Abstract
Biomechanic studies can provide a powerful theoretical and scientific basis for studies on knee osteoarthritis (OA), which is of great significance for clinical management as it provides new concepts and methods in clinical and research settings. This study aimed to discuss and summarize biomechanical research on lower extremities in individuals with knee OA in the past ten years. The methodology of this review followed the framework outlined in the Joanna Briggs Institute (JBI) guidelines and strictly followed the checklist for drafting the findings. A literature search was conducted using PubMed, Scopus, Cochrane Library, Embase, Web of Science, Grey literature search in Open Library, and Google Academic databases. Relevant literature was searched from 2011 to 2023. Sixteen studies were included in this scoping review. Biomechanical research on knee OA in the last decade demonstrates that the biomechanics of the hip, knee, and ankle have a profound influence on the pathogenesis and treatment of knee OA. Individuals with knee OA have biomechanical changes in hip, knee, and ankle joints such as a significant defect in the strength of ankle varus muscles, weakness of hip abductor muscle, walking with toes outwards, increased knee adduction moment and angle, and decreased knee extensor moment. As the severity of knee OA increases, the tendency of hip abduction positions also increases. Further research with a longitudinal study design should focus on the determination of the relative importance of different biomechanical and neuromuscular factors in the development and progression of the disease.
Keywords: Knee osteoarthritis, Biomechanics change, Knee varus, Knee moment, Scoping review
1. Introduction
Osteoarthritis (OA) of the knee is a chronic joint disease characterized by cartilage degeneration and secondary bone deformation of the knee joint [1]. Individuals with knee OA typically suffer from pain, swelling, stiffness, and deformity, resulting in functional limitations, which is the main cause of disability among older adults aged over 65 years. The incidence of knee arthritis in women is higher than that in men [2]. The incidence rate of knee OA is related to age, obesity, inflammation, trauma, and genetic factors [3] but the etiology and pathogenesis of knee arthritis are unclear [1].
Biomechanical factors constitute an important risk for the progression of knee OA. For example, the higher adduction moment of the knee joint and the smaller muscle strength are considered factors leading to OA of the knee joint [4]. The severity of knee OA disease usually increases pain, swelling, cartilage loss, and bone spur formation, and may reduce the range of motion, thus affecting the movement changes in individuals with knee OA during functional tasks. Dynamic research on biomechanics is typically used to study motion patterns in humans [4], which helps display motion changes owing to different severities [5]. In recent years, to better understand and formulate effective exercise therapy programs, more attention to biomechanical factors related to the pathological mechanism of OA is warranted [6]. A better understanding of the contribution of biomechanics will help design effective intervention and prevention programs and also help clinicians educate individuals with OA. Moreover, wedge-shaped insoles or other auxiliary devices are made by using the spatial parameters obtained from biomechanical measurements to reduce the damage to the knee joint caused by the applied force [7].
In most cases, the application of biomechanics in the exploration and treatment of knee OA mainly includes the study of muscle strength around the knee joint, the change in knee joint torque, and the movement of hip and ankle joints and their muscles [7]. Previous studies proved that the integrity of the lower limb chain plays an important role in knee OA [8,9]. The systematic review conducted by Mills et al. [10] had specifically pinpointed the gait deviations that are consistently linked with knee OA. However, a clear summary of the biomechanical changes in the lower limb joints is lacking. The last decade has seen an increase in research equipment for biomechanics, a curiosity in the study of biomechanical changes in knee OA, and a theoretical and clinical need for understanding biomechanics of knee OA. Therefore, the purposes of this systematic review were to study the current status of studies on biomechanical changes of lower limbs in individuals with knee OA using data from the past decade; to explore outcomes and common research equipment use, and to provide a descriptive summary of perspective and clinical implications. We also discussed the prospects for biomechanical treatment of knee OA and the lack of research sites. This review provides some theoretical support, knowledge gap identification, and avenues for further research in this field.
2. Materials and methods
The steps of the research method were guided by and strictly followed the PRISMA Extension for Scoping Reviews (PRISMAScR): Checklist and Explanation 2020 updated version of the Joanna Briggs Institute (JBI) [11,12].
2.1. Identifying the research question
Through retrieval and result sorting, we aimed to address the following questions, specifically in the last decade of research: a) What are the lower limb biomechanical changes that have been reported so far in individuals with knee OA? b) What equipment was used to study the biomechanical changes of knee OA? c) What is the primary perspective of biomechanical study in knee OA? The study aimed to address the above question for screening, reading, and extraction of references.
2.2. Identifying relevant studies
The electronic sources accessed from 2011 to July 2023 for this review included PubMed, Scopus, Cochrane Library, Embase, and Web of Science. Grey literature was also searched and data were extracted using Google Scholar, Open Doar and Open Grey. Search terms mainly included knee osteoarthritis, Knee OA, lower extremity, biomechanical, and their extension and free words, with wildcard characters. The logical words “AND” and “OR” were used to extend the search scope. The two authors screened and identified studies for inclusion in the review independently. Discrepancies were then resolved through discussion and a third author was consulted. The study inclusion criteria were based on the patients who are diagnosed as KOA. The relevant studies were published with English language and reported biomechanics or electromyography outcomes of lower-limb joints during static or dynamic task.
