Abstract
Maldevelopment of the vagina and cervix is frequently accompanied by uterine aplasia or hypoplasia. Complete cervico-vaginal aplasia with a normally developing uterus is a very uncommon type of developmental failure. Failure to treat the condition can result in complications such as hematometra and hematosalpinx caused by the retrograde flow of blood into the fallopian tubes. In this case report, we describe the case of a 32-year-old woman experiencing cyclic abdominal pain and primary amenorrhea. The patient exhibited cervico-vaginal agenesis, with a functional uterus that was complicated by hematometra and bilateral hematosalpinx.
Keywords: Pelvic pain, vaginal agenesis, hematometra, amenorrhea
Introduction
Vaginal aplasia or vaginal agenesis, is a rare congenital abnormality of the female genital tract, occurring in approximately 1 in 4000 female births. 1 The Mayer-Rokitansky-Kuster-Hauser syndrome (MRKH syndrome) is the most common cause of this anomaly. Despite extensive gene research, the syndrome’s etiology is still unknown, though it is thought to be hereditary. 2 However, in 9% of cases, vaginal aplasia can be isolated in the presence of a functional uterus. 3
Case report
A 32-year-old woman with no prior medical conditions presented with primary amenorrhea and has been experiencing chronic and cyclic pelvic pain since the age of 12. The patient reported not having any gynecological history or sexual activity and had never seeking medical attention before due to financial constraints and limited accessibility to healthcare.
During the clinical examination, the patient had a normal physical appearance and well-developed secondary sexual characteristics. In addition, a hard and painful pelvic mass was detected.
During the examination of the vulvo-perineal area, the external genitalia appeared normal, with well-defined labia majora, labia minora, and clitoris. However, there was an absence of a vaginal opening.
Ultrasonography revealed an enlarged uterus with a significant mass occupying the uterine cavity (Figure 1).
Figure 1.
Axial and sagittal ultrasonography images showing a large heterogeneous mass in the uterine cavity.
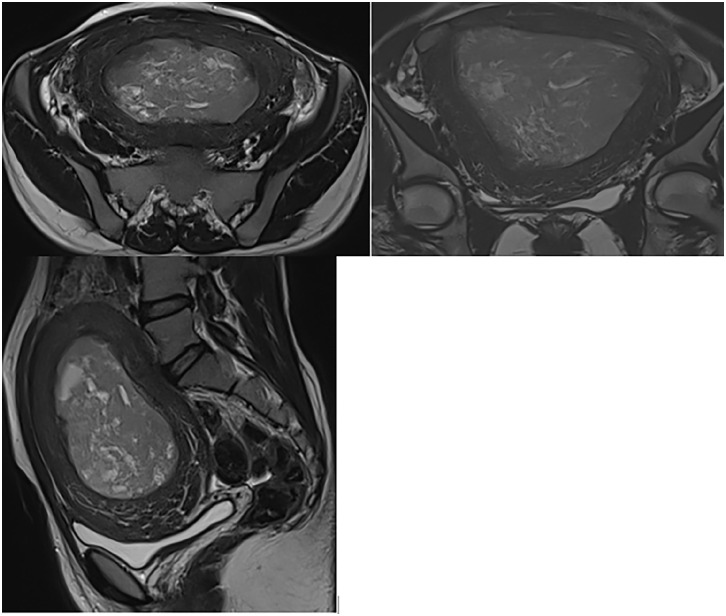
A pelvic magnetic resonance imaging (MRI) scan showed an anteverted uterus measuring 106 mm in height, 53 mm in thickness, and 122 mm in width. There was a pronounced accumulation of blood (hematometra) at the empty line of the uterus. The junctional zone appeared normal, and the myometrium was homogeneous. In addition, there were bilateral hematosalpinx and a hemorrhagic cyst in the left ovary. The cervix and vagina were not visualized (Figure 2).
Figure 2.
Magnetic resonance imaging revealing a cystic mass consistent with clotted blood filling the uterine cavity, without uterine cervix and vagina.
The diagnosis of hematometra and hematosalpinx secondary to total cervico-vaginal agenesis on a functional uterus was retained. There were no MRI findings of endometriosis.
The condition was discussed with the patient. A hysterectomy was suggested for the patient and her family. After consultations with other specialists, the consensus was that a hysterectomy would be the best treatment for her case.
Abdominal hysterectomy was performed using the usual techniques. At the lower part of the uterus, a cervix was not demonstrated.
The postoperative period was uneventful, and the patient was discharged in satisfactory condition.
The histopathological examination of the hysterectomy specimen revealed no evidence of endometriosis.
Discussion
Congenital anomalies of the genital tract depend on the degree of development of the müllerian system. The disorder known as müllerian agenesis, also known as Rokitansky Kuster-Hauser syndrome, results from the failure of the development of the müllerian system. In rare cases, the müllerian system’s cranial part develops while the caudal part fails to develop, resulting in a functional uterus with congenital cervix and vaginal aplasia. 4 Typically, vaginal aplasia is partial, and the distal, medial, or cranial third is affected. 5 The incidence rate of congenital absence of the vagina is approximately 1 in 4000 to 10,000 live births. Among these cases, it is estimated that around 7%–8% will have a functioning uterus. 4 Cervicovaginal aplasia, considered the most uncommon form of developmental failure, has an incidence of 1 in 80,000 to 100,000 live births. 6
Adolescent females affected by this disease frequently present with primary amenorrhea, normal ovarian function, normal developed secondary sexual features, and a 46,XX karyotype.
Vaginal agenesis often coexists with other anomalies, with urinary tract anomalies being the most prevalent. Among these, unilateral renal agenesis (21%), pelvic kidney, horseshoe kidney, and ureteric duplication are commonly reported, accounting for approximately 40% of cases. 2
The accumulation of menstrual blood leads to the dilation of the uterus, causing a backflow that fills both fallopian tubes and spills into the abdominal cavity. This retrograde menstruation contributes to the blockage of the tubes and the development of hematosalpinx. It can also result in the formation of adhesions within the pelvic region or membranes, gradually straightening from the ostium to the tuba. Each patient may have a varying capacity for collecting menstrual blood, with the highest reported capacity being 3000 ml, according to a study. 7 Furthermore, the dilation of the genital area creates a mass sensation that can be felt near the umbilical cord, as in our case. 8
During childhood, vaginal malformations remain asymptomatic; they become noticeable in adolescence if they stop the flow of menstrual blood. 5
Patients tend to underreport their vaginal agenesis symptoms until they become sexually active. The incapacity to have coitus, primary amenorrhea, and infertility are the symptoms. Patients with vaginal agenesis may also be uncomfortable with some symptoms that affect their quality of life. Periodic soreness in the lower abdomen is one of the symptoms. The pain is consistently experienced on approximately the same date each month. It represents the menstrual period, which is obstructed and collected. Some patients (like the patient in this case) still have a normal uterus despite not having a vagina. 8
The diagnosis is confirmed by a pelvic ultrasound, which can reveal a hematometra along with the complete absence of the vagina while demonstrating normal functioning of the ovaries and uterus. Renal ultrasound or intravenous urography may be performed to assess for any associated urinary abnormalities. 3
While pelvic ultrasonography is widely accessible and can provide a pretty precise image of the uterus, it is not as sensitive as a magnetic resonance imaging scan when it comes to clearly defining the morphology of the uterus.
MRI is recognized as the gold standard for imaging anomalies of the upper urogenital tract. 9 According to Humphries et al., the application of MRI also extends to anomalies of the vagina, and it provides valuable information in children and adolescents where clinical examination of the vagina may not be possible.
On T2-weighted sequences, in the sagittal and coronal uterine planes, the junctional zone has low signal intensity, the outer myometrium has moderate to high signal intensity, and the endometrium has high signal intensity. Because the cervix only typically exhibits two distinct zones: a narrow inner endocervical canal with a high signal intensity and a larger outside zone with a low signal intensity that resembles the uterine corpus’ junctional zone, it may be easily distinguished from the uterine corpus. Consequently, an MRI examination makes it easy to recognize when the cervix is absent. 4
The treatment of vaginal aplasia depends on whether there are coexistent uterine anomalies. The literature describes a wide range of strategies, indicating that the perfect approach has not yet been discovered. 5 The creation of a neovagina and neocervix is a complex procedure associated with high morbidity and limited success. Many patients eventually require a hysterectomy. According to the literature, several authors10,11 have concluded that hysterectomy should be the treatment of choice, with psychological support provided, as reconstructive surgery carries serious complications such as sepsis, endometriosis, and the need for multiple surgeries due to restenosis. In addition, due to endometriosis, the patient has a low possibility of spontaneous conception. 12
However, with advancing surgical skills and assisted reproductive techniques, conservative surgery could be considered as the primary treatment option. It is important to consider the patient’s femininity and the potential impact on her self-esteem caused by a distortion of her physical image. 12 In this particular case, we opted for hysterectomy after obtaining informed consent from the patient.
