Abstract
Purpose
This study aimed to compare knowledge and attitudes towards obstetric danger signs and care between females receiving maternal care and their male partners.
Methods and Materials
A community-based comparative cross-sectional study was conducted in the rural setting of Jimma, Ethiopia. Female and their male partners were selected randomly. The number of participants included from each sex was 3235 totaling 6470. Face-to-face data collection was employed using open data kit (ODK) software. A pre-test was performed before the data collection. Descriptive and analytical statistical analysis was used to compare knowledge and attitudes regarding obstetric danger signs and care. Predictor variables were declared considering a 95% confidence interval, adjusted odds ratio (AOR) and P-value less than 0.05.
Results
On average, male and female participants identified at least two obstetric danger signs. More females could mention more antenatal, childbirth, and postnatal danger signs than their male partners. Both females and their male partners who listened to the radio at least once per week had a statistically significant positive attitude towards obstetric care. Nonetheless, both had an almost similar magnitude of attitude towards obstetric care irrespective of belonging to different occupational, educational, and other social strata. Males’ knowledge of danger signs during pregnancy (95% CI = (1.07–1.62), AOR = 1.32, P < 0.008) and postnatal care (95% CI = (1.16–1.89), AOR = 1.48, P < 0.002) had a statistically significant association with the females utilization antenatal care (ANC) service, though not delivery care (DC) or postnatal (PNC).
Conclusion
There were inequalities in obstetric danger signs knowledge between females and their male partners. Male partners’ knowledge of obstetric danger signs is not only significant during pregnancy and delivery but also has a lasting impact on post-natal service utilization, which underscores the importance of their involvement in maternal healthcare.
Keywords: sex, obstetric danger signs, knowledge, attitude, Ethiopia
Introduction
Maternal health is the health of women during the prenatal, childbirth, and postnatal period, whereas maternal morbidity refers to health conditions that complicate pregnancy, childbirth, and postnatal period; in addition, maternal mortality is described as the death of women directly related to pregnancy, childbirth, and postnatal conditions.1 The Sustainable Development Goal-3 agenda is to reach global maternal mortality less than 70 per 100,000 live births and reduce the death rate of neonates at least as low as 12 per 1000 live births.2 Therefore, Essential health services, including four-antenatal care (ANC), Skilled birth attendants (SBA), and postnatal care (PNC), are crucial for preventing complications, managing birth and postnatal issues, and reducing maternal and newborn morbidity, mortality, and stillbirths.3
Globally, male engagement in maternal health and healthcare service utilization is highly encouraged.4,5 Full participation and involvement of females and males are essential in both productive and reproductive activities, including joint responsibility for caring for and nurturing children and maintaining the household.6–8 According to the sexual and reproductive guidelines of Ethiopia, strategies of empowering the women, men, and the communities were focused on recognizing pregnancy-related risks and taking responsibility for developing and implementing appropriate to them, increasing knowledge and attitude to reduce delays in health-seeking behavior of the pregnant women, ensure utilization of maternal and neonatal health services, create a supportive environment to safe motherhood and newborn health, especially in a rural area where health facilities are limited.9
Hence, Ethiopia has shown progress in maternal health care;10 as globally, it was found fifth, next to Nigeria and Democratic Congo from Africa, in maternal death, stillbirth, and neonatal death,3 which was commonly associated with obstetric complications that occur during pregnancy, childbirth, and the postnatal period.11 Obstetric emergency danger indicators are warning signs and symptoms that women may encounter during pregnancy, childbirth, and right after delivery that could indicate a potentially fatal issue.12,13 Danger signs knowledge of maternal health care is critical in the safe motherhood initiative.14,15 The leading cause of maternal mortality in Sub-Saharan Africa (SSA) was direct obstetric complications, mainly hemorrhage, infection (maternal sepsis), hypertensive disorder, and obstructed labor.16
Studies in Africa indicated that knowledge of women’s obstetric danger signs was low.14,17–19 The most frequently mentioned danger signs during pregnancy were: vaginal bleeding, severe headache and fever at birth, including: vaginal bleeding, prolonged labor, and severe abdominal pain.18 However, some studies identified vaginal bleeding as a pregnancy danger sign; a study in Nigeria identified danger signs during the intrapartum period were severe vaginal bleeding, seizures, and loss of consciousness, as well as in the postnatal period, severe bleeding, seizures, and high-grade fever.20
Moreover, factors associated with danger sign knowledge were women with higher income and education, age, and occupation,17,18,21 those with functional radio,22 and exposure to media.23,24 In studies in Oromia, Ethiopia, pregnancy-related vaginal bleeding followed by severe headache was the most identified obstetric danger sign by men.25 A study in Nigeria indicated that females are more likely to perceive danger sign risk than males.20 In Tanzania, men’s ability to identify at least one danger sign was higher during pregnancy, 53%, than during delivery, 43.9%, and postnatal, 34.6%.11 Although antenatal care service utilization and institutional delivery have also been associated with good knowledge of obstetric danger signs.14,19 In southern Ethiopia, pregnant women know at least two danger signs: 30.4% during pregnancy, 41.3% during childbirth, and 37.7% in postnatal care,26 which is nearly similar in Oromia, Goba, 31.9% during pregnancy, 27% during childbirth and 22.1% in postnatal.27 In Eastern Ethiopia, Somali women’s danger sign knowledge in the continuum of maternal health care was collectively 15.5%.28
This study aimed to compare knowledge and attitudes towards obstetric danger signs and care between females with maternal care and their male partners because knowledge of obstetric danger signs studies have been conducted commonly among pregnant women, irrespective of sex considerations in all maternal care. Therefore, quantified knowledge and attitude of danger sign knowledge and maternal health care, in addition to the qualitative understanding of the roles and perceptions of females and males in maternal health care, will play a substantial role in achieving maternal health or safe motherhood initiatives. In Ethiopia, the health extension programme (HEP) enrolled at the community level as well as the intervention phase of the Innovative Maternal and Child Health Care in Africa (IMCHA) Safe Motherhood project as part of the study aimed at delivering maternal health care information and education, both for females and their male partner. However, this study only focuses on the baseline data as a comparative study of danger sign knowledge and attitude toward maternal health care and its effect on maternal health care service utilization.
Methods and Materials
Study Design, Period and Setting
A comparative cross-sectional study was carried out in the Jimma Zone of the Oromia region in Ethiopia between October 2016 and January 2017. Jimma Zone is situated in the Southwest, 352 km from Addis Ababa, the capital city of Ethiopia. The Zone comprises 21 districts, 42 urban, and 512 rural kebeles.29 According to reports from the Oromia Regional Health Bureau, the coverage of maternal health services utilization in the Jimma zone is as follows: 35.6% for ANC before the 16th week of pregnancy, 40.3% for skilled birth attendants (SBA) excluding cesarean section, and 37.6% for PNC within the first seven days.30
Study Population
The study population included all randomly selected index women who gave live birth, stillbirth, and abortion before data collection and their partners. During the analysis, women who did not have partners were excluded and made paired matches at the household level.
Variables
Dependent variables in the study were obstetric knowledge of danger signs during pregnancy, delivery, and the first 48 hours of postnatal time, as well as attitudes toward maternal care. Independent variables for danger sign knowledge and maternal service utilizations in the continuum of maternal healthcare included age, sex, education, occupation, annual income, literacy level (socio-demographic variables), time to health facility, and health facility evaluation (perceived accessibility and quality of services), having their mobile and listening to the radio (access to resources and exposure to media).
