Abstract
Health disparities continue to plague racial and ethnic underserved patients in the United States. Disparities extend to the most critically ill patients, including those experiencing neurologic injury and patients at the end of life. Achieving health equity in palliative care in the neurointensive care unit requires clinicians to acknowledge and address structural racism and the social determinants of health. This article highlights racial and ethnic disparities in neurocritical care and palliative care and offers recommendations for an anti-racist approach to palliative care in the neurointensive care unit for clinicians.
Keywords: Equity, Neurocritical care, Palliative care, Disparities, Racism, Social determinants of health
Historical Background of Racial and Ethnic Health Inequities in the United States
Health inequities for racial and ethnic minoritized people in the United States is a public health emergency resulting in significant disparities in outcomes, including among seriously ill patients with neurologic injury who could benefit from palliative care [1, 2]. Our goal as clinicians is to provide high-quality, evidence-based care to all patients. Unfortunately, providing quality clinical care is an insufficient standalone approach to bridge the chasm of health disparities. To achieve health equity, disparities must be understood in the context of structural racism and the social determinants of health (SDOH) [3].
Health behaviors, social and economic factors, and the physical environment are modifiable conditions and environments collectively referred to as SDOH and account for 80–90% of contributors to health outcomes [4, 5]. Racism is a significant driver of differences in SDOH and creates a barrier to achieving health equity because it systematically disadvantages and disempowers racial and ethnic minoritized people.
Mechanistically, racism was and continues to be embedded in US laws and policies that determine access to and the allocation of resources, including health care resources; this is known as structural racism [6].
The impact of structural racism on medicine dates to the nineteenth century and includes the legal, unethical experimentation on enslaved women by Marion Sims [7], the Tuskegee Syphilis Study [8], the experimentation on Black, Puerto Rican, and Asian Soldiers [9], compulsory eugenics [10, 11], and many other injustices in the twentieth century [12]. Concertedly, US policies such as the Hill-Burton Act of 1946, which allowed “separate but equal” health care facilities, operationalized differential care and inequitable access to health care during the Jim Crow era [6]. In clinical practice and research, race was widely considered a biologic construct until 1999 when the Human Genome Project showed no genetic basis for race [13]. As such, decision-making [14] and varying treatment decisions and algorithms [14, 15] inappropriately considered race.
Race is now largely considered a social construct without any biologic influence on health outcomes [16–18]; therefore, clinicians should consider factors such as racism and other SDOH in their approach to addressing health disparities and achieving health equity. Knowing that racial and ethnic minoritized patients will likely experience racism in their health care journey, it is imperative to consider strategies to provide equitable care to our most vulnerable patients—those with serious illness, possibly at the end of life. In this article, we provide a review on disparities in palliative care and neurocritical care and introduce a framework for equitable palliative care in the neurointensive care unit (neuro-ICU).
Racial Disparities in Neurologic Disease Outcomes
Neurology has not been spared from the prevalence of racial disparities [19]. Black patients have disproportionately higher mortality rates from neurological disorders [20] with a widening Black–White patient mortality gap for neurologic diseases between 2011 and 2019 [21]. Among the 15 most common neurologic diseases, including stroke and other cerebrovascular diseases, Black Americans have the highest age-adjusted mortality rates [21]. To compound the disparity, Black patients have poorer access to neurologic care in general [1]. In neurology and neurocritical care, factors rooted in SDOH and influenced by racism contribute to health disparities, including neighborhood and environmental factors, individual-level factors, structural/societal factors, and health care system factors [19]. In the following section, we highlight disparities in outcomes for patients with stroke and traumatic brain injury (TBI), who are commonly cared for in the neuro-ICU, recognizing that disparities in other neurologic disorders are likely similar.
