain may become more constant and severe, leading to limitations with certain physical activities and activities of daily living.
Patients’ medication history should be reviewed for use of fluroquinolones and/or corticosteroids. Systemic fluoroquinolone and corticosteroid use have been correlated with the development of various Achilles tendinopathies, including IAT.42,58
Physical Examination
On physical examination, a palpable posterosuperior calcaneal prominence may be noted in patients with HD.48,68 Point tenderness and swelling may be found medial and/or lateral to the Achilles insertion, as well as directly over the Achilles insertion. Similarly, an insertional prominence is typically, although not always, noted in patients with IAT. With IAT, tenderness is more centrally localized. Specificity regarding location of tenderness is important in distinguishing between IAT and noninsertional Achilles tendinopathies. 48 The surgeon should ensure that the patient does not have pain over the Achilles midsubstance, as MIS Achilles insertional techniques will not adequately address midsubstance disease. Additional findings on physical examination relevant to IAT may include reduced dorsiflexion, tenderness over the retrocalcaneal bursa, gastrocnemius contracture, and/or diminished plantarflexion strength.
Imaging and Other Testing
Initial imaging studies should consist of weightbearing radiographs of the ankle including anteroposterior, mortise, and lateral views. A hindfoot alignment view may also be considered. Radiographs allow for assessment of the patient’s alignment as well as the presence of a bony prominence on the posterosuperior calcaneus and calcifications within the Achilles tendon.48,68
Magnetic resonance imaging may be used for assessment of the regional soft tissues including the Achilles tendon and retrocalcaneal region. This typically demonstrates retrocalcaneal bursitis, thickening of the Achilles tendon at its insertion, and increased edema within the tendon and calcaneal insertion.1,68
Pertinent laboratory evaluation may include an autoimmune panel, especially for younger adults, to rule out alternative pathologies such as inflammatory disorders (rheumatoid arthritis, ankylosing spondylitis, reactive arthritis, etc). These disorders may present with similar symptoms, often bilaterally or associated with other sites of joint pain.16,32,68
Treatment
Nonoperative Treatment
The initial treatment of HD and IAT begins with anti-inflammatory medications, activity limitation, physical therapy, and shoe-wear modification.8,48,61,68 Heel lifts may reduce tension on the Achilles, though evidence to support their use is mixed. 7 Pulsed ultrasound therapy has demonstrated some success in this patient population. 57 Night splints and physical therapy with eccentric Achilles strengthening exercises are also effective.8,48,61,68 Recently, there has been some success with extracorporeal shockwave therapy (ESWT) in patients with IAT; however, this has been less successful in treating patients with concomitant HD. 73 In 20% to 40% of patients, these conservative approaches will fail to provide relief and surgical treatment may be indicated. 42
Operative Treatment
When at least 3-6 months of conservative treatment strategies for HD and IAT have failed to provide adequate pain relief, surgical intervention should be considered.12,47,49,53
Clinically, HD and IAT can present similarly; however, it is very important to specify between these pathologies when deciding on specific surgical treatment. Haglund syndrome is considered a spectrum of disease. Accordingly, treatment must be tailored to individual patient pathology. Patients who present with a simple HD, without IAT, should be considered separate from those who present with IAT. It is critical to make this distinction as it will guide treatment.
For patients who present with a HD and no IAT, a percutaneous Haglund resection, typically referred to as an endoscopic calcaneoplasty (ECP), may be suitable. For patients with HD and mild IAT, a Zadek osteotomy or ECP with limited Achilles debridement and reattachment may be considered.14,47 In the setting of more advanced IAT (with or without HD), a percutaneous Zadek osteotomy can offer significant improvement in pain and function, with a low complication rate.10,29,49 In these patients, open debridement is also a reasonable option. Finally, when patients present with attritional Achilles lengthening or extensive Achilles degeneration (>50%), an open reconstruction with or without a flexor hallucis longus (FHL) tendon transfer may be warranted.14,36,53
Of note, a gastrocnemius recession should be considered in the setting of a gastrocnemius contracture. 63 However, this should not be performed when performing a Zadek osteotomy, as the osteotomy itself functionally lengthens the triceps surae.
The recent literature has demonstrated consistent evidence that minimally invasive procedures can produce similar results to open procedures.6,27,33,49,50,59,71 Interventions reported in the literature can be broadly classified as endoscopic, minimally invasive, and/or percutaneous. Despite the advantages of minimally invasive foot and ankle surgeries, these procedures may entail increased technical difficulty and an associated learning curve.26,51 Despite this, numerous authors further report that learning curves with MIS procedures are often overcome after a relatively small number of cases.3,23,26,28,51,65
Endoscopic calcaneoplasty (Haglund resection)
Endoscopic calcaneoplasty was first described by van Dijk et al 69 for the correction of isolated HD. The authors argued that this method was superior to open surgery because of reduced pain and morbidity, earlier rehabilitation, and the ability to perform the procedure in an outpatient setting. ECP resection uses smaller incisions and an endoscope for visualization. 55 Surgeons who are accustomed to the arthroscope may easily transition from open techniques to ECP, which offers enhanced visibility. 69 A learning curve has been associated with endoscopic approaches, but it is typically overcome after approximately 10 cases.14,27,53,59,75
Historically, an endoscopic approach has been limited to patients presenting with HD alone, in the absence of IAT.14,59 Recently, studies have demonstrated that endoscopic debridement of the Achilles and suture anchor repair is possible, allowing some surgeons to address IAT as well. 47 ECP has also been recommended for patients at risk for wound healing complications, or patients who need to return to full activity or sport in a short time frame. 69 This includes patients with HD and/or IAT.47,53 Contraindication to endoscopic repair includes substantial calcific metaplasia at the Achilles insertion, significant degeneration (>50%) of the Achilles, or attritional Achilles lengthening.31,47,53,77 In these cases, an open debridement is preferred.
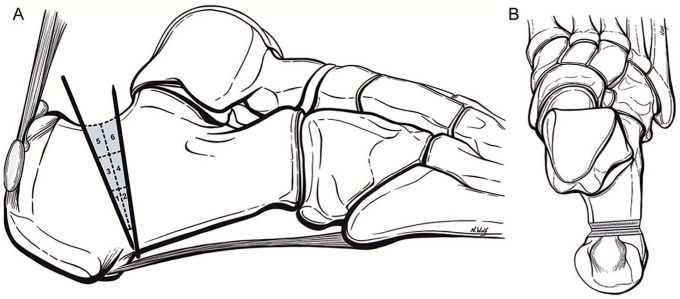
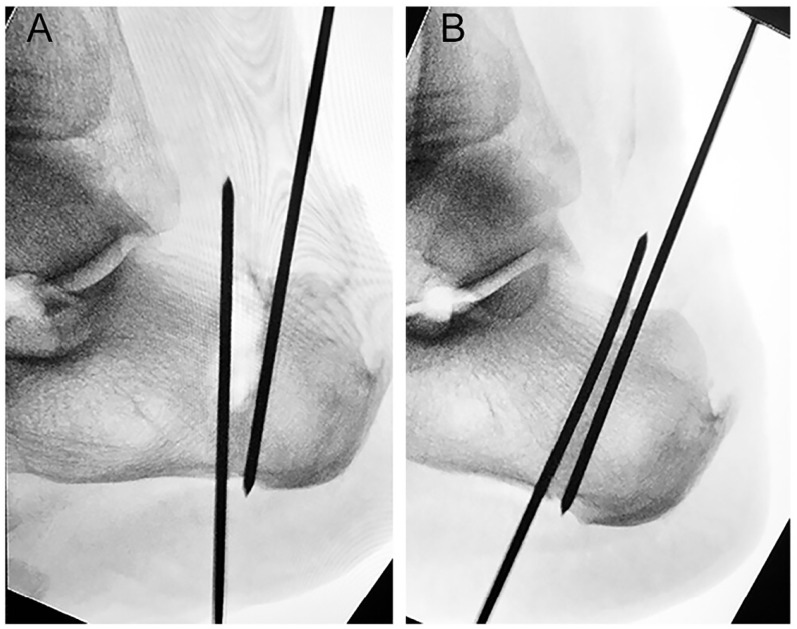
As described by van Dijk et al, ECP uses 2 portals, lateral and medial to the Achilles, at the level of the posterosuperior aspect of the calcaneus (Figure 1).44,69 The Achilles bony insertion is visualized through the endoscope and then the offending bone is removed with an arthroscopic burr (Figures 2 and 3).45,50,70 Scholten and van Dijk stress the importance of adequate bone removal and warn of suboptimal results if this is not achieved. 59 Miller et al 47 described an endoscopic resection of HD paired with a percutaneous double-row Achilles repair to address any comorbid IAT. This technique uses 4 endoscope portals (2 endoscopic working planes) to first remove the posterosuperior prominence and then perform a double-row suture repair of the Achilles on the calcaneus percutaneously. 47 For patients with HD and IAT, Ehredt et al recommend endoscopic gastrocnemius recession (GR), followed by endoscopic posterosuperior prominence resection. ECP described by Ehredt et al is similar to that by van Dijk et al but adds the use of Kirschner wire (K-wire) guidance so that the surgeon can have direct endoscopic visualization of the osseous resection level during the procedure. 14
Figure 1.
