Abstract
Introduction
Human immunodeficiency virus (HIV) infection is a major global public health issue, affecting millions of people annually. University students are among the risk groups in the community because of their high-risk behaviors. Few studies have been conducted on HIV/AIDS preventive behaviors and associated factors among university students. Therefore, focusing on these target populations is crucial because it will help university managers and different stakeholders be informed about the burden of the problem and take different measures to halt the distribution of the infection.
Objective
To assess the predictors of HIV/AIDS preventive behaviors among undergraduate Health Science University students in Northwest Ethiopia in 2022.
Methods
This study used an institution-based cross-sectional design with a single-population proportion formula, and participants were selected using a simple random sampling technique. Data were entered into Epi Data version 4.6.0.2 and exported to SPSS version 26 for cleaning and analysis, and the results were presented using text, graphs, pie charts, percentages, and frequencies. Bivariate and multivariable logistic regression analyses were used, and variables with a p-value of ≤0.25 in the bivariate analysis were entered into the multivariable analysis. A p-value of less than or equal to 0.05 in the multivariable analysis was considered statistically significant.
Result
Out of 287 study participants, 284 of them responded completely, with a response rate of 99.0 %. Among the total respondents, 42.3 % (95 % CI: 37.7, 47.8) of the participants had poor HIV/AIDS preventive behavior. Younger age (AOR: 3.05; 95 % CI (1.243, 7.496)), low perceived susceptibility (AOR: 2.12; 95 % CI (1.179, 3.809), low perceived severity (AOR: 3.00; 95 % CI (1.636, 5.509)), high perceived barriers (AOR: 2.78; 95 % CI (1.487, 5.202)), and having poor HIV/AIDS preventive knowledge (AOR: 3.87; 95 % CI (2.170, 6.919)) were significantly associated with poor HIV/AIDS preventive behaviors.
Conclusion
The HIV/AIDS preventive behavior of participants in this study was poor. Young age, low perceived susceptibility, low perceived severity, high perceived barriers, and poor HIV/AIDS preventive knowledge were predictors of poor HIV/AIDS preventive behavior. It is better to design strategies and programs by the Ministry of Health, the Ministry of Education, university top managers, and other stakeholders to provide appropriate information and focus on behavioral changes in vulnerable population groups.
Keywords: HIV/AIDS, Preventive behavior, University students
1. Introduction
Human immunodeficiency virus (HIV) infection is a major global public health issue that affects millions of people annually [1,2]. According to the United Nations AIDS epidemiological updates, 33.2 million people live with HIV/AIDS throughout the world [3].
It is Africa's 2nd biggest cause of morbidity and mortality and the 5th leading cause of global death among infectious diseases [2].
Sub-Saharan Africa remains most severely affected, with nearly one in every 20 adults living with HIV, accounting for nearly 70 % of the people living with HIV worldwide. The vast majority of people living with HIV are in low- and middle-income countries, including Ethiopia [4,5].
HIV-positive individuals can spread the illness through unprotected sex; however, the disease can be prevented if populations are aware of these risks [6]. Abstinence from sexual activity is the most efficient method for preventing unwanted pregnancy and sexually transmitted illnesses such as HIV/AIDS. Peer pressure, sex myths, misconceptions, and the influence of drugs and alcohol have made this problem difficult to overcome [7]. Abstinence and interventions emphasize the use of condoms and other safer sexual practices as the best approaches to avoid HIV infection [8].
Students of higher learning institutions are assets of society and agents of change; therefore, neglecting their sexual and reproductive health can lead to high social and economic costs [9,10]. Undergraduates are particularly vulnerable to HIV/AIDS as they are part of sexually active population groups, which constitute the peak period for sexual activity, inclination towards sexual networking, and the consequent risk of HIV infection [10,11]. Furthermore, the increased privacy afforded by living away from parents’ homes provides a greater opportunity for students to increase their sexual expression [11]. Therefore, strengthening the preventive behaviors of these students concerning HIV/AIDS is the focus of institutions and nations. Competent and efficient professionals and personnel can be produced if students receive help and support during their stay at the university concerning their HIV/AIDS preventive behavior. Based on the principles of information-motivation behavioral (IMB) skills to fight HIV/AIDS, there has to be a true link between knowledge, attitude, and practice against HIV/AIDS. Yet, the results of studies demonstrate paradoxical findings.
