Abstract
This case report details the journey of a 51-year-old man residing in a remote Iranian village, involved in livestock rearing, who was hospitalized due to Brucellosis contracted from consuming traditional cheese and dairy products. Initially treated with doxycycline and rifampin, complications arose during antituberculosis therapy, with the patient developing symptoms of nausea, vomiting, and edema alongside renal function deterioration necessitating medication cessation. Subsequent manifestations of proteinuria, toxic hepatitis, and nephrotic syndrome prompted renal biopsy, revealing drug-induced glomerular and tubular damage. Swift cessation of rifampicin, combined with prednisolone therapy, led to symptom amelioration, resulting in the cessation of dialysis and the patient's discharge within three weeks. This case underscores the intricate relationship between traditional cheese consumption, medication-induced renal complications, and the importance of timely intervention and appropriate management in achieving a successful patient outcome.
Keywords: Hemodialysis, Renal failure, Cheese, Brucellosis, Rifampin
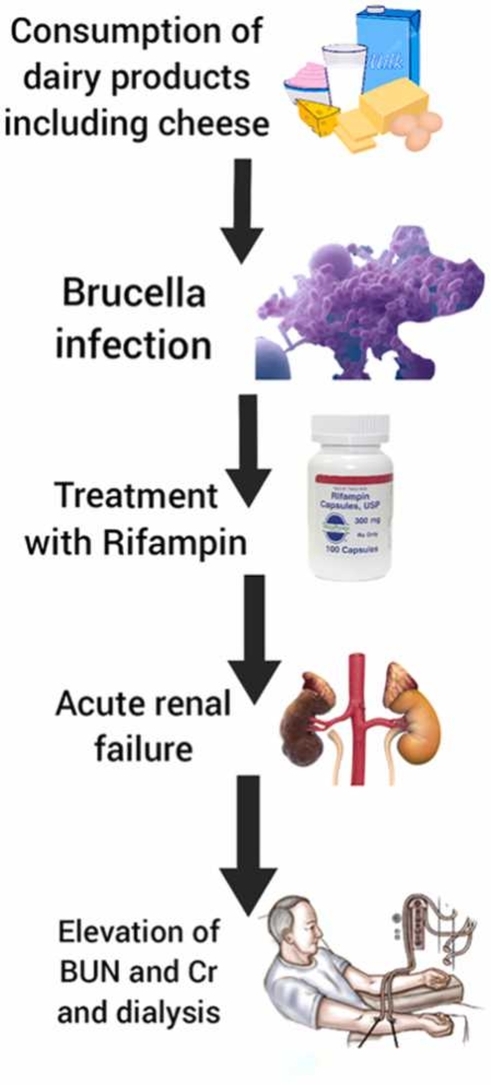
Graphical Abstract
Highlights
-
•
Brucellosis is caused by species of the Brucella bacteria.
-
•
Rifampin is commonly used as part of the treatment regimen for Brucellosis.
-
•
Rifampin may sometimes lead to complications like acute renal failure.
1. Introduction
Consuming dairy products, including cheese, can be a delicious part of a balanced diet [1]. However, there is a risk of developing Brucellosis, a bacterial infection that can be transmitted to humans through unpasteurized dairy products [2]. Brucellosis is caused by species of the Brucella bacteria, commonly found in infected animals like cows, sheep, and goats [1].
When dairy products such as cheese are made from unpasteurized milk, the bacteria can survive and potentially infect individuals who consume them [3]. Symptoms of Brucellosis in humans may include fever, sweats, fatigue, joint and muscle pain, as well as other flu-like symptoms [4]. In severe cases, the infection can lead to more serious complications affecting the heart, liver, or even the central nervous system [5], [6], [7], [8], [9].
Brucellosis, caused by the Brucella bacteria, is typically treated with a combination of antibiotics [3]. Rifampin is commonly used as part of the treatment regimen for Brucellosis due to its effectiveness against the bacteria [10]. Rifampin works by inhibiting the growth of Brucella, helping to eliminate the infection from the body [3]. When combined with other antibiotics like doxycycline or trimethoprim-sulfamethoxazole, rifampin can enhance the treatment efficacy and reduce the risk of relapse [10].