Dual portal system used in endoscopic Haglund resection, demonstrated by Michalski et al. 44
Figure 2.
Endoscopic visualization of Haglund resection, A. during shaving and B. after removal of the bony prominence as demonstrated by Ortmann and McBryde. 50
Figure 3.
(A) Preoperative and (B) postoperative measurements following endoscopic Haglund resection by Vega et al. 70
A recent review by Yuen et al 75 demonstrated a reduction in postoperative complications from 12.3% to 5.3% using an endoscopic approach to HD compared with open approaches. The authors found endoscopic techniques to have shorter surgical times, fewer complications, and better outcomes in comparison to open approaches to HS. 75 ECP has previously demonstrated a 204% increase in Achilles pullout strength in comparison to open midline splitting calcaneoplasty in a cadaveric study by Michalski et al. 44 Separately, in a similar analysis, pullout strength was positively correlated with bone mineral density. 52 Therefore, endoscopic Haglund resection may lead to improved postoperative tendon strength in specific patient populations.
In a study by Scholten and van Dijk, 30 of 34 patients who underwent ECP demonstrated excellent outcomes as assessed by Ogilvie-Harris score. 59 At a mean 4.5-year follow-up, ECP demonstrated no complications other than 1 minor case of hypoesthesia over the heel pad. The authors reported an average recovery time of 8 weeks with an 11-week average for return to sports. 59 In another series of 75 cases, ECP as recently described by Miller et al46,47 demonstrated a full return to weightbearing at 10 days postoperatively with no wound complications reported. These findings are consistent with other investigations, all citing improved function and pain, with minimal complications following ECP management of HD and/or IAT.11,13,24,33,35,53,55
Of note, patients who present with substantial calcific metaplasia at the Achilles insertion are not candidates for ECP. However, ECP is possible for patients with HD who present with lesser degrees of mild Achilles calcification.46,47 With mild IAT, the surgeon may consider ECP with concomitant debridement of the Achilles tendon and percutaneous double-row Achilles repair. Double-row reattachment of the Achilles tendon includes overlapping suture anchors to secure the Achilles tendon to the calcaneus, allowing for faster postoperative weightbearing and healing.46,47
Percutaneous (MIS) Haglund Resection
The percutaneous Haglund resection entails isolated removal of the HD using a Shannon burr inserted through a small stab incision. 19 However, this procedure is contraindicated in patients with additional intratendinous Achilles pathology and moderate to advanced IAT. In these cases, an open procedure or percutaneous Zadek osteotomy is preferred. The percutaneous Haglund resection includes the direct removal of the posterosuperior prominence without the benefit of endoscopic visualization. As such, care must be taken to avoid injury to the Achilles insertion.
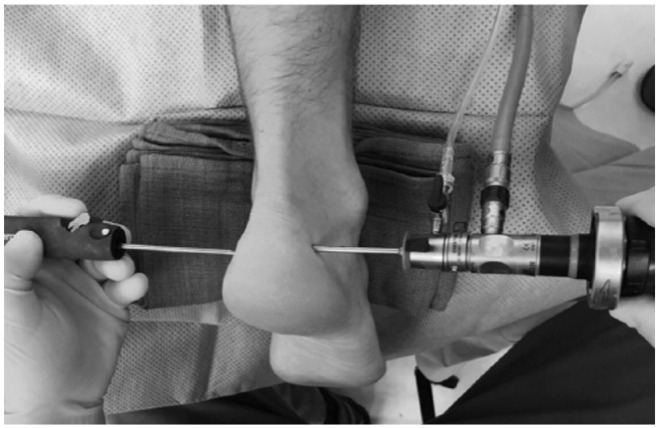
Ferranti et al 19 reported the use of a 2-mm incision anterolateral to the Achilles insertion on the calcaneus, followed by direct excision of the posterosuperior tuberosity with a Shannon burr (Figures 4 and 5). Percutaneous Haglund resection has been similarly described by Sergio et al 60 and Madarevic et al 39 using fluoroscopic or ultrasonographic guidance, respectively.
Figure 4.
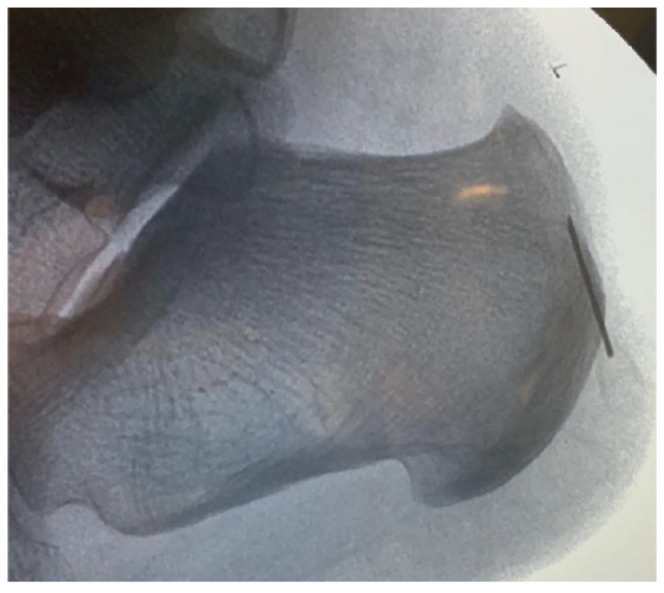
Preoperative fluoroscopy of MIS Haglund resection with needle to define the Haglund deformity by Ferranti et al. 19
Figure 5.
