Abstract
Background and Aim
Preconceptual care aiming to improve health is influenced by various factors including health literacy. Considering the importance and necessity of high quality preconceptual care, this study aimed to determine the relationship between health literacy and receiving components of preconceptual care prior to pregnancy.
Methods
This cross-sectional study included 693 participants with pregnancies of less than 14 weeks gestation referred to health centers and gynecologists in Shiraz city, Iran. Multi-stage sampling was done from May 2021 to February 2022 in 18 comprehensive urban health centers and 20 gynecology offices via proportional allocation method. The data collection tool comprised a questionnaire consisting of 3 parts: (1) individual and fertility characteristics, (2) information related to the components of preconceptual care and (3) health literacy for Iranian adults. This was completed by individual participants via the self-reporting method.
Results
The majority of participants were between 30 and 34 years old. They also identified as women with a university education and were predominantly unemployed. The mean health literacy of participants was 76.81%. Health literacy obtained the highest mean score in the dimension of ‘understanding’ and the lowest mean score in the dimension of ‘access’. The frequency of preconceptual counseling, folic acid supplement consumption, exercise, blood testing, dental visits, genetic counseling, Pap smear testing and rubella, diphtheria, and hepatitis vaccinations prior to pregnancy was 66.8%, 53.8%, 45.6%, 71.86%, 44.44%, 12%, 53.4%, 10.83%, respectively. Many (> 64%) received preconceptual care at specialist gynecology offices. Results demonstrated that health literacy had a statistically significant relationship with preconceptual care, folic acid consumption, exercise and dental care, (p < 0.001), along with blood testing and Pap smear testing (p < 0.05).
Conclusion
Overall, our results demonstrate that despite health literacy being optimal, uptakes of some components of preconceptual care are low. As such, it will be important to further raise awareness of the importance of preconceptual care for people prior to pregnancy as a priority in health promotion and education.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12875-024-02467-5.
Keywords: Health literacy, Preconceptual care, Pregnancy, Folic acid consumption, Preventative healthcare
Introduction
Preconceptual care (PCC) is carried out with those of reproductive age, prior to becoming pregnant or in the interval between pregnancies. PCC is considered necessary to promote health and wellbeing during pregnancy and childbirth [1, 2]. It leads to improved diet, increased folic acid supplementation, reduced smoking, weight loss and improved management of diabetes, all of which enhance perinatal outcomes [3–6]. According to the World Health Organization, PCC also reduces the occurrence of unwanted pregnancy by 50% [7], thus further reducing the risk of adverse perinatal outcomes [8]. PCC is particularly important in a context where perinatal mortality occurs most frequently in those who report not having had it [9, 10]. Nevertheless, the frequency of receiving PCC varies globally. For example, in the United States of America (USA), only one-third receive PCC [11]. Elsewhere, 40% in China [12], 18.2% in Ethiopia [13], 15.8% in France [14], 15.9% in Brazil [15], 27.2% in southern Sri Lanka [16] and 2.5% in Nigeria [17] receive PCC. In Iran, the prevalence of PCC differs from city to city, as 34.2% receive PCC in Mashhad [18] and 47.7% receive PCC in Isfahan [19]. Considering the above, there is considerable scope to improve both the provision and uptake of PCC on an international scale, particularly as considering the above, its relevance to primary care is clear.
Various factors are related to receiving PCC, including the availability of public and private health centers [10, 14], the cost of some services [20], treatment of healthcare workers [20], family support [13], access to information sources [21], age, education level, socio-economic status [11], chronic disease history [13], number of births [14] and health literacy [22, 23]. Health literacy refers to a person’s ability to evaluate, understand and use health-related information that promotes and maintains health [23, 24]. Thus, health literacy is closely related to preventive and health-promoting behaviors [25, 26]. Nevertheless, levels of health literacy are reportedly low [27]. In eight European countries 59% of people had insufficient health literacy [28]. In Iran, 44% of people reportedly have limited health literacy [29], with levels of health literacy being particularly low in Shiraz [30]. This is significant, as low levels of health literacy can result in people being less likely to receive PCC [31], including preconceptual counseling, folic acid supplementation, and vaccination [32]. Conversely, those who have higher levels of health literacy are more likely to receive preventive measures related to childbearing [33]. Consequently, it will be important to explore these relationships further and identify primary care strategies for increased health literacy and uptake of PCC globally.
Results regarding the relationship between health literacy and the receiving of preventive health services are contradictory [34, 35]. Moreover, no studies to date have explored the relationship between health literacy and PCC specifically, particularly in geographical areas where significantly low levels of healthcare literacy are reported, such as in Shiraz, Iran [30]. For this reason, this study aimed to determine the relationship between health literacy and the receiving of PCC including participants referring to urban health centers and the offices of gynecologists in Shiraz, Iran.
Methods
Study design and setting
This cross-sectional study was conducted with participants referring to health centers and gynecology offices in Shiraz, Iran. The selection of urban health centers as study settings was done using a multi-stage method. In the first stage, health centers were divided into 5 clusters based on the socio-economic level of potential participants in the Shiraz Municipality. The first cluster was classified as ‘high level’ (6 centers), the second cluster consisted of ‘upper middle level’ (5 centers), the third cluster consisted of ‘normal level’ (11 centers), the fourth cluster was classified as ‘average downward’ (7 centers) and the fifth cluster was classified as ‘weak’ (6 centers), from which 50% of the centers were selected via a simple random method. From all private gynecology offices in Shiraz (n = 165), 20 were selected via a simple random method (Supplementary file 1). Sampling occurred between May 2021 and February 2022 in both health centers and gynecology offices continuously until the sample size was reached. Informed consent was obtained by the research team from participants after providing information about the purpose of the research and the study method and assuring participants’ confidentiality at all times.
Inclusion and exclusion criteria
Participants who met the inclusion criteria were pregnant (≤ 14 weeks gestation), aged between 18 and 45 years, and Iranian residents of Shiraz city with the ability to complete the questionnaire. Participants were excluded if they did not complete their questionnaire.
Study sample
To determine the minimum sample size required to estimate the receipt of preconception care at a 95% confidence level and with the accuracy of estimation d = 0.03 and considering that the receipt of PCC in Shiraz city is 20% [35], after quantification in the following formula, the minimum required sample size was estimated to be n = 685.
 |
Outcome measures and measurements
Data collection tools included three questionnaires measuring (1) individual and fertility characteristics, (2) PCC information, and (3) health literacy of Iranian adults (HELIA) aged 18 to 65 years.
Questionnaire of individual and fertility characteristics included: age, education level, employment status, insurance status, socio-economic level, marital status, number of pregnancies, and source of receiving health information, current status of pregnancy, pregnancy gestation, and method of contraception.
PCC information questionnaire includes: PCC, provider of PCC, folic acid supplement consumption prior to pregnancy, exercise, blood testing, dental care access, genetic counseling, Papanicolaou (Pap) smear testing and preconceptual vaccination uptake [1, 10, 18, 19].
Health literacy of Iranian adults (HELIA) aged 18 to 65 years: HELIA was designed and psychometrically evaluated by Montazeri et al. (2013). The questionnaire has 33 items in 5 domains, including access to information (6 items), reading skill (4 items), understanding (7 items), appraisal (4 items) and the decision-making/behavioral intention dimension with 12 items. Scores obtained from this questionnaire for each person range between 33 and 165. The literacy level score for each person ranges between 0 and 100, whereby a higher score is indicative of a higher level of health literacy. A score between 0 and 50 is interpreted as ‘inadequate’, a score between 50.1 and 66 is ‘problematic’, 66.1–84 is ‘sufficient’ and 84.1–100 is ‘excellent’. HELIA is a reliable and valid instrument for measuring health literacy in Iran, and it’s internal consistency is satisfactory, with Cronbach’s alpha coefficients ranging from 0.72 to 0.89 [36].
Data analysis
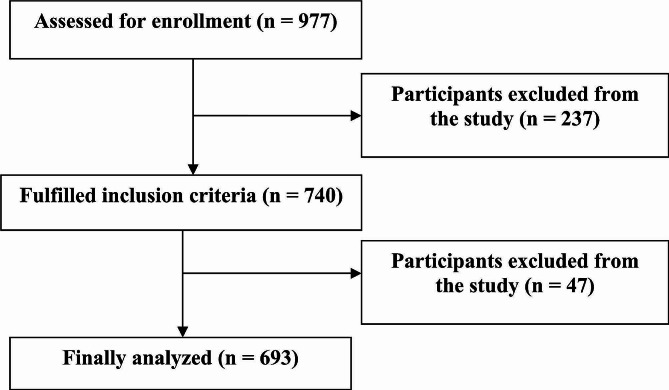
Data analysis was done using SPSS version 16 software via both descriptive and inferential statistics. For descriptive statistics, frequency distributions were used for the qualitative variables and numerical indicators of minimum, maximum, average along with standard deviation for the quantitative variables. For inferential statistics, an independent sample t-test and analysis of variance were used to analyze the data. To compare the health literacy score among the components consisting of two-modes (e.g., folic acid consumption, and exercise), Student’s t-test was used, and in variables with more than two modes (e.g., place where PCC was received, blood testing, dental care, genetic counseling, Pap smear testing, and vaccination), one-way analysis of variance was used (See Fig. 1).
Fig. 1.
Flow chart of participant selection
Results
Participants
As demonstrated in Table 1, an examination of the frequency of variables related to individual and fertility characteristics demonstrated that most participants were aged between 30 and 34 years old (32.2%) (Total age range: 17–44 years old), and that the majority of participants had a university level of education (59.3%), were unemployed (80.7%) with a relatively favorable self-reported economic status (58%). Overall, 78.2% of participants were of Persian ethnicity, and 56.7% had a current pregnancy between 7 and 12 weeks in gestation.
Table 1.
Frequency distribution of individual and fertility characteristics of participants
| Individuals and fertility characteristics | n | % | |
|---|---|---|---|
| Age (years) | < 20 | 24 | 3.5 |
| 20–24 | 80 | 11.5 | |
| 25–29 | 203 | 29.3 | |
| 30–35 | 262 | 37.8 | |
| 36–40 | 116 | 16.7 | |
| 41–45 | 8 | 1.2 | |
| Level of education | Primary | 23 | 3.3 |
| Secondary | 40 | 5.8 | |
| Diploma | 219 | 31.6 | |
| University education | 411 | 59.3 | |
| Occupational status | Unemployed | 559 | 80.7 |
| Employed | 134 | 19.3 | |
| Economic status | Unfavorable | 138 | 19.9 |
| Relatively favorable | 402 | 58 | |
| Favorable | 153 | 22.1 | |
| Insurance status | Yes | 559 | 80.7 |
| No | 134 | 19.3 | |
| Family relationship with spouse | Yes | 284 | 41 |
| No | 409 | 59 | |
| History of previous pregnancy | 1 | 257 | 37.1 |
| 2 | 247 | 35.6 | |
| 3 | 117 | 16.9 | |
| > 4 | 72 | 10.4 | |
| Pregnancy planning status | Planned | 570 | 82.3 |
| Unplanned | 123 | 17.7 | |
| Previous use of family planning | Yes | 397 | 57.3 |
| No | 269 | 42.7 | |
| Method of Contraception | Hormonal methods | 41 | 10.3 |
| Withdrawal | 228 | 57.4 | |
| Condom | 113 | 28.5 | |
| IUD | 15 | 3.8 | |
| Gestational age (Weeks) | ≤ 6 | 64 | 9.2 |
| 7–12 | 393 | 56.7 | |
| 12–14 | 236 | 34.1 | |
| Source of health information | Health care providers | 463 | 66.8 |
| Friends and relatives | 117 | 16.9 | |
| National media (including TV/radio/newspaper) | 60 | 8.7 | |
| Reading books, pamphlets, educational and promotional brochures & Newspapers, periodicals and magazines | 137 | 19.8 | |
| Social media (including WhatsApp/Telegram/Instagram, etc.) | 293 | 42.3 | |
| I don’t know where to get the information | 37 | 5.3 | |
Health literacy and domains
As shown in Tables 2 and 40.3% of participants scored ‘sufficient’ in the access to information dimension, 38.4% scored ‘sufficient’ in the appraisal dimension, and 44.7% scored ‘sufficient’ in the decision-making and behavioral intention dimension more than any other level. However, in the two dimensions related to reading and understanding, participants had a high level of health literacy (37.7% and 58.9%, respectively), more frequently than any other level. Overall, 49.4% of participants demonstrated a ‘sufficient’ level of health literacy in this context.
Table 2.
Frequency distribution of health literacy and domains
| Health literacy and its dimensions | Inadequate | Problematic | Sufficient | Excellent | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Access to information | 137 | 19.8 | 112 | 16.2 | 279 | 40.3 | 165 | 23.8 |
| Reading | 81 | 11.7 | 93 | 13.4 | 258 | 37.2 | 261 | 37.7 |
| Understanding | 27 | 3.9 | 57 | 8.2 | 201 | 29 | 408 | 58.9 |
| Appraisal | 106 | 15.3 | 112 | 16.2 | 266 | 38.4 | 209 | 30.2 |
|
Decision making/ behavioral intention |
39 | 5.6 | 113 | 16.3 | 310 | 44.7 | 231 | 33.3 |
| Health literacy | 21 | 3 | 111 | 16 | 342 | 49.4 | 219 | 31.6 |
As presented in Table 3, health literacy is most highly scored within the ‘understanding’ dimension with a mean of 83.84 and a standard deviation of 15.22. The lowest scores relate to the ‘access to information’ dimension with a mean of 70.14 and a standard deviation of 20.5. Health literacy obtained a mean of 76.81 with a standard deviation of 13.22.
Table 3.
Numerical indicators of health literacy
| Health literacy and its dimensions | Minimum | Maximum | Mean | SD | Base 0 to 100 | |||
|---|---|---|---|---|---|---|---|---|
| Minimal | Maximum | Mean | SD | |||||
| Access to information (6–30) | 6 | 30 | 22.83 | 4.92 | 0 | 100 | 70.14 | 20.5 |
| Reading (4–20) | 4 | 20 | 16.35 | 2.96 | 0 | 100 | 77.24 | 18.59 |
| Understanding (7–35) | 11 | 35 | 30.75 | 4.26 | 14.29 | 100 | 84.83 | 15.22 |
| Appraisal (4–20) | 4 | 20 | 15.78 | 3.14 | 0 | 100 | 73.66 | 19.62 |
|
Decision making/ behavioral intention (12–60) |
24 | 60 | 48.64 | 7.3 | 25 | 100 | 76.33 | 15.21 |
| Health literacy (33–165) | 61 | 165 | 134.38 | 17.45 | 21.21 | 100 | 76.81 | 13.22 |
Health literacy correlates
As presented in Table 4, health literacy had a statistically significant relationship with PCC, folic acid consumption, exercise and dental care, (p < 0.001), along with blood testing and Pap smear testing (p < 0.05).
Table 4.
Mean and standard deviation of health literacy according to PCC
| PCC information | Percent (%) | Frequency (n) |
Health literacy | P - value | ||
|---|---|---|---|---|---|---|
| Mean | SD | |||||
| PCC received | Yes | 463 | 66.8 | 78.45 | 12.26 | < 0.001 * |
| No | 230 | 33.2 | 73.48 | 14.44 | ||
| Place where PCC was received | General practitioner office | 75 | 16.2 | 78 | 13.37 | 0.75** |
| Health care workers in health centers | 36 | 7.8 | 76.52 | 11.73 | ||
| Midwifery office | 55 | 11.9 | 78.59 | 11.84 | ||
| Gynecologist’s office | 297 | 64.1 | 78.78 | 12.14 | ||
| Folic acid consumption | Yes | 373 | 53.8 | 78.67 | 11.89 | < 0.001 * |
| No | 320 | 46.2 | 74.63 | 14.34 | ||
| Exercise | Yes | 316 | 45.6 | 78.41 | 12.09 | < 0.001 * |
| No | 377 | 54.4 | 74.88 | 14.24 | ||
| Blood testing | Yes | 498 | 71.86 | 77.94 | 12.34 | 0.001 ** |
| No | 160 | 23.09 | 73.38 | 15.11 | ||
| Not recommended | 35 | 5.05 | 76.27 | 13.81 | ||
| Dental care | Yes | 308 | 44.44 | 79.2 | 12.19 | < 0.001 ** |
| No | 348 | 50.21 | 74.94 | 13.59 | ||
| Not recommended | 37 | 5.35 | 74.34 | 14.96 | ||
| Genetic counseling | Yes | 83 | 12 | 77.51 | 12.83 | 0.688** |
| No | 530 | 76.5 | 76.56 | 13.2 | ||
| Not recommended | 80 | 11.5 | 77.66 | 13.84 | ||
| Pap smear testing | Yes | 370 | 53.4 | 78.01 | 12.92 | 0.035 ** |
| No | 295 | 42.6 | 75.46 | 13.49 | ||
| Not recommended | 28 | 4 | 75 | 13.21 | ||
|
Vaccination (DT, HBS, Rubella) |
Yes | 75 | 10.83 | 79.55 | 14.75 | 0.156 ** |
| No | 518 | 74.74 | 76.4 | 12.65 | ||
| Not recommended | 100 | 14.43 | 76.83 | 14.76 | ||
* Independent t-test, ** One way ANOVA
Discussion
The present study examined the relationship between health literacy and PCC. Results demonstrated that the mean health literacy of participants (76.81%) and health literacy had the highest mean score in the dimension of ‘understanding’, and the lowest mean score in the dimension related to ‘access to information’ when compared to others. Health literacy was limited in 19% of participants, (‘inadequate’ 3% and ‘problematic’ 16%). Contrariwise, health literacy was good in 81% of participants (‘sufficient’ 49.9% and ‘excellent’ 31.6%). For comparison, a mean total health literacy score of 68.32% (highest score related to ‘understanding’ and lowest score related to the dimension of ‘appraisal’) has previously been reported for Iranian adults aged 18 to 65 years living in the cities of Iran [29]. In contrast, the pregnant participants in the present study were between 18 and 45 years old, their mean score of health literacy and the level of health literacy were higher. Yet unemployed people, and those over 55 years old and people with 1 to 5 years of education have reportedly lower health literacy elsewhere [29], and so this may explain some of the difference noted. In another study including participants who had recently given birth, health literacy was reported to be relatively favorable [37]. This suggests that there may be nuanced understandings and opportunities in relation to the health literacy of Iranian childbearing populations in particular to explore.
A seperate study conducted in Iran exploring the relationship between health literacy and physical self-efficacy and including participants in the postpartum period identified that 27.5% had sufficient health literacy [38]. This is in distinct contrast to the results of the present study. Yet the rapid estimate of adult literacy in medicine tool was used in contrast to the present study, and participant numbers were much lower (n = 120). In another Iranian study conducted with a higher number of pregnant participants (n = 775) (Busher, Ahvaz, Bandar Abbas and Zahedan), results showed that despite the average age of participants being 31.89 years and similar to the present study, 15.5% had insufficient health literacy, 41.7% had borderline health literacy and 42.8% had sufficient health literacy [39]. Whilst the picture of health literacy and childbearing in Iran remains complex, differing health literacy levels are also noted elsewhere such as in Turkey, where only 33.9% of pregnant participants had a sufficient level of health literacy [40]. Considering the above, studies with larger cohorts which cover a variety of geographical areas may improve understanding in this area overall.
In relation to educational level, only 37% of participants living on the Myanmar-Thailand border were found to have sufficient health literacy despite the fact that more than half (63.1%) were able to read [41]. In the current study, approximately 60% of participants had university education, while in Gilder’s study (2019), approximately half of the studied population had no education. This could be the reason for the lower level of health literacy in such immigrant populations. In the comparisons between the present study and the studies conducted in different cities of Iran and other parts of the world, differences were notable. Seemingly, ethnicity and local culture can affect a person’s health and health literacy. Other researchers have proposed a variety of explanations for the differences seen between provinces and countries [32]. There are also differences to be noted in the measurement tools used, the uniqueness of each research population, the method of implementation, the sampling type (probability or non-probability), the method of data collection (interview or self-report), which may also affect the results of the studies and lead to differences in the health literacy scores of individuals. A standardized approach to this area of research may avoid unnecessary inconsistencies, and coupled with more qualitative approaches, enable a richer understanding of the context in which studies are being conducted.
Regarding the frequency of receiving PCC components and the relationship between health literacy and receiving PCC components, the results of this study showed that the frequency of preconceptual counseling, folic acid supplement consumption, exercise, blood testing, dental visits, genetic counseling, Pap smear testing and rubella, diphtheria, and hepatitis vaccinations prior to pregnancy was 66.8%, 53.8%, 45.6%, 71.86%, 44.44%, 12%, 53.4%, 10.83%, respectively. Many (> 64%) received PCC at specialist gynecology offices. In the current study, among the components of PCC, the highest frequency related to pre-pregnancy blood testing, and the lowest was related to receiving vaccines. Overall, 66.8% of participants received their health information from health care providers. We identified a statistically significant relationship between health literacy and PCC, taking folic acid supplements, performing blood tests, going to the dentist, and performing a Pap smear test. Ultimately, the mean score of health literacy in participants who received these components was higher than the group that did not. This suggests that those who had higher health literacy received more preventive measures and health care, a finding consistent within the literature elsewhere [33]. Indeed, people with low health literacy are less likely to receive PCC and participate in taking folic acid supplements and smoking cessation [31]. They are also less likely to receive PCC, including counseling, and prenatal vaccines [32]. Yet those who have a higher awareness of PCC have an increased chance of engaging in such preventative measures [42–45]. Thus, future healthcare strategies could usefully seek to increase uptake and knowledge of PCC alongside health literacy to increase uptake of preventative healthcare measures overall prior to pregnancy.
In the present study, the health literacy score of those who exercised before pregnancy was higher than those who did not. Among the factors of awareness, attitude, abstract norms and enabling factors, awareness is known to have the greatest impact on physical activity [46]. Thus, the first step in improving the level of physical activity is to increase awareness about the importance and correct form in physical activity. Increasing awareness in this way is likely to lead to behavior change [46]. Moreover, health literacy can promote healthier lifestyles [47], as those who have higher health literacy exercise more [47]. Thus, the challenge for future research will be to ascertain how people of reproductive age may best increase their health literacy and physical activity for healthier lives and improved outcomes in health.
Again, our results demonstrate that health literacy was higher in people receiving dental services. Consistent with this, oral health literacy has been found related to periodontal status [48], health literacy and outcomes have also found to be related to oral health and oral hygiene behaviors [49, 50]. Yet in another study conducted in Japan, health literacy was found to have no statistically significant relationship with dental visits [34]. Yet this may be because in this study, the health checkup tool was used to measure health literacy, which measures people’s health literacy in two dimensions, communicative and critical health literacy [51]. Regarding the relationship between health literacy and Pap smear testing, health literacy has been shown to be related to cancer screening in non-working people [34]. This finding is also consisted with those presented here, and suggests that where people have higher literacy levels, engagement with screening and preventative services may increase. Contrariwise, where health literacy is low, services are placed under increased pressure as people are more likely to be readmitted to healthcare units and attend emergency departments more frequently [52–54].
Strengths and limitations and suggestions for future research
A key strength of the present study is that it has employed multi-stage sampling techniques and has achieved a high sample size. Nevertheless, there have been some non-completions of the questionnaire by participants living in more rural areas. The results presented are not generalisable. Moreover, as over half of those participating had university education, our sample may not be representative of the population of reproductive age in Shiraz. Also, the components of PCC were measured as ‘yes’ or ‘no’ rather than in more nuanced ways, and neither the number of days of folic acid consumption nor the amount of exercise taken per week was investigated. Due to the COVID-19 pandemic at the time of sampling, the majority of participants we collected data from were referred to private gynecology offices. Consequently, it was not possible to include larger numbers of participants from health centers for comparison. Future research could usefully include participants from rural areas and health centers to examine such relationships further, including those between health literacy and regular consumption of folic acid and exercise prior to pregnancy.
Conclusion
Overall, our results demonstrate that despite health literacy being optimal, uptakes of some components of PCC are low. As such, it will be important to further raise awareness of the importance of PCC for people prior to pregnancy as a priority in health promotion and education.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
This research was supported by the research grant no. IR.IUMS.REC.1399.1318 from Iran University of Medical Sciences. The author would like to thank the women who participated in this study.
Author contributions
Authors’ contributions: F.S. and L.A.F. designed the study. F.S., L.A.F., and S.H. analyzed and interpreted the data. F.S., S.P., and L.A.F. provided interpretations, supervision and wrote and revised the paper.
Funding
Current study was funded and supported by Iran University of Medical Sciences (Grant no. IR.IUMS.REC.1399.1318).
Data availability
The datasets generated and analyzed during the current study are not publicly available due to the confidentiality of information, but they can be available through the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee of Iran University of Medical Sciences, Tehran, Iran (Number: IR.IUMS.REC.1399.1318. In addition, informed written consent was obtained from the participants and the respondents were fully informed of the purpose and procedures of the study. They were also assured of confidentiality of information. All methods were carried out in accordance with our study protocol, along with relevant guidelines and regulation associated with the Iran University of Medical Sciences and professional regulatory bodies such as the Nursing and Midwifery Council.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ministry of Health TaME, Office of Family and Population Health, Department of Maternal Health . Safe Mother Country Program: Integrated Maternal Health Care. 7, editor. IRAN: PADIDEH GOYA; 2023. [Google Scholar]
- 2.CDC. PERCONCEPTION CARE Content source: Centers for Disease Control and Prevention2020 [updated February 26,2020. https://www.cdc.gov/preconception/overview.html.
- 3.de Lima A, Zelinkova Z, Mulders AGMGJ, van der Woude CJ. Preconception Care reduces relapse of inflammatory bowel disease during pregnancy. Clin Gastroenterol Hepatol. 2016;14(9):1285–e921. doi: 10.1016/j.cgh.2016.03.018. [DOI] [PubMed] [Google Scholar]
- 4.Schummers L, Hutcheon JA, Bodnar LM, Lieberman E, Himes KP. Risk of adverse pregnancy outcomes by prepregnancy body mass index: a population-based study to inform prepregnancy weight loss counseling. Obstet Gynecol. 2015;125(1):133. doi: 10.1097/AOG.0000000000000591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bortolus R, Oprandi NC, Rech Morassutti F, Marchetto L, Filippini F, Agricola E et al. Why women do not ask for information on preconception health? A qualitative study. BMC Pregnancy Childbirth. 2017;17(1). [DOI] [PMC free article] [PubMed]
- 6.Khan NN, Boyle JA, Lang AY, Harrison CL. Preconception Health attitudes and behaviours of women: a qualitative investigation. Nutrients. 2019;11(7):1490. doi: 10.3390/nu11071490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO. Meeting to develop a global consensus on preconception care to reduce maternal and childhood mortality and morbidity: World Health Organization Headquarters, Geneva, 6–7 February 2012: meeting report. 2013.
- 8.Fowler JR, Mahdy H, Jack BW. Preconception Counseling: StatPearls Publishing, Treasure Island (FL); 2019 2019.
- 9.Beigi M, Sadatmahaleh SJ, Changizi N, Mohammadi E, Kazemi A. Analysis of the Iranian maternal mortality surveillance system and providing system improvement strategies: study protocol for strategy formulation. Reproductive Health. 2020;17(1):1–6. doi: 10.1186/s12978-020-00963-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ghafoori O, Pakpour A, Jourabchi Z. Factors affecting preconception care in married women participating in premarital educational courses: application of planned behavior theory. J Torbat Heydariyeh Univ Med Sci. 2018;6(3):60–70. [Google Scholar]
- 11.Wally MK, Huber LRB, Issel LM, Thompson ME. Matern Child Health J. 2018;22(1):2009–11. The Association Between Preconception Care Receipt and the Timeliness and Adequacy of Prenatal Care: An Examination of Multistate Data from Pregnancy Risk Assessment Monitoring System (PRAMS). [DOI] [PubMed]
- 12.Ding Y, Li XT, Xie F, Yang YL. Survey on the implementation of Preconception Care in S Hanghai, C hina. Paediatr Perinat Epidemiol. 2015;29(6):492–500. doi: 10.1111/ppe.12218. [DOI] [PubMed] [Google Scholar]
- 13.Asresu TT, Hailu D, Girmay B, Abrha MW, Weldearegay HG. Mothers’ utilization and associated factors in preconception care in northern Ethiopia: a community based cross sectional study. BMC Pregnancy Childbirth. 2019;19(1):1–7. doi: 10.1186/s12884-019-2478-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paradis S, Ego A, Bosson J-L. Preconception care among low-risk mothers in a French perinatal network: frequency of utilization and factors associated. J Gynecol Obstet Hum Reprod. 2017;46(7):591–6. doi: 10.1016/j.jogoh.2017.05.002. [DOI] [PubMed] [Google Scholar]
- 15.Borges AL, Santos OA, Nascimento Nde C, Chofakian CB, Gomes-Sponholz FA. Preconception health behaviors associated with pregnancy planning status among Brazilian women. Volume 50. Revista da Escola de Enfermagem da U S P; 2016. pp. 208–16. 2. [DOI] [PubMed]
- 16.Patabendige M, Goonewardene I. Preconception care received by women attending antenatal clinics at a Teaching Hospital in Southern Sri Lanka. Sri Lanka J Obstet Gynecol. 2013;35(1).
- 17.Lawal TA, Adeleye AO. Determinants of folic acid intake during preconception and in early pregnancy by mothers in Ibadan, Nigeria. Pan Afr Med J. 2014;19:113. doi: 10.11604/pamj.2014.19.113.4448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Latifnejad Roudsari R, Bayrami R, Javadnoori M, Allahverdipour H, Esmaily H. Patterns and Determinants of Preconception Health Behaviors in Iranian Women. Iran Red Crescent Med J. 2016;18(12):e59044. doi: 10.5812/ircmj.28565. [DOI] [Google Scholar]
- 19.Shadab P, Nekuei N, Yadegarfar G. The prevalence of preconception care, its relation with recipients’ individuality, fertility, and the causes of lack of checkup in women who gave birth in Isfahan hospitals in 2016. J Educ Health Promotion. 2017;6. [DOI] [PMC free article] [PubMed]
- 20.ShamshiriMilani H, Khazaie F, Rassouli M, Ramezankhani A. Explanation of women’s and family health care personnel’s perception of the barriers of pre-pregnancy care coverage: a qualitative study. J Health Field. 2016;1(3):18–27. [Google Scholar]
- 21.Afshari M, Khazaei S, Bahrami M, Merati H. Investigating Adult Health Literacy in Tuyserkan City. J Educ Community Health. 2014;1(2):48–55. doi: 10.20286/jech-010248. [DOI] [Google Scholar]
- 22.Dorney E, Black KI. Preconception care. Australian J Gen Pract. 2018;47(7):424–9. doi: 10.31128/AJGP-02-18-4485. [DOI] [PubMed] [Google Scholar]
- 23.Fransen MP, Hopman ME, Murugesu L, Rosman AN, Smith SK. Preconception counselling for low health literate women: an exploration of determinants in the Netherlands. Reproductive Health. 2018;15(1):192. doi: 10.1186/s12978-018-0617-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12(1):80. doi: 10.1186/1471-2458-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mahdavi Z, Ramezani A, GHanbari S, KHodakaram L. RELATIONSHIP BETWEEN HEALTH LITERACY AND FEMALE CANCERS PREVENTIVE BEHAVIORS. PAYESH. 2017;16(5):–.
- 26.Castro-Sánchez E, Chang PWS, Vila-Candel R, Escobedo AA, Holmes AH. Health literacy and infectious diseases: why does it matter? Int J Infect Dis. 2016;43:103–10. doi: 10.1016/j.ijid.2015.12.019. [DOI] [PubMed] [Google Scholar]
- 27.Espanha R, Ávila P. Health literacy survey Portugal: a contribution for the knowledge on health and communications. Procedia Comput Sci. 2016;100:1033–41. doi: 10.1016/j.procs.2016.09.277. [DOI] [Google Scholar]
- 28.Sørensen K, Pelikan JM, Röthlin F, Ganahl K, Slonska Z, Doyle G, et al. Health literacy in Europe: comparative results of the European health literacy survey (HLS-EU) Eur J Pub Health. 2015;25(6):1053–8. doi: 10.1093/eurpub/ckv043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tavousi M, Haeri Mehrizi A, Rafieifar SH, Soleimanian A, Sarbandi F, Ardestani MS, et al. Health literacy in Iran: findings from a national study. Health Monit J Iran Inst Health Sci Res. 2016;15(1):95–102. [Google Scholar]
- 30.Khosravi A, Kh A, Sh A, Tahmasbi R. Health literacy levels of diabetic patients referred to Shiraz health centers and its effective factors. Health Inf Manage. 2015;12(2):205. [Google Scholar]
- 31.Sodergren SC, Husson O, Robinson J, Rohde GE, Tomaszewska IM, Vivat B, et al. Systematic review of the health-related quality of life issues facing adolescents and young adults with cancer. Qual Life Res. 2017;26:1659–72. doi: 10.1007/s11136-017-1520-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tang C, Wu X, Chen X, Pan B, Yang X. Examining income-related inequality in health literacy and health-information seeking among urban population in China. BMC Public Health. 2019;19:1–9. doi: 10.1186/s12889-019-6538-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ghanbari S, Majlessi F, Ghaffari M, Mahmoodi Majdabadi M. Evaluation of health literacy of pregnant women in urban health centers of Shahid Beheshti Medical University. Daneshvar Med. 2020;19(6):1–12. [Google Scholar]
- 34.Goto E, Ishikawa H, Okuhara T, Kiuchi T. Relationship of health literacy with utilization of health-care services in a general Japanese population. Prev Med Rep. 2019;14:100811. doi: 10.1016/j.pmedr.2019.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.sib.sums.ac.ir. Integrated health electronic system 2021 [ https://sib.sums.ac.ir/SibReport/PublicUserReport_Count/Index?id_Group=1014&Id_ParentReport=111350&showType=1.
