Abstract
Spinal manipulation learning requires intensive practice, which can cause injuries in students. Motor imagery (MI) paired with physical practice (PP) appears to be a suitable means to reduce the number of physical repetitions without decreasing skill outcomes. This study examines whether a session of MI paired with PP leads to a similar improvement in the ability to precisely produce peak forces during a thoracic manipulation as PP alone. Chiropractic students participated in a thoracic manipulation training program for five weeks. They were randomised in two groups: the MI+PP group performed sessions combining physical and mental repetitions with 1/3 fewer PP sessions, while the PP group performed only PP. Thoracic manipulation performance was assessed in pre and post-tests, consisting of thoracic manipulations at three different strength targets. Absolute error (AE), corresponding to the difference between the force required and the force applied by the student, was recorded for each trial. The main result revealed that AE was significantly lower in post-test than in pre-test for both groups. Despite fewer physical repetitions, the MI+PP participants showed as much improvement as the PP participants. This result supports the use of MI combined with PP to optimise the benefits of physical repetitions on thoracic manipulation learning.
Keywords: motor imagery, mental practice, spinal manipulation, chiropractic students, motor skill
Abstract
La combinaison de la pratique de l’imagerie motrice avec la pratique physique optimise l’amélioration du contrôle de la force maximale pendant la manipulation vertébrale thoracique.
L’apprentissage de la manipulation vertébrale nécessite une pratique intensive qui peut entraîner des blessures chez les étudiants. L’imagerie motrice (IM) associée à la pratique physique (PP) semble être un moyen approprié pour réduire le nombre de répétitions physiques sans diminuer les acquis de compétences. Cette étude examine de quelle manière une séance d’IM combinée à la pratique physique entraîne une amélioration similaire pour doser avec précision leur force lors d’une manipulation thoracique par rapport à la pratique physique seule. Des étudiants en chiropratique ont participé à un programme de formation à la manipulation thoracique pendant cinq semaines. Ils ont été répartis au hasard en deux groupes: le groupe IM + PP a effectué des séances combinant des répétitions physiques et mentales avec 1/3 de séances PP en moins, tandis que le groupe PP n’a effectué que des séances PP. Les résultats des manipulations thoraciques ont été évalués lors de prétests et de post-tests, consistant en des manipulations thoraciques à trois niveaux de force différents. L’erreur absolue (EA), correspondant à la différence entre la force requise et la force appliquée par l’étudiant, a été enregistrée pour chaque essai. Le résultat principal a révélé que l’EA était significativement plus faible dans le post-test que dans le pré-test pour les deux groupes. Malgré un nombre inférieur de répétitions physiques, les participants IM+PP ont montré autant d’amélioration que les participants PP. Ce résultat soutient l’utilisation de l’IM combinée à la PP pour optimiser les avantages des répétitions physiques sur l’apprentissage de la manipulation thoracique.
MOTS CLÉS: imagerie motrice, pratique mentale, manipulation vertébrale, étudiants en chiropratique, habileté motrice
Introduction
Spinal manipulation (SM) is a complex bimanual skill widely used by chiropractors to treat their patients.1 Expertise in spinal manipulation relies on strength dosage and reproducibility to be administered safely and effectively by controlling several biomechanical variables (e.g. speed and magnitude/duration of applied force). The acquisition of this skill requires intensive practice before it can be adaptive and context dependent, with graduated targeted learning outcomes.2,3 For instance, in their 4th and 5th years of study, students practice SM in order to be able to control and adapt their strength to the patient’s morphology. However, this intensive learning can sometimes lead to injuries. The prevalence of musculoskeletal injuries amongst students when learning and performing SM is well documented in the literature.3–10 The authors especially point out the impact of repetitive forceful work on lower back, wrist and shoulder disorders in manual therapists. A recent study proposed a strength and conditioning program based on preventative exercises to reduce the risk of injuries in chiropractic students learning spinal manipulation.11 Other chiropractic scholars also seek to develop specific didactic strategies to optimise chiropractic teaching techniques.3–7 For instance, several studies based on motor learning research investigated the potential of augmented feedback using an instrumented mannequin to facilitate the learning of SM.11–13 Practicing with such a device provides immediate quantitative feedback on specific biomechanical aspects of SM, which may be useful for both the student and the teacher, who would be able to individualise teaching by focusing on aspects of spinal manipulation that have not been acquired fully.