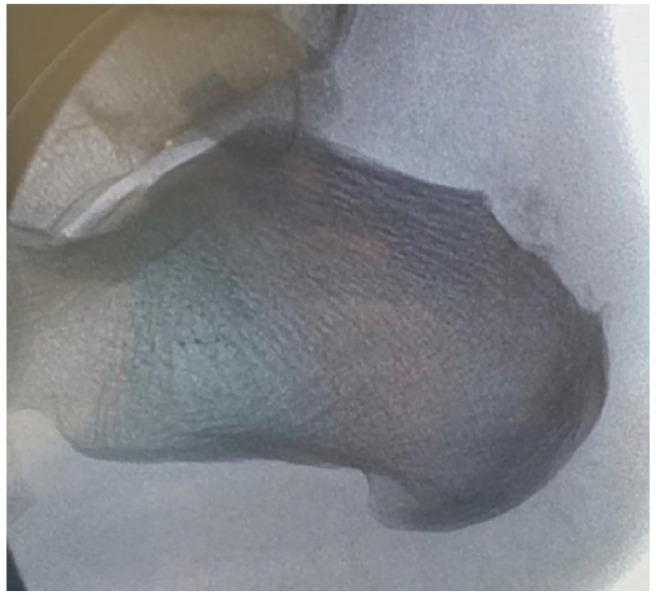
Postoperative fluoroscopy of MIS Haglund deformity resection by Ferranti et al. 19
Sergio et al 60 used a 5-mm lateral incision just superior to the insertion of the Achilles on the calcaneus. These authors reported first using a small rasp to remove fibrous tissue and periosteum off the bony surface. Then, a Shannon burr was used to remove the posterosuperior prominence. The authors suggest consistent monitoring of burr placement by using a second hand as a guide to make sure there was no medial penetration and fluoroscopic surveillance to avoid vascular, nerve, or tendon injury. After the HD is removed with the Shannon burr, light pressure is used to expel the bony fragments and debris. If there are any remaining bony fragments, the small rasp can be used again to remove them. 60
At a mean of 16.76 months’ follow-up, Sergio et al 60 reported that the mean American Orthopaedic Foot & Ankle Society ankle-hindfoot score (AOFAS) score significantly improved from 50.57 to 97.43. Mean visual analog scale (VAS) scores significantly improved from 6.85 to 0.19 at final follow-up (P < .001). At 1 month postoperatively, the Fowler-Philip angle had significantly improved from 79.57 to 53.76 degrees . Improvement of Fowler-Philip angle was correlated with the improvement of VAS score in this population. No major complications were reported in this study, and patients returned to activity at an average of 4 weeks. 60
Meanwhile, Madarevic et al 39 described a percutaneous Haglund resection through a single posteromedial incision under surveillance with a linear ultrasound probe. The authors recommended this posteromedial approach as it allows gradual bone resection from medial to lateral, with better protection of the sural nerve. The procedure is performed with the ankle fully dorsiflexed, and resection is considered complete when there is no longer impingement between the tendon and calcaneus as visualized by ultrasonography.
At the 3-month follow-up, Madarevic et al 39 reported improved pain and function. Mean AOFAS scores significantly improved from 57.5 to 97.5 whereas the mean Ogilvie-Harris scores improved from 7.4 to 15.3. Additionally, at 3-month follow-up there was no significant change in triceps surae strength (583 N preoperative vs 578 N postoperative). Only 1 complication was observed in this study, a minor superficial wound infection that resolved with antibiotics in 10 days. 39
Most recently, Ferranti et al reported significant improvement in VAS and Victorian Institute of Sports Assessment–Achilles (VISA-A) scores, as well as 90% patient satisfaction with this technique. VAS scores significantly improved from 8.1 to 2.4 at a mean of 26.5 months’ follow-up. Similarly, VISA-A scores improved from 20.7 to 75.7 at final follow-up. No major complications were observed; however, 3 of 27 patients presented with recurrence of their symptoms and required a revision surgery. 19
We recommend the percutaneous Haglund resection for patients who present with HD alone, without IAT.
Zadek osteotomy
The Zadek osteotomy (ZO) is a percutaneous technique that can be used for the treatment of both HD and IAT. This procedure is characterized by a dorsal closing wedge osteotomy of the calcaneal tuberosity. It was first described in 1939 as an open technique for the treatment of IAT.20,43,76 The ZO was subsequently demonstrated to be an effective approach to Haglund syndrome by Keck and Kelly in 1965.4,8,30 The ZO rotates the Achilles insertion anteriorly, decompressing the posterior heel and functionally lengthening the gastrocnemius complex, which in turn improves dorsiflexion and relieves pathological strain at the Achilles insertion.34,66,67,76 The technique also obviates the need for a gastrocnemius recession as patients on average gain 7 degrees of dorsiflexion compared to baseline. 67
Historically, open ZO was primarily indicated for patients with significant HD and retrocalcaneal bursitis.30,49,62 The indications for this procedure have since been expanded to include patients presenting with chronic IAT with or without intratendinous calcification.12,43,49 The Achilles insertion remains untouched during the ZO correction, reducing recovery time. Therefore, this may be a preferred intervention for patients presenting with significant IAT or concomitant Achilles pathology.12,49
ZO has been classically performed as an open procedure. However, the percutaneous approach has gained popularity to minimize wound complications while maintaining improved functional outcomes. The percutaneous ZO is typically performed in the lateral decubitus position often on the image intensifier platform of the mini fluoroscopic C-arm. The safe zone of over the calcaneal tuberosity as defined by Talusan is identified under fluoroscopic imaging. 64 At this point, a 5-mm incision is made in the safe zone to avoid the sural nerve, and blunt dissection with a small hemostat is preformed down to the calcaneus. Next, either the 3 × 20-mm or 3 × 30-mm Shannon burr is used to complete an approximately 10-mm dorsal closing wedge osteotomy. The osteotomy begins just anterior to the HD and ends just anterior to the insertion of the plantar fascia. A plantar hinge of 5-8 mm should be preserved to minimize plantar cortex violation and fracture, which potentially increases risk of nonunion.12,22,29,49
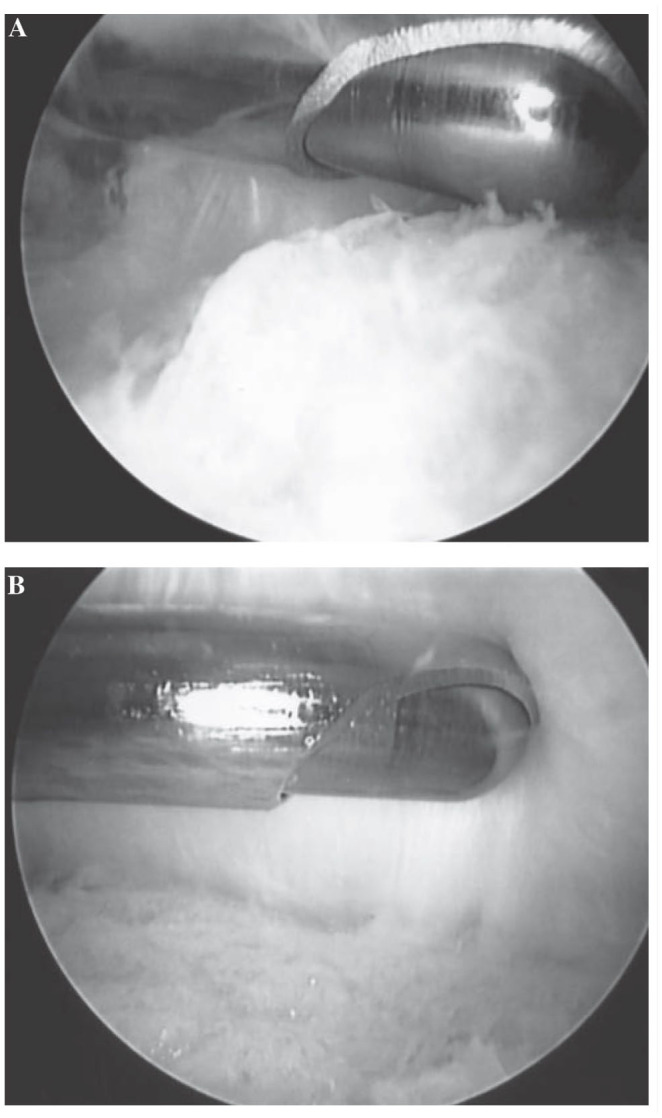
Although several osteotomy techniques have been described in the literature, we prefer the technique described by Kaplan et al. 29 This technique includes percutaneous wires that act as a cutting guide for the osteotomy, as well as a system for cutting the dorsal wedge (Figure 6). In their technique, Kaplan et al describe the quadrants in 2 planes, coronal and sagittal. In the coronal plane, the osteotomy should be completed lateral to medial in quadrants to ensure sufficient bone resection. In the sagittal plane, they prefer to divide the osteotomy into 3 sections: the plantar third, middle third, and dorsal third. Each section is then divided into a posterior and anterior section, thus creating 6 regions (Figure 6). They recommend starting at the junction of the middle and plantar third, with removal of the posterior plantar third from lateral to medial. The anterior plantar third is then removed, with special care being taken to maintain the plantar hinge. Next, the surgeon will remove the middle posterior third and the middle anterior third, followed by the dorsal posterior third and dorsal anterior third. 29
Figure 6.
