Abstract
Objectives
Gestational diabetes mellitus (GDM) is a common pregnancy complication with adverse fetal and maternal outcomes. Currently, there are only a few validated tools available that address knowledge in GDM. Recognition of the inconsistencies will provide an effective learning program to achieve optimal results. This study aimed at validating the “Gestational Diabetes Mellitus Knowledge Questionnaire” (GDMKQ).
Methodology
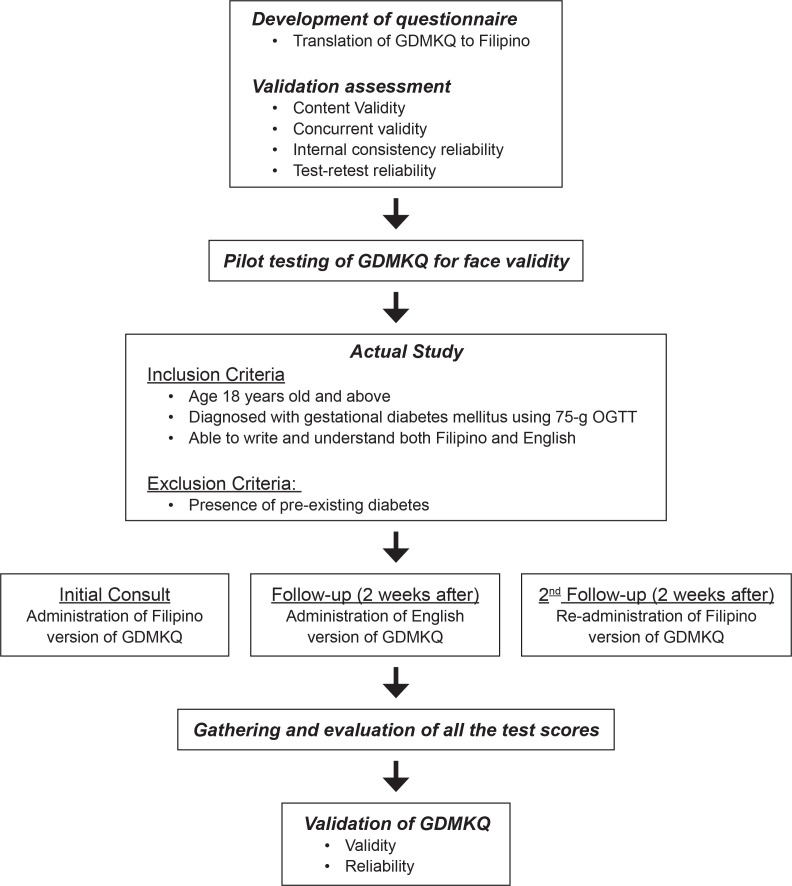
A cross-sectional validation study on GDMKQ among 51 GDM patients aged at least 18 years was conducted in the outpatient clinics of a tertiary hospital. Excluded were those with pre-existing diabetes. The questionnaire was submitted for peer review for translation to Filipino and back-translation. Concurrent validity, internal consistency and test-retest reliability of the questionnaire were undertaken as part of the validation process. Descriptive analysis was used for data elaboration by using SPSS v23.
Results
The Filipino version of GDMKQ demonstrated sensible content and face validity. As measured, respondents obtained higher total and domain scores with better knowledge levels of GDM compared to its English version. Overall adequate knowledge was observed among those married and college subgroups as compared to single women and those with secondary levels of education. The reliability of the questionnaire was calculated at 0.632 using the Kuder-Richardson 20. The test-retest scores using the Filipino-translated questionnaire have a Pearson correlation coefficient of 0.853 with moderate to good level of agreement with each other, and Cohen’s kappa of 0.564 with an intra-class correlation coefficient of 0.828.
Conclusion
The Filipino-translated version of GDMKQ is a valid screening tool that assesses a patient’s knowledge on gestational diabetes. Identifying the level of their understanding will enable clinicians to develop an individualized, effective learning program to improve pregnancy outcomes.
