Abstract
Background:
Identifying and targeting common preventable causes of 30-day hospital readmissions could help improve survival rates and reduce the healthcare burden.
Objective:
To determine the rate and causes of unplanned hospital return/readmission to the Outpatient Department (OPD) or Emergency Department (ED) within 30 days after discharge following head and neck surgery (HNS) at a tertiary hospital in Western Saudi Arabia.
Methods:
This retrospective study included all adult patients (aged ≥18 years) who had undergone HNS at King Abdulaziz University Hospital, Jeddah, Saudi Arabia, between January 2015 and December 2022 and returned to the OPD or ED within 30 days of being discharged.
Results:
Of 1041 patients who had undergone HNS, 84 (8.1%) returned to the hospital within 30 days after discharge: 63 (6.1%) to the OPD and 21 (2.0%) to the ED. A total of 9 (0.9%) patients were readmitted as inpatients, most commonly for infections (33.3%) and neurological symptoms, including weakness and seizures (22.2%). For OPD visits, common causes were wound swelling (25.4%) and neurological symptoms (17.5%). For ED returns, frequent causes were neurological symptoms (23.8%) and surgical site bleeding (19.1%). Readmission was associated with intensive care unit (ICU) admission during the primary hospital stay (P = 0.003) and higher preoperative baseline health burdens when examined using the American Society of Anesthesiology score (P = 0.022), the Cumulative Illness Rating Scale (P = 0.007), and the Charlson Comorbidity Index (CCI) (P = 0.006).
Conclusion:
The rate of 30-day unplanned hospital return following head and neck surgery was 6.1% and 2.0% through the OPD and the ED, respectively; 0.9% were readmitted as inpatients. Common causes of return included wound swelling, infections, bleeding, and neurological symptoms.
Keywords: 30-day readmission, causes, emergency department, head and neck surgery, infection rates, readmission, Saudi Arabia
INTRODUCTION
Unplanned hospital returns post-surgery are frequent, costly, and avoidable with careful planning and patient education.[1,2,3] Such readmissions remain a significant contributor to healthcare spending: about one in seven patients are readmitted after a major surgery, of which 12.3% are preventable readmissions.[4,5] A 30-day unplanned hospital readmission is commonly considered an indicator of treatment quality.[6] Therefore, decreasing hospital revisits is vital for clinicians, hospitals, and policymakers.[7]
Readmissions in otolaryngology range from 2% to 8% depending on the procedure, and thus single readmission rates are not reflective of this specialty.[8,9] Head and neck surgeries (HNS), especially oncologic HNS, are complex and incorporate multiple-step procedures, including excisions, vascular reconstructions, and primary neck dissection, and use various techniques.[10] Unplanned readmissions expose these vulnerable patients to hospital-acquired complications, which may affect their survival rates.[7] The rates of revisits after HNS have been reported to range from 7.3% to 26.5%.[6,11,12,13] The most commonly reported reasons for hospital readmissions following HNS are infections[11] and wound complications.[7]
Identifying the common causes for revisits can help target preventable causes, which may lower the unplanned revisit rates, decrease the risk of hospital-acquired complications, improve survival rates and quality of life, and lower the healthcare burden. Nevertheless, the rate and causes for unplanned hospital returns following HNS are not clearly described in populations within Saudi Arabia. Therefore, this study aimed to identify the rate and causes of 30-day return/readmission to the Outpatient Department (OPD) or Emergency Department (ED) following HNS at King Abdulaziz University Hospital (KAUH), Jeddah, Saudi Arabia, as this data may be utilized to produce rate-lowering interventions.
METHODS
Study design, setting, and participants
This retrospective study included all adult patients (aged ≥18 years) who had undergone HNS at KAUH between January 01, 2015, and December 31, 2022, and returned to the OPD or ED within 30 days of being discharged.
Data were collected from the electronic medical records using the International Classification of Diseases codes, Tenth Revision (ICD-10), after obtaining approval from the Institutional Review Board of KAUH. Patients with missing data for key variables, such as the reason for hospitalization, were excluded. During the 30-day period, if more than one episode of unplanned return/readmission was found, only the initial episode was considered.