Hence, considering the high-risk behaviors of university students and their potential risks to society may help identify potential abilities to engage in risk reduction behaviors. In addition, little is known about HIV/AIDS preventive behaviors among undergraduate Health Science University students in Northwest Ethiopia. This study aimed to assess the predictors of HIV/AIDS preventive behaviors among undergraduate health science students at Debre Tabor University, Northwest Ethiopia, in 2022.
The findings from this study will help university management know the magnitude of the problem in its society and will allow them to consider different measures to prevent the impact of the problem. Further, it will be used as an input for the Ministry of Health, the Ministry of Education, and other stakeholders to formulate policies and strategies to protect the productive population group from HIV/AIDS and related infections.
2. Methods and materials
2.1. Study design, period, and setting
An institution-based cross-sectional study design was conducted at Debre Tabor University, Health Science College, from August 3 to May 5, 2022. The university is located east of Debre Tabor town, which is the capital city of the South Gondar zone in the Amhara region. It is located 103 km northeast of Amhara and Bahir Dar and 667 km northwest of Addis Ababa.
2.2. Source population
All undergraduate health science students at Debre Tabor University.
2.3. Study population
All selected undergraduate health science students of Debre Tabor University who were available during the data collection period and willing to participate in the study.
2.4. Inclusion criteria
All selected students who were available during the data collection period and willing to participate in the study.
2.5. Exclusion criteria
Students who are unable to provide information due to critical illness or sensory disabilities.
2.6. Sampling procedure and sample size determination
A proportional allocation formula was used to allocate the number of students to each department and year of study in the college. Then a sampling frame was prepared for each department and year of study by having lists of students from the registrar's office. Finally, the study participants were selected using a simple random sampling technique.
The sample size was calculated using the single population proportion formula by taking the estimated proportion of HIV/AIDS preventive behavior at 50 % due to no previous study done in the study area, a 95 % confidence interval (CI), and a 5 % margin of error. To determine the final sample size, a correction formula was used because the total number of health sciences students (source population) was 817 (less than 10,000). The final sample size was 287 after adding a 10 % non-response rate.
2.7. Dependent variable
-
•
HIV/AIDS preventive behavior
2.8. Independent variables
-
•
Sociodemographic variables: sex, age, religion, marital status, origin of residence, ethnicity, department, year of study, and institution of the preparatory school
-
•
Knowledge of HIV/AIDS prevention
-
•
Attitude towards HIV/AIDS prevention
-
•
Practices towards HIV/AIDS prevention
2.9. Operational definitions
Knowledge of HIV/AIDS prevention: This is assessed by 10 yes-or-no knowledge questions with a response of 0 or 1. Then, the mean score was computed, and participants who scored less than the mean score of the knowledge questions were categorized as having poor knowledge, while those who answered the mean and above knowledge questions were classified as having good knowledge [12].
Attitude on HIV/AIDS prevention: This was assessed by nine yes-or-no attitude questions with a response of 0 and 1. Then, the mean scores were computed, and participants who answered below the mean score were considered to have an unfavorable attitude, whereas those who answered mean and above were classified as having a favorable attitude [12]. Practice on HIV/AIDS prevention: This was assessed using Likert scale questions ranging from strongly disagree [1] to strongly agree [5]. The questionnaire contained four components: perceived susceptibility, perceived severity, perceived benefit, and perceived barriers. The mean score was then computed, and participants who scored below the mean score were recorded as having low perceived susceptibility, severity, benefit, and barrier, whereas those who responded mean and above were classified as having high perceived susceptibility, severity, benefit, and barrier [13].
HIV preventive behavior was measured if an individual abstained from sexual intercourse in the last year until the time of data collection or used condoms consistently at each sexual intercourse in the last six months [13].
2.10. Data collection methods and tools
Data was collected with a close-ended Structured self-administered questionnaire, which was adapted from previous studies [[12], [13], [14], [15]]. The questionnaire was prepared in English and translated into Amharic by language and clinical experts. Finally, it was converted into the English language to check its consistency. Three diploma nurses were recruited as data collectors, and one supervisor with an academic rank as an assistant professor was assigned. Training on the content of the questionnaire and how to collect the data was given for one day. The questionnaire consists of five parts. Section One: socio-demographic characteristics of participants; Section Two: knowledge of HIV/AIDS prevention; Section Three: attitude toward HIV/AIDS prevention; Section Four: health belief model; and Section Five: practices towards HIV/AIDS prevention. Participants filled out the questionnaire in the classroom individually under the supervision of the data collectors.