Rifampin may sometimes lead to complications like acute renal failure, a condition characterized by a sudden loss of kidney function [11]. Common symptoms of acute renal failure encompass reduced urine output, swelling in limbs or other areas, nausea, and fatigue [10].
Managing acute renal failure in Brucellosis patients requires a comprehensive approach that addresses both the underlying infection and kidney dysfunction [12]. Treatment may involve close monitoring of kidney function, fluid and electrolyte management, and in severe cases, dialysis to support kidney function [13], [14]. It is important for healthcare providers to closely monitor Brucellosis patients receiving rifampin and other antibiotics for any signs of kidney involvement to promptly address and manage acute renal failure if it occurs.
2. Case presentation
A 51-year-old man living in a remote village in Iran, whose occupation involved raising livestock, was hospitalized for three weeks due to Brucellosis contracted from consuming traditional cheese and dairy products. Upon hospital admission, he received a prescription for doxycycline at 100 mg orally twice daily and rifampin at a dosage of 600–900 mg per day orally, to be continued for a period of 6 weeks. The patient had no significant medical history, with normal laboratory findings showing a serum creatinine level of 0.76 mg/dL and blood urea nitrogen level of 12.9 mg/dL.
During the course of antituberculosis therapy, the patient experienced nausea, vomiting, general weakness, and edema. His serum creatinine and blood urea nitrogen levels rose to 1.1 mg/dL and 19 mg/dL, respectively, prompting the discontinuation of rifampicin. However, his symptoms worsened, leading to a 6-day progression characterized by proteinuria and the onset of dyspnea and pulmonary edema necessitating hospitalization for further evaluation.
On admission, the patient exhibited signs of fluid retention, with a weight gain of 7.8 kg over the previous month. Suspected nephrotic syndrome coupled with acute nonoliguric renal failure prompted renal biopsy, which revealed nonsclerotic glomeruli with normocellularity and mild focal tubular injury (Fig. 1). The heavy proteinuria postulated to be induced by antituberculosis medications manifested as toxic hepatitis and nephrotic syndrome.
Fig. 1.
Renal biopsy histology showed a glomerulus with moderate initial segmental sclerosis and intense interstitial inflammation marked by lymphocytes and granulocytes.
Following the discontinuation of rifampicin and isoniazid alongside prednisolone therapy, the patient's symptoms gradually ameliorated. Nausea, vomiting, and pulmonary edema improved after a week of steroid treatment, leading to the cessation of dialysis. With a recovery in body weight and overall condition, the patient was discharged three weeks after the cessation of rifampicin, marking a successful resolution of the medication-induced complications.
3. Discussion
The presented case highlights the complex interplay between Brucellosis, treatment with rifampin and doxycycline, and the subsequent development of medication-induced nephrotic syndrome and toxic hepatitis. This unique case underscores the importance of close monitoring and prompt intervention in patients undergoing antibiotic therapy for Brucellosis, especially in regions where unpasteurized dairy consumption is common.
Comparing this case with previous studies and cases, several key similarities and differences emerge [15], [16]. While Brucellosis-related renal complications have been documented in literature, the development of medication-induced nephrotic syndrome and toxic hepatitis following rifampin and isoniazid therapy is relatively rare [17]. Previous studies have primarily focused on the renal manifestations of Brucellosis itself, emphasizing the need for early diagnosis and appropriate antibiotic treatment to prevent severe complications [18].
In contrast, the presented case sheds light on the potential adverse effects of rifampin and isoniazid, commonly used in tuberculosis treatment, in the context of Brucellosis. The rapid onset of symptoms, including proteinuria, acute renal failure, and pulmonary edema, underscores the need for vigilance in monitoring patients undergoing antibiotic therapy for zoonotic infections like Brucellosis.
The management of medication-induced nephrotoxicity and hepatotoxicity in this case involved a combination of discontinuing the offending agents, initiating prednisolone therapy, and providing supportive care [19], [20], [21], [22], [23], [24]. The favorable response to treatment and subsequent recovery of the patient's renal function further emphasize the importance of early recognition and intervention in drug-induced complications [10].
