Abstract
The safety and efficacy of Yttrium-90 (Y-90) radio-embolization therapy is partly dependent on the lung shunt fraction (LSF). There may be a notable disparity between LSF when calculated using 2D planar imaging vs 3D single photon emission CT (SPECT); this can affect the total allowable Y-90 dose delivered and therefore change the effectiveness of the procedure. The case presented demonstrates an 81% decrease in LSF when calculated by SPECT as compared to 2D planar imaging. This case highlights the importance of considering the imaging technique and the potential discrepancies that can arise between planar and SPECT imaging in LSF assessment.
Keywords: Y-90, planar imaging, hepatocellular carcinoma, trans-arterial radioembolization, single photon emission CT (SPECT), lung shunt fraction
Introduction
Hepatocellular Carcinoma (HCC) is one of the leading causes for cancer-related mortality and ranks as the second leading cause of years of life lost due to cancer worldwide.1 Nevertheless, prognosis varies from patient to patient, influenced by specific tumour characteristics. It is well documented that patients who receive timely treatment tend to have longer average survival rates. Depending on the stage, localization, and other factors, there are multiple treatment options available today including radiofrequency ablation, hepatic resection, bridging to transplant, radio-embolization, and combination therapy.1
The treatment with radioactive Yttrium-90 (Y-90) glass microsphere-based trans arterial radioembolization (TARE) is an effective and well-tolerated treatment by eligible patients with HCC.2 However, for proper dosing of Y-90 and to prevent extrahepatic complications, it is essential to perform mapping with Technetium-99m macro aggregated albumin (99mTc-MAA) and assess the pulmonary shunt fraction or its abnormal distribution to other organs.2,3 A catheter is guided by fluoroscopy to the artery supplying the tumour during this mapping. 99mTc-MAA, which has a similar distribution to Y-90, is injected and the patient undergoes a single photon emission CT/CT (SPECT/CT) scan in NM to determine tumour size, location, and the optimal blood vessels for Y-90 delivery. This information aids in developing a treatment plan based on the images.
Lung shunt fraction (LSF) represents the proportion of blood flow from the hepatic artery that bypasses the liver and instead perfuses the lungs. It is a critical parameter to calculate the potential risk of radiation-induced lung toxicity during Y-90 therapy. Accurate measurement of lung shunt fraction is vital to ensure that the radiation dose to the lungs is within acceptable limits to prevent adverse effects while delivering an effective therapeutic dose to the target liver lesions.
A major impact of this detailed planning prior to Y-90 radioembolization is that the incidence of radiation pneumonitis is less than 1% when lung studies are conducted correctly.4 Typically, in routine clinical practice, standard LSF calculation involves a single 2D anterior and a 2D posterior Nuclear Medicine (NM) planar imaging, but LSF obtained from the 2D planar images might be over-estimated due to scatter counts from the liver into the lungs.5,6 Recent literature suggests that alternative methods, such as SPECT, can provide more precise LSF percentages5,6 due to additional scatter correction. If an accurate LSF was obtained, the patient would benefit from receiving precise doses of Y-90 ensuring treatment efficacy.
For this reason, we intended to process the LSF from 3D SPECT images of patients diagnosed with HCC who underwent Y90-TARE. This case report presents a scenario of a lung shunt discrepancy between planar imaging and SPECT imaging. Such a discrepancy could raise concerns regarding the safety and efficacy of Y-90 radio embolization therapy in the case of a patient diagnosed with HCC. During the preliminary investigations of Y-90 treatment, a notable disparity was observed between the planar LSF and the SPECT results and how this affected the total Y-90 dose delivered.
IRB approval was obtained for the study. All images were anonymized, and the autonomy and privacy of the patient were respected throughout the preparation and publication of this case report.
Case presentation
A 47-year-old male patient was diagnosed with portal hypertension after presenting to the Emergency Room with upper gastrointestinal bleeding. Management according to clinical guidelines for gastrointestinal bleeding was performed, including transjugular intrahepatic portosystemic shunt (TIPS) placement. An MRI was performed, revealing cirrhosis with an indeterminate lesion with subtle peripheral enhancement in the superior right hepatic lobe (segment 7), measuring 1.5 × 1.3 cm, determined to be LR-3. The patient was advised to return for follow-up regarding this finding. The patient remained clinically stable, and a follow-up MRI was performed three months later that showed cirrhotic liver with probable small siderotic nodules. In segment 7, a 2.1 × 1.7 cm lesion with peripheral enhancement was identified with interval growth, best classified as LR-4 (Figure 1). A TIPS was present, along with stable splenomegaly and a trace of ascites.
Figure 1.
Lesion in liver segment 7 as observed on: (A) Coronal T1-weighted LAVA post-contrast MRI showing a lesion with central hypoenhancement and a thick enhancing capsule (red arrow), (B) Axial 2D FIESTA fat sat MRI showing a hyperintense, slightly heterogeneous lesion (red arrow), (C) Axial arterial phase postcontrast MRI showing a hypointense lesion with a thick enhancing capsule (red arrow), and (D) Axial DWI MRI demonstrating diffusion restriction in the nodular lesion (red arrow).