2.3. Study selection
The results from the electronic search were imported into an EndNote 20.0 library, and duplications were removed. Two authors (LYY, FS) first reviewed and screened the title and abstract independently. Relevant studies were included in this review. A third author (BQZ) was asked for help when the first two authors could not reach a consensus. Then, the full text of the included literature was searched. Criteria for study inclusion and exclusion are shown in Table 1.
Table 1.
Inclusion and exclusion criteria for this study.
| Inclusion criteria | Exclusion criteria |
|---|---|
|
|
|
|
|
|
2.4. Charting the data
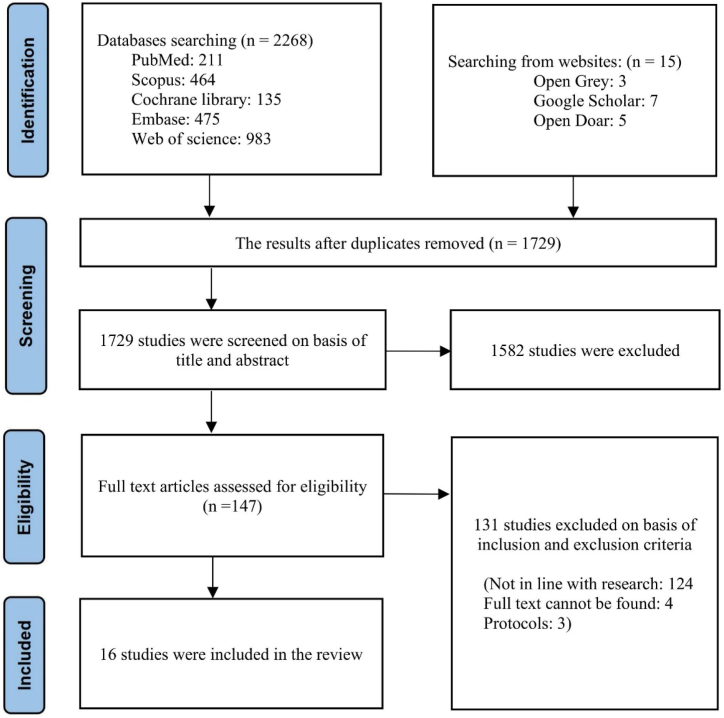
Sixteen studies were finally included (Fig. 1). Data were extracted from included studies and organized into the table format. The primary information was collected and organized in a structured form under the following headings: first author and year of publication, country, study sample, study purpose, study design, study measurements, main results, biomechanical changes and other reports.
Fig. 1.
Flow chart of the literature search strategy.
2.5. Collation, summarizing, and reporting results
In line with the approach of scope review, below we present the results in the form of narrative synthesis to provide more detailed information and integrate multiple evidence for researchers and healthcare professionals.
3. Results
A total of 2268 studies were retrieved which were published from January 1, 2011–July 31, 2023, with 539 duplicates; these were deleted. After reading the title and abstracts, 1582 papers were removed because they were not relevant to the content of the study. Fifteen articles in the first consideration were retrieved from the grey literature website (http://www.greylit.org/). One more paper was included after repeated consideration in the second round. Finally, 16 studies were included in this scoping review. To ensure the reliability of the journals that published these articles, the SCImago Journal & Country Rank portal was used to verify their scientific nature. The characteristics of 16 studies were extracted and are shown in Table 2.
Table 2.
Characteristics and main result from the 16 studies.