Moving forward, more research is warranted to elucidate the mechanisms underlying medication-induced renal and hepatic complications in Brucellosis patients undergoing antibiotic therapy. Clinicians should maintain a high index of suspicion for such adverse effects, particularly in individuals with pre-existing renal impairment or liver disease. Collaborative efforts between infectious disease specialists, nephrologists, and hepatologists are crucial for optimizing the management of complex cases like the one presented here and improving patient outcomes.
Drug toxicity is a serious concern in patient care, exacerbated by the complexities of managing drug interactions and adverse effects [20]. Nurses play a crucial role in monitoring patients for signs of drug toxicity, such as altered mental status, organ dysfunction, or abnormal vital signs, especially in the context of COVID-19 where medication regimens may be altered [25], [26], [27], [28]. Nursing interventions involve close monitoring of medication administration, promptly recognizing and reporting symptoms of toxicity, collaborating with healthcare teams to adjust dosages or change medications, and educating patients on medication management to mitigate risks associated with drug toxicity during the ongoing pandemic [29], [30].
4. Conclusion
In conclusion, acute interstitial nephritis is increasingly recognized as a significant cause of reversible acute renal failure, often linked to drug hypersensitivity reactions. While the exact pathogenesis of tubular necrosis remains unclear, renal biopsy stands out as the definitive diagnostic tool. Particularly in patients undergoing treatment for pulmonary tuberculosis with rifampicin, vigilance for rifampicin-induced acute renal failure is crucial. Swift diagnosis and discontinuation of rifampicin play a pivotal role in renal function recovery. This case presentation underscores the unique interplay between polyuria development and rifampicin administration, potentially enriching clinical understanding in this context.
CRediT authorship contribution statement
Ali Mseri: Software, Supervision, Validation. Rasoul Goli: Supervision, Validation, Writing – original draft, Writing – review & editing. Milad Ahangarzadeh: Formal analysis, Validation, Visualization, Writing – original draft. Razieh Janghiyamachi: Project administration, Investigation. Kamal Rahimi: Investigation, Methodology, Resources, Supervision. Navid Faraji: Validation, Supervision, Software, Data curation. Behnam Babamiri: Software, Writing – original draft, Writing – review & editing. Mohammad Reza Faramarzi: Supervision, Software, Resources. Mahin Roohani: Funding acquisition. Hiva Lotfy: Formal analysis, Funding acquisition.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Handling Editor: L.H. Lash
Contributor Information
Rasoul Goli, Email: Rasoulgoli94@gmail.com.
Mohammad Reza Faramarzi, Email: Faramarzimohammedreza@gmail.com.
Data Availability
No data was used for the research described in the article.
References
- 1.Dadar M., Tabibi R., Alamian S., Caraballo-Arias Y., Mrema E.J., Mlimbila J., Chandrasekar S., Dzhusupov K., Sulaimanova C., Alekesheva L.Z., Manar S.A. Safety concerns and potential hazards of occupational brucellosis in developing countries: a review. J. Public Health. 2023;31(10):1681–1690. [Google Scholar]