Keywords: gestational diabetes, knowledge, questionnaire, validation
INTRODUCTION
Pregnancy is associated with hyperinsulinemia and insulin resistance which may cause some patients to develop diabetes mellitus (DM).1 DM is responsible for 2 to 5% of pregnancy complications, and 90% of these cases are caused by gestational diabetes mellitus (GDM).2,3 According to the International Association of Diabetes and Pregnancy Study Groups (IADPSG), GDM is defined as any degree of glucose or carbohydrate intolerance that is first diagnosed during pregnancy.1-6 It occurs in 0.6 to 20% of the pregnant population worldwide.1,5 The prevalence differs across geographical settings but was found to be highest among Asians. In the Philippines, it affects 14% of pregnancies as reported by the Asian Federation of Endocrine Societies Study Group on Diabetes in Pregnancy (ASGODIP).7 Predisposing factors include ethnicity (Asian, African, Hispanic, Native American and Pacific Island descent), overweight pre-pregnant body mass index (BMI), age of mother (more than 25 to 35 years old), family history of DM or previous history of GDM, sleep disturbance and socioeconomic status.5-9 If left untreated, gestational diabetes may result in several maternal and fetal adverse outcomes.2,6,9,10 Maternal adverse outcomes include preeclampsia, cesarean section, prolonged labor pain and miscarriages.4,6-9 Whereas neonatal adverse outcomes include fetal macrosomia, neonatal metabolic disturbances (hypoglycemia), respiratory disorders, decreased 5-minute APGAR scores, neonatal intensive care unit (NICU) admission, impaired neurodevelopmental outcomes, autism spectrum disorder, polycythemia, hypocalcemia, jaundice, stillbirth and neonatal death.2,4,6-11 These myriad of events was also reported in our local data by Malong et al., and Urbanozo et al.12, 13 Other possible long-term adverse effects include obesity, metabolic syndrome, and diabetes of the child and the mother.2,4,8-11 In fact, mothers with GDM are noted to have a seven-fold increase in developing type 2 diabetes.10 In a tertiary hospital in Manila, the incidence of postpartum prediabetes and diabetes was 34.7% and 7.3%, respectively.12
With proper management of GDM, the risk of both maternal and fetal complications decreases and possibly improves health-related quality of life.2,4,8,9 However, in some cases, there are no reduced risks, despite adequate medical treatment. This could be attributed to the need for a multidisciplinary approach in the management of GDM, which includes patient education on disease pathophysiology, compliance to medical treatment, disease monitoring to maintain normal glycemic levels and lifestyle modification that includes medical nutrition therapy, and physical activity.2,4,9 Management of GDM is a labor-intensive discipline that poses several challenges to maintaining the highest quality of patient care.4 But several impediments to the management of GDM exist such as the patient’s low socioeconomic condition, inadequate knowledge, misbeliefs, myths, and social discrimination.9 In a cross-sectional study done in Luzon, a higher level of education was a significant factor in the degree of selfefficacy and confidence to perform self-care (p = 0.023). In that same study, it also appeared that those who avail of free clinical services have better self-management practices (p <0.001).14
Health literacy is the measure of the patient’s ability to read, understand and follow medical instructions.2 Knowledge is one of the most vital components of health literacy. Insufficient health literacy is associated with poor knowledge about the disease, which would lead to poor adherence to management strategies.9 According to studies, health literacy is of great importance in the management of complex chronic medical diseases, such as type 2 DM and human immunodeficiency virus (HIV) infection.2 Individuals who do not know about their disease are less likely to comply with their treatment regimens as they do not understand its significance.2,3,9 Appropriate knowledge about the disease accompanied with positive attitude and behavior, can help prevent complications of the disease through proper multidisciplinary management.3,6 To prevent DM in two successive generations, patients with GDM will require thorough education that focuses on immediate care and their long-term health implications.3,9 Patient education should be composed of information regarding normal and abnormal glycemic values, food restrictions, dietary values and the importance of exercise.8 Hence, healthcare professionals must develop strategies to influence positive behavioral changes in these patients for them to adhere to proper exercise, diet and blood glucose monitoring.6 It is therefore necessary to develop an efficient tool to reliably assess the diabetes knowledge of patients.3
Gestational Diabetes Mellitus Knowledge Questionnaire (GDMKQ) is a 15-item multiple-choice questionnaire that explores on the basic knowledge of GDM, risk factors, food and diet values, treatment options and management and complications or outcomes. This was developed by Hussain and colleagues in 2014 and was validated in Malaysia for knowledge assessment among pregnant patients with diabetes. Each item has 4 options with 1 correct answer. Each correct answer corresponds to 1 point. The score ranges from a maximum of 15 to a minimum of 0. Inadequate knowledge is indicated by a score ≤8 while a score >8 imparts adequate knowledge about GDM.6,8
In an extensive review of the literature and based on the researcher’s knowledge, no local study has measured the patients’ level of understanding of gestational diabetes. Identification of the domains which need improvement will help clinicians implement an effective learning program for use by pregnant women to improve health literacy and pregnancy outcomes.
This study aims to validate the Filipino-translated version of the Gestational Diabetes Mellitus Knowledge Questionnaire (GDMKQ) in evaluating the understanding of pregnant patients regarding gestational diabetes mellitus.
METHODOLOGY
Study design
This is a cross-sectional validation study conducted for a period of 2 months from January to February 2022 at the outpatient setting of Chinese General Hospital and Medical Center (CGHMC), Blumentritt, Manila.
Study population
A sample size of 45 participants was required in this study to have a ratio of 3 participants: 1 question item using the Andrew Fisher’s formula with confidence level set at 95%. A total of 51 consecutive pregnant women were selected and enrolled in the study. Inclusion criteria were patients at least 18 years of age and with a clinical diagnosis of gestational diabetes mellitus (GDM) based on 75g OGTT with one or more of the following values: fasting plasma glucose ≥92 mg/dL (5.1 mmol/L), 1-hour plasma glucose ≥ 180 mg/dL (10 mmol/L), 2-hour plasma glucose ≥153 mg/dL (8.5 mmol/L). Participants must be able to read and understand both Filipino and English at a basic level. Those with pre-existing diabetes were excluded. All were assigned alphanumeric codes to hide their identity. Age, civil status, age of gestation, educational attainment, socioeconomic status, comorbidities, obstetric scores (gravidity and parity) and the date of initial diagnosis of GDM were documented in the data information sheet to ensure avoidance of missing data. Their contact numbers were collected to minimize loss to follow-up and address transfer bias.