2.11. Data quality assurance
Pretests were conducted on 5.0 % [15] of the samples at Fekede Egzi Health Science and Business College to determine the consistency and applicability of the instrument. The data were checked for completeness before being entered into a computer for analysis. Finally, the collected data were reviewed and checked for completeness before data entry.
2.12. Data processing and analysis
Data were entered and coded in EPI data version 4.6.02 and exported to SPSS version 26.0 for cleaning and analysis. The results are presented in text, percentages, and frequencies using tables and figures. Bivariate and multivariable logistic regression analyses were performed to determine the association of independent variables with the independent and dependent ones. The association between the independent and dependent variables was analyzed to identify factors associated with the outcome variable. Then, variables with a significance level (p-value) of ≤0.25 in bivariate analysis were entered into multivariable analysis. In multivariable analysis, the association between an independent variable and the outcome variable, which was measured using adjusted odds ratios, 95 % confidence intervals (CI), and a p-value less than or equal to 0.05, was considered statistically significant.
2.13. Ethical approval and consent to participate
All methods were performed in accordance with the relevant guidelines and regulations. Ethical approval was obtained from College of Health Sciences Research and Community Service Ethical Review Board on behalf of Debre Tabor University with protocol number of 1884/2022. Written consent was obtained from each subject after the study objectives were explained. In addition to these, before conducting the study, the sample populations were reassured that their participation in the study was voluntary and that they would be free to withdraw from it at any point, and confidentiality was ensured by telling them that their personal information, including their name, would not be recorded. Participants were also informed that the study had no physical or psychological harm and that no incentive would be given.
3. Result
3.1. Socio-demographic characteristics of participants
Among the total participants, 284 (99.0 %) completed the questionnaire completely. Of those respondents, 241 (84.9 %) are within the age group of 18–24 years old. The mean age of participants was 23 with a S.D. ± 1.4 years. The majority (51.4 %) of the respondents were from urban residences, and 88.7 % of them completed their preparatory school in government schools (Table 1).
Table 1.
Socio-demographic characteristics of HIV/AIDS preventive behaviour of undergraduate Health Science University students in Northwest Ethiopia, August 3 to May 5, 2022 (n = 284).
| Variables | Category | Frequency (N) | Percent (%) |
|---|---|---|---|
| Age | 18–24 years | 241 | 84.9 |
| 25–34 years | 43 | 15.1 | |
| Sex | Female | 96 | 33.8 |
| Male | 188 | 66.2 | |
| Marital status | Single | 182 | 64.1 |
| Have a boy/girlfriend | 87 | 30.6 | |
| Married | 15 | 5.3 | |
| Origin of residency | Urban | 146 | 51.4 |
| Rural | 138 | 48.6 | |
| Religion | Orthodox | 270 | 95.1 |
| Muslim | 13 | 4.6 | |
| Protestant | 1 | 0.4 | |
| Ethnicity | Amhara | 159 | 56.0 |
| Oromo | 74 | 26.1 | |
| SNNP | 38 | 13.4 | |
| Others | 13 | 4.6 | |
| Department | Nursing | 40 | 14.1 |
| Anesthesia | 22 | 7.1 | |
| Medicine | 109 | 38.4 | |
| Pharmacy | 51 | 18.0 | |
| Midwifery | 31 | 10.9 | |
| Medical laboratory | 31 | 10.9 | |
| Year of Study | 2nd year | 97 | 34.2 |
| 3rd year | 76 | 26.8 | |
| 4th year | 67 | 23.6 | |
| 5th year | 23 | 8.1 | |
| 6th year | 21 | 7.4 | |
| Institution the student accomplished his/her preparatory school | Governmental | 252 | 88.7 |
| Non-governmental | 32 | 11.3 |
Abbreviations: Southern Nations Nationalities and People.
3.2. Knowledge of HIV/AIDS prevention
The majority of the participants, 221 (77.8 %), responded that avoiding the sharing of sharp materials would prevent HIV/AIDS transmission. Two hundred fifteen (75.7 %) of the participants answered that being faithful would prevent the transmission of HIV/AIDS (Table 2).
