Abstract
Objectives
To evaluate literature from a 12-year period (2010–2021) on the antimicrobial resistance profile of Pseudomonas aeruginosa from the Arabian Gulf countries (Bahrain, Kuwait, Oman, Qatar, Saudi Arabia, and the United Arab Emirates).
Methods
An electronic literature search was conducted for articles on antimicrobial resistance in P. aeruginosa and associated phenotypes, covering the period of 1st January 2010 to 1st December 2021.
Results
Antimicrobial resistance in the Arabian Gulf was highest to meropenem (10.3–45.7%) and lowest to colistin (0.0–0.8%), among the agents tested. Annual data showed that ceftazidime resistance (Kuwait), piperacillin-tazobactam non-susceptibility (Qatar), and aztreonam, imipenem, and meropenem resistance (Saudi Arabia) increased by 12–17%. Multiple mechanisms of carbapenem resistance were identified and multiple clones were detected, including high-risk clones such as ST235. The most common carbapenemases detected were the VIM-type metallo-β-lactamases.
Conclusions
Among P. aeruginosa in the Arabian Gulf countries, resistance to meropenem was higher than to the other agents tested, and meropenem resistance increased in Saudi Arabia during the study period. Resistance to colistin, a classic antibiotic used to treat Pseudomonas spp. infections, remained low. The VIM-type β-lactamase genes were dominant. We recommend local and regional antimicrobial resistance surveillance programs to detect the emergence of resistance genes and to monitor antimicrobial resistance trends in P. aeruginosa.
Supplementary Information
The online version contains supplementary material available at 10.1007/s44197-024-00191-y.
Keywords: Pseudomonas aeruginosa, Arabian Gulf region, Antimicrobial resistance, Resistance mechanisms, Resistance phenotypes
Introduction
Globally, Pseudomonas aeruginosa is a leading cause of nosocomial infections [1], and in 2019, was estimated to have caused more than 500,000 deaths across 11 infection types, and more than 250,000 deaths associated with antimicrobial resistance [2, 3]. P. aeruginosa is an opportunistic pathogen exhibiting multiple mechanisms of resistance to multiple classes of antibiotics, including efflux pumps, enzymatic degradation, and target site modification [4]. P. aeruginosa is intrinsically-resistant to many antimicrobials, including members of the cephalosporins and fluoroquinolones [4]. As a result, multidrug-resistant (MDR; defined as non-susceptible to ≥1 agent in ≥3 antimicrobial classes [5]) P. aeruginosa has been listed as a ‘serious threat’ [6] and carbapenem-resistant (CR) P. aeruginosa has been designated a ‘Priority 1/critical’ pathogen [7]. Some CR strains produce carbapenemases, with VIM being the most common carbapenemase in P. aeruginosa, globally [8, 9].
P. aeruginosa with difficult-to-treat resistance (DTR-P. aeruginosa; defined as non-susceptible to piperacillin-tazobactam, ceftazidime, cefepime, aztreonam, meropenem, imipenem-cilastatin, ciprofloxacin and levofloxacin [10]) has also been highlighted in treatment guidance from the Infectious Diseases Society of America (IDSA) [11]. Treatment choices for antimicrobial-resistant P. aeruginosa should be dependent on local antimicrobial susceptibility patterns; however, the polymyxins, carbapenems, and aminoglycosides are available antipseudomonal options [4, 11]. For infections caused by DTR-P. aeruginosa, novel agents such as ceftolozane-tazobactam or ceftazidime-avibactam may be prescribed [4, 11].
The Arabian Gulf region is burdened by the same challenges of treating antimicrobial-resistant P. aeruginosa infections as other geographical regions; however, fewer data from this region are available compared with others. Therefore, this review aims to present currently available literature describing the antimicrobial resistance profile of P. aeruginosa and to identify the gaps in data from selected countries of the Arabian Gulf region: Bahrain, Kuwait, Oman, Qatar, Saudi Arabia, and the United Arab Emirates (UAE).
Material and Methods
Search Strategy and Selection Criteria
This review evaluated relevant studies addressing isolates of P. aeruginosa, published between 1st January 2010 and 1st December 2021 on the PubMed (Medline®), PubMed Central and Embase® databases. The search terms included keywords from MeSH and Emtree thesaurus. The primary search term was “Pseudomonas aeruginosa”, including synonyms or variations thereof. In addition, synonyms for the Arabian Gulf region were included, and the Arabian Gulf country names (Bahrain, Kuwait, Oman, Qatar, Saudi Arabia, and the UAE). The mid-search terms relating to the review topics were “resistance” and “infections”, including any synonyms or variations. A free text search with those terms in the title and abstract fields was also performed. Examples of the synonyms or variations for the search terms are shown in Supplementary Table 1.
Accepted publication types included journal articles, systematic reviews, meta-analyses, clinical studies, randomised clinical trials, and global/regional/national reports. Case reports, letters, editorials, notes, conference abstracts, and non-English publications were excluded, as were study abstracts with no mention of P. aeruginosa or <10 isolates tested, unclear methodology, or environmental samples. Extracted study information from each article are presented in Table 1 (study findings) and Supplementary Table 2 (study methodologies). Study data are presented in Table 1, 2, Figs. 2, 3, and Supplementary Tables 3, 4.
Table 1.
Summary table of study findings on antimicrobial resistance in P. aeruginosa from the Arabian Gulf countries (2010–2021)
| Study reference, country | Study aims | P. aeruginosa isolates (N) | Study findings |
|---|---|---|---|
| Joji et al. [16], Bahrain | To study the presence of the metallo‑beta‑lactamase (MbL) genes of VIM family and NDM‑1 in carbapenem‑resistant P. aeruginosa strains | 50 (CR) | Among 40 IPM‑R strains, 21 (52%) were carrying MBL genes. Nineteen (47.5%) strains were positive for the VIM gene; one (2.5%) strain was carrying the NDM‑1 gene, while one strain was carrying both VIM and NDM‑1. No IPM-sensitive strains carried VIM or NDM‑1 genes. This is the first study to report the presence of the VIM family gene and NDM‑1 genes in IPM-R P. aeruginosa isolates in the Kingdom of Bahrain. The study also confirms the multiple drug resistance by the MBL strains |
| Al Rashed et al. [17], Bahrain | To study efflux pump‑mediated fluoroquinolone resistance among P. aeruginosa isolates using phenotypic (E‑test and agar dilution) and genotypic (real‑time‑polymerase chain reaction) methods | 50 (CIP‑R) | Four isolates showed reduction in CIP MIC after addition of carbonyl cyanide 3‑chlorophenylhydrazone. These four isolates showed upregulation of expression of at least one of the four genes by RT‑PCR. The mean gene expression of MexB, MexD, MexF, and MexY increased by 1.6, 4.65, 3.4, and 3.68‑fold, respectively. The results demonstrate the presence and type of efflux pump overexpression |
| Alfouzan et al. [18], Kuwait | To investigate the antimicrobial susceptibility patterns of selected strains (those with MDR profile) of E. coli, K. pneumoniae, and P. aeruginosa, which were isolated from various clinical specimens | 48 | P. aeruginosa isolates presented susceptibility rates of 97.9% to CST; followed by 47.9% to AMK; 39.6% to CZA; and 33.3% to C/T. Only one isolate was found to be CST-R and PDR |
| Alhubail et al. [19], Kuwait | To determine the microbiological profile of diabetic foot ulcers in patients attending Dasman Diabetes Institute clinics in Kuwait and to analyze the distribution of microbial isolates according to wound grade, sex, age and diabetes control | 102 | P. aeruginosa was predominantly found in ulcers with infection and ischemia as reflected by the number of patients in each of the diabetic foot ulcer grades. Antimicrobial susceptibility was highest to MEM (88.4%), AMK (87.0%), IPM (85%), and GEN (80.0%); and was lowest to CAZ (65.7%) |
| Al Rahmany et al. [20], Oman | To identify the prevalence of resistant pathogens and their susceptibility pattern in Northern Oman | 2362 (2 ESBL-producers) | Among all 15,733 isolates. 22.2% were P. aeruginosa. ESBL enzyme production was rare in P. aeruginosa (2/2362 [0.1%] cases). The highest susceptibility of P. aeruginosa was to CST (100%), followed by TZP (93%) and CAZ (90%) |
| Balkhair et al. [21], Oman | To address the monthly cumulative frequencies and prevalence rates of hospital-acquired multidrug-resistant organisms during the year of 2012. Also, to describe the distribution of hospital-acquired multidrug-resistant organisms by site of infection and types of bacteria | 27 | Among all 329 isolated MDR organisms, the percentage of P. aeruginosa was 8.1% |
| Balkhair et al. [22], Oman | To examine the burden of carbapenem colistin resistance in Klebsiella pneumoniae, Pseudomonas aeruginosa, and Acinetobacter baumannii blood isolates, describe trends in carbapenem resistance in blood isolates over a 10-year period, and investigate 30-day all-cause mortality in patients with bacteraemia caused by CR isolates in Oman | 231 (41 CR) | Among all 775 bacteremia isolates, 30% were P. aeruginosa (69% of P. aeruginosa were healthcare-associated and 31% were community-acquired). P. aeruginosa caused 18.1% of all CR bacteremia (88% of which was healthcare-associated and 12% community-associated). The overall rate of carbapenem resistance was 18.6% (41/221); the yearly rate increased from 20% in 2007 to 25% in 2016. All three patients with P. aeruginosa bacteremia that was carbapenem- and CST-R died within 30 days of onset of bacteremia (30-day all-cause mortality, 100%) |
| AbdulWahab et al. [23], Qatar | To describe the frequency of MDR P. aeruginosa recovered from the lower respiratory samples of pediatric and adult cystic fibrosis patients, and its antibiotic resistance pattern to commonly used antimicrobial agents including β-lactams, aminoglycosides, and fluoroquinolones | 61 (12 MDR) | A total of 61 P. aeruginosa samples were isolated from 30 cystic fibrosis patients from 20 families. Twelve (19.7%) sputum samples (seven non-mucoid and five mucoid) were MDR from five patients with moderate-to-very severe lung disease. The MDR P. aeruginosa showed the highest resistance to GEN, AMK and FEP (100%), followed by 91.7% to CIP. None of the isolates were resistant to CST during the study |
| Sid Ahmed et al. [24], Qatar | To assess the prevalence and antimicrobial susceptibility patterns of MDR P. aeruginosa from 5 major hospitals in Qatar | 2533 (205 MDR) | The overall prevalence of MDR P. aeruginosa was 8.1%; most MDR isolates were from patients exposed to antibiotics during 90 days prior to isolation (85.4%, 177/205), and the infections were mainly hospital-acquired (95.1%, 195/205) with only 4.9% from the community. The majority of MDR isolates were resistant to FEP (96.6%, 198/205), CIP, TZP (91%, 186/205), and MEM (90%, 184/205). Patient comorbidities with MDR P. aeruginosa were diabetes mellitus (47.3%, n = 97), malignancy (17.1%, n = 35), end-stage renal disease (13.7%, n = 28) and heart failure (10.7%, n = 22) |
| Sid Ahmed et al., [25], Qatar | To describe how implementation of an institutional multimodal antimicrobial stewardship program affected the susceptibility of P. aeruginosa, the prevalence of MDR P. aeruginosa and antibiotic use in the hospital setting | 6501 (525 MDR) | The overall prevalence of MDR P. aeruginosa was 8.1%, and the yearly prevalence decreased from 9.0% (166/1844) in 2015 (pre-implementation) to 5.5% (122/2234) in 2017 (post-implementation) (P = 0.019). Likewise, resistance of MDR P. aeruginosa decreased to TZP (90.4–80.3%), MEM (89.2–86.9%), CIP (91–88.5%) and AMK (58.4–47.5%). Studied antimicrobial consumption also decreased by 23.9% post-implementation (P = 0.008). The yearly consumption of MEM (P = 0.012), TZP (P < 0.001) and CIP (P = 0.015) significantly decreased from 2014 to 2017 |