Outcomes
The primary objective was to determine the causes of unplanned return through the ED or OPD, extracted as the final diagnosis from the medical record system. The secondary objective was to determine the readmission rate as inpatients among those who returned and well as compare the variables between admitted and non-readmitted patients.
Variables
Demographic data, such as age and gender, and body mass index (BMI) were extracted. The primary surgical location, condition type (benign or malignant), and dates of primary admission and hospital course, including history of intensive care unit (ICU) admission, or intubation, procedure, discharge, and return, were also collected. Procedures involving skin, ears, adenoids, and tonsils were not included in the study. Table 1 shows examples of the included procedures classified into procedural categories.
Table 1.
Procedure-based categories included in the study
| Category | Example |
|---|---|
| Salivary gland | Parotidectomy |
| Thyroid/parathyroid | Thyroidectomy |
| Sinonasal/skull base | Endoscopic resection of sinonasal tumor |
| Limited neck | Sistrunk procedure |
| Neck dissection only | Cervical lymph node dissection |
| Major head and neck surgery with no flap | Laryngectomy |
| Major head and neck surgery with pedicled flap | Resection of the oropharynx with pectoralis myocutaneous rotation flap reconstruction |
| Major head and neck surgery with free flap | Oropharyngeal resection with forearm free flap reconstruction |
| Open airway | Tracheostomy |
| Limited oral cavity | Hemiglossectomy |
Furthermore, details of patients’ comorbidities were collected and examined using the preoperative American Society of Anesthesiology score of physical well-being (ASA), the Charlson Comorbidity Index (CCI), and the Cumulative Illness Rating Scale (CIRS). The CCI is a validated scale that is used to predict long-term prognosis and survival, depending on the individual’s comorbidities.[14] The CIRS is a comorbidity scale that assesses the overall burden of disease through 13 generally different body systems.[15]
Data analysis
The data was submitted into Google Forms and then exported to Excel version 16.0. SPSS version 21.0 for Windows was used to analyze the data, and statistical significance was set at P < 0.05. Continuous variables are expressed as means and standard deviation (SD) or median with interquartile ranges (IQR) depending on the distribution. Number and frequency are used to summarize categorical variables. To compare means, medians, and frequencies, Student’s t-test, Mann-Whitney U test, and Chi-square test were used, respectively. Variables with significant associations were used in the multivariate regression analysis.
RESULTS
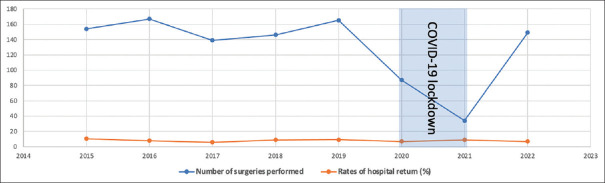
During the study period, 1041 patients underwent HNS. Within 30 days of discharge, 84 (8.1%) patients returned to the hospital, with 9 (0.9%) admitted as inpatients. Of these, 63 (6.1%) patients had returned to the OPD; 3 (0.3%) were readmitted as inpatients. On the other hand, 21 (2.0%) patients returned to the ED, of which 6 (0.6%) were readmitted. Table 2 provides the demographic data and baseline characteristics of patients included in the study. The rate of hospital returns between 2015 and 2022 ranged from 5.8% to 10.4%. Because of the lockdown during the peak of the COVID-19 pandemic, the number of surgeries performed decreased during 2020–21, yet the rates were similar to those during the rest of the study period [Figure 1].
Table 2.
Baseline characteristics and demographic data of the patients (N=84)
| Variable | Included |
|---|---|
| Age (years), mean±SD | 48.2±15.4 |
| Female, n (%) | 53 (63.1) |
| Length of primary stay in days, median (IQR) | 3 (2–7) |
| CIRS, mean±SD | 3.9±2.9 |
| CCI, mean±SD | 2.5±1.9 |
| ASA, mean±SD | 2±0.6 |
| Previous radiotherapy, n (%) | 23 (27.4) |
| Previous chemotherapy, n (%) | 2 (2.4) |
| Previous chemoradiation therapy, n (%) | 3 (3.6) |
CIRS – Cumulative Illness Rating Scale; CCI – Charlson Comorbidity Index; ASA – American Society of Anesthesiologists; SD – Standard deviation; IQR – Interquartile range
Figure 1.