This study protocol received approval from the Institutional Research and Ethics Review Board. Informed consent was obtained from each of the participants who agreed to be enrolled in the study.
Outcome measured
The primary outcome is the distribution of correct answers to each question, including the total and domain scores, while the secondary endpoint is the adequacy of knowledge of GDM.
Data collection and validation process
The Gestational Diabetes Mellitus Knowledge Questionnaire (GDMKQ) by Hussain et al. was used in this study. This was submitted to 4 healthcare professionals (2 Endocrinologists and 2 Obstetricians) who were all experts in GDM and fluent in both English and Filipino. One from each subspecialty performed the forward translation. The original version was not shown to the remaining medical experts who performed the backward translation to ensure an unbiased result. All of them gave their expert opinion on the comprehensibility of the questionnaire to improve its applicability. Clarifications of uncertainties were emailed to the principal investigator. The changes were collated and the revised questionnaire was sent back to the medical experts until a consensus was reached. The four medical experts evaluated the final forward-translated questionnaire. Following their recommendation, amendments were made to ensure its appropriateness for the target population.
Thirteen patients were then randomly selected for preliminary testing to ensure the readability and understandability of GDMKQ. This number was based on the article of Moore et al., wherein at least 12 participants are recommended for pilot studies.15 Validation of the questionnaire involves validity measures such as content validity and concurrent validity and reliability measures like internal consistency and test-retest reliability. Content validity refers to the degree to which the questions adequately cover all the required content.16 The translated questionnaire was pilot-tested on 13 actual patients with GDM for face validity. None reported any confusion about any of the items; hence, no further revisions were made.
Fifty-one eligible subjects seen in the out-patient clinics of Chinese General Hospital and Medical Center were given the self-administered GDMKQ questionnaire, in both Filipino and English translations, with a two-week interval in between. Concurrent validity and other reliability measures were then initiated.
Internal consistency is a measure of how reliable the items within a questionnaire are based on the intended construct. Statistically, this is computed by Cronbach’s alpha and a value of at least 0.7 is considered statistically reliable. To ensure the reliability of answers, the Kuder-Richardson formula 20 (KR-20), which is based on the consistency of all responses to all items in the test, was used. Test-retest, which is statistically analyzed by Pearson’s productmoment correlation coefficient r was performed. This gauges the consistency of a questionnaire by administering the same test over some time.16 This was conducted by re-administering the GDMKQ Filipino version a month after the initial Filipino version over the same group of individuals. The average duration of completing each questionnaire was 5-8 minutes and those who completed all three questionnaires were included in the analysis.
Statistical analysis
SPSS v23 (IBM, Chicago, Illinois) was used in data analysis. Data were presented as mean ± standard deviation (SD) for continuous data following a normal distribution, as median (range) for discrete and highly skewed continuous data and as count (percent) for categorical data. Kolmogorov-Smirnov test for normality was used to determine the normal distribution of the variables. Age was noted to be normally distributed, while income and gestational age were skewed data. No missing data on patient characteristics were noted. The difference between the scores of the English version and the Filipino version of the questionnaire was determined using the student t-test. Independent t-test, Kuder-Richardson 20 (KR-20) and Pearson’s product-moment correlation coefficient r were used to assess the validity and reliability of the questionnaire. P ≤0.05 were considered statistically significant (Figure 1).
Figure 1.
Overall recruitment flow.
RESULTS
A total of 51 respondents were included and the demographic characteristics are summarized in Table 1. The mean age was 31.49 ± 6.445 years. The majority were married (60.8%) and college graduates (72.5%), with income classification ranging from poor to low middle-class income. The median gestational age was 27 weeks and most were multigravid (72.5%) and multiparous (37.3%). Some reported concomitant comorbidities including hypertension (4), dyslipidemia (2), hyperthyroidism (1) and bronchial asthma (1).
Table 1.
Baseline demographic characteristics of the GDM patients enrolled
| Demographic data | n = 51 |
|---|---|
| Age, in years (mean ± SD) | 31.49 ± 6.445 |
| Civil status, n (%) Single Married |
20 (39.2%) 31 (60.8%) |
| Level of education, n (%) Secondary / High School Tertiary / College |
14 (27.5%) 37 (72.5%) |
| Gravidity, n (%) Primigravida Multigravida |
14 (27.5%) 37 (72.5%) |
| Parity (median, range) n (%) Nullipara Primipara Multipara |
14 (27.5%) (35.3%) (37.3%) |
| Gestational age, in weeks (median, range) | 27 (18-38) |
| Monthly income (median, range) | ₱13,000 (₱5,000- ₱35,000) |
| GDM management n (%) Diet-controlled On oral hypoglycemic agent On insulin |
27 (53%) 11 (21.6%) 13 (25.4%) |
| Comorbidities n (%) Hypertension Dyslipidemia Hyperthyroidism Bronchial asthma |
4 (0.08%) 2 (0.04%) 1 (0.02%) 1 (0.02%) |
Table 2 shows the distribution of correct answers in the English and Filipino versions of GDMKQ. Comparing the two questionnaires, correct answers were noted to be higher in the Filipino version, as well as the total scores and domain scores. The majority of the respondents have adequate knowledge of GDM in both versions of the questionnaire (English and Filipino, 82.4 and 86.3%, respectively) with a higher proportion in the Filipino version but not significantly different. Although there was an increase in the proportion with adequate knowledge, majority still had low knowledge on item 5 even after the re-test. In decreasing order, the scores among the five domains of the GDMKQ (both English and Filipino versions) are as follows: Knowledge about diet/food values > Basic knowledge of GDM > Knowledge about GDM complications > Knowledge about risk factors > Knowledge about GDM management.