Sample Size and Sampling Procedure
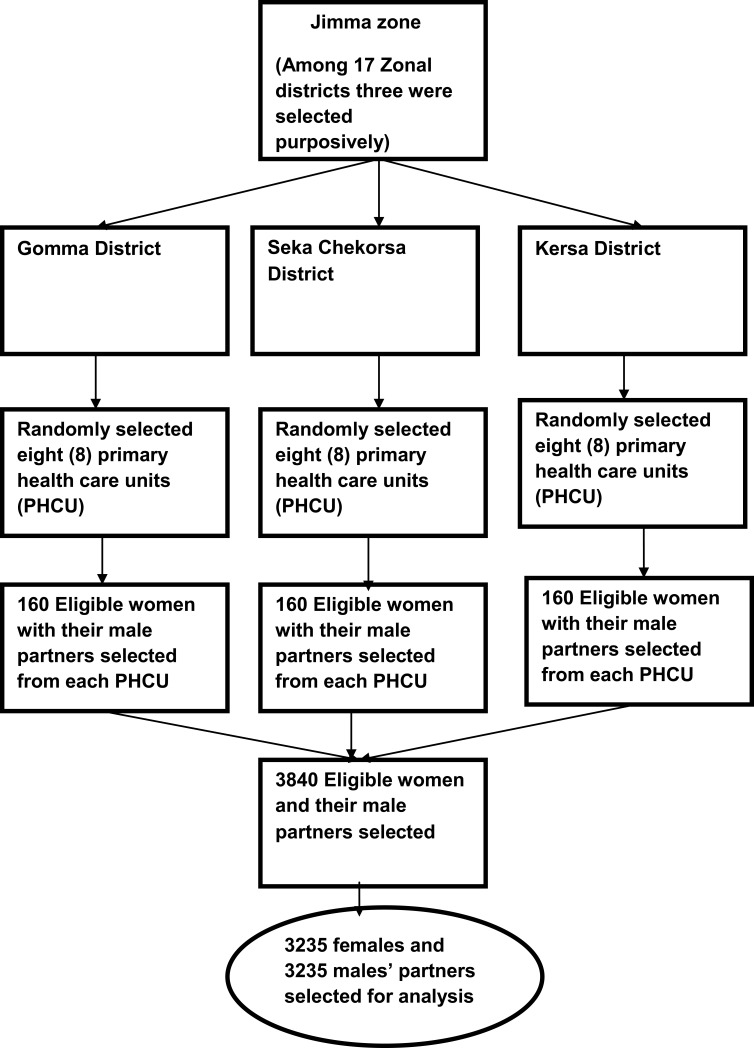
The survey was conducted targeting a total of 3840 index women and equivalent number of their partners. The selection was conducted from three rural districts, Gomma, Seka Chekorsa, and Kersa, guided by the Jimma zonal health bureau. A total of 24 primary healthcare units (PHCU) were chosen. Eight primary healthcare units were chosen randomly from each district. Then, from each selected primary healthcare unit, 160 eligible index women (who had pregnancy outcomes of live birth, stillbirth, miscarriage, and abortion) with their partners were chosen randomly from the registered health post by the health extension workers; resulting in a final sample size of 3840. The response rate of index women initially was 3784 (98.5%), while the response rate of partners was 3255 (84.7%); this suggests that some husbands may have died or separated. However, 3235 index women and their partners who participated in the study were identified and included in the analysis. The rest of the participants were excluded from the analysis due to only one partners was involved in the study (Figure 1).
Figure 1.
Schematic presentation of participants’ selection in Jimma rural Zonal district.
Data Collection Tool and Procedure
The structured interview questioners were adopted and adapted after reviewing relevant literature in the local socio-cultural context. First, the tool was prepared in English and then translated into the local language, Oromiffa, and back-translated into English by language experts in both languages. The tool comprises four significant parts: socio-demographic, danger sign knowledge, attitude towards maternal health services, and maternal health care service utilization. The tool was pre-tested with 5% of the sample size outside and adjacent to the actual study area, and substantial amendments were made to make it plausible to the interviewer and the respondents.
Data Collection Method
Qualified and experienced male and female interviewers have been used for the face-to-face data collection method. The interview schedules programmed into Open Data Kit (ODK) software were loaded onto tablets, and data was collected. An index woman was not available for two subsequent scheduled visits and was replaced by another eligible woman living next to the household who fulfilled the inclusion criteria. However, when male partners were not available, the basic socio-demographic information was obtained from the wives.
Data Sources
As part of the Innovative Maternal and Child Health in Africa (IMCHA) project, data was collected from three rural districts in the Jimma Zone. The project aimed to improve maternal and child health through two interventions: 1) providing information, education, and communication (IEC) on maternal health care for women and men’s health development army, who acted as messengers to the target audience and health extension workers, and 2) improving maternal waiting areas with necessary equipment. This study was based on the baseline data.
Measurements
The measurement tools we used to assess knowledge were based on the participants spontaneously mentioning the true obstetric danger signs without being asked the sign by name. The knowledge was categorized into two for each pregnancy, childbirth, and postnatal danger signs: (1) good obstetric danger sign knowledge if they mentioned more than two major danger signs during pregnancy, child birth and postnatal care (2) otherwise categorized as poor obstetric danger sign knowledge.14 Regarding maternal health care service attitudes, ten items with three categories each, such as agree (1), no opinion (2), and disagree (3) were used, hence summed up after reverse coding of the negative items and categorized into positive attitude for those scored less than or equal to the mean and negative attitude for those scored greater than the mean.
Data Quality Assurance
Data quality was given utmost importance right from the beginning of item development. We carefully recruited qualified data collectors and supervisors with a first-degree or above qualification. Some of them were even Ph.D. candidates. They underwent rigorous theoretical and practical training, which included learning how to use tablets and GPS devices to collect data in the field. Once the data was collected, each data collector automatically sent it to a secure server, which the principal investigator authorized to maintain confidentiality.
Data Analysis
The data were meticulously analyzed using the widely recognized Statistical Package for Social Sciences (SPSS) version 20. This tool was instrumental in providing descriptive statistics that summarized the frequency and percentage of each primary and predictor variable. For knowledge of danger signs, all participants were asked to identify any danger signs they knew during pregnancy, childbirth, and the postnatal period. The most commonly identified danger signs by participants were considered for further analysis, while some rarely identified danger signs during childbirth were also noted by both participants (Table S1).
In order to assess the participants’ knowledge of danger signs during pregnancy, childbirth, and postnatal care, they were coded as either (0) if not identified or (1) if identified. The total count of identified danger signs for each category was recorded, and new variables were created; those who identified at least two danger signs in each category were coded as one (1), indicating good danger signs knowledge, and those who identified less than two were coded as zero (0), representing poor danger sign knowledge.28,31 Regarding attitudes towards obstetric maternal care, ten items with three categories: agree, no opinion, and disagree, first reverse coding of the negative items, then the items were summed up and categorized into positive attitudes when less than the mean and coded as one (1) and negative attitude when greater than the mean coded as zero (0). Furthermore, knowledge of danger signs as a predictor variable was used to determine the utilization of maternal health care in the continuum. The analysis also considered antenatal service utilization during the last pregnancy, place of delivery in the last pregnancy, and postnatal care within the first 48 hours of delivery to determine attitudes toward maternal care. Chi-square and multivariate logistic regression analyses determined the relationship and associations between dependent and explanatory variables for obstetric danger signs and attitudes toward maternal care. Variables with a p-value of less than 0.25 in bivariate analysis were considered for multivariable analysis. The final predictors were declared with statistically significance values with 95% confidence interval, adjusted odds ratio (AOR), and a p-value of less than 0.05 (Table S2; Supplementary Materials Bivariate regression analysis).
Ethical Consideration
The willingness of the potential respondents was obtained through written informed consent. The aim of the study was told by the data collectors and invited to participate with their willing consent. A face-to-face interview data collection method was employed; the participants’ names were not mentioned in the study to ensure confidentiality and anonymity; all the issues above were acceptable and approved by Jimma University Research Ethics Institutional Review Board based on compliance with the ethical principles of the Declaration of Helsinki (Reference No RPGE/449/2016).
Result
Background Characteristics of the Participants
Most participants were between the age category of 26–30 years, with a mean age of 27.7 ± 6 for females and 36.7 ± 8 for males. Of the total participants, 3046 (94.2%) female and 3033 (93.8%) male were Oromo in ethnicity. In addition, 55.6% of females and 43.7% of males had no education, but at least 47.8% of males had completed primary education, which was more than the female participants. About an equal proportion of men and women reported that they have taken less than 30 minutes to reach the health facilities, and a large proportion of both sexes rated maternal health services as poor. Only a few women, 184 (5.7%), had their mobile phones. However, more than half of males have mobile phones (Table 1).
Table 1.