Rates of hospital returns for each year during the study period
As demonstrated in Table 3, the most common reason for OPD visits was wound swelling (25.4%). Table 4 outlines the reasons for ED visits, with neurological symptoms (23.8%), such as seizures, paralysis, and numbness, being the most common. Infections such as surgical site infection, urinary tract infection, pneumonia, and sepsis were the most common reasons for readmission as an inpatient (26.3%) [Table 5].
Table 3.
Rates and causes of outpatient department visits (N=63)
| Causes | n (%) |
|---|---|
| Wound swelling: Hematoma, seroma | 16 (25.4) |
| Neurological: Seizure, weakness, peripheral numbness | 11 (17.5) |
| Infections: Surgical site, UTI, sepsis, pneumonia | 9 (14.3) |
| Hoarseness | 6 (9.5) |
| Respiratory: Dyspnea, wheezing | 6 (9.5) |
| Pain in the surgical site | 4 (6.4) |
| Fatigue | 4 (6.4) |
| Equipment issues: Tracheostomy, surgical drain | 3 (4.8) |
| Facial nerve paralysis | 1 (1.6) |
| Gastrointestinal: Nausea, vomiting | 1 (1.6) |
| Cardiac: Chest pain, palpitation | 1 (1.6) |
| Fistula | 1 (1.6) |
UTI – Urinary tract infection
Table 4.
Rates and causes of emergency department visits (N=21)
| Causes | n (%) |
|---|---|
| Neurological: Seizure, weakness, peripheral numbness | 5 (23.8) |
| Surgical site bleeding | 4 (19.1) |
| Hematoma | 3 (14.3) |
| Infections: Surgical site, UTI, sepsis, pneumonia | 3 (14.3) |
| Equipment issues: Tracheostomy, surgical drain | 2 (9.5) |
| Cardiac: Chest pain, palpitation | 2 (9.5) |
| Gastrointestinal: Nausea, vomiting | 1 (4.8) |
| Respiratory: Dyspnea, wheezing | 1 (4.8) |
UTI – Urinary tract infection
Table 5.
Rate and causes of readmission as an inpatient (N=9)
| Causes | n (%) |
|---|---|
| Infections: Surgical site | 3 (33.3) |
| Neurological: Seizure, weakness, peripheral numbness | 2 (22.2) |
| Gastrointestinal: Nausea, vomiting | 1 (11.1) |
| Equipment issues: Tracheostomy, surgical drain | 1 (11.1) |
| Wound swelling: Hematoma, seroma | 1 (11.1) |
| Wound dehiscence | 1 (11.1) |
The ED and OPD groups are compared in Table 6. Male patients were found to be more likely to return to the ED than female patients (66.7% vs. 33.3%; P = 0.003). Further, ED patients had a significantly higher mean age than OPD patients (56.2 years vs. 45.6 years; P = 0.005). In addition, malignancy as a reason for surgery was linked to ED visits (P = 0.006). Patients who returned to the ED had a greater rate of readmission as inpatients (P = 0.008), and also significantly higher ASA (P = 0.012), CCI (P = 0.001), and CIRS (P = 0.001) values than those who visited the OPD.
Table 6.