Table 2.
Distribution of correct answers among the English version and initial versus follow-up Filipino version in the GDMKQ questionnaire (n=51)
| Domains/ Questions | English version Correct, n (%) | Initial Filipino version Correct, n (%) | Follow-up Filipino version Correct, n (%) |
|---|---|---|---|
|
Basic knowledge about GDM
Q1. Gestational Diabetes Mellitus is the type of diabetes that occur: *Correct: During pregnancy Q2. In uncontrolled Gestational Diabetes Mellitus, the blood sugar level is: *Correct: Increased Q3. What is the best way for testing blood glucose level for Gestational Diabetes Mellitus patients? *Correct: Blood test |
42 (82.4) 43 (84.3) 40 (78.4) |
40 (78.4) 49 (96.1) 41(80.4) |
41 (80.4) 49 (96.1) 42 (82.4) |
|
Knowledge about risk factors
Q4. You are at increased risk of developing Gestational Diabetes Mellitus if you are: *Correct: Overweight Q5. You have increased chances of developing Gestational Diabetes Mellitus if: *Correct: previously gave birth to a stillborn baby Q6. You are more likely to develop Gestational Diabetes Mellitus if you have: *Correct: Family history of diabetes |
39 (76.5) 4 (7.8) 41 (80.4) |
42 (82.4) 3 (5.9) 40 (78.4) |
41 (80.4) 6 (11.8) 43 (84.3) |
|
Knowledge about diet/food values
Q7. If you have Gestational Diabetes Mellitus, you should avoid food containing high content of: *Correct: carbohydrates and fats Q8. Which of the following food can be eaten without restriction during Gestational Diabetes Mellitus: *Correct: Fresh salad Q9. What is the type of nutritional source mainly provided by rice? *Correct: carbohydrates |
47 (92.2) 46 (90.2) 48 (94.1) |
43 (84.3) 46 (90.2) 49 (96.1) |
47 (92.2) 45 (88.2) 49 (96.1) |
|
Knowledge about the management of GDM
Q10. The most common sign of hyperglycemia (high blood sugar) is: *Correct: increased thirst |
23 (45.1) | 28 (54.9) | 33 (64.7) |
| Q11.The normal value of fasting blood sugar (FBS) is: *Correct: 3.6 – 6.1 mmol/l (64.8 - 109.8 mg/dL) | 30 (58.8) | 25 (49) | 29 (56.9) |
| Q12.If you feel the onset of hypoglycemic (low blood sugar) symptoms, you should: *Correct: Immediately eat or drink something sweet | 23 (45.1) | 27 (52.9) | 30 (58.8) |
|
Knowledge about GDM complications
Q13. In uncontrolled Gestational Diabetes Mellitus, your baby may be: *Correct: Larger than usual size Q14. If you have Gestational Diabetes Mellitus you have: *Increased chances of developing diabetes in later life Q15. Gestational Diabetes Mellitus is a condition that: *Correct: May affect mother or baby |
34 (66.7) 39 (76.5) 48 (94.1) |
37 (72.5) 37 (72.5) 49 (96.1) |
35 (68.6) 41 (80.4) 51 (100) |
| Total score: | 551 | 553 | 577 |
| Average score: | 10.80 | 10.84 | 11.31 |
Concerning civil status and educational attainment, an overall adequate knowledge of GDM was documented across all subgroups for both versions of GDMKQ.
However, the total scores were higher in the married and college populations. The adequacy of their knowledge was higher in the Filipino version (52.9%, 66.7%) versus the English version (42%, 62.7%); meanwhile, the single and high school subgroup did not show a change. Between the two versions, those married and high school graduates scored higher in the Filipino version while the single and college graduates did better in English but were not significantly different. Better test scores were documented among college graduates than high school graduates in the English survey (11.24 ± 1.877 vs. 9.64 ± 2.951, p = 0.025) and Filipino retest survey (11.81 ± 1.664 vs. 10.07 ± 2.303, p = 0.04) while no significant difference was seen between different civil status. (Table 3)
Table 3.