(A) Sagittal and (B) axial schematic drawings of quadrant cut guide for percutaneous Zadek osteotomy as provided by Kaplan et al. 29
At this time the osteotomy is reduced with ankle dorsiflexion and held with percutaneous K-wires. Fluoroscopic imaging should be used to confirm that the osteotomy has closed down with good bony apposition (Figure 7). The osteotomy is then fixed with two 7.0- or 5.0-mm headless cannulated compression screws (Figure 8). 29 Both Kaplan et al 29 and Nordio et al 49 have described the percutaneous technique as an effective treatment for HD and IAT. 62
Figure 7.
Fluoroscopic imaging demonstrating oblique position of K-wires following percutaneous Zadek osteotomy (A) prior to and (B) following reduction maneuver. 29
Figure 8.
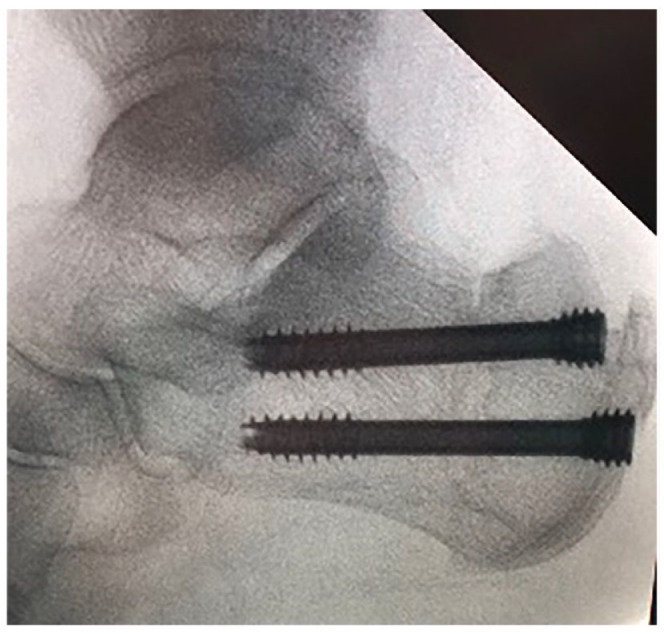
Final fluoroscopic imaging, demonstrating placement of two headless cannulated compression screws, perpendicular to the percutaneous Zadek osteotomy as described by Kaplan et al. 29
Numerous studies have demonstrated the effectiveness and safety of ZO in treating HD and IAT (Tables 1 and 2).8,12,20,22,34,40,49,66,67,78 Zhang et al 77 demonstrated improved VAS and AOFAS scores and no complications at a mean of 3.1 years of follow-up for the treatment of HS. VAS scores significantly improved from a preoperative mean of 7.23 to 0.43; AOFAS scores also significantly improved from 50.60 to 94.27. López-Capdevila et al 34 demonstrated 100% patient satisfaction following ZO for IAT. At a mean of 18.3-month follow-up, mean VAS pain scores significantly improved from 8.25 to 2.16; AOFAS scores also significantly improved from 41.5 to 86.5. 34 Finally, Georgiannaos et al 21 observed improvement in AOFAS and VISA-A scores in 52 athletes treated with ZO for IAT at a minimum 3 years’ follow-up. All professional athletes returned to their preinjury competition level at a mean of 15 weeks postoperatively. However, only 22 of 29 (75.9%) of recreational athletes returned to their preinjury competition level at a mean of 18 weeks of follow-up. The authors reported an improvement in AOFAS scores from a preoperative mean of 59.5 to 95.7 (P < .001); VISA-A scores improved from a preoperative mean of 65.9 to 90.2 (P < .001). 21
Table 1.
Demographics and Characteristics of Zadek Osteotomy Studies.
| Author | Zadek Osteotomy Type | Country | Level of Evidence | Participants, n | Mean Age, y | Feet, n | Women, n | Follow-up, mo, Mean or Range |
|---|---|---|---|---|---|---|---|---|
| Choi and Suh 10 | Percutaneous | South Korea | III | 10 | 37.4 | 11 | 6 | 20.3 |
| Nordio et al 49 | Percutaneous | Italy | III | 26 | 57 | 26 | 14 | 12 |
| deMeireles et al 12 | Percutaneous | USA | IV | 32 | 56.1 | 32 | NR | 16.1 |
| Zheng et al 78 | Open | China | III | 19 | 48.6 | 19 | NR | 16.3 |
| Lopez-Capdevila et al 34 | Open | Spain | IV | 18 | 49 | 18 | 11 | 18.3 |
| Georgiannos et al 22 | Open | Greece | IV | 52 | 32.5 | 64 | 30 | 36-60 |
| Ge et al 20 | Open | China | III | 12 | 32.8 | 12 | 3 | 86.5 |
| Tourné et al 67 | Open | France | II | 22 | 48.5 | 22 | 9 | 12 |
| Tourne et al 66 | Open | France | III | 50 | 54 | 50 | 15 | 84 |
| Maffulli et al 40 | Open | Italy | IV | 28 | 54.7 | 28 | 15 | 24-30 |
| Cengiz and Karaoglu 8 | Open | Turkey | III | 20 | 45.8 | 20 | 14 | 72 |
| Maffulli et al 41 | Open | Ireland | II | 25 | 53.5 | 25 | 14 | 24-28 |
Abbreviation: NR, not reported.
Table 2.