| No | Author, Country, Year |
Sample | Study design | Study purpose | Measurement system | Biomechanical changes of lower extremity | Other reports |
|---|---|---|---|---|---|---|---|
| 1 | Wang Y et al., China, 2021 [28] | n = 44, individuals with late-stage Knee OA n = 22, healthy subjects | CSS | To investigate the patterns and variability of lower limb inter-segmental coordination of individuals with knee OA and healthy subjects during walking, and to evaluate inter-segmental coordination alterations in individuals |
|
|
– |
| 2 | Petrella M et al., Brazil, 2021 [18] | n = 12, individuals with unilateral Knee OA n = 16, individuals with bilateral Knee OA |
CSS | To investigate biomechanical and neuromuscular similarities and differences in the transition from sitting to standing in individuals with unilateral and bilateral Knee OA |
|
|
|
| 3 | Costa e Silva Cabral AL et al., Brazil, 2021 [7] | n = 12, individuals with Knee OA n = 16, healthy subjects | CSS | To analyze the EMG pattern, kinematics, and postural control in individuals with and without Knee OA during SLS |
|
|
|
| 4 | Parekh S et al., India, 2019 [15] |
n = 50, individuals with Knee OA | CSS | To assess the association between the lower extremity biomechanical factors with knee OA | WOMAC and NRS |
|
|
| 5 | Fukaya T et al., Japan, 2019 [29] | n = 8 (3 men and 5 women), recorded a KL scale score of 1–2 n = 9 (3 men and six women), recorded a KL scale score of 3–4 | CSS | To investigate the effect of structural destruction of the knee joint on frontal plane hip and ankle joint kinematics and kinetics during the stance phase of walking in individuals with differing severities of knee OA. |
|
|
– |
| 6 | Monil K et al., UK, 2018 [13] |
n = 84, no known pathology n = 24,18 had medial knee OA and 6 had lateral knee OA | CSS | To characterize knee adduction angle and moment and compare these with foot CoP in volunteers with and without Knee OA |
|
|
|
| 7 | Neila M et al., Canada, 2017 [30] |
n = 32, individuals with Knee OA n = 15, asymptomatic subjects (AS) | CSS | To analyze the impact of knee OA on ipsilateral hip, knee, and ankle joints during gait |
|
|
|
| 8 | Park SK et al., Canada, 2016 [31] |
n = 24 (17 females and 7 males) with mild-to-moderate Knee OA n = 24 (16 females and 8males) healthy subjects | CSS | The relationship between muscle strength, gait biomechanics, and self-reported physical function and pain for individuals with knee OA is not well known. The study's objective was to investigate these relationships in this population |
|
|
|
| 9 | Farrokhi S et al., USA, 2016 [32] |
n = 11, individuals with Knee OA n = 11, control volunteers | CSS | To evaluate tibiofemoral joint contact point excursions and velocities during downhill gait and assess the relationship between tibiofemoral joint contact mechanics with frontal-plane knee joint motion and lower extremity muscle weakness in individuals with knee OA |
|
|
|
| 10 | Anan M et al., Japan, 2016 [23] |
n = 13, individuals with Knee OA n = 11, asymptomatic controls | CSS | To examine the muscle activities of the lower extremity both quantitative and qualitative data |
|
|
|
| 11 | Bouchouras G et al., Greece, 2015 [26] | n = 11, women with Knee OA n = 11, healthy women |
CSS | To compare joint kinematics, knee and trunk muscle activation, and coactivation patterns during a sit-to-stand movement in women with knee OA and age-matched controls |
|
|
WOMAC Function (mean ± SD): OA group vs control group = 22.54 ± 4.74 vs 3.36 ± 3.88 |
| 12 | Igawa T et al., Japan, 2014 [14] |
n = 4, elders with early-stage unilateral Knee OA n = 8, healthy elders | CSS | To investigate the lower extremity joint kinematics and kinetics of individuals with knee OA during stair descent and clarify the biomechanical factors related to their difficulty in stair descent |
|
|
|
| 13 | Son H et al., South Korea, 2013 [16] |
n = 14, subjects with bilateral Knee OA (KL score ≥2) | CSS | To examine the biomechanical changes in the lower extremities of individuals with degenerative knee osteoarthritis during gait on level ground, ramps, and stairs |
|
|
|
| 14 | Metcalfe AJ et al., United Kingdom, 2013 [21] |
n = 20, subjects with Knee OA | CSS | To examine the loading of the other joints of the lower limb in individuals with unilateral knee OA |
|
|
|
| 15 | Turcot K et al., Switzerland, 2012 [24] | n = 25, individuals with advanced Knee OA n = 20, healthy elders | CSS | To investigate the full-body strategies utilized during an STS task in individuals with knee OA and the association between STS alterations and clinical measurements |
|
|
|
| 16 | Hicks-Little CA et al., The United States of America, 2011 [17] | n = 18 with knee OA n = 18 healthy matched controls | CSS | To compare various hip, knee, and ankle joint kinematic variables between knee OA subjects and matched healthy controls during stair ascent and descent |
|
|
|
CSS = Cross Section Study; OA = Osteoarthritis; WOMAC = Western Ontario McMaster; EMG = Electromyography; NRS = Numeric Rating Scale; CoP = centre of pressure; STS = sit-to-stand motion; KL = Kellgren-Lawrence scale scores; KOOSs = Knee Osteoarthritis Outcome Score.
3.1. Walking ability
With age, the function of the neuromuscular system declines, and therefore, the risk of falling increases. The internal factors causing knee joint function decline include age, balance, gait ability, decreased muscle strength, decreased cognitive and visual function, and pain [13]. Kinematic variables of horizontal walking, ramp, and stair climbing in individuals with degenerative arthritis show significant differences in the joint angles of the sagittal plane [14]. Compared with horizontal walking, individuals with degenerative arthritis have significantly increased flexion angles of the hip, knee, and ankle joints [15]. Abnormal hip joints and contralateral knee could be a consequence in individuals with unilateral severe knee OA. Compared with horizontal walking, the bending angles of the hip, knee, and ankle joints of individuals with degenerative arthritis significantly increase with an increase in slope angle and stair gait. The change in joint angle increases the load on the knee joint of individuals with OA and, potentially leads to aggravated symptoms [16].