Percentages of correct and incorrect scores for questions in each domain of the GDMKQ (n=51)
| GDMKQ | English version |
Initial Filipino version |
Follow-up Filipino version |
|||
|---|---|---|---|---|---|---|
| Correct, n (%) | Incorrect, n (%) | Correct, n (%) | Incorrect, n (%) | Correct, n (%) | Incorrect, n (%) | |
| Domain 1: Basic knowledge of GDM | ||||||
| Q1 | 42 (82.4%) | 9 (17.6%) | 40 (78.4%) | 11 (21.6%) | 41 (80.4%) | 10 (19.6%) |
| Q2 | 43 (84.3%) | 8 (15.7%) | 49 (96.1%) | 2 (3.9%) | 49 (96.1%) | 2 (3.9%) |
| Q3 | 40 (78.4%) | 11 (21.6%) | 41 (80.4%) | 10 (19.6%) | 42 (82.4%) | 9 (17.6%) |
| Average score: | 41.67 | 43.3 | 44 | |||
|
| ||||||
| Domain 2: Risk factors | ||||||
| Q4 | 39 (76.4%) | 12 (23.5%) | 42 (82.4%) | 9 (17.6%) | 41 (80.4%) | 10 (19.6%) |
| Q5 | 4 (7.8%) | 47 (92.2%) | 3 (5.9%) | 48 (94.1%) | 6 (11.8%) | 45 (88.2%) |
| Q6 | 41 (80.4%) | 10 (19.6%) | 40 (78.4%) | 11 (21.6%) | 43 (84.3%) | 8 (15.7%) |
| Average score: | 28 | 28.3 | 30 | |||
|
| ||||||
| Domain 3: Food and diet values | ||||||
| Q7 | 47 (92.2%) | 4 (7.8%) | 43 (84.3%) | 8 (15.7%) | 47 (92.2%) | 4 (7.8%) |
| Q8 | 46 (90.2%) | 5 (9.8%) | 46 (90.2%) | 5 (9.8%) | 45 (88.2%) | 6 (11.8%) |
| Q9 | 48 (94.1%) | 3 (5.9%) | 49 (96.1%) | 2 (3.9%) | 49 (96.1%) | 2 (3.9%) |
| Average score: | 47 | 46 | 47 | |||
|
| ||||||
| Domain 4: Treatment options and management | ||||||
| Q10 | 23 (45.1%) | 28 (54.9%) | 28 (54.9%) | 23 (45.1%) | 33 (64.7%) | 18 (35.3%) |
| Q11 | 30 (58.8%) | 21 (41.2%) | 25 (49%) | 26 (51%) | 29 (56.9%) | 22 (43.1%) |
| Q12 | 23 (45.1%) | 28 (54.9%) | 27 (52.9%) | 24(47.1%) | 30 (58.8%) | 21 (41.2%) |
| Average score: | 25.3 | 26.67 | 30.67 | |||
|
| ||||||
| Domain 5: Complications or outcomes | ||||||
| Q13 | 34 (66.7%) | 17 (33.3%) | 37 (72.5%) | 14 (27.5%) | 35 (68.6%) | 16 (31.4%) |
| Q14 | 39 (76.5%) | 12 (23.5%) | 37 (72.5%) | 14 (27.5%) | 41 (80.4%) | 10 (19.6%) |
| Q15 | 48 (94.1%) | 3 (5.9%) | 49 (96.1%) | 2 (3.9%) | 51 (100%) | 0 (0%) |
| Average score: | 40.3 | 41 | 42.3 | |||
|
| ||||||
| Knowledge Score, median | 11 [IQR: 10-12] | 11 [IQR: 10-12] | 11 [IQR: 10-13] | |||
| Adequate, n (%) | 42 (82.4%) | 44 (86.3%) | 44 (86.3%) | |||
| Inadequate, n (%) | 9 (17.6%) | 7 (13.7%) | 7 (13.7%) | |||
The test-retest scores using the Filipino-translated questionnaire have a Pearson Correlation coefficient of 0.853 which showed a good positive correlation between the two scores (p<0.001). The Cohen’s kappa was 0.564, while the intraclass correlation coefficient was 0.828, which means that there is a moderate to good level of agreement between the test scores. For reliability, the questionnaire yielded a KR-20 value of 0.632, which ranked strong (0.61 – 0.80), as shown in Table 4.
Table 4.
Comparison of total scores according to civil status and educational attainment
| n | Filipino version |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| English version |
Initial |
Follow-up |
||||||||
| Knowledge scores | Comparison of test scores | Betweengroup P | Knowledge scores | Comparison of test scores | Betweengroup P | Knowledge scores | Comparison of test scores | Betweengroup P | ||
| Civil status | ||||||||||
| Single | 20 | 214 | 10.70 ± 1.949 | 0.799 | 213 | 10.65 ± 2.084 | 0.585 | 224 | 11.20 ± 2.118 | 0.706 |
| Adequate, n (%) | 17(33.3%) | 17 (33.3%) | 17 (33.3%) | |||||||
| Inadequate, n (%) | 3 (5.9%) | 3 (5.9%) | 3 (5.9%) | |||||||
| Married | 31 | 337 | 10.87 ± 2.54 | 340 | 10.97 ± 1.975 | 354 | 11.42 ± 1.945 | |||
| Adequate, n (%) | 25 (49%) | 27 (52.9%) | 28 (54.9%) | |||||||
| Inadequate, n (%) | 6 (11.8%) | 4 (7.8%) | 3 (5.9%) | |||||||
|
| ||||||||||
| Educational attainment | ||||||||||
| High school | 14 | 135 | 9.64 ± 2.951 | 0.025* | 140 | 10 ± 2.353 | 0.064 | 141 | 10.07 ± 2.303 | 0.004* |
| Adequate, n (%) | 10 (19.6%) | 10 (19.6%) | 9 (17.6%) | |||||||
| Inadequate, n (%) | 4 (7.8%) | 4 (7.8%) | 5 (9.8%) | |||||||
| College | 37 | 416 | 11.24 ± 1.877 | 413 | 11.16 ± 1.788 | 437 | 11.81 ± 1.664 | |||
| Adequate, n (%) | 32 (62.7%) | 34 (66.7%) | 36 (70.6%) | |||||||
| Inadequate, n (%) | 5 (9.8%) | 3 (5.9%) | 1 (2%) | |||||||
aWilcoxon signed-rank test was used; bindependent t-test was used; One Way ANOVA
DISCUSSION
This is the first Filipino-validated study of GDMKQ. Worldwide, the prevalence of gestational diabetes complicating pregnancy approaches 20%.5 Based on literature searches, not much attention has been given to the assessment of understanding of this condition, as compared to type 1 and type 2 diabetes. In the study of Malong et al., the incidence of diabetes and prediabetes postpartum was 7.3% and 34.7% respectively; hence, the importance of vigilance in peripartum care.