In the same vein, motor imagery practice (MIP), which is “the act of mentally repeating movements (without physically doing it) several times with the intention of learning a new ability or perfecting a known skill”14, could be a promising tool to optimise SM training. The seminal theory proposed by Marc Jeannerod20, and supported by robust neurophysiological and behavioural studies, suggests the existence of shared neural representations; i.e. motor imagery (MI) activates neural substrates that partially overlap those activated by movement execution. On the functional level, the same processes involved in the planning and programming of motor skills appear to underly MI.15,18–20 Indeed, a bulk of evidence from fundamental to applied research in various domains such as cognitive neuroscience, sport science and neurorehabilitation show the benefits of MIP paired with physical practice (PP) to enhance the efficacy of motor training or recovery. 15–19 For instance, in a seminal experimental study, Allami and collaborators21 investigated the optimal proportions of MIP paired with PP to improve the movement time of an action that involved grasping an object and to inserting it in an appropriate slot. The results showed that participants who performed 120 imagined trials of the action followed by 120 physical repetitions reached the same level of performance as the participants who performed 240 physical repetitions. These findings illustrate the potential of MIP paired with PP, suggesting that MIP could be used to partially replace physical practice when learning a motor skill. Therefore, MIP paired with PP appears to be a suitable technique for learning SM to reduce the risk of injuries associated with excessive physical repetitions. The present study aimed to examine whether MIP paired with a reduced number of PP might lead to a similar improvement of thoracic spinal manipulation as PP alone.
Methods
Participants
Forty-two 4th- and 5th-year chiropractic students at the Franco-European Institute of Chiropractic (IFEC) in Paris (France) were recruited through advertisements sent via IFEC’s student mailing lists. Exclusion criteria included suffering musculoskeletal pain in the shoulder, neck or low back region currently or in the past three months, or any reported history of chronic physical disability. The study was approved by the Ethics Committee of IFEC (#CE 2018-03-15-3) and participants gave written informed consent to take part in this study. They were randomly assigned to the PP group (mean age = 23 years, SD =1.5, range = 21–26 years, 9 women) or the PP+MI group (mean age = 23 years, SD =1.5, range = 21–26 years, 16 women).
Materials and tasks
Thoracis spinal manipulation task
In pre-test and post-test, the participants performed a thoracic spinal manipulation (TSM) task using a mannequin made of a plastic spine and high-density foam padding that permitted anteroposterior compression of the thorax and for which skeletal landmarks were palpable through the foam (H.A.M. series; CMCC, Toronto, Ontario). The mannequin was resting on a force-sensing table (Leander 900 Z series table) equipped with an imbedded force plate which can reliably assess forces and moments transmitted to the table in an x-y-z coordinate system using custom-made software (AMTI Watertown, MA; see for similar material and an illustration of the experimental environment).
The task comprised two phases: a warm-up phase composed of two TSM at three intensities of peak force (low: peak force applied = 300 Newton (N); medium = 450 N; high = 600 N) = six pseudo-randomised TSM (pseudorandomized meaning that the randomization was done by the experimenter without following specific rules or algorithms), and an experimental phase composed of four TSM at the same three intensities (low, medium, high) = 12 TSM in total in the experimental phase (Figure 1). Note that a preload force of 200 N was required for all three intensity conditions. For each trial, the experimenter verbally told the participants which peak force intensity to apply. In the experimental phase of each trial, the force applied by the participant on the mannequin’s contact point was recorded in real time on a computer connected to the force plate using Labview software (National Instruments, Austin, TX). Visual feedback on performance (i.e. force-time profile displayed in real time) was hidden from the participants.
Figure 1.
Training session for(A) the PP group and (B) the PP + MI group. TSM = Thoracic Spinal Manipulation. L = Low, M = Medium, H = High.
