Abstract
Introduction and importance
Spigelian hernias are rare, constituting about 1–2 % of all abdominal wall hernias. They present clinically significant challenges due to their potential for incarceration and strangulation. This case report highlights a unique presentation of a Spigelian hernia involving sigmoid colon strangulation, emphasizing the critical need for awareness and timely intervention.
Case presentation
A 60-year-old female with hypertension and diabetes presented with severe left abdominal pain, nausea, and vomiting. Examination revealed leukocytosis, neutrophilia, and signs of acute abdomen. CT imaging showed a complicated left lateral abdominal wall hernia containing the sigmoid colon. Surgical intervention included sigmoidectomy with colorectal anastomosis and hernia repair. Postoperative recovery was successful with subsequent elective ileostomy reversal.
Clinical discussion
The rarity of Spigelian hernias and their atypical presentations can complicate diagnosis and management. This case was particularly challenging due to the strangulation of the sigmoid colon within the hernial sac. Surgical management was necessary to address the incarcerated bowel segment and prevent further complications. This case underscores the utility of CT scans in diagnosing complex cases and guiding surgical strategy.
Conclusion
Despite their rarity, Spigelian hernias carry significant risks of strangulation. Prompt diagnosis and treatment are essential to avoid severe complications. This case highlights the importance of including Spigelian hernia in the differential diagnosis for acute abdominal symptoms, especially when they are nonspecific.
Keywords: Spigelian hernia, Sigmoid colon strangulation, Computed tomography (CT), Surgical management, Case report
Highlights
-
•
Describes a unique instance of Spigelian hernia involving sigmoid colon strangulation in a 60-year-old female, leading to severe symptoms.
-
•
Emphasizes the importance of CT in diagnosis and details the complex surgical intervention required for treatment.
-
•
Notes the successful recovery following surgery, highlighting the effective management of this complicated case.
1. Introduction
A Spigelian hernia, although uncommon, represents a clinically important category of abdominal hernia, constituting about 1–2 % of all hernias within the abdominal wall framework [[1], [2], [3]]. Adrian Van der Spighel was credited with the initial documentation of the semilunar line in 1645, giving his name to these hernias [2]. They are distinguished by the protrusion of abdominal contents, such as organs, a peritoneal sac, or preperitoneal fat, through the Spiegel's fascia. This fascia is located between the medial edge of the rectus abdominis muscle and the semilunar line on the lateral side, marking the precise location for this hernia type [1,2,4]. Spigelian hernias are more frequently diagnosed in individuals between 40 and 70 years old, showing a slight inclination towards females [2,5], and The majority of Spigelian hernias are found within a specific area known as the Spigelian belt, which spans 6 cm across the lower quadrant of the abdomen. The clinical presentation might include nonspecific abdominal discomfort, and without appropriate intervention, it could progress to severe outcomes, such as the strangulation of the herniated segments [5,6].
Risk factors for developing a Spigelian hernia encompass both congenital and acquired elements, including heightened intra-abdominal pressure, persistent coughing, obesity, and having had multiple pregnancies [7,8]. The risk of incarceration and strangulation of the hernia necessitates a vigilant approach for an early and accurate diagnosis [9,10]. For cases where the diagnosis is not straightforward, an abdominal computed tomography (CT) scan with contrast is considered the most reliable method for identifying Spigelian hernias [9]. This investigation is conducted in accordance with the SCARE criteria [11]. The purpose of this case report is to shed light on an atypical occurrence of a Spigelian hernia, where the trapped content was the sigmoid colon, noted as a palpable and sensitive mass. This instance presents distinctive surgical treatment considerations for Spigelian hernias.
2. Case presentation
A 60-year-old female, non-smoker patient with a known history of hypertension and diabetes mellitus, and without any previous surgical interventions, was admitted to the emergency department due to severe abdominal pain. The pain, predominantly located in the left abdomen and accompanied by an abdominal bulge, had been worsening progressively over the past three days. It was described as gradual in onset, progressive, and severe, with a severity score of 8 out of 10. Notably, the pain did not radiate and was neither aggravated nor alleviated by any factors. It was also associated with nausea-induced vomiting of a large volume of food contents, occurring four times. The patient reported experiencing multiple episodes of fever spikes, yet no significant changes in bowel habits, abdominal distension, stool color, or weight loss were observed. The review of other systems revealed no notable abnormalities.
Upon physical examination, vital signs were as follows: temperature 37.7 °C, pulse rate 120 beats per minute, blood pressure 81/50 mmHg, and respiratory rate 22 breaths per minute. Local examination of the abdomen unveiled a tender, irreducible left lower abdominal bulge with negative cough impulse and redness of the overlying skin, indicative of inflammation. Guarding was present in the left abdomen, while the remainder of the physical examination was unremarkable. Laboratory findings highlighted a leukocytosis with a white blood cell count of 14.6 × 10^9/L, neutrophilia at 88 %, elevated C-reactive protein at 278 mg/L, and a creatinine level suggestive of renal impairment at 2.25 mg/dL.
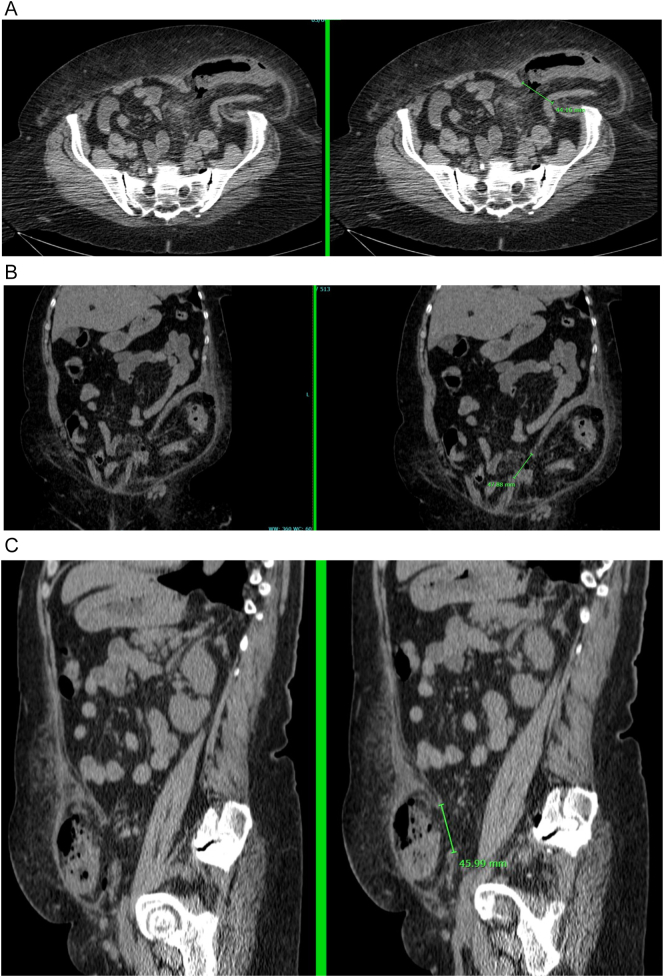
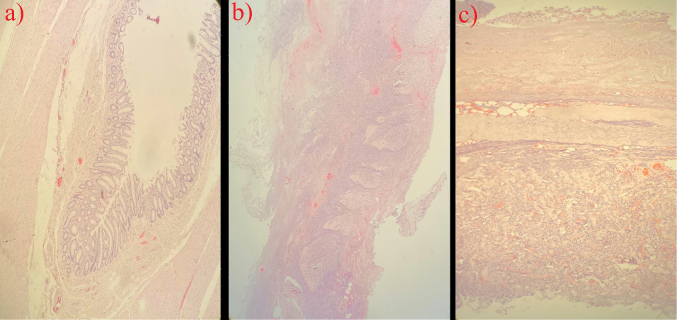
An emergent computed tomography scan elucidated a left lateral abdominal wall hernia containing the sigmoid colon, surrounded by fat stranding and air foci, suggesting a complicated Spigelian hernia with microperforation (Fig. 1a-c). Initial management entailed resuscitation with intravenous fluids and commencement of a broad-spectrum antibiotic regimen consisting of ceftriaxone and metronidazole, followed by urgent surgical intervention. The laparotomy revealed an incarcerated sigmoid colon with ischemic changes within a left Spigelian hernia. Consequently, a sigmoidectomy with side-to-side colorectal anastomosis and a diverting right ileostomy was performed, alongside primary repair of the hernial defect. The decision for primary anastomosis was made after a thorough intraoperative assessment of the proximal and distal colon ends. Additionally, the anastomosis was secured using a gastrointestinal stapler (80 mm), followed by primary suturing of the stapler defects and closure of the mesenteric defect of the sigmoid mesocolon. The decision was solidified by the presence of well-perfused ends of the colon. Furthermore, a diverting ileostomy 15 cm from the ileocecal valve was performed. There was necrotic tissue within the hernial defect, which measured approximately 4 cm by 3 cm. Due to these findings, mesh repair of the hernial defect was deemed challenging due to the potential for high tension and increased risk of infection. Therefore, primary repair of the hernial defect was undertaken. Histopathological examination of the excised sigmoid segment, measuring 28 cm, disclosed a 7 cm region of significantly attenuated wall exhibiting greenish discoloration, necrotic mucosa, and exudative serosa. Dissection revealed multiple diverticula, some laden with fecal matter. Additional findings encompassed adipose tissue fragments and membrane-like structures, without evident luminal masses. The pathological diagnosis underscored localized transmural necrosis accompanied by severe localized peritonitis, diverticulitis, and evidence of bowel segment strangulation. Numerous fecal-filled diverticula were observed, and peritoneal tissue displayed extensive necrosis and acute inflammation. A few reactive lymph nodes were identified, and both resection margins of the segment were intact. Notably, the analysis confirmed the absence of dysplasia or malignancy within the examined sections (Fig. 2).
Fig. 1.
CT Scan of Left Spigelian Hernia with Sigmoid Colon and Perforation Indicators.
(a-c): A left-sided lateral abdominal wall hernia with a 3.6 cm wide neck, containing segments of the sigmoid colon. Multiple diverticula are present within the contained bowel segment. Surrounding fat stranding and intra-hernia air foci indicate gas within the hernia. Adjacent subcutaneous fat stranding and intra-abdominal free air foci near the distal sigmoid segment to the hernia site indicate a complicated hernia with bowel perforation.
Fig. 2.
Microscopic Views of Sigmoid Colon with Diverticulum and Transmural Necrosis.
a:Diverticulum within the wall. H&E 40×.
b:Full thickness, transmural necrosis with thinning of the bowel wall. H&E 40×.
c:Transmural necrosis of bowel wall H&E 100×.
The postoperative course was marked by a successful recovery, underpinned by intravenous administration of broad-spectrum antibiotics, including meropenem, vancomycin, and fluconazole. The patient was initially managed in an intermediate medical unit overnight, before being transferred to a general ward. A clear fluid diet was initiated the subsequent morning with the ileostomy commencing function the next day. Discharge followed on the third postoperative day, with prescriptions for multimodal oral analgesia and oral antibiotics. Follow-up in the outpatient clinic was largely unremarkable, barring a wound infection one month post-surgery, which was managed effectively with bedside dressing changes and oral antibiotics.
Three months postoperatively, the patient was readmitted electively for ileostomy reversal. In light of her intermediate risk associated with general anesthesia, a preoperative cardiac evaluation was conducted. The procedure involved segmental resection of the ileum with side-to-side anastomosis. Postoperative recovery was uncomplicated, with the patient tolerating a diet well and being discharged on the fifth postoperative day. Subsequent follow-up visits have been unremarkable.
3. Discussion
Spigelian hernia, a relatively rare form of ventral abdominal wall hernia, represents a small fraction of abdominal hernias, with an incidence of 1 to 2 per 1000 abdominal hernias [2]. These hernias predominantly occur in individuals between their fifth and seventh decades of life, exemplified by our 60-year-old female patient, and exhibit a higher prevalence in females [6]. The symptomatology, as manifested in our case, frequently involves abdominal pain and symptoms indicative of intestinal obstruction [12], with the severity of abdominal pain varying widely, affecting 31 % to 86 % of patients [13].
In our patient, the hernia was situated in the lower left quadrant, adjacent to the rectus muscle, aligning with the most commonly reported location for Spigelian hernias [14,15]. Notably, the hernia sac contained the sigmoid colon, diverging from the more typical contents such as omentum, small bowel, or colon [16,17]. The patient reported severe, persistent abdominal pain, a symptom often precipitating medical consultation for Spigelian hernia [3,18].
Diagnostic approaches favor ultrasound as an initial imaging modality due to its accessibility and effectiveness, albeit its performance may be hindered by operator dependency and diminished accuracy in obese patients [19]. Computed tomography (CT) scans, utilized in this instance, offer a definitive diagnostic tool, especially in complex cases where hernias are not readily apparent [19]. CT imaging boasts a sensitivity and positive predictive value of 100 %, underscoring its reliability in diagnosing Spigelian hernias [19].
Surgical repair stands as the conclusive treatment for Spigelian hernias, aiming to avert complications such as strangulation, a significant concern for our patient [20]. Although laparoscopic approaches have been increasingly adopted due to their less invasive nature and associated benefits like quicker recovery and reduced morbidity [9,17], an open surgical technique was deemed most appropriate for our case. This decision was informed by the case's intricacies, the presence of strangulation, and the necessity for meticulous exploration and repair. A mesh was used to achieve a tension-free repair, widely regarded as an effective strategy for repairing large hernial defects [21,22].
Postoperative care is critical, as complications such as wound infection can arise, as observed in our patient. Nevertheless, with appropriate management, including broad-spectrum antibiotics and wound care, such complications can be effectively managed, promoting a positive outcome for the patient [23,24].
The comparison of our case with those documented in the literature reveals a diverse range of presentations and therapeutic strategies for Spigelian hernias (Table 1). Panaccio et al. and Anilir et al. have delineated instances managed through polypropylene mesh repair, reporting no post-operative complications, illustrating a straightforward approach. In contrast, our case necessitated a more intricate surgical intervention owing to the hernia's contents and ischemic alterations observed [25,26]. This complexity mirrors the variability in symptomatology and diagnostic outcomes, as evidenced by the accounts of Oen E.Y. and Som et al., where presentations ranged from acute abdominal discomfort to asymptomatic conditions [27,28]. Additionally, the application of laparoscopic techniques by Habib et al. contrasts with our preference for an open surgical method, highlighting the bespoke nature of hernia management strategies [29]. The diversity in diagnostic modalities—from computed tomography scans to barium enemas—and the variety of hernia contents observed, including sigmoid loops to epiploic appendages [[25], [26], [27], [28], [29], [30], [31], [32]], further underscores the clinical heterogeneity characterizing spigelian hernias.
Table 1.
Clinical Characteristics and Management of Spigelian Hernia Cases.