The GDMKQ underwent three revisions until a consensus was reached. The medical experts simplified some of the terms to make the questionnaire more comprehensible and relevant. In the original GDMKQ, question 12 reads “If you feel the onset of hypoglycemia (low blood sugar) symptoms, you should” and the options were listed. Since hypoglycemia has several symptoms, one of the panelists deemed that examples of it should be stated. They also suggested placing conventional units aside from the SI units since some patients may be more acquainted with the other unit of measurement. One of them also suggested keeping the term “stillbirth” and place it beside its Filipino translation. All the suggestions of the medical experts were implemented to ensure acceptability across ethnicities. For the pilot testing, thirteen participants were randomly selected. While all participants agreed that the GDMKQ was easy to understand, majority incorrectly answered question 5 and claimed that it was the first time they learned that a previous “stillbirth” was a risk factor for developing GDM.
The study showed that the majority (86.3%) had adequate knowledge of GDM as demonstrated by the number of correct answers and total scores. This was exhibited across all subgroups regardless of civil status and educational attainment but was particularly found among married and college graduates. The significant increase in this proportion is because their number was higher upon enrollment as opposed to their counterparts (31 vs 20; 37 vs 14, respectively) and the good knowledge is likely due to the counseling done by the primary physician during prenatal visits even before their recruitment. The knowledge adequacy of these respondents was higher in the Filipino version of GDMKQ, likely because Filipino is our basic and national language. Those who were single and high school graduates, on the other hand, did not demonstrate change for both versions of GDMKQ and retest of the Filipino version.
Between the two versions, total scores were found to be higher in the English GDMKQ among the single and college graduates while those married and high school graduates fared better in the Filipino version. A possible explanation would be more than half (65%) of those who were single were college graduates and English is the medium of instruction in the academe and universities. However, no significant difference has been found between the English and Filipino versions of GDMKQ (p = 0.834). The scores in both versions were almost the same, which means that the translated version is valid.
In decreasing order, the frequency of correct responses among the five domains of gestational diabetes is as follows: knowledge about diet and food values > basic knowledge about GDM > knowledge about GDM complications > knowledge about risk factors > knowledge about management of GDM. Only limited studies can be used for the comparison of these findings, as there were only three studies examining the validity and reliability of GDM knowledge questionnaires have been found.16 Alayoub et al., Hussain et al., and Ogu et al., developed a questionnaire on knowledge assessment but no one elaborated on the validation process.6,8,17,18 The high literacy on diet and food values documented in this study, along with that of Hussain’s, may be explained by the greater number of patients who were diet-controlled and did not require medications.6,8 On the other hand, the domain with the lowest frequency of correct answers was GDM management. This finding is likely due to the little emphasis on self-management principles and lockdown implementation during the surge of COVID-19 disease which limited the patient’s follow-up consult. As opposed to the finding of Carolan-Olah, this domain garnered the highest response in Australia, where the study was done, which may be due to its economic status as a developed country.16
For the test-retest reliability (Tables 5 and 6), a coefficient of stability of 0.853 was obtained, indicating a very high correlation with a moderate to good level of agreement as reflected by the computed Cohen’s kappa of 0.564 and intra-class correlation coefficient of 0.828. When analyzing the internal consistency of all test items of the GDMKQ, a good internal consistency (KR-20 = 0.632) was identified but was noted to be lower than the findings of Carolan-Olah which reported Cronbach’s alpha coefficient (ɑ = 0.88). Nevertheless, both signify good internal consistency or reliability as KR-20 values of at least 0.6 (Table 6) and Cronbach’s coefficient of at least 0.7 are considered satisfactory.16
Table 5.