| Sid Ahmed et al., [26], Qatar | To investigate the in vitro activity of CZA and C/T against clinical isolates of MDR Pseudomonas aeruginosa from Qatar, as well as the mechanisms of resistance | 205 MDR (of which 10 were sequenced) | Of all MDR P. aeruginosa, susceptibility was 68.8% to CZA, 62.9% to C/T, 59.0% to CZA and C/T, and 27.3% to neither. Less than 50% of XDR isolates were susceptible to CZA or C/T. The 10 sequenced isolates belonged to six different STs and all produced AmpC and OXA enzymes; 5 (50.0%) produced ESBL and 4 (40.0%) produced VIM enzymes. Non-susceptibility to CZA and C/T was largely due to the production of ESBL and VIM enzymes |
| Sid Ahmed et al., [27], Qatar | To identify the predominant STs and β-lactamase genes in clinical isolates of MDR-P. aeruginosa from Qatar | 75 MDR | The highest susceptibility was to CZA (48%), followed by C/T (40%). Most isolates possessed Class C and/or Class D β-lactamases (96% each), while MBLs were detected in 26.7%. Eight (40%) MBL-producers were susceptible to ATM and did not produce any concomitant ESBLs. High-risk ST235 (21.3%), ST357 (10.7%), ST389 and ST1284 (8% each) were most frequent. Most ST235 isolates (93.8%) were resistant to all tested β-lactams and had an MDR phenotype |
| Tawfik et al. [28], Saudi Arabia | To determine the prevalence rate of classes A, B and D β-lactamases among extended-spectrum cephalosporin-non-susceptible Pseudomonas aeruginosa clinical isolates from burned patients | 156 (35 CAZ-R were tested for EBSLs and MBLs) | The CAZ resistance rate was 22.4%. CAZ-R isolates had resistance rates to piperacillin, TZP, FEP, ATM, IPM, AMK, GEN and CIP of 100%, 71.1%, 88.6%, 48.6%, 70.0%, 82.5%, 87.5%, and 90.0% respectively. No resistance was detected to polymyxine B. The prevalence of ESBL and MBL in CAZ-R P. aeruginosa was 69.4% and 42.9%, respectively. VEB-1 (68%) and OXA-10 (56%) are the predominant ESBL genes in CAZ-R P. aeruginosa and blaVIM is the dominant MBL gene (100%). OXA-10 like gene was concomitant with VEB, GES and/or VIM but PER was not detected |
| Al-Agamy et al. [29], Saudi Arabia | To profile ESBLs and MBLs in clinical isolates of P. aeruginosa resistant to CAZ at a hospital in Riyadh | 200 (39 CAZ-R were tested for EBSLs and MBLs) | Resistance was highest to GEN (41%), ticarcillin (35%), piperacillin (32.5%), and CIP (30%). All isolates were sensitive to CST. Among the 39 CAZ-R isolates, 59.0% were ESBL positive, of which 87.0% carried blaVEB and 21.7% carried blaGES genes. Among the 39 CAZ-R isolates, 41.0% had MBLs, all of which carried blaVIM genes. The collection was not dominated by any single clone. This dominance of acquired CAZ-inactivating β-lactamases rather than being attributable to AmpC and efflux |
| Somily et al. [30], Saudi Arabia | To examine susceptibility of P. aeruginosa and Acinetobacter baumannii against carbapenems along with CST and tigecycline as alternative therapeutic options | 33 MDR | Most MDR P. aeruginosa were resistant to IPM (90.9%), and MEM (81.8%), with only 39.4% resistant to doripenem. Colistin had excellent activity against P. aeruginosa (93.9% susceptibility). Among the carbapenems, doripenem was found to be the most potent against P. aeruginosa, and CST proved to be an effective alternative antimicrobial agent for treatment of P. aeruginosa. |
| Memish et al. [31], Saudi Arabia | To report the first national molecular characterization of carbapenemase production among the main Gram-negative bacteria in the Kingdom, namely members of the Enterobacteriaceae family and the non-fermenters P. aeruginosa and A. baumannii | 39 IPM-R, MEM-R and CAZ-R (11 CP) | VIM is the most prevalent MBL in P. aeruginosa, in 8/11 CP isolates, with blaVIM-2 detected in 54.5%. We detected MBLs in only 20% of the CR P. aeruginosa, suggesting that resistance in the majority of the isolates was due to other mechanisms |
| Khan & Faiz [32], Saudi Arabia | To determine the pattern of antimicrobial resistance of P aeruginosa | 121 | Overall drug resistance was low to moderate to commonly used anti-pseudomonal drugs (4.9–30.6%). Significantly less resistance was exhibited by TZP (4.9%; P < 0.05) and MEM showed significantly high resistance (30.6%; P < 0.05) as compared to other antibiotics, followed by ticarcillin (22.3%) and IPM (19%), irrespective of the site of infection. Antibiotics with < 10% resistance were FEP (8.3%), AMK (7.4%) and TZP (4.9%). Although, data varied between hospitals, MEM and ticarcillin had the highest drug resistance In all hospitals. Multidrug resistance was 10.7%. This pattern of resistance indicates probable overuse of broad-spectrum antibiotics like carbapenems |
| Ibrahim [33], Saudi Arabia | To determine the distribution and resistance profiles of Gram-negative bacteria in ICUs at King Abdullah Hospital in Bisha, Saudi Arabia | 69 | P. aeruginosa showed low to moderate resistance rates for aminoglycosides (18.8% to AMK; 20% to tobramycin, 31.7% to GEN). Higher resistance rates were observed to cephalosporins, ATM, MEM, piperacillin, and TZP. Multidrug resistance was 60.9%. P. aeruginosa was commonly isolated from ICU infections in this tertiary hospital |
| Alhussain et al. [34], Saudi Arabia | To determine the risk factors, antimicrobial susceptibility pattern and patient outcomes of P. aeruginosa infection in ICU | 90 | The study included 90 cases and 90 controls. Cases had significantly higher mean (SD) ICU days stay compared with controls; 37.7 (37.8) and 8.37 (8.7) respectively; P = 0.001. Resistance was highest to IPM (41.1%) and MEM (27.8%), while 36.7% were MDR. Mortality was similar in both groups: 54 (60.0%) cases and 51 (56.7%) controls; P = 0.650. In the final multivariate model, factors independently associated with P. aeruginosa were ICU duration, previous surgery, having invasive indwelling devices (tracheostomy tube and urethral catheter), previous surgery and duration of stay in the ICU, and prior use of aminoglycosides |
| Bukhari et al. [35], Saudi Arabia | To reduce VAP incidence rate, lessen the cost of care, and correlate VAP bundles compliance with VAP incidence rate | Not reported | The predominant pathogen was P. aeruginosa, (30.8% of all isolates), of which 93.1% were MDR |
| Ayoub Moubareck et al. [36], UAE | To investigate mechanisms of carbapenem resistance and genetic relatedness of P. aeruginosa isolates recovered in Dubai hospitals | 37 (carbapenem-NS) | Of 1969 P. aeruginosa isolated during the study period, 471 (23.9%) showed reduced carbapenem susceptibility. Of these, 37 were analyzed and 32% of them produced VIM-type MBLs, including VIM-2, VIM-30, VIM-31, and VIM-42, while GES-5 and GES-9 co-existed with VIM in 5.4% of isolates. Outer membrane impermeability was observed in 73% of isolates and 75.6% displayed overproduced MexAB-OprM. Sequencing revealed one large clone including most CP isolates indicating clonal dissemination. This is the first study on carbapenem NS P. aeruginosa from Dubai to show VIM production as well as outer membrane permeability and efflux systems as resistance mechanisms |
| Alatoom et al. [37], UAE | To compare the activity of C/T and CZA against 120 bacterial strains, including ESBL-producers, CR Enterobacteriaceae, and P. aeruginosa, isolated from patients admitted to Cleveland Clinic Abu Dhabi, UAE | 31 | Twenty-nine (94%) P. aeruginosa isolates were susceptible to CZA (MIC50, 1.5 µg/ml), whereas 30 (97%) isolates were susceptible to C/T (MIC50, 0.75 µg/ml). Overall, C/T and CZA showed comparable activity against P. aeruginosa |
| Sid Ahmed et al. [38], Qatar | To investigate the clinical impact and molecular epidemiology of MDR P. aeruginosa in Qatar over a 3-year period | 8892 (525 MDR, of which 78 were sequenced) | The overall prevalence of MDR P. aeruginosa was 5.9% (525/8892), with the yearly prevalence ranging from 8.1% in 2014 to 4.8% in 2017. MDR isolates demonstrated > 86% resistance to FEP, CIP, MEM and TZP, but 97.5% susceptibility to CST. There were 29 different STs: 20.5% ST235, 10.3% ST357, 7.7% ST389, and 7.7% ST1284. ST233 was associated with bloodstream infections and increased 30-day mortality. All ST389 isolates were obtained from patients with cystic fibrosis |
| Al-Agamy et al. [39], Saudi Arabia | To describe various molecular and epidemiological characters determining antibiotic resistance patterns in P. aeruginosa isolates | 34 (CR) | All isolates were CAZ-R. VEB-1 (47.1%) and OXA-10 (41.2%) were the most prevalent ESBL and penicillinase, respectively. VIM-1, VIM-2, VIM-4, VIM-11, VIM-28, and IMP-7 were found in MBL-producers. A decrease in outer membrane porin gene (oprD) expression was seen in nine isolates, and an increase in efflux pump gene (MexAB) expression was detected in five. Six serotypes (O:1, O:4, O:7, O:10, O:11, and O:15) were found among the 34 isolates. The predominant serotype was O:11 (16 isolates), followed by O:15 (nine isolates). These results revealed diverse mechanisms conferring carbapenem resistance to P. aeruginosa isolates from Saudi Arabia |
| Abdalhamid et al. [40], Saudi Arabia | To detect the prevalence of gastrointestinal tract colonization of CR Enterobacteriaceae and CR P. aeruginosa in patients admitted to intensive care units in Saudi Arabia | 13 (CR) | An NDM type gene was detected in four CR P. aeruginosa isolates and a VIM type gene in one isolate. AmpC overexpression was detected in eight CR P. aeruginosa isolates. It is possible that ampC overexpression was due to overuse of β-lactam agents such as CAZ, which can cause derepression of ampC |
| Somily et al. [41], Saudi Arabia | To estimate the prevalence and resistance trends of isolated non-fermenting Gram-negative bacteria in Saudi Arabia | 73,728 | P. aeruginosa was the most common Gram-negative pathogen isolated. Resistance trends of P. aeruginosa were increasing for ATM (absolute increase during the study was 17.3%), IPM (12.3%), and MEM (11.6%). Resistance trends were decreasing for netilmicin (absolute decrease during the study was − 10.0%), AMK (− 5.9%), and tobramycin (− 5.0%). The resistance trends of other tested drugs were generally stable with < 5% change. These included CIP, TZP, CAZ, levofloxacin, FEP, CST, and GEN |
| Al-Tawfiq et al. [42], Saudi Arabia | To present antibiotic resistance pattern of Gram-negative bacteria over 6 years (2013–2018) in a hospital in Saudi Arabia | 4210 | Overall susceptibility of P. aeruginosa to CAZ was 81–92%, and was 84–91% for FEP, 70–82% for IPM, 92–98% for AMK, and 72–86% for CIP. The susceptibility of P. aeruginosa decreased over time (2013–2018) to ceftriaxone, CAZ, and MEM but remained stable to FEP, AMK, CIP, and slightly improved to GEN and trimethoprim-sulfamethoxazole |
AMK amikacin, AmpC ampicillin class C, ATM aztreonam, CAZ ceftazidime, CIP ciprofloxacin, CP carbapenemase-producing, CR carbapenem-resistant, CST colistin, C/T ceftolozane-tazobactam, CZA ceftazidime-avibactam, FEP cefepime, GEN gentamicin, ICU intensive care unit, IMP imipenemase, IPM imipenem, MBL metallo‑β‑lactamase, MDR multidrug-resistant, MEM meropenem, MIC minimum inhibitory concentration, NS non-susceptible, OXA oxacillinase, PDR pandrug-resistant, R resistant, SD standard deviation, ST sequence type, TZP piperacillin-tazobactam, UAE United Arab Emirates, VEB Vietnamese extended-spectrum β-lactamase, VIM Verona integron-encoded metallo-β-lactamase, XDR extensively drug-resistant
Table 2.
