Abstract
This case report discusses a diagnosis of uterine torsion in an 84-year-old woman who presented with five days of right lower quadrant abdominal pain, nausea, vomiting, constipation, and poor intake. Computed tomography (CT) imaging demonstrated a whorled configuration at the junction of the cervix and lower uterine segment, with the left gonadal vein crossing midline, and two previously known right leiomyomas now appearing on the left. These findings were consistent with the diagnosis of uterine torsion. She then underwent an urgent exploratory laparotomy, and the uterus was found to be dextroverted 270 degrees, with dark mottled purple tissue and engorged vessels. A supracervical hysterectomy and bilateral salpingo-oopherectomy were performed. Final pathology demonstrated extensive necrosis. This case reviews the classic presentation and imaging findings for the rare diagnosis of uterine torsion and options for management of both non-gravid and gravid patients.
Keywords: Uterine Torsion, Leiomyoma, Gynecologic Emergency, Whirlpool Sign, X-Shaped, Pelvic MRI, Pelvic CT
CASE REPORT
An 84-year-old woman with no significant medical or surgical history initially presented to the emergency department (ED) after five days of right lower quadrant abdominal pain, nausea, vomiting, constipation, and poor oral intake. The pain was positional, mainly when she laid on her right side and felt the abdominal mass shift to her right side. She previously had similar episodes of less severe pain over the last few years which usually resolved spontaneously. She had additionally noted an increased size of her abdomen, but she otherwise denied bleeding, bloating, pelvic pain, early satiety, decreased appetite, or weight loss, or family history of malignancy. She had no prior imaging of her abdomen.
In the ED, her labs were significant for an acute kidney injury (AKI) due to poor oral intake from pain, which resolved with intravenous fluids. She had otherwise normal vitals and tenderness in the right lower quadrant. She underwent a CT Abdomen/Pelvis without contrast (due to her AKI) that showed a large 20cm calcified uterine leiomyoma. There was trace free fluid, potentially related to degeneration of the fibroid.
The leading diagnosis at the time was a degenerating leiomyoma causing acute abdominal pain, and the patient was admitted for pain control. A magnetic resonance imaging (MRI) Abdomen/Pelvis with contrast was recommended to better characterize the leiomyoma and evaluate for signs of malignancy given the concern in a postmenopausal patient with an enlarging uterine mass.
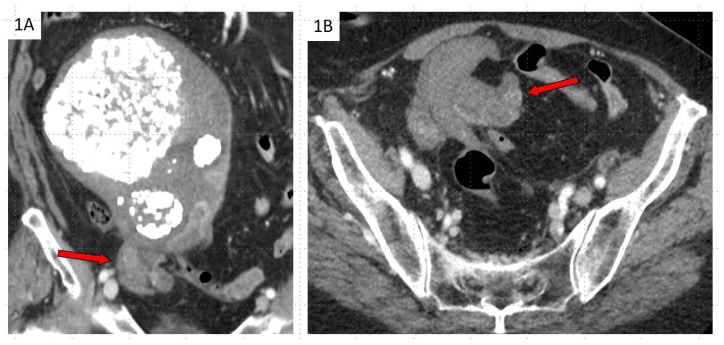
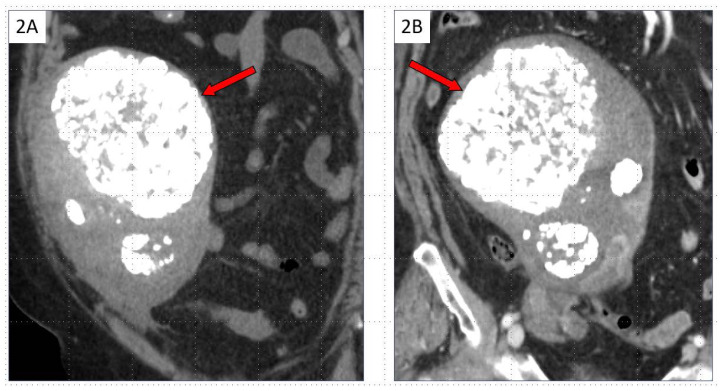
The patient was not able to tolerate MRI, and she underwent a CT Abdomen/Pelvis with contrast on hospital day (HD#5), which demonstrated a whorled configuration at the junction of the cervix and lower uterine segment (Figure 1), with the left gonadal vein crossing midline, wrapping around the anterior aspect of the lower uterus. Two calcified leiomyomas that were previously positioned on the right aspect of the uterus on the day of admission were now positioned on the left of the uterus (Figure 2). These findings were consistent with uterine torsion.
Figure 1.
84 yo with uterine torsion of large leiomyoma. FINDINGS: (A) Coronal and (B) axial contrast-enhanced CT obtained on HD#5 shows swirling at the junction of the cervix and lower uterine segment (arrows) and involving the gonadal veins bilaterally. The “whirlpool sign” is a highly specific imaging marker for torsion. TECHNIQUE: (A) Coronal contrast-enhanced CT, CTDIvol Min: 16.8 mGy, CTDIvol Max: 16.8 mGy, DLP: 1001.6 mGy.cm, 2.50 mm slice thickness, 350–150 ml iohexol (B) Axial contrast-enhanced CT, CTDIvol Min: 16.8 mGy, CTDIvol Max: 16.8 mGy, DLP: 1001.6 mGy.cm, 2.50 mm slice thickness, 350–150 ml iohexol
Figure 2.
84 yo with uterine torsion of large leiomyoma. FINDINGS: (A) Coronal non-contrast CT on initial presentation shows multiple calcified leiomyomas with the dominant leiomyoma positioned at the medial superior aspect of the uterus (arrow). (B) Coronal contrast-enhanced CT obtained 5 days later shows flipped or reversed configuration of the leiomyomas with the dominant leiomyoma now at the lateral superior aspect of the uterus (arrow). In patients with short interval repeat imaging and intermittent torsion, leiomyomas can serve as landmarks to determine changes in orientation. TECHNIQUE: (A) Coronal CT without contrast, CTDIvol Min: 15.4 mGy, CTDIvol Max: 15.4, DLP: 818 mGy.cm, 1.25 mm slice thickness, no radiation (B) Coronal contrast-enhanced CT, CTDIvol Min: 16.8 mGy, CTDIvol Max: 16.8 mGy, DLP: 1001.6 mGy.cm, 2.50 mm slice thickness, 350–150 ml iohexol
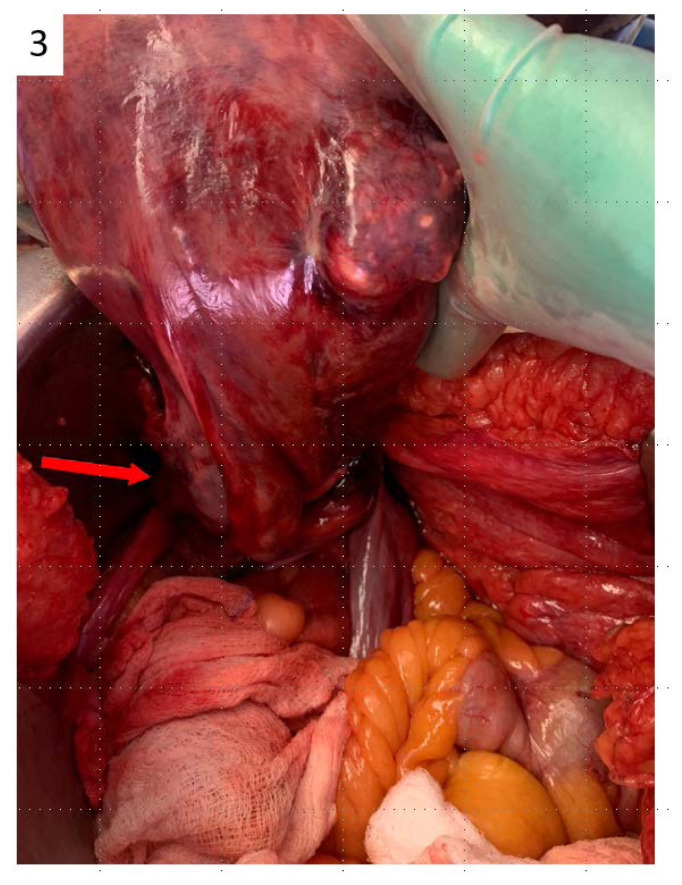
She was recommended urgent surgical management. On HD#6, she underwent an exploratory laparotomy, supracervical hysterectomy, and bilateral salpingo-oopherectomy. Intraoperatively, the uterus was dextroverted 270 degrees along the vertical axis, appearing ischemic with a dark mottled purple hue and markedly engorged gonadal vessels bilaterally (Figure 3). The cervix was extremely attenuated and not able to be identified with palpation, and so the decision was made not to attempt removal of the cervix. Her surgery was otherwise uncomplicated.
Figure 3.
Intraoperative image of the uterus shows twisting along its vertical axis (arrow)
Her postoperative course was complicated by a pulmonary embolism. The morning of her surgery, prophylactic dose enoxaparin was held for surgery. Six hours postoperatively, prophylactic dose heparin was restarted. On postoperative day (POD#1), she had an increasing oxygen requirement with new cough and increased work of breathing. CT Chest showed findings consistent with a right lower lung segmental pulmonary embolism, and she was started on a heparin drip. She was eventually transitioned to rivaroxaban with plans to continue treatment for 3 months.
She ultimately was discharged in stable condition on HD#17 once meeting all postoperative milestones. Final pathology demonstrated extensive necrosis and stromal hemorrhage. She was feeling well at her post-operative appointment and has not required care since then.
DISCUSSION
Etiology & demographics
Uterine torsion occurs when there is rotation of the uterus greater than 45° around the long axis [1,2]. While the uterus can rotate physiologically up to 45°, greater than 45° is pathologic with irreversible damage starting at 60°. With only a few cases found in the literature, it is extremely rare, with most case reports of uterine torsion reported in gravid patients in the 2nd or 3rd trimester of pregnancy [2]. Although it has been reported more commonly among gravid patients in all trimesters, it can also present in non-gravid patients, including premenarchal and post-menopausal patients [3]. Risk factors include pelvic masses including uterine leiomyomas, adnexal masses, Mullerian anomalies and uterine malformations, fetal malpresentation, and adhesions around which the uterus can twist [4–9].
Clinical & Imaging findings
Patient presentation is nonspecific, with abdominal pain as the most commonly described symptom in case reports. Additional symptoms include vaginal bleeding, nausea, vomiting, decreased fetal movement, fetal distress, hemodynamic instability, syncope, maternal pallor, maternal tachycardia, uterine size greater than dates, rapid enlargement of the uterus, or labor obstruction. Alternatively, patients can be asymptomatic with torsion diagnosed incidentally upon surgery [2–8]. Imaging may further raise suspicion for surgery with findings including a “swirl” or “whirlpool sign” on ultrasound, CT, or MRI at the level of the cervix and engorged myometrial vessels [7,10,11]. In gravid patients with uterine torsion, management includes emergent laparotomy and detorsion to restore perfusion to the uterus and decrease risk of fetal injury [8,9,12]. In the non-gravid patient, surgery is performed typically to alleviate the patient’s pain.
Preoperative diagnosis of uterine torsion is difficult, but can be made with ultrasound, CT or MRI. On ultrasound, a change in location of fibroids from prior scan or change in the location of the placenta in a gravid uterus may increase concern for uterine torsion. CT or MRI may demonstrate a whorled configuration (the “whirlpool sign”) of vessels or of the cervix; additionally, axial MRI may show an X-shaped configuration of the upper vagina (instead of the normal H shape). This patient’s imaging demonstrated both a shift in the location of her fibroids as well as the “whirlpool sign” on CT with contrast consistent with uterine torsion. A prior literature review of 26 cases of uterine torsion noted that 18 of the cases had pre-operative imaging with CT or MRI. Of those eighteen cases, eight (44.4%) were noted to have the “whirlpool sign” [3].
Differential diagnosis
These above imaging findings of a “whirlpool sign” may be similarly noted in cases of ovarian torsion, which also leads to twisted vascular pedicles. Ovarian torsion is much more common diagnosis. It additionally requires expeditious surgical management which would confirm the diagnosis of either ovarian or uterine torsion. As patients with reported uterine torsion often have leiomyoma, another diagnosis to consider is pain from a degenerating fibroid that has outgrown its blood supply. Pain from a degenerating fibroid is often localized to the fibroid itself. Imaging findings can vary; the most common type of degeneration is hyaline degeneration, which has a heterogenous appearance and produces low signal on T2W images [19].
Treatment & prognosis
Management of uterine torsion is surgical and involves consideration of the age of the patient, the fertility desires of the patient, and whether tissue necrosis is present. For both premenopausal and postmenopausal women, the majority of cases have been managed by laparotomy and both hysterectomy and bilateral salpingo-oophorectomy as there is frequently uterine, ovarian, and tubal ischemia due to prolonged torsion [3]. Management of gravid cases usually requires emergency cesarean and detorsion to prevent to fetal compromise due to reduce uterine perfusion.
In cases in which there is not yet extensive necrosis identified upon laparoscopy or laparotomy, it appears reasonable to untwist the uterus and remove only the tissue that appears necrotic [13,14]. This allows for future fertility and ovarian preservation for pediatric and pre-menopausal patients [13]. Removal of the pelvic mass with cystectomy, myomectomy, or correction of the mullerian anomaly is usually performed at this time to decrease risk for future occurrence [15]. For pregnant patients, cesarean section should be considered depending on the gestational age of the pregnancy.
Regardless of approach, emergency surgery is indicated at all ages due to concern for worsening tissue necrosis with delayed management, which in turn can cause acute anemia from stromal hemorrhage, coagulopathy, and renal dysfunction [16–18].
TEACHING POINT
Uterine torsion is a rare diagnosis in which imaging (“whirlpool sign” or X-shaped configuration of the upper vagina) can play a crucial role in making a difficult pre-operative diagnosis. If uterine torsion is suspected, emergent surgery is indicated as expedited management may lead to possible uterine preservation for future fertility and decrease medical complications.
CONSENT
No. We attempted to obtain written informed consent from the patient – we called the patient multiple times and sent a letter. We were able to contact the patient’s power of attorney who felt that publishing her case as a case report would be concordant with her wishes (she intends to donate her body to UCSF after her death).
Table 1.
Summary table of the discussion in this case report
| SUMMARY TABLE | |
|---|---|
| ETIOLOGY | Uterine torsion occurs when there is rotation of the uterus greater than 45° around the long axis. Rotation of greater than 45° is pathologic with irreversible damage starting at 60°. |
| INCIDENCE | Uterine torsion is extremely rare with only around 20–30 cases reported in the last 20 years. |
| AGE PREDILECTION | Most case reports of uterine torsion have been reported in patients in their 20s–30s as post case reports have been reported in gravid patients in the 2nd or 3rd trimester of pregnancy |
| RISK FACTORS | Pregnancy, pelvic masses including uterine leiomyomas, adnexal masses, Mullerian anomalies and uterine malformations, fetal malpresentation, and adhesions around which the uterus can twist |
| TREATMENT | Management of uterine torsion is surgical. For both premenopausal and postmenopausal women, the majority of cases have been managed by laparotomy and both hysterectomy and bilateral salpingo-oophorectomy. Management of gravid cases usually requires emergency cesarean and detorsion to prevent to fetal compromise due to reduce uterine perfusion. |
| PROGNOSIS | Significant fetal mortality and morbidity in gravid cases, and significant maternal/patient morbidity has been reported (acute anemia from stromal hemorrhage, coagulopathy, and renal dysfunction) have been reported [12]. |
| FINDINGS ON IMAGING | CT or MRI may demonstrate a whorled configuration (the “whirlpool sign”) of vessels or of the cervix; additionally, axial MRI may show an X-shaped configuration of the upper vagina (instead of the normal H shape). Either modality may also note a shift in the location of the fibroids from a prior scan. |
Table 2.
Differential table reviews the differences between imaging findings between uterine torsion and ovarian torsion. Ultimately, both require expeditious surgical management, which would confirm diagnosis.
| DIFFERENTIAL TABLE | |
|---|---|
| OVARIAN TORSION | Transvaginal ultrasound: enlarged ovary, stromal edema leading to peripheralization of follicles, whorled configuration (the “whirlpool sign”) of vessels CT/MRI: Similar findings as on ultrasound |
| UTERINE TORSION | Transvaginal ultrasound: whorled configuration (the “whirlpool sign”) of vessels CT/MRI: whorled configuration (the “whirlpool sign”) of vessels or of the cervix; additionally, axial MRI may show an X-shaped configuration of the upper vagina (instead of the normal H shape). Either modality may also note a shift in the location of the fibroids from a prior scan. |
| DEGENERATING FIBROIDS | MRI: heterogenous appearance with low signal on T2W images |
QUESTIONS
Question 1: What is a possible description of a normal appearance of the upper vagina on an axial MRI?
H-shaped configuration (applies)
X-shaped configuration
U-shaped configuration
T-shaped configuration
W-shaped configuration
Answer 1: H-shaped configuration: A normal appearing upper vagina can appear as an H-shaped configuration on axial MRI. [CT or MRI may demonstrate a whorled configuration (the “whirlpool sign”) of vessels or of the cervix; additionally, axial MRI may show an X-shaped configuration of the upper vagina (instead of the normal H shape)].
Question 2: What is a possible description of the upper vagina on an axial MRI in the case of uterine torsion?
H-shaped configuration
X-shaped configuration (applies)
U-shaped configuration
T-shaped configuration
W-shaped configuration
Answer 2: X-shaped configuration: A reported imaging finding of uterine torsion is an X-shaped configuration of the upper vagina on axial MRI. [CT or MRI may demonstrate a whorled configuration (the “whirlpool sign”) of vessels or of the cervix; additionally, axial MRI may show an X-shaped configuration of the upper vagina (instead of the normal H shape)].
Question 3: What is a risk factor for uterine torsion?
Unicornuate uterus
Fibroids
Breech presentation
Post-surgical adhesions
All of the above (applies)
Answer 5: All of the above: [Risk factors include pelvic masses including uterine leiomyomas, adnexal masses, Mullerian anomalies and uterine malformations, fetal malpresentation, and adhesions around which the uterus can twist.]
Question 4: What are potential complications of uterine torsion?
Acute anemia
Coagulopathy
Renal dysfunction
Loss of fertility
All of the above (applies)
Answer 5: All of the above: Acute anemia from stromal hemorrhage, coagulopathy, renal dysfunction, and widespread necrosis requiring hysterectomy are all complications from uterine torsion [Regardless of approach, emergency surgery is indicated at all ages due to concern for worsening tissue necrosis with delayed management, which in turn can cause acute anemia from stromal hemorrhage, coagulopathy, and renal dysfunction.]
Question 5. Which of these statements is false?
Uterine torsion is an indication for emergent surgical management
Uterine conservation should not be attempted in cases of uterine torsion due to widespread necrosis (applies)
A whirlpool sign from whorled vessels can be seen in uterine torsion
Uterine torsion is more commonly reported in gravid patients
None of the above
Answer 2: Uterine conservation can be attempted. The other statements are all true. [In cases in which there is not yet extensive necrosis identified upon laparoscopy or laparotomy, it appears reasonable to untwist the uterus and remove only the tissue that appears necrotic.]
ABBREVIATIONS
- CT
computed tomography
- ED
emergency department
- AKI
acute kidney injury
- MRI
magnetic resonance imaging
- HD
hospital day
- POD
postoperative day
REFERENCES
- 1.Collinet P, Narducci F, Stien L. Torsion of a nongravid uterus: an unexpected complication of an ovarian cyst. Eur J Obstet Gynecol Reprod Biol. 2001;98(2):256–257. doi: 10.1016/s0301-2115(01)00334-7. [DOI] [PubMed] [Google Scholar]
- 2.Ramseyer AM, Whittington JR, Resendez VA, Whitcombe DD, Magann EF. Torsion in the Gravid and Nongravid Uterus: A Review of the Literature of an Uncommon Diagnosis. Obstet Gynecol Surv. 2020;75(4):243–252. doi: 10.1097/OGX.0000000000000767. [DOI] [PubMed] [Google Scholar]
- 3.Matsumoto H, Aoyagi Y, Morita T, Nasu K. Open Med Case Rep. 2021. Uterine torsion in non-gravid women: A case report and review of cases reported in the last 20 years SAGE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Deshpande G, Kaul RPM. A Case of Torsion of Gravid Uterus Caused by Leiomyoma. Case Rep Obstet Gynecol. 2011 doi: 10.1155/2011/206418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yap FY, Radin R, Tchelepi H. Torsion, infarction, and rupture of a nongravid uterus: a complication of a large ovarian cyst. Abdom Radiol (NY) 2016;41(12):2359–2363. doi: 10.1007/s00261-016-0789-5. [DOI] [PubMed] [Google Scholar]
- 6.Grover S, Sharma Y, Mittal S. Uterine torsion: a missed diagnosis in young girls? J Pediatr Adolesc Gynecol. 2009;22(1):e5–8. doi: 10.1016/j.jpag.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 7.Davies JH. Case report: Torsion of a nongravid nonmyomatous uterus. Clin Radiol. 1998;53(10):780–782. doi: 10.1016/s0009-9260(98)80326-7. [DOI] [PubMed] [Google Scholar]
- 8.Cipullo LMA, Milosavljevic S, van Oudgaarden ED. Uterus didelphys: report of a puerperal torsion and a review of the literature. Case Rep Obstet Gynecol. 2012 doi: 10.1155/2012/190167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jensen JG. Uterine torsion in pregnancy. Acta Obstet Gynecol Scand. 1992;71(4):260–265. doi: 10.3109/00016349209021049. [DOI] [PubMed] [Google Scholar]
- 10.Cheong EHT, Tan TJ, Wong KM. Torsion of a Myomatous, Non-gravid Uterus: CT Findings. J Radiol Case Rep. 2018;12(4):6–14. doi: 10.3941/jrcr.v12i4.3360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sen A. Engorged myometrial vein sign in uterine torsion. Eur J Obstet Gynecol Reprod Biol. 2016;198:176–177. doi: 10.1016/j.ejogrb.2016.01.013. [DOI] [PubMed] [Google Scholar]
- 12.Jovanovic D, Del Granado A, Stiller A. Torsion of the gravid uterus: a review and a case. J Reprod Med. 1972;8(2):81–84. [PubMed] [Google Scholar]
- 13.LaHood J, You W. Uterine torsion and subsequent rupture in a gravid bicornuate uterus associated with an elevated alpha-fetoprotein. BMJ Case Rep. 2018 doi: 10.1136/bcr-2018-224388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu S, Zhou L, Song B, et al. Uterine torsion complicated by severe placental abruption in the second trimester: a case report and literature review. BMC Pregnancy Childbirth. 2023;23(1):51. doi: 10.1186/s12884-023-05377-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Omurtag K, Session D, Brahma P, Matlack A, Roberts C. Horizontal uterine torsion in the setting of complete cervical and partial vaginal agenesis: a case report. Fertil Steril. 2009;91(5):1957e13–15. doi: 10.1016/j.fertnstert.2009.01.058. [DOI] [PubMed] [Google Scholar]
- 16.Sikora-Szczęśniak D, Szczęśniak G, Łęgowik T, Sikora W. Torsion of the uterus with myomas in a postmenopausal woman – case study and review of the literature. Prz Menopauzalny. 2014;13(2):145–149. doi: 10.5114/pm.2014.42718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang G, Ishikawa H, Sato A, Shozu M. Torsion of a Large Myomatous Uterus Associated with Progressive Renal Failure and Paralytic Ileus in an 86-Year-Old Woman. Case Rep Obstet Gynecol. 2019 doi: 10.1155/2019/1601368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nagose VB, Sadanandan Rosemary R, Anandrajan RC, Hubert N, Raj R. Torsion of Non-gravid Uterus: A Life-Threatening Condition in a Postmenopausal Lady. J Obstet Gynaecol India. 2020;70(5):393–396. doi: 10.1007/s13224-020-01332-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilde S, Scott-Barrett S. Radiological appearances of uterine fibroids. Indian J Radiol Imaging. 2009;19(3):222–231. doi: 10.4103/0971-3026.54887. [DOI] [PMC free article] [PubMed] [Google Scholar]