Comparison between emergency department and outpatient department groups
| Variable | ED | OPD | P |
|---|---|---|---|
| Age, mean±SD | 56.19±19.82 | 45.56±12.74 | 0.005 |
| Gender, n (%) | |||
| Male | 14 (66.7) | 17 (27) | 0.003 |
| Female | 7 (33.3) | 46 (73) | |
| BMI, n (%) | |||
| <18.5 | 4 (19) | 4 (6.3) | 0.236 |
| 18.5–24.9 | 3 (14.3) | 12 (19) | |
| 25–29.9 | 8 (38.1) | 19 (30.2) | |
| 30–34.9 | 5 (23.8) | 13 (20.6) | |
| 35–39.9 | 0 | 10 (15.9) | |
| >40 | 1 (4.8) | 5 (7.9) | |
| Type of condition, n (%) | |||
| Benign | 1 (4.8) | 25 (39.7) | 0.006 |
| Malignant | 20 (95.2) | 38 (60.3) | |
| Readmission as inpatient, n (%) | |||
| Yes | 6 (28.6) | 3 (4.8) | 0.008 |
| No | 15 (71.4) | 60 (95.2) | |
| ASA, mean±SD | 2.29±0.56 | 1.91±0.62 | 0.012 |
| CCI, mean±SD | 3.86±2.03 | 2.02±1.58 | 0.001 |
| CIRS, mean±SD | 5.95±3.15 | 3.18±2.41 | 0.001 |
CIRS – Cumulative Illness Rating Scale; CCI – Charlson Comorbidity Index; ASA – American Society of Anesthesiologists; SD – Standard deviation; BMI – Body mass index; ED – Emergency department; OPD – Outpatient department
The mean age of readmitted patients was considerably higher (57.78 ± 18.73 years) than that of non-readmitted patients (47.07 ± 14.67 years) (P = 0.048). Patients who were readmitted (2.44 ± 0.73) had higher ASA scores than those who were not (1.95 ± 0.59) (P = 0.022). Furthermore, readmitted patients had higher CIRS scores (7.22 ± 3.11) than those who were not readmitted (3.47 ± 2.57) (P = 0.007). Similarly, readmitted patients had significantly higher CCI values (4.67 vs. 2.21, P = 0.006). Those who were admitted to the ICU during the primary hospital course had a higher chance of having an unplanned hospital readmission (P = 0.008). A weak positive correlation was found between the length of primary hospital admission and being readmitted (r = 0.111, P = 0.313). Table 7 shows a comparison between readmitted and non-readmitted patients. In addition, the multivariate regression analysis found multiple independent risk factors for hospital readmission, including the ASA [odds ratio (OR) =0.125; 95% confidence interval (CI): 0.018–0.232; P = 0.022], CIRS (OR = 0.044; 95% CI: 0.023–0.066; P < 0.001), and CCI (OR = 0.068; 95% CI: 0.034–0.101; P < 0.001) scores as well as ICU admission (OR = 0.524; 95% CI: 0.261–0.787; P < 0.001) and older age (OR = 0.04; 95% CI: 0.001–0.009; P = 0.048).
Table 7.
Comparison between readmitted and nonreadmitted patients
| Variable | Readmitted | Nonreadmitted | P |
|---|---|---|---|
| Age, mean±SD | 57.78±18.73 | 47.07±14.67 | 0.048 |
| Gender, n (%) | |||
| Male | 4 (44.4) | 27 (36) | 0.720 |
| Female | 5 (55.6) | 48 (64) | |
| BMI, n (%) | |||
| <18.5 | 1 (11.1) | 7 (9.3) | 0.653 |
| 18.5–24.9 | 3 (33.3) | 12 (16) | |
| 25–29.9 | 3 (33.3) | 24 (32) | |
| 30–34.9 | 1 (11.1) | 17 (22.2) | |
| 35–39.9 | 0 | 10 (13.3) | |
| >40 | 1 (11.1) | 5 (6.7) | |
| Type of condition, n (%) | |||
| Benign | 0 | 26 (34.7) | 0.081 |
| Malignant | 9 (100) | 49 (65.3) | |
| ASA, mean±SD | 2.44±0.73 | 1.95±0.59 | 0.022 |
| CCI, mean±SD | 4.67±2 | 2.21±1.69 | 0.006 |
| CIRS, mean±SD | 7.22±3.11 | 3.47±2.57 | 0.007 |
| ICU admission, n (%) | |||
| Yes | 3 (33.33) | 2 (2.67) | 0.003 |
| No | 6 (66.67) | 73 (97.33) | |
| History of intubation during hospital course, n (%) | |||
| Yes | 1 (11.11) | 5 (6.67) | 0.505 |
| No | 8 (88.89) | 70 (93.33) |
CIRS – Cumulative Illness Rating Scale; CCI – Charlson Comorbidity Index; ASA – American Society of Anesthesiologists; SD – Standard deviation; BMI – Body mass index; ICU – Intensive care unit
DISCUSSION