Rates of antimicrobial resistance or non-susceptibility among P. aeruginosa from Kuwait, Qatar, Saudi Arabia, and the UAE (2011–2021)
| Country/antimicrobial agent | % resistant (Kuwait, Saudi Arabia, the UAE) or non-susceptible (Qatar) P. aeruginosa of totala | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | |
| Kuwaitb | |||||||||||
| AMK | – | 1.9 | 10.8 | 8.9 | 12.2 | 9.6 | 10.5 | 15.8 | 14.8 | 10.9 | 5.1 |
| CAZ | – | 7.4 | 20.0 | 22.8 | 18.7 | 17.6 | 25.2 | 19.7 | 27.4 | 24.0 | 22.5 |
| FEP | – | 7.4 | 20.0 | 17.8 | 14.6 | 15.4 | 21.7 | 18.4 | 21.5 | 20.9 | 13.0 |
| LVX | – | 18.5 | 21.5 | 20.8 | 25.2 | 26.5 | 28.0 | 26.3 | 32.6 | 20.2 | 18.1 |
| MEM | – | 24.1 | 30.8 | 26.7 | 23.6 | 35.3 | 34.3 | 35.5 | 28.9 | 23.3 | 16.7 |
| TZP | – | 7.4 | 18.5 | 22.8 | 16.3 | 16.2 | 20.3 | 18.4 | 20.0 | 18.6 | 14.5 |
| Total isolates tested (N) | 1 | 54 | 65 | 101 | 123 | 136 | 143 | 76 | 135 | 129 | 138 |
| Qatarc | |||||||||||
| AMK | 5 | 6 | 7 | 7 | 3 | 0 | 4 | 5 | 2.6 | 10.3 | 0.0 |
| CAZ | 25 | 25 | 26 | 26 | 16 | 26 | 27 | 24 | 26.3 | 51.3 | 43.6 |
| FEP | 26 | 24 | 23 | 20 | 22 | 25 | 34 | 30 | 23.7 | 46.2 | 46.2 |
| LVX | – | – | – | – | – | – | – | – | 21.1 | 43.6 | 48.7 |
| MEM | 26 | 33 | 34 | 22 | 14 | 38 | 37 | 30 | 36.8 | 69.2 | 56.4 |
| TZP | 15 | 26 | 28 | 22 | 22 | 31 | 35 | 28 | 28.9 | 56.4 | 48.7 |
| Total isolates tested (N) | 390 | 383 | 213 | 155 | 1668 | 38 | 80 | 99 | 38 | 39 | 39 |
| Saudi Arabiad | |||||||||||
| AMK | 13.2 | 5.0 | 35.0 | – | 0.0 | 5.0 | – | 7.7 | 5.1 | 4.9 | 0.0 |
| CAZ | 23.7 | 35.0 | 50.0 | – | 10.5 | 15.0 | – | 23.1 | 12.8 | 17.1 | 5.9 |
| FEP | 13.2 | 30.0 | 50.0 | – | 5.3 | 10.0 | – | 15.4 | 15.4 | 9.8 | 2.9 |
| LVX | 23.7 | 50.0 | 55.0 | – | 5.3 | 10.0 | – | 26.9 | 23.1 | 17.1 | 5.9 |
| MEM | 10.5 | 40.0 | 50.0 | – | 21.1 | 15.0 | – | 30.8 | 25.6 | 19.5 | 2.9 |
| TZP | 10.5 | 35.0 | 30.0 | – | 5.3 | 10.0 | – | 11.5 | 12.8 | 14.6 | 2.9 |
| Total isolates tested (N) | 38 | 20 | 20 | – | 19 | 20 | – | 26 | 39 | 41 | 34 |
| UAEe | |||||||||||
| AMK | 4.7 | 3.8 | 4.7 | 4.9 | 5.0 | 5.8 | 4.9 | 3.9 | 3.5 | 2.9 | – |
| CAZ | 7.7 | 6.7 | 8.5 | 9.6 | 10.0 | 10.2 | 10.3 | 8.5 | 8.3 | 8.5 | – |
| FEP | 7.0 | 5.3 | 6.4 | 7.2 | 8.0 | 8.4 | 7.8 | 6.5 | 6.2 | 6.0 | – |
| LVX | – | – | – | – | – | – | – | – | – | – | – |
| MEM | 10.2 | 9.1 | 12.0 | 14.7 | 14.4 | 16.0 | 14.5 | 11.0 | 10.7 | 10.3 | – |
| TZP | 10.5 | 11.1 | 10.6 | 13.5 | 13.3 | 13.7 | 11.9 | 6.9 | 6.9 | 6.7 | – |
| Total isolates (N) | 1753 | 2030 | 2521 | 3174 | 4132 | 4913 | 6445 | 7989 | 8989 | 9402 | – |
AMK amikacin, CAZ ceftazidime, FEP cefepime, LVX levofloxacin, MEM meropenem, TZP piperacillin-tazobactam, UAE United Arab Emirates
–, no data collected for these years or agents
aRates are presented as the percentage of resistant or non-susceptible P. aeruginosa (determined using CLSI breakpoints [64]) of the total isolates collected. Percentages not given when N < 10 isolates. All rates are presented to 1 decimal place, with the exception of the non-susceptibility data from Qatar for 2011–2018 [56]
bKuwait resistance data from the ATLAS database [53]
cQatar 2011–2018 non-susceptibility data provided by Hamad Medical Corporation [56]. 2019–2021 non-susceptibility data from the ATLAS database [53]
dSaudi Arabia resistance data from the ATLAS database [53]
eUAE resistance data provided by UAE MOHAP [57]
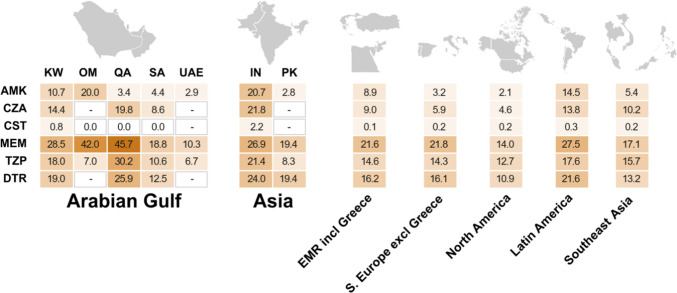
Fig. 2.
Rates of antimicrobial resistance (resistance data from the ATLAS database [53], except for the UAE [57]) or nonsusceptibility (non-susceptibility data from Oman presented to 1 decimal place but presented to the nearest whole number in the publication [20]) and difficult-to-treat resistance (DTR data from the ATLAS database [53]) among P. aeruginosa (2016–2021). Rates of antimicrobial resistance or non-susceptibility were presented as the percentage of resistant or non-susceptible P. aeruginosa (determined using CLSI breakpoints [64]) of the total isolates collected. DTR was defined as resistance to >1 antimicrobial in each of the following classes: cephalosporins (ceftazidime, cefepime or ceftriaxone), carbapenems (imipenem, meropenem, doripenem or ertapenem), and quinolones (ciprofloxacin or levofloxacin). Total isolate numbers [years of collection] were: KW, 757 (CZA, CST: 721) [2016–2021]; OM, 2362 [2016 and 2017]; QA, 116 [2019–2021]; SA, 160 (CZA, CST: 140) [2016, 2018–2021]; UAE, 9402 [2020]; IN, 1405 (CZA and CST: 1365) [2016, 2018–2021]; PK, 36 [2016 and 2017]; EMR incl Greece (Greece, Jordan, Israel, and Turkey), 2561 (CZA and CST: 2413) [2016–2021]; S. Europe excl Greece (Croatia, Italy, Portugal, Serbia and Spain), 6185 (CZA and CST: 5063) [2016–2021]; North America (Canada and United States), 5601 (CZA and CST: 4876) [2016–2021]; Latin America (Argentina, Brazil, Chile, Colombia, Costa Rica, Dominican Republic, Mexico, Panama and Venezuela), 6380 (CZA and CST: 5808) [2016–2021]; and Southeast Asia (Malaysia, Philippines, Singapore, Thailand and Vietnam), 2126 (CZA and CST: 2027) [2016–2021]). AMK, amikacin; CZA, ceftazidime-avibactam; CST, colistin; DTR, difficult-to-treat resistance; EMR, Eastern Mediterranean region; excl, excluding; IN, India; incl, including; KW, Kuwait; MEM, meropenem; OM, Oman; PK, Pakistan; QA, Qatar; S., Southern; SA, Saudi Arabia; TZP, piperacillin-tazobactam; and UAE, United Arab Emirates. -, no data collected for these antimicrobial agents in the selected countries
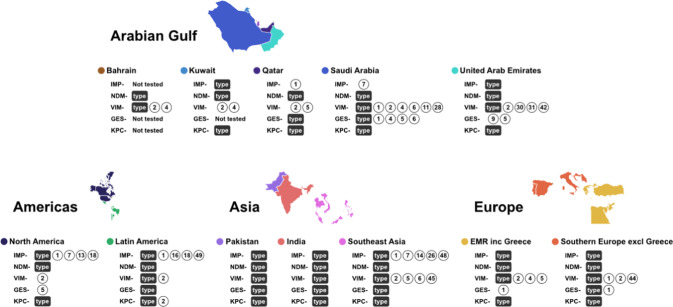
Fig. 3.