Background Characteristics of the Study Participants in Rural Jimma, Ethiopia
| Variables | Category | Female | Male | ||
|---|---|---|---|---|---|
| Frequency | % | Frequency | % | ||
| Age | 15–25 | 1276 | 40.6 | 262 | 8.3 |
| 26–35 | 1514 | 48.3 | 1388 | 43.7 | |
| 36–49 (45) | 350 | 11.1 | 1125 | 35.4 | |
| ≥46 | 399 | 12.6 | |||
| Total | 3140 | 100 | 3174 | 100 | |
| Ethnicity | Oromo | 3046 | 94.2 | 3033 | 93.8 |
| Amhara | 57 | 1.8 | 56 | 1.7 | |
| yem | 51 | 1.6 | 58 | 1.8 | |
| Dawro | 23 | 0.7 | 24 | 0.7 | |
| Kefa | 28 | 0.9 | 28 | 0.9 | |
| Other | 30 | 0.9 | 36 | 1.1 | |
| Total | 3235 | 100 | 3235 | 100 | |
| Education | No education | 1800 | 55.6 | 1413 | 43.7 |
| Primary | 1279 | 39.5 | 1546 | 47.8 | |
| Secondary | 134 | 4.1 | 230 | 7.1 | |
| Higher | 22 | 0.7 | 46 | 1.4 | |
| Total | 3235 | 100 | 3235 | 100 | |
| Occupation | House wife | 2536 | 78.4 | ||
| Farmer | 483 | 14.9 | 2749 | 85.0 | |
| Merchant | 193 | 6.0 | 453 | 14.0 | |
| Government | 23 | 0.7 | 33 | 1.0 | |
| Total | 3235 | 100 | 3235 | 100 | |
| Annual Income | ≥10,000 | 2266 | 70.0 | 2266 | 70.0 |
| 10,001–20,000 | 590 | 18.2 | 590 | 18.2 | |
| 20,001–30,000 | 119 | 3.7 | 119 | 3.7 | |
| ≥31.000 | 260 | 8.0 | 260 | 8.0 | |
| Total | 3235 | 100 | 3235 | 100 | |
| Literacy level | Able to read whole | 714 | 22.0 | 1117 | 34.5 |
| Able to read part | 387 | 12/0 | 611 | 18.9 | |
| Cannot read all | 2134 | 66.0 | 1507 | 46.6 | |
| Total | 3235 | 100 | 3235 | 100 | |
| Time to health facility | <=30 minutes | 2467 | 79.6 | 2496 | 80.5 |
| ≥30 minutes | 633 | 20.4 | 605 | 19.5 | |
| Total | 3100 | 100 | 3101 | 100 | |
| Health facility evaluation | Good | 589 | 19.0 | 770 | 24.8 |
| Not good | 2511 | 81.0 | 2331 | 75.2 | |
| Total | 3100 | 100 | 3101 | 100 | |
| Own mobile | Yes | 184 | 5.7 | 1724 | 53.3 |
| No | 3051 | 94.3 | 1511 | 46.7 | |
| Total | 3235 | 100 | 3235 | 100 | |
| Listening radio | Not at all | 1447 | 44.7 | 907 | 28.0 |
| Once/week | 878 | 27.1 | 918 | 28.4 | |
| More than one/week | 910 | 28.1 | 1410 | 43.6 | |
| Total | 3235 | 100 | 3235 | 100 | |
Notes: NB: 36–49(45); 49 in the age category indicate the maximum age of female and 45 is the age category of men in the cell.
Sex-Disparities in Knowledge of Danger Signs During Pregnancy, Delivery, and Postnatal Period
The top three danger signs during pregnancy were severe weakness, severe headache, and vomiting, most frequently reported by women and men (Table 2). Specifically, 40.7% of women and 44.5% of men identified severe weakness as a danger sign. In comparison, severe headache was reported by 37.3% of women and 32.0% of men, and vomiting was reported by 46.3% of women and 35.5% of men. On the other hand, the least frequently mentioned danger sign by both women and men was the water break or Pre-Rupture of Membrane (PROM), with only 3.4% of women and 2.9% of men reporting it.
Table 2.
Sex-Disparity Obstetrics Danger Signs Knowledge in Maternal Health Care
| Danger Signs | Female | Male | ||
|---|---|---|---|---|
| Yes (3235) | (%) | Yes (3235) | % | |
| Obstetric danger sign knowledge during pregnancy | ||||
| Sever weakness | 1318 | 40.7 | 1438 | 44.5 |
| Vomiting | 1205 | 46.3 | 957 | 29.6 |
| Headache | 1206 | 37.3 | 1036 | 32.0 |
| Abdominal problem/Distention | 852 | 26.3 | 958 | 29.6 |
| Blurred vision | 888 | 27.4 | 713 | 22.0 |
| Bleeding | 742 | 22.9 | 617 | 19.1 |
| Swelling | 322 | 10.0 | 339 | 10.5 |
| Fetal movement problem | 241 | 7.4 | 225 | 7.0 |
| Fit (convulsion) | 199 | 6.2 | 213 | 6.6 |
| Difficulty of breathing | 134 | 4.1 | 163 | 5.0 |
| Faint | 141 | 4.4 | 187 | 5.8 |
| Water break (PROM) | 111 | 3.4 | 95 | 2.9 |
| Fever | 354 | 10.9 | 274 | 8.5 |
| Obstetric danger sign knowledge during childbirth | ||||
| Labour >12 h | 2319 | 72.1 | 1980 | 61.2 |
| Vaginal bleeding | 1555 | 48.1 | 1387 | 42.9 |
| Placenta not delivered 30 min after birth | 1051 | 32.5 | 1025 | 31.7 |
| Severe headache | 498 | 18.8 | 398 | 14.6 |
| Loss of consciousness | 248 | 7.7 | 240 | 7.4 |
| Blurred vision | 258 | 8.0 | 228 | 7.0 |
| Fit (Convulsion) | 217 | 6.7 | 295 | 9.1 |
| High fever | 196 | 6.1 | 183 | 5.7 |
| Obstetric danger sign knowledge during postnatal | ||||
| Vaginal bleeding | 1356 | 41.9 | 1088 | 33.6 |
| Offensive vaginal discharge | 188 | 5.8 | 300 | 9.3 |
| Sever weakness | 769 | 23.8 | 809 | 25.0 |
| Fever | 208 | 6.4 | 195 | 6.0 |
| Severe headache | 498 | 15.4 | 367 | 11.3 |
| Body swelling | 213 | 6.6 | 162 | 5.0 |
| Fit/convulsion | 220 | 6.8 | 87 | 2.7 |
| Difficulty of breathing | 153 | 4.7 | 134 | 4.1 |
During labor and delivery, the three most frequently identified obstetric danger signs by both men and women were as follows: labor lasting more than twelve hours (women 72.1%, men 61.2%), followed by vaginal bleeding (women 48.1%, men 42.9%), and failure of the placenta to be expelled within 30 minutes (women 32.5%, men 31.7%).
In the postnatal period, vaginal bleeding was the most commonly identified danger sign, reported by 70.2% of women and 56.7% of men, followed by severe weakness, reported by 39.8% of women and 42.1% of men.
Knowledge of Obstetric Danger Signs During the Maternal Health Care
The chi-square analysis of the data found that sex has a statistically significant impact on the level of knowledge about danger signs. According to the study, women during pregnancy, delivery, and postnatal care have significantly better knowledge about danger signs than men, with X2(1, 3235) = 27.70, p < 0.001, X2(1, 3235) = 4.58, p < 0.032, and X2(1, 3235) = 5.91, p < 0.015, respectively.
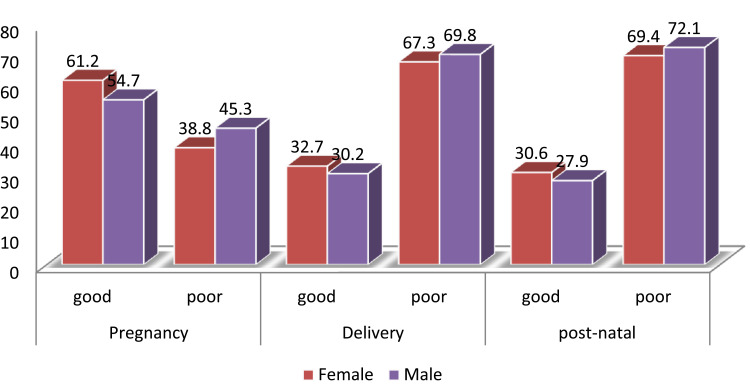
(Figure 2) illustrates that women had a better understanding of at least two danger signs during pregnancy (61.2%), labor and delivery (32.7%), and postnatal (30.6%) compared to their male partners who knew danger signs during pregnancy (54.7%), labor and delivery (30.2%), and postnatal (27.9%). However, both men and women had good knowledge of danger signs during pregnancy compared to delivery and postnatal.
Figure 2.
Percentage of sex-disparity obstetric danger signs knowledge in the continuum of maternal health care (sample for female=3235 and sample for male=3235).
Multivariate Analysis of Attitude Towards Maternal Healthcare
The study found that 48.0% of women and 49.8% of men have positive attitudes towards maternal health care. In the bivariate analysis, sex has no statistically significant association with attitude toward maternal health care. Variables significantly associated with the bivariate analysis were inserted together to control the confounding effect in the multivariate analysis.Eight variables for women and six variables for men were found to be significantly associated with positive attitude of maternal health care. The characteristics of women who had positive attitude were literate, p < 0.005, had good knowledge of obstetrics danger signs during pregnancy p < 0.001, postnatal care p < 0.001 and received antenatal care during the last pregnancy p < 0.001 (Table 3).