3.2. Kinematics alterations
The proprioception of individuals with knee OA is impaired, which may affect the correct perception of the position and movement of the knee joint and lead to individuals being unable to fully control the end trajectory of the affected limb [17]. Due to pain, the individuals will delay the heel off the ground and extend the double support time to reduce the load on the single stance, to maintain stability or reduce pain. Knee dysfunction is mainly manifested as knee instability, knee pain, and impaired proprioception [7,18]. The natural response to knee instability is to reduce the range of motion and make the knee joint stiff by activating the muscles at a higher amplitude or using higher muscle contractions [8]. There was a large difference in the coordination between the thigh and the lower leg of the affected limb in the late stance and swing stage, likely caused by knee dysfunction. Both gait speed and inter-segment coordination mode were affected by knee OA [19]. The decrease in the individual's gait speed may bring more challenges to stable motion control, possibly because more effort is required to dynamically maintain a slow speed. The individuals change the coordination mode between the segments to adapt to the dysfunction of the knee joint [20]. Reducing the leads of the thigh and foot on the calf may be a strategy for the hip and ankle joints to compensate for the knee joint. The study of inter-segmental coordination provides insights into changes in neuromuscular control of gait in individuals with knee OA. The mean average continuous relative phase (MACRP) of the individual's thigh and calf decreases significantly during the late standing and swinging phases [15]. Individuals with knee OA show alteration in coordination patterns and increased coordination variability of the thighs and lower leg. The MACRP of the lower leg of individuals reduces significantly in the early stage of standing, and increases in the late standing and swing stages [15]. Knee dysfunction leads to changes in coordination of the lower limbs and unstable movement control during functional activities.
3.3. Muscle functions
Contraction of the quadriceps and hamstrings may cause significant alterations in joint loading due to a change in knee reaction force and joint moment. According to Metcalfe's study, individuals with severe unilateral knee OA are at risk of biomechanical abnormalities in the contralateral knee joint and possibly both hip joints [21]. Co-contraction has an additional effect on exceeding the joint load measured using external moments. Individuals with unilateral medial knee OA exhibit abnormal moments in both knees and hips [22].
Findings reported by Anan et al. [23] provide new insights into the quantitative and qualitative improvement of muscle function in individuals with knee OA, where type II fibers of the gluteal and rectus femoris are more active during sit-stand exercise (STS) in individuals with knee OA. STS increases the relative muscle activity of the vastus medialis (VM), utilizing RF to improve muscle contractility during knee extension [24,25]. This may indicate that the completion of the STS itself is maintained, whereas the muscle activity and contraction patterns required for STS differ. Therefore, the efficiency of using the hip and knee extensors to obtain proper motion reduces the overload of the knee extensors [19]. Bouchouras et al. showed that, from standing to sitting, individuals with moderate knee OA preferred to use the larger muscles of knee muscles which activate the hamstrings earlier [26]. The combination of larger muscle co-contraction and co-activation (premature activation of the antagonist muscles) can lead to a massive inactivation of the knee extensors [27].
4. Discussion
The review aimed to study and provide a descriptive summary of the current state of biomechanical changes in people with knee OA. The review focused on evidence from the biomechanics of the lower extremity in the past decade. Emphasis is paid to lower limb changes, as well as the development status of the application of biomechanics in exercise therapy or rehabilitation for individuals with knee OA.
4.1. Biomechanical changes in the lower limbs of individuals with knee OA
Various biomechanical factors influence knee joint pain such as muscle strength and muscle length. There is a strong correlation between BMI and knee OA [33]. The reduction of the hamstring muscle length affects the knee joint. The shortening of the hamstrings leads to the weakening of the quadriceps muscles, resulting in muscle imbalance [34]. Neila et al. studied and suggested that when the knees are stretched and the hamstrings are tight, extra strength of the quadriceps is required, which increases the reaction force to the patella and causes pain in the hip joint [30]. Focusing on hip abductors, training is recommended as an effective intervention to reduce knee abduction in individuals with knee pain. Another reason may be that there is more vertical force on the knee joint which causes the axial load in the articular cartilage to change, leading to the risk of cartilage degenerative changes or knee OA and resulting in joint stiffness and reduced soft tissue flexibility [15].
Individuals with knee OA can walk with their toes outward which can change biomechanics by moving the center of the pressure outwards. In this case, the knee abduction moment can be reduced. As the severity of Knee OA increases, the tendency of hip abduction positions also increases [29]. The abduction position of the hip joint produces a larger abduction moment on the knee joint. This torque requires more force to maintain balance with the knee adduction torque, causing the outside of the knee joint to feel tight. According to the results of Fukaya's study, the mechanical load in the frontal plane of the knee joint is affected by the motion of the hip joint and the moment of the ankle joint [34,35]. The abduction position of the hip joint produces a larger knee abduction moment. Excessive knee abduction moment can be the cause of tightness in lateral structures of the thigh, which is a factor that reduces the function of the knee joint [36].
