Abstract
Intramuscular lipomas, typically found in subcutaneous tissue, rarely affect deeper muscular planes, especially those of the head and neck region. The following are 3 cases of intramuscular lipomas involving the sternocleidomastoid muscle. The first 2 patients presented with painless, palpable masses confirmed by diagnostic imaging as well-circumscribed intramuscular lipomas. One was treated surgically, while the other was managed conservatively with monitoring and close follow-up. The third patient reported dysphagia associated with occasional dyspnea and mild pain. The mass was identified as infiltrative lipoma and was resected surgically. Complete tumor removal with no recurrence at 6 months was observed for the first and last cases. The second case was serially followed at 3 and 6 months with no interval changes. We report the largest case series on intramuscular lipomas of the sternocleidomastoid muscle to enhance our understanding of this rare entity.
Keywords: Intramuscular, lipoma, sternocleidomastoid muscle, lipomatous tumor, benign pathology
Introduction
Benign lipomas are the most common type of soft-tissue neoplasms, characterized by mature adipose cells enclosed within thin fibrous capsules. While lipomas can develop anywhere on the body, they tend to occur superficially in the subcutaneous tissue. In rare cases, they may involve deeper muscular planes or the fascia. Lipomas are commonly present on the trunk and upper extremities and can have a round, oval, or multilobulated appearance. 1
Intramuscular lipomas account for less than 1% of all lipomas and occur more frequently in men than women. These tumors become exceedingly rare when occurring in the head and neck regions such as the sternocleidomastoid muscle (SCM), the larynx, and the tongue. The etiology of intramuscular lipomas is largely unknown, although they are thought to result from aberrant differentiation of mesenchymal cells. 2 Patients may clinically present with either an asymptomatic mass that causes only cosmetic concern or a painless, slowly growing mass that can cause discomfort and functional limitations depending on its location. When occurring in the head and neck region, common symptoms include a palpable mass, neck pain, and stiffness while in more severe cases, it can result in dysphagia and dyspnea. 3 The primary treatment for large intramuscular lipomas is surgical excision, while smaller lesions may be observed.
Case 1
A 52-year-old male patient presented to the otolaryngology clinic complaining of a left neck mass, stable in size for the past 5 years that recently started growing. He denied pain, skin changes, and swallowing or airway symptoms. On physical examination, an oval mass was palpated along the left SCM muscle. The mass was soft, non-tender to palpation, and measured 60 × 21 mm2 in size. The overlying skin showed normal color without erythema or inflammatory findings. Preoperative computed tomography (CT) scan showed a well-circumscribed non-enhancing fat-attenuating mass in the left side of the neck, suggestive of an intramuscular lipoma. There were no features of local tissue infiltration (Figure 1a). To confirm tissue diagnosis, a fine needle aspiration biopsy (FNA) was obtained which revealed mature fat cells consistent with lipoma. The physician opted to surgically remove the tumor because of its size and esthetic burden on the patient.
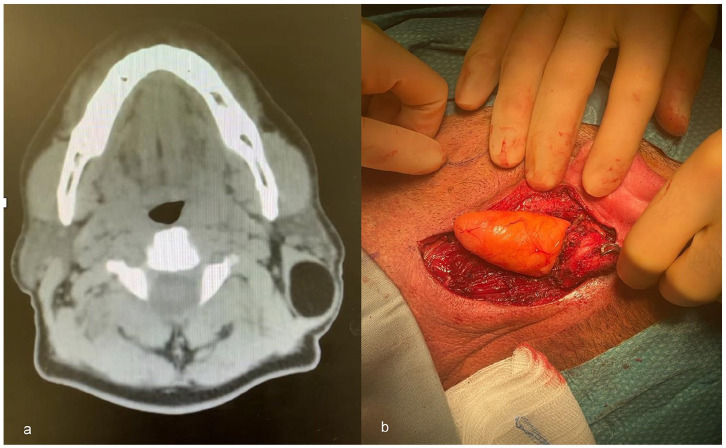
Figure 1.
(a) Preoperative axial CT scan showing a well-circumscribed well-defined non-enhancing fat-attenuating mass in the left side of the neck; (b) Intraoperative image of the lipoma invading the SCM muscle and adhering to the muscle fascia.