Movement of imagery questionnaire short-version (MIQ-SV)
The MIQ-SV (Hall and Pongrac, 198322) consists of 16 items relating to either the visual imagery (VI) of movement (i.e. movement is visualised from an external, third-person perspective) and the kinaesthetic imagery (KI) of movement (i.e. movement simulation based on proprioceptive and internal sensations associated to the movement). For each imagery perspective, the difficulty of movement simulation was assessed on a 7-point Likert-type scale (from 1 = movement very easy to visualise or feel, to 7= movement very difficult to visualise or feel).
Training program
The training program was composed of two 20-minute sessions per week (Tuesday and Thursday afternoon) for five weeks for a total of 10 sessions. During the Tuesday session, the participants worked in pairs and practiced on the sensor table used in pre-test or post-test with visual feedback being visible. During the Thursday session, the participants were in groups of five and practiced on classical tables with no feedback on performance.
Each session began with two video clips displaying a teacher performing TSM from either a 1st-person perspective (the camera was attached to his forehead) or a 3rd-person perspective (the camera faced the teacher). Then, training involved two phases: a warm-up phase and a practice phase. For each session, the participants were given a technical form with instructions and the training sequence. For the PP + MI group, there was also a Mental Imagery (MI) form provided, which included detailed instructions on what participants were supposed to visualize and feel during the mental practice of thoracic manipulation. This form served as a guide, specifying the imagery content to enhance the effectiveness of the mental practice component.
For the PP group, the warm-up phase was the same as the TSM task. The practice phase was composed of 12 physical repetitions for each intensity (low: peak force applied = 300 N; medium = 450 N; high = 600 N) for a total of 36 physical repetitions. The session was organised in blocks of 3 repetitions with the same intensity. The order of the blocks was pseudo-randomised by the experimenter and was changed at each session.
For the PP + IM group, the warm-up phase included six TSM with four physical repetitions and two mental repetitions. The practice phase was composed of eight physical repetitions and eight mental repetitions for each intensity (low: peak force applied = 300 N; medium = 450 N; high = 600 N) for a total of 48 TSM with 24 physical repetitions and 24 mental repetitions. The session was organised in blocks of two physical repetitions followed by two mental repetitions at the same intensity. The order of the blocks was pseudo-randomised by the experimenter and was changed at each session (see a sample session for each group in supplementary files).
Protocol
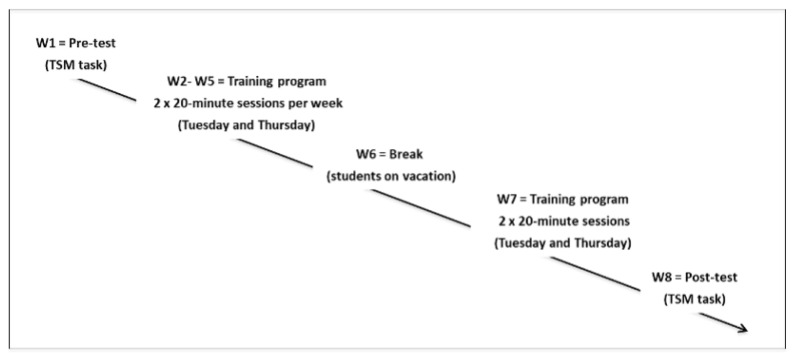
The experiment was conducted at the IFEC in April and May 2018, with W1 and W8 = pre-test and post-test respectively; W2–W5 + W7 = training program; and W6 = break (students on vacation). At the end of pre-test and post-test, all of the participants completed the Movement Imagery Questionnaire MIQ; Hall, Pongrac, 1983) (Figure 2).
Figure 2.
Illustration of the protocol.
Data analysis
Thoracic spine manipulation task
The peak force (in Newton, N) corresponding to the maximal value of force application after the preload phase, was computed for each TSM. Then, absolute error (AE), representing the absolute deviation, irrespective of direction, between participants’ results and the targeted peak force (i.e., participants’ accuracy), was calculated for each trial using the formula:
The peak force required corresponded to the intensity of a trial: low, medium or high (see the description of the TSM task above). High AE represented low performance, while low AE represented high performance.
MIQ
A score was calculated for each perspective (IV, IK) from the sum of corresponding items. High scores represented difficulty performing motor imagery, while low scores represented motor imagery with ease.