The combination of lower limb gait kinematics and self-report function can be monitored to observe the response of muscle strengthening intervention in individuals with knee OA [37]. Specifically, by evaluating baseline gait parameters of the hip, knee, and ankle in a multivariate model, as well as self-reported functions, individuals with knee OA exhibited reduced hip external rotator, knee extensor, and ankle inversion muscle force output, along with increased peak knee adduction angles. Ankle inversion, hip abduction, and knee flexion strength were significant predictors of peak pelvic drop angle [31].
A summary of the current literature reveals the following: individuals with knee OA show biomechanical changes of hip, knee, and ankle joints such as a significant defect in strength of ankle varus muscles, weakness of hip abductor muscle, walking with toes outwards, increased knee adduction moment and angle, and decreased knee extensor moment. These findings indicate that there is a complex relationship between lower limb muscle strength and gait, and further examination of the interaction between these factors and how they affect the rehabilitation process is needed [32]. Currently, more biomechanical evidence from explorative, experimental, or longitudinal studies is needed, especially a more complete and comprehensive approach, including the assessment of multiple joints, and combining factors such as individually reported pain and function to improve research and clinical management of knee OA.
4.2. Research equipment and outcome measurement
WOMAC is commonly used to measure functional ability in individuals with knee OA. In the last decade, 3-dimensional motion analysis systems seem to be a common research equipment for detecting biomechanical change in individuals with knee OA during level walking, sit-to-stand, and stair climbing. However, most studies focus on knee mechanics rather than the relative movement of hip, knee, and ankle joints and studies on biomechanical parameters for rotational movement are lacking. Studies typically investigate sagittal and frontal planes. Although knee alignment changes are mainly observed in the frontal plane as bowleg, to better understand knee stability, it is interesting to observe knee rotational kinematics and kinetics. In further studies, we believe that trunk biomechanics and hip abductor muscle activity should be explored more in functional tasks. In the last decade, research using 2-dimensional (2D) measurement has not been reported in individuals with knee OA. Applied 2D measurement is simple and would help gain a better understanding of biomechanical changes in individuals with knee OA. A study by Farrokhi et al. [32] is the only report in the last decade on knee joint contact during walking with dynamic stereo X-ray which explored the details of joint contact area and bone segment movement in gait during motion, which the analysis system could not. However, dynamic stereo X-ray is not common in the biomechanics of knee OA due to some limitations such as cost, researcher skill for performing X-ray examinations, and radiation exposure.
Centre of pressure (COP) is a simple and individual-friendly assessment method. The study investigated standardized COP positions, knee adduction angles (KAA), and knee adduction moments (KAM) patterns in a large group of healthy individuals and compared them with individuals with medial and lateral knee OA [13]. The study also determined the stage of gait where the greatest mechanical adaptation was observed in individuals with knee OA. Although the COP measurement does prove that there are some differences in the gait process between lateral knee OA and healthy individuals, it does not seem to be a sufficiently sensitive marker to be used alone when distinguishing gait patterns between individuals with OA and healthy individuals [38]. Conversely, it may be useful in addition to other gait measurements when evaluating knee OA (such as KAA).
4.3. Perspective, clinical implications, and future research direction
Research demonstrates biomechanical differences in the lower limb between healthy individuals and those with knee OA. All studies presented in Table 2 are cross-sectional explorations. These are difficult to explain in terms of possible cause-effect change. We believe that, in the future, a longitudinal study should be performed to better understand the progressive change in individuals with knee OA.
Measurement of biomechanical factors in individuals with OA is important for monitoring disease and evaluating surgical and non-surgical interventions [39]. In 2005, Alison Chang et al. [40] found that the hip abduction moment slowed down the progression of medial knee OA. They suggested that the hip abductor would help prevent excessive ipsilateral trunk leaning, thereby reducing loading to the knee. Previous studies examined the effect of hip abductor exercise on knee mechanics and found no significant importance on knee adduction moment in individuals with knee OA [41,42]. Although the knee adduction moment did not change after hip abductor training, pain, and functional activity showed improvements. This is interesting for exploring the biomechanical changes underlying the phenomenon. The lack of data on hip, knee, and ankle mechanics in one study may be a limitation of previous studies [41,42]. Therefore, existing data suggests that a more complete and holistic approach, including assessment of hip, knee, and ankle joints in one study, is needed to improve research and clinical management of knee OA [43]. The trunk should be included in the biomechanical study because a high proportion of body weight is located at the trunk. Trunk movement control can highly influence lower limb biomechanics in individuals with knee OA. For a better understanding of lower limb biomechanics in individuals with knee OA, an effective rehabilitation strategy could be developed to delay the progression of knee bowleg.