Postoperative Results of Zadek Osteotomy.
| Author | Zadek Osteotomy Type | AOFAS Improvement | VAS Improvement | VISA-A Improvement | Complication (Total) | Complication Rate, % | Satisfaction Rate, % |
|---|---|---|---|---|---|---|---|
| Choi and Suh 10 | Percutaneous | NR | 5.3* | 51.9* | 1 | 9.1 | NR |
| Nordio et al 49 | Percutaneous | 57* | 8* | NR | 2 | 7.7 | 92 |
| deMeireles et al 12 | Percutaneous | NR | NR | NR | 1 | 3.1 | NR |
| Zheng et al 78 | Open | 33.2* | 5.4* | NR | 1 | 5.3 | 95 |
| Lopez-Capdevila et al 34 | Open | 45.0* | 6.1* | 50.7* | 3 | 16.7 | 100 |
| Georgiannos et al 22 | Open | 36.2* | NR | 24.3* | 8 | 12.5 | NR |
| Ge et al 20 | Open | 46.2* | NR | 61.1 | 1 | 8.3 | NR |
| Tourné et al 67 | Open | 32.0* | NR | NR | 0 | 0 | NR |
| Tourne et al 66 | Open | 38.4* | NR | 24.9* | 3 | 6 | NR |
| Maffulli et al 40 | Open | NR | NR | NR | 3 | 10.7 | NR |
| Cengiz and Karaoglu 8 | Open | 32.6* | 4.5* | NR | 0 | 0 | NR |
| Maffulli et al 41 | Open | NR | 35.5* | 51* | 3 | 12 | NR |
Abbreviations: AOFAS, American Orthopaedic Foot & Ankle Society ankle-hindfoot score; NR, not reported; VAS, visual analog scale; VISA-A, Victorian Institute of Sports Assessment–Achilles.
Reported P < .05, indicating statistical significance.
In a retrospective cohort study comparing ZO to an open Haglund resection, Ge et al 20 demonstrated a significant improvement in AOFAS and VISA-A scores at 3 months following ZO. Functional outcome and pain scores continued to improve throughout a mean 86.5 months of follow-up. At last follow-up, AOFAS scores improved from a preoperative mean of 52.0 to 98.2 (P < .001), whereas VISA-A scores improved from a preoperative mean of 37.1 to 98.2 (P < .001). 20 Further, in direct comparison to an open Haglund resection, ZO demonstrated significantly improved AOFAS and VISA-A scores at final follow-up. AOFAS scores improved to 98.2 following ZO vs 93.4 following open resection at final follow-up (P = .03). Similarly, VISA-A scores were higher in the ZO group at final follow-up (98.2 vs 94.3; P = .010).
Similarly, Choi and Suh 10 compared the percutaneous ZO to open Haglund resection in a retrospective cohort study. Significant improvements in VAS and VISA-A scores were observed in both groups. However, MIS-DCWCO achieved earlier clinical improvement than open Haglund resection. Fowler-Philip and Böhler angles were significantly improved in both groups, indicating successful reduction of HD and strain on the Achilles. The percutaneous ZO was found to be a significantly shorter procedure (P = .001). One case of loss of fixation was noted in the ZO cohort, which required revision. 10
Finally, Nordio et al reported significant improvements in mean Functional Foot Index scores, which decreased from 65 preoperatively to 8 at an average of 12 months of follow-up. Similarly, VAS scores significantly improved from 9 to 1 following percutaneous intervention. The percutaneous ZO demonstrated an 8% complication rate in this study, with 1 patient requiring conversion to open debridement because of persistence of pain. Overall, patients took a mean of 12 weeks to achieve full pain relief and demonstrated a 92% satisfaction rate with percutaneous ZO intervention. 49
We recommend ZO for patients who present with IAT (with or without HD), including those with substantial insertional calcificaiton. 19 For those patients who present with attritional lengthening of the Achilles, we do not recommend a ZO.
Complications
Open procedures have been associated with an increased incidence of impaired wound healing, infection, pain, longer hospital stay, prolonged recovery time, and increased blood loss.6,27,33,49,50,59,71 Endoscopic and percutaneous procedures can have similar complications, although at a lower rate (5.3% vs 12.3% with open procedures).3,75 Complications particular to endoscopic and percutaneous procedures are low but still include skin burns, sural nerve injury, nonunion, and inflammation.11,18 Additional risks of the percutaneous Zadek osteotomy include sural nerve damage, plantar fasciitis, nonunion, malunion, hardware failure, hardware irritation, and persistent pain. These complications were observed in only a small percentage of patients (average 6.6% across reported studies), which was slightly lower compared with open procedures (7.9%).
Summary
Insertional Achilles tendinopathy with or without HD is one of the most common causes of heel pain managed by foot and ankle surgeons. Management begins with at least 3-6 months of conservative therapy. If this fails, surgical management may be considered. Historically, surgeons have used open techniques to manage IAT and HD. Although effective, open procedures have been reported to be associated with a longer recovery and slightly higher complication rates. 13 Endoscopic and percutaneous alternatives are safe and effective alternatives to open procedures and should now be considered by surgeons who treat patients with HD and IAT.
For patients who present with HD alone and no IAT, a percutaneous Haglund resection may be used. ECP is best reserved for those who present with HD and minimal IAT. 14 Further, for the patient who presents with more severe calcification at the Achilles insertion with (or without) HD, a percutaneous Zadek osteotomy can offer significant improvement in pain and function, with few complications.10,29,49 These techniques and indications should be considered carefully when deciding among surgical approaches for appropriate management of HD and IAT.
Supplemental Material
Supplemental material, sj-pdf-1-fai-10.1177_10711007241237529 for Minimally Invasive Approaches to Haglund’s Deformity and Insertional Achilles Tendinopathy: A Contemporary Review by SarahRose Hall, Jonathan R. M. Kaplan, Oliver N. Schipper, Ettore Vulcano, A. Holly Johnson, J. Benjamin Jackson, Amiethab A. Aiyer and Tyler A. Gonzalez in Foot & Ankle International
Footnotes
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Jonathan R. M. Kaplan, MD, reports royalties or licenses and consulting fees from Enovis and Novastep. Oliver N. Schipper, MD, reports royalties or licenses and consulting fees from Enovis. Ettore Vulcano, MD, reports royalties or licenses and consulting fees from Novastep. Tyler A. Gonzalez, MD, MBA, reports consulting fees from Enovis. Disclosure forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: SarahRose Hall, BA,  https://orcid.org/0000-0002-4026-3118
https://orcid.org/0000-0002-4026-3118
Jonathan R. M. Kaplan, MD,  https://orcid.org/0000-0002-0821-7939