Table 3.
Sex Disparity Multivariate Analysis of Attitude on Maternal Health Care
| Sex | Variables Category | Maternal Health Care Attitude | AOR | (95% CI) | |
|---|---|---|---|---|---|
| Positive | Negative | ||||
| Male occupation | Farmer | 1393 | 1356 | ||
| Trader | 199 | 254 | |||
| Govn’t | 20 | 13 | |||
| Female occupation | House wife | 1203 | 1333 | 1 | 1 |
| Farmer | 276 | 207 | 1.32 | (1.05–1.65)* | |
| Trader | 69 | 124 | 0.77 | (0.56–1.08) | |
| Govn’t | 6 | 17 | 0.80 | (0.30–2.15) | |
| Male HH annual income | <=10,000 | 1122 | 1144 | 1 | 1 |
| 10,001–20,000 | 285 | 305 | 0.97 | (0.80–1.17) | |
| 20,001–30,000 | 47 | 72 | 0.69 | (0.46–1.04) | |
| ≥30,001 | 158 | 102 | 1.69 | (1.28–2.23)** | |
| Female annual income | <=10,000 | 1100 | 1166 | ||
| 10,001–20,000 | 261 | 329 | |||
| 20,001–30,000 | 56 | 63 | |||
| ≥30,001 | 137 | 123 | |||
| Literacy level of male | Not read all | 1011 | 496 | ||
| Read partly | 389 | 222 | |||
| Read all | 855 | 262 | |||
| Literacy level of female | Not read all | 1460 | 674 | 1 | 1 |
| Read partly | 274 | 113 | 0.51 | (0.40–0.64)** | |
| Read all | 584 | 130 | 0.93 | (0.72–1.21) | |
| Time to health facility by male | <=30min | 1197 | 1299 | 1 | 1 |
| ≥31min | 333 | 272 | 1.28 | (1.06–1.55)* | |
| Time taken to health facility by female | <=30min | 1124 | 1343 | 1 | 1 |
| ≥31min | 343 | 290 | 1.23 | (1.01–1.48)* | |
| Male listen radio | Not at all | 667 | 240 | 1 | 1 |
| Once per week | 612 | 305 | 1.30 | (1.06–1.58)* | |
| More than once per week | 1039 | 371 | 1.14 | (0.95–1.37) | |
| Female listen radio | Not at all | 1045 | 402 | 1 | 1 |
| Once per week | 592 | 286 | 1.34 | (1.11–1.62)** | |
| More than once per week | 681 | 229 | 1.15 | (0.95–1.39) | |
| Male health facility evaluative | Not good | 1058 | 1273 | 1 | 1 |
| Good | 472 | 298 | 1.93 | (1.63–2.29)** | |
| Female health facility evaluative | Not good | 1102 | 1409 | 1 | 1 |
| Good | 365 | 224 | 1.99 | (1.63–2.42)** | |
| Male danger sign knowledge during pregnancy | Poor | 743 | 722 | ||
| Good | 869 | 901 | |||
| Female danger sign knowledge during pregnancy | Poor | 661 | 595 | 1 | 1 |
| Good | 893 | 1086 | 0.75 | (0.63–0.89)* | |
| Male danger sign knowledge during labor | Poor | 1104 | 1153 | 1 | 1 |
| Good | 508 | 470 | 1.25 | (1.06–1.48)* | |
| Female danger sign knowledge during labor | Poor | 1034 | 1143 | 1 | 1 |
| Good | 520 | 538 | 1.26 | (1.06–1.49)* | |
| Male danger sign knowledge during postnatal | Poor | 1223 | 1110 | 1 | 1 |
| Good | 389 | 513 | 0.70 | (0.59–0.83)** | |
| Female danger sign knowledge during postnatal | Poor | 1171 | 1073 | 1 | 1 |
| Good | 383 | 608 | 0.63 | (0.53–0.75)** | |
| ANC last pregnancy | No | 322 | 150 | 1 | 1 |
| Yes | 1232 | 1531 | 0.66 | (0.52–0.83)** | |
| Place of delivery | Home | 702 | 1008 | 1 | 1 |
| Health facility | 852 | 673 | 1.81 | (1.54–2.13)** | |
| Postnatal first 2 hours | No | 1056 | 906 | 1 | 1 |
| Yes | 498 | 775 | 0.63 | (0.53–0.75)** | |
Note: *P<0.05, **P<0.02.
The women who evaluated the maternal health care services as good P < 0.001, women listened to radio at least once per week p < 0.001, were farmer p < 0.014, perceived time taken to health facility more than thirty minutes p < 0.031, good danger sign knowledge during delivery p < 0.008, and who gave birth in the health p < 0.001 had more likely developed positive attitude towards maternal health care (Table 3).
Men in multivariate analysis who able to read partially p < 0.032, good danger sign knowledge during the postnatal period p < 0.001 had more likely reduced positive attitude towards maternal health care. However, men who evaluated the health facility as good p < 0.001 listen radio at least one per week p < 0.009, perceived the time taken to the health facility to be more than thirty minutes p < 0.008, annual income more than 30,000 Ethiopia birr (ETB) p < 0.000 had more likely develop positive attitude towards the maternal health care (Table 3).
Predictors of Female Obstetric Danger Signs Knowledge During Pregnancy, Childbirth, and Postnatal Period
In the multivariate logistic regression analysis, women’s age between 26 and 35 P < 0.004), completed secondary education P <0.004, being farmer P < 0.001, became government employee P < 0.048), annual income above 10,000 ETB P <0.001, own mobile phone P < 0.001, able to read partly P < 0.038, listened to the radio once P <0.001 and more than once per week P < 0.027, and evaluated positively the maternal health care P < 0.001 had statistically significance association with good knowledge of obstetric danger signs during pregnancy.
Women’s during childbirth, age between 26 and 35 years P< 0.005 completed primary education P < 0.004 or secondary education P <0.013, being farmer P < 0.001 and merchant P <0.003, annual income between 10,000 and 20,000ETB P < 0.047, between 20,001 and 30,000ETB P < 0.004, and above 30,001ETB P < 0.001, own mobile phone P < 0.019, listened to the radio at least once or more per week P < 0.001, and evaluated positively the maternal health facility P < 0.001 had statistically significance association with good knowledge of obstetric danger signs during childbirth (Table 4).
Table 4.