All statistical analyses were conducted using SPSS (version 19). A mixed analysis of Variance (ANOVA) was performed on AE with the intensity of each trial (low, medium, high) as a within-subject factor and the group (PP, MI+PP) as a between-subject factor. A Greenhouse-Geisser correction was used when the sphericity assumption was violated (p < .05 for Mauchly’s sphericity test). Alpha was set at .05. In the event of significance, pairwise comparisons using the Bonferroni correction were applied. Shapiro-Wilk tests showed that IK and IV scores were normally distributed (p >.05) and there was homogeneity of variances, as determined by Levene’s test for equal variances (p > .05). Paired t-tests were performed on the IK and IV scores to compare MI abilities in pre-test vs. post-test.
Results
Thoracic spine manipulation task
Mixed ANOVA on AE revealed a main effect of intensity [F(1.7, 67.6) = 4.05, p = .027, η2 = .94] and a main effect of test [F(1,39) = 28.9, p < .0001, η2 < .42]. As illustrated by Figure 3, post-hoc tests with the Bonferroni correction revealed that AE was significantly higher for high intensity (mean = 72 N, SD =49) than low (mean = 57 N, SD =34.5, p=.03) or medium intensities (mean = 59 N, SD =32, p=.02). There was no significant difference between low and medium intensities (p= .61). Figure 4 shows that AE was significantly lower in post-test (mean = 51 N, SD =27) than in pre-test (mean = 74 N, SD =46). There was no significant interaction between the test and the group [F(1.39) = 0.46, p = .46, η2 < .012].
Figure 3.
Absolute Error (AE) in pre-test and post-test. Error bars indicate standard deviation. ** = p<0.0001
Figure 4.
Absolute Error (AE) as a function of intensity of force required (low, mediu,, high). Error bars indicate standard deviion. * p<0.05
Figure 5.
Mean (SD) of Absolute Error (AE) as a function of group (PP, MI+PP), test (pre-test, post-test) and intensity of force required (low, medium, high).
MIQ
Paired t-tests on IK and IV scores revealed a significant difference between pre-test and post-test IK = [t(19) = 3.868, p < .0001]; IV = [t(19) = 4.884, p = .001], with lower scores in post-test (IK mean = 13; SD =5; IV mean = 13, SD =4 ) compared to pre-test (IK mean = 20; SD = 9; IV mean = 17, SD =6 ).
Discussion
This study aimed to examine the potential of MIP as a learning technique in chiropractic training, particularly in improving strength dosage in thoracic spinal manipulation in fourth and fifth-year chiropractic students. The results show that the number of physical repetitions is reduced when PP is paired with MIP while reaching a similar level of performance compared with PP alone. Therefore, MIP appears to be a suitable tool to reduce physical practice to limit the risks related to repetitive spinal manipulation practice in students. The results observed in the present study showed that the participants in both the MI+PP and PP groups improved the accuracy of strength application significantly during SM, as shown by a lower difference between the intensity of SM required and the force applied during the TSM task. Moreover, the significant improvement of MI abilities in the MI+PP group appear to suggest that the chiropractic students were able to apply mental practice efficiently. Overall, these findings confirm that MIP can be used to partially reduce PP in the learning of thoracic spinal manipulation. This study agrees with previous experiments exploring the potential of MIP paired with PP in surgical training, although the results observed in these works might be debatable.23–25
Another question may be raised when combining MIP with PP. Indeed, the authors investigated whether motor learning can be optimised by adding MIP, i.e. MIP could be considered a supplement to physical practice.26–28 These studies imply a similar amount of physical practice in both training groups, with one of the two groups performing additional MIP. For instance, Hidalgo-Perez and collaborators25 investigated the impact of MI combined with PP when healthy participants practiced motor control exercises (generally used in a therapeutic program to manage neck pain) to improve sensorimotor function. Their results showed that craniocervical neuromotor control, and the subjective perception of fatigue after effort were significantly higher in the group for which MI was added to PP, compared with the group that trained only physically. Thus, it would be of interest to test the impact of MIP+PP compared with PP alone on the learning of spinal manipulation, while maintaining a similar amount of PP in each group.