Distribution of β-lactamase genes among P. aeruginosa from the Arabian Gulf countries and other countries/regions (2010–2021) (genotype data from each country/region are shown in Supplementary Table 4). Circles show the genotype number of each β-lactamase gene detected in a country or region and ‘type’ represents an identified β-lactamase gene that has not been sub-typed. EMR, Eastern Mediterranean Region; inc, including; excl, excluding; NDM, New Delhi metallo-β-lactamase; VIM, Verona integron-encoded metallo-β-lactamase; IMP, imipenemase; GES, Guiana extended-spectrum; KPC, Klebsiella pneumoniae carbapenemase; and UAE, United Arab Emirates
Studies Included in This Review
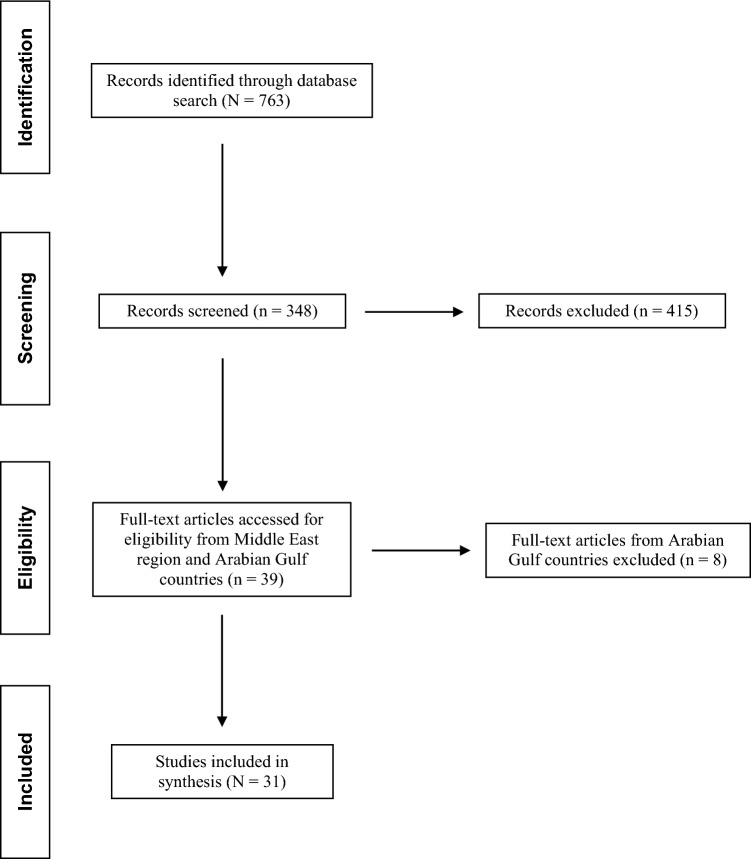
Following initial identification and screening of publication titles, 34 full-text articles included data on the Middle East region [8, 9, 12–15, 50] or the Arabian Gulf countries (Bahrain, 2; Kuwait, 2; Oman, 3; Qatar, 6; Saudi Arabia, 12; and the UAE, 2) [16–34, 36–42] (Fig. 1). For the Arabian Gulf countries, there were 22 prospective studies (Bahrain: [16, 17]; Kuwait: [18]; Qatar: [23–27, 38]; Saudi Arabia: [28–32, 34, 35, 39–42]; and UAE: [36, 37]) and 5 retrospective studies (Kuwait: [19]; Oman: [20–22]; and Saudi Arabia: [33]). Several studies included data on other species and were presented separately from the P. aeruginosa subset (Kuwait: [18, 19]; Oman: [20–22]; and UAE: [37]).
Fig. 1.
Flow chart for selection of publications on P. aeruginosa from the Arabian Gulf countries and other countries/regions (2010–2021)
Across the 26 Arabian Gulf studies with documented isolate numbers, a total of 101,839 P. aeruginosa isolates contributing data on antimicrobial resistance were distributed as follows: Bahrain, 100 isolates (0.1%) [16, 17]; Kuwait, 150 isolates (0.1%) [18, 19]; Oman, 2620 isolates (2.6%) [20–22]; Qatar, 18,267 isolates (17.9%) [23–27, 38]; Saudi Arabia, 78,702 isolates (77.3%) [28–34, 39–42]; and the UAE, 2000 isolates (2.0%) [36, 37]. These studies were most frequently set in hospital wards (50.0%), followed by a mixture of hospital wards, community settings and ICUs (34.6%). Most studies collected isolates from a variety of culture sources associated with infection (76.9%; including blood, lower respiratory tract, and skin and soft tissue), with only three studies (11.5%) including a proportion of isolates associated with no infection (from colonized patients). Automated antimicrobial susceptibility testing was most frequently used (57.7%), followed by disk diffusion (23.1%), and broth microdilution methodology or E-test (3.8% each). Almost all of these studies used CLSI breakpoints to interpret MIC results (92.3%).
Antimicrobial Surveillance Data from the ATLAS Program
In addition to the published studies that met the eligibility criteria, this review included global antimicrobial surveillance data from the Antimicrobial Testing Leadership and Surveillance (ATLAS) program (accessible through a publicly available database [53]). The ATLAS program is industry-sponsored and aims to monitor and assess the in vitro activities of selected antimicrobial agents against clinical bacterial isolates collected from hospitalized patients worldwide. The ATLAS program annually collects a prerequisite number of nonduplicate bacterial isolates of clinically significant species (one isolate per species per patient) from documented infection types (intra-abdominal, urinary tract, skin and soft tissue, lower respiratory tract, and bloodstream) [8, 9, 12].
This review presented ATLAS data from other countries and regions, in addition to a total of 1474 isolates from the Arabian Gulf countries (Kuwait, 1101 isolates; Qatar, 116 isolates; and Saudi Arabia, 257 isolates) presented in Table 2 and Fig. 2 [53].
Antimicrobial Resistance in Pseudomonas aeruginosa
Rates of Antimicrobial Resistance and Phenotypes from the Middle East/Arabian Gulf Region
Figure 2 presents data on the rates of antimicrobial resistance and DTR phenotypes among isolates of P. aeruginosa from the Arabian Gulf countries, and other countries or regions [20, 43, 57]. The highest resistance rates observed in each Arabian Gulf country, and the others presented, were to meropenem, ranging from 10.3% (UAE) to >40.0% in Oman and Qatar (higher than the other countries and regions) (Fig. 2). The meropenem resistance rates in Oman and Qatar are reflective of single center data and not necessarily indicative of the resistance status in the country as a whole. Colistin resistance was low (<2.2%) globally (Fig. 2). Amikacin resistance was <5% in Qatar, Saudi Arabia, and the UAE (similar to Southern Europe, North America and Southeast Asia), but higher in Kuwait (10.7%) and Oman (20.0%). There were lower rates of DTR-P. aeruginosa (10.9–13.2%) in North America, Saudi Arabia, and Southeast Asia; rates of 16% in Southern Europe and EMR; and rates of 19.0–25.9% elsewhere (data not collected in Oman or the UAE; Fig. 2). Published rates of antimicrobial resistance or susceptibility from the Arabian Gulf countries, and other countries or regions are presented in Supplementary Table 3 [8–10, 12–20, 23, 24, 26–30, 32–34, 36, 37, 41–44].
The rates of antimicrobial susceptibility among a collection of P. aeruginosa isolates from Middle East countries (Israel, Jordan, Kuwait, and Saudi Arabia) ranged from 62.8% (levofloxacin) to >90% (amikacin and colistin) [12], according to the European Committee on Antimicrobial Susceptibility Testing (EUCAST) 2020 breakpoints [54]. However, there was no susceptibility breakpoint, and only intermediate or resistance breakpoints, for colistin when using Clinical and Laboratory Standards Institute (CLSI) 2020 breakpoints [55]. Susceptibility to ceftazidime-avibactam and ceftolozane-tazobactam was >90% in the Middle East and Middle East-Africa regions [12, 13].
MDR rates among. P. aeruginosa were 30.6% and 38.1%, and the rate with a DTR phenotype was 7.4% for the Middle East region [12, 14]. Among MDR P. aeruginosa isolates, cefepime, meropenem and piperacillin-tazobactam susceptibility was 30–50%, which decreased to 0% among DTR isolates [12]. A 2016–2018 ATLAS surveillance study reported that no isolates of carbapenemase-producing P. aeruginosa collected in the Middle East-Africa region were resistant to colistin, whereas 32.3% were resistant to aztreonam, and ≥92.3% were resistant to the other tested agents, including amikacin, ceftazidime-avibactam, imipenem and meropenem [9]. These findings reflected the high proportions of MBL-positive isolates that were detected in all regions included in the study [9]. Rates of meropenem non-susceptibility were 25–35% among P. aeruginosa collected in the Middle East and Africa [12, 13, 15]. Among meropenem-non-susceptible respiratory P. aeruginosa isolates collected from adult intensive-care unit (ICU) patients in the Middle East-Africa region, susceptibility was 68.1% to ceftolozane-tazobactam, 34.9% to ceftazidime, and 28.2% to piperacillin-tazobactam [15].
In the above studies, the range of countries comprising the Middle East-Africa region (including Egypt, Israel, Jordan, Kenya, Kuwait, Lebanon, Morocco, Qatar, South Africa, and Tunisia) were from a wide range of social and economic settings. Antimicrobial susceptibility or resistance data and reports on P. aeruginosa isolates from the individual Arabian Gulf countries are described below. The main study findings are summarized in Table 1 and data presented in Supplementary Table 3.