Multivariate Logistic Regression of Obstetric Danger Signs Knowledge in Maternal Health Care
| Variable Category | Danger Sign Knowledge During Pregnancy | AOR,(95% CI) P-value | Danger Sign Knowledge During Delivery | AOR,(95% CI), P-value | Danger Sign Knowledge During Postnatal | AOR, (95% CI) P-value | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Poor | Good | Poor | Good | Poor | Good | |||||
| Male age | 15–25 | 133 | 129 | 196 | 66 | 189 | 73 | |||
| 26–35 | 604 | 784 | 959 | 429 | 973 | 415 | ||||
| 36–45 | 515 | 609 | 792 | 333 | 841 | 284 | ||||
| ≥46 | 189 | 210 | 273 | 126 | 274 | 125 | ||||
| Female age | 15–25 | 529 | 747 | 1 | 881 | 395 | 1 | 898 | 378 | |
| 26–35 | 558 | 956 | 1.27(1.07–1.51)** 0.005 | 995 | 519 | 1.30(1.09–1.57)*.004 | 1037 | 477 | ||
| 36–49 | 123 | 222 | 1.31(1.00–1.71)*.045 | 237 | 113 | 1.09(0,83–1.45)) | 240 | 110 | ||
| Male education | No education | 691 | 722 | 1 | 1039 | 374 | 1 | 1082 | 331 | 1 |
| Primary | 680 | 866 | 1.11(0.95–1.31) | 1051 | 495 | 1.35(1.02–1.79)*.035 | 1091 | 455 | 1.30(1.10–1.55)***.002 | |
| Secondary | 84 | 146 | 1.47(1.07–2.00)*.015 | 143 | 87 | 2.00(1.33–3.01)*.001 | 138 | 92 | 2.06(1.52–2.79)***.000 | |
| Higher | 10 | 36 | 2.93(1.39–6.17)**.004 | 24 | 22 | 2.74(1.38–5.40)**004 | 22 | 24 | 3.18(1.74–5.81)***.000 | |
| Female education | No education | 719 | 1080 | 1261 | 539 | 1 | 1279 | 521 | ||
| Primary | 484 | 795 | 826 | 453 | 1.31(1.09–1.57)**.003 | 862 | 417 | |||
| Secondary | 47 | 87 | 79 | 55 | 1.66(1.11–2.48)*.013 | 92 | 42 | |||
| Higher | 6 | 15 | 11 | 11 | 1.90(0.56–6.40) | 11 | 11 | |||
| Male occupation | Farmer | 1268 | 1481 | 1939 | 810 | 1983 | 766 | |||
| Trader | 185 | 268 | 296 | 157 | 323 | 130 | ||||
| Government | 12 | 21 | 22 | 11 | 27 | 6 | ||||
| Female occupation | House wife | 1031 | 1505 | 1 | 1773 | 763 | 1 | 1807 | 729 | 1 |
| Farmer | 153 | 330 | 1.75 (1.38–2.21)***.000 | 278 | 205 | 2.10(1.68–2.63)***.000 | 314 | 169 | 1.40(1.12–1.75)**.003 | |
| Trader | 68 | 125 | 1.30(0.93–1.81) | 115 | 78 | 1.62(1.18–2.23)**.003 | 113 | 80 | 1.71(1.25–2.35)***.001 | |
| Gover’t | 4 | 19 | 3.16(1.01–9.86)*.048 | 11 | 12 | 2.29(0.71–7.37) | 10 | 13 | 3.29(1.32–8.17)**.010 | |
| Male HH Annual income | <=10,000 | 1043 | 1223 | 1 | 1591 | 675 | 1 | 1645 | 621 | |
| 10,001–20,000 | 242 | 348 | 1.12(0.92–1.36) | 399 | 191 | 1.03(0.84–1.27) | 411 | 179 | ||
| 20,001–30,000 | 33 | 86 | 1.77(1.16–2.70)*.008 | 71 | 48 | 1.39(0.93–2.08) | 79 | 40 | ||
| ≥30,001 | 147 | 113 | 0.56(0.43–0.74)*.000 | 196 | 64 | 0.67(0.49–0.92)*.015 | 198 | 62 | ||
| Female annual income | <=10,000 | 941 | 1325 | 1 | 1551 | 715 | 1 | 1586 | 680 | 1 |
| 10,001–20,000 | 160 | 430 | 1.73(1.40–2.14)***.000 | 368 | 222 | 1.22(1.00–1.49)**.047 | 379 | 211 | 1.31(1.07–1.50)**.007 | |
| 20,001–30,000 | 26 | 93 | 2.23(1.40–3.54)**.001 | 61 | 58 | 1.79(1.20–2.65)**.004 | 71 | 48 | 1.42(0.95–2.22) | |
| ≥30,001 | 129 | 131 | 0.68(0.51–0.90)*.007 | 197 | 63 | 0.58(0.42–0.81)*.001 | 208 | 52 | 0.53(0.38–0.75)***.001 | |
| Male own mobile | No | 743 | 768 | 1 | 1095 | 416 | 1134 | 377 | ||
| Yes | 722 | 1002 | 1.17(1.00–1.38)*.048 | 1162 | 562 | 1199 | 525 | |||
| Female own mobile | No | 1175 | 1876 | 1 | 2050 | 1001 | 1 | 2112 | 939 | 1 |
| Yes | 81 | 103 | 0.57(0.40–0.80)**.001 | 127 | 57 | 0.64(0.44–0.92)*.019 | 132 | 52 | 0.66(0.46–0.95*.029) | |
| Literacy level of male | Not read all | 723 | 784 | 1093 | 414 | 1151 | 356 | |||
| Read partly | 256 | 355 | 398 | 213 | 443 | 168 | ||||
| Read all | 486 | 631 | 766 | 351 | 739 | 378 | ||||
| Literacy level of female | Not read all | 861 | 1273 | 1 | 1488 | 646 | 1516 | 618 | 1 | |
| Read partly | 146 | 241 | 1.35(1.01–1.79)*.038 | 238 | 149 | 273 | 114 | 1.32(1.08–1.61)*.006 | ||
| Read all | 249 | 465 | 1.16(0.85–1.57) | 451 | 263 | 455 | 259 | 1.01(0.79–1.31) | ||
| Time to health facility/ Male | <=30min | 1129 | 1367 | 1740 | 756 | 1771 | 725 | |||
| ≥31min | 277 | 328 | 425 | 180 | 457 | 148 | ||||
| Time to reach to health facility/ Female | <=30min | 929 | 1538 | 1646 | 821 | 1658 | 809 | 1 | ||
| ≥31min | 250 | 383 | 437 | 196 | 478 | 155 | 0.68(0.55–0.83)***.000 | |||
| Listen radio/Male | Not at all | 393 | 514 | 1 | 658 | 249 | 1 | 672 | 235 | 1 |
| Once per week | 326 | 591 | 1.36(1.12–1.65)**.002 | 579 | 338 | 1.58(1.27–1.96)***.000 | 601 | 316 | 1.50(1.20–1.86)***.000 | |
| More than once per week | 536 | 874 | 1.23(1.02–1.48)*.029 | 939 | 471 | 1.45(1.18–1.78)**.003 | 970 | 440 | 1.17(0.95–1.43) | |
| Listen radio/Female | Not at all | 642 | 805 | 1 | 1059 | 388 | 1 | 1041 | 406 | 1 |
| Once per week | 288 | 590 | 1.61(1.33–1.94)***.000 | 546 | 332 | 1.62(1.34–1.97)***.000 | 558 | 320 | 1.40(1.15–1.69)**.001 | |
| More than once per week | 326 | 584 | 1.24(1.02–1.50)*.027 | 572 | 338 | 1.41(1.16–1.72)***.000 | 645 | 265 | 0.88(0.72–1.08) | |
| Health facility evaluative/Male | Not good | 1090 | 1241 | 1 | 1646 | 685 | 1670 | 661 | ||
| Good | 316 | 454 | 1.24(1.05–1.47)*.010 | 519 | 251 | 558 | 212 | |||
| Health facility evaluative/Female | Not good | 1013 | 1498 | 1 | 1746 | 765 | 1 | 1738 | 773 | |
| Good | 166 | 423 | 1.67(1.36–2.05)**.001 | 337 | 252 | 1.75(1.44–2.12)***.000 | 398 | 191 | ||
Note: *P<0.05, **P<0.02, ***P<0.01.
In the postnatal period, women became farmer P < 0.003, merchants P < 0.001, government employees P < 0.010; annual income above 10,000 ETB P < 0.007), own mobile phone P < 0.029; able to P < 0.006; listened to the radio once per week P < 0.001); and perceived time to reach the health facility more than thirty minutes P < 0.001 had significantly associated with good knowledge of obstetric danger signs during postnatal care (Table 4).
Predictors of Male Obstetric Danger Signs Knowledge During Pregnancy, Childbirth, and Postnatal Period
In the multivariate logistic regression analysis, men who had an educational status of secondary level P < 0.015 or higher education P < 0.004), annual income above 20,001P < 0.008), own mobile phone P < 0.048, listened to the radio at least once per week P < 0.029, and positively evaluated of the maternal health care P < 0.010 had significance association with good knowledge of danger signs during pregnancy (Table 4).
During childbirth, men who had completed primary education P < 0.035, secondary education P < 0.001, and higher education P < 0.004, annual income above 30,001 ETB P < 0.015, listened to the radio at least once or more per week P < 0.001 had statistically association with knowledge of obstetric danger signs during labor and delivery (Table 4).
In the postnatal period, men who reached in primary education P < 0.002), secondary education P < 0.001), higher education P < 0.001, listened to the radio once per week P < 0.001 had statistically associated with good knowledge of obstetric danger signs during postnatal period (Table 4).
By merging all the obstetric care (ANC, childbirth (CB), PNC) events, we finally generated a latent variable that summarized sex disparity along the continuum of obstetric care. Accordingly, women identified an average of 2.96 (SD = 1.49) obstetric danger signs during pregnancy, but men identified an average of 2.28 (SD = 1.53) danger signs. During labor and delivery, women identified an average of 2.26 (SD = 1.10) danger signs, slightly higher than the men, 2.03 (SD = 1.24). On the other hand, women had more knowledge of obstetric danger signs 2.07 (SD = 1.34) during postnatal care than the men 2.02 (1.24) (Table 4).