Moreover, the students who participated in this experiment were in 4th and 5th year at the chiropractic college. Therefore, they would be in the second stage of SM learning, which consists of reducing trial-to-trial variability of force production, indicating automated control of movement. At the end of this stage, students will be able to vary precisely the degree of force production between successive trials. This ability is critical, and ensures that the chiropractor is able to deliver effective SM and adapt SM to patient morphology. MI focused mainly on the sensations associated with the force applied to the mannequin (i.e. kinaesthetic imagery). It is likely that MI would have facilitated the integration of proprioceptive inputs used by the central system to update internal models or memories of motor programs.29 In the future, it would be interesting to investigate the potential of MI to enhance the acquisition of SM in the 1st stage of learning, i.e. when students learn the correct posture in the different phases of SM (e.g. pre-load force, time to peak force) so as to stabilise the rate of force production over time2,4. Other MI modalities might be also considered, such as visual imagery, which might be interesting very early in the learning of SM skills.
Limitations
There are some limitations to this study. First, the contents of the training sessions were similar to the TSM task used when evaluating SM performance (i.e. in pre-test and post-test sessions) since each training session consisted of repetitions of SM at the same intensities as those used in the TSM task. Moreover, only three levels of force intensity were used within a training session, which may have reinforced these specific motor programs of SM, and probably favoured the development of automaticity in performance. However, the lack of variability in training sessions and skill transfer evaluation did not allow us to conclude that the students improved their ability to regulate the rate of force production when performing SM trials. Thus, although the results showed that the students did reduce the mean variability of SM peak at the given intensities, the task was probably quite simple with respect to their level of expertise. It would have been more suitable to use other intensities from one training session to another, and to propose a TSM task with other intensities than those used during practice. Secondly, performance was evaluated quantitatively, based on knowledge of results (i.e. difference between the force required compared to the force applied), which was appropriated to evaluate the effect of the training program. However, it is likely that the study set very easy targets for the participants, which were not representative of the full spectrum of forces seen in their practice. It would have been more relevant to require students to modulate forces across a wide spectrum of force within corridors of +/− 75N, as well as to use target ranges rather than AE to evaluate their performance in the pre-test and post-test. Moreover, it did not make it possible to specify which aspects of SM skill were improved consecutive to practice, and whether certain aspects would benefit more from MI than others. Future studies including qualitative indicators of SM performance and learning (namely, biomechanical variables usually used to describe SM4) will contribute to the understanding of the effect of MI paired with PP in the learning of SM skills. Moreover, a recent study30 demonstrated that MI may be an effective strategy (used as a teaching method) to explain a motor task. It would be pedagogically interesting to use MI as a teaching method to encourage the understanding of biomechanical aspects of SM skill, which are not always easy to verbalise.
Conclusion
The results of this study highlighted the potential of MI practice paired with physical practice to improve the ability to precisely control the impulse (or peak) force when performing a spinal manipulation technique by chiropractic students. It encourages the use of MI as a teaching tool in the context of the learning of manual therapies, notably to limit the risk of injury caused by intensive practice. MI could be introduced into the curriculum as early as the first year of education. This approach would serve as a valuable tool to help students enhance their posture, weight transfer, and overall movement awareness, enabling them to adapt their strength according to the body types of their future patients. Additionally, MI would empower students to continue learning independently at home or for those who may be recovering from injuries. However, future investigations are needed to clarify the effectiveness of MIP in the context of SM skills learning, for example, by examining which biomechanical variables would be sensitive to mental practice.
Practical applications
Potential of MIP paired with PP was examined to reduce physical repetitions while reaching the same level of performance.
Despite fewer physical repetitions, MI+PP participants improved as much as PP participants.
Motor Imagery should be considered in the development of didactic strategies related to SM skills.
Acknowledgments
The authors thank chiropractic students for their participation in the experiment, and individuals (teachers/administration) of IFEC for their assistance in completion of this study.
Footnotes
The authors have no disclaimers, competing interests, or sources of support or funding to report in the preparation of this manuscript.