Currently, most functional assessments of individuals with knee OA are based on self-reports or performance measurements and may not capture changes in motion control. Continuous relative phase (CRP) analysis can be used as an additional outcome measure of knee joint function, providing objective evidence for coordination assessment [44].
Biomechanical study during functional tasks should be carefully interpreted when comparing the findings on the cause of variation of gait speed, instrument, number of limb OA, and knee OA severity. It is difficult and impractical to control the gait speed in individuals with knee OA.
Knee OA severity is ax factor influencing the biomechanics of the lower limb. Therefore, severity information should be reported in every study. It is undeniable that the movement of one joint may affect the movement of another joint [45]. Although the severity of knee OA may vary, usually both knee joints are disturbed. Therefore, future studies need to recruit a sufficient number of subjects and consider the longitudinal changes from the initial stage of knee OA to verify these results. These are the challenges that future research should address [28].
Future studies will need to provide additional information on the overall role of lower limb muscles in influencing knee contact mechanics in individuals with knee OA [46]. These data may help develop the optimal preoperative and postoperative rehabilitation plan for these individuals and help improve their overall quality of life. Future investigators may turn their attention to knee kinematics and compensatory adaptations to pathologically altered proximal and distal joints, incorporating it into rehabilitation programs to increase the range of motion, strength, and balance of lower limb joints. These programs will ultimately help slow the progression of knee OA and improve function, thus improving the individual's ability to perform activities of daily living [47,48]. Moreover, studies on effective rehabilitation should be developed to delay knee OA progression.
5. Conclusions
Biomechanical research on knee OA in the past decade has demonstrated the biomechanics of the hip, knee, and ankle joints and the integrity of the lower limb motor chain have a profound influence on the pathogenesis and treatment of knee OA. According to the aforementioned problems, researchers should pay more attention to the effects of ankle, hip, and even trunk on knee joints in future studies on knee OA. Further research with longitudinal study design should determine the relative importance of different biomechanical and neuromuscular factors in the development and progression of the disease.
Ethical approval
None required for this study design.
Data availability statement
Data included in article/tables/figures/supplementary file. Material/referenced in article. Any other information will be made available on request.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Liying Yang: Conceptualization, Formal analysis, Methodology, Writing – original draft. Komsak Sinsurin: Conceptualization, Formal analysis, Supervision, Writing – review & editing. Fang Shen: Formal analysis, Validation. Binquan Zhao: Formal analysis, Visualization. Ting Gao: Project administration, Validation.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
We appreciate all studies in the review.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2024.e32642.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Corbett M.S., et al. Acupuncture and other physical treatments for the relief of pain due to osteoarthritis of the knee: network meta-analysis. Osteoarthritis Cartilage. 2013;21(9):1290–1298. doi: 10.1016/j.joca.2013.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sharma L. Osteoarthritis of the knee. N. Engl. J. Med. 2021;384(1):51–59. doi: 10.1056/NEJMcp1903768. [DOI] [PubMed] [Google Scholar]
- 3.Escamilla R.F. Knee biomechanics of the dynamic squat exercise. Med. Sci. Sports Exerc. 2001;33(1):127–141. doi: 10.1097/00005768-200101000-00020. [DOI] [PubMed] [Google Scholar]
- 4.Jackson B.D., et al. Reviewing knee osteoarthritis--a biomechanical perspective. J. Sci. Med. Sport. 2004;7(3):347–357. doi: 10.1016/s1440-2440(04)80030-6. [DOI] [PubMed] [Google Scholar]
- 5.Sharma L., et al. Knee instability and basic and advanced function decline in knee osteoarthritis. Arthritis Care Res. 2015;67(8):1095–1102. doi: 10.1002/acr.22572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.da Silva H.G., et al. Biomechanical changes in gait of subjects with medial knee osteoarthritis. Acta Ortop Bras. 2012;20(3):150–156. doi: 10.1590/S1413-78522012000300004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Costa e Silva Cabral A.L., Jorge J.G., Dionisio V.C. Biomechanical analysis during single-leg squat in individuals with knee osteoarthritis. Knee. 2021;28:362–370. doi: 10.1016/j.knee.2020.12.031. [DOI] [PubMed] [Google Scholar]