Sex-Disparity Obstetric Danger Signs Knowledge and Maternal Health Care Utilizations
A large proportion of women, 2763 (85.4%), attended ANC services in the last pregnancy, of whom 1528 (47.2%) gave birth in the health institutes, and 1273 (39.4%) attended the postnatal care proceeding to the study. In the bivariate analysis, all knowledge of danger signs in the continuum of maternal health care was statistically significant in association with maternal health services. However, in multivariate analysis, women’s good knowledge of obstetric danger signs during pregnancy P < 0.001) and postnatal care P < 0.001) had statistically associated with ANC service utilization in the last pregnancy. Women with good knowledge of obstetric danger signs during pregnancy P < 0.003 had statistically associated with birth given in the health facility (Table 5).
Table 5.
Association of Obstetric Danger Sign Knowledge in the Continuum of Maternal Health Care and Maternal Health Care Service Utilization
| KNOWLEDGE | Category | Women Used ANC in Last Pregnancy N=3235 (%) | AOR (95% CI) P-value | Women Gave Birth in the Health Facility N=3235 (%) | AOR (95% CI) P-value | Women Received Postnatal care with in 48 hrs N=3235 (%) | AOR (95% CI) P-value |
|---|---|---|---|---|---|---|---|
| Female danger sign knowledge during pregnancy | Poor | 1019(36.9) | 1 | 552(36.2) | 1 | 416(32.7) | 1 |
| Good | 1744(63.1) | 1.44(1.16–1.78).001*** | 973(63.8) | 1.26(1.08–1.47).003** | 857(67.3) | 1.43(1.22–1.68).000*** | |
| Male danger sign knowledge during pregnancy | Poor | 1216(44.0) | 1 | 653(42.8) | 1 | 514(40.4) | 1 |
| Good | 1547(56.0) | 1.32(1.07–1.62).008* | 872(57.2) | 1.13(0.97–1.31).095 | 759(59.6) | 1.34(1.15–1.55).000*** | |
| Female danger sign knowledge during labor and delivery | Poor | 1827(66.1) | 1 | 1039(68.1) | 1 | 782(61.4) | 1 |
| Good | 936(33.9) | 1.19(0.94–1.50).136 | 486(31.9) | 0.86(0.73–1.00).057 | 491(38.6) | 1.41(1.21–1.65).000*** | |
| Male danger sign knowledge during labor and delivery | Poor | 1914(69.3) | 1 | 1037(68.0) | 1 | 856(67.2) | 1 |
| Good | 849(30.7) | 1.00(0.80–1.26).953 | 488(32.0) | 1.08(0.92–1.26).336 | 417(32.8) | 1.10(0.94–1.29).215 | |
| Female danger sign knowledge during postnatal care | Poor | 1865(67.5) | 1 | 1042(68.3) | 1 | 863(67.8) | 1 |
| Good | 898(32.5) | 1.67(1.29–2.15).000*** | 483(31.7) | 1.04(0.89–1.22).557 | 410(32.2) | 1.10(0.79–1.10).421 | |
| Male danger sign knowledge during postnatal care | Poor | 1958(70.9) | 1 | 1055(69.2) | 1 | 896(70.4%) | 1 |
| Good | 805(29.1) | 1.48(1.16–1.89).002** | 470(30.8) | 1.26(1.07–1.47).005** | 377(29.6) | 1.10(0.89–1.23).533 |
Note: *P<0.05, **P<0.02, ***P<0.01.
For postnatal services utilization, women’s good knowledge of danger signs during pregnancy P < 0.001 and labor and delivery P < 0.001 had statistically associated with postnatal care service utilizations. Similarly, men knowledge of danger signs during pregnancy P < 0.008 and postnatal care P < 0.002 had statistically associated with ANC service utilization in the last pregnancy. Men’s knowledge of obstetric danger signs during postnatal care P < 0.001 had statistically significant association for the women to give birth in the health institutions, men’s knowledge of obstetric danger signs knowledge during pregnancy P < 0.008 had statistically associated with postnatal service utilization (Table 5).
Discussion
Key Findings
This study’s discussion was centered on a comparative analysis of females and their male partners. The aim was to underscore the significant sex differences in knowledge and attitude towards obstetric danger signs and care. This comparison was particularly insightful, highlighting the unique perspectives and understanding of females receiving maternal care and their respective male partners. The profound implications of these sex differences in maternal health care underscore the importance of our findings.
The data suggested that, on average, at least two danger signs were identified by male and female participants in maternal health care. Females could mention more danger signs than males in every maternal health care (pregnancy, delivery, and postnatal). The analysis also identified that females are more knowledgeable and have statistically associated with knowledge of obstetric danger signs than male participants. Both participants identified the top three danger signs in every maternal health care, although the numbers of females were more than that of males. The data also identified that knowledge of obstetric danger signs during pregnancy was higher in both participants than during childbirth and postnatal care. The finding underscores the crucial role of women in maternal care and their heightened knowledge of danger signs.
In the logistic regression analysis during pregnancy, knowledge of danger signs was statistically associated with females’ age, males’ education, females’ occupation, males’ and females’ annual income, having their mobile phones in both sexes, females’ literacy level, and frequency of listened to radio in both sexes and health facility evaluation. During childbirth, knowledge of danger signs was associated with women’s age, occupation, mobile owner, health facility evaluation, and occupation. In addition, education, annual income, and frequency of listening to the radio were associated with both sexes. Postnatal knowledge of danger signs was associated with male education, female occupation, annual income, mobile owner, literacy level, perception of time to reach health facilities, and frequency of listening to the radio in both sexes.
Danger signs knowledge of females during pregnancy has a statistical association with all maternal health care in the continuum. However, male knowledge of danger signs was not associated with women’s institutional delivery. The study also suggests that only females’ danger sign knowledge during delivery as a predictor of postnatal care service utilization, female and male postnatal danger signs knowledge, and male danger signs knowledge during postnatal were statistically significant predictors for the women’s ANC utilization and institutional delivery, respectively. In both sexes, attitude towards maternal health care was associated with time taken to reach the health facility, listening to the radio, and maternal health care evaluations, which were non-obstetric common factors in both sexes.
Sex-Disparity in Knowledge of Obstetric Danger Signs in Maternal Health Care
The study suggests that males have more than females in good danger signs knowledge during pregnancy, whereas females during delivery and postnatal periods were higher than males. These gender-based differences may be associated with male being given more attention during pregnancy, and they tend to get information while they accompany. During pregnancy, most health professionals provide obstetric health information.32 In contrast, females continue to identify and recognize unusual manifestations during and after delivery and continue maternal health communication with health professionals.
Obstetric Danger Signs Identified in the Continuum of Maternal Healthcare
As the study showed, males and females identified a nearly similar number of danger signs; the average number of danger signs identified by each of them was at least two, which was higher than for females in democratic Congo;33 however, it was going decreased from pregnancy to delivery and postnatal, and there was no significant difference among the males and females participants, this was in agreement with the study in South Mozambique.34 The two most frequently identified danger signs during pregnancy by the majority of the males and the females participants were severe weakness and headache, in which males were more knowledgeable of the former and females were the latter danger sign; males more knowledge may be associated with females involvement in the household activity commonly decreased during pregnancy and this could be easily identified by the males participants as well as males household chores increased. In contrast, the females became pregnant,32 similar to the study in Kenya,18 but not mentioned at all by the women in Ethiopia, Aleta Wendo.26 In contrast, women in Shashemene14 Angolela Tera district,35 Aleta Wondo,26 Goba,27 and men in Burayu.25 The most frequently identified danger sign was vaginal bleeding; severe headache was the second most identified danger sign by men in Burayu.25 In the current study, the danger signs during pregnancy identified by females were different from the previously conducted studies; this may be associated with intensive activity to reduce maternal mortality, might reduce the leading cause such as vaginal bleeding, and could not consider a common danger sign during pregnancy, which was supported by World Health Organization African region report in 2020, in Ethiopia maternal mortality was reduced by 33%.36 During childbirth and the postnatal period, the most frequently identified danger signs by females and male participants were labor greater than twelve hours (prolonged labor) and vaginal bleeding, respectively. However, the proportion of females was higher than the male participants in both maternal health care, despite differences in the percentage of the respondents; in many studies, there was agreement on the common danger signs identified by women during delivery and postnatal.14,22,27,28 However, that was incongruent with a study in Tanzania.11 Less than five percent of the men mentioned prolonged labor during childbirth; this may be associated with the current study area’s expanded health extension program and improved maternal health care information among females.
