Abstract
Background
The incidence of airborne respiratory infections fell as a result of the protective measures taken during the COVID-19 pandemic and rose again when these were stopped. In 2022, there was a notable rise in invasive group A streptococcal (iGAS) infections in many countries, including Germany. This rise was also reflected in the data of the university otorhinolaryngology department in Ulm, Germany.
Methods
This review is based on publications retrieved by a selective literature search on the rise of iGAS infections in Europe, with particular attention to the timing of disease onset, clinical presentation, pathogenic strains, and potential causes and risk factors.
Results
The rise in infections after the pandemic was especially marked among children up to age 10 and in older adults; in Germany, it affected all age groups equally, but predominantly persons older than 65. Rising prevalence figures were seen in Germany and elsewhere as early as the fall of 2022, outside the usual season, and peaked mainly in the first and second quarters of 2023. The increased incidence of iGAS-associated pneumonia was paralleled by that of viral airway infections and led to greater use of intensive-care measures for children. The main bacterial strain identified was emm1; a new variant (M1DK) played a role in Denmark, and an emm4 variant (M4NL22) became increasingly important in the Netherlands. In Germany, initial evidence suggested the predominance of M1UK. Increased antibiotic resistance was not found.
Conclusion
The reduced confrontation of the immune system with pathogens during the pandemic, along with the increased incidence of viral airway infections immediately after it, apparently accounted for the exceptionally high post-pandemic rise in iGAS infections and the increase in invasive pulmonary diseases in Europe. Consistent vaccination programs against coincident respiratory viruses could reduce the burden of iGAS infections. The further extension of multinational surveillance programs with obligatory participation could aid in the detection of factors affecting the course of disease and the spread of new bacterial strains.
CME plus+
This article has been recognized by the Medical Association North Rhine for the Medical Association‘s CME certificate. The CME questions on this article can be found at http://daebl.de/RY95.
The deadline for submission is 3 October 2025.
Participation is possible at cme.aerztebatt.de
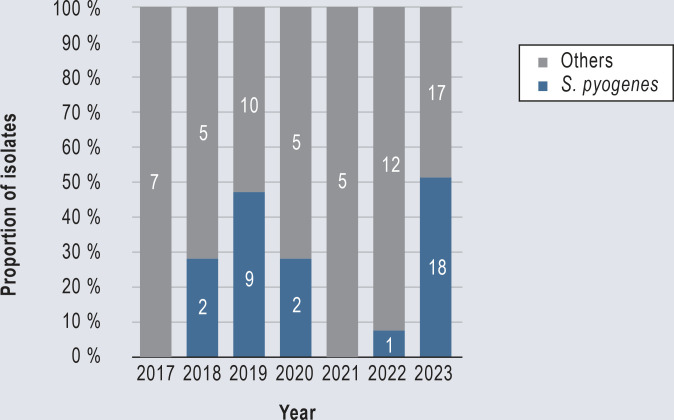
In early December 2022, the UK reported a particularly high and early incidence of infections with invasive group A streptococci in children (iGAS) and older adults compared with the years before the COVID-19 pandemic (1). At almost exactly the same time, the European Centre for Disease Control and Prevention (ECDC) and the World Health Organization (WHO) warned of an increase in iGAS infections in several European countries (2, 3). In the university otorhinolaryngology department in Ulm, Germany, which looks after patients from a catchment area of around 100 km diameter (about 3.5 million population), a rapid increase in cases of mastoiditis was observed, primarily caused by Streptococcus pyogenes (group A streptococci, GAS) (Figure, eFigure). Such infections were especially marked in children. In Germany, an increase in iGAS cases was observed in all age groups but older people were predominantly affected (4). The national reference center for streptococci did not see any association with the emergence of a new bacterial strain (4).
Figure.
Isolates of causative pathogens in acute mastoiditis, Department for Diseases of Ear, Nose and Throat medicine, head and neck surgery, of the University Hospital Ulm, 2017–2023
eFigure.
Proportion of pathogenic isolates in acute mastoiditis of the total number of cases per year, Department for Diseases of Ear, Nose and Throat medicine, head and neck surgery, of the University Hospital Ulm, 2017–2023
Case fatality rates of iGAS infections vary depending on the geographical location, income per head, and clinical symptoms: in industrialized countries they were between 5% and 23% and in countries in the global South between 3% and 50% (5). Socioeconomic factors and a genetic predisposition seem to have an influence on the development of invasive group A streptococcal disease (e1). The international increase in iGAS infections was the more important because beforehand, when pandemic measures were established in early 2020, a substantial fall was observed in viral and bacterial disorders transmitted by the respi ratory route, including iGAS infections (6–9). Different host related and pathogen related factors have been discussed as triggers. Box 1 and eBox 1 provide a brief overview of GAS and the virulence factors that are responsible for the development of invasive infections.
Box 1. Profile: group A streptococci (GAS)* (5, 26, 30, 36, e2, e3, e7–e17).
Gram positive coccal bacteria of Lancefield Group A
Main representative: Streptococcus pyogenes
-
Epidemiology of GAS infections:
High incidence and mortality in the 19th century, declining incidence in the beginning of the 20th century, continually rising incidence since the 1980s
Incidence of invasive infections in industrialized countries: 2–4/100 000 population
Case fatality rate of invasive infections in industrialized countries: 5–23%.
Periodic peaks with clusters of infection every 4–7 years
Increases in winter and spring months
-
Clinical symptoms:
Asymptomatic colonization of the nasopharynx and skin
Frequently: non-invasive disease: tonsillopharyngitis, impetigo
Rarely: invasive disease: phlegmons, necrotizing fasciitis, necrotizing pneumonias, meningitis, sepsis, scarlet fever (toxin mediated), streptococcal toxic shock syndrome (toxin mediated)
Secondary diseases: acute poststreptococcal glomerulonephritis, acute rheumatic fever
-
Risk factors developing invasive disease:
Older persons with underlying diseases, children < 10 years
Infection with Varicella zoster virus
Infections with respiratory viruses, particularly influenza viruses
-
Important virulence factors:
Surface protein, such as M protein (cell adhesion, reduced phagocytosis, inflammatory reaction)
Secreted toxins, among others superantigenes
Typing by surface M proteins (> 220 emm genotypes)
Dominant strains in Europe: emm1, emm3, emm12, emm28, emm89
* More detailed information about GAS is in eBox 1.
eBox 1. Group A streptococci (GAS) and virulence factors.