This retrospective study described the rate and causes of unplanned hospital readmission within 30 days after HNS in a Saudi tertiary academic center. The 30-day readmission rates have been used as a quality measure for hospital care, as it is more related to the surgical complications and quality of life post-surgery rather than the longer follow-up periods.[6] However, its use may be limited. While there are possibly preventable reasons for readmission, non-modifiable factors that can contribute to patient readmission and ED utilization exist. Patient’s gender, race, socioeconomic level, and comorbidities are among these characteristics.[16] The reasons for readmission vary depending on the patient demographics. As a result, by evaluating a specialty population, such as HNS patients, the specialized needs of that group can be determined. Although the preventable causes of 30-day readmission are low due to various non-modifiable factors, this study revealed common reasons for hospital returns, such as infection and wound complications, which may be avoidable with modifications to discharge planning and enhanced patient education.
In our study, the rate of hospital revisits after HNS was 8.07%, of which 0.87% were readmitted as inpatients; this is below the 3.2%–16.1% readmission rates reported in other studies.[7,11,13,17,18,19] In the United States, a nationwide study on the rate and causes of readmission after HNS in head and neck cancer patients found that the rate of readmissions was 16.1%, with infections and wound complications being the most common causes.[13] In our study, all readmitted patients were malignant cases. However, including benign and malignant causes of HNS in our study may have resulted in the lower return rates. Nonetheless, our findings regarding the causes of readmission were consistent, with infections and wound complications being the most common causes.[13] Such etiologies may be preventable with proper patient and caregiver education. Patients with head and neck cancer are likelier to have a higher rate of unplanned readmissions than patients treated in other subspecialties of otolaryngology. Readmissions are especially critical in this patient population, as it not only exposes them to hospital-acquired complications but can also delay adjuvant therapy, potentially leading to a decrease in survival rates.[20] Cancer patients are highly prone to infections, and vigorous preventative treatment for head and neck cancer patients should receive more attention. Because most returning patients in our study had malignancies as an indication of HNS, planned interventions around this may reduce the risk of unnecessary hospital returns.
The rate of ED revisits post-HNS in our study was 2.0%, with frequent causes being neurological symptoms, such as weakness and seizures, and surgical site bleeding. In a similar study, Wu and Hall observed a return rate of 8.4% to the ED, with pain being the most common cause.[11] Young et al. studied patients undergoing thyroidectomy and parathyroidectomy, and found that the rate of ED utilization following discharge after surgery was 11.2%, with the most frequent causes being wound complications and paresthesia.[21]
Medication review with personalized caregiver and patient education about the significance of proper hydration and red flags for electrolyte problems may all help prevent ED visits.[22,23] Several studies have shown the effectiveness of various coordinated programs.[24,25,26] Project Better Outcomes by Optimizing Safe Transitions (BOOST) focuses on approaches such as enhanced patient education, polypharmacy reduction, and outpatient follow-up verification.[26] The Re-Engineered Discharge (RED) project facilitates phone calls between pharmacists and patients 2–4 days after discharge to answer queries and avoid medication-related complications.[25] These projects have been associated with lower readmission rates and lower emergency department returns. The findings highlight the significance of extensive pre-discharge planning and maintaining contact between physician and patient.