Knowledge of Obstetric Danger Signs in Maternal Healthcare
The spontaneous response of at least two danger signs, which was considered as good knowledge, observed in females during pregnancy (61.2%), delivery (32.7%), and postnatal (30.6%) were higher than the males during pregnancy (54.7%), delivery (30.2%), and postnatal (27.9%), this inequality may be associated with the focus of maternal health information was commonly on females. There is an increased frequency of female contact with health professionals in maternal health care and a less male-friendly maternal health care approach in the study area. The current finding is nearly similar to the systematic review study in Ethiopia; the pregnant women’s danger sign knowledge had shown a decrease in the continuum of maternal health care during pregnancy, ranging from 30% to 78%, childbirth 23%–78%, and postnatal 4%–73%.37 The study also indicates that females during pregnancy, labor and delivery, and postnatal care have a statistically significant relationship with a good danger sign knowledge than the males, X2 = (1, 2594) = 27.70. p < 0.001, X2(1, 2594) = 4.58, p < 0.032, X2(1, 2594) = 5.91, p < 0.015 respectively.
Factors Affecting Danger Sign Knowledge in the Continuum of Maternal Healthcare
In the current study, males’ age, occupation, literacy level, and time to reach the health facility were not significantly associated with knowledge of danger signs in the continuum of maternal health care. However, no variables included in the multivariate analysis were associated with female danger signs knowledge in all maternal health care.
The study suggests that in multivariate analysis during pregnancy, women over 26 years have good knowledge of danger signs, supported by the meta-analysis study in Ethiopia;37 this may be associated with an increased frequency of contact with health professionals to get more information. However, male age was not significantly associated. However, unlike females, males in secondary and higher education have 1.47 and 2.93 times more knowledge of danger signs than those without education; this was incongruent with Anglia Tera Districts in Northern Ethiopia,35 Arba Minch,38 and Meta-Analysis, women higher education and get formal education have good danger signs knowledge.37 In the current study, the number of educated females was much less than the number of uneducated, which affected its significant associations.
The analysis identified both males and females whose annual income of more than 30,000 had decreased good danger signs knowledge by 44% for males and 32% for females. The qualitative study of the same study area explained that high-income females were less interested in visiting the health facility during pregnancy, assuming they could do anything at any time if they faced health problems that might reduce to get obstetric danger signs health information from the health facilities.32 However, contradicting the Meta-Analysis study in Ethiopia,37 this may be a previous experience of the participants and their parents and the accessibility of the health facility. Female mobile phones had reduced good danger sign knowledge by 43%, whereas male mobile phones increased by 1.17 times good danger sign knowledge. This significance was associated with the number of female having mobile phones, which was much less than the male, which might increase access to health information and improve communication with the health extension workers.39 Listening to the radio at least once or more daily helped women and men to have a good knowledge of danger signs, which may be associated with the rural parts of Ethiopia. The primary media means was radio, and most government and nongovernment organizations preferred to broadcast health information to reduce maternal mortality, supported by the study in Northern Tigray and the Meta Analysis.22,37 Both female and male who evaluated the maternal health facility as good were significantly associated with danger sign knowledge; this was supported by the qualitative study in which women and men had increased interest in the health facility services according to their evaluations.
In the multivariate analysis controlling other variables during the delivery and postnatal period, the likelihood of knowledge of danger signs for men’s secondary and higher educational levels was higher than for the uneducated. Females with private and government employees had more good knowledge of danger signs, similar to a study in Goba;27 this is because the female who had an opportunity to communicate with others might have a chance to get more information on danger signs than the housewives. However, male occupations have no significant association during delivery and postnatal. A female whose annual income is above 30,000 ETB has shown reduced knowledge of danger signs, unlike the male participants, who had no significant association with knowledge of danger signs. Women whose economic condition is found to be in a better condition have shown less interest in visiting maternal health care similarly. A qualitative study of the same study area explored economically better individuals showed less interest in utilizing regular maternal health care.32 Both females and males listening to the radio at least once per day and evaluated the maternal health facility as good, the likelihood of knowing at least two danger signs increased, which is similar to the study in Ethiopia Meta-Analysis,37 female who evaluated the quality of the maternal health care, and exposed to media had a better danger sign knowledge, this may be associated with the more the quality of the health care the more it motivates the female and exposed to media have increased to get more health information to give value for themselves and their children.
Sex-Disparity Knowledge of Obstetric Danger Signs in Maternal Health Care
The current study identified danger signs knowledge during pregnancy, delivery, and postnatal as predictors of maternal health care; females and males good danger signs knowledge during pregnancy and postnatal had a statistically significant predictor of the utilization of antenatal care (ANC) services: this is consistence with Somali, Ethiopia,28 this is because, in the health belief model, perceived seriousness about the health condition increased the likelihood of an action.40 However, inconsistent with Tanzania,41 this may be a socio-cultural and intervention difference. Females’ and males’ good knowledge of danger signs during delivery had no significant association with ANC service utilization. Females during pregnancy and males during postnatal good danger signs knowledge had shown significant association to the women delivery service utilization in the health facility. However, it was both males and females during pregnancy, and only females with good danger sign knowledge during delivery had a statistically significant association with postnatal service utilization in the health facility: this may be associated with men, and partly women the danger signs during delivery were considered as part of the birth process. Nevertheless, danger signs both during pregnancy and postnatal are considered life-threatening, which leads to maternal health-seeking behavior.
This study’s strength was data collected from a large sample size, from female and male members of the same households, and from women who experienced pregnancy and delivery. However, the weakness might be recall bias, as the female participants were not pregnant at the time of the study, which would have caused the chicken or egg dilemma effect of the cross-sectional study design. Significant variations in some variable response categories might cause statistically significant associations.
Attitude Toward Maternal Health Care
In the current study, nearly 50% of men have formed positive attitudes towards maternal health care, consistent with the study conducted in Nigeria.42 Factors that commonly determine the positive attitude of men and women towards maternal health care were perceived time took more than thirty minutes (Cognitive), evaluation of the maternal health care services as good (Affective), and who listens to the radio at least once per week (Behavioral), which was consistency with the theory of attitude formation in psychological studies.43 This may be associated with the more time taken to reach the maternal health care facility, which will cost the life of the woman and the fetus; therefore, they would have developed a positive attitude. Conversely, those who perceived the health facility were near would develop the wrong perception that they would pretend to reach if any unprecedented health conditions happened they would easily reach the health facility.
Conclusion
There were inequalities in obstetric danger signs knowledge among females and their male partners. Male partners’ knowledge of obstetric danger signs is not only significant during pregnancy and delivery but also has a lasting impact on post-natal service utilization, which underscores the importance of their involvement in maternal healthcare. For the proper delivery of maternal health care services, it is crucial to identify factors that affect females and their male partner’s obstetric danger signs knowledge and maternal health service attitude. Experience of media exposure, like radio at least once per week, gives the partners a variety of obstetric danger signs knowledge, which helps to develop a positive attitude towards maternal health care services.
Acknowledgments
The authors thank the study participants for their time and efforts. We want to thank the Innovative Maternal and Child Health in Africa (IMCHA) project for supporting this study through the government of Canada’s International Development Research Center (IDRC) and Ottawa University in Canada.
Funding Statement
The Safe Motherhood Project is supported by Innovating for Maternal and Child Health in Africa Initiative grants #108028-001 (Jimma University) and #108028-002 (University of Ottawa), which are co-funded by Global Affairs Canada, the Canadian Institute for Health Research, and Canada’s International Development Research Center. This study does not reflect the views of these organizations. They solely offered financial assistance for the research’s execution, without involvement in the research process. Ensuring the information is accurate, and grant numbers are correct.
Data Sharing Statement
All relevant data are within the paper and in the supporting information file.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or all these areas; took part in drafting, revising, or critically reviewing the article; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.World Health Organization. Managing Maternal and Child Health Programmes: A Practical Guide. World Health Organization; 1997. [Google Scholar]
- 2.Stipčić A, Ćorić T, Erceg M, Mihanović F, Kolčić I, Polašek OJI. Socioeconomic inequalities show remarkably poor association with health and disease in Southern Croatia. Int J Public Health. 2015;60(4):417–426. doi: 10.1007/s00038-015-0667-x [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Improving Maternal and Newborn Health and Survival and Reducing Stillbirth: Progress Report 2023. World Health Organization; 2023. [Google Scholar]
- 4.Firoz T, McCaw‐Binns A, Filippi V, et al. A framework for healthcare interventions to address maternal morbidity. Int J Gynaecol Obstetr. 2018;141(Suppl 1):61–68. doi: 10.1002/ijgo.12469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Doyal L. Gender Equity in Health*: debates and Dilemmas. In: Gender, Health and Healing. Routledge; 2012:183–197. [Google Scholar]
- 6.World Health Organization. Trends in Maternal Mortality 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. World Health Organization; 2019. [Google Scholar]
- 7.World Health Organization. Programming for Male Involvement in Reproductive Health: Report of the Meeting of WHO Regional Advisers in Reproductive Health, WHO/PAHO, Washington DC, USA 5–7 September 2001. World Health Organization; 2002. [Google Scholar]
- 8.Speizer IS, Whittle L, Carter MJI. Gender relations and reproductive decision making in Honduras. Int Fam Plann Perspect. 2005;31(3):131–139. doi: 10.1363/3113105 [DOI] [PubMed] [Google Scholar]
- 9.Federal Democratic Repoblic of Ethiopa MoH. National Reproductive Health Strategy 2020–2016; 2016.