Stroke
Black Americans have a higher incidence of ischemic and hemorrhagic stroke when compared with White Americans [19, 22]. For patients experiencing stroke, several studies reported delayed time to initiation of treatment for Black and Mexican American/Hispanic patients. This may be related to emergency medical services (EMS) utilization, with most studies showing lower EMS utilization rates for racially minoritized patients experiencing stroke symptoms [23]. This may also be related to emergency department wait times. One study reported a longer emergency department wait time for Black patients with a longer emergency department to needle time when compared with White patients [23]. In the treatment of stroke, Black and Hispanic patients are less likely to be transferred to endovascular capable centers or to be evaluated by a stroke team when compared with their White counterparts. In addition, there are lower rates of tissue plasminogen activator (tPA) [23, 24] use and thrombectomy in Black and Hispanic patients [23]. Finally, when assessing outcomes, racially minoritized patients have a longer hospital length of stay [24], more ICU days after thrombectomy [25], and increased likelihood of placement of chronic life-sustaining therapies, such as percutaneous gastrostomy tubes following acute ischemic strokes [26].
TBI
Along the continuum of care from prehospital through rehabilitation, racially and ethnically minoritized patients experience health inequities. Black and Hispanic patients have higher injury severity at presentation [27]. In the acute diagnosis and management of TBI, racially and ethnically minoritized patients experience longer emergency department wait times, have lower triage scores, and have higher rates of leaving the emergency department undiagnosed. Racially and ethnically minoritized patients are also less likely to receive analgesia and different diagnostic procedures and treatments. Hispanic, Asian, and Black veterans are less likely to receive a TBI diagnosis when presenting with positive TBI screens and symptoms [27]. Regarding hospitalization, racially and ethnically minoritized patients have longer lengths of stay; Black patients have a higher odds of experiencing a complication; Black and Hispanic patients with moderate to severe TBI are more likely to have higher in-hospital mortality [27]; and American Indian/Alaska native children and adults have the highest TBI hospitalization and mortality rates [28]. When considering posthospitalization care, Black and Hispanic patients are less likely to receive follow-up care and rehabilitation [27, 28]. When receiving rehabilitation, they are less likely to receive therapies, such as physical therapy, occupational therapy, and speech therapy, and are less likely to receive inpatient rehabilitation, even when adjusting for injury severity [27]. Finally, racially and ethnically minoritized patients are more likely to have poorer psychosocial and functional outcomes after sustaining a TBI [27, 28].
Racial Disparities in Palliative and End-of-Life Care
Racial and ethnic disparities extend to palliative care, end-of-life care (EOLC), and hospice [2, 29]. The primary goals of palliative care services include reducing pain and symptoms, aligning treatment with values, alleviating emotional distress, and providing EOLC (Fig. 1). Unfortunately, Black and Hispanic patients are less likely to receive palliative care services, specifically for patients with intracerebral hemorrhage [30] and ischemic stroke [31]. The consequences of not receiving palliative care resources can result in patients living with more pain and suffering, discordant goals, and worse end-of-life experiences [30, 32].
Fig. 1.
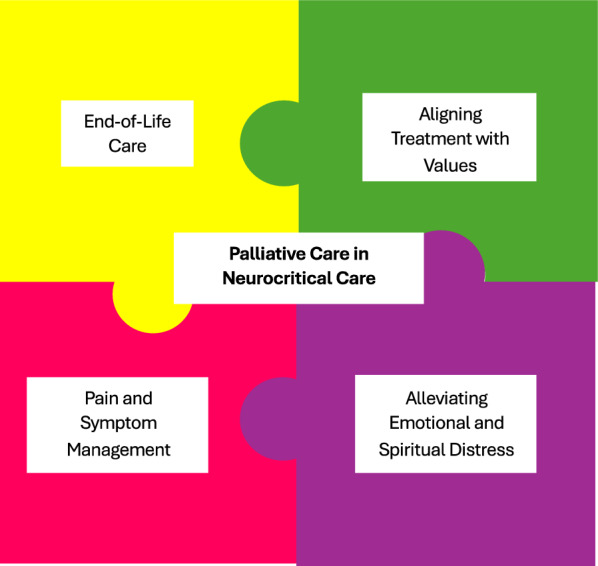
The role of palliative care in neurocritical care
Pain and Symptom Management
Decades of research have shown that Black and Hispanic patients receive less pain medications compared with White patients [33–36]. Although not specific to neurocritical care, racially and ethnically minoritized patients are more likely to experience lower quality palliative pain care [30], with Black patients feeling their reports of pain are not believed [37]. More specifically, racial and ethnic minority patients receive less comprehensive diagnostic and treatment approaches for pain and are less likely to receive opioid medications for pain across indications and treatment settings [37, 38]. In addition, racially minoritized patients are more likely to be asked about drug use, receive drug testing, and have opioids withheld when controlling for factors such as previous drug use, symptoms on presentation, and diagnosis [33].