In this study, we used three different validated comorbidity scores to evaluate patients’ comorbidities and their predictive value for readmission after HNS. All three scores showed a significant association with readmission and ED utilization within 30 days of discharge. Previous reports confirmed that the ASA score is closely linked with predicting readmissions and is positively associated with increased readmission rates.[11,27,28] In addition, the CIRS comorbidity score has been used in HNS patients, with larger scores suggesting worsening baseline health.[11,15,29] Moreover, the CCI score has been used in patients undergoing HNS as a predictor for ED revisits, with higher scores being a risk factor for ED return within 30 days after surgery.[30] Hence, returned patients in our study had a higher baseline health burden, which exposed them to more significant complications and led to them returning to the hospital. Furthermore, it is well recognized that patients with head and neck cancer have higher comorbidities, which are generally the consequence of long-term exposure to risk factors such as alcohol and tobacco use.[31,32,33] Nonetheless, more extensive and close post-surgery follow-ups for individuals with high baseline health burdens may reduce unplanned hospital readmissions.
Strengths and limitations
To the best of the authors’ knowledge, this is the first such study from western Saudi Arabia. However, our findings are to be interpreted with several limitations. Owing to the retrospective study design, the authors could not conclusively report the specific cause and the exact time of returning to the hospital post-discharge. Moreover, because of poor documentation, valuable variables that can potentially affect the results, such as the tumor subtype and stage in malignant cases, were not discussed in the study. This study was conducted at a referral center in western Saudi Arabia, and many patients in the studied population live in peripheral areas. The process of referral and transportation may make it difficult to achieve consistent follow-up during the first 30 days after surgery. Furthermore, the fact that our study was limited to a single area may limit the generalizability of findings. Another factor that can affect the accuracy of the results is the relatively small sample size. Therefore, further multicentric prospective studies with extended follow-up periods on larger populations are required.
CONCLUSION
The 30-day unplanned hospital return rate after HNS was 6.1% and 2.0% through the OPD and the ED respectively, and 0.9% were readmitted as inpatients. The most common causes for readmission were wound swelling, infections, neurological symptoms, and surgical site bleeding. Using the current study findings, strategies can be developed to reduce the burden by addressing the common causes of hospital readmission and return rates.
Ethical considerations
The study was approved by the Unit of Biomedical Ethics, Research Ethics Committee of the Faculty of Medicine, King Abdulaziz University and King Abdulaziz University Hospital (Ref. No: 561-22; date: November 22, 2022). The requirement for written consent was waived owing to the study design. The study adhered to the principles of the Declaration of Helsinki, 2013.
Peer review
This article was peer-reviewed by two independent and anonymous reviewers.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Frankl SE, Breeling JL, Goldman L. Preventability of emergent hospital readmission. Am J Med. 1991;90:667–74. [PubMed] [Google Scholar]
- 2.Anderson GF, Steinberg EP. Hospital readmissions in the Medicare population. N Engl J Med. 1984;311:1349–53. doi: 10.1056/NEJM198411223112105. [DOI] [PubMed] [Google Scholar]
- 3.Soeken KL, Prescott PA, Herron DG, Creasia J. Predictors of hospital readmission. A meta-analysis. Eval Health Prof. 1991;14:262–81. doi: 10.1177/016327879101400302. [DOI] [PubMed] [Google Scholar]