Bahrain, Kuwait and Oman
More than 80% of ciprofloxacin-resistant P. aeruginosa isolates from Bahrain were also resistant to imipenem, meropenem and piperacillin-tazobactam; however, none were resistant to colistin [16, 17]. Similarly, high resistance rates to meropenem (≥87.5%) and low resistance rates to colistin (2.1%) were observed among MDR P. aeruginosa isolates from Kuwait (one of which was pandrug-resistant [PDR]; defined as resistant to all antimicrobial agents [5]) [18]. The rates of susceptibility to amikacin, ceftazidime, ciprofloxacin, imipenem and piperacillin-tazobactam were also notably lower in the study of MDR P. aeruginosa from Kuwait, compared with non-MDR isolates [18]. Conversely, P. aeruginosa from diabetic foot infections, collected in Kuwait, exhibited susceptibility rates of ≥65.7% to ceftazidime, meropenem, gentamicin, imipenem, and amikacin [19].
In Oman, extended-spectrum β-lactamase (ESBL) enzyme production was only detected in 2 of 2362 P. aeruginosa isolates collected [20]. The lowest rate of susceptibility among P. aeruginosa from Oman was to meropenem (58.0%), with ≥80.0% of isolates susceptible to amikacin, ceftazidime, ciprofloxacin, gentamicin and piperacillin-tazobactam. All isolates were susceptible to colistin. Another study in Oman found that 8.1% of all MDR isolates from a tertiary care teaching hospital were P. aeruginosa [21]. In the same hospital, the rate of CR P. aeruginosa in bacteremia was 22% between 2012 and 2016, with a rate of 43% reported in 2015 alone [22].
Qatar
Among P. aeruginosa from cystic fibrosis patients in Qatar, antimicrobial non-susceptibility ranged from 9.8% (piperacillin-tazobactam) to 41.0% (gentamicin); all isolates were susceptible to colistin [23]. Meropenem non-susceptibility was 11.5% and meropenem resistance was 58.3% among MDR isolates. Among the MDR subset, resistance rates ranged from 50.0% (piperacillin-tazobactam) to 100% (gentamicin, amikacin and cefepime), whereas none of the MDR isolates were resistant to colistin [23].
In a multi-hospital study, the rate of MDR isolates collected in Qatar between 2014 and 2015 was 8.1% (2.4% of which were PDR) [24]. The rate of MDR P. aeruginosa at one of these hospitals before the implementation of an antimicrobial stewardship program was 9.0% and was 5.5% after implementation [25]. Most MDR P. aeruginosa isolates were resistant to cefepime, ciprofloxacin, piperacillin-tazobactam and meropenem (>90%); in addition, aminoglycoside resistance was 50–75%, and 3.4% were colistin-resistant [25]. Non-susceptibility to ceftazidime-avibactam and ceftolozane-tazobactam was 31.2% and 37.1%, respectively, among MDR P. aeruginosa [26]. The authors attributed ceftazidime-avibactam and ceftolozane-tazobactam non-susceptibility rates among the MDR isolates in their study to the production of ESBL and VIM enzymes [26]. Among a smaller subset of eight MDR isolates that produced metallo-β-lactamases (MBLs), but not ESBLs, all were susceptible to aztreonam but resistant to the other agents studied [27].
Saudi Arabia
Two studies of P. aeruginosa isolates reported low resistance to ceftazidime-clavulanic acid (<10%) and high resistance to gentamicin (41%) [28, 29]. All isolates were susceptible to colistin. In a single-center study of 156 P. aeruginosa isolates, 22.4% were ceftazidime-resistant, of which 71.4% were ESBL-producers and 42.9% were MBL-producers [28]. Thirty-nine (19.5%) of 200 clinical P. aeruginosa isolates collected at another center were ceftazidime-resistant, most of which were also resistant to other tested agents; however, all isolates were susceptible to colistin [29]. In a single-center study of 33 MDR P. aeruginosa isolates, the rates of resistance to colistin and the carbapenems were 6.1% (colistin), 39.4% (doripenem), 81.8% (meropenem), and 90.9% (imipenem) [30]. In a multi-hospital study, the percentage of carbapenemase production among 39 ceftazidime- and carbapenem-resistant isolates of P. aeruginosa collected was 28.2% [31].
Another multicenter study statistically compared the overall resistance rates to tested agents among 121 P. aeruginosa isolates [32]. The rate of resistance to piperacillin-tazobactam (4.9%) was significantly lower than to ceftazidime, levofloxacin, aztreonam, ciprofloxacin, piperacillin, imipenem, ticarcillin and meropenem (P < 0.05). In contrast, the rate of resistance to meropenem (30.6%) was significantly higher than to piperacillin-tazobactam, amikacin, cefepime, gentamicin, ceftazidime, levofloxacin, aztreonam, ciprofloxacin, piperacillin and imipenem (P < 0.05). The overall MDR rate was 10.7% [32]. A higher rate of meropenem resistance was observed among respiratory isolates than among other infection types (41.5%; P < 0.05).
P. aeruginosa isolates from three different ICUs in one hospital showed the lowest rates of resistance to the class of aminoglycosides (amikacin [18.8%], tobramycin [20.0%] and gentamicin [31.7%]), while 30.0% of isolates were resistant to colistin [33]. The study recorded a multidrug resistance rate of 60.9% among P. aeruginosa [33]. Similarly, the resistance rates among P. aeruginosa isolates from seven ICUs ranged from 8.9% (cefepime) to 41.1% (imipenem). The rate of meropenem resistance was 27.8% [34]. In that ICU study, 36.7% of 90 P. aeruginosa isolates collected were MDR [34]. A higher rate of 93.1% MDR P. aeruginosa isolates were associated with ventilator-associated pneumonia (VAP) in another ICU study in Saudi Arabia [35].
United Arab Emirates
A total of 1969 P. aeruginosa were collected in a cross-sectional multicenter study, of which 23.9% of isolates were identified as carbapenem-non-susceptible [36]. Among a subset of 37 carbapenem-non-susceptible isolates that underwent molecular characterization, 10.8% of isolates were MDR and 37.8% were XDR. No study isolates were characterized as PDR because all were susceptible to colistin [36]. A single-center study of 31 P. aeruginosa isolates reported rates of resistance ranging from 16.1% (gentamicin) to 51.6% (meropenem) [37]. High susceptibility was reported to ceftazidime-avibactam and ceftolozane-tazobactam among all P. aeruginosa isolates (93.5% and 96.8%, respectively).
Studies on Molecular Resistance Mechanisms from the Middle East/Arabian Gulf Regions
Figure 3 (data shown in Supplementary Table 4) shows the distribution of β-lactamase genes among P. aeruginosa from the Arabian Gulf countries, and other countries or regions. The variety of documented VIM and GES genes appears to be greater in the countries of the Arabian Gulf, compared with the other countries and regions. In contrast, fewer IMP-type genes were reported in the Arabian Gulf, compared with North America, Latin America, and Southeast Asia. Fewer types of NDM and KPC genes were documented among P. aeruginosa in the Arabian Gulf and the other countries and regions (Fig. 3, Supplementary Table 4). Molecular characterization studies conducted in the individual Arabian Gulf countries are described below.
Bahrain, Kuwait and Qatar
The upregulated expression of genes mexB, mexD, mexF and mexY was identified in 8% of tested ciprofloxacin-resistant P. aeruginosa isolates [17]. The same isolates also showed a decrease in ciprofloxacin minimum inhibitory concentration (MIC) by the efflux pump inhibitor carbonyl cyanide 3-chlorophenylhydrazone. Among imipenem-resistant P. aeruginosa isolates collected from community, hospital, and ICU patients in Bahrain, 52.5% carried MBL genes; mostly VIM-type (90.4%) [16]. One isolate was NDM‑1-positive, and one isolate carried both VIM and NDM‑1 genes.
Data on the β-lactamase genes carried by P. aeruginosa isolates in Kuwait are scarce. A global antimicrobial surveillance study that included countries in the Middle East-Africa region showed that 11 isolates of VIM-2-positive and 3 VIM-4-positive P. aeruginosa were collected in Kuwait [8].
Among 75 MDR (defined according to [5]) P. aeruginosa isolates from two centers in Qatar, 96.0% possessed class C and/or class D β-lactamases, while MBLs were detected in 26.7% of the isolates (blaVIM-2, blaVIM-5 and blaIMP-2) [27]. One (1.3%) isolate co-carried both blaVIM-2 and blaIMP-1 and all four β-lactamase classes were present in three (4.0%) isolates. The ESBL gene blaVEB-9 (formerly known as blaVEB-1a) was identified as the most frequent ESBL gene (25.3%). High-risk clones ST235 (21.3%), ST357 (10.7%), ST389 and ST1284 (8.0% each) were mostly identified. Most ST235 isolates (93.8%) were resistant to all tested β-lactams. In an additional study from Qatar, sequencing of 78 MDR P. aeruginosa revealed 29 different sequence types with the predominance of ST235 (20.5%), followed by ST357 (10.3%), and ST389 and ST1284 (7.7% each) [38]. ST233 was associated with bloodstream infections and increased 30-day mortality, while all ST389 were isolated from cystic fibrosis patients.
Saudi Arabia
Two studies found that blaVEB genes were predominantly harbored by phenotypically ESBL-positive P. aeruginosa isolates (68.0% and 87.0%, respectively) [28, 29]. Tawfik et al. [28] also identified blaOXA-10 genes in 56.0% of ESBL-producing isolates, followed by blaGES in 20.0%. Both studies found that all MBL-producing P. aeruginosa isolates carried blaVIM genes but neither study found blaPER, blaTEM, blaSHV or blaCTX-M among the ESBL genes, nor blaIMP, blaGIM, blaSIM, blaSPM or blaNDM among the MBL genes [28, 29]. Tawfik et al. [28] suggested that the higher percentage of blaVEB than blaOXA-10 and blaGES ESBL genes could be due to residents from regions with a higher prevalence of blaVEB genes (such as blaVEB-1 in Southeast Asia) living in Saudi Arabia. In addition, the collection of clinical P. aeruginosa isolates was not dominated by any single clone and the identification of multiple bla genes did not solely reflect the spread of a single outbreak strain [28, 29].
A subsequent study by Al-Agamy et al. [39] also found that the predominant ESBL was VEB-1 (47.1%), followed by OXA-10 (41.2%) and GES (8.8% [GES-1, GES-4 and GES-6]) among CR P. aeruginosa isolates. As previously found, the most common MBLs were VIM-type, but in this later study, IMP-7 was also found [28, 29, 39]. Further analysis showed the downregulation of OprD porin gene expression in nine (26.5%) isolates and an upregulation of MexAB efflux pump gene expression in five (14.7%) isolates [39]. Six different serotypes and 14 different pulsotypes were detected; of which all 9 serotype O:15 strains were found to have the same pulsotype (F) and the same mechanism of resistance (OXA-10 and VEB-1a).
A multicenter study investigating the carriage of MBL genes in 39 CR P. aeruginosa isolates found that 28.2% were phenotypic carbapenemase-producers, with VIM being the dominant MBL detected (72.7% [VIM-2, VIM-6 and VIM-28]). Three isolates carried the blaGES-5 gene. No IMP-producing genes were detected among any P. aeruginosa isolates [31].