Table 2.
Knowledge of HIV/AIDS prevention among undergraduate Health Science University students in Northwest Ethiopia, August 3 to May 5, 2022 (n = 284).
| Variables | Category | Frequency (N) | Percent (%) |
|---|---|---|---|
| Do you think abstinence increases the prevention of HIV/AIDS? | Yes | 201 | 70.8 |
| No | 30 | 10.6 | |
| Do you think being faithful prevents the transmission of HIV/AIDS? | Yes | 215 | 75.7 |
| No | 69 | 24.3 | |
| Do you think using condoms consistently prevents HIV/AIDS? | Yes | 184 | 64.8 |
| No | 100 | 35.2 | |
| Do you think not sharing sharp materials will prevent HIV/AIDS? | Yes | 221 | 77.8 |
| No | 63 | 22.2 | |
| Do you think getting health information for HIV/AIDS prevents you from the disease? | Yes | 207 | 72.9 |
| No | 77 | 27.1 | |
| Do you think treatment of STIs decreases the risk of getting HIV/AIDS? | Yes | 177 | 62.3 |
| No | 107 | 37.7 | |
| Do you think male circumcision increases the risk of getting HIV/AIDS? | Yes | 114 | 40.1 |
| No | 170 | 59.9 | |
| Do you think PMTCT decrease the risk of HIV/AIDS? | Yes | 168 | 59.2 |
| No | 116 | 40.8 | |
| Do you think giving ART to HIV patients decreases the risk of HIV/AIDS? | Yes | 167 | 58.8 |
| No | 117 | 41.2 | |
| Do you think giving ART to exposed individuals prevents HIV/AIDS? | Yes | 122 | 43.0 |
| No | 162 | 57.0 |
Abbreviations: AIDS; Acquired Immune Deficiency Syndrome: ART; Anti Retro-viral Therapy: HIV; Human Immunodeficiency Virus: PMTCT; Prevention of Mother to Child Transmissions.
3.3. Attitude-related questions on HIV/AIDS prevention
Of 284 respondents, 61 perceived that HIV/AIDS could not be transmitted at night, and only 111 perceived that HIV/AIDS could be transmitted by kissing (Table 3).
Table 3.
Attitude on HIV/AIDS prevention among undergraduate Health Science University students in Northwest Ethiopia, August 3 to May 5, 2022 (n = 284).
| Variables | Category | Frequency (N) | Percent (%) |
|---|---|---|---|
| Do you perceive the withdrwal of the penis before ejaculation prevents HIV/AIDS transmission? | Yes | 134 | 47.2 |
| No | 150 | 52.8 | |
| Do you perceive washing genitals after sexual intercourse prevents HIV/AIDS transmission? | Yes | 140 | 49.3 |
| No | 144 | 50.7 | |
| Do you perceive HIV/AIDS can be transmitted by kissing? | Yes | 111 | 39.1 |
| No | 173 | 60.9 | |
| Do you perceive sharing of sharp materials can transmit HIV/AIDS? | Yes | 202 | 71.1 |
| No | 82 | 28.9 | |
| Do you perceive HIV/AIDS can be transmitted through mosquito bites? | Yes | 62 | 21.8 |
| No | 222 | 78.2 | |
| Do you perceive HIV/AIDS is transmitted through anal/oral sex? | Yes | 192 | 67.6 |
| No | 92 | 32.4 | |
| Does coitus interrupt the prevention of HIV/AIDS? | Yes | 70 | 24.6 |
| No | 214 | 75.4 | |
| Is there any vaccination for HIV/AIDS? | Yes | 157 | 55.3 |
| No | 127 | 44.7 | |
| Do you perceive HIV/AIDS can not be transmitted at night? | Yes | 61 | 21.5 |
| No | 223 | 78.5 |
3.4. Health belief model for assessment of HIV/AIDS preventive behavior
Among the total participants, 83 (29.2 %) of them never had sexual intercourse. However, only 115 (40.5 %) of them had HIV testing in the last three months (Table 4).
Table 4.