An ultrasound-guided liver biopsy was performed, confirming the diagnosis of HCC. The patient was scheduled for Y-90 TARE through a selective right posterior radiation segmentectomy (RADSEG) (Figure 2). As part of the protocol, LSF estimation was performed manually, by a NM technologist, using the 2D anterior and posterior planar imaging. The results showed no presence of tracer outside the liver, with the majority of the tracer deposited within the right lobe. The estimated lung shunt was 10.6% on the 2D planar images (Figure 3), and the therapeutic dosage of Y-90 to be delivered was calculated as 466 Gy.
Figure 2.
Coronal (A) and Axial (B) views of a 3D reconstructed SPECT/CT NM Pre Y-90 images demonstrating the majority of the Tc99m uptake deposited within the right lobe of the liver. No abnormal localization was noted outside of the liver.
Figure 3.
Anterior (A) and Posterior (B) 2D planar views showing delineated liver and lung regions and counts using coronal slices from 99mTc-MAA planar imaging for the calculation of LSF (C). The planar lung shunt fraction was calculated to be 10.6%.
3D SPECT images were reconstructed using ordered subset expectation maximization technique with CT pre Y-90 images for attenuation, scatter correction and recovery co-coefficients applied in Q-Volumetrix software on General Electric Xeleris. Q-Volumetrix generated 3D images of the organs with 99mTc-MAA activity in the liver and lungs were clearly visualized. A semi-automatic threshold-based segmentation was performed to outline the liver and the lungs. This provided a more precise and automated LSF calculation from 3D SPECT than 2D planar images.
The LSF was estimated using 3D segmentation techniques, revealing an estimated lung shunt fraction of 1% and 3%, between liver and left lung and right lung, respectively (Figure 4). This provided a difference of 81% between 2D planar and 3D SPECT imaging (average liver-to-lungs). With this new LSF, the cumulative liver dose was determined to be 510 Gy, resulting in a 9.4% increase from the initially received dose that could have been potentially delivered.
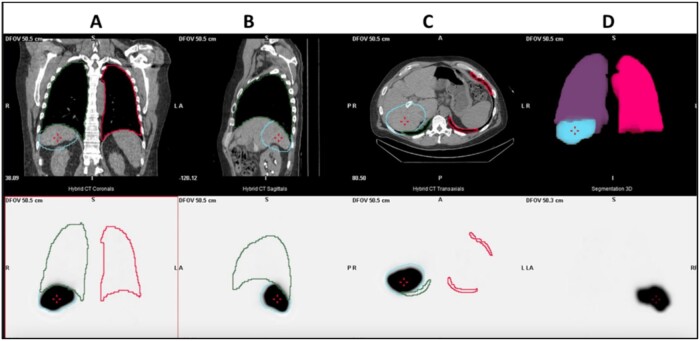
Figure 4.
Top row showing the (A) Coronal (B) Sagittal (C) Axial CT views generated by QVolumetrix using 3D SPECT and (D) 3D images of the segmented lung lobes and the liver. The bottom row shows the same views for the 3D SPECT images with clear visualization of the 99mTc-MAA activity and uptake in liver and spill out into the lung regions. SPECT lung shunt fraction was 2%.
Discussion
The LSF is determined by calculating the ratio of the 99mTc-MAA counts of a specific lung region with the total counts of both the lung and the liver. For resin microspheres, an LSF greater than 20% is a contraindication to Y-90, and an LSF greater than 10% may require a Y-90 dose reduction.7 It has been observed that this calculation, when obtained using planar images, tends to overestimate the result.5 2D planar imaging, often using 99mTc-MAA particles, is a commonly employed method for pre-therapy assessment of lung shunt fraction providing a global assessment of lung shunt, which can be influenced by several factors, including injection site, particle size, and particle distribution. SPECT imaging, on the other hand, provides a 3D visualization of the distribution of radiopharmaceuticals within the body. SPECT can offer a more detailed and accurate assessment of lung shunt fraction compared to planar imaging. In a study conducted in 2020 involving 298 subjects, a significant discrepancy of 8.27% vs 3.27% was noted in the LSF when comparing the results obtained from planar imaging to those obtained from SPECT, respectively.8 The relevance of this issue lies in the fact that this overestimated result leads to a decrease in the therapeutic Y-90 dose. It was found that out of ten patients who initially required a dose reduction based on planar imaging, only two needed a dose reduction after using SPECT imaging.8 In 2020, Struycken et al7 reported similar findings, with the mean LSF from planar imaging at 25.1%, whereas the LSF from SPECT imaging averaged 16.0%. The use of SPECT rather than planar imaging for calculation of LSF would have avoided unnecessary dose reduction or shunt-reduction procedure in 11 out the 36 patients studied. When comparing both methods, choosing SPECT allows for a more accurate shunt calculation, potentially resulting in a more precise dosage determination.7 This is exemplified in the case presented, where the potential increase was nearly 10%.