- 2.Elbehiry A., Aldubaib M., Marzouk E., Abalkhail A., Almuzaini A.M., Rawway M., Alghamdi A., Alqarni A., Aldawsari M., Draz A. The development of diagnostic and vaccine strategies for early detection and control of human brucellosis, particularly in endemic areas. Vaccines. 2023;11(3):654. doi: 10.3390/vaccines11030654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ghanbari M.K., Gorji H.A., Behzadifar M., Sanee N., Mehedi N., Bragazzi N.L. One health approach to tackle brucellosis: a systematic review. Trop. Med. Health. 2020;48(1):0. doi: 10.1186/s41182-020-00272-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jiang H., O’Callaghan D., Ding J.B. Brucellosis in China: history, progress and challenge. Infect. Dis. Poverty. 2020;9(03):101–104. doi: 10.1186/s40249-020-00673-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Faraji N., Goli R., Ghalandari M., Taghavinia S., Malkari B., Abbaszadeh R. Treatment of severe extravasation injury in a newborn by using tilapia fish skin: a case report. Int. J. Surg. Case Rep. 2022;91 doi: 10.1016/j.ijscr.2022.106759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Faraji N., Goli R., Choobianzali B., Bahrami S., Sadeghian A., Sepehrnia N., Ghalandari M. Ozone therapy as an alternative method for the treatment of diabetic foot ulcer: a case report. J. Med. Case Rep. 2021;15(1):8. doi: 10.1186/s13256-021-02829-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goli R., Faraji N., Shakorzadeh S., Abbasi M., Abbaszadeh R., Mostafaei B. Treating extravasation injury by honey antibacterial wound dressing in a neonate: a case report. Int. J. Surg. Case Rep. 2022;95 [Google Scholar]
- 8.Babamiri B., Nikkhah F., Faraji N., Goli R., Moghaddam N.V., Rahimi K. Diabetic foot ulcer: Successful healing with combination therapy, including surgical debridement, maggot therapy, and negative pressure wound therapy. Int. J. Surg. Case Rep. 2023;110 doi: 10.1016/j.ijscr.2023.108695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Faraji N., Parizad N., Goli R., Nikkhah F., Golhkar M. Fighting diabetic foot ulcer by combination therapy, including larva therapy, Medi honey ointment, and silver alginate dressings: a case report. Int. J. Surg. Case Rep. 2023 Dec 1;113 doi: 10.1016/j.ijscr.2023.109055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bosilkovski M., Keramat F., Arapović J. The current therapeutical strategies in human brucellosis. Infection. 2021;49(5):823–832. doi: 10.1007/s15010-021-01586-w. [DOI] [PubMed] [Google Scholar]
- 11.Young E.J. Treatment of brucellosis in humans. InBrucellosis 2020 Jul 24 (pp. 127-141). CRC Press.
- 12.Edathodu J., Alamri M., Alshangiti K.A., Alfagyh N.S., Alnaghmush A.S., Albaiz F., Alothman B., Khalil H., Edathodu Z., Alrajhi A.A. Clinical manifestations and treatment outcomes of human brucellosis at a tertiary care center in Saudi Arabia. Ann. Saudi Med. 2021;41(2):109–114. doi: 10.5144/0256-4947.2021.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arad M., Goli R., Parizad N., Vahabzadeh D., Baghaei R. Do the patient education program and nurse-led telephone follow-up improve treatment adherence in hemodialysis patients? A randomized controlled trial. BMC Nephrol. 2021;22:1–3. doi: 10.1186/s12882-021-02319-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yavari S., Radfar M., Faraji N., Goli R., Bagherzadi A., Atharifar R., Kazemi S., Dadashi M. Self-esteem and optimism in patients with major depression disorder: a cross-sectional study. Ann. Med. Surg. 2023;85(11):5379–5383. doi: 10.1097/MS9.0000000000001263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang Z., Wu W., Ou P., Zeng F., Xie D., Yang L., Yang G., Zhou B. Discussion on treatment courses of brucellosis with spondylitis-a report of two cases. IDCases. 2023 Jan 1;31 doi: 10.1016/j.idcr.2022.e01650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dagli O., Dokur M., Guzeldag G., Ozmen Y. Acute renal failure due to Brucella melitensis. J. Infect. Dev. Ctries. 2011;5(12):893–895. doi: 10.3855/jidc.1442. [DOI] [PubMed] [Google Scholar]
- 17.Toprak O., Kaptan F., Cirit M., Ormen B., Uzum A., Ersoy R., Turker N. Recurrent rhabdomyolysis and mild acute renal failure associated with acute Brucella infection. Nephrol. Dial. Transplant. 2005;20(4):848–849. doi: 10.1093/ndt/gfh703. [DOI] [PubMed] [Google Scholar]