In a study of digestive tract colonization by P. aeruginosa in ICU patients, 5 of 13 CR P. aeruginosa isolates from rectal swabs were shown to carry MBL carbapenemases (4 with NDM and 1 with VIM) [40]. AmpC overexpression, which has been linked with carbapenem resistance when coupled with porin mutations, was detected in eight isolates of CR P. aeruginosa. The overexpression of blaAmpC in these isolates may have arisen due to the overuse of β-lactams, such as ceftazidime, which can cause derepression of AmpC. The authors reported that this was the first study in the Arabian Gulf region to document AmpC overexpression in CR P. aeruginosa isolates [40].
United Arab Emirates
In a cross-sectional survey on carbapenem-non-susceptible P. aeruginosa, the VIM-type MBL carbapenemases were most common among a subset of 37 that were analyzed (32.4% [VIM-2, VIM-30, VIM-31 and VIM-42]) [36]. A single VIM-2-carrying isolate was also GES-9-positive, while one VIM-42-positive isolate co-carried GES-5. No other investigated MBL genes were detected, nor were KPC carbapenemases. Outer membrane impermeability was observed in 73% of isolates and 75.6% displayed overproduced MexAB-OprM efflux pump. Seven distinct clones were identified, one of which comprised 81.1% of isolates across all hospitals (including 11 out of the 12 isolates that were VIM- and GES-positive), suggesting clonal dissemination [36].
Changes in Antimicrobial Resistance Since 2011 in the Arabian Gulf Region
Kuwait
Between 2012 and 2021, there were net increases of antimicrobial resistance to amikacin (3.2%), ceftazidime (15.1%), cefepime (5.6%), and piperacillin-tazobactam (7.1%) [53] (Table 2). Resistance to levofloxacin remained stable (−0.4% net change), and to meropenem (−7.4% net change). Following 2019, the rates to all agents appeared to decrease annually.
Qatar
Between 2011 and 2018, the rates of non-susceptibility to amikacin and ceftazidime remained stable (net changes, 0.0% and −1.0%, respectively), whereas non-susceptibility to cefepime, meropenem and piperacillin-tazobactam increased (by 4.0%, 4.0%, and 13.0%, respectively) [56] (Table 2). ATLAS 2021 data showed higher rates of non-susceptibility than in 2011 for all tested agents except amikacin [53] (Table 2).
Saudi Arabia
In a 6-year, multicenter national antimicrobial surveillance study, the trend was increased resistance to aztreonam, imipenem and meropenem, with overall percentage increases during the study period of 17.3%, 12.3% and 11.6%, respectively [41]. Overall percentage decreases in resistance during the study period were shown to netilmicin, amikacin and tobramycin (by 10.0%, 5.9% and 5.0%, respectively). Resistance to the other antimicrobials on the test panel (including ciprofloxacin, piperacillin-tazobactam, ceftazidime, levofloxacin, cefepime, colistin and gentamicin), remained stable with <5% overall change. In another 6-year antimicrobial surveillance study, the susceptibility of. P. aeruginosa to ceftriaxone, ceftazidime and meropenem decreased over the study period, but remained stable to cefepime, amikacin, ciprofloxacin, and increased to gentamicin and trimethoprim-sulfamethoxazole [41].
ATLAS antimicrobial resistance data were not collected in 2014 or 2017, but resistance rates to all tested agents were higher in 2011–2013 than 2018–2021. Between 2018 and 2021, there appeared to be a decrease in resistance to all agents tested [53] (Table 2).
United Arab Emirates
In the UAE, P. aeruginosa showed a horizontal trend for resistance to fluoroquinolones, and to third- and fourth-generation cephalosporins, and showed a decreasing trend for resistance to aminoglycosides. Amikacin and piperacillin-tazobactam resistance decreased by 1.8% and 3.8%, respectively, and resistance to ceftazidime, cefepime and meropenem remained stable (net changes, 0.8%, −1.0%, and 0.1%, respectively) (Table 2). Nevertheless, from 2016 to 2020, both carbapenems, imipenem and meropenem, showed a decreasing trend of resistance. The percentage of MDR, XDR, and possible PDR isolates generally declined from 2010 to 2020 [57].
Discussion
The studies above describe important published findings on antimicrobial resistance among isolates of P. aeruginosa in the Arabian Gulf countries since 2010. More information is now known about the genes and mechanisms driving resistance among P. aeruginosa in these countries, and about the antimicrobial agents that could be used against P. aeruginosa infections in a hospital or ICU setting. Recent data (2016–2021) on antimicrobial resistance among clinical isolates of P. aeruginosa show that resistance to meropenem was highest (10.3–45.7%) among the agents presented [53]. In Kuwait, there was an overall increase in resistance rates from 2012 to 2021 to most antimicrobial agents presented, although levofloxacin and meropenem resistance appeared to fluctuate [53]. Data collected over the last 12 years from Saudi Arabia showed an increase in resistance to aztreonam, imipenem and meropenem, and a decrease in susceptibility of. P. aeruginosa to ceftriaxone and ceftazidime [41, 42]. The reported increase in resistance rates is alarming, and continued surveillance is needed to monitor these upward trends. The significantly higher rate of resistance to meropenem than to other tested agents among P. aeruginosa in one study from Saudi Arabia was suggested to be due to over-prescribing of broad-spectrum antimicrobial agents, such as carbapenems [32]. Prior antibiotic treatment was found to be associated with MDR P. aeruginosa infections, according to studies in Saudi Arabia and Qatar [24, 34]. Further studies are warranted to correlate antimicrobial use in P. aeruginosa infections with the current resistance profiles in the Arabian Gulf countries.
In treatment guidance from the IDSA, DTR among P. aeruginosa is defined as non-susceptibility to piperacillin-tazobactam, ceftazidime, cefepime, aztreonam, meropenem, imipenem-cilastatin, ciprofloxacin and levofloxacin [8]. The most common MDR profile among P. aeruginosa in the study by Karlowsky et al. [14] was non-susceptibility to aztreonam, ceftazidime, cefepime, ciprofloxacin, imipenem and piperacillin-tazobactam. These resistance profiles leave few antimicrobial agents with known activity against P. aeruginosa, one of which is colistin. Colistin demonstrated the highest antimicrobial activity among the studies reported in this review, including those with subsets of antimicrobial-resistant phenotypes; however, owing to the increased use of colistin as a last-resort agent for infections caused by MDR and XDR strains, colistin resistance among MDR and XDR P. aeruginosa is emerging worldwide. Thus, resistance mechanisms in these antimicrobial-resistant phenotypes are being investigated [58–60]. Therefore, colistin resistance among P. aeruginosa requires continued surveillance and suitable monitoring systems to report the dissemination rate of these resistance genes.
It has been suggested that the Middle East region could act as a secondary reservoir for NDM carbapenemases, on account of population flow to the Middle East from countries of the Asian subcontinent, such as India or Pakistan [61, 62]. While NDM- and VIM-type β-lactamase genes are predominant in the Asian subcontinent, only four isolates included in this review were found to harbor NDM-type genes (one from Bahrain and three from Saudi Arabia) [16, 40]. The lack of molecular data and proper representation could be a contributing factor to this observation. Further research and enhanced surveillance efforts are needed to fully understand the distribution and prevalence of NDM-type genes. Although the VIM β-lactamase appears to be dominant in the Arabian Gulf, multiple resistance mechanisms were found to cause carbapenem resistance in most P. aeruginosa isolates from Saudi Arabia and the UAE [28, 29, 31, 36, 39]. Multiple clones of MDR P. aeruginosa were also identified in Bahrain, Qatar, Saudi Arabia, and the UAE, including ST235, ST233 and ST357 which are deemed as high-risk clones [27, 38]. Their associated MDR phenotypes are a cause for concern. Clonal dissemination was also discussed by Ayoub Moubareck et al. [36] regarding their study findings of seven distinct clones among carbapenem-non-susceptible P. aeruginosa isolates from the UAE. This is also concerning as clonal dissemination contributes to the spread of P. aeruginosa pathogens that carry β-lactamase genes and are antimicrobial-resistant.
When comparing antimicrobial susceptibility or resistance data from different studies of antimicrobial surveillance or prevalence (whether national, regional or global), it is vital to be aware of the limitations of comparisons made. We express similar limitations to the observations noted by the European Centre for Disease Prevention and Control on inter-country comparisons and national trends of surveillance data on antimicrobial resistance, such as population coverage, sampling, laboratory routines [63]. Some of the most important potential sources of bias are the various protocols for antimicrobial susceptibility testing, the use of guidelines for clinical breakpoints, various isolate sources and numbers of isolates, the sizes of the hospitals (and whether single- or multi-center), and single versus multiple study years. Details on isolate collection and susceptibility testing, where available, for each study are noted in Supplementary Table 2. Data from individual non-national studies may not reflect the trends of the whole country and might generate inaccurate reporting bias for prevalence rates, microbiological characteristics, or mechanisms of genetic resistance. Furthermore, it is important to acknowledge that excluding papers published in Arabic language may limit the scope of the study and the perspectives represented.
Despite these limitations, the sharing of data on the local, national, and international levels of antimicrobial-resistant P. aeruginosa may serve to improve public health, inform health policies, provide evidence for developing treatment guidelines, and monitor the trends and spread of resistance. Local epidemiology data can inform the implementation of infection prevention and control, and antimicrobial stewardship programs in the respective healthcare institutions. Together, these factors need to be addressed as a matter of urgency to establish a more comprehensive and representative antimicrobial resistance surveillance system to monitor the threat of the opportunistic pathogen P. aeruginosa.
Supplementary Information
Below is the link to the electronic supplementary material.
Abbreviations
- AmpC
Ampicillin class C
- bla
β-Lactamase gene
- CDC
Centers for Disease Control and Prevention
- CLSI
Clinical and Laboratory Standards Institute
- CR
Carbapenem-resistant
- DTR
Difficult-to-treat resistance
- ESBL
Extended-spectrum β-lactamase
- EUCAST
European Committee on Antimicrobial Susceptibility Testing
- GES
Guiana extended-spectrum
- IDSA
Infectious Diseases Society of America
- I
Intermediate
- ICMR
Indian Council of Medical Research
- ICU
Intensive care unit
- IMP
Imipenemase
- KPC
Klebsiella pneumoniae carbapenemase
- MBL
Metallo-β-lactamase
- MDR
Multidrug-resistant
- mex
Multidrug efflux pump
- MIC
Minimum inhibitory concentration
- NDM
New Delhi metallo-β-lactamase
- NS
Non-susceptible
- Opr
Outer membrane porin
- OXA
Oxacillinase
- PDR
Pandrug-resistant
- PER
Plasmid-mediated extended spectrum
- R
Resistant
- S
Susceptible
- SPM
São Paulo metallo-β-lactamase
- ST
Sequence type
- TZP
Piperacillin-tazobactam
- UAE
United Arab Emirates
- VAP
Ventilator-associated pneumonia
- VEB
Vietnamese extended-spectrum β-lactamase
- VIM
Verona integron-encoded metallo-β-lactamase
- XDR
Extensively drug-resistant
Author Contributions
All authors were involved in the article design and data interpretation, as well as drafting and reviewing the manuscript. All authors read and approved the final submitted version.