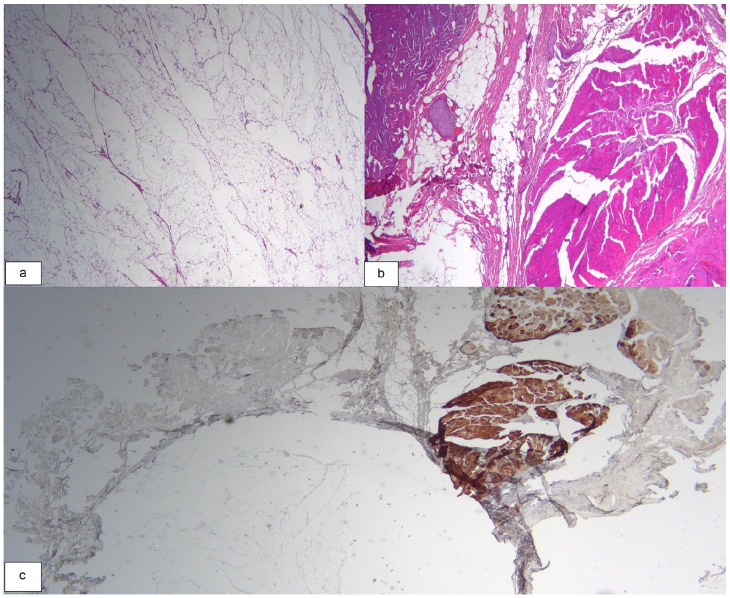
Under general anesthesia, an incision was extended from the mastoid tip along the neck creases. Dissection through the skin, subcutaneous tissues, until the anterior border of the SCM muscle, revealed a lipoma focally invading the muscle and adhering to its fascia (Figure 1b). Careful dissection was achieved around the mass until adequately freeing all edges to achieve complete resection. On gross examination, the oval-shaped mass measured 6.5 × 2 × 2 cm3, with soft, bright-yellow homogenous fatty tissue, and a rubbery consistency. Histologic findings showed mature fat cells within muscle tissues. Cellular dysplasia, mitosis, necrosis, or excessive proliferation of blood vessels were not observed (Figure 2). At the last follow-up visit 6 months after the procedure, no recurrence of the mass was observed.
Figure 2.
(a) Histologic appearance of an overall well circumscribed intramuscular lipoma with mature univacuolated adipocytes of fairly uniform size (H&E, X20); (b) Focal area of infiltration within the surrounding skeletal muscle (H&E, X40); (c) Desmin immunostaining to highlight the skeletal muscle.
Case 2
A 74-year-old male patient presented to the otolaryngology clinic for a left posterior triangle neck mass found incidentally 1 month before presentation. The patient reported mild pain, dysphagia to both solids and liquids, and occasional dyspnea without signs of respiratory distress such as stridor or cyanosis. On physical exam, a 10 cm mass was identified in the posterior triangle of the neck. It was soft, non-tender to palpation, with no overlying skin discoloration, and a preserved range of motion of the neck. Because of the presenting compressive symptoms, a preoperative CT scan was ordered, which showed an 11 × 7 × 7 cm3 mass within the SCM muscle. Magnetic resonance imaging (MRI) was further requested to rule out a sarcomatous component within the lesion because of its large size and unusual presentation. MRI revealed that the lesion is an intramuscular lipoma extending between neck level VB and the supraclavicular region, anteriorly limited by the SCM muscle (Figure 3a). Ultrasound-guided FNA confirmed that the tumor is consistent with benign adipose tissue as seen in lipoma. The patient was planned for surgical resection of the mass.
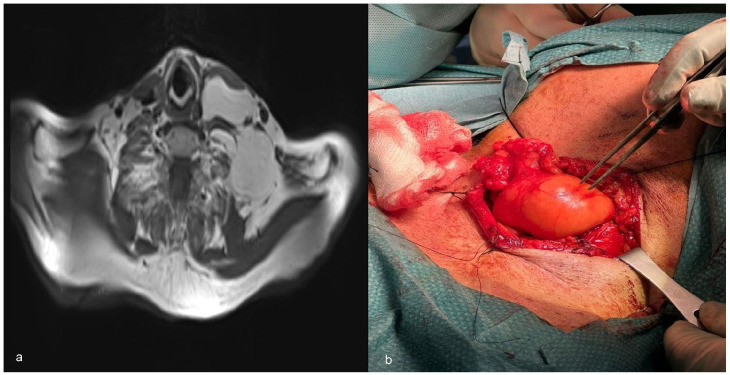
Figure 3.