- 8.Krowchuk N.M., et al. Relationship between foot, ankle and knee biomechanics during walking in those with knee osteoarthritis. Osteoarthritis Cartilage. 2017;25:S120. [Google Scholar]
- 9.Fransen M., et al. Exercise for osteoarthritis of the knee: a Cochrane systematic review. Br. J. Sports Med. 2015;49(24):1554–1557. doi: 10.1136/bjsports-2015-095424. [DOI] [PubMed] [Google Scholar]
- 10.Mills K., Hunt M.A., Ferber R. Biomechanical deviations during level walking associated with knee osteoarthritis: a systematic review and meta-analysis. Arthritis Care Res. 2013;65(10):1643–1665. doi: 10.1002/acr.22015. [DOI] [PubMed] [Google Scholar]
- 11.Page M.J., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int. J. Surg. 2021;88 doi: 10.1016/j.ijsu.2021.105906. [DOI] [PubMed] [Google Scholar]
- 12.Peters M.D.J., et al. Best practice guidance and reporting items for the development of scoping review protocols. JBI Evid Synth. 2022;20(4):953–968. doi: 10.11124/JBIES-21-00242. [DOI] [PubMed] [Google Scholar]
- 13.Monil K., et al. Comparison of gait biomechanics in patients with and without knee osteoarthritis during different phases of gait. Journal of Orthopaedics Trauma and Rehabilitation. 2018;25:11–15. [Google Scholar]
- 14.Igawa T., Katsuhira J. Biomechanical analysis of stair descent in patients with knee osteoarthritis. J. Phys. Ther. Sci. 2014;26(5):629–631. doi: 10.1589/jpts.26.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parekh S., et al. Association between the lower extremity biomechanical factors with osteoarthritis of knee. JMS - Journal of Medical Society. 2019;33(2):76–80. [Google Scholar]
- 16.Son H., Kim K. A kinematic analysis of patients with knee osteoarthritis during gait on level ground, ramps and stairs. J. Phys. Ther. Sci. 2013;25(3):277–280. [Google Scholar]
- 17.Hicks-Little C.A., et al. Lower extremity joint kinematics during stair climbing in knee osteoarthritis. Med. Sci. Sports Exerc. 2011;43(3):516–524. doi: 10.1249/MSS.0b013e3181f257be. [DOI] [PubMed] [Google Scholar]
- 18.Petrella M., et al. Kinetics, kinematics, and knee muscle activation during sit to stand transition in unilateral and bilateral knee osteoarthritis. Gait Posture. 2021;86:38–44. doi: 10.1016/j.gaitpost.2021.02.023. [DOI] [PubMed] [Google Scholar]
- 19.Bokaeian H.R., et al. Effects of an exercise therapy targeting knee kinetics on pain, function, and gait kinetics in patients with knee osteoarthritis: a randomized clinical trial. Adapt. Phys. Act. Q. (APAQ) : Adapt. Phys. Act. Q. (APAQ) 2021:1–19. doi: 10.1123/apaq.2020-0144. [DOI] [PubMed] [Google Scholar]
- 20.Zhou X., et al. Different prevention and treatment strategies for knee osteoarthritis (KOA) with various lower limb exoskeletons-A comprehensive review. Robotica. 2021;39(8):1345–1367. [Google Scholar]
- 21.Metcalfe A.J., et al. The effect of osteoarthritis of the knee on the biomechanics of other joints in the lower limbs. Bone & Joint Journal. 2013;95B(3):348–353. doi: 10.1302/0301-620X.95B3.30850. [DOI] [PubMed] [Google Scholar]
- 22.Drew M.D., Krammer S.M., Brown T.N. Effects of prolonged walking with body borne load on knee adduction biomechanics. Gait Posture. 2021;84:192–197. doi: 10.1016/j.gaitpost.2020.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Anan M., et al. Dynamic frequency analyses of lower extremity muscles during sit-to-stand motion for the patients with knee osteoarthritis. PLoS One. 2016;11(1) doi: 10.1371/journal.pone.0147496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Turcot K., et al. Sit-to-stand alterations in advanced knee osteoarthritis. Gait Posture. 2012;36(1):68–72. doi: 10.1016/j.gaitpost.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 25.Komaris D.S., et al. Identification of movement strategies during the sit-to-walk movement in patients with knee osteoarthritis. J. Appl. Biomech. 2018;34(2):96–103. doi: 10.1123/jab.2016-0279. [DOI] [PubMed] [Google Scholar]
- 26.Bouchouras G., et al. Kinematics and knee muscle activation during sit-to-stand movement in women with knee osteoarthritis. Clin. BioMech. 2015;30(6):599–607. doi: 10.1016/j.clinbiomech.2015.03.025. [DOI] [PubMed] [Google Scholar]
- 27.Bouchouras G., et al. Women with knee osteoarthritis increase knee muscle co-contraction to perform stand to sit. Aging Clin. Exp. Res. 2020;32(4):655–662. doi: 10.1007/s40520-019-01245-z. [DOI] [PubMed] [Google Scholar]
- 28.Wang Y., et al. Coordination of lower limbs in patients with knee osteoarthritis during walking. Gait Posture. 2021;83:160–166. doi: 10.1016/j.gaitpost.2020.10.024. [DOI] [PubMed] [Google Scholar]