Aligning Treatment with Values
Racially and ethnically minoritized patients experience lower quality of dying and death [39]. Black patients are less likely to receive goals-of-care conversations [30] or be offered an opportunity to complete an advance directive [40]. Even when advance care planning is completed, end-of-life preferences are documented closer to the patient’s death [40] and are less likely to be honored at the end of life [41]. When Black patients express a preference for life-extending EOLC, their preferences are three times less likely to be honored than White patients. Patient preference is also not honored when a do-not-resuscitate order is in place [41, 42]. Similarly, in assessing family conference documentation, clinicians are more likely to recommend withdrawal of life-sustaining therapies for racial and ethnic minority patients [43].
Alleviating Emotional Distress
Conversations with patients and families with serious neurologic injuries are filled with emotions. Families are grappling with the loss of their loved one as they knew them if they can no longer speak, or have dementia-related memory issues or emotional dysregulation. Clinicians need to be able to recognize these emotions and respond with empathy. Studies show that Black patients are less likely to reveal spontaneous emotions [44] and when they do, clinicians are less likely to address emotional issues or respond with empathy [45, 46].
In addition to emotional support, spiritual support is essential to holistic palliative care. Patients often turn to religion when coping with serious illness [47]. For Black patients, a lack of trust in a health care system that has been untrustworthy increases the reliance on spirituality to guide decision-making [48]. The church is often viewed as a trusted source for health care knowledge, support, and guidance [48, 49], yet clinicians refrain from discussing spirituality with patients [50]. This failure to engage in spiritual discussions leaves patients and families feeling unsupported and further erodes trust.
EOLC
Life-prolonging therapies and dying with full support are associated with lower quality of dying and death [39], yet racial and ethnic minority patients are more likely to prefer life-sustaining therapies [29, 40]. This disparity may be due to preferences, but it also may be impacted by racial and ethnic minority patients’ access to palliative and hospice services. Racially and ethnically minoritized patients are more likely to have a delay in hospice referral [30] and are less likely to use hospice benefits [51]. Black and Hispanic patients are less likely to die at home or in a nursing home rather than in the hospital when compared with their White counterparts [40]. When considering overall hospital utilization at the end of life, Black patients are more likely to have multiple emergency department visits and hospitalizations and undergo intensive treatment in the last 6 months of life when compared with White decedents [52]. Black and Hispanic patients are also more likely to be exposed to the use of life support or use of dialysis before death compared with White patients [40].
Palliative Care in the Neuro-ICU
Studies show an association between early integration of palliative care into the ICU and improved outcomes, yet there are limited data on best practices for integrating palliative care into the neuro-ICU [53]. Given the difficulty with early prognostication in the setting of neurologic injury and decreased capacity-making of patients experiencing neurologic injury, early integration of palliative care may be helpful [53, 54]. A few studies identify and highlight palliative care needs or indications in the neuro-ICU, including (1) family emotional support and (2) setting goals of care [53, 55, 56]. Recommendations from the Improving Palliative Care in the ICU Project Advisory Board and the Center to Advance Palliative Care provided a framework to aid clinicians in addressing decision-making around goals of care. The framework includes input from the clinician, with consideration of prognosis using prognostic scores and individual patient factors, and patient/family input, which centers the patient’s values, preferences, and advance directive [54].
Sadly, the literature shows us that racially and ethnically minoritized patients face challenges with engagement of palliative care, and with disparities in access, uptake, and implementation of palliative care services. We also know these same patients are more likely to experience disparities in care after sustaining serious neurologic injury. The intersection of increased need and decreased interface with palliative care services heightens the need for clinicians to provide culturally sensitive, equitable care to these vulnerable patients. In the next section we offer recommendations for a multifaceted anti-racist approach to achieve health equity. These are recommendations clinicians can implement with all patients but are particularly important for historically marginalized patients for whom dignity and respect are often denied during their health care journey.