- 10.EPHI IJEMD, Indicators HSK. Ethiopian public health Institute (EPHI)[Ethiopia] and ICF; 2019.
- 11.August F, Pembe AB, Mpembeni R, Axemo P, EJPo D. Men’s knowledge of obstetric danger signs, birth preparedness and complication readiness in rural Tanzania. PLoS One. 2015;10(5):e0125978. doi: 10.1371/journal.pone.0125978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization. Managing Complications in Pregnancy and Childbirth: A Guide for Midwives and Doctors. World Health Organization; 2003. [Google Scholar]
- 13.Barreix M, Lawrie TA, Kidula N, et al. Development of the WHO Antenatal Care Recommendations Adaptation Toolkit: a standardised approach for countries. Health Res Policy Syst. 2020;18(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wassihun B, Negese B, Bedada H, et al. Knowledge of obstetric danger signs and associated factors: a study among mothers in Shashamane town, Oromia region, Ethiopia. Reprod Health. 2020;17:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sufiyan MB, Adam N, Umar AA, et al. Knowledge, attitude and perception of pregnancy danger signs among women of childbearing age in samaru community northwestern Nigeria: results from a cross-sectional survey. Arch Med Surg. 2016;1(2):24. [Google Scholar]
- 16.Musarandega R, Nyakura M, Machekano R, Pattinson R; Munjanja SPJJo GH. Causes of maternal mortality in Sub-Saharan Africa: a systematic review of studies published from 2015 to 2020. J Glob Health. 2021:2:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Salem A, Lacour O, Scaringella S, et al. Cross-sectional survey of knowledge of obstetric danger signs among women in rural Madagascar. BMC Pregnancy Childbirth. 2018;18(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Phanice OK, Zachary MOJR. Gynecology. Knowledge of obstetric danger signs among pregnant women attending antenatal care clinic at health facilities within Bureti Sub-County of Kericho County, Kenya. Res Obstetr Gynecol. 2018;6(1):16–21. [Google Scholar]
- 19.Teshoma Regasa M, Markos J, Habte A, Upashe SPJO, International G. Obstetric danger signs: knowledge, attitude, health-seeking action, and associated factors among postnatal mothers in nekemte town, Oromia region, western Ethiopia—A community-based cross-sectional study. Obstetr Gynecol Int. 2020;2020:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Iliyasu Z, Galadanci HS, Abdurrahim A, Jibo A, Salihu HM, Aliyu MHJAo GH. Correlates of obstetric risk perception and recognition of danger signs in Kano, Northern Nigeria. Ann Glob Health. 2019;85(1). doi: 10.5334/aogh.376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nambala B, Ngoma CJMJo Z. Knowledge and perception of women towards danger signs in pregnancy in Choma Rural District, Zambia Medical Journal of Zambia. 2013;40(2):43–47. [Google Scholar]
- 22.Hailu D, Berhe HJP. Knowledge about obstetric danger signs and associated factors among mothers in Tsegedie district, Tigray region, Ethiopia 2013: community based cross-sectional study. PLoS one. 2014;9(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Damme TGJ. Knowledge of obstetric danger signs and associated factors among pregnant women attending ANC Service at Gedo town health facilities, 2015. Signs. 2016;28:50–56. [Google Scholar]
- 24.Endalamaw M, Hawult TJT. The level of awareness on danger signs of pregnancy and associated factors among ANC attendant pregnant women in Debark town, north west Ethiopia. Transl Med Biotechnol. 2014;2(5). [Google Scholar]
- 25.Gize A, Eyassu A, Nigatu B, Eshete M, Wendwessen NJB. Men’s knowledge and involvement on obstetric danger signs, birth preparedness and complication readiness in Burayu town, Oromia region, Ethiopia. BMC Preg Childbirth. 2019;19(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hailu M, Gebremariam A, Alemseged FJE. Knowledge about obstetric danger signs among pregnant women in Aleta Wondo District, Sidama Zone, Southern Ethiopia. Ethiopian J Health Sci. 2010;20(1):25–32. doi: 10.4314/ejhs.v20i1.69428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bogale D, Markos DJB. Knowledge of obstetric danger signs among child bearing age women in Goba district, Ethiopia: a cross-sectional study. BMC Preg Childbirth. 2015;15(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maseresha N, Woldemichael K, Dube LJB. Knowledge of obstetric danger signs and associated factors among pregnant women in Erer district, Somali region, Ethiopia. BMC Women's health. 2016;16(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dadi LS, Berhane M, Ahmed Y, et al. Maternal and newborn health services utilization in Jimma Zone, Southwest Ethiopia: a community based cross-sectional study. BMC Preg Childbirth. 2019;19(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Population EOot, Commission HC. Summary and statistical report of the 2007 population and housing census: Population size by age and sex. Federal Democratic Republic of Ethiopia, Population Census Commission; 2008. [Google Scholar]
- 31.Nigussie AA, Emiru AA, Demilew YM, Mersha EAJ. Factors associated with knowledge on obstetric danger signs among women who gave birth within 1 year in Bahir Dar city administration, North West, Ethiopia. J Personal Soc Psychol. 2019;12:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shibeshi K, Lemu Y, Gebretsadik L, Gebretsadik A, Morankar SJIJoWs H. Understanding Gender-Based Perception During Pregnancy: a Qualitative Study. Int J Women's Health. 2023;15:1523–1535. doi: 10.2147/IJWH.S418653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Imani Ramazani B-E, Mabakutuvangilanga Ntala S-D, Katuashi Ishoso D, Rothan-Tondeur M; Rothan-Tondeur MJIJo ER, Health P. Knowledge of Obstetric Danger Signs among Pregnant Women in the Eastern Democratic Republic of the Congo. Int J Enviro Res Public Health. 2023;20(8):5593. doi: 10.3390/ijerph20085593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Galle A, De Melo M, Griffin S, et al. A cross-sectional study of the role of men and the knowledge of danger signs during pregnancy in southern Mozambique. BMC Preg Childbirth. 2020;20(1):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Woldeamanuel GG, Lemma G, Zegeye BJB. Knowledge of obstetric danger signs and its associated factors among pregnant women in Angolela Tera District, Northern Ethiopia. BMC Res Note. 2019;12(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.World Health Organization. Maternal Mortality: The Urgency of a Systemic and Multisectoral Approach in Mitigating Maternal Deaths in Africa. World Health Organization; 2023. [Google Scholar]
- 37.Geleto A, Chojenta C, Musa A, Loxton DJS. WOMEN’s Knowledge of Obstetric Danger signs in Ethiopia (WOMEN’s KODE): a systematic review and meta-analysis. System Rev. 2019;8(1):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Workineh Y, Hailu D, Gultie T, et al. Knowledge of obstetric danger signs and its associated factors in Arba Minch town, Ethiopia. Am J Health Res. 2014;2(5):255–259. [Google Scholar]
- 39.Assefa Y, Gelaw YA, Hill PS, Taye BW, Van Damme WJG. Community health extension program of Ethiopia, 2003–2018: successes and challenges toward universal coverage for primary healthcare services. Global Health. 2019;15:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jones CL, Jensen JD, Scherr CL, Brown NR, Christy K, Weaver JJH. The health belief model as an explanatory framework in communication research: exploring parallel, serial, and moderated mediation. Health Commun. 2015;30(6):566–576. doi: 10.1080/10410236.2013.873363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shewiyo EJ, Mjemmas MG, Mwalongo FH, Diarz EJ, Msuya SE, Leyaro BJ Does knowledge of danger signs influence use of maternal health services among rural women? Findings from Babati Rural district, Northern Tanzania; 2019.
- 42.Olugbenga-Bello Adenike I, Asekun-Olarinmoye Esther O, Adewole Adefisoye O, Adeomi Adeleye A, Olarewaju Sunday OJJo PH. Perception, attitude and involvement of men in maternal health care in a Nigerian community. J Publ Health. 2013;5(6):262–270. [Google Scholar]
- 43.Bagozzi RP; Burnkrant REJJop, psychology s. Attitude organization and the attitude–behavior relationship. J Personal Soc Psychol. 1979;37(6):913. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper and in the supporting information file.