- 4.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 5.Goldfield NI, McCullough EC, Hughes JS, Tang AM, Eastman B, Rawlins LK, et al. Identifying potentially preventable readmissions. Health Care Financ Rev. 2008;30:75–91. [PMC free article] [PubMed] [Google Scholar]
- 6.Graboyes EM, Yang Z, Kallogjeri D, Diaz JA, Nussenbaum B. Patients undergoing total laryngectomy: An at-risk population for 30-day unplanned readmission. JAMA Otolaryngol Head Neck Surg. 2014;140:1157–65. doi: 10.1001/jamaoto.2014.1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goel AN, Yang JY, Wang MB, Lee JT, St John MA, Long JL. Predictors, costs, and causes of readmission after surgery for sinonasal cancer: A national perspective. Int Forum Allergy Rhinol. 2018;8:1056–64. doi: 10.1002/alr.22134. [DOI] [PubMed] [Google Scholar]
- 8.Graboyes EM, Liou TN, Kallogjeri D, Nussenbaum B, Diaz JA. Risk factors for unplanned hospital readmission in otolaryngology patients. Otolaryngol Head Neck Surg. 2013;149:562–71. doi: 10.1177/0194599813500023. [DOI] [PubMed] [Google Scholar]
- 9.Jain U, Chandra RK, Smith SS, Pilecki M, Kim JY. Predictors of readmission after outpatient otolaryngologic surgery. Laryngoscope. 2014;124:1783–8. doi: 10.1002/lary.24533. [DOI] [PubMed] [Google Scholar]
- 10.Cannon RB, Houlton JJ, Mendez E, Futran ND. Methods to reduce postoperative surgical site infections after head and neck oncology surgery. Lancet Oncol. 2017;18:e405–13. doi: 10.1016/S1470-2045(17)30375-3. [DOI] [PubMed] [Google Scholar]
- 11.Wu V, Hall SF. Rates and causes of 30-day readmission and emergency room utilization following head and neck surgery. J Otolaryngol Head Neck Surg. 2018;47:36. doi: 10.1186/s40463-018-0283-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chaudhary H, Stewart CM, Webster K, Herbert RJ, Frick KD, Eisele DW, et al. Readmission following primary surgery for larynx and oropharynx cancer in the elderly. Laryngoscope. 2017;127:631–41. doi: 10.1002/lary.26311. [DOI] [PubMed] [Google Scholar]
- 13.Chen MM, Orosco RK, Harris JP, Porter JB, Rosenthal EL, Hara W, et al. Predictors of readmissions after head and neck cancer surgery: A national perspective. Oral Oncol. 2017;71:106–12. doi: 10.1016/j.oraloncology.2017.06.010. [DOI] [PubMed] [Google Scholar]
- 14.Tuty Kuswardhani RA, Henrina J, Pranata R, Anthonius Lim M, Lawrensia S, Suastika K. Charlson comorbidity index and a composite of poor outcomes in COVID-19 patients: A systematic review and meta-analysis. Diabetes Metab Syndr. 2020;14:2103–9. doi: 10.1016/j.dsx.2020.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Linn BS, Linn MW, Gurel L. Cumulative illness rating scale. J Am Geriatr Soc. 1968;16:622–6. doi: 10.1111/j.1532-5415.1968.tb02103.x. [DOI] [PubMed] [Google Scholar]
- 16.Benbassat J, Taragin M. Hospital readmissions as a measure of quality of health care: Advantages and limitations. Arch Intern Med. 2000;160:1074–81. doi: 10.1001/archinte.160.8.1074. [DOI] [PubMed] [Google Scholar]
- 17.Bur AM, Brant JA, Mulvey CL, Nicolli EA, Brody RM, Fischer JP, et al. Association of clinical risk factors and postoperative complications with unplanned hospital readmission after head and neck cancer surgery. JAMA Otolaryngol Head Neck Surg. 2016;142:1184–90. doi: 10.1001/jamaoto.2016.2807. [DOI] [PubMed] [Google Scholar]
- 18.Offodile AC, 2 nd, Pathak A, Wenger J, Orgill DP, Guo L. Prevalence and patient-level risk factors for 30-day readmissions following free tissue transfer for head and neck cancer. JAMA Otolaryngol Head Neck Surg. 2015;141:783–9. doi: 10.1001/jamaoto.2015.1323. [DOI] [PubMed] [Google Scholar]
- 19.Dziegielewski PT, Boyce B, Manning A, Agrawal A, Old M, Ozer E, et al. Predictors and costs of readmissions at an academic head and neck surgery service. Head Neck. 2016;38(Suppl 1):E502–10. doi: 10.1002/hed.24030. [DOI] [PubMed] [Google Scholar]