An Anti-racist Approach to Palliative Care in the Neuro-ICU
Anti-racism is an active approach that seeks to identify and eliminate racist systems and practices [1]. Applying an anti-racist approach to clinical practice in the neuro-ICU is the responsibility of all clinicians practicing in the neuro-ICU. We know bias and racism exist in each of these components as, described previously. In the following section, we offer strategies clinicians can use to meet the goals of palliative care using an anti-racist approach (Table 1).
Table 1.
A roadmap for an anti-racist approach to palliative care in the neurointensive care unit
| Actionable approach | Associated tenet of palliative care | |
|---|---|---|
| Affirm narratives |
Acknowledge the impact of racism and its contributions to medical mistrust Use high-quality communication skills (actively listen, ask open-ended questions, provide empathetic responses) |
Reduce pain and symptoms Align treatment with values Alleviate emotional distress |
| Lead with empathy and dignity |
Restore dignity Make eye contact Use open body language |
Alleviate emotional distress |
| Honor values |
Assess the patient’s values and goals Align treatment plans with the patient’s values and goals Engage family early in decision-making |
Reduce pain and symptoms Alleviate emotional distress Align treatment with values Provide end-of-life care |
| Practice cultural humility |
Acknowledge biases Self-reflect and be aware of your own identity and how it may differ from others’ |
Provide end-of-life care Alleviate emotional distress |
Affirm Narratives
An overwhelming body of literature confirms the pervasive pattern of dismissal of racially and ethnically minoritized patient’s concerns when they report pain or share their story with clinicians [57–61]. In addition, racially and ethnically minoritized patients report worse communication with their physicians [62]. Paralleling this data, for patients with severe acute brain injury, family members of racially and ethnically minoritized patients have a higher odds ratio of prognostic discordance with their physician [63].
Patient–clinician communication impacts trust, adherence, disease outcomes, and mortality [64]. To improve outcomes, clinicians must invest in the patient–clinician relationship [65]. This begins with acknowledging the impact of racism and its contributions to medical mistrust for racially and ethnically minoritized patients. To accomplish this feat without causing harm, clinicians should employ high-quality communication skills, in which active listening takes center stage. Patients and families need to feel heard and believed. Clinicians should ask open-ended questions, provide space for emotions, and offer empathetic responses. These important communication skills can be learned, and compassionate clinicians must invest in their professional development to strengthen these skills [66]. Patients remember what we say and how we make them feel. It is our job to listen to their truth and empathize with their experience.
Lead with Empathy and Dignity
Black patients have experienced significant indignities within the medical community, including medical exploitation for research and medical maltreatment. Furthermore, they experience microaggressions in their day-to-day life. Minoritized patients have described clinicians not willing to touch them or to learn about them as people. Restoring dignity can be an important step in lessening the normalized disrespect minoritized patients experience. Restoring dignity can include greeting Black patients by saying “Good morning,” asking permission to engage and touch, and using surnames when addressing minoritized patients [2]. In addition, clinicians should make eye contact and use open body language; these nonverbal cues can aid in establishing rapport [67] and improve the interpretation of verbal communication [59].
Honor Values
A larger percentage of Black and Hispanic patients report never having their preferences considered by health care clinicians when compared with White adults [68]. Clinicians not only need to assess the patient’s values and preferences, but they should incorporate these dynamics into their treatment plan and include the patient’s family early in the decision-making [65]. The desire for more therapies at the end of life is rooted in mistrust in a system that has withheld treatments from minoritized patients. Minoritized patients carry that weight with them and need trusting caregivers who truly see them and listen to their story to be able to agree to less therapies. This means that clinicians may need to support life-sustaining therapies if it aligns with the patient’s overall goals, even if they do not align with our own values and preferences as clinicians.
Practice Cultural Humility
As humans, our experiences, culture, and background shape the lens in which we navigate the world. Practicing with cultural humility acknowledges that our patients also have a complex background that shapes their approach to medical decision-making, which may differ from our own identity. Cultural humility is an iterative process that requires continual refinement and an exploration and awareness of each patient’s lived experience. It also includes recognizing how racism and its sequalae shape individual preferences [37]. Employing cultural humility requires empathy, active listening, acknowledgment of biases, and self-reflection and awareness. To achieve equity in palliative care in the neuro-ICU, clinicians must embrace cultural humility in their approach to patient care, especially when assessing the values of patients and aligning a care plan with their goals and preferences.
Conclusions
Evidence documents disparities in neurologic outcomes and in palliative care and EOLC for racially and ethnically minoritized patients. Practicing medicine without an appreciation for and an active attempt to dismantle the systems that lead to disparate health outcomes can no longer be considered providing quality care. Applying an anti-racist approach to caring for the most clinically and socially vulnerable patients experiencing serious neurologic illness acknowledges the pervasive nature of racism in medicine and brings us closer to achieving equity.
Author Contributions
This manuscript complies with all instructions to authors and all authorship requirements have been met. Dr. Paula M. Magee contributed to the conception of the manuscript, wrote the draft manuscript, and critically reviewed the manuscript. Dr. Tessie W. October contributed to the conception of the manuscript, contributed to and edited the draft manuscript, and critically reviewed the manuscript. The final manuscript was approved by all authors.
Source of Support
There was no funding source for this article.
Conflicts of interest
Dr. Magee has no Conflicts of Interests disclosures. Dr. October is a government employee at the National Institutes of Health.
Ethical Approval/Informed Consent
Ethical guidelines have been reviewed and Institutional Review Board approval was not required because this was not a research article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Robbins NM, Charleston L 4th, Saadi A, Thayer Z, Codrington WU 3rd, Landry A, et al. Black patients matter in neurology: race, racism, and race-based neurodisparities. Neurology. 2022;99(3):106–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rosa W, Gray T, Chambers B, et al. Palliative care in the face of racism: a call to transform clinical practice, research, policy, and leadership. Health Aff Forefr. 2022. 10.1377/forefront.20220207.574426. [Google Scholar]
- 3.Akande M, Paquette ET, Magee P, Perry-Eaddy MA, Fink EL, Slain KN. Screening for social determinants of health in the pediatric intensive care unit: recommendations for clinicians. Crit Care Clin. 2023;39(2):341–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.U.S. Department of Health and Human Services. Social Determinants of Health. Healthy People 2030. 2020. https://health.gov/healthypeople/priority-areas/social-determinants-health.
- 5.Magnan S. Social determinants of health 101 for health care: five plus five. NAM Perspect. 2017. 10.31478/201710c. [Google Scholar]
- 6.Yearby R, Clark B, Figueroa JF. Structural racism in historical and modern US health care policy. Health Aff (Millwood). 2022;41(2):187–94. [DOI] [PubMed] [Google Scholar]
- 7.Holland B. The “Father of Modern Gynecology” performed shocking experiments on slaves. History.com. Published December 4, 2018. https://www.history.com/news/the-father-of-modern-gynecology-performed-shocking-experiments-on-slaves.
- 8.Centers for Disease Control and Prevention. The untreated syphilis study at Tuskegee timeline. Centers for disease control and prevention. Published December 5, 2022. https://www.cdc.gov/tuskegee/timeline.htm.
- 9.PBS NewsHour. Why the U.S. military exposed minority soldiers to toxic mustard gas. PBS NewsHour. Published June 22, 2015. Accessed 12 Jan 2024. https://www.pbs.org/newshour/show/u-s-military-exposed-minority-soldiers-toxic-mustard-gas#.
- 10.Nuriddin A, Mooney G, White AI. Reckoning with histories of medical racism and violence in the USA. Lancet. 2020;396(10256):949–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Human Genome Research Institute. Eugenics and Scientific Racism. Genome.gov. Published May 18, 2022. https://www.genome.gov/about-genomics/fact-sheets/Eugenics-and-Scientific-Racism.
- 12.Washington HA. Medical apartheid: the dark history of medical experimentation on Black Americans from colonial times to the present. Paw Prints; 2010.
- 13.Mersha TB, Beck AF. The social, economic, political, and genetic value of race and ethnicity in 2020. Hum Genomics. 2020;14(1):37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tong M, Artiga S. Use of race in clinical diagnosis and decision making: overview and implications. KFF. Published December 9, 2021. https://www.kff.org/racial-equity-and-health-policy/issue-brief/use-of-race-in-clinical-diagnosis-and-decision-making-overview-and-implications/.
- 15.Hall WD. A rational approach to the treatment of hypertension in special populations. Am Fam Phys. 1999;60(1):156–62. [PubMed] [Google Scholar]
- 16.AAFP. Race Based Medicine. www.aafp.org. Published July 2020. https://www.aafp.org/about/policies/all/racebased-medicine.html
- 17.American Medical Association. New AMA policies recognize race as a social, not biological, construct. American Medical Association. Published November 16, 2020. https://www.ama-assn.org/press-center/press-releases/new-ama-policies-recognize-race-social-not-biological-construct.
- 18.American Academy of Pediatrics Board of Directors and Executive Committee. AAP perspective: race-based medicine. Pediatrics. 2021;148(4):e2021053829. [DOI] [PubMed]
- 19.Perez MA, Reyes-Esteves S, Mendizabal A. Racial and ethnic disparities in neurological care in the United States. Semin Neurol. 2024;44(2):178–92. [DOI] [PubMed] [Google Scholar]
- 20.Johnston KC, Trevathan E. NINDS health equity strategic planning process overview, high-level recommendations, and guide. Neurology. 2023;101(7 Suppl 1):S1-8. [DOI] [PubMed] [Google Scholar]
- 21.Woolf SH, Chapman DA, Lee JH, Johnston KC, Benson RT, Trevathan E, et al. The lives lost to inequities: avertable deaths from neurologic diseases in the past decade. Neurology. 2023;101(7 Suppl 1):S9-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Office of Minority Health. Stroke and African Americans | Office of Minority Health. minorityhealth.hhs.gov. Published 2022. Accessed January 12, 2024. https://minorityhealth.hhs.gov/stroke-and-african-americans.
- 23.Ikeme S, Kottenmeier E, Uzochukwu G, Brinjikji W. Evidence-based disparities in stroke care metrics and outcomes in the United States: a systematic review. Stroke. 2022;53(3):670–9. [DOI] [PubMed] [Google Scholar]
- 24.Metcalf D, Zhang D. Racial and ethnic disparities in the usage and outcomes of ischemic stroke treatment in the United States. J Stroke Cerebrovasc Dis. 2023;32(12):107393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thirunavu V, Abdalla R, Cantrell D, Hurley M, Shaibani A, Jahromi B, et al. LB-001 Racial disparities in acute stroke thrombectomy management and outcomes in the United States: evidence from the NVQI-QOD registry. J Neurointerv Surg. 2020;12(Suppl 1):A160. [Google Scholar]
- 26.George BP, Kelly AG, Schneider EB, Holloway RG. Current practices in feeding tube placement for US acute ischemic stroke inpatients. Neurology. 2014;83(10):874–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Saadi A, Bannon S, Watson E, Vranceanu AM. Racial and ethnic disparities associated with traumatic brain injury across the continuum of care: a narrative review and directions for future research. J Racial Ethn Health Disparities. 2022;9(3):786–99. [DOI] [PubMed] [Google Scholar]
- 28.Centers for Disease Control and Prevention. Health Disparities and TBI | Concussion | Traumatic Brain Injury | CDC Injury Center. www.cdc.gov. Published October 19, 2023. Accessed 8 Jan 2024. https://www.cdc.gov/traumaticbraininjury/health-disparities-tbi.html.
- 29.Jones T, Luth EA, Lin SY, Brody AA. Advance care planning, palliative care, and end-of-life care interventions for racial and ethnic underrepresented groups: a systematic review. J Pain Symptom Manag. 2021;62(3):e248–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bazargan M, Bazargan-Hejazi S. Disparities in Palliative and hospice care and completion of advance care planning and directives among non-hispanic blacks: a scoping review of recent literature. Am J Hosp Palliat Care. 2021;38(6):688–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khan MZ, Zahid S, Kichloo A, Jamal S, Minhas AM, Khan MU, et al. Gender, racial, ethnic and socioeconomic disparities in palliative care encounters in ischemic strokes admissions. Cardiovasc Revasc Med. 2022;35:147–54. [DOI] [PubMed] [Google Scholar]
- 32.Center to Advance Palliative Care. Health Care for Black Patients with Serious Illness. www.capc.org. Published August 2021. Accessed 13 Feb 2024. https://www.capc.org/health-care-for-black-patients-with-serious-illness-a-literature-review/.
- 33.Enzinger AC, Ghosh K, Keating NL, Cutler DM, Clark CR, Florez N, et al. Racial and ethnic disparities in opioid access and urine drug screening among older patients with poor-prognosis cancer near the end of life. J Clin Oncol. 2023;41(14):2511–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rencsok EM, Slopen N, McManus HD, Autio KA, Morgans AK, McSwain L, et al.; IRONMAN Registry. Pain and its association with survival for black and white individuals with advanced prostate cancer in the United States. Cancer Res Commun. 2024;4(1):55–64. [DOI] [PMC free article] [PubMed]
- 35.Schoenthaler A, Williams N. looking beneath the surface: racial bias in the treatment and management of pain. JAMA Netw Open. 2022;5(6):e2216281. [DOI] [PubMed] [Google Scholar]
- 36.Hoffman KM, Trawalter S, Axt JR, Oliver MN. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proc Natl Acad Sci USA. 2016;113(16):4296–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jones KF, Laury E, Sanders JJ, Starr LT, Rosa WE, Booker SQ, et al. Top ten tips palliative care clinicians should know about delivering antiracist care to black Americans. J Palliat Med. 2022;25(3):479–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Meints SM, Cortes A, Morais CA, Edwards RR. Racial and ethnic differences in the experience and treatment of noncancer pain. Pain Manag (Lond). 2019;9(3):317–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee JJ, Long AC, Curtis JR, Engelberg RA. The influence of race/ethnicity and education on family ratings of the quality of dying in the ICU. J Pain Symptom Manag. 2016;51(1):9–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Orlovic M, Smith K, Mossialos E. Racial and ethnic differences in end-of-life care in the United States: evidence from the Health and Retirement Study (HRS). SSM Popul Health. 2018;7:100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mack JW, Paulk ME, Viswanath K, Prigerson HG. Racial disparities in the outcomes of communication on medical care received near death. Arch Intern Med. 2010;170(17):1533–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Loggers ET, Maciejewski PK, Paulk E, DeSanto-Madeya S, Nilsson M, Viswanath K, et al. Racial differences in predictors of intensive end-of-life care in patients with advanced cancer. J Clin Oncol. 2009;27(33):5559–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Muni S, Engelberg RA, Treece PD, Dotolo D, Curtis JR. The influence of race/ethnicity and socioeconomic status on end-of-life care in the ICU. Chest. 2011;139(5):1025–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Park J, Beach MC, Han D, Moore RD, Korthuis PT, Saha S. Racial disparities in clinician responses to patient emotions. Patient Educ Couns. 2020;103(9):1736–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.You H, Ma JE, Haverfield MC, Oyesanya TO, Docherty SL, Johnson KS, et al. Racial differences in physicians’ shared decision-making behaviors during intensive care unit family meetings. Ann Am Thorac Soc. 2023;20(5):759–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ashana DC, Welsh W, Preiss D, Sperling J, You H, Tu K, et al. Racial differences in shared decision-making about critical illness. JAMA Intern Med. 2024;184(4):424–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Best MC, Vivat B, Gijsberts MJ. Spiritual care in palliative care. Religions (Basel). 2023;14(3):320. [Google Scholar]
- 48.Siler S, Arora K, Doyon K, Fischer SM. Spirituality and the illness experience: perspectives of African American older adults. Am J Hosp Palliat Care. 2021;38(6):618–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Coats HL. African American elders’ psychological-social-spiritual cultural experiences across serious illness: an integrative literature review through a palliative care lens. Ann Palliat Med. 2017;6(3):253–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gradick K, October T, Pascoe D, Fleming J, Moore D. “I’m praying for a miracle”: characteristics of spiritual statements in paediatric intensive care unit care conferences. BMJ Support Palliat Care. 2020;12(e5):bmjspcare-2020–002436. 10.1136/bmjspcare-2020-002436. [DOI] [PubMed]
- 51.National Hospice and Palliative Care Organization. NHPCO Facts and Figures 2023 Edition. 2023. Accessed 8 Jan 2024. https://www.nhpco.org/wp-content/uploads/NHPCO-Facts-Figures-2023.pdf.