• Klinisches Erscheinungsbild
S. pyogenes is a gram positive coccus and—based on specific lipoteichoic acid and polysaccharide antigens in its cellular wall—is the main representative of Lancefield group A (e7). The bacterium can asymptomatically colonize mucosa and skin, but it can also cause several diseases of different degrees of severity. In addition to the most common non-invasive diseases, such as tonsillopharyngitis and contagious impetigo, GAS is also responsible for life threatening invasive infections, such as necrotizing fasciitis, necrotizing pneumonia, meningitis, sepsis, and the toxin mediated diseases scarlet fever and streptococcal toxic shock syndrome (STSS) (e8, e9). Cutaneous infections and sepsis are the most common manifestations (e8, e10). Furthermore, recurrent infections with GAS can trigger autoimmune reactions and cause secondary diseases such as acute post-streptococcal glomerulonephritis and acute rheumatic fever (e8). The association between GAS infections and the development of a pediatric autoimmune neuropsychiatric disorder (pediatric autoimmune neuropsychiatric disorders associated with streptococcal infection, PANDAS) is the subject of controversy in the literature (e8).
While in the 19th century, GAS infections were associated with very high morbidity and mortality (e11), the incidence fell drastically at the beginning of the 20th century, even before antibiotics were discovered; the likely reason being improved living conditions and diets (5, e11). Since the 1980s a continual increase in iGAS infections has been observed in Europe, with periodic peaks in the winter and spring months; this increase is being attributed—among others—to the emergence and selection of new, genetically modified GAS strains (25, 29, e2, e3, e10, e12, e13). But other phenomena, such as improved diagnostics and surveillance, probably also have a role in this context.
Older people with underlying diseases are markedly affected (5, e14), whereas in pediatric collectives it affects primarily children younger than 10 years (e10). The case fatality rate of GAS infection in Europe is between 2% and 80%, depending on the disease symptoms and collective (e8, e10). It is notably lower in children than in adults (10). Treatment in intensive care is on average more common in younger children (21–83 months, Ø 40 months) than in older ones (36–85 months, Ø 57 months) (e10). In addition to host related factors, complex virulence mechanisms, such as surface proteins and secreted toxin, are responsible for the wide range of clinical manifestations (e15). The release of extracellular toxins—so called superantigens—activates T-lymphocytes antigen-independently and thus effects the excess secretion of pro-inflammatory cytokines, with resultant tissue destruction and organ failure (e15).
• M-protein
M protein is a surface protein of relevance for cell adhesion, preventing phagocytosis, and inducing the inflammatory response (e9, e16). It is used to type clinical isolates for epidemiologic purposes. In the meantime more than 200 emm genotypes have been detected by molecular analysis (36, e15). In Europe, emm1, emm3, emm12, emm28, and emm89 dominate, but regional differences are relevant (35, e7). Some M types are more commonly presumed to be associated with certain clinical presentations and epidemiologic phenomena (e9). During the course of epidemics, in the past molecular changes were a regular occurrence within a strain, which enabled the development of highly virulent clones (e3). This also possibly explains the infection peaks that are being observed every 4–7 years (e33). One M strain that gained relevance over the past decade in Europe, is M1UK. It was detected for the first time in 2010 in nGAS infections and in 2012 in iGAS infections in the UK and is characterized by a particularly high production of the superantigen SpeA (e17).
• Antimicrobial treatment
In contrast to other streptococci, GAS are fully susceptible to penicillins; these are administered as the treatment of choice (e18). Individual cases of limited penicillin susceptibility have been described primarily outside Europe (e18). In treating iGAS the combination with clindamycin improves survival (e19). Macrolides constitute an alternative in the setting of penicillin allergy; their resistance rates vary drastically by country and they should therefore be administered for monotherapy in iGAS infections only after resistance testing (28).
Methods
We carried out a selective literature search in PubMed, regarding the increase in iGAS infections at the end of the COVID-19 pandemic from January 2022 compared with pre-pandemic years. We searched primarily for national surveillance data from European countries and for large prospective and retrospective studies that wherever pos sible included all age groups and an analysis of the causative bacterial strains. We did not include case reports and case series from individual hospitals. Since postpandemic data for Germany are largely lacking to date, we included prepandemic publications on the epidemiology of iGAS infections.
The epidemiologic situation in Europe 2022/2023
We analyzed 13 studies from six countries (Table) (10–22). The data were collected mainly through compulsory or voluntary surveillance programs (10, 11, 13–15, 17, 20, 21) and partly by different laboratories or hospitals/clinics joining forces (12, 16, 19, 22).
Table. Overview of evaluated publications on the increase in invasive Group A streptococcal-infections in Europe in 2022/2023.
| Country | Literature citations | Data course/study format | Time period of increase | Comparison period | Age of study collective | Dominant clinical presentation | M classification | Virus association | Case fatality |
| Netherlands | de Gier B. et al., 2023 (11); Rapid Communication | National surveillance data | 01/2022– 12/2022 | 01/2016– 12/2019 | All age groups | Necrotising fasciitis, puerperal fever/-sepsis, STSS | emm1, 4, 12, 22, 98 (> 80%) | VZV | 9/42 (21%) children up to 5 years of age (2022) |
| van Kempen AB. et al., 2023 (18); Brief Report | Multicenter study (7 hospitals) | 07/2021– 06/2022 | 01/2018– 12/2019 | 0–18 years | Pneumonia with empyema, necrotizing fasciitis |
emm12 (38%) emm1 (25%) emm4 (13%) |
VZV (33%), IV (18%) |
9% | |
| van der Putten BCL. et al., 2023 (19); Short Communication | Nationwide data from different studies | 01/2022– 05/2022 | 01/2009– 12/2019 | All age groups | N/A | 100% emm4; M4NL22 (85%) |
N/A | N/A | |
| van der Putten BCL. et al., 2023 (20); Original Article | National surveillance data | 01/2022– 03/2023 | 01/2013– 12/2021 | All age groups | Meningitis |
emm1 (86%) 5/2022–03/2023: emm1UK (100%) |
N/A | N/A | |
| UK | Guy R. et al., 2023 (21); Rapid Communication | National surveillance data | 09/2022– 11/2022 | 01/2017– 09/2022 | All age groups | N/A |
> 14 years: emm 1 (31%) emm 12 (16%) emm 89 (6%) emm 33 (5%) < 15 years: emm 1 (57%) emm 12 (23%) emm 4 (7%) |
RSV > hMPV RV (25.8%) |
14/202 (6.9%) children < 15 years |
| Davies PJB. et al., 2023 (22); Dispatch | Nationale public health and laboratory data from central Scotland | 12/2022– 02/2023 | 12/2017– 11/2022 | > 17 years | Invasive pulmonary infections | emm1/M1UK (96%) | IV A (57.6%) | 6/36 (16%) | |
| Holdstock V. et al., 2023 (12); Correspondence | Clinical data and lab data from three maximum care hospitals in Scotland | 09/2022– 12/2022 | 01/2017– 12/2021 (excl 2020) | 0–15 years | Pleural empyema |
emm1 (75%) emm12 (12,5%) emm1.25 (12,5%) |
60% (hMPV > RSV > IV A/RV/VZV) |
0% | |
| Denmark | Johannesen TB. et al., 2023 (10); Rapid Communication | National surveillance data | 01/2023– 02/2023 | Seasons since 01/2018 | All age groups | N/A |
emm1 (57%) emm1DK (30%) emm12 (24%) |
N/A | Total: 10–20% 84 years: 30% < 5 years: 5% |
| Nielsen H. et al., 2023 (13); Research Letter | National surveillance data | 10/2022– 04/2023 | 01/2015– 10/2022 | > 17 years | Meningitis |
emm1 (36%) emm12 (18%) emm87 (9%) |
N/A | 1/11 (9%) | |
| Belgium | Rodriguez-Ruiz JP. et al., 2023 (14); Rapid Communication | National surveillance data | 01/2022– 08/2023 | 01/2018– 12/2019 | All age groups | Sepsis | 2022: emm1 (45%) 2023: emm1 (34%) emm1UK (78%) |
N/A | 13/149 (8%) |
| Portugal | Gouveia C. et al., 2023 (15); Rapid Communication | National surveillance data | 09/2022– 05/2023 | 09/2014– 08/2019 | 0–17 years | Pneumonia +/- empyema |
emm1 (54,5%) emm1UK (47%) emm12 (22%) |
VZV (24,6%), respirato ry viruses (24.6%) | 4/79 (5.1%) |
| Spain | Cobo-Vázquez E. et al., 2023 (16); Correspondence | Multicenter network data (24 hospitals) | 01/2022– 12/2022 | 01/2019– 12/2019 | 0–16 years | Pneumonia, skin-/soft tissue- infections, STSS | N/A | RSV | 3/105 (2.9%) |
| Bellés-Bellés A. et al., 2023 (17); Research Letter | Regional surveillance data Lleida province | 11/2022– 05/2023 | 01/2011– 12/2019 | All age groups | N/A |
emm1 (48%) emm12 (16%) emm49 (16%) emm89 (13%) |
N/A | 3/31 (9.7%) |
hMPV, human metapneumovirus; IV, influenza virus; N/A, not available; RSV, respiratory syncytial virus; RV, rhinovirus; STSS, streptococcal toxic shock syndrome; VZV, Varicella zoster virus
Progress and dynamic
In the UK, Denmark, and Spain, above average steep and high increases were observed from October/November 2022 (10, 16, 17, 21), whereas in the Netherlands, Belgium, and Portugal, case numbers were already higher from spring 2022 onwards and rose again notably at the end of 2022 to reach a maximum in the first half of 2023 (11, 14, 15, 18). Dutch surveillance data showed differences in the annual maximum values for the different clinical pictures (11). In Belgium, case numbers remained high until August 2023 (14).
Age distribution
In the 2022/2023 season, the UK, the Netherlands, and Denmark noted a particularly steep rise in iGAS infections in children compared with prepandemic years (10, 11, 21). Children up to 5 years of age were typically most affected (10, 11, 18). A study in a pediatric population in Spain found a fourfold increase in iGAS infections in December 2022 compared with 2019 (16). By contrast, another Spanish study reported the most infections in older adults (17). In Denmark, incidence rates were highest in persons older than 85 but the relative increase compared with children younger than 5 was notably lower (10). In Belgium during the rise in iGAS infections from 2022 onwards, no age group was more markedly affected than before the pandemic.
Clinical manifestations and association with viral infections
Of note was the increase in invasive pneumonias with or without empyema in children in the Netherlands, the UK, Spain, and Portugal (12, 15, 16, 18, 21). In the UK, and especially in central Scotland, the increase in pulmonary iGAS infections was evident (21, 22). Prior respiratory infections or those existing in parallel were associated in 18–60% of cases (12, 16, 18, 21, 22) (Table). In Belgium, much as in the preceding years, sepsis was the pathology most often triggered by iGAS in all age groups (74–82% of all iGAS infections from 2018 to 2023) (14). In the Netherlands, necrotizing fasciitis (NF) occurred frequently in the first six months of 2022 (11); six cases were in children, all of whom showed an association with prior infection with the Varicella zoster virus (VZV) (18). This pathology was not seen in children in the comparison period 2018/2019 (18). Prior VZV infections were observed in Portugal in 24.6% of pediatric cases without any association with a specific pathology (15). Nielsen et al did a time series analysis of national surveillance data in Denmark and showed a 23-fold increase in the incidence of iGAS meningitis in adults compared with the preceding seven years (13). A time series analysis of national specimens of cerebrospinal fluid from the Netherlands also showed a cluster of meningitis cases compared with earlier years (20).
Severity of illness and case fatality rates
In the 2022/2023 season, death rates in most countries remained unchanged (10, 17, 21, 22) (Table). An increase in the case fatality rate in children from 3% to 9% was observed only in the Netherlands, but this was primarily due to cases of necrotizing fasciitis, which did not occur in the comparison season (18). The iGAS outbreak did not increase the probability for intensive care in adults (13, 22). In pediatric collectives with mainly pulmonary infections, the need for intensive care rose compared with the pre-COVID season from 30.4% (24 of 79 cases, 2019) to 48.6% (51 of 105 cases, 2022) in Spain (16) and from 21% (8 of 39 cases, 2018/2019) to 32% (18 of 57 cases, 2021/2022) in the Netherlands (18).
Bacterial strains
Group A streptococci are typed at the molecular level by the emm genes coding for the M protein. The M protein, which is located on the cellular surface, is a crucial virulence factor of these bacteria (Box 1, eBox 1)
Independently of age, emm1 was detected most often, followed by emm12 (10–15, 17, 20–22) (Table). Variants of the emm1 gene were more frequently associated with intensive care (10, 15). Only in one pediatric study from the Netherlands (18) was emm12 confirmed more often than emm1. Furthermore, a relative increase in emm4 isolates was observed particularly in young children (11, 18). A selective analysis of these cases detected independently of age and clinical picture a new bacterial strain M4NL22 in 85% (19). Cases of meningitis were not associated with emm4. They were caused by M1 (especially M1UK) in 86% (20). Studies from England, Belgium, and Portugal also reported a dominance of M1UK (14, 15, 22). In Denmark, where M1UK was the most common bacterial strain responsible for iGAS infections before the pandemic, a new M1DK strain was confirmed in August 2022, which in 2023 caused 30% of all iGAS infections (10). M1DK differs from the original M1UK and M1global variants thanks to the exotoxin SpeC, which is also typical for M12 (10, 23). While for M1DK an association with iGAS infections was seen, M12 was much more commonly detected in non-invasive group A streptococcal (nGAS) infections (10). Possible relevance also applies to the emm49 variant, which to date has been confirmed only in the US and since 2021 for the first time in Spain (17).
Antibiotic resistance
Currently available surveillance data do not provide any indication of increased resistance development as a cause of the postpandemic rise in iGAS infections, especially not in the confirmed new variant M4NL22 (14, 15, 19). Only in the Netherlands have increasing rates of resistance to clindamycin (from 4% to 9%) and erythromycin (from 6% to 11%) been described between 2017 and 2021 (11).
The situation in Germany
For Germany, only limited national data exist regarding the postpandemic increase in iGAS infections. The surveillance of iGAS infections via the national reference center is carried out on a voluntary basis. To date, whole genome sequencing of specimens is not yet standard procedure. The analysis of routine data to identify pathogens causing invasive bacterial infections between 2017 and the first quarter of 2023 showed a strong and early rise in infections with S. pyogenes from the fourth quarter of 2022 in all age groups (24). The study did not provide any more detailed information about the clinical course or the case fatality rate of the infections, nor about the confirmed bacterial strains. A first single center study of iGAS isolates (10/2022–03/2023) confirmed M1UK for the first time in Germany as the dominant M1 strain (14 of 17 emm isolates, 30% of all isolates) (25). The isolates emm12 and emm89 were detected as the second most common variants (25). The single center study did not include any information on the kind of clinical presentation, its extent, or the therapeutic measures employed.
A national analysis of German iGAS specimens from 2009 to 2014 found that emm28 and emm29 were the most common strains (26). The comparison with earlier analyses showed apart from an increase in emm89 since 1996 no relevant change regarding the emm variants (26). Rates of resistance rates to macrolides and clindamycin were low in the international comparison (27, 28). The most common clinical diagnoses were sepsis (59.4%), erysipelas (7.6%), and pneumonia (7%) (26). Most iGAS infections affected children up to 5 years of age and adults older than 70 (24, 26). The most recent data regarding the lethality of iGAS infections in Germany were collected for the time period 1996–2002 in a collective of 165 cases. Case fatality rates were notably lower in children and young adults (11.1–20.8%) than in older people (42.1–65.2%) (e2).
Discussion
Analyzing studies of the increase in iGAS infections in Europe since 2022 provides only partial answers to the question about causes and future effects. Because of heterogeneous approaches to data collection and processing, international comparisons and general conclusions are possible only to a limited extent.
Crucial observations relate to the shift in the usual periods of infection (earlier and higher rise in absolute case numbers) (11, 14, 15, 18), changes in the age distribution of infected patients (10, 11, 16, 18, 21), and a shift in clinical presentations towards invasive pneumonias with empyema (12, 15, 16, 18, 22).
Reports about the increase in iGAS infections in children at the end of 2022 coincided in many countries with the end of pandemic measures, which makes an association seem obvious (2, 3). But in many countries a continuous increase in infections with scarlet fever and iGAS was observed years before the COVID-19 pandemic, whose causes have thus far not been sufficiently explained (17, 29, 30). As our own data for acute mastoiditis show (Figure, eFigure), repeated high case numbers every 4–7 years are typical for iGAS infections (e3). It is possible that the pandemic only interrupted this periodic event and, in principle, the high case numbers of nGAS and iGAS infections after the pandemic are not unusual. The markedly high increase in case numbers after the pandemic could have been triggered by factors we list in what follows.
The effectiveness of diverse hygiene measures and contact restrictions on the transmission of respiratory pathogens was shown as early as during the Spanish flu (e4) and was also evident during the COVID-19 pandemic (6, 9). The lifting of certain restrictions (such as the wearing of protective face masks) resulted in different countries as early as in 2021 in an increase in viral and bacterial infections outside the usual season (7, 9, 10, 14), long before the WHO declared the pandemic over in 2023 (e5). The different time points of the observed increase in iGAS infections in the individual European countries are bound to be associated with different management of restrictions and lifting of restrictions. More precise conclusions cannot be drawn because of the poor data. Bacterial respiratory infections can be reduced by means of protective measures (7, 8), but certain pathogens will still persist as colonization pathogens in the nasopharynx (31). Even though no concrete data are available for GAS it seems possible that after the pandemic restrictions were lifted, group A streptococci spread more easily as colonization pathogens in the context of viral infections of the upper respiratory tract. Because of low test rates, the current data relating to a coincidence between viral and iGAS infections probably do not reflect the actual postpandemic incidence rates. A relevant association was seen in the UK, the Netherlands, Portugal, and Spain (12, 15, 16, 18, 21, 22). Of interest, coinfection with SARS-CoV-2 was reported only in individual cases (21). The analyses imply that the coincidence with viral infection stimulates especially pulmonary infections and could be responsible for the observed shift towards more cases of pneumonia and empyema. Viral infections enable bacterial superinfection by directly injuring the mucosal barrier of the respiratory tract and the lung, thus enabling easier adhesion and invasion of the bacteria and, on the other hand, triggering changes to the host’s protective immune response (32). The complex interaction of viral, bacterial, and host related factors remains insufficiently understood (33).
During the 2022/2023 season, children in some countries were particularly affected by scarlet fever and iGAS infections (10, 11, 21). The suspected cause, among others, lies in immunologic factors. The increased susceptibility to airborne respiratory pathogens is partly explained with the reduced peripandemic exposure—among others, because of the closure of educational institutions (“immunity debt or gap”) (6, 10, 11, 15, 21, 34). The general fall in standard vaccinations during the pandemic and the lacking recommendation for vaccination against pathogens that enable iGAS infections (for example, influenza virus IV and VZV), should be discussed as a possible cause (6). Infection with VZV can increase the risk for developing iGAS infections by a factor of almost 60 (23, e6). The presumed cause is—in addition to the weakened immune system—the penetration of path ogenic bacteria through the damaged skin barrier, which could explain the clusters of NF (5, 18, 23). The Netherlands and the UK reported a particularly high incidence of VZV in 2022 (18, 21). An association between iGAS and VZV infections in younger children was observed in the Netherlands and also in Portugal (11, 15, 18). As in the UK, Belgium, Spain, and Denmark, no general recommendation for vaccination exists here: the risk for coinfection could, however, crucially depend on mandatory vaccination recommendations and vaccination rates (34, 35).
The postpandemic rise in iGAS infections in Europe cannot be explained with the expansion and selection of a specific new bacterial strain. For most infections, strains were responsible that were widespread before the pandemic, especially emm1 variants (26, 36, 37). The M1UK variant, which is currently dominant in Belgium (14), the UK (21, 22), the Netherlands (20), and Portugal, was already dominant before the COVID-19 pandemic in Denmark (10), the UK (30), and the Netherlands (38). Even though emm1 variants bore a higher risk for treatment in intensive care (10, 15), this was not the case for M1UK and M1DK specially (10, 14). For the first time, M1UK was also confirmed in German specimens (25). Further work-up of data from the prepandemic years may enable insights into the relevance during the observed rise in infections in Germany. In the increase of iGAS infections, colonization advantages of certain variants in association with certain special genes may play a role; for the new variants M1DK and M4NL22 this will have to be investigated in molecular genetic studies in larger (inter)national collectives (10, 15, 19).
An increase in antibiotic resistance in Europe has not been noticed to date, which means that standard treatment (Box 2) will work (11, 14, 15, 19). In the autumn/winter season 2022/2023, reported bottlenecks in the supply of oral antibiotics, especially penicillins (39), and additionally the rapidly increasing consumption of antibiotics in some countries after the pandemic (4) will in future have to be considered risk factors for the increasing development of resistance and need to be stringently monitored.
Box 2. Treating group A streptococcal infections (27, 28, e18–e20).
Narrow spectrum penicillins are the treatment of choice for infections caused by group A streptococci. Uncomplicated infections are treated orally, with dosage and duration of treatment depending on the patient’s age, type of disease, and clinical response. In contrast to other gram-positive pathogens, such as staphylococci, enterococci, but also pneumococci, GAS are fully susceptible to ß-lactam. The underlying mechanism is largely unexplained. Individual cases of impaired susceptibility to penicillin have been explained with mutations in the penicillin binding protein(pbp) gene.
Especially oral penicillin V has repeatedly been subject to supply bottlenecks. Alternatively, broad spectrum ß-lactams, such as aminopenicillins with ß-lactamase inhibitors or first generation cephalosporins, should be administered. In penicillin anaphylaxis and for the purpose of eradication of persistent pathogens, macrolides (clarithromycin or azithromycin) and lincosamides (clindamycin) are available. As GAS resistance rates to macrolides vary considerably (1.5% to 22.4% in Europe), these drugs should be used for monotherapy only after resistance testing.
In life threatening invasive GAS infections, penicillin G or, in case of penicillin anaphylaxis, third generation cephalosporins administered by the parenteral route are the treatment of choice. As clindamycin inhibits the synthesis of superantigens and other virulence factors, combination treatment is recommended to lower mortality. Recurring infections with GAS or a poor therapeutic response of invasive infections to penicillin are explained with different mechanisms. These include the secretion of ß-lactamases by resident mucosal pathogens, the development of biofilms, and the intracellular persistence of GAS in macrophages and epithelial cells. Macrolides or clindamycin are effective against intracellular persistent bacteria. Furthermore, in invasive tissue infections such as necrotizing fasciitis, extensive surgical debridement is required as the penetration of antimicrobial substances in tissue necroses is severely reduced.
Despite gaps in the data, which cannot completely explain the remarkably early and steep rise in iGAS infections, observations to date can be used to deduct general recommendations to prevent further relevant increases in iGAS infections in the future. These recommendations are summed up in Box 2.
eBox 2. Measures aiming to prevent increases in iGAS infections.
The work-up of historical data and comparisons between the observations regarding the latest increase in iGAS infections at the end of the COVID-19 pandemic allow drawing conclusions about potential risk factors for the development of such outbreaks. From these, fundamental recommendations can be drawn to prevent a further rise in iGAS infections.
Patients with risk factors should receive early antibiotic treatment because of their risk of developing invasive iGAS infections (11, 18). In treating sore throats and nGAS infections, a considered use of antibiotics is essential according to antibiotic stewardship and in adherence to valid guidelines, so as to prevent supply bottlenecks and the development of resistance. Testing for associated viruses does not only help identify coinfections but also better to understand associations with clinical courses of iGAS in the future (12). The development and introductions of new vaccines against high-risk virus infections—for example, respiratory syncytial virus (RSM) and human metapneumovirus (hMPV)—should be supported and promoted, as should the stringent recommendation of existing vaccinations (such as against Varicella zoster virus [VZV] and influenza virus [IV]) (12). To improve the comparability of European data, mandatory, standardized surveillance concepts should be developed and applied across countries; these should include not only whole genome sequencing but also data on clinical symptoms, course, and risk factors (10, e21). Recent suggestions for the standardized collection of data and case definitions can be found in Miller et al (e21). Until such time, sending microbiologic specimens to national reference centers on a voluntary basis (e22) supports the surveillance of further trends in iGAS infections.
Questions on the article.
Invasive Group A Streptococcal Infections in Europe After the COVID-19 Pandemic
The submission deadline is 3 October 2025. Only one answer is possible per question.
Please select the answer that is most appropriate.
Question 1
According to the article, which percentage range applies for the case fatality rate for iGAS infections in industrialized countries?
Between 0.5% and 2,3%
Between 2.5% and 4%
Between 5% and 23%
Between 25% and 33%
Between 35% and 50%
Question 2
Which three countries mentioned in the article noted a particularly steep rise in iGAS infections in children in the 2022/2023 season compared with prepandemic years
The UK, Netherlands, and Denmark
Spain, France, and Switzerland
France, Sweden, and Belgium
Norway, Switzerland, and Portugal
Switzerland, Finland und Luxemburg
Question 3
Typing of Group A streptococci is done on the basis of which molecular structure?
E protein
G protein
L protein
M protein
A protein
Question 4
Which statement pertaining to the collection of data on iGAS infections in Germany is correct?
The surveillance of iGAS infections is carried out on a voluntary basis via the national reference center.
iGAS infections are notifiabl. Cases are notified to the Robert Koch-Institute by public health departments.
At the moment, no notification option exists for iGAS infections because of the lack of a reference center.
For the past four years, complete and extensive data sets exist for iGAS infections.
For each iGAS infection, whole genome sequencing of the pathogen is standard.
Question 5
Which country reported a rise in fatalities in children as a result of iGAS (mainly necrotizing fasciitis) in the 2022/2023 season?
Germany
The UK
France
Denmark
Netherlands
Question 6
Which of the following diseases caused by GAS is toxin mediated - according to the article?
Meningitis
Necrotizing fasciitis
Scarlet fever
Tonsillopharyngitis
Phlegmons
Question 7
What is the drug treatment of choice to treat life threatening invasive infections caused by Group A streptococci?
Doxycycline or minocycline
Penicillin G, if required in combination with clindamycin
Erythromycin in combination with imipenem
Rifampicin or rifamixin
Fosfomycin in combination with rifampicin
Question 8
Which substances are effective against intracellular persistent GAS?
Fosfomycin or rifampicin
Metronidazole or trimethoprim-sulfamethoxazole
Macrolides or clindamycin
Gentamicin and amikacin
Ciprofloxacin and gentamicin
Question 9
Which GAS variants does the article refer to as “new variants” because of their more frequent occurrence after the pandemic?
M2UK and M533DE
E12DE and G4UK
M4DE and L122SE
M1DK and M4NL22’
L522UK and A4DK
Question 10
According to the article, which statement regarding GAS infections is most applicable?
GAS infections happen primarily in the autumn and summer months.
Periodic peaks with clusters of infection occur every 2-3 years.
GAS infections occur exclusively in association with viral respiratory infections (opportunistic infections).
The postpandemic increase in GAS infections is explained primarily with a growing trend of antibiotic resistance.
Periodic peaks with clusters of infection occur every 4–7 years.
Acknowledgments
Translated from the original German by Birte Twisselmann, PhD.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
References
- 1.UK Health Security Agency (UKHSA) Group A streptococcal infections: report on seasonal activity in England, 2022 to 2023. www.gov.uk/government/publications/group-a-streptococcal-infections-activity-during-the-2022-to-2023-season/group-a-streptococcal-infections-report-on-seasonal-activity-in-england-2022-to-2023 (last accessed on 17 December 2023) 2022 [Google Scholar]
- 2.World Health Organization (WHO) Disease outbreak news: Increased incidence of scarlet fever and invasive group A streptococcus infection—multi-country. www.who.int/emergencies/disease-outbreak-news/item/2022-DON429 (last accessed on 22 December 2023) 2022 [Google Scholar]
- 3.European Centre for Disease Prevention and Control (ECDC) Increase in invasive group A streptococcal infections among children in Europe, including fatalities. European Centre for Disease Prevention and Control www.ecdc.europa.eu/en/news-events/increase-invasive-group-streptococcal-infections-among-children-europe-including (last accessed on 22 December 2023) 2022 [Google Scholar]
- 4.Robert Koch Institut (RKI) Update: Anstieg bakterieller Infektionen durch Gruppe-A-Streptokokken, Pneumokokken und Haemophilus influenzae in Deutschland seit Ende 2022. Vol. 8, Epidemiologisches Bulletin. www.rki.de/DE/Content/Infekt/EpidBull/Archiv/2023/Ausgaben/08_23.pdf?__blob=publicationFile (last accessed on 19 August 2023) 2023;45 [Google Scholar]
- 5.Steer AC, Lamagni T, Curtis N, Carapetis JR. Invasive group A streptococcal disease: epidemiology, pathogenesis and management. Drugs. 2012;72:1213–1227. doi: 10.2165/11634180-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oh KB, Doherty TM, Vetter V, Bonanni P. Lifting non-pharmaceutical interventions following the COVID-19 pandemic—the quiet before the storm? Expert Rev Vaccines. 2022;21:1541–1553. doi: 10.1080/14760584.2022.2117693. [DOI] [PubMed] [Google Scholar]
- 7.Shaw D, Abad R, Amin-Chowdhury Z, et al. Trends in invasive bacterial diseases during the first 2 years of the COVID-19 pandemic: analyses of prospective surveillance data from 30 countries and territories in the IRIS consortium. Lancet Digit Health. 2023;5:e582–e593. doi: 10.1016/S2589-7500(23)00108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Amarsy R, Fournier S, Trystram D, et al. Decrease of hospital- and community-acquired bloodstream infections due to Streptococcus pneumoniae and Streptococcus pyogenes during the first year of the COVID-19 pandemic: a time-series analysis in Paris region. Am J Infect Control. 2023;51:475–477. doi: 10.1016/j.ajic.2022.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chow EJ, Uyeki TM, Chu HY. The effects of the COVID-19 pandemic on community respiratory virus activity. Nat Rev Microbiol. 2023;21:195–210. doi: 10.1038/s41579-022-00807-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johannesen TB, Munkstrup C, Edslev SM, et al. Increase in invasive group A streptococcal infections and emergence of novel, rapidly expanding sub-lineage of the virulent Streptococcus pyogenes M1 clone, Denmark, 2023. Euro Surveill. 2023;28 doi: 10.2807/1560-7917.ES.2023.28.26.2300291. 2300291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de Gier B, Marchal N, de Beer-Schuurman I, et al. Increase in invasive group A streptococcal (Streptococcus pyogenes) infections (iGAS) in young children in the Netherlands, 2022. Euro Surveill. 2023;28 doi: 10.2807/1560-7917.ES.2023.28.1.2200941. 2200941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holdstock V, Twynam-Perkins J, Bradnock T, et al. National case series of group A Streptococcus pleural empyema in children: clinical and microbiological features. Lancet Infect Dis. 2023;23:154–156. doi: 10.1016/S1473-3099(23)00008-7. [DOI] [PubMed] [Google Scholar]
- 13.Nielsen H, Storgaard M, Helweg-Larsen J, et al. Group A streptococcus meningitis in adults, Denmark. Emerg Infect Dis. 2023;29:1937–1939. doi: 10.3201/eid2909.230627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rodriguez-Ruiz JP, Lin Q, Lammens C, et al. Increase in bloodstream infections caused by emm1 group A Streptococcus correlates with emergence of toxigenic M1UK, Belgium, May 2022 to August 2023. Euro Surveill. 2023;28 doi: 10.2807/1560-7917.ES.2023.28.36.2300422. 2300422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gouveia C, Paula Bajanca-Lavado M, Mamede R, et al. Sustained increase of paediatric invasive Streptococcus pyogenes infections dominated by M1UK and diverse emm12 isolates, Portugal, September 2022 to May 2023. Euro Surveill. 2023;28 doi: 10.2807/1560-7917.ES.2023.28.36.2300427. 2300427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cobo-Vázquez E, Aguilera-Alonso D, Carrasco-Colom J, et al. In creasing incidence and severity of invasive group A streptococcal disease in Spanish children in 2019-2022. Lancet Reg Heal Eur. 2023;27 doi: 10.1016/j.lanepe.2023.100597. 100597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bellés-Bellés A, Prim N, Mormeneo-Bayo S, et al. Changes in group A Streptococcus emm types associated with invasive infections in adults, Spain, 2023. Emerg Infect Dis. 2023;29:2390–2392. doi: 10.3201/eid2911.230857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van Kempen EB, Bruijning-Verhagen PCJ, Borensztajn D, et al. Increase in invasive group a streptococcal infections in children in the Netherlands, a survey among 7 hospitals in 2022. Pediatr Infect Dis J. 2023;42:e122–e124. doi: 10.1097/INF.0000000000003810. [DOI] [PubMed] [Google Scholar]
- 19.van der Putten BCL, Bril-Keijzers WCM, Rumke LW, et al. Novel emm4 lineage associated with an upsurge in invasive group A streptococcal disease in the Netherlands, 2022. Microb Genom. 2023;9 doi: 10.1099/mgen.0.001026. mgen001026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van der Putten BCL, Vlaminckx BJM, De Gier B, Freudenburg-De Graaf W, Van Sorge NM. Group A streptococcal meningitis with the M1UK variant in the Netherlands. JAMA. 2023;329:1791–1792. doi: 10.1001/jama.2023.5927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guy R, Henderson KL, Coelho J, et al. Increase in invasive group A streptococcal infection notifications, England, 2022. Euro Surveill. 2023;28 doi: 10.2807/1560-7917.ES.2023.28.1.2200942. 2200942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Davies PJB, Russell CD, Morgan AR, et al. Increase of severe pulmonary infections in adults caused by M1UK Streptococcus pyogenes, central Scotland, UK. Emerg Infect Dis. 2023;29:1638–1642. doi: 10.3201/eid2908.230569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Imöhl M, van der Linden M, Reinert RR, Ritter K. Invasive group A streptococcal disease and association with varicella in Germany, 1996-2009. FEMS Immunol Med Microbiol. 2011;62:101–109. doi: 10.1111/j.1574-695X.2011.00788.x. [DOI] [PubMed] [Google Scholar]
- 24.Singer R, Abu Sin M, Tenenbaum T, et al. The increase in invasive bacterial infections with respiratory transmission in Germany, 2022/2023. Dtsch Arztebl Int. 2024;121:114–120. doi: 10.3238/arztebl.m2023.0261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wolters M, Berinson B, Degel-Brossmann N, et al. Population of invasive group A streptococci isolates from a German tertiary care center is dominated by the hypertoxigenic virulent M1UK genotype. Infection. 2024;52:667–671. doi: 10.1007/s15010-023-02137-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Imöhl M, Fitzner C, Perniciaro S, Van Der Linden M. Epidemiology and distribution of 10 superantigens among invasive Streptococcus pyogenes disease in Germany from 2009 to 2014. PLoS One. 2017;12 doi: 10.1371/journal.pone.0180757. e0180757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Imöhl M, Van Der Linden M. Antimicrobial susceptibility of invasive Streptococcus pyogenes isolates in Germany during 2003-2013. PLoS One. 2015;10 doi: 10.1371/journal.pone.0137313. e0137313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Silva-Costa C, Friães A, Ramirez M, Melo-Cristino J. Macrolide- resistant Streptococcus pyogenes: prevalence and treatment strategies. Expert Rev Anti Infect Ther. 2015;13:615–628. doi: 10.1586/14787210.2015.1023292. [DOI] [PubMed] [Google Scholar]
- 29.Venkatesan P. Rise in group A streptococcal infections in England. Lancet Respir Med. 2023;11 doi: 10.1016/S2213-2600(22)00507-0. e16. [DOI] [PubMed] [Google Scholar]
- 30.Lynskey NN, Jauneikaite E, Li HK, et al. Emergence of dominant toxigenic M1T1 Streptococcus pyogenes clone during increased scarlet fever activity in England: a population-based molecular epidemiological study. Lancet Infect Dis. 2019;19:1209–1218. doi: 10.1016/S1473-3099(19)30446-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rybak A, Levy C, Angoulvant F, et al. Association of nonpharmaceutical interventions during the COVID-19 pandemic with invasive pneumococcal disease, pneumococcal carriage, and respiratory viral infections among children in France. JAMA Netw Open. 2022;5 doi: 10.1001/jamanetworkopen.2022.18959. e2218959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Herrera AL, Huber VC, Chaussee MS. The association between invasive group A streptococcal diseases and viral respiratory tract infections. Front Microbiol. 2016;7:342. doi: 10.3389/fmicb.2016.00342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Okamoto S, Nagase S. Pathogenic mechanisms of invasive group A Streptococcus infections by influenza virus-group A Streptococcus superinfection. Microbiol Immunol. 2018;62:141–149. doi: 10.1111/1348-0421.12577. [DOI] [PubMed] [Google Scholar]
- 34.Cohen R, Ashman M, Taha MK, et al. Pediatric infectious disease group (GPIP) position paper on the immune debt of the COVID-19 pandemic in childhood, how can we fill the immunity gap? Infect Dis Now. 2021;51:418–423. doi: 10.1016/j.idnow.2021.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abo YN, Oliver J, McMinn A, et al. Increase in invasive group A streptococcal disease among Australian children coinciding with northern hemisphere surges. Lancet Reg Health West Pac. 2023;41 doi: 10.1016/j.lanwpc.2023.100873. 100873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Luca-Harari B, Darenberg J, Neal S, et al. Clinical and microbiological characteristics of severe Streptococcus pyogenes disease in Europe. J Clin Microbiol. 2009;47:1155–1165. doi: 10.1128/JCM.02155-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jespersen MG, Lacey JA, Tong SYC, Davies MR. Global genomic epidemiology of Streptococcus pyogenes. Infect Genet Evol. 2020;86 doi: 10.1016/j.meegid.2020.104609. 104609. [DOI] [PubMed] [Google Scholar]
- 38.Rümke LW, de Gier B, Vestjens SMT, et al. Dominance of M1UK clade among Dutch M1 Streptococcus pyogenes. Lancet Infect Dis. 2020;20:539–540. doi: 10.1016/S1473-3099(20)30278-4. [DOI] [PubMed] [Google Scholar]
- 39.Bundesinstitut für Arzneimittel und Medizinprodukte (BfArM) Informationen zur Verfügbarkeit von Antibiotikasäften und Empfehlungen zur Abmilderung möglicher Engpässe—Stand: 07.12.2023. www.bfarm.de/DE/Arzneimittel/Arzneimittelinformationen/Lieferengpaesse/Antibiotika.html (last accessed on 30 December 2023) [Google Scholar]
- 40.Ventura-Gabarró C, Leung VH, Vlahovic-Palčevski V, Machowska A, Monnet DL, Högberg LD. Rebound in community antibiotic consumption after the observed decrease during the COVID-19 pandemic, EU/EEA, 2022. Euro Surveill. 2023;28 doi: 10.2807/1560-7917.ES.2023.28.46.2300604. 2300604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E1.Parks T, Elliott K, Lamagni T, et al. Elevated risk of invasive group A streptococcal disease and host genetic variation in the human leucocyte antigen locus. Genes Immun. 2020;21:63–70. doi: 10.1038/s41435-019-0082-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E2.Wahl RU, Lütticken R, Stanzel S, van der Linden M, Reinert RR. Epidemiology of invasive Streptococcus pyogenes infections in Germany, 1996-2002: results from a voluntary laboratory surveillance system. Clin Microbiol Infect. 2007;13:1173–1178. doi: 10.1111/j.1469-0691.2007.01821.x. [DOI] [PubMed] [Google Scholar]
- E3.Lynskey NN, Lawrenson RA, Sriskandan S. New understandings in Streptococcus pyogenes. Curr Opin Infect Dis. 2011;24:196–202. doi: 10.1097/QCO.0b013e3283458f7e. [DOI] [PubMed] [Google Scholar]
- E4.Bootsma MCJ, Ferguson NM. The effect of public health measures on the 1918 influenza pandemic in U.S. cities. Proc Natl Acad Sci USA. 2007;104:7588–7593. doi: 10.1073/pnas.0611071104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E5.Lenharo M. WHO declares end to COVID-19’s emergency phase. Nature. 2023 doi: 10.1038/d41586-023-01559-z. DOI: 10.1038/d41586-023-01559-z (online ahead of print) [DOI] [PubMed] [Google Scholar]
- E6.Patel RA, Binns HJ, Shulman ST. Reduction in pediatric hospitalizations for varicella-related invasive group A streptococcal infections in the varicella vaccine era. J Pediatr. 2004;144:68–74. doi: 10.1016/j.jpeds.2003.10.025. [DOI] [PubMed] [Google Scholar]
- E7.Lannes-Costa PS, Oliveira JSS, Silva Santos G, Nagao PE. A current review of pathogenicity determinants of Streptococcus sp. J Appl Microbiol. 2021;131:1600–1620. doi: 10.1111/jam.15090. [DOI] [PubMed] [Google Scholar]
- E8.Walker MJ, Barnett TC, McArthur JD, et al. Disease manifestations and pathogenic mechanisms of group A Streptococcus. Clin Microbiol Rev. 2014;27:264–301. doi: 10.1128/CMR.00101-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E9.Metzgar D, Zampolli A. The M protein of group A Streptococcus is a key virulence factor and a clinically relevant strain identification marker. Virulence. 2011;2:402–412. doi: 10.4161/viru.2.5.16342. [DOI] [PubMed] [Google Scholar]
- E10.Boeddha NP, Atkins L, de Groot R, et al. Group A streptococcal disease in paediatric inpatients: a European perspective. Eur J Pediatr. 2023;182:697–706. doi: 10.1007/s00431-022-04718-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E11.Gale AH. A century of changes in the mortality and incidence of the principal infections of childhood. Arch Dis Child. 1945;20:2–21. doi: 10.1136/adc.20.101.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E12.Gaworzewska E, Colman G. Changes in the pattern of infection caused by Streptococcus pyogenes. Epidemiol Infect. 1988;100:257–269. doi: 10.1017/s095026880006739x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E13.Lamagni T, Guy R, Chand M, et al. Resurgence of scarlet fever in England, 2014-16: a population-based surveillance study. Lancet Infect Dis. 2018;18:180–187. doi: 10.1016/S1473-3099(17)30693-X. [DOI] [PubMed] [Google Scholar]
- E14.Avire NJ, Whiley H, Ross K. A review of Streptococcus pyogenes: public health risk factors, prevention and control. Pathogens. 2021;10:248. doi: 10.3390/pathogens10020248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E15.Brouwer S, Rivera-Hernandez T, Curren BF, et al. Pathogenesis, epidemiology and control of group A Streptococcus infection. Nat Rev Microbiol. 2023;21:431–447. doi: 10.1038/s41579-023-00865-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E16.Commons RJ, Smeesters PR, Proft T, Fraser JD, Robins-Browne R, Curtis N. Streptococcal superantigens: categorization and clinical associations. Trends Mol Med. 2014;20:48–62. doi: 10.1016/j.molmed.2013.10.004. [DOI] [PubMed] [Google Scholar]
- E17.Li HK, Zhi X, Vieira A, et al. Characterization of emergent toxigenic M1UK Streptococcus pyogenes and associated sublineages. Microb Genom. 2023;9 doi: 10.1099/mgen.0.000994. mgen000994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E18.Yu D, Guo D, Zheng Y, Yang Y. A review of penicillin binding protein and group A Streptococcus with reduced-ß-lactam susceptibility. Front Cell Infect Microbiol. 2023;13 doi: 10.3389/fcimb.2023.1117160. 1117160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E19.Carapetis JR, Jacoby P, Carville K, Ang SJJ, Curtis N, Andrews R. Effectiveness of clindamycin and intravenous immunoglobulin, and risk of disease in contacts, in invasive group A streptococcal infections. Clin Infect Dis. 2014;59:358–365. doi: 10.1093/cid/ciu304. [DOI] [PubMed] [Google Scholar]
- E20.Johnson AF, LaRock CN. Antibiotic treatment, mechanisms for failure, and adjunctive therapies for infections by group A Streptococcus. Front Microbiol. 2021;12 doi: 10.3389/fmicb.2021.760255. 760255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E21.Miller KM, Lamagni T, Cherian T, et al. Standardization of epidemiological surveillance of invasive group A streptococcal infections. Open Forum Infect Dis. 2022;9:31–40. doi: 10.1093/ofid/ofac281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E22.Institut für medizinische Mikorbiologie. Referenzlabor für Streptokokken. www.ukaachen.de/kliniken-institute/institut-fuer-medizinische-mikrobiologie/forschung/nationales-referenzzentrum-fuer-streptokokken/ (last accessed on 10 June 2024) [Google Scholar]