Among all congenital anomalies, the absence of the vagina in a normal uterus is one of the most difficult to manage. Though it is always tempting to keep the uterus to allow conception and delivery, excision of a functional uterus is an established treatment option for such anomalies, providing relief from pelvic pain caused by hematocrit. 5
Conclusion
A diagnosis of congenital cervico-vaginal agenesis is comparatively uncommon and has a variety of presentations. This might cause misdiagnosis and treatment delays. To elucidate the type of obstructive mullerian anomaly present, a thorough history, physical exam, and confirmatory imaging studies are necessary.
Acknowledgments
None.
Footnotes
Author contributions: C.F. was responsible for the manuscript concept, design, editing, and literature search; S.E. helped in manuscript editing and literature search, manuscript editing, and manuscript review. N.B. contributed to the conception and design. N.A. contributed to acquisition, analysis, and interpretation. S.E.H. contributed to acquisition, analysis, and interpretation; L.C. critically revised the manuscript and gave final approval.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics approval: Our institution does not require ethical approval for reporting individual cases or case series.
Informed consent: Written informed consent was obtained from the patient for their anonymized information to be published in this article.
Guarantor of submission: The corresponding author is the guarantor of submission.
ORCID iDs: Chaymae Faraj  https://orcid.org/0009-0003-2192-8756
https://orcid.org/0009-0003-2192-8756
Fatima Chait  https://orcid.org/0000-0003-3780-3934
https://orcid.org/0000-0003-3780-3934
References
- 1. Creatsas G, Deligeoroglou E. Vaginal aplasia and reconstruction. Best Pract Res Clin Obstet Gynaecol 2010; 24(2): 185–191. [DOI] [PubMed] [Google Scholar]
- 2. Kimberley N, Hutson JM, Southwell BR, et al. Vaginal agenesis, the hymen, and associated anomalies. J Pediatr Adolesc Gynecol 2012; 25(1): 54–58. [DOI] [PubMed] [Google Scholar]
- 3. Meklaa A, Rahali Moussaoui D, Dehayni M. Aplasie vaginale avec utérus fonctionnel: a propos d’un cas. Res J fr 2017; 4: 2268. [Google Scholar]
- 4. Badawy SZ, Prasad M, Powers C, et al. Congenital cervicovaginal aplasia with septate uterus and functioning endometrium. J Pediatr Adolesc Gynecol 1997; 10(4): 213–217. [DOI] [PubMed] [Google Scholar]
- 5. Sparac V, Stilinovic K, Ilijas M, et al. Vaginal aplasia associated with anatomically and functionally normal uterus. Eur J Obstet Gynecol Reprod Biol 2004; 115(1): 110–112. [DOI] [PubMed] [Google Scholar]
- 6. Jain N, Sircar R. Laparoscopic management of congenital cervico-vaginal agenesis. J Gynecol Endosc Surg 2011; 2(2): 94–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bakos O, Berglund L. Imperforate hymen and ruptured hematosalpinx: a case report with a review of the literature. J Adolesc Health 1999; 24(3): 226–228. [DOI] [PubMed] [Google Scholar]
- 8. Moegni F, Meutia AP, Kouwagam AD, et al. Secondary pyosalpinx after reconstructive surgery of vaginal agenesis patient with bilateral hematosalpinx: a case report. Int J Surg Case Rep 2021; 85: 106166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Humphries PD, Simpson JC, Creighton SM, et al. MRI in the assessment of congenital vaginal anomalies. Clin Radiol 2008; 63(4): 442–448. [DOI] [PubMed] [Google Scholar]
- 10. Rock JA, Schlaff WD, Zacur HA, et al. The clinical management of congenital absence of the uterine cervix. Int J Gynaecol Obstet 1984; 22(3): 231–235. [DOI] [PubMed] [Google Scholar]
- 11. Hampton HL. Role of the gynaecologic surgeon in the management of urogenital anomalies in adolescents. CurrOpin Obstet Gynaecol 1990; 2: 812–818. [PubMed] [Google Scholar]
- 12. Khoiwal K, Singh M, Agarwal A, et al. The path of birth is not always normal: a case report of cervicovaginal agenesis. Gynecol Minim Invasive Ther 2021; 10(4): 247–251. [DOI] [PMC free article] [PubMed] [Google Scholar]