Health belief model on HIV/AIDS preventive behaviour of undergraduate Health Science University students in Northwest Ethiopia, August 3 to May 5, 2022 (n = 284).
| Variables | Category | Frequency (N) | Percent (%) |
|---|---|---|---|
| Ever sexual intercourse | Yes | 83 | 29.2 |
| No | 201 | 70.8 | |
| Do you have Sexual activity in the last 12 months? | Yes | 141 | 49.6 |
| No | 143 | 50.4 | |
| Do you have a sexual partner? | Yes | 101 | 35.6 |
| No | 183 | 64.4 | |
| Type of sexual partners | Regular partner | 71 | 25.0 |
| Casual partner | 26 | 9.2 | |
| Commercial sex worker | 4 | 1.4 | |
| Number of sexual partners | One | 77 | 27.1 |
| Two and above | 24 | 8.5 | |
| Condom use on last sexual intercourse | Yes | 90 | 31.7 |
| No | 194 | 68.3 | |
| The habit of condom use | Consistently | 28 | 9.9 |
| Sometimes | 46 | 16.2 | |
| Rarely | 23 | 8.1 | |
| No | 187 | 65.8 | |
| HIV test within the last three months | Yes | 115 | 40.5 |
| No | 169 | 59.5 | |
| Shared sharp materials in the last three months | Yes | 80 | 28.2 |
| No | 202 | 71.1 |
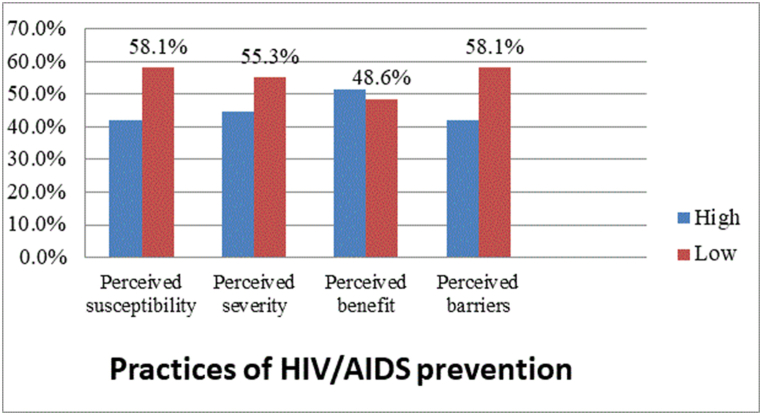
3.5. Practices of HIV/AIDS prevention
More than fifty eight percent of the respondents had low perceived susceptibility and perceived barriers to HIV/AIDS prevention (Fig. 1).
Fig. 1.
Practices on HIV/AIDS prevention among undergraduate Health Science University students in Northwest Ethiopia, August 3 to May 5, 2022 (n = 284).
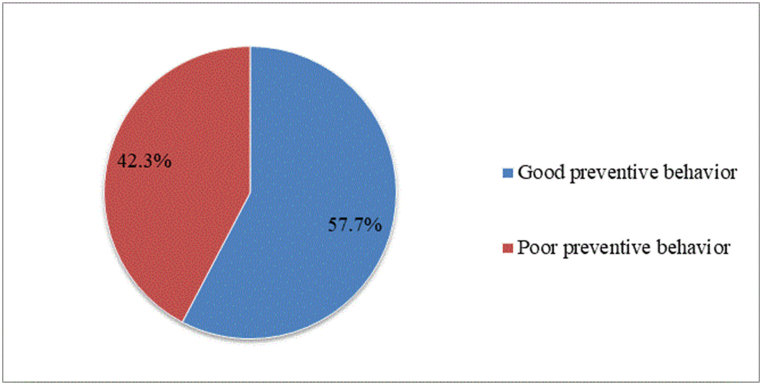
3.6. HIV/AIDS preventive behavior of participants
Out of the total respondents, 42.3 % (95 % CI: 37.7, 47.8) of them had poor HIV/AIDS preventive behavior (Fig. 2).
Fig. 2.
HIV/AIDS preventive behaviour of undergraduate Health Science University students in Northwest Ethiopia, August 3 to May 5, 2022 (n = 284).
3.7. Factors associated with HIV/AIDS preventive behavior
Bivariate logistic regression was performed to identify the factors associated with HIV/AIDS preventive behavior. In the bivariate analysis, age, origin of residence, previous preparatory school, perceived susceptibility, perceived severity, perