Abstract
Background:
Lower socioeconomic status and public insurance lead to a longer delay to surgery and a higher likelihood of concomitant pathology before undergoing anterior cruciate ligament reconstruction (ACLR). However, few studies have examined the influence of community deprivation on ACLR timing and outcomes.
Purpose/Hypothesis:
The primary aim of this study was to define the effect of the area deprivation index (ADI) and insurance classification on access to orthopaedic care after an ACL rupture, and the secondary aim was to determine whether these variables were associated with a second ACL injury after primary ACLR. It was hypothesized that patients with a greater national ADI percentile and Medicaid insurance would experience longer delays to care and an increased risk of reinjury after ACLR.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
A retrospective study was performed to evaluate patients undergoing primary ACLR between 2016 and 2019. The national ADI percentile was obtained utilizing the Neighborhood Atlas website. The relationship between national ADI percentile and care characteristics (eg, time to specialized care) was investigated using the Spearman rho correlation coefficient (r). The association between patient and care characteristics and second ACL injury after the index procedure (ie, graft rerupture or contralateral ACL rupture) was investigated using binary logistic regression.
Results:
A total of 197 patients met the inclusion criteria. Longer times from injury to surgery (r = 0.238; P < .001) and from specialized care to surgery (r = 0.217; P = .002) were associated with a greater national ADI percentile. The second injury group reported significantly greater national ADI (P = .026) and included a greater percentage of patients with Medicaid insurance (31.3%) compared with the no second injury group. Patients experienced 5.1% greater odds of a second ACL injury for each additional month between evaluation and surgery.
Conclusion:
Greater national ADI percentile and Medicaid insurance status were associated with adverse ACLR timing and outcomes. Patients with a greater national ADI percentile took significantly longer to obtain surgery after ACL injury. Those who sustained a second ACL injury after ACLR had an overall higher mean national ADI percentile and included a greater proportion of patients with Medicaid compared with those who did not sustain a second ACL injury. Future studies should critically investigate the underlying factors of these associations to reach equity in orthopaedic care.
Keywords: anterior cruciate ligament, area deprivation index, general, knee, ligaments, socioeconomic status
Anterior cruciate ligament (ACL) tears occur with an annual incidence of 68.6 per 100,000 person-years. 34 The current standard of care for this injury—ACL reconstruction (ACLR)—is performed to restore stability and knee function to return to sports and an elevated activity level. The time to surgery from the initial injury has been shown to vary in different patient populations, irrespective of the health care system, and delayed treatment leads to an increase in additional knee pathology and a decrease in long-term prognosis.7,8,21,25,27,41,42 While cost is readily assumed to be a significant barrier to accessing care, this may be only 1 of many factors that delay patients from seeking prompt treatment. 7
Socioeconomic disadvantage is a complex entity resulting from a combination of factors such as low income, limited education, poor living conditions, and decreased social support. 43 Recently, there has been increased interest in how socioeconomic status (SES) affects patient outcomes. 4 SES and insurance status have been shown to affect patient care and access to surgery throughout orthopaedic surgery subspecialties. ‡‡ In the context of ACL injuries, it has been reported that lower SES and public insurance status lead to a lower likelihood of receiving operative treatment, a longer delay from initial injury to surgery, and a higher likelihood of concomitant pathology before undergoing ACLR.3-4,6 However, many of the metrics utilized in previous studies relied on self-reports of indicators of SES and overlooked the influence of community deprivation on interactions with the health care system.
The area deprivation index (ADI) is a quantitative measure of social deprivation developed to provide researchers with an easily accessible geographic metric of community disadvantage at the level of a Census block group.16,40 Area deprivation has been shown to influence a person's health outcomes independently of other frequently reported SES measures; thus, health interventions that do not consider area deprivation may not provide a complete analysis of a person's disadvantage.16,22,38 In an orthopaedic setting, the ADI has been previously used to identify disparities in patients undergoing surgery in various orthopaedic subspecialties.2,6,28 Therefore, it has been suggested that the ADI and insurance classification used in conjunction may capture the most holistic picture of a patient's social deprivation. 6 However, to our knowledge, the ADI has not yet been studied as a tool to measure the effect of social deprivation on the care of patients with ACL injuries.
As a result, the primary aim of this study was to define the effect of the ADI and insurance classification on access to orthopaedic care after an ACL rupture. We hypothesized that Medicaid insurance status and a greater national ADI percentile, indicating greater area deprivation, would be associated with delays in accessing specialized care and operative treatment. The secondary aim was to determine whether these variables were associated with a second ACL injury after primary ACLR. We hypothesized that patients with a greater national ADI percentile and Medicaid insurance would have an increased risk of reinjury.
Methods
We performed a retrospective study to evaluate the association between patient characteristics, surgical characteristics, insurance status, ADI, and the prevalence of second ACL injury among a cohort of patients who underwent ACLR. This study was approved by the Western Institutional Review Board-Copernicus Group, and a waiver of consent was granted based on the nature of the investigation.
Participants
After the institutional review board approval, all ACLRs performed between 2016 and 2019 by 5 sports medicine fellowship-trained orthopaedic surgeons (including E.S.C.) underwent a chart review by the research team. The inclusion criteria were as follows: aged between 12 and 40 years; had undergone a primary, unilateral ACLR; and had a home address on file in our electronic medical record (EMR). The exclusion criteria were as follows: were not within the age range of 12 to 40 years (N = 42); had a revision or contralateral ACLR (N = 30); did not have complete descriptive data (N = 34); underwent ACLR with allograft tissue (N = 11); obtained care via a worker's compensation claim (N = 8); or did not have at least 2-year follow-up data available (N = 123).
Chart Review
Descriptive data—including age, self-reported race, biological sex, body mass index, smoking status, and insurance type—were collected via chart review at the patient's first clinical visit. Insurance was classified as being either commercial (eg, employer-provided) or Medicaid. Other types of government insurance (eg, Medicare) and worker's compensation were excluded because of previous reports that Medicaid status alone may be an independent predictor of inability to access orthopaedic care.17,24,26,31,35 Clinical information collected included the date of injury, date of the first visit with either an orthopaedic sports medicine surgeon or nonoperative sports medicine provider, date of surgery, and graft type. If a patient was unable to recount the exact date of their injury, a date was calculated based on their best estimation of the time frame stated on the date of their initial visit. Calculations were done to determine the time from the initial injury to the first visit with an orthopaedic sports medicine provider (including nonoperative sports medicine), the initial injury to surgery, and the initial orthopaedic sports medicine visit to the surgery.
Area Deprivation Index
National ADI percentiles were obtained through Version 3.1 of the Neighborhood Atlas from the University of Wisconsin-Madison School of Medicine and Public Health. 40 The ADI was developed by the Health Resources and Services Administration in 2003 as a measure of neighborhood-based social deprivation based on 17 variables using the data from the American Community Survey (ACS) Five Year Estimates and has been refined, validated, and made publicly available via the Neighborhood Atlas by Kind and Buckingham 16 and Singh. 38 The factors included in determining the national ADI and the factor weights in the ADI equation are summarized in Table 1, adapted from the initial calculation of the ADI by Singh. 38 ADI values—as portrayed on the Neighborhood Atlas—are regularly updated with new ACS data and recalculated to include more pertinent variables. Version 3.1 represents which values were most recently available at the time of data collection by the study team. The Neighborhood Atlas relies on only home addresses to report the national ADI percentile; patient addresses were collected during the chart review.
Table 1.
National Area Deprivation Index Percentile Factors and Factor Weights as Described by Singh 38
| Census Block Group Components | Factor Score Coefficients |
|---|---|
| Percent of the block group's population at least 25 years old, with <9 years of education | 0.0849 |
| Percent of the population at least 25 years old, with greater than or equal to a high school diploma education | −0.0970 |
| Percent of employed persons at least 16 years old in white-collar occupations | −0.0874 |
| Median family income | −0.0977 |
| Income disparity | 0.0936 |
| Median home value | −0.0688 |
| Median gross rent | −0.0781 |
| Median monthly mortgage | −0.0770 |
| Home ownership rate | −0.0615 |
| The civilian unemployment rate of the population at least 16 years old | 0.0806 |
| Percent of families below the poverty level | 0.0977 |
| Percent of the population below 150% of the poverty threshold | 0.1037 |
| Percent of single-parent households with children <18 years old | 0.0719 |
| Percent of occupied housing units without a motor vehicle | 0.0694 |
| Percent of occupied housing units without a telephone | 0.0877 |
| Percent of occupied housing units without complete plumbing | 0.0510 |
| Percent of occupied housing units with more than 1 person per room | 0.0556 |
Statistical Plan
Descriptive statistics were calculated for patient characteristics, national ADI percentiles, injury and surgical characteristics, and second ACL injury prevalences. A priori alpha level was established as .05, and all statistical analyses were completed in Jamovi Version 2.2.5—an open-source statistical software.
Access to Care
The relationships between care characteristics—including the time from injury to specialized care and the time from injury to surgery—and the national ADI percentile were characterized using the Spearman rho correlation coefficient (r). Correlation coefficients were interpreted as weak ≤0.4, moderate ≤0.6, and strong >0.6.
Second ACL Injury
Second, ACL injuries were categorized as ipsilateral or contralateral to the index ACL injury and compared using a binomial proportions test. Ipsilateral second ACL injuries were defined as post-ACLR graft ruptures. Contralateral second ACL injuries were defined as ACL ruptures that occurred in the contralateral knee after the index surgery. Participant age and body mass index were compared between second injury groups using independent samples t tests. The National ADI percentile and the time to evaluation or surgery were compared between groups using the Mann-Whitney U test. Sex assigned at birth, smoking status, race, graft source, and insurance type were compared between groups using chi-square tests. Binary logistic regression was used to determine the association between the national ADI percentile and secondary ACL injury, patient demographics, care characteristics, and surgical characteristics. Nonstandardized model estimates, odds ratios, and 95% CIs were reported for this regression model.
Results
A total of 197 patients met the inclusion criteria and had complete datasets for all variables of interest. The distribution of the national ADI percentile among our sample is depicted in Figure 1.
Figure 1.
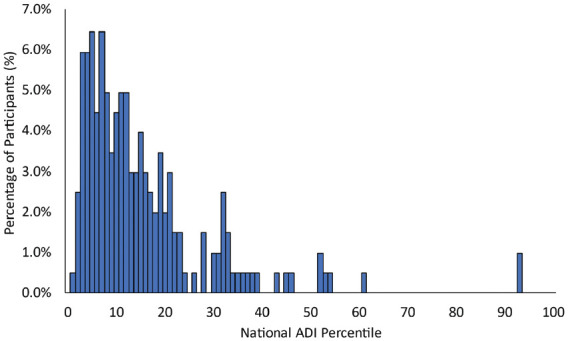
A histogram and density plot depicting the distribution of the national ADI among the sample. ADI, area deprivation index.
Access to Care
Longer times from injury to surgery (r = 0.238; P < .001) and longer times from specialized care to surgery (r = 0.217; P = .002) were associated with greater national ADI percentile, indicating greater deprivation and lower SES. Longer times from injury to specialized care (r = 0.119; P = .088) were not significantly associated with greater national ADI percentiles.
Second ACL Injury
A total of 32 (16.2%) patients experienced a second ACL injury. Comparisons of participant characteristics, injury characteristics, care characteristics, and surgical characteristics are summarized in Table 2. There were significantly more (n = 24 [75%]) contralateral injuries compared with ipsilateral graft failures (n = 8 [25%]; P = .007). No significant difference was observed in the prevalence of the second ACL injury (range, 10.7%-24.5%) among the 5 surgeons whose patients were included in this study (P = .406).
Table 2.
Patient and Surgical Characteristics Compared With Those Who Did and Did Not Experience a Second ACL Injury a
| No Second Injury | Second ACL Injury | P | |
|---|---|---|---|
| Sex assigned at birth | |||
| Female | 76 (46.1) | 16 (50) | .683 |
| Male | 89 (53.9) | 16 (50) | |
| Age, y | 23.4 ± 7.5 | 19.6 ± 6.5 | .008 b |
| BMI, kg/m2 | 25.3 ± 4.4 | 24.9 ± 3.9 | .555 |
| Smoking status | |||
| Current smoker | 8 (4.8) | 1 (3.1) | .284 |
| Former smoker | 11 (6.7) | 0 (0) | |
| Nonsmoker | 146 (88.5) | 31 (96.9) | |
| Race | |||
| American Indian or Alaska Native | 1 (0.5) | 0 (0) | .812 |
| Asian | 2 (15.2) | 3 (9.4) | |
| Black or African American | 27 (15.6) | 5 (15.6) | |
| Hispanic or Latino | 14 (8.5) | 3 (9.4) | |
| More than 1 race | 9 (5.5) | 1 (3.1) | |
| Native Hawaiian or Pacific Islander | 0 (0) | 0 (0) | |
| White | 73 (44.2) | 13 (40.6) | |
| Other/did not report | 19 (11.5) | 7 (21.9) | |
| National ADI c | 11 [13] | 14.5 [23.5] | .026 b |
| Weeks from injury to specialized care c | 17.1 [63] | 4.8 [10.5] | .730 |
| Months from injury to surgery c | 5.1 [14.5] | 2.8 [3.5] | .982 |
| Months from specialized care to surgery c | 1.4 [1.8] | 1.7 [1.8] | .481 |
| Months from surgery to chart review c | 48.8 [21.8] | 41.3 [20] | .331 |
| Graft source | |||
| Bone-patellar tendon-bone autograft | 87 (52.7) | 21 (65.6) | .005 b |
| Hamstring tendon autograft | 76 (46.1) | 8 (25) | |
| Quadriceps tendon autograft | 2 (1.2) | 3 (9.4) | |
| Meniscus procedure during ACLR | |||
| Repair | 55 (33.3) | 10 (31.3) | .384 |
| Partial meniscectomy | 47 (28.5) | 6 (18.8) | |
| None | 63 (38.2) | 16 (50) | |
| Insurance type | |||
| Commercial | 140 (84.8) | 22 (68.8) | .029 b |
| Medicaid | 25 (15.2) | 10 (31.3) | |
| Second ACL injury limb | |||
| Ipsilateral graft failure | — | 8 (25) | .007 b |
| Contralateral injury | — | 24 (75) | |
Data are presented as mean ± SD, n (%), or n [IQR]. ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction; ADI, area deprivation index; BMI, body mass index. Dashes indicate no second injury data.
Indicates a significant between-group difference.
Indicates between-group comparison via Mann-Whitney U test.
The second injury group was significantly younger (P = .008) and reported a significantly greater national ADI (P = .026) than the no second injury group. In addition, the second injury group significantly differed based on the distribution of the ACLR graft source (P = .005) and insurance type (P = .029), with the second injury group including a greater percentage of patients with bone-patellar tendon-bone autografts (65.6%) and Medicaid insurance (31.3%) when compared with the no second injury group (Table 2).
The statistics derived from our logistic regression model predicting a second ACL injury can be found in Table 3. The model significantly predicted a second ACL injury (P = .003). Those who experienced longer time from evaluation by an orthopaedic surgeon to surgery (P = .033) had a 1.051 (95% CI, 1.011-1.311) times greater odds of experiencing a second ACL injury. This means that for each month between evaluation and surgery, patients experienced 5.1% greater odds of experiencing a second ACL injury. The national ADI percentile (P = .180) and the time from injury to specialized care (P = .415) did not significantly contribute to the model.
Table 3.
Patient and Surgical Characteristics
| β Value | Odds Ratio (95% CI) | P | |
|---|---|---|---|
| Intercept | −1.263 | 0.283 (0.057-1.399) | .121 |
| Sex assigned at birth | |||
| Male-female | −0.253 | 0.777 (0.318-1.896) | .579 |
| Age, y | −0.034 | 0.966 (0.897-1.041) | .365 |
| Graft source | |||
| Bone-patellar tendon-bone, hamstring tendon autograft | −0.621 | 0.538 (0.191-1.514) | .240 |
| Bone-patellar tendon-bone, quadriceps tendon autograft | 1.707 | 5.514 (0.808-37.616) | .081 |
| Months from injury to specialized care | −0.039 | 0.962 (0.876-1.056) | .415 |
| Months from specialized care to surgery | 0.005 | 1.051 (1.011-1.311) | .033 |
| National area deprivation index | 0.018 | 1.018 (0.992-1.046) | .180 |
| Insurance type | |||
| Commercial-Medicaid | 0.604 | 1.830 (0.644-5.204) | .257 |
Discussion
The most important finding of this study was that indicators of low SES—such as high national ADI percentile and Medicaid status—were significantly correlated with delays in care after ACL injury and a greater risk of reinjury after ACLR. While recent research2,6,29 has demonstrated how SES affects patient outcomes after orthopaedic injuries, our study is the first, to our knowledge, to investigate ADI in the context of ACL injury. We found that patients with a greater national ADI percentile experienced a longer time from injury to surgery and a longer time from specialized care to surgery. Our results also showed that the cohort of patients who experienced a second ACL injury had a significantly greater mean national ADI percentile and were more likely to use Medicaid insurance than the cohort of patients who did not experience a second ACL injury. These findings introduce the novel findings that greater area deprivation increases delays to care after ACL injury and greater area deprivation and Medicaid insurance negatively affect patient outcomes after ACLR.
Previous studies have described the effect that SES has on access to care and surgical outcomes for patients with ACL injury. In 2014, Newman et al 25 reported that pediatric and adolescent patients with lower household income and noncommercial insurance were more likely to experience a delay in treatment after ACL injury and were at a greater risk of an additional knee injury before surgery. Williams et al 41 later confirmed these findings in younger patients undergoing ACLR at a single pediatric sports medicine center in conjunction with a free-standing children's hospital. They found that patients with public health insurance experienced greater delays from injury to presentation and had more severe chondral and meniscal injuries than their counterparts with commercial insurance. In 2019, the Multicenter Orthopaedic Outcomes Network (MOON) Group found that patients undergoing ACLR with lower SES reported poorer subjective outcomes and were less active at a 2-year follow-up. 14 More recently, Chava et al 5 reported that patients with Medicaid insurance who underwent ACLR had lower postoperative subjective functional outcomes and were less likely to return to sport. Thus, patients with lower SES experience longer delays to treatment, are at greater risk for an additional knee injury, and have worse postoperative outcomes.
However, there are some limitations to the previous research that has been performed on SES in patients with ACL injury. First, these studies frequently use solely household income or insurance classification as a surrogate for SES, which can ignore other factors that affect a patient's access to care and, in some cases, introduce response bias. Second, these studies typically focus on individual SES and do not account for community-level deprivation, which may be equally as important as individual deprivation.13,23 To our knowledge, the 2019 MOON Group study is the only one thus far to have examined community-level SES as a predictor of ACLR outcomes. 14 In their study, the MOON group created their own “SES Index” using 6 variables from the 2000 United States Census data. While this creates an index similar to the ADI, its index has not been validated.
In contrast, the ADI is a quantitatively defined combination of 17 measures of SES that is regularly updated when new data become available, has been validated for various health outcomes, and does not rely on individual patient-reported surveys, thereby minimizing recall bias.15-16,40 In addition, the public can easily obtain the ADI at no cost through the Neighborhood Atlas. 40 Therefore, the ADI may characterize aspects of a patient's environment and SES that have not been previously considered in orthopaedic sports medicine. In recent years, multiple orthopaedic studies assessing ADI have been published. In 2018, Okoroafor et al 28 evaluated patients with upper extremity fractures and found that ADI predicts patient-reported outcomes. More recently, Sheth et al 37 found that the ADI is predictive of postoperative function, pain, and opioid use in patients who underwent primary total shoulder arthroplasty. In patients with carpal tunnel syndrome, both Wright et al 42 and Bernstein et al 2 found that the ADI is predictive of physical and mental symptom severity. While the ADI has been less frequently studied in patients with lower extremity injuries, Glogovac et al 10 found that the ADI is predictive of postoperative opioid consumption after arthroscopic knee surgery.
With the rising interest in measures of area deprivation in orthopaedics, Cheng et al 6 recently evaluated how different measures of SES could predict patient-reported outcomes after evaluations of 79,818 orthopaedic patients. They found that the combined use of the national ADI and insurance classification predicted the most variability in age-adjusted patient-reported physical and behavioral health. However, despite the high incidence of ACL injuries, no study has investigated the correlation between ADI and care characteristics for patients with ACL injuries. 34 In our retrospective evaluation of 197 patients who underwent ACLR, we found that patients with a greater national ADI percentile experienced delays in undergoing surgery. This finding is important, as it has previously been reported that patients with longer delays to ACLR sustain cartilage and meniscal injuries at an increased rate, requiring additional concomitant procedures that could affect outcomes and rehabilitation.3,43 Our regression model found that patients experienced a 5.1% greater odds of second ACL injury with each added month between evaluation and surgery. Thus, our results should be taken into consideration when developing future health policy and local interventions to increase awareness and access to specialized orthopaedic care for communities with high levels of area deprivation.
Compared with the cohort of patients who did not experience a second ACL injury, we found that the cohort of patients who did experience a second ACL injury had a greater mean national ADI percentile and a greater proportion of patients with Medicaid. While our study did not directly explore factors that could contribute to this difference, it has been previously reported that lower SES leads to decreased access to postoperative physical therapy. A 2018 study by Rogers et al 31 reported that 43% fewer physical therapy clinics accept Medicaid compared with commercial insurance for postoperative ACLR rehabilitation and that patients with Medicaid must wait significantly longer for an initial appointment. In 2022, Chava et al 5 supported these findings by reporting that patients with Medicaid attended fewer physical therapy visits after ACLR than commercially insured patients. While no study has investigated the effect of the ADI on access to physical therapy, it has been previously postulated that communities with lower SES may attend less physical therapy because of a lack of access to transportation and inability to take time off work to attend physical therapy.14,44 Together, these findings may be just as important as access to surgery, as it has been shown that postoperative rehabilitation for patients who had ACLR leads to improved knee function, a greater chance of returning to sport, and a decreased rate of reinjury.5,12,20 Therefore, the lack of access to physical therapy could partially explain our reported higher rate of ACL reinjury among patients with Medicaid and patients with a greater national ADI percentile.
This study had several strengths. Studying ADI as a predictor of access to care for patients with ACL injury is novel, and we are the first study to attempt this. Moreover, our study includes a large population from a health system that is the primary provider of care for patients with Medicaid insurance in Northern Virginia, meaning that our cohort encapsulates a full spectrum of demographic characteristics of our area. Our health system also offers visits on a first-come, first-served basis regardless of insurance classification, which may not be true for every orthopaedic practice. 41 Because the patients in our cohort all received care at our health system, delays in care between patients are not due to an internal triage system that places commercially insured or more affluent patients ahead of those with Medicaid or lower SES. Last, all included patients had at least a 2-year follow-up available in the EMR, which is important given that second ACL injury risk is greatest in the first 2 years after ACLR and functional deficits seem to normalize 2 years after ACLR.1,29-30 Therefore, by excluding patients for whom a 2-year follow-up was unavailable, we can be more confident that our chart review accounted for most of the second ACL injuries among our cohort.
Our study had several limitations that should be considered when interpreting the results. This study was retrospective, and, as a result, the strength of evidence is diminished. As with any retrospective study, recall bias may have affected the recorded date of the initial injury in the EMR. We attempted to mitigate this by using as much data from the EMR as possible, such as emergency department or urgent care visits, primary care visits, or any available outside records. Second, because descriptive data were collected by chart review, SES information besides the ADI was limited. Because an ADI score relies solely on the patient's home address, we did not individually collect information on education, income, or other factors of SES. However, we believe that this is mitigated by how ADI is calculated, which utilizes 17 different measures to more comprehensively describe indicators of SES. Therefore, this calculation takes into consideration the Census-reported values for all individual measures of SES that we would have otherwise collected.16,40 While the ADI has been previously validated in measuring access to health care at the Census block level, we may have also ignored individual outliers. However, because it has been shown that community deprivation has an independent effect on health (eg, poor patients in wealthy neighborhoods may be healthier than poor people in disadvantaged neighborhoods), we do not believe patient outliers had a major effect on our analysis.13,23 Last, it is possible that patients who sustained a reinjury received care at another institution, limiting the ability to predict a precise reinjury rate. The effect of this limitation is somewhat mitigated by the nature of our EMR: our institution has access to the records of nearly all external hospitals, urgent cares, and orthopaedic providers in the Northern Virginia area; thus, we are confident that the likelihood of a patient receiving care outside our network is low. In addition, our institution is 1 of the only orthopaedic groups in Northern Virginia that accepts Medicaid insurance. However, patients with commercial insurance have considerable treatment options around the area, which may have affected the reported reinjury rate of this group.
Conclusion
Lower SES is associated with adverse timing of care after ACL injury and second injury rates after ACLR. Patients with a greater national ADI percentile took significantly longer to obtain surgery after ACL injury. Those who sustained a second ACL injury after ACLR had an overall higher mean national ADI percentile and included a greater proportion of patients with Medicaid compared with those who did not sustain a second ACL injury. To reach equity in orthopaedic care, future studies should critically investigate patient outcomes in the context of area deprivation and insurance classification, as well as what underlying factors may lead these patients to experience more delays and worse outcomes.
Footnotes
Final revision submitted August 22, 2023; accepted October 5, 2023.
Presented at the annual meeting of the AOSSM, Washington, DC, July 2023
The authors declared that they have the following conflicts of interest: A.J.C. has received education payments from Arthrex, Medwest Associates, Mid-Atlantic Surgical Systems LLC, Smith+Nephew, and Supreme Orthopedic Systems LLC; hospitality payments from Stryker; and a grant from Arthrex. B.M.B. has received education payments from Conetic Solutions, Arthrex, Smith+Nephew, and Medwest Associates; hospitality payments from Stryker, Smith+Nephew, Conetic Solutions, and Medical Device Business Services; honoraria from Encore Medical LP; and a grant from Arthrex. C.M.C. has received education payments from Liberty Surgical and hospitality payments from Medical Device Business Services. E.S.C. has received consulting fees from Avanos Medical; education payments from Arthrex and Supreme Orthopedic Systems LLC; and hospitality payments from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Western Institutional Review Board-Copernicus Group (ref No. 20216925).
References
- 1. Abrams GD, Harris JD, Gupta AK, et al. Functional performance testing after anterior cruciate ligament reconstruction: a systematic review. Orthop J Sports Med. 2014;2(1):2325967113518305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bernstein DN, Kurucan E, Fear K, Hammert WC. Evaluating the impact of patient social deprivation on the level of symptom severity at carpal tunnel syndrome presentation. Hand (N Y). 2022;17(2):339-345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Brambilla L, Pulici L, Carimati G, et al. Prevalence of associated lesions in anterior cruciate ligament reconstruction: correlation with surgical timing and with patient age, sex, and body mass index. Am J Sports Med. 2015;43(12):2966-2973. [DOI] [PubMed] [Google Scholar]
- 4. Buller LT, Best MJ, Baraga MG, Kaplan LD. Trends in anterior cruciate ligament reconstruction in the United States. Orthop J Sports Med. 2014;3(1):2325967114563664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chava NS, Fortier LM, Verma N, et al. Patients with Medicaid insurance undergoing anterior cruciate ligament reconstruction have lower postoperative International Knee Documentation Committee scores and are less likely to return to sport than privately insured patients. Arthrosc Sports Med Rehabil. 2022;4(4):e1457-e1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cheng AL, McDuffie JV, Schuelke MJ, Calfee RP, Prather H, Colditz GA. How should we measure social deprivation in orthopaedic patients? Clin Orthop Relat Res. 2022;480(2):325-339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Collins JE, Katz JN, Donnell-Fink LA, Martin SD, Losina E. Cumulative incidence of ACL reconstruction after ACL injury in adults: role of age, sex, and race. Am J Sports Med. 2013;41(3):544-549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dodwell ER, Lamont LE, Green DW, Pan TJ, Marx RG, Lyman S. 20 years of pediatric anterior cruciate ligament reconstruction in New York State. Am J Sports Med. 2014;42(3):675-680. [DOI] [PubMed] [Google Scholar]
- 9. Feng JE, Roof MA, Adnan M, et al. Do patient point of entry and Medicaid status affect quality outcomes following total knee arthroplasty? J Arthroplasty. 2020;35(7):1761-1765. [DOI] [PubMed] [Google Scholar]
- 10. Glogovac G, Kennedy M, Parman MD, Bowers KA, Colosimo AJ, Grawe BM. Opioid requirement following arthroscopic knee surgery: are there predictive factors associated with long-term use. J Knee Surg. 2021;34(8):810-815. [DOI] [PubMed] [Google Scholar]
- 11. Halawi MJ, Cote MP, Savoy L, Williams VJ, Lieberman JR. The effect of payer type on patient-reported outcomes in total joint arthroplasty is modulated by baseline patient characteristics. J Arthroplasty. 2019;34(6):1072-1075. [DOI] [PubMed] [Google Scholar]
- 12. Han F, Banerjee A, Shen L, Krishna L. Increased compliance with supervised rehabilitation improves functional outcome and return to sport after anterior cruciate ligament reconstruction in recreational athletes. Orthop J Sports Med. 2015;3(12):2325967115620770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hu J, Kind AJH, Nerenz D. Area deprivation index predicts readmission risk at an urban teaching hospital. Am J Med Qual. 2018;33(5):493-501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jones MH, Reinke EK, Zajichek A, et al. Neighborhood socioeconomic status affects patient-reported outcome 2 years after ACL reconstruction. Orthop J Sports Med. 2019;7(6):2325967119851073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kind AJ, Jencks S, Brock J, et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Ann Intern Med. 2014;161(11):765-774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible—the neighborhood atlas. N Engl J Med. 2018;378(26):2456-2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Labrum JT IV, Paziuk T, Rihn TC, et al. Does Medicaid insurance confer adequate access to adult orthopaedic care in the era of the patient protection and Affordable Care Act? Clin Orthop Relat Res. 2017;475(6):1527-1536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lakomkin N, Hutzler L, Bosco JA, III. The relationship between Medicaid coverage and outcomes following total knee arthroplasty: a systematic review. JBJS Rev. 2020;8(4):e0085. [DOI] [PubMed] [Google Scholar]
- 19. Lansdown DA, Ma GC, Aung MS, et al. Do patient outcomes and follow-up completion rates after shoulder arthroplasty differ based on insurance payor? J Shoulder Elbow Surg. 2021;30(1):65-71. [DOI] [PubMed] [Google Scholar]
- 20. Law MA, Ko YA, Miller AL, et al. Age, rehabilitation and surgery characteristics are re-injury risk factors for adolescents following anterior cruciate ligament reconstruction. Phys Ther Sport. 2021;49:196-203. [DOI] [PubMed] [Google Scholar]
- 21. Lawrence JT, Argawal N, Ganley TJ. Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: is there harm in delay of treatment? Am J Sports Med. 2011;39(12):2582-2587. [DOI] [PubMed] [Google Scholar]