Reliability analysis using Kuder Richardson-20 item analysis
| Scale mean if item deleted | Scale variance if item deleted Corrected item - total correlation | Corrected item - total correlation | KR-20 if item deleted | |
|---|---|---|---|---|
| Q1 | 30.45 | 24.093 | 0.061 | 0.637 |
| Q2 | 29.63 | 23.678 | 0.519 | 0.618 |
| Q3 | 31.29 | 24.492 | -0.050 | 0.657 |
| Q4 | 31.27 | 21.563 | 0.259 | 0.615 |
| Q5 | 29.37 | 20.598 | 0.328 | 0.602 |
| Q6 | 31.12 | 20.506 | 0.300 | 0.608 |
| Q7 | 30.53 | 23.774 | 0.098 | 0.634 |
| Q8 | 31.41 | 21.767 | 0.296 | 0.609 |
| Q9 | 30.59 | 23.447 | 0.291 | 0.618 |
| Q10 | 29.98 | 21.140 | 0.389 | 0.594 |
| Q11 | 30.04 | 24.038 | -0.040 | 0.671 |
| Q12 | 29.86 | 20.601 | 0.407 | 0.589 |
| Q13 | 30.96 | 18.118 | 0.490 | 0.563 |
| Q14 | 30.24 | 20.064 | 0.531 | 0.570 |
| Q15 | 30.59 | 23.447 | 0.291 | 0.618 |
Table 6.
Summary of reliability analysis done
| Summary of reliability analysis | ||
|---|---|---|
|
| ||
| Test statistics | Value | Interpretation |
|
| ||
| Cohen’s kappa | 0.564 | Moderate strength of agreement |
| ICC overall | 0.632 | Substantial agreement |
| ICC domain 1 | 0.149 | Slight agreement |
| ICC domain 2 | 0.433 | Moderate agreement |
| ICC domain 3 | 0.079 | Slight agreement |
| ICC domain 4 | 0.505 | Moderate agreement |
| ICC domain 5 | 0.497 | Moderate agreement |
| Kuder Richardson 20 | 0.632 | Moderate correlation, substantial agreement |
|
| ||
| Kuder-Richardson coefficient of reliability rank | ||
|---|---|---|
|
| ||
| Reliability coefficient | Level of reliability | |
|
| ||
| 0.81 or more | Near complete agreement | |
| 0.61 – 0.80 | Strong | |
| 0.41 – 0.60 | Moderate | |
| 0.21 – 0.40 | Fair | |
|
| ||
The retest scores were also found to be significantly higher than the initial test (p = 0.002) which is likely due to patient education that occurred within the period of follow-up. Among the respondents, those with a tertiary level of education aced the questionnaire as shown in Table 3. This is in accordance with the statement of Spoelman that those with higher education levels perform more health searches on the internet or websites and, thus, are likely to achieve a higher score.19
Some limitations recognized by the researchers include the use of Andrew Fisher’s formula in the sample size, lack of quantitative assessment of content validity and self-selection bias. The evaluation of content validity is a subjective process. The majority of women who participated had a tertiary level of education which was also seen in the study of Carolan-Olah.16 According to studies, women with higher levels of education are more likely to participate.19 They have increased access to health-related literature, books and internet sources, hence portending a higher knowledge score.8 Rasch analysis can be used in future assessments to evaluate the different personal qualities such as education of respondents. Secondly, the participants have been recruited within the hospital, hence, they tend to possess better health knowledge and better health-seeking behavior. Lastly, this is only a single-centered trial which may not reflect the overall patient characteristics. Addressing these factors is necessary and a multi-center study is recommended.
CONCLUSION
The Filipino-translated version of GDMKQ is a valuable tool in evaluating the knowledge of women on gestational diabetes. This can be used as a simple screening device in the outpatient setting to recognize the facts and misconceptions of pregnant women about GDM and its management. Therefore, clinicians will be able to develop an individualized, effective learning program that will help mitigate the risks and improve pregnancy outcomes.
Acknowledgments
The authors wish to express their sincere gratitude to the panel of experts who evaluated the questionnaire, Dr. Francis Xavier Mislang, Dr. Maria Guia Estrella Dela Cruz, Dr. Jonie Tan and Dr. Vicar Ong. Gratitude is also extended to the patients who consented to participate and to the consultants of the Section of Endocrinology, Diabetes and Metabolism of the Chinese General Hospital and Medical Center for their continued support for this research.
Funding Statement
Funding Source None.
Statement of Authorship
All authors certified fulfillment of ICMJE authorship criteria.
CRediT Author Statement
HG: Conceptualization, Methodology, Software, Validation, Formal Analysis, Investigation, Resources, Data curation, Writing – original draft preparation, Writing – review and editing, Visualization, Project administration; FRG: Conceptualization, Methodology, Validation, Formal Analysis, Resources, Writing – review and editing, Supervision
Author Disclosure
The authors declared no conflict of interest.