| Study ID | Age | Gender | Symptoms | Diagnostic tools | Diagnostic findings | Management | post-operative complications |
|---|---|---|---|---|---|---|---|
| Panaccio et al. [25] | 88 | Male | RLQ pain, abdominal distension | CT | Intestinal obstruction, Spigelian hernia of about 3 cm | Surgical exploration, Hernia content reduction, Defect repair with polypropylene mesh. | None |
| Anilir et al. [26] | 36 | Female | Abdominal pain, nausea, tender mass in left quadrant | US, CT. | Incarcerated Spigelian hernia with a defect contining sigmoid loop | Surgery with polypropylene mesh repair. | None |
| Oen E.Y. [27] | 41 | Male | Acute abdominal pain, lump in lower abdomen | X-ray, Barium Enema | Spigelian hernia contining Redundant sigmoid colon | laparotomy, hernia excision. | None |
| Som et al. [28] | 67 | Male | Asymptomatic left lower quadrant mass, congestive heart failure | Barium enema | Spigelian hernia contining sigmoid loop | Surgery | None |
| Som et al. [28] | 55 | Not reported | Left lower quadrant pain | Barium enema | Spigelian hernia contining sigmoid loop | Surgery | None |
| Habib et al. [29] | Not Specified | Not Specified | Pain and mass in the left lower quadrant, symptoms mimicking sigmoid diverticulitis | CT Scan | Left-sided Spigelian Hernia containing a small bowel loop and a sigmoid loop | Laparoscopic treatment with Gore-Tex mesh stapled on the posterior side of the anterolateral abdominal wall | None |
| Capaccio et al. [30] | 84 | Male | Abrupt onset of focal abdominal pain in the left lower quadrant | plain abdominal radiograph, sonography, non-contrast-enhanced CT | small Spigelian hernia containing epiploic appendage of the sigmoid colon in a | Surgery | None |
| Miller et al. [31] | 57 | Male | LLQ pain, abdominal distention, constipation | abdominal X-rays, liquid contrast enema study, abdominal CT scan | incarcerated sigmoid colon in a Spigelian hernia sac | Non-resective sigmoid colon release and hernia repair with polypropylene mesh. | None |
| Polikarpova et al. [32] | 82 | Female | Erythema and tenderness of left flank, haematuria | CT of abdomen and pelvis | Large left Spigelian hernia with perforated sigmoid colon due to diverticulitis, hernia neck 35 mm, oedema, subcutaneous emphysema | Palliative care due to patient's comorbidities and poor premorbid function | None |
RLQ: Right Lower Quadrant, CT: Computed Tomography, US: Ultrasound, LLQ: Left Lower Quadrant.
This case illustrates the diagnostic and therapeutic complexities of Spigelian hernias, underscoring the importance of heightened awareness, accurate imaging techniques, and tailored surgical approaches to improve patient outcomes. However, it is crucial to recognize several limitations. The insights derived from this single case study may not be widely applicable, as the diagnosis and management of Spigelian hernias, especially those containing unusual contents like the sigmoid colon, can vary significantly depending on available resources and expertise. This might restrict the broader application of our findings in diverse clinical settings. Additionally, while CT scans provide a high level of diagnostic precision, the reliance on such sophisticated imaging modalities may not be practical in all healthcare contexts, particularly in settings with limited resources. Furthermore, the choice of an open surgical procedure over the increasingly favored laparoscopic techniques reflects a specific decision-making process that may not coincide with standard practices in less complex cases. This confluence of diagnostic insights and operational constraints highlights the intricate nature of Spigelian hernia management and underscores the necessity for a nuanced understanding of each patient's unique clinical presentation.
4. Conclusion
Spigelian hernias, though infrequent within the broad category of abdominal hernias, constitute a significant clinical concern. These hernias often remain unnoticed in their initial stages, yet they typically present through the manifestations of their complications, such as strangulation, underscoring the critical need for enhanced vigilance among healthcare providers, especially general surgeons, in the assessment of anterior abdominal swellings. The pivotal role of diagnostic imaging, particularly CT scans, in the precise diagnosis and management of Spigelian hernias cannot be overstated. Strangulation, being the most severe and common complication, demands immediate surgical resolution. The intricate characteristics of Spigelian hernias, ranging from their discreet presentation to their potential for grave complications, underscore the importance of prompt and effective intervention to ameliorate patient outcomes.
Consent
Written informed consent for publication of this case report and accompanying images was obtained from the patient. A copy of the consent document is available for the Editor-in-Chief of this journal upon request.
Ethical approval
Patient consent was received for this anonymized case report presentation. No separate approval from the ethics committee was required.
Funding
This case report did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
-
•
Saleh A. Ba-shammakh, Bourhan Alrayes, Sami A. Almasarweh: Study concept, data collection, writing the paper, and revising the manuscript as per reviewer's instructions.
-
•
Muna A. Alseragi, Daher K. Rabadi: Study concept, writing the paper, reviewing, and validating the manuscript's credibility.