- 20.Tribius S, Donner J, Pazdyka H, Münscher A, Gröbe A, Petersen C, et al. Survival and overall treatment time after postoperative radio (chemo) therapy in patients with head and neck cancer. Head Neck. 2016;38:1058–65. doi: 10.1002/hed.24407. [DOI] [PubMed] [Google Scholar]
- 21.Young WG, Succar E, Hsu L, Talpos G, Ghanem TA. Causes of emergency department visits following thyroid and parathyroid surgery. JAMA Otolaryngol Head Neck Surg. 2013;139:1175–80. doi: 10.1001/jamaoto.2013.4505. [DOI] [PubMed] [Google Scholar]
- 22.Jack BW, Chetty VK, Anthony D, Greenwald JL, Sanchez GM, Johnson AE, et al. Areengineered hospital discharge program to decrease rehospitalization: A randomized trial. Ann Intern Med. 2009;150:178–87. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Evans RL, Hendricks RD. Evaluating hospital discharge planning: A randomized clinical trial. Med Care. 1993;31:358–70. doi: 10.1097/00005650-199304000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Meehan Sr TP, Qazi DJ, Van Hoof TJ, Ho SY, Eckenrode S, Spenard A, et al. Process evaluation of a quality improvement project to decrease hospital readmissions from skilled nursing facilities. J Am Med Dir Assoc. 2015;16:648–53. doi: 10.1016/j.jamda.2015.02.015. [DOI] [PubMed] [Google Scholar]
- 25.Sanchez GM, Douglass MA, Mancuso MA. Revisiting project re-engineered discharge (RED): The impact of a pharmacist telephone intervention on hospital readmission rates. Pharmacotherapy. 2015;35:805–12. doi: 10.1002/phar.1630. [DOI] [PubMed] [Google Scholar]
- 26.Hansen LO, Greenwald JL, Budnitz T, Howell E, Halasyamani L, Maynard G, et al. Project BOOST: Effectiveness of a multihospital effort to reduce rehospitalization. J Hosp Med. 2013;8:421–7. doi: 10.1002/jhm.2054. [DOI] [PubMed] [Google Scholar]
- 27.Merkow RP, Ju MH, Chung JW, Hall BL, Cohen ME, Williams MV, et al. Underlying reasons associated with hospital readmission following surgery in the United States. JAMA. 2015;313:483–95. doi: 10.1001/jama.2014.18614. [DOI] [PubMed] [Google Scholar]
- 28.AlDardeir N, Alzhrani G, Alqutub A, Kabli R, Sait D, Alsaeed R, et al. Rates and causes of readmission within 60 days following hysterectomy in a tertiary care center in Saudi Arabia. Cureus. 2023;15:e36500. doi: 10.7759/cureus.36500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Castro MA, Dedivitis RA, Ribeiro KC. Comorbidity measurement in patients with laryngeal squamous cell carcinoma. ORL J Otorhinolaryngol Relat Spec. 2007;69:146–52. doi: 10.1159/000099223. [DOI] [PubMed] [Google Scholar]
- 30.Baskin RM, Zhang J, Dirain C, Lipori P, Fonseca G, Sawhney R, et al. Predictors of returns to the emergency department after head and neck surgery. Head Neck. 2018;40:498–511. doi: 10.1002/hed.25019. [DOI] [PubMed] [Google Scholar]
- 31.Hashibe M, Brennan P, Benhamou S, Castellsague X, Chen C, Curado MP, et al. Alcohol drinking in never users of tobacco, cigarette smoking in never drinkers, and the risk of head and neck cancer: Pooled analysis in the international head and neck cancer epidemiology consortium. J Natl Cancer Inst. 2007;99:777–89. doi: 10.1093/jnci/djk179. [DOI] [PubMed] [Google Scholar]
- 32.Blot WJ, McLaughlin JK, Winn DM, Austin DF, Greenberg RS, Preston-Martin S, et al. Smoking and drinking in relation to oral and pharyngeal cancer. Cancer Res. 1988;48:3282–7. [PubMed] [Google Scholar]
- 33.Hashibe M, Boffetta P, Zaridze D, Shangina O, Szeszenia-Dabrowska N, Mates D, et al. Evidence for an important role of alcohol- and aldehyde-metabolizing genes in cancers of the upper aerodigestive tract. Cancer Epidemiol Biomarkers Prev. 2006;15:696–703. doi: 10.1158/1055-9965.EPI-05-0710. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.