Funding
This work is funded by Pfizer. Medical writing support was provided by Neera Hobson, PhD of Micron Research Ltd. (Ely, UK), and was funded by Pfizer Gulf FZ LLC.
Data Availability
The datasets generated and/or analyzed during the current study are included in this published article [and its supplementary information files], or available from the corresponding author on reasonable request.
Declarations
Conflict of Interest
AA, BA, MA, CAM, WJ, AS, AMS, and HZ declare no competing interests. AH and NM are current Pfizer employees. AK is a former employee of Pfizer.
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
References
- 1.Raoofi S, Pashazadeh Kan F, Rafiei S, Hosseinipalangi Z, Noorani Mejareh Z, Khani S, et al. Global prevalence of nosocomial infection: a systematic review and meta-analysis. PLoS ONE. 2023;18: e0274248. 10.1371/journal.pone.0274248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD 2019 Antimicrobial Resistance Collaborators. Global mortality associated with 33 bacterial pathogens in 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2022;400(10369):2221–48. 10.1016/S0140-6736(22)02185-7. [DOI] [PMC free article] [PubMed]
- 3.Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399(10325):629–55. 10.1016/S0140-6736(21)02724-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Horcajada JP, Montero M, Oliver A, Sorlí L, Luque S, Gómez-Zorrilla S, et al. Epidemiology and treatment of multidrug-resistant and extensively drug-resistant Pseudomonas aeruginosa infections. Clin Microbiol Rev. 2019;32(4):e00031-19. 10.1128/CMR.00031-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18:268–81. 10.1111/j.1469-0691.2011.03570.x. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC). Antibiotic resistance threats in the United States, 2019. Atlanta, GA: US Department of Health and Human Services, CDC; 2019. AT Threats; 2019.
- 7.Tacconelli E, Carrara E, Savoldi A, Harbarth S, Mendelson M, Monnet DL. Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect Dis. 2018;18:318–27. 10.1016/S1473-3099(17)30753-3. [DOI] [PubMed] [Google Scholar]
- 8.Kazmierczak KM, Rabine S, Hackel M, McLaughlin RE, Biedenbach DJ, Bouchillon SK, et al. Multiyear, multinational survey of the incidence and global distribution of metallo-β-lactamase-producing Enterobacteriaceae and Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2015;60:1067–78. 10.1128/AAC.02379-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kiratisin P, Kazmierczak K, Stone GG. In vitro activity of ceftazidime-avibactam and comparators against carbapenemase-producing Enterobacterales and Pseudomonas aeruginosa isolates collected globally between 2016 and 2018. J Glob Antimicrob Resist. 2021;S2213–7165(21):00202–12. 10.1016/j.jgar.2021.08.010. [DOI] [PubMed] [Google Scholar]
- 10.Kadri SS, Adjemian J, Lai YL, Spaulding AB, Ricotta E, Prevots DR, et al. Difficult-to-treat resistance in gram-negative bacteremia at 173 US hospitals: retrospective cohort analysis of prevalence, predictors, and outcome of resistance to all first-line agents. Clin Infect Dis. 2018;67:1803–14. 10.1093/cid/ciy378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tamma PD, Aitken SL, Bonomo RA, Mathers AJ, van Duin D, Clancy CJ. Infectious Diseases Society of America guidance on the treatment of extended-spectrum β-lactamase producing Enterobacterales (ESBL-E), carbapenem-resistant Enterobacterales (CRE), and Pseudomonas aeruginosa with difficult-to-treat resistance (DTR-P. aeruginosa). Clin Infect Dis. 2021;72:e169–83. 10.1093/cid/ciaa1478. [DOI] [PubMed] [Google Scholar]
- 12.Karlowsky JA, Bouchillon SK, El Mahdy KR, Mohamed N, Stone GG, Sahm DF. In vitro activity of ceftazidime/avibactam against clinical isolates of Enterobacterales and Pseudomonas aeruginosa from Middle Eastern and African countries: ATLAS global surveillance programme 2015–2018. JAC Antimicrob Resist. 2021;3:dlab067. 10.1093/jacamr/dlab067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nichols WW, de Jonge BL, Kazmierczak KM, Karlowsky JA, Sahm DF. In vitro susceptibility of global surveillance isolates of Pseudomonas aeruginosa to ceftazidime-avibactam (INFORM 2012–2014). Antimicrob Agents Chemother. 2016;60:4743–9. 10.1128/AAC.00220-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Karlowsky JA, Lob SH, Young K, Motyl MR, Sahm DF. Activity of imipenem/relebactam against Pseudomonas aeruginosa with antimicrobial-resistant phenotypes from seven global regions: SMART 2015–2016. J Glob Antimicrob Resist. 2018;15:140–7. 10.1016/j.jgar.2018.07.012. [DOI] [PubMed] [Google Scholar]
- 15.Moise PA, Gonzalez M, Alekseeva I, Lopez D, Akrich B, DeRyke CA, et al. Collective assessment of antimicrobial susceptibility among the most common Gram-negative respiratory pathogens driving therapy in the ICU. JAC Antimicrob Resist. 2021;3:dlaa129. 10.1093/jacamr/dlaa129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Joji RM, Al-Rashed N, Saeed NK, Bindayna KM. Detection of VIM and NDM-1 metallo-beta-lactamase genes in carbapenem-resistant Pseudomonas aeruginosa clinical strains in Bahrain. J Lab Phys. 2019;11:138–43. 10.4103/JLP.JLP_118_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Al Rashed N, Joji RM, Saeed NK, Bindayna KM. Detection of overexpression of efflux pump expression in fluoroquinolone-resistant Pseudomonas aeruginosa isolates. Int J Appl Basic Med Res. 2020;10:37–42. 10.4103/ijabmr.IJABMR_90_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alfouzan W, Dhar R, Nicolau DP. In vitro activity of newer and conventional antimicrobial agents, including fosfomycin and colistin, against selected Gram-negative bacilli in Kuwait. Pathogens. 2018;7:75. 10.3390/pathogens7030075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alhubail A, Sewify M, Messenger G, Masoetsa R, Hussain I, Nair S, et al. Microbiological profile of diabetic foot ulcers in Kuwait. PLoS ONE. 2020;15: e0244306. 10.1371/journal.pone.0244306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Al Rahmany D, Albeloushi A, Alreesi I, Alzaabi A, Alreesi M, Pontiggia L, et al. Exploring bacterial resistance in Northern Oman, a foundation for implementing evidence-based antimicrobial stewardship program. Int J Infect Dis. 2019;83:77–82. 10.1016/j.ijid.2019.04.004. [DOI] [PubMed] [Google Scholar]
- 21.Balkhair A, Al-Farsi YM, Al-Muharrmi Z, Al-Rashdi R, Al-Jabri M, Neilson F, et al. Epidemiology of multi-drug resistant organisms in a teaching hospital in Oman: a 1-year hospital-based study. ScientificWorldJournal. 2014;2014: 157102. 10.1155/2014/157102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Balkhair A, Al-Muharrmi Z, Al’Adawi B, Al Busaidi I, Taher HB, Al-Siyabi T, et al. Prevalence and 30-day all-cause mortality of carbapenem-and colistin-resistant bacteraemia caused by Acinetobacter baumannii, Pseudomonas aeruginosa, and Klebsiella pneumoniae: description of a decade-long trend. Int J Infect Dis. 2019;85:10–5. 10.1016/j.ijid.2019.05.004. [DOI] [PubMed] [Google Scholar]
- 23.AbdulWahab A, Zahraldin K, Sid Ahmed MA, Jarir SA, Muneer M, Mohamed SF, et al. The emergence of multidrug-resistant Pseudomonas aeruginosa in cystic fibrosis patients on inhaled antibiotics. Lung India. 2017;34:527–31. 10.4103/lungindia.lungindia_39_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sid Ahmed MA, Hassan AAI, Abu Jarir S, Abdel Hadi H, Bansal D, Abdul Wahab A, et al. Emergence of multidrug- and pandrug-resistant Pseudomonas aeruginosa from five hospitals in Qatar. Infect Prev Pract. 2019;1: 100027. 10.1016/j.infpip.2019.100027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sid Ahmed MA, Abdel Hadi H, Abu Jarir S, Al Khal AL, Al-Maslamani MA, Jass J, et al. Impact of an antimicrobial stewardship programme on antimicrobial utilization and the prevalence of MDR Pseudomonas aeruginosa in an acute care hospital in Qatar. JAC Antimicrob Resist. 2020;2:dlaa050. 10.1093/jacamr/dlaa050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sid Ahmed MA, Abdel Hadi H, Hassan AAI, Abu Jarir S, Al-Maslamani MA, Eltai NO, et al. Evaluation of in vitro activity of ceftazidime/avibactam and ceftolozane/tazobactam against MDR Pseudomonas aeruginosa isolates from Qatar. J Antimicrob Chemother. 2019;74:3497–504. 10.1093/jac/dkz379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sid Ahmed MA, Khan FA, Sultan AA, Söderquist B, Ibrahim EB, Jass J, et al. Beta-lactamase-mediated resistance in MDR-Pseudomonas aeruginosa from Qatar. Antimicrob Resist Infect Control. 2020;9:170. 10.1186/s13756-020-00838-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tawfik AF, Shibl AM, Aljohi MA, Altammami MA, Al-Agamy MH. Distribution of Ambler class A, B and D β-lactamases among Pseudomonas aeruginosa isolates. Burns. 2012;38:855–60. 10.1016/j.burns.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 29.Al-Agamy MH, Shibl AM, Tawfik AF, Elkhizzi NA, Livermore DM. Extended-spectrum and metallo-beta-lactamases among ceftazidime-resistant Pseudomonas aeruginosa in Riyadh. Saudi Arabia J Chemother. 2012;24:97–100. 10.1179/1120009X12Z.00000000015. [DOI] [PubMed] [Google Scholar]
- 30.Somily AM, Absar MM, Arshad MZ, Al Aska AI, Shakoor ZA, Fatani AJ, et al. Antimicrobial susceptibility patterns of multidrug-resistant Pseudomonas aeruginosa and Acinetobacter baumannii against carbapenems, colistin, and tigecycline. Saudi Med J. 2012;33:750–5. [PubMed] [Google Scholar]
- 31.Memish ZA, Assiri A, Almasri M, Roshdy H, Hathout H, Kaase M, et al. Molecular characterization of carbapenemase production among gram-negative bacteria in Saudi Arabia. Microb Drug Resist. 2015;21:307–14. 10.1089/mdr.2014.0121. [DOI] [PubMed] [Google Scholar]