- 22. Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995;Spec No:80-94. [PubMed] [Google Scholar]
- 23. Ludwig J, Sanbonmatsu L, Gennetian L, et al. Neighborhoods, obesity, and diabetes—a randomized social experiment. N Engl J Med. 2011;365(16):1509-1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Medford-Davis LN, Lin F, Greenstein A, Rhodes KV. "I broke my ankle": access to orthopedic follow-up care by insurance status. Acad Emerg Med. 2017;24(1):98-105. [DOI] [PubMed] [Google Scholar]
- 25. Newman JT, Carry PM, Terhune EB, et al. Delay to reconstruction of the adolescent anterior cruciate ligament: the socioeconomic impact on treatment. Orthop J Sports Med. 2014;2(8):2325967114548176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nguyen J, Anandasivam NS, Cooperman D, Pelker R, Wiznia DH. Does Medicaid insurance provide sufficient access to pediatric orthopedic care under the Affordable Care Act? Glob Pediatr Health. 2019;6:2333794X19831299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Nordenvall R, Marcano AI, Adami J, et al. The effect of socioeconomic status on the choice of treatment for patients with cruciate ligament injuries in the knee: a population-based cohort study. Am J Sports Med. 2017;45(3):535-540. [DOI] [PubMed] [Google Scholar]
- 28. Okoroafor UC, Gerull W, Wright M, Guattery J, Sandvall B, Calfee RP. The impact of social deprivation on pediatric PROMIS health scores after upper extremity fracture. J Hand Surg Am. 2018;43(10):897-902. [DOI] [PubMed] [Google Scholar]
- 29. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med. 2012;22(2):116-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42(7):1567-1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rogers MJ, Penvose I, Curry EJ, DeGiacomo A, Li X. Medicaid health insurance status limits patient accessibility to rehabilitation services following ACL reconstruction surgery. Orthop J Sports Med. 2018;6(4):2325967118763353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Roof MA, Feng JE, Anoushiravani AA, et al. The effect of patient point of entry and Medicaid status on quality outcomes following total hip arthroplasty. Bone Joint J. 2020;102-B(7)(suppl B):78-84. [DOI] [PubMed] [Google Scholar]
- 33. Sabesan VJ, Petersen-Fitts G, Lombardo D, Briggs D, Whaley J. Medicaid payer status is linked to increased rates of complications after treatment of proximal humerus fractures. J Shoulder Elbow Surg. 2017;26(6):948-953. [DOI] [PubMed] [Google Scholar]
- 34. Sanders TL, Maradit Kremers H, Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med. 2016;44(6):1502-1507. [DOI] [PubMed] [Google Scholar]
- 35. Segal DN, Grabel ZJ, Shi WJ, Gottschalk MB, Boden SD. The impact of insurance coverage on access to orthopedic spine care. J Spine Surg. 2018;4(2):260-263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Shau D, Shenvi N, Easley K, Smith M, Bradbury T, Guild G, III. Medicaid payer status is associated with increased 90-day morbidity and resource utilization following primary total hip arthroplasty: a propensity-score-matched analysis. J Bone Joint Surg Am. 2018;100(23):2041-2049. [DOI] [PubMed] [Google Scholar]
- 37. Sheth MM, Morris BJ, Laughlin MS, Elkousy HA, Edwards TB. Lower socioeconomic status is associated with worse preoperative function, pain, and increased opioid use in patients with primary glenohumeral osteoarthritis. J Am Acad Orthop Surg. 2020;28(7):287-292. [DOI] [PubMed] [Google Scholar]
- 38. Singh GK. Area deprivation and widening inequalities in US mortality, 1969-1998. Am J Public Health. 2003;93(7):1137-1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Strotman P, Perry M, LeDuc R, Joyce C, Garbis N. Effect of insurance status on clinical outcomes after shoulder arthroplasty. Orthopedics. 2020;43(6):e523-e528. [DOI] [PubMed] [Google Scholar]
- 40. University of Wisconsin School of Medicine Public Health. 2019 Area Deprivation Index v3.1. Accessed July 1, 2022. https://www.neighborhoodatlas.medicine.wisc.edu/
- 41. Williams AA, Mancini NS, Solomito MJ, Nissen CW, Milewski MD. Chondral injuries and irreparable meniscal tears among adolescents with anterior cruciate ligament or meniscal tears are more common in patients with public insurance. Am J Sports Med. 2017;45(9):2111-2115. [DOI] [PubMed] [Google Scholar]
- 42. Wright MA, Adelani M, Dy C, O’Keefe R, Calfee RP. What is the impact of social deprivation on physical and mental health in orthopaedic patients? Clin Orthop Relat Res. 2019;477(8):1825-1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Zoller SD, Toy KA, Wang P, Ebramzadeh E, Bowen RE. Temporal relation of meniscal tear incidence, severity, and outcome scores in adolescents undergoing anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):215-221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Ziedas A, Abed V, Swantek A, et al. Social determinants of health influence access to care and outcomes in patients undergoing anterior cruciate ligament reconstruction: a systematic review. Arthroscopy. 2022;38(2):583-594.e4. [DOI] [PubMed] [Google Scholar]