- 18.Nunan T.O., Eykyn S.J., Jones N.F. Brucellosis with mesangial IgA nephropathy: successful treatment with doxycycline and rifampicin. Br. Med. J. (Clin. Res. Ed.) 1984;288(6433):1802. doi: 10.1136/bmj.288.6433.1802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Faraji N., Goli R., Mohsennezhad P., Mohammadpour Y., Parizad N., Salamat E., Pourbahram R., Bazbandi S. NSAID (nonsteroidal anti-inflammatory drugs) Induced Stevens Johnson Syndrome in a 50-year-old woman: a case study. Toxicol. Rep. 2024 doi: 10.1016/j.toxrep.2024.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goli R., Faraji N., Janghiyamachi R., Talebiazar N. Nicolau syndrome after intramuscular injection of methocarbamol: a rare case report. Toxicol. Rep. 2023;11:346–348. doi: 10.1016/j.toxrep.2023.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lagzi N., Bateni A., Goli R., Talebiazar N. The effect of multivitamins on anxiety and depression in patients undergoing methadone maintenance treatment: A double-blind randomized controlled trial. Int. J. Psychiatry Med. 2023;58(6):576–590. doi: 10.1177/00912174231179320. [DOI] [PubMed] [Google Scholar]
- 22.Rahimi K., Goli R., Faraji N., Pourheidar B., Nabavi S., Pourheidar M., Babamiri B. The effects of coadministration of curcumin and vitamin E on the reproductive system of diabetic male rats; An experimental study. Toxicol. Rep. 2023;11:241–248. doi: 10.1016/j.toxrep.2023.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Faraji N., Nikkhah F., Goli R., Hassanpour A., Imanzadeh F., Yavari S. Pyknodysostosis: a case report of an 8-year-old male with a rare genetic disorder. Int. J. Surg. Case Rep. 2023;110 doi: 10.1016/j.ijscr.2023.108793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parizad N., Faraji N., Hassanpour A., Goli R., Rostami S., Amanollahzadeh A. Cyclopia, a newborn with a single eye, a rare but lethal congenital anomaly: a case report. Int. J. Surg. Case Rep. 2021;88 doi: 10.1016/j.ijscr.2021.106548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heidari S., Parizad N., Goli R., Mam-Qaderi M., Hassanpour A. Job satisfaction and its relationship with burnout among nurses working in COVID-19 wards: a descriptive correlational study. Ann. Med. Surg. 2022;82 doi: 10.1016/j.amsu.2022.104591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aghakhani N., Faraji N., Alinejad V., Goli R., Kazemzadeh J. The effect of guided imagery on the quality and severity of pain and pain-related anxiety associated with dressing changes in burn patients: a randomized controlled trial. Burns. 2022;48(6):1331–1339. doi: 10.1016/j.burns.2021.11.020. [DOI] [PubMed] [Google Scholar]
- 27.Aghakhani N., Faraji N., Parizad N., Goli R., Alinejad V., Kazemzadeh J. Guided imagery: an effective and practical complementary medicine method to alleviate pain severity and pain-related anxiety during dressing change in burn victims. J. Burn Care Res. 2022;43(3):756. doi: 10.1093/jbcr/irac024. [DOI] [PubMed] [Google Scholar]
- 28.Jasemi M., Goli R., Zabihi R.E., Khalkhali H. Educating ethics codes by lecture or role-play; which one improves nursing students' ethical sensitivity and ethical performance more? A quasi-experimental study. J. Prof. Nurs. 2022;40:122–129. doi: 10.1016/j.profnurs.2021.11.002. [DOI] [PubMed] [Google Scholar]
- 29.Goli R., Faraji N., Maroofi H., Hassanpour A. Effect of spiritual care on the quality of life in patients who underwent intracranial hemorrhage surgery: a randomized controlled trial. Int. J. Surg. 2024;110(1):167–175. doi: 10.1097/JS9.0000000000000813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Molaee H., Goli R., Faraji N., Dizaji N.N., Bagheri M., Shakorzadeh S., Hassanpour A., Imanzadeh F., Lameei R. The effect of acupressure on sleep quality in patients with leukemia: a single-center, randomized controlled trial. Annals of Medicine and Surgery.:10-97.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data was used for the research described in the article.