- 32.Khan MA, Faiz A. Antimicrobial resistance patterns of Pseudomonas aeruginosa in tertiary care hospitals of Makkah and Jeddah. Ann Saudi Med. 2016;36:23–8. 10.5144/0256-4947.2016.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ibrahim ME. High antimicrobial resistant rates among Gram-negative pathogens in intensive care units. A retrospective study at a tertiary care hospital in Southwest Saudi Arabia. Saudi Med J. 2018;39:1035–43. 10.15537/smj.2018.10.22944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alhussain FA, Yenugadhati N, Al Eidan FA, Al Johani S, Badri M. Risk factors, antimicrobial susceptibility pattern and patient outcomes of Pseudomonas aeruginosa infection: a matched case-control study. J Infect Public Health. 2021;14:152–7. 10.1016/j.jiph.2020.11.010. [DOI] [PubMed] [Google Scholar]
- 35.Bukhari SZ, Hussain WM, Banjar AA, Fatani MI, Karima TM, Ashshi AM. Application of ventilator care bundle and its impact on ventilator associated pneumonia incidence rate in the adult intensive care unit. Saudi Med J. 2012;33:278–83. [PubMed] [Google Scholar]
- 36.Ayoub Moubareck C, Hammoudi Halat D, Akkawi C, Nabi A, AlSharhan MA, AlDeesi ZO, et al. Role of outer membrane permeability, efflux mechanism, and carbapenemases in carbapenem-nonsusceptible Pseudomonas aeruginosa from Dubai hospitals. Int J Infect Dis. 2019;84:143–50. 10.1016/j.ijid.2019.04.027. [DOI] [PubMed] [Google Scholar]
- 37.Alatoom A, Elsayed H, Lawlor K, AbdelWareth L, El-Lababidi R, Cardona L, et al. Comparison of antimicrobial activity between ceftolozane-tazobactam and ceftazidime-avibactam against multidrug-resistant isolates of Escherichia coli, Klebsiella pneumoniae, and Pseudomonas aeruginosa. Int J Infect Dis. 2017;62:39–43. 10.1016/j.ijid.2017.06.007. [DOI] [PubMed] [Google Scholar]
- 38.Sid Ahmed MA, Hadi HA, Jarir SA, Khan FA, Arbab MA, Hamid JM, et al. Prevalence and microbiological and genetic characteristics of multidrug-resistant Pseudomonas aeruginosa over 3 years in Qatar. Antimicrob Stewardship Healthc Epidemiol. 2022;2:E96. 10.1017/ash.2022.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Al-Agamy MH, Jeannot K, El-Mahdy TS, Samaha HA, Shibl AM, Plésiat P, et al. Diversity of molecular mechanisms conferring carbapenem resistance to Pseudomonas aeruginosa isolates from Saudi Arabia. Can J Infect Dis Med Microbiol. 2016;2016:4379686. 10.1155/2016/4379686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Abdalhamid B, Elhadi N, Alabdulqader N, Alsamman K, Aljindan R. Rates of gastrointestinal tract colonization of carbapenem-resistant Enterobacteriaceae and Pseudomonas aeruginosa in hospitals in Saudi Arabia. New Microbes New Infect. 2016;10:77–83. 10.1016/j.nmni.2016.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Somily A, Balkhy HH, Mas E, Althawadi SI, Alawi M, Al Johani SM, et al. Antimicrobial resistance trends of non-fermenter Gram negative bacteria in Saudi Arabia: a 6-year national study. J Infect Public Health. 2021;14:1144–50. 10.1016/j.jiph.2021.07.007. [DOI] [PubMed] [Google Scholar]
- 42.Al-Tawfiq JA, Rabaan AA, Saunar JV, Bazzi AM. Antimicrobial resistance of gram-negative bacteria: a 6-year longitudinal study in a hospital in Saudi Arabia. J Infect Public Health. 2020;13:737–45. 10.1016/j.jiph.2020.01.004. [DOI] [PubMed] [Google Scholar]
- 43.Garg A, Garg J, Kumar S, Bhattacharya A, Agarwal S, Upadhyay GC. Molecular epidemiology & therapeutic options of carbapenem-resistant Gram-negative bacteria. Indian J Med Res. 2019;149:285–9. 10.4103/ijmr.IJMR_36_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Indian Council of Medical Research (ICMR). AMR surveillance network Indian Council of Medical Research 2018. Annual report: Antimicrobial Resistance Surveillance Network January 2018-December 2018. https://main.icmr.nic.in/sites/default/files/reports/AMRSN_Annual_Report_2018_0.pdf. Accessed 01 October 2021.
- 45.Pragasam AK, Veeraraghavan B, Anandan S, Narasiman V, Sistla S, Kapil A, et al. Dominance of international high-risk clones in carbapenemase-producing Pseudomonas aeruginosa: Multicentric molecular epidemiology report from India. Indian J Med Microbiol. 2018;36:344–51. 10.4103/ijmm.IJMM_18_294. [DOI] [PubMed] [Google Scholar]
- 46.Lee YL, Ko WC, Hsueh PR. Geographic patterns of carbapenem-resistant Pseudomonas aeruginosa in the Asia-Pacific region: results from the Antimicrobial Testing Leadership and Surveillance (ATLAS) program, 2015–2019. Antimicrob Agents Chemother. 2022;66(2): e0200021. 10.1128/AAC.02000-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ahmed N, Ali Z, Riaz M, Zeshan B, Wattoo JI, Aslam MN. Evaluation of antibiotic resistance and virulence genes among clinical isolates of Pseudomonas aeruginosa from cancer patients. Asian Pac J Cancer Prev. 2020;21:1333–8. 10.31557/APJCP.2020.21.5.1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Saleem S, Bokhari H. Resistance profile of genetically distinct clinical Pseudomonas aeruginosa isolates from public hospitals in central Pakistan. J Infect Public Health. 2020;13:598–605. 10.1016/j.jiph.2019.08.019. [DOI] [PubMed] [Google Scholar]
- 49.Awan AB, Yan A, Sarwar Y, Schierack P, Ali A. Detection of synergistic antimicrobial resistance mechanisms in clinical isolates of Pseudomonas aeruginosa from post-operative wound infections. Appl Microbiol Biotechnol. 2021. 10.1007/s00253-021-11680-6. [DOI] [PubMed] [Google Scholar]
- 50.Kazmierczak KM, Biedenbach DJ, Hackel M, Rabine S, de Jonge BL, Bouchillon SK, et al. Global dissemination of blaKPC into bacterial species beyond Klebsiella pneumoniae and in vitro susceptibility to ceftazidime-avibactam and aztreonam-avibactam. Antimicrob Agents Chemother. 2016;60:4490–500. 10.1128/AAC.00107-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kazmierczak KM, de Jonge BLM, Stone GG, Sahm DF. Longitudinal analysis of ESBL and carbapenemase carriage among Enterobacterales and Pseudomonas aeruginosa isolates collected in Europe as part of the International Network for Optimal Resistance Monitoring (INFORM) global surveillance programme, 2013–17. J Antimicrob Chemother. 2020;75:1165–73. 10.1093/jac/dkz571. [DOI] [PubMed] [Google Scholar]
- 52.McCracken MG, Adam HJ, Blondeau JM, Walkty AJ, Karlowsky JA, Hoban DJ, et al. Characterization of carbapenem-resistant and XDR Pseudomonas aeruginosa in Canada: results of the CANWARD 2007–16 study. J Antimicrob Chemother. 2019;74(Suppl 4):iv32-iv38. 10.1093/jac/dkz285. [DOI] [PubMed]
- 53.ATLAS (Antimicrobial Testing Leadership and Surveillance) database. Pfizer. Available from https://atlas-surveillance.com/. Accessed 13 Jan 2023.
- 54.European Committee on Antimicrobial Susceptibility Testing (EUCAST). Breakpoint tables for interpretation of MICs and zone diameters–Version 10.0. January 2020. http://www.eucast.org/clinical_breakpoints/.
- 55.Clinical and Laboratory Standards Institute (CLSI). Performance standards for antimicrobial susceptibility testing: 30th informational supplement, M100. 30th ed. Wayne, PA: CLSI; 2020. [Google Scholar]
- 56.Hamad Medical Corporation. Annual cumulative report of the antimicrobial susceptibility rates of common microbial pathogens to antimicrobials available in Hamad General Hospital Formulary. (2020).
- 57.United Arab Emirates Ministry of Health and Prevention (UAE MOHAP). National Sub-Committee for AMR Surveillance. United Arab Emirates Surveillance of Antimicrobial Resistance Annual Report 2022. Document ref. number: AMR/NSR 2022. https://mohap.gov.ae/assets/download/ade73514/National%20AMR%20Surveillance%20Report%202022%20MOHAP.pdf.aspx. Accessed 4 Oct 2022.
- 58.Del Barrio-Tofiño E, López-Causapé C, Cabot G, Rivera A, Benito N, Segura C, et al. Genomics and susceptibility profiles of extensively drug-resistant Pseudomonas aeruginosa isolates from Spain. Antimicrob Agents Chemother. 2017;61:e01589-17. 10.1128/AAC.01589-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Abd El-Baky RM, Masoud SM, Mohamed DS, Waly NG, Shafik EA, Mohareb DA, et al. Prevalence and some possible mechanisms of colistin resistance among multidrug-resistant and extensively drug-resistant Pseudomonas aeruginosa. Infect Drug Resist. 2020;13:323–32. 10.2147/IDR.S238811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Torrens G, van der Schalk TE, Cortes-Lara S, Timbermont L, Del Barrio-Tofiño E, Xavier BB, et al. Susceptibility profiles and resistance genomics of Pseudomonas aeruginosa isolates from European ICUs participating in the ASPIRE-ICU trial. J Antimicrob Chemother. 2022;77:1862–72. 10.1093/jac/dkac122. [DOI] [PubMed] [Google Scholar]
- 61.Nordmann P, Poirel L, Toleman MA, Walsh TR. Does broad-spectrum β-lactam resistance due to NDM-1 herald the end of the antibiotic era for treatment of infections caused by Gram-negative bacteria? J Antimicrob Chemother. 2011;66:689–92. 10.1093/jac/dkq520. [DOI] [PubMed] [Google Scholar]
- 62.Patel G, Bonomo RA. “Stormy waters ahead”: global emergence of carbapenemases. Front Microbiol. 2013;4:48. 10.3389/fmicb.2013.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.European Centre for Disease Prevention and Control. https://www.ecdc.europa.eu/en/about-us/networks/disease-networks-and-laboratory-networks/ears-net-data. Accessed 31 May 2023.
- 64.Clinical and Laboratory Standards Institute (CLSI). Performance standards for antimicrobial susceptibility testing: 31st informational supplement, M100. 32nd ed. Wayne, PA: CLSI; 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and/or analyzed during the current study are included in this published article [and its supplementary information files], or available from the corresponding author on reasonable request.