References
- 1.Chung JH, Voss KJ, Caughey AB, Wing DA, Henderson EJD, Major CA. Role of patient education level in predicting macrosomia among women with gestational diabetes mellitus. J Perineonatol. 2006;26(6): 328-32. PMID: 16642026. 10.1038/sj.jp.7211512. [DOI] [PubMed] [Google Scholar]
- 2.Evans E, Patry R. Management of gestational diabetes mellitus and pharmacists’ role in patient education. Am J Health-Syst Pharmacol. 2004;61(14):1460-5. PMID: 15332693. 10.1093/ajhp/61.14.1460. [DOI] [PubMed] [Google Scholar]
- 3.McLarty C. Development of a questionnaire to assess knowledge in women with gestational diabetes. Edith Cowan University. 1993. Accessed August 9, 2022. https://ro.ecu.edu.au/theses_hons/639. [Google Scholar]
- 4.Minschart C, Amuli K, Delameillieure A, Calewaert P, Mathieu C, Benhalima K. Multidisciplinary group education for gestational diabetes mellitus: A prospective observational cohort study. J Clin Med. 2020;9(2):509-25. PMID: 32069855. PMCID: . 10.3390/jcm9020509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alfadhli EM. Gestational diabetes mellitus. Saudi Med J. 2014;36(4): 399-406. PMID: 25828275. PMCID: . 10.15537/smj.2015.4.10307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hussain Z, Yusoff ZM, Sulaiman SAS. Gestational diabetes mellitus: Pilot study on patient’s related aspects. Arch Pharm Pract. 2014;5(2): 84-91. https://archivepp.com/storage/models/article/NyXHz47l-cxLXYyvIKpABXRFXxN0jq0yAIspgQ9Guf0kLrq7UZa7pG91nOF3y/gestational-diabetes-mellitus-pilot-study-on-patients-related-aspects.pdf. [Google Scholar]
- 7.Tan G. Diabetes care in the Philippines. Ann Glob Health. 2015;81(6): 863-9. PMID: 27108153. 10.1016/j.aogh.2015.10.004 [DOI] [PubMed] [Google Scholar]
- 8.Hussain Z, Yusoff ZM, Sulaiman SAS. Evaluation of knowledge regarding gestational diabetes mellitus and its association with glycaemic level: A Malaysian study. Prim Care Diabetes. 2014;9(3): 184-190. PMID: 25132140. 10.1016/j.pcd.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 9.Monir N, Zeba Z, Rahman A. Comparison of knowledge of women with gestational diabetes mellitus and healthy pregnant women attending a hospital in Bangladesh. J Sci Found. 2018;16(1):20-6. 10.3329/jsf.v16i1.38175. [DOI] [Google Scholar]
- 10.Coustan D. Gestational diabetes mellitus. Clin Chem. 2013;59(9): 1310-21. PMID: 23536513. 10.1373/clinchem.2013.203331. [DOI] [PubMed] [Google Scholar]
- 11.Szmuilowicz E, Josefson J, Metzger B. Gestational diabetes mellitus. Endocrinol Metab Clin North Am. 2019;48(3):479-93. PMID: 31345518. PMCID: . 10.1016/j.ecl.2019.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malong CL, Sia-Atanacio A, Andag-Silva A, Cunanan E. Incidence of postpartum diabetes and glucose intolerance among Filipino patients with gestational diabetes mellitus seen at a tertiary hospital. J ASEAN Fed Endocr Soc. 2013;28(1):56-63. 10.15605/jafes.028.01.11. [DOI] [Google Scholar]
- 13.Urbanozo H, Isip-Tan I. Association of gestational diabetes mellitus diagnosed using the IADPSG and the POGS 75-gram oral glucose tolerance test cut-off values with perinatal outcomes in the Philippine General Hospital. 2012;29(2):157-162. [Google Scholar]
- 14.Ku GM, Kegels G. Knowledge, attitude and perceptions of people with type 2 diabetes as related to self-management practices: Results of a cross-sectional study conducted in Luzon, Philippines. Chronic Illn. 2015;11(2):93-107. PMID: 24907237. 10.1177/1742395314538291. [DOI] [PubMed] [Google Scholar]
- 15.Moore CG, Nietert PJ, Stewart PW. Recommendations for planning pilot studies in clinical and translational research. Clin Transl Sci. 2011;4(5):332-7. PMID: 22029804. PMCID: . 10.1111/j.1752-8062.2011.00347.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carolan-Olah M, Vasilevski V. Development and validation of the ‘Knowledge of Gestational Diabetes (GDM)’ questionnaire among a sample of women with GDM in Australia. PMID: 33568322. 10.1016/j.pec.2021.01.029. [DOI] [PubMed]
- 17.Alayoub H, Curran S, Coffey M, Hatunic M, Higgins M. Assessment of the 476 effectiveness of group education on knowledge for women with newly 477 diagnosed gestational diabetes. Ir J Med Sci. 2018;187(1): 65-8. PMID: 28477326. 10.1007/s11845-017-1609-9. [DOI] [PubMed] [Google Scholar]
- 18.Ogu RN, Maduka O, Agala V, et al. Gestational diabetes mellitus knowledge among women of reproductive age in southern Nigeria: Implications for diabetes education. Int Quart Community Health Educ. 2020;40(3):177-83. PMID: 31554478. https://doiorg/10.1177/0272684X19876526. [DOI] [PubMed] [Google Scholar]
- 19.Spoelman WA, Bonten TN, de Waal MW, et al. Effect of an evidence-based website on healthcare usage: An interrupted timeseries study. BMJ Open. 2016; 6(11):e013166. PMID: 28186945. PMCID: . 10.1136/bmjopen-2016-013166. [DOI] [PMC free article] [PubMed] [Google Scholar]