References
- 1.Beliveau PJH, Wong JJ, Sutton A, Simon NB, Bussières AE, Mior SA, French SD. The chiropractic profession: a scoping review of utilization rates, reasons for seeking care, patient profiles, and care provided. Chiropr Man Ther. 2017;25(1) doi: 10.1186/s12998-017-0165-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Descarreaux M, Dugas C. Learning spinal manipulation skills: assessment of biomechanical parameters in a 5-year longitudinal study. J Manip Physiol Ther. 2010;33(3):226–230. doi: 10.1016/j.jmpt.2010.01.011. [DOI] [PubMed] [Google Scholar]
- 3.Ndetan HT, Rupert RL, Bae S, Singh KP. Prevalence of musculoskeletal injuries sustained by students while attending a chiropractic college. J Manip Physiol Ther. 2009;32(2):140–148. doi: 10.1016/j.jmpt.2008.12.012.. [DOI] [PubMed] [Google Scholar]
- 4.Triano JJ, Descarreaux M, Dugas C. Biomechanics – Review of approaches for performance training in spinal manipulation. J Electromyograph Kinesiol. 2012;22(5):732–739. doi: 10.1016/j.jelekin.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 5.Bisiacchi DW, Huber LL. Physical injury assessment of male versus female chiropractic students when learning and performing various adjustive techniques: a preliminary investigative study. Chiropr Osteopath. 2006;14:17. doi: 10.1186/1746-1340-14-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holm SM, Rose KA. Work-related injuries of doctors of chiropractic in the United States. J Manipulative Physiol Ther. 2006;29(7):518–523. doi: 10.1016/j.jmpt.2006.06.023.. [DOI] [PubMed] [Google Scholar]
- 7.Macanuel K, Deconinck A, Sloma K, LeDoux M, Gleberzon BJ. Characterization of side effects sustained by chiropractic students during their undergraduate training in technique class at a chiropractic college: a preliminary retrospective study. J Can Chiropr Assoc. 2005;49(1):46–55. [PMC free article] [PubMed] [Google Scholar]
- 8.Stock SR. Workplace ergonomic factors and the development of musculoskeletal disorders of the neck and upper limbs: a meta-analysis. Am J Ind Med. 1991;19(1):87–107. doi: 10.1002/ajim.4700190111.. [DOI] [PubMed] [Google Scholar]
- 9.Thomsen JF, Mikkelsen S, Andersen JH, Fallentin N, Loft IP, Frost P, Kjærgaard A, Bonde JP, Overgaard E. Risk factors for hand-wrist disorders in repetitive work. Occup Environ Med. 2007;64(8):527–533. doi: 10.1136/oem.2005.021170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hansen MC, Aagaard T, Christensen HW, et al. Workrelated acute physical injuries, chronic overuse complaints, and the psychosocial work environment in Danish primary care chiropractic practice – a cross-sectional study. Chiropr Man The4. 2018;26:4. doi: 10.1186/s12998-018-0174-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Descarreaux M, Dugas C, Lalanne K, Vincelette M, Normand MC. Learning spinal manipulation: the importance of augmented feedback relating to various kinetic parameters. Spine J. 2006;6:138–145. doi: 10.1016/j.spinee.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 12.Scaringe JG, Chen D, Ross D. The effects of augmented sensory feedback precision on the acquisition and retention of a simulated chiropractic task. J Manipulative Physiol Ther. 2002;25:34–41. doi: 10.1067/mmt.2002.120419. [DOI] [PubMed] [Google Scholar]
- 13.Triano JJ, Rogers CM, Combs S, Potts D, Sorrels K. Quantitative feedback versus standard training for cervical and thoracic manipulation. J Manipulative Physiol Ther. 2003;26:131–138. doi: 10.1016/S0161-4754(02)54105-1. [DOI] [PubMed] [Google Scholar]
- 14.Malouin F, Jackson P, Richards CL. Towards the integration of mental practice in rehabilitation programs. A critical review. Front Hum Neurosci. 2013;7:576. doi: 10.3389/fnhum.2013.00576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guillot A, Di Rienzo F, Collet C. 2014. The Neurofunctional Architecture of Motor Imagery in: “Advanced Brain Neuroimaging Topics in Health and Disease - Methods and Applications”, by Papageorgiou et al. [Google Scholar]