Having a more precise LSF measurement will also enable more precise dosimetry. Recently, Garin et al9 compared standard versus personalized dosimetry and found that the objective response in patients with locally advanced HCC was significantly improved with personalized dosimetry.9 In 2022, a retrospective multicentre investigation including 209 patients showed that increasing glass microsphere dose increased probability of tumour response and longer overall survival rate without a significant increase in toxicity.10
The discrepancy between planar and SPECT imaging results in this case report emphasizes the importance of choosing an accurate method for lung shunt fraction assessment in Y-90 therapy.
Contributor Information
Paula Gamero Kubota, Department of Radiology and Medical Imaging, Loyola University School of Medicine, Maywood, IL60153, United States.
Christopher Molvar, Department of Radiology and Medical Imaging, Loyola University School of Medicine, Maywood, IL60153, United States.
Robert Wagner, Department of Radiology and Medical Imaging, Loyola University School of Medicine, Maywood, IL60153, United States.
Emad Allam, Department of Radiology and Medical Imaging, Loyola University School of Medicine, Maywood, IL60153, United States.
James Halama, Department of Radiology and Medical Imaging, Loyola University School of Medicine, Maywood, IL60153, United States.
Judy R James, Department of Radiology and Medical Imaging, Loyola University School of Medicine, Maywood, IL60153, United States.
Learning point
Accurate assessment of LSF is crucial for the safe and effective administration of Y-90 radioembolization therapy.
There is a clinical necessity to minimize variations between LSF calculation methods and enhance the overall accuracy of LSF assessment in clinical practice.
3D SPECT quantification is superior to 2D planar quantification for evaluation of LSF assessment.
Discrepancies between 2D planar and 3D SPECT LSF assessment methods can impact the patient Y-90 dose.
Clinicians should be aware of the potential discrepancies between planar and SPECT imaging and their implications for patient treatment planning in Y-90 radioembolization therapy.
Funding
None declared.
Conflicts of interest
None declared.
References
- 1. Kulik L, El-Serag HB.. Epidemiology and management of hepatocellular carcinoma. Gastroenterology. 2019;156(2):477-491.e1. 10.1053/j.gastro.2018.08.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Salem R, Padia SA, Lam M, et al. Clinical, dosimetric, and reporting considerations for Y-90 glass microspheres in hepatocellular carcinoma: updated 2022 recommendations from an international multidisciplinary working group. Eur J Nucl Med Mol Imaging. 2023;50(2):328-343. 10.1007/s00259-022-05956-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mikell JK, Dewaraja YK, Owen D.. Transarterial radioembolization for hepatocellular carcinoma and hepatic metastases: clinical aspects and dosimetry models. Semin Radiat Oncol. 2020;30(1):68-76. 10.1016/j.semradonc.2019.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Spina JC, Hume I, Pelaez A, Peralta O, Quadrelli M, Garcia Monaco R.. Expected and unexpected imaging findings after 90 Y transarterial radioembolization for liver tumors. Radiographics. 2019;39(2):578-595. 10.1148/rg.2019180095 [DOI] [PubMed] [Google Scholar]
- 5. Braat AJ, Smits ML, Braat MN, et al. 90Y hepatic radioembolization: an update on current practice and recent developments. J Nucl Med. 2015;56(7):1079-1087. 10.2967/jnumed.115.157446 [DOI] [PubMed] [Google Scholar]
- 6. Allred JD, Niedbala J, Mikell JK, Owen D, Frey KA, Dewaraja YK.. The value of 99mTc-MAA SPECT/CT for lung shunt estimation in 90Y radioembolization: a phantom and patient study. EJNMMI Res. 2018;8(1):50. 10.1186/s13550-018-0402-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Struycken L, Patel M, Kuo P, Hennemeyer C, Woodhead G, McGregor H.. Clinical and dosimetric implications of calculating lung shunt fraction for hepatic 90Y radioembolization using SPECT/CT versus planar scintigraphy. Am J Roentgenol. 2022;218(4):728-737. 10.2214/AJR.21.26663 [DOI] [PubMed] [Google Scholar]
- 8. Elsayed M, Cheng B, Xing M, et al. Comparison of Tc-99m MAA planar versus SPECT/CT imaging for lung shunt fraction evaluation prior to Y-90 radioembolization: are we overestimating lung shunt fraction? Cardiovasc Intervent Radiol. 2021;44(2):254-260. 10.1007/s00270-020-02638-8 [DOI] [PubMed] [Google Scholar]
- 9. Garin E, Tselikas L, Guiu B, et al. Personalised versus standard dosimetry approach of selective internal radiation therapy in patients with locally advanced hepatocellular carcinoma (DOSISPHERE-01): a randomised, multicentre, open-label phase 2 trial. Lancet Gastroenterol Hepatol. 2021;6(1):17-29. 10.1016/S2468-1253(20)30290-9 [DOI] [PubMed] [Google Scholar]
- 10. Lam M, Garin E, Maccauro M, et al. A global evaluation of advanced dosimetry in transarterial radioembolization of hepatocellular carcinoma with Yttrium-90: the TARGET study. Eur J Nucl Med Mol Imaging. 2022;49(10):3340-3352. 10.1007/s00259-022-05774-0 [DOI] [PMC free article] [PubMed] [Google Scholar]