- 36.Montazeri A, Tavousi M, Rakhshani F, Azin SA, Jahangiri K, Ebadi M, et al. Health literacy for Iranian adults (HELIA): development and psychometric properties. Health Monit J Iran Inst Health Sci Res. 2014;13(5):589–99. [Google Scholar]
- 37.Nodooshan T, Pirzadeh A, Nasirian M. The relationship between Maternal Health Literacy and Pregnancy Status in New Mothers Who Referred to Health Centers of Yazd. Tolooebehdasht. 2020;18(6):22–33. [Google Scholar]
- 38.Peyman N, Abdollahi M. The relationship between health literacy and self-efficacy physical activity in postpartum women. J Health Lit. 2016;1(1):5–12. [Google Scholar]
- 39.Dadipoor S, Ramezankhani A, Alavi A, Aghamolaei T, Safari-Moradabadi A. Pregnant women’s health literacy in the south of Iran. J Family Reproductive Health. 2017;11(4):211. [PMC free article] [PubMed] [Google Scholar]
- 40.Guler DS, Sahin S, Ozdemir K, Unsal A, Uslu Yuvacı H. Health literacy and knowledge of antenatal care among pregnant women. Health Soc Care Commun. 2021;29(6):1815–23. doi: 10.1111/hsc.13291. [DOI] [PubMed] [Google Scholar]
- 41.Gilder ME, Moo P, Praisaengdet AHIDN, Wai K, Pimanpanarak M et al. I can’t read and don’t understand: Health literacy and health messaging about folic acid for neural tube defect prevention in a migrant population on the Myanmar-Thailand border. 2019. [DOI] [PMC free article] [PubMed]
- 42.Adeyemo AA, Bello OO. Preconception care: what women know, think and do. Afr J Med Health Sci. 2021;20(2):18–26. [Google Scholar]
- 43.Fekene DB, Woldeyes BS, Erena MM, Demisse GA. Knowledge, uptake of preconception care and associated factors among reproductive age group women in West Shewa zone, Ethiopia, 2018. BMC women’s health. 2020;20:1–8. [DOI] [PMC free article] [PubMed]
- 44.Roudsari RL, Bayrami R, Javadnoori M, Allahverdipour H, Esmaily H. Patterns and determinants of preconception health behaviors in Iranian women. Iran Red Crescent Med J. 2016;18(12).
- 45.Pandolfi E, Gonfiantini MV, Gesualdo F, Romano M, Carloni E, Mastroiacovo P, et al. Women participating in a web-based preconception study have a high prevalence of risk factors for adverse pregnancy outcomes. BMC Pregnancy Childbirth. 2014;14(1):1–6. doi: 10.1186/1471-2393-14-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bayrami R, Didarloo A, Asadinejad A. Prediction of physical activity based on the BASNEF model constructs during preconception period among women referred to Uremia health centers. Hayat J. 2020;26(1):105–17. [Google Scholar]
- 47.Eftekhari MJ, Rahimnia M, Esfahanian H, Bazoobandi B, Shams M. Health literacy level of adults in Neyshabur City: a cross-sectional study. J Educ Community Health. 2019;6(3):161–7. doi: 10.29252/jech.6.3.161. [DOI] [Google Scholar]
- 48.Ardakani AH, Sharifabad MAM, Rezapour Y, Ardakani AP. Investigation of the relationship of oral health literacy and oral hygiene self-efficacy with DMFT and Gingival index in students of Ardakan University. Payesh (Health Monitor) 2015;14(3):351–62. [Google Scholar]
- 49.Firmino RT, Ferreira FM, Paiva SM, Granville-Garcia AF, Fraiz FC, Martins CC. Oral health literacy and associated oral conditions: a systematic review. J Am Dent Association. 2017;148(8):604–13. doi: 10.1016/j.adaj.2017.04.012. [DOI] [PubMed] [Google Scholar]
- 50.Vann W, Jr, Lee JY, Baker D, Divaris K. Oral health literacy among female caregivers: impact on oral health outcomes in early childhood. J Dent Res. 2010;89(12):1395–400. doi: 10.1177/0022034510379601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ishikawa H, Nomura K, Sato M, Yano E. Developing a measure of communicative and critical health literacy: a pilot study of Japanese office workers. Health Promot Int. 2008;23(3):269–74. doi: 10.1093/heapro/dan017. [DOI] [PubMed] [Google Scholar]
- 52.Griffey RT, Kennedy SK, McGownan L, Goodman M, Kaphingst KA. Is low health literacy associated with increased emergency department utilization and recidivism? Acad Emerg Med. 2014;21(10):1109–15. doi: 10.1111/acem.12476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Khalife-Ghaderi F, Amiri‐Farahani L, Haghani S, Hasanpoor‐Azghady SB. Examining the experience of childbirth and its predictors among women who have recently given birth. Nurs open. 2021;8(1):63–71. doi: 10.1002/nop2.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sohbati F, Hasanpoor-Azghady SB, Jafarabadi M, Amiri-Farahani L, Mohebbi M. Psychological well-being of infertile women and its relationship with demographic factors and fertility history: a cross-sectional study. BMC Womens Health. 2021;21:1–7. doi: 10.1186/s12905-020-01167-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and analyzed during the current study are not publicly available due to the confidentiality of information, but they can be available through the corresponding author on reasonable request.