- 16.Rannaud Monany D, Papaxanthis C, Guillot A, Lebon F. Motor imagery and action observation following immobilisation-induced hypoactivity: a narrative review. Ann Phys Rehab Med. 2022;65(4):101541. doi: 10.1016/j.rehab.2021.101541. [DOI] [PubMed] [Google Scholar]
- 17.Díaz López N, Pereira EM, Centeno EJ, Miangolarra Page JC. Motor imagery as a complementary technique for functional recovery after stroke: a systematic review. Top Stroke Rehabil. 2019;26(8):576–587. doi: 10.1080/10749357.2019.1640000. [DOI] [PubMed] [Google Scholar]
- 18.Guillot A, Di Rienzo F, Frank C, Debarnot U, MacIntyre TE. From simulation to motor execution: a review of the impact of dynamic motor imagery on performance. Intl Rev Sport Exercise Psychol. 2021 doi: 10.1080/1750984X.2021.2007539. [DOI] [Google Scholar]
- 19.Cuenca-Martínez F, Suso-Martí L, León-Hernández JV, La Touche R. The role of movement representation techniques in the motor learning process: a neurophysiological hypothesis and a narrative review. Brain Sci. 2020;10(1):27. doi: 10.3390/brainsci10010027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jeannerod M. Neural simulation of action: a unifying mechanism for motor cognition. Neuroimage. 2001;14:429–439. doi: 10.1006/nimg.2001.0832.. [DOI] [PubMed] [Google Scholar]
- 21.Allami N, Paulignan Y, Brovelli A, Boussaoud D. Visuomotor learning with combination of different rates of motor imagery and physical practice. Exp Brain Res. 2008;184:105–113. doi: 10.1007/s00221-007-1086-x. [DOI] [PubMed] [Google Scholar]
- 22.Hall C, Pongrac J. The measurement of imagery ability. Human Movement Sci. 1983;4(2):107–118. [Google Scholar]
- 23.Sanders CW, Sadoski M, Bramson R, Wiprud R, Van Walsum K. Comparing the effects of physical practice and mental imagery rehearsal on learning basic surgical skills by medical students. Am J Obstet Gynecol. 191(5):1811–1814. doi: 10.1016/j.ajog.2004.07.075. [DOI] [PubMed] [Google Scholar]
- 24.Sanders CW, Sadoski M, van Walsum K, Bramson R, Wiprud R, Fossum TW. Learning basic surgical skills with mental imagery: using the simulation centre in the mind: Learning basic surgical skills with mental imagery. Med Educ. 2008;42:607–612. doi: 10.1111/j.1365-2923.2007.02964.x. [DOI] [PubMed] [Google Scholar]
- 25.Immenroth M, Bürger T, Brenner J, Nagelschmidt M, Eberspächer H, Troidl H. Mental training in surgical education. Ann Surg. 2007;245(3):385–391. doi: 10.1097/01.sla.0000251575.95171.b3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hidalgo-Perez A, Fernández-García A, López-de-Uralde-Villanueva I, Gil-Martínez A, Paris-Alemany A, Fernández-Carnero J, La Touche R. Effectiveness of a motor control therapeutic exercise program combined with motor imagery on the sensorimotor function of the cervical spine: a randomized controlled trial. Int J Sports Phys Ther. 2015;10(6):877–892. [PMC free article] [PubMed] [Google Scholar]
- 27.Dana A, Gozalzadeh E. Internal and external imagery effects on tennis skills among novices. Percept Mot Skills. 2017;124(5):1022–1043. doi: 10.1177/0031512517719611. [DOI] [PubMed] [Google Scholar]
- 28.Slimani M, Tod D, Chaabene H, Miarka B, Chamari K. Effects of mental imagery on muscular strength in healthy and patient participants: a systematic review. J Sports Sci Med. 2016;15(3):434. [PMC free article] [PubMed] [Google Scholar]
- 29.Wolpert DM, Ghahramani Z. Computational principles of movement neuroscience. Nat Neurosci. 2000;3:1212–1217. doi: 10.1038/81497. [DOI] [PubMed] [Google Scholar]
- 30.La Touche R, Sánchez-Vázquez M, Cuenca-Martínez F, Prieto-Aldana M, Paris-Alemany A, Navarro-Fernández G. Instruction modes for motor control skills acquisition: a randomized controlled trial. J Mot Behav. 2020;52(4):444–455. doi: 10.1080/00222895.2019.1645087. [DOI] [PubMed] [Google Scholar]