(a) T1-weighted MRI revealing an intramuscular lipoma extending between neck level VB and the supraclavicular region, anteriorly limited by the sternocleidomastoid muscle; (b) Intraoperative image of the lipoma invading the SCM muscle and adhering to the muscle fascia.
Under general anesthesia, a horizontal incision over the neck mass was designed along the skin crease extending from its posterior edge to the anterior edge of the SCM muscle. Dissections through the skin, subcutaneous tissues, external jugular vein, and SCM muscle were achieved to expose the lipoma, which was infiltrating the muscle. Careful dissection was carried out to free its borders circumferentially while keeping its capsule intact (Figure 3b). The mass was friable and was delivered in fragmented parts. A specimen was sent for pathological examination which revealed mature adipose tissue consistent with lipoma. No cytological atypia was identified in the multiple sections of the adipose neoplasm, ruling out liposarcoma. At 6-month follow-up visit, no recurrence of the mass was observed.
Case 3
A 38-year-old male patient presented to the otolaryngology clinic with a 3-month history of a left neck mass, stable in size. The patient denied neck pain, difficulty articulating, dysphagia, odynophagia, limitation in neck motion, and other systemic symptoms. On physical examination, there was a 2 × 2 cm2 bulge at the anterior upper third of the left SCM muscle. It was non-tender to palpation with no overlying skin changes. There was no trismus and no limitation in the range of motion of the neck.
Initial ultrasound imaging the presence of an intramuscular lesion, which required an MRI for better soft tissue assessment. MRI showed a well-circumscribed small lipoma (4 × 2 cm2), within the muscle planes, and lacking solid or nodular components. Only one faintly enhancing septum was detected with no high-grade features. The lesion was labeled as a low-grade lipomatous tumor confirmed by FNA.
Given the size, lack of symptoms, and benign nature of the mass, the decision was made to conservatively manage the tumor with monitoring and close follow-up. Serial follow-up visits at 3 and 6 months showed stable size of the mass with no interval changes.
Discussion
Intramuscular lipomas can be classified into 2 subtypes: infiltrative and well-circumscribed. Histologically, infiltrative lipomas exhibit a mass with an irregular distribution of uniform, mature, and uni-vacuolated adipocytes. In contrast, the well-circumscribed subtype consists of a discrete mass of uniform, mature adipocytes that are demarcated from the surrounding muscle tissue. 4 Both subtypes share common features such as the absence of nuclear atypia, scattered capillaries, muscle bundles within the fat lobules, and an incomplete fibrous capsule covering the tumor. 2 Intramuscular lipomas can be differentiated from liposarcomas by the absence of atypical cells or vacuolated lipoblasts admixed with fibroblast-like spindle cells, particularly within the septa, and by the presence of fewer and thinner fibrous septae with less prominent blood vessels. 5
The etiology and pathogenesis of intramuscular lipomas remain unknown although many theories have been suggested. Factors such as trauma, metabolic disorders, metaplasia, and chronic irritation may be implicated in the formation of lipomas. 6 Type-selective muscle fiber atrophy coupled with an increase in the lysosomal catabolic enzyme cathepsin D may be associated with the development of intramuscular lipoma, highlighting the potential link between local muscle atrophy and lipoma formation. 7 Another interesting theory is the fibrohistiocytic differentiation of cells in fatty tumors: CD34+ perimysial fibroblasts and interstitial dendritic cells appear to undergo an adipocytic transformation, contributing to the pathogenesis of intramuscular lipomas. 8 Moreover, an immunohistochemical study demonstrated that structures within the head and neck region are abundantly covered with CD34+ fibrous tissues, especially the parotid gland and the sternocleidomastoid muscle. 9 This can potentially explain how an intramuscular lipoma could have arisen within the SCM muscle.
FNA can serve as valuable tool in confirming the lipomatous nature of the lesion as well as differentiating benign from malignant tumors with a high diagnostic accuracy and more than 90% specificity. 10 The primary treatment for large intramuscular lipomas is surgical excision, with complete removal being the preferred approach to reduce the risk of recurrence. In other cases, where the mass is smaller, observation may be considered. These benign tumors have an excellent prognosis with a low risk of recurrence and malignant transformation following complete resection. 5
After exploring PubMed library, only 6 relevant reports on intramuscular lipomas of the SCM muscle were identified, the majority of which being infiltrative,6,11 -13 except for 2 which were well-circumscribed.14,15 (Table 1). These articles focused on the recurrence rate of these benign tumors and their differentiation from malignant liposarcoma. MRI features may help distinguish between the 2 pathologies; the presence of thick septa, a maximum tumor diameter of more than 13 cm, and contrast enhancement constitute solid predictors of well-differentiated liposarcoma. 16 Moreover, both disease entities exhibit acceptably low rates of local recurrence with high 10-year local recurrence-free survival rates of 95% and 81% for intramuscular lipoma and atypical lipomatous tumor, respectively. 17
Table 1.