Guarantor
Saleh A. Ba-shammakh.
Research registration number
Not applicable.
Declaration of competing interest
None of the authors have any conflicts of interest to declare.
References
- 1.Zachariah S.K., Jose P. Laparoscopic diagnosis of incarcerated “spigelian hernia”: report of a case and review of the literature. Case Rep Surg. 2011;2011 doi: 10.1155/2011/491802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pinna L., Maria P.C., Panagiotis P., Giorgio C.G., Alessandro F., Alberto P. Spigelian hernia: a series of cases and literature review. Ann. Ital. Chir. 2016;87:306–311. [PubMed] [Google Scholar]
- 3.Zacharakis E., Papadopoulos V., Ganidou M., Zacharakis E. Incarcerated Spigelian hernia: a case report. Med. Sci. Monit. 2006;12:CS64–6. [PubMed] [Google Scholar]
- 4.George R., Vasanthi M.S., Prasad K., Prasad A. Spigelian hernia: rare so, beware! Int. Surg. J. 2014;1:50–52. [Google Scholar]
- 5.Chaouch M.A., Nacef K., Chaouch A., Khalifa M.B., Boudokhane M. A Spigelian hernia: single-center experience in an uncommon hernia. Int. J. Abdom. Wall Hernia Surg. 2019;2:59–62. [Google Scholar]
- 6.Skandalakis P.N., Zoras O., Skandalakis J.E., Mirilas P. Spigelian hernia: surgical anatomy, embryology, and technique of repair. Am. Surg. 2006;72:42–48. [PubMed] [Google Scholar]
- 7.Weiss J., Lernan O.Z., Nilson S. Spigelian hernia. Ann. Surg. 1974;180:836–839. doi: 10.1097/00000658-197412000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baucom C., Nguyen Q.D., Hidalgo M., Slakey D. Minimally invasive Spigelian hernia repair. JSLS. 2009;13:263–268. [PMC free article] [PubMed] [Google Scholar]
- 9.Foster D., Nagarajan S., Panait L. Richter-type Spigelian hernia: a case report and review of the literature. Int. J. Surg. Case Rep. 2014;11(6):160–162. doi: 10.1016/j.ijscr.2014.10.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bevilacqua M., Ahmed S., Miller M., Sallee D., Angel W. Case of Spigelian hernia with incarcerated appendix. J. Radiol. Case Rep. 2016;10:23–28. doi: 10.3941/jrcr.v10i11.2815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. Lond. Engl. 2023;109(5):1136. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Subramanya M.S., Chakraborty J., Memon B., Memon M.A. Emergency intraperitoneal onlay mesh repair of incarcerated Spigelian hernia. JSLS. 2010;14:275–278. doi: 10.4293/108680810X12785289144683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bastidas J.G., Khan A.R., LeBlanc K.A. Spigelian hernia as a cause of small bowel obstruction. South. Med. J. 2010;103:567–569. doi: 10.1097/SMJ.0b013e3181de2dc8. [DOI] [PubMed] [Google Scholar]
- 14.Christianakis E., Paschalidis N., Filippou G., Rizos S., Smailis D., Filippou D. Low Spigelian hernia in a 6-year-old boy presenting as an incarcerated inguinal hernia: a case report. J Med Case Reports. 2009;3:34. doi: 10.1186/1752-1947-3-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thomasset S.C., Villatoro E., Wood S., Martin A., Finlay K., Patterson J.E. An unusual Spigelian hernia involving the appendix: a case report. Cases J. 2010;3:22. doi: 10.1186/1757-1626-3-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Malik K.A., Chopra P. Spigelian hernia: a rarity. J. Pak. Med. Assoc. 2006;56:417–419. [PubMed] [Google Scholar]