https://orcid.org/0000-0002-0821-7939
Oliver N. Schipper, MD,  https://orcid.org/0000-0003-1248-640X
https://orcid.org/0000-0003-1248-640X
J. Benjamin Jackson, MD, MBA,  https://orcid.org/0000-0002-9444-087X
https://orcid.org/0000-0002-9444-087X
Amiethab A. Aiyer, MD  https://orcid.org/0000-0001-5070-2770
https://orcid.org/0000-0001-5070-2770
Tyler A. Gonzalez, MD, MBA,  https://orcid.org/0000-0002-3210-8097
https://orcid.org/0000-0002-3210-8097
References
- 1. AccessMedicine, McGraw Hill Medical. Ankle MRI. Basic Musculoskeletal Imaging, 2e. 2021. https://accessmedicine.mhmedical.com/content.aspx?sectionid=255923635&bookid=3075#1181070803
- 2. Agostinho De Lima Gomes M, Monteiro GF, Fernandes J, Neto A. Percutaneous surgery in the treatment of Haglund syndrome. J Foot Ankle. 2020;14(3):285-292. doi: 10.30795/JFOOTANKLE.2020.V14.1192 [DOI] [Google Scholar]
- 3. American Academy of Orthopaedic Surgeons. Minimally invasive surgery gains traction among foot and ankle surgeons. Accessed February 21, 2023. https://www.aaos.org/aaosnow/2019/sep/clinical/clinical02/
- 4. Boffeli TJ, Peterson MC. The Keck and Kelly wedge calcaneal osteotomy for Haglund’s deformity: a technique for reproducible results. J Foot Ankle Surg. 2012;51(3):398-401. doi: 10.1053/j.jfas.2012.03.002 [DOI] [PubMed] [Google Scholar]
- 5. Boniface O, Vervoort T. Endoscopic treatment of insertional Achilles tendinopathy: a cadaver feasibility study. Orthop Traumatol Surg Res. 2021;107(6):102893. doi: 10.1016/J.OTSR.2021.102893 [DOI] [PubMed] [Google Scholar]
- 6. Carmont MR, Maffulli N. Management of insertional Achilles tendinopathy through a Cincinnati incision. BMC Musculoskelet Disord. 2007;8:82. doi: 10.1186/1471-2474-8-82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Caudell GM. Insertional Achilles tendinopathy. Clin Podiatr Med Surg. 2017;34(2):195-205. doi: 10.1016/J.CPM.2016.10.007 [DOI] [PubMed] [Google Scholar]
- 8. Cengiz B, Karaoglu S. Clinical results of the Keck and Kelly wedge osteotomy approach in Haglund’s deformity: minimum 3-year follow-up. Foot Ankle Surg. 2022;28(2):269-275. doi: 10.1016/J.FAS.2021.10.006 [DOI] [PubMed] [Google Scholar]
- 9. Chimenti RL, Cychosz CC, Hall MM, Phisitkul P. Current concepts review update: insertional Achilles tendinopathy. Foot Ankle Int. 2017;38(10):1160-1169. doi: 10.1177/1071100717723127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Choi JY, Suh JS. A novel technique of minimally invasive calcaneal osteotomy for intractable insertional Achilles tendinopathy associated with Haglund deformity. Foot Ankle Orthop. 2022;7(4):2473011421S0061. doi: 10.1177/2473011421S00618 [DOI] [PubMed] [Google Scholar]
- 11. Cusumano A, Martinelli N, Bianchi A, Bertelli A, Marangon A, Sansone V. Transtendinous approach calcaneoplasty versus endoscopic calcaneoplasty for Haglund’s disease. Int Orthop. 2021;45(1):225-231. doi: 10.1007/S00264-020-04761-0 [DOI] [PubMed] [Google Scholar]
- 12. deMeireles AJ, Guzman JZ, Nordio A, Chan J, Okewunmi J, Vulcano E. Complications after percutaneous osteotomies of the calcaneus. Foot Ankle Orthop. 2022;7(3):24730114221119731. doi: 10.1177/24730114221119731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ebben BJ, Buckley SE, Hewitt MA, Moon DK, Metzl JA, Hunt KJ. Outcomes in open and endoscopic treatment for Haglund’s syndrome and insertional Achilles tendinopathy. Foot Ankle Orthop. 2022;7(4):2473011421S00652. doi: 10.1177/2473011421S00652 [DOI] [Google Scholar]
- 14. Ehredt DJ, Razzante MC, Darji D, Miggantz SH. Endoscopic calcaneoplasty with gastrocnemius recession for Haglund’s syndrome: is it safe and effective? Results from a retrospective case series. Foot. Published online January 13, 2023. doi: 10.1016/J.FOOT.2023.101960 [DOI] [PubMed] [Google Scholar]
- 15. ElGioshy A, Zayed E, Mostafa M. Endoscopic treatment of insertional Achilles tendinopathy. Egypt J Hosp Med. 2019;75(6):3124-3130. doi: 10.21608/EJHM.2019.34257 [DOI] [Google Scholar]
- 16. Erickson AR, Anderson J, Feely M, Snow MH. Seronegative spondyloarthropathy. In: Mikuls TR, Cannella AC, Moore GF, Erikson AR, Thiele GM, O’Dell JR, eds. Rheumatology: A Color Handbook. CRC Press; 2022:73-102. doi: 10.2169/naika.99.2439 [DOI] [Google Scholar]
- 17. Ewais WM, Romaih MAE. Hind-foot endoscopic decompression of the retrocalcaneal space as an appropriate treatment for refractory Haglund’s syndrome. Egypt Orthop J. 2020;55(2):121. doi: 10.4103/EOJ.EOJ_52_21 [DOI] [Google Scholar]
- 18. Fathi Mahmoud H, Feisal W, Samir Fahmy F. Satisfactory functional outcome and significant correlation with the length of Haglund’s deformity after endoscopic calcaneoplasty: a minimum 4-year follow-up study. Adv Orthop. 2022;2022:7889684. doi: 10.1155/2022/7889684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ferranti S, Migliorini F, Liuni FM, et al. Outcomes of percutaneous calcaneoplasty for insertional Achilles tendon problems. Foot Ankle Int. 2021;42(10):1287-1293. doi: 10.1177/10711007211004963 [DOI] [PubMed] [Google Scholar]
- 20. Ge Z, Ma L, Tang H, et al. Comparison of dorsal closing wedge calcaneal osteotomy versus posterosuperior prominence resection for the treatment of Haglund syndrome. J Orthop Surg Res. 2020;15(1):168. doi: 10.1186/s13018-020-01687-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Georgiannos D, Kitridis D, Bisbinas I. Dorsal closing wedge calcaneal osteotomy for the treatment of insertional Achilles tendinopathy: a technical tip to optimize its results and reduce complications. Foot Ankle Surg. 2018;24(2):115-118. doi: 10.1016/J.FAS.2016.12.004 [DOI] [PubMed] [Google Scholar]
- 22. Georgiannos D, Lampridis V, Vasiliadis A, Bisbinas I. Treatment of insertional Achilles pathology with dorsal wedge calcaneal osteotomy in athletes. Foot Ankle Int. 2016;38(4):381-387. doi: 10.1177/1071100716681139 [DOI] [PubMed] [Google Scholar]
- 23. Ghioldi ME, Chemes LN, Dealbera ED, De Prado M, Del Vecchio JJ. Modified Bösch osteotomy combined with a percutaneous adductor tendon release for the treatment of hallux valgus deformity: learning curve. Foot Ankle Spec. Published online March 3, 2022. doi: 10.1177/19386400221079198 [DOI] [PubMed] [Google Scholar]
- 24. Gonzalez T, Michalski M, Metzger M, Nelson T, Eberlein S, Pfeffer G. Biomechanical comparative study of postoperative Achilles pull-out strength after open versus endoscopic calcaneoplasty for Haglund’s syndrome. Foot Ankle Orthop. Published online September 18, 2018. doi: 10.1177/2473011418S00227 [DOI] [Google Scholar]