Characteristics of the SCM intramuscular lipoma case reports mentioned in the literature and in the present series.
| Study | Age, gender | Presentation | Imaging | Intra-operative findings/procedure | Histology | Recurrence |
|---|---|---|---|---|---|---|
| Mattel, 1983 | 29, M | Right neck mass, 17 × 9 cm along SCM | Soft tissue mass occupying SCM | Lipomatous mass splaying SCM fibers | Infiltrating fat between muscle fascicles | No recurrence at 18 months |
| Ozcan, 2004 | 29, M | Left neck mass, 4 × 5 cm adjacent to SCM | Lobulated well-defined adipose tissue signal density | Well-circumscribed mass between SCM fibers | Mature fat cells diffusely infiltrating striated muscle tissue | No recurrence at 3 years |
| Moumoulidis, 2004 | 52, M | Right neck swelling, 3 × 2 cm along SCM | Well-defined non-enhancing, low attenuation mass | Complete excision with 2 cm margin of SCM | Well-circumscribed adipose nodule encased in muscle | No recurrence at 36 months |
| Song, 2008 | 48, M | Left neck mass, 2.5 × 2.5 cm adjacent to SCM | Well-defined non-enhancing, low attenuation mass | Total excision | Mature fat cells infiltrating and splaying muscle fibers | No recurrence at 6 months |
| Sohn, 2010 | 46, F | Right neck mass, 5 × 2 cm along SCM | Fat-attenuating mass | Lipoma invading SCM, completely excised with portion of muscle | Fat within muscle tissue | No recurrence at 6 months |
| Lee, 2020 | 60, F | Right neck mass, 4.4 × 1.3 cm beneath the mastoid insertion site of the SCM | Well-circumscribed mass with adipose tissue signal density | Well-circumscribed lipomatous mass between the SCM muscle fibers | Mature fat cells, without lipoblasts or cytologic atypia | No recurrence at 41 months |
| Hadi, 2023 | 52, M | Left neck mass, 6 × 2 cm along and within the SCM | Well-circumscribed non-enhancing fat-attenuating mass | Complete excision of oval-shaped mass with soft, bright yellow, homogenous fatty tissue, and a rubbery consistency | Mature fat cells within muscle tissues with no cellular dysplasia, mitosis, or necrosis | No recurrence at 6 months |
| Mourad, 2023 | 38, M | Left neck mass, 2 × 2 cm at the anterior upper third of the left SCM muscle | Well-circumscribed small lipoma (4 × 2 cm) | Conservative management and close follow-up | FNA confirmed the diagnosis of lipoma | No interval changes at 3 and 6 months |
| Mourad, 2023 | 74, M | Left neck mass, 11 × 7 cm in the posterior triangle of the neck | Intramuscular lipoma anteriorly limited by the SCM. | Complete excision of friable lipoma infiltrating the SCM muscle | Mature adipose tissue with no cytological atypia | No recurrence at 6 months |
To the best of our knowledge, this is the largest series to date reporting on such a rare entity with 2 cases of well-circumscribed and 1 case of infiltrative intramuscular lipomas of the SCM muscle.
Conclusion
Intramuscular lipomas of the SCM muscle are rare benign tumors that occur in the neck region. Patients may present with an asymptomatic mass causing only cosmetic concern or a painless, slowly growing mass leading to discomfort and limited neck movement. In severe cases, the tumor can cause neck pain, stiffness, dysphagia, and dyspnea. Surgical excision is the primary treatment for larger intramuscular lipomas, aiming for complete removal to minimize the risk of recurrence. Smaller masses may be observed. The prognosis of intramuscular lipomas of the SCM muscle is excellent, with a low likelihood of recurrence or malignant transformation after successful resection.
Acknowledgments
None.
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author contributions: All authors contributed to the study conception and design. Material preparation, data collection was performed by Jad Hosri, Yara Yammine, and Nadine El Hadi. The first draft of the manuscript was written by Jad Hosri and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Ethics Approval Statement: The American University of Beirut Institutional Review Board has determined that this is not a “Human Subject Research” and hence no ethical approval is required. Therefore, this article does not contain any studies with human participants performed by any of the authors.
Informed Consent: For this type of study, informed consent is not required.
Consent for Publication: Consent for publication was obtained for every individual person’s data included in the study.
Data Availability Statement: The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- 1. Johnson CN, Ha AS, Chen E, Davidson D. Lipomatous soft-tissue tumors. J Am Acad Orthop Surg. 2018;26:779-788. [DOI] [PubMed] [Google Scholar]
- 2. Pélissier A, Sawaf MH, Shabana AH. Infiltrating (intramuscular) benign lipoma of the head and neck. J Oral Maxillofac Surg. 1991;49:1231-1236. [DOI] [PubMed] [Google Scholar]
- 3. de Bree E, Karatzanis A, Hunt JL, et al. Lipomatous tumours of the head and neck: a spectrum of biological behaviour. Eur Arch Otorhinolaryngol. 2015;272:1061-1077. [DOI] [PubMed] [Google Scholar]
- 4. Fletcher CD, Martin-Bates E. Intramuscular and intermuscular lipoma: neglected diagnoses. Histopathology. 1988;12:275-287. [DOI] [PubMed] [Google Scholar]
- 5. McTighe S, Chernev I. Intramuscular lipoma: a review of the literature. Orthop Rev (Pavia). 2014;6:5618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ozcan C, Görür K, Talas D, Aydin O. Intramuscular benign lipoma of the sternocleidomastoid muscle: a rare cause of neck mass. Eur Arch Otorhinolaryngol. 2005;262:148-150. [DOI] [PubMed] [Google Scholar]
- 7. Mori K, Chano T, Matsumoto K, Ishizawa M, Matsusue Y, Okabe H. Type-selective muscular degeneration promotes infiltrative growth of intramuscular lipoma. BMC Musculoskelet Disord. 2004;5:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Silverman JS, Tamsen A. Fibrohistiocytic differentiation in subcutaneous fatty tumors. Study of spindle cell, pleomorphic, myxoid, and atypical lipoma and dedifferentiated liposarcoma cases composed in part of CD34+ fibroblasts and FXIIIa+ histiocytes. J Cutan Pathol. 1997;24:484-493. [DOI] [PubMed] [Google Scholar]
- 9. Katori Y, Kiyokawa H, Kawase T, Murakami G, Cho BH. CD34-positive primitive vessels and other structures in human fetuses: an immunohistochemical study. Acta Otolaryngol. 2011;131:1086-1090. [DOI] [PubMed] [Google Scholar]
- 10. González-Cámpora R. Fine needle aspiration cytology of soft tissue tumors. Acta Cytol. 2000;44:337-343. [DOI] [PubMed] [Google Scholar]
- 11. Mattel SF, Persky MS. Infiltrating lipoma of the sternocleidomastoid muscle. Laryngoscope. 1983;93:205-207. [DOI] [PubMed] [Google Scholar]
- 12. Song HJ, Hong WK, Lee HS, Shin JH, Choi GS. Intramuscular lipoma of the sternocleidomastoid muscle. J Eur Acad Dermatol Venereol. 2008;22:363-364. [DOI] [PubMed] [Google Scholar]
- 13. Sohn WI, Kim JH, Jung SN, Kwon H, Cho KJ. Intramuscular lipoma of the sternocleidomastoid muscle. J Craniofac Surg. 2010;21:1976-1978. [DOI] [PubMed] [Google Scholar]
- 14. Moumoulidis I, Durvasula P, Jani P. Well-circumscribed intramuscular lipoma of the sternocleidomastoid muscle. Auris Nasus Larynx. 2004;31:283-285. [DOI] [PubMed] [Google Scholar]
- 15. Lee J, Han K, Kim CH. Rare tumors presenting as a mastoid mass. Case Rep Otolaryngol. 2020;2020:8985730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Knebel C, Neumann J, Schwaiger BJ, et al. Differentiating atypical lipomatous tumors from lipomas with magnetic resonance imaging: a comparison with MDM2 gene amplification status. BMC Cancer. 2019;19:309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Presman B, Jauffred SF, Kornø MR, Petersen MM. Low recurrence rate and risk of distant metastases following marginal surgery of intramuscular lipoma and atypical lipomatous tumors of the extremities and trunk wall. Med Princ Pract. 2020;29:203-210. [DOI] [PMC free article] [PubMed] [Google Scholar]