- 17.Ribeiro E.A., Cruz R.J., Jr., Moreira S.M. Intestinal obstruction induced by a giant incarcerated Spigelian hernia: case report and review of the literature. Sao Paulo Med. J. 2005;123:148–150. doi: 10.1590/S1516-31802005000300012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Savikko J., Kokkola A. Incarcerated Spigelian hernia. [Article in Finnish] Duodecim. 2012;128:518–522. [PubMed] [Google Scholar]
- 19.Xu L., Dulku G., Ho R. A rare presentation of Spigelian hernia involving the appendix. Eur. J. Radiol. Open. 2017 Nov;9(4):141–143. doi: 10.1016/j.ejro.2017.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cúrdia Gonçalves T., Monteiro S., Marinho C., Monteiro S., Marinho C., Cotter J. Strangulated Spiegel’s hernia mimicking ischaemic colitis: endoscopic diagnosis of a rare surgical emergency. Case Reports. 2018 doi: 10.1136/bcr-2017-223260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Flores B.M., Moreno-Egea A., Girela E., Martin J.G., Aguayo J.L., Canteras M. Spigelian hernia: bibliographical study and presentation of a series of 28 patients. Hernia. 2002;6:167–170. doi: 10.1007/s10029-002-0077-x. [DOI] [PubMed] [Google Scholar]
- 22.Celdrán A., Senaris J., Manas J., Frieyro O. The open mesh repair of Spigelian hernia. Am. J. Surg. 2007 Jan;193(1):111–113. doi: 10.1016/j.amjsurg.2006.04.016. [DOI] [PubMed] [Google Scholar]
- 23.Nieuwenhuizen J., van Ramshorst G.H., ten Brinke J.G., de Wit T., van der Harst E., Hop W.C., et al. The use of mesh in acute hernia: frequency and outcome in 99 cases. Hernia. 2011;15:297–300. doi: 10.1007/s10029-010-0779-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilson R.B., Farooque Y. Risks and prevention of surgical site infection after hernia mesh repair and the predictive utility of ACS-NSQIP. J. Gastrointest. Surg. 2022 Apr;26(4):950–964. doi: 10.1007/s11605-022-05248-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Panaccio P., Raimondi P., Fiordaliso M., Dell’Osa A., Cotellese R., Innocenti P. Left colon obstruction due to non-reducible Spigelian hernia of the right side. Ann. Ital. Chir. 2016 Jul 15;87 [PubMed] [Google Scholar]
- 26.Anilir E., Buyuker F., Tosun S., Alimoglu O. Incarcerated Spigelian hernia: a rare cause of abdominal wall tender mass. North Clin Istanb. 2019 Nov 20;7(1):74–77. doi: 10.14744/nci.2018.09582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oen E.Y. Spigelian hernia and a “redundant” sigmoid colon. Med. J. Aust. 1971 Feb 6;1(6):329–331. [PubMed] [Google Scholar]
- 28.Som P.M., Khilnani M.T., Wolf B.S., Beranbaum S.L. Spigelian hernia. Acta Radiol. Diagn. (Stockh). 1976 May;17(3):305–312. doi: 10.1177/028418517601700306. [DOI] [PubMed] [Google Scholar]
- 29.Habib E., Elhadad A. Spigelian hernia long considered as diverticulitis: CT scan diagnosis and laparoscopic treatment. Surg. Endosc. 2003 Jan;17(1):159. doi: 10.1007/s00464-002-4237-y. [DOI] [PubMed] [Google Scholar]
- 30.Capaccio E., Di Vito L., Derchi L.E. Epiploic appendage torsed within a spigelian hernia: US and CT findings. J. Clin. Ultrasound. 2012 Jun;40(5):310–313. doi: 10.1002/jcu.20872. [DOI] [PubMed] [Google Scholar]
- 31.Miller R., Lifschitz O., Mavor E. Incarcerated Spigelian hernia mimicking obstructing colon carcinoma. Hernia. 2008 Feb;12(1):87–89. doi: 10.1007/s10029-007-0217-4. [DOI] [PubMed] [Google Scholar]
- 32.Polikarpova A., Ziaziaris W.A., Manoharan V. An unusual case of perforated sigmoid diverticulitis within a large left spigelian hernia. ANZ J. Surg. 2023 Dec;93(12):3018–3019. doi: 10.1111/ans.18696. [DOI] [PubMed] [Google Scholar]