- 25. Güler Y, Birinci M, Hakyemez ÖS, et al. Achilles tendon-splitting approach and double-row suture anchor repair for Haglund syndrome. Foot Ankle Surg. 2021;27(4):421-426. doi: 10.1016/J.FAS.2020.05.009 [DOI] [PubMed] [Google Scholar]
- 26. Jackson JB, Kennedy B, Deal P, Gonzalez T. The surgical learning curve for modified Lapidus procedure for hallux valgus deformity. Foot Ankle Spec. Published online July 11, 2021. doi: 10.1177/19386400211029148 [DOI] [PubMed] [Google Scholar]
- 27. Jerosch J, Schunck J, Sokkar SH. Endoscopic calcaneoplasty (ECP) as a surgical treatment of Haglund’s syndrome. Knee Surg Sports Traumatol Arthrosc. 2007;15(7):927-934. doi: 10.1007/s00167-006-0279-3 [DOI] [PubMed] [Google Scholar]
- 28. Jowett CRJ, Bedi HS. Preliminary results and learning curve of the minimally invasive Chevron Akin operation for hallux valgus. J Foot Ankle Surg. 2017;56(3):445-452. doi: 10.1053/j.jfas.2017.01.002 [DOI] [PubMed] [Google Scholar]
- 29. Kaplan J, Hall S, Schipper O, Vulcano E, Jackson B, Gonzalez T. Percutaneous Zadek osteotomy for insertional Achilles tendinopathy and Haglund’s deformity: a technique tip. Foot Ankle Int. 2023;44(9):931-935. [DOI] [PubMed] [Google Scholar]
- 30. Keck S, Kelly P. Bursitis of the posterior part of the heel: evaluation of surgical treatment of eighteen patients. J Bone Joint Surg. 1965;47(2):267-273. Accessed March 28, 2023. https://journals.lww.com/jbjsjournal/Abstract/1965/47020/Bursitis_of_the_Posterior_Part_of_the_Heel_.3.aspx [PubMed] [Google Scholar]
- 31. Kondreddi V, Krishna Gopal R, Yalamanchili RK. Outcome of endoscopic decompression of retrocalcaneal bursitis. Indian J Orthop. 2012;46(6):659-663. doi: 10.4103/0019-5413.104201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kucuksen S, Karahan AY, Erol K. Haglund syndrome with pump bump. Med Arh. 2012;66(6):425-427. doi: 10.5455/medarh.2012.66.425-427 [DOI] [PubMed] [Google Scholar]
- 33. Leitze Z, Sella EJ, Aversa JM. Endoscopic decompression of the retrocalcaneal space. J Bone Joint Surg Am. 2003;85(8):1488-1496. doi: 10.2106/00004623-200308000-00009 [DOI] [PubMed] [Google Scholar]
- 34. López-Capdevila L, Santamaria Fumas A, Dominguez Sevilla A, et al. Dorsal wedge calcaneal osteotomy as surgical treatment for insertional Achilles tendinopathy. Rev Esp Cir Ortop Traumatol (Engl Ed). 2020;64(1):22-27. doi: 10.1016/J.RECOT.2019.09.004 [DOI] [PubMed] [Google Scholar]
- 35. Lughi M. Haglund’s syndrome: endoscopic or open treatment? Acta Biomed. 2020;91(4-S):167. doi: 10.23750/ABM.V91I4-S.9576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lui TH. Endoscopic Achilles tendon shortening. Foot. 2018;35:5-10. doi: 10.1016/J.FOOT.2017.12.006 [DOI] [PubMed] [Google Scholar]
- 37. Lui TH. Endoscopic calcaneoplasty and Achilles tendoscopy with the patient in supine position. Arthrosc Tech. 2016;5(6):e1475-e1479. doi: 10.1016/j.eats.2016.08.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lui TH, Lo CY, Siu YC. Minimally invasive and endoscopic treatment of Haglund syndrome. Foot Ankle Clin. 2019;24(3):515-531. doi: 10.1016/J.FCL.2019.04.006 [DOI] [PubMed] [Google Scholar]
- 39. Madarevic T, Rakovac I, Ruzic L, et al. Ultrasound-assisted calcaneoplasty. Knee Surg Sports Traumatol Arthrosc. 2014;22(9):2250-2253. doi: 10.1007/S00167-013-2692-8 [DOI] [PubMed] [Google Scholar]
- 40. Maffulli N, D’Addona A, Gougoulias N, Oliva F, Maffulli GD. Dorsally based closing wedge osteotomy of the calcaneus for insertional Achilles tendinopathy. Orthop J Sports Med. 2020;8(3):2325967120907985. doi: 10.1177/2325967120907985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Maffulli N, Gougoulias N, D’Addona A, Oliva F, Maffulli GD. Modified Zadek osteotomy without excision of the intratendinous calcific deposit is effective for the surgical treatment of calcific insertional Achilles tendinopathy. Surgeon. 2021;19(6):e344-e352. doi: 10.1016/J.SURGE.2020.08.018 [DOI] [PubMed] [Google Scholar]
- 42. Maffulli N, Saxena A, Wagner E, Torre G. Achilles insertional tendinopathy: state of the art. J ISAKOS. 2019;4(1):48-57. doi: 10.1136/JISAKOS-2017-000144 [DOI] [Google Scholar]
- 43. Mazura M, Goldman T, Stanislav P, Kachlik D, Hromadka R. Calcaneal osteotomy due to insertional calcaneal tendinopathy: preoperative planning. J Orthop Surg Res. 2022;17(1):1-5. doi: 10.1186/S13018-022-03359-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Michalski MP, Gonzalez TA, Metzger MF, Nelson TJ, Eberlein S, Pfeffer GB. Biomechanical comparison of Achilles tendon pullout strength following midline tendon-splitting and endoscopic approaches for calcaneoplasty. Foot Ankle Int. 2019;40(10):1219-1225. doi: 10.1177/1071100719856939 [DOI] [PubMed] [Google Scholar]
- 45. Michels F, Guillo S, King A, Jambou S, De Lavigne C. Endoscopic calcaneoplasty combined with Achilles tendon repair. Knee Surg Sports Traumatol Arthrosc. 2008;16(11):1043-1046. doi: 10.1007/S00167-008-0602-2 [DOI] [PubMed] [Google Scholar]
- 46. Miller CP, Acevedo JI, McWilliam JR, Michalski M. Endoscopic insertional Achilles reconstruction with double row suture bridge reconstruction: a technique tip. Foot Ankle Orthop. 2022;7(1):2473011421S00369. doi: 10.1177/2473011421S00369 [DOI] [Google Scholar]
- 47. Miller CP, McWilliam JR, Michalski MP, Acevedo J. Endoscopic Haglund’s resection and percutaneous double-row insertional Achilles repair. Foot Ankle Spec. 2021;14(6):534-543. doi: 10.1177/19386400211002707 [DOI] [PubMed] [Google Scholar]
- 48. Myerson CL, Shimozono Y, Kennedy JG. Haglund’s deformity and chronic Achilles tendonitis. Oper Tech Orthop. 2018;28(2):104-109. doi: 10.1053/J.OTO.2018.02.006 [DOI] [Google Scholar]
- 49. Nordio A, Chan JJ, Guzman JZ, Hasija R, Vulcano E. Percutaneous Zadek osteotomy for the treatment of insertional Achilles tendinopathy. Foot Ankle Surg. 2020;26(7):818-821. doi: 10.1016/J.FAS.2019.10.011 [DOI] [PubMed] [Google Scholar]
- 50. Ortmann FW, McBryde AM. Endoscopic bony and soft-tissue decompression of the retrocalcaneal space for the treatment of Haglund deformity and retrocalcaneal bursitis. Foot Ankle Int. 2016;28(2):149-153. doi: 10.3113/FAI.2007.0149 [DOI] [PubMed] [Google Scholar]
- 51. Palmanovich E, Ohana N, Atzmon R, et al. MICA: a learning curve. J Foot Ankle Surg. 2020;59(4):781-783. doi: 10.1053/J.JFAS.2019.07.027 [DOI] [PubMed] [Google Scholar]
- 52. Pfeffer G, Gonzalez T, Zapf M, Nelson TJ, Metzger MF. Achilles pullout strength after open calcaneoplasty for Haglund’s syndrome. Foot Ankle Int. 2018;39(8):966-969. doi: 10.1177/1071100718770391 [DOI] [PubMed] [Google Scholar]
- 53. Pi Y, Hu Y, Guo Q, et al. Open versus endoscopic osteotomy of posterosuperior calcaneal tuberosity for Haglund syndrome: a retrospective cohort study. Orthop J Sports Med. 2021;9(4):23259671211001055. doi: 10.1177/23259671211001055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Reddy NS, Narsimlu D. Minimally invasive endoscopic management of Haglund syndrome. J Cont Med Dent. 2023;8(1):43-47. Accessed February 11, 2023. www.jcmad.com [Google Scholar]
- 55. Roth KE, Mueller R, Schwand E, et al. Open versus endoscopic bone resection of the dorsolateral calcaneal edge: a cadaveric analysis comparing three dimensional CT scans. J Foot Ankle Res. 2014;7(1):1-8. doi: 10.1186/S13047-014-0056-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Sammarco GJ, Taylor AL. Operative management of Haglund’s deformity in the nonathlete: a retrospective study. Foot Ankle Int. 1998;19(11):724-729. doi: 10.1177/107110079801901102 [DOI] [PubMed] [Google Scholar]
- 57. Saxena A, Ramdath S, O’Halloran P, Gerdesmeyer L, Gollwitzer H. Extra-corporeal Pulsed-activated Therapy (“EPAT” Sound Wave) for Achilles tendinopathy: a prospective study. J Foot Ankle Surg. 2011;50(3):315-319. doi: 10.1053/j.jfas.2011.01.003 [DOI] [PubMed] [Google Scholar]
- 58. Sayana MK, Maffulli N. Insertional Achilles tendinopathy. Foot Ankle Clin. 2005;10(2):309-320. doi: 10.1016/J.FCL.2005.01.010 [DOI] [PubMed] [Google Scholar]
- 59. Scholten PE, van Dijk CN. Endoscopic calcaneoplasty. Foot Ankle Clin. 2006;11(2):439-446. doi: 10.1016/J.FCL.2006.02.004 [DOI] [PubMed] [Google Scholar]
- 60. Sergio F, Catani O, Fusini F, et al. Treating Haglund’s deformity with percutaneous Achilles tendon decompression: a case series. Muscles Ligaments Tendons J. 2018;8(4):488-494. doi: 10.11138/MLTJ/2018.8.4.488 [DOI] [Google Scholar]
- 61. Strasser NL, Farina KA. Haglund’s syndrome and insertional Achilles tendinopathy. Oper Tech Sports Med. 2021;29(3):150850. doi: 10.1016/j.otsm.2021.150850 [DOI] [Google Scholar]
- 62. Syed TA, Perera A. A proposed staging classification for minimally invasive management of Haglund’s syndrome with percutaneous and endoscopic surgery. Foot Ankle Clin. 2016;21(3):641-664. doi: 10.1016/J.FCL.2016.04.004 [DOI] [PubMed] [Google Scholar]
- 63. Tallerico VK, Greenhagen RM, Lowery C. Isolated gastrocnemius recession for treatment of insertional Achilles tendinopathy. Foot Ankle Spec. 2014;8(4):260-265. doi: 10.1177/1938640014557077 [DOI] [PubMed] [Google Scholar]
- 64. Talusan PG, Cata E, Tan EW, Parks BG, Guyton GP. Safe zone for neural structures in medial displacement calcaneal osteotomy: a cadaveric and radiographic investigation. Foot Ankle Int. 2015;36(12):1493-1498. doi: 10.1177/1071100715595696 [DOI] [PubMed] [Google Scholar]
- 65. Toepfer A, Strässle M. The percutaneous learning curve of 3rd generation minimally-invasive Chevron and Akin osteotomy (MICA). Foot Ankle Surg. 2022;28(8):1389-1398. doi: 10.1016/J.FAS.2022.07.006 [DOI] [PubMed] [Google Scholar]
- 66. Tourne Y, Baray AL, Barthelemy R, Karhao T, Moroney P. The Zadek calcaneal osteotomy in Haglund’s syndrome of the heel: clinical results and a radiographic analysis to explain its efficacy. Foot Ankle Surg. 2022;28(1):79-87. doi: 10.1016/J.FAS.2021.02.001 [DOI] [PubMed] [Google Scholar]
- 67. Tourné Y, Francony F, Barthélémy R, Karhao T, Moroney P. The Zadek calcaneal osteotomy in Haglund’s syndrome of the heel: its effects on the dorsiflexion of the ankle and correlations to clinical and functional scores. Foot Ankle Surg. 2022;28(6):789-794. doi: 10.1016/J.FAS.2021.11.001 [DOI] [PubMed] [Google Scholar]
- 68. Vaishya R, Agarwal AK, Azizi AT, et al. Haglund’s syndrome: a commonly seen mysterious condition. Cureus. 2016;8(10):e820. doi: 10.7759/cureus.820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. van Dijk CN, van Dyk GE, Scholten PE, Kort NP. Endoscopic calcaneoplasty. Am J Sports Med. 2001;29(2):185-189. doi: 10.1177/03635465010290021101 [DOI] [PubMed] [Google Scholar]
- 70. Vega J, Baduell A, Malagelada F, Allmendinger J, Dalmau-Pastor M. Endoscopic Achilles tendon augmentation with suture anchors after calcaneal exostectomy in Haglund syndrome. Foot Ankle Int. 2018;39(5):551-559. doi: 10.1177/1071100717750888 [DOI] [PubMed] [Google Scholar]
- 71. Wang CL, Chen PY, Yang KC, Wu HC, Wang CC. Ultrasound-guided minimally invasive surgical resection of retrocalcaneal bursitis: a preliminary comparison with traditional open surgery. J Foot Ankle Surg. 2019;58(5):855-860. doi: 10.1053/J.JFAS.2018.12.023 [DOI] [PubMed] [Google Scholar]
- 72. Wendler DE, Stewart GW, Bailey EJ, Shofoluwe AI, Nwaibu U. Minimally invasive foot & ankle surgery: a review and a novel technique. Foot Ankle Orthop. 2022;7(4):2473011421S0100. doi: 10.1177/2473011421S01001 [DOI] [Google Scholar]
- 73. Wu Z, Yao W, Chen S, Li Y. Clinical study outcome of extracorporeal shock wave therapy for insertional Achilles tendinopathy with and without Haglund’s deformity. Biomed Res Int. 2016;2016:6315846. doi: 10.1155/2016/6315846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Xu JH, Ding SL, Chen B, Wu SC. Modified Bunnell suture expands the surgical indication of the treatment of Haglund’s syndrome heel pain with endoscope. Exp Ther Med. 2018;15(6):4817-4821. doi: 10.3892/ETM.2018.6071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Yuen WLP, Tan PT, Kon KKC. Surgical treatment of Haglund’s deformity: a systematic review and meta-analysis. Cureus. 2022;14(7):e27500. doi: 10.7759/cureus.27500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Zadek I. An operation for the cure of achillobursitis. Am J Surg. 1939;43(2):542-546. doi: 10.1016/S0002-9610(39)90877-9 [DOI] [Google Scholar]
- 77. Zhang C, Cao J, Yang L, Duan X. Surgical treatment for insertional Achilles tendinopathy and retrocalcaneal bursitis: more than 1 year of follow-up. J Int Med Res. 2021;49(3):300060521992959. doi: 10.1177/0300060521992959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Zheng W, Du J, Liang J, Zhang Y, Liang X, Zhao H. Zadek osteotomy for the treatment of Haglund’s syndrome. Research Square. Published online June 23, 2020. doi: 10.21203/rs.3.rs-37115/v1 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-fai-10.1177_10711007241237529 for Minimally Invasive Approaches to Haglund’s Deformity and Insertional Achilles Tendinopathy: A Contemporary Review by SarahRose Hall, Jonathan R. M. Kaplan, Oliver N. Schipper, Ettore Vulcano, A. Holly Johnson, J. Benjamin Jackson, Amiethab A. Aiyer and Tyler A. Gonzalez in Foot & Ankle International