- 52.Ornstein KA, Roth DL, Huang J, Levitan EB, Rhodes JD, Fabius CD, et al. Evaluation of racial disparities in hospice use and end-of-life treatment intensity in the REGARDS Cohort. JAMA Netw Open. 2020;3(8):e2014639-2014639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tran LN, Back AL, Creutzfeldt CJ. Palliative care consultations in the neuro-ICU: a qualitative study. Neurocrit Care. 2016;25(2):266–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Frontera JA, Curtis JR, Nelson JE, Campbell M, Gabriel M, Mosenthal AC, et al. Integrating palliative care into the care of neurocritically ill patients: a report from the IPAL-ICU (improving palliative care in the intensive care unit) project advisory board and the center to advance palliative care. Crit Care Med. 2015;43(9):1964–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bar B, Creutzfeldt CJ, Rubin MA. Palliative care in the neuro-ICU: perceptions, practice patterns, and preferences of neurointensivists. Neurocrit Care. 2020;32(1):302–5. [DOI] [PubMed] [Google Scholar]
- 56.Creutzfeldt CJ, Engelberg RA, Healey L, Cheever CS, Becker KJ, Holloway RG, et al. Palliative care needs in the neuro-ICU. Crit Care Med. 2015;43(8):1677–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Stafford K. Medical Racism: Why Maternal Mortality Is Higher for Black Women. NBC10 Philadelphia. Published online May 23, 2023. https://www.nbcphiladelphia.com/news/national-international/why-do-so-many-black-women-die-in-pregnancy-one-reason-doctors-dont-take-them-seriously/3571702/.
- 58.Sakala C, Declercq E, Turon J, Corry M. Listening to mothers in California. 2018. https://www.chcf.org/wp-content/uploads/2018/09/ListeningMothersCAFullSurveyReport2018.pdf.
- 59.The New York State Department of Health. Voice your vision—share your birth story a conversation on maternal health in New York State. New York State Department of Health. Published 2018. Accessed 12 Jan 2024. https://www.health.ny.gov/community/adults/women/task_force_maternal_mortality/docs/listening_session_report.pdf.
- 60.Artiga S, Hamel L, Gonzalez-Barrera A, et al. Survey on racism, discrimination and health—findings—10257. KFF. Published December 5, 2023. https://www.kff.org/report-section/survey-on-racism-discrimination-and-health-findings/.
- 61.Funk C. Black Americans’ views about health disparities, experiences with health care. Pew Research Center Science & Society. Published April 7, 2022. https://www.pewresearch.org/science/2022/04/07/black-americans-views-about-health-disparities-experiences-with-health-care/.
- 62.Elliott AM, Alexander SC, Mescher CA, Mohan D, Barnato AE. Differences in physicians’ verbal and nonverbal communication with black and white patients at the end of life. J Pain Symptom Manag. 2016;51(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Muehlschlegel S. When doctors and families disagree in the neurologic intensive care unit-misunderstandings and optimistic beliefs. JAMA Netw Open. 2021;4(10):e2129079. [DOI] [PubMed] [Google Scholar]
- 64.Street RL Jr, Makoul G, Arora NK, Epstein RM. How does communication heal? Pathways linking clinician-patient communication to health outcomes. Patient Educ Couns. 2009;74(3):295–301. [DOI] [PubMed] [Google Scholar]
- 65.Dierfeldt D, Knopf K, Jackson L. Racial disparities at the end of life. Am Fam Phys. 2021;104(4):346–7. [PubMed] [Google Scholar]
- 66.Berns S, Hurd C, Carl J, Roshal A, Lindenberger E. Practice makes permanent: VitalTalk techniques for drilling communication skills (FR482F). J Pain Symptom Manag. 2016;51(2):385. [Google Scholar]
- 67.Harrigan JA, Oxman TE, Rosenthal R. Rapport expressed through nonverbal behavior. J Nonverbal Behav. 1985;9(2):95–110. [Google Scholar]
- 68.Center for Consumer Engagement in health innovation. The state of person-centered care: 2014–2018. Center for consumer engagement in health innovation. Published March 22, 2022. Accessed 22 Jan 2024. https://www.healthinnovation.org/resources/publications/tracking-progress-on-person-centered-care-for-older-adults-how-are-we-doing.