- 29.Fukaya T., et al. Characteristics of frontal plane lower limb movement during walking in patients with knee osteoarthritis of varying severity. J. Orthop. Surg. 2019;27(2):7. doi: 10.1177/2309499019848085. [DOI] [PubMed] [Google Scholar]
- 30.Neila M., et al. Biomechanical analysis to characterize the impact of knee osteoarthritis on hip, knee, and ankle kinematics. Journal of Biomedical Engineering and Informatics. 2017;3(2):36. [Google Scholar]
- 31.Park S.K., Kobsar D., Ferber R. Relationship between lower limb Muscle strength, self-reported pain and function, and frontal plane gait kinematics in knee osteoarthritis. Clin. BioMech. 2016;38:68–74. doi: 10.1016/j.clinbiomech.2016.08.009. [DOI] [PubMed] [Google Scholar]
- 32.Farrokhi S., et al. Knee joint contact mechanics during downhill gait and its relationship with varus/valgus motion and muscle strength in patients with knee osteoarthritis. Knee. 2016;23(1):49–56. doi: 10.1016/j.knee.2015.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Elisabeta A., Calina S.S., Maria T. Elements of biomechanics correlated to the body mass index in knee osteoarthritis. Balneo Research Journal. 2020;11(3):379–385. [Google Scholar]
- 34.Kobsar D., et al. Wearable inertial sensors for gait analysis in adults with osteoarthritis-A scoping review. Sensors. 2020;20(24):24. doi: 10.3390/s20247143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fukaya T., et al. Characteristics of frontal plane lower limb movement during walking in patients with knee osteoarthritis of varying severity. J. Orthop. Surg. 2019;27(2) doi: 10.1177/2309499019848085. [DOI] [PubMed] [Google Scholar]
- 36.Raghava Neelapala Y.V., Bhagat M., Shah P. Hip muscle strengthening for knee osteoarthritis: a systematic review of literature. J. Geriatr. Phys. Ther. 2020;43(2):89–98. doi: 10.1519/JPT.0000000000000214. 2001. [DOI] [PubMed] [Google Scholar]
- 37.Steidle-Kloc E., et al. Is muscle strength in a painful limb affected by knee pain status of the contralateral limb? — Data from the Osteoarthritis Initiative. Ann. Anat. 2019;221:68–75. doi: 10.1016/j.aanat.2018.08.003. [DOI] [PubMed] [Google Scholar]
- 38.Kobsar D., et al. Reliability of gait analysis using wearable sensors in patients with knee osteoarthritis. J. Biomech. 2016;49(16):3977–3982. doi: 10.1016/j.jbiomech.2016.11.047. [DOI] [PubMed] [Google Scholar]
- 39.Raghava Neelapala Y.V. Self-reported instability in knee osteoarthritis: a scoping review of literature. Curr. Rheumatol. Rev. 2019;15(2):110–115. doi: 10.2174/1573397114666180628111858. [DOI] [PubMed] [Google Scholar]
- 40.Chang A.H., et al. The relationship between the external knee adduction moment during gait and progression of knee tissue damage over two years in persons with knee osteoarthritis. Osteoarthritis Cartilage. 2014;22:S44–S45. [Google Scholar]
- 41.Bennell K.L., et al. Hip strengthening reduces symptoms but not knee load in people with medial knee osteoarthritis and varus malalignment: a randomised controlled trial. Osteoarthritis Cartilage. 2010;18(5):621–628. doi: 10.1016/j.joca.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 42.Kean C.O., et al. Relationship between hip abductor strength and external hip and knee adduction moments in medial knee osteoarthritis. Clin. Biomech. 2015;30(3):226–230. doi: 10.1016/j.clinbiomech.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 43.Fang M.A., et al. Effects of contralateral versus ipsilateral cane use on gait inPeople with knee osteoarthritis. PM and R. 2015;7(4):400–406. doi: 10.1016/j.pmrj.2014.09.018. [DOI] [PubMed] [Google Scholar]
- 44.Wang Y., et al. Coordination of lower limbs in patients with knee osteoarthritis during walking. Gait Posture. 2021;83:160–166. doi: 10.1016/j.gaitpost.2020.10.024. [DOI] [PubMed] [Google Scholar]
- 45.Yin K.Y., et al. The biomechanical research of lower extremity during stance phase of walking in knee osteoarthritis patients. Med. Sci. Sports Exerc. 2016;48(5):884. 884. [Google Scholar]
- 46.Emery C.A., et al. Establishing outcome measures in early knee osteoarthritis. Nat. Rev. Rheumatol. 2019;15(7):438–448. doi: 10.1038/s41584-019-0237-3. [DOI] [PubMed] [Google Scholar]
- 47.Goncalves G.H., et al. Kinematic alterations of the lower limbs and pelvis during an ascending stairs task are associated with the degree of knee osteoarthritis severity. Knee. 2017;24(2):295–304. doi: 10.1016/j.knee.2017.01.007. [DOI] [PubMed] [Google Scholar]
- 48.Gonçalves G.H., et al. The strategies used by individuals with knee osteoarthritis differ between individuals with early degrees and individuals with moderate degrees of the disease. Osteoarthritis Cartilage. 2017;25:S137. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data included in article/tables/figures/supplementary file. Material/referenced in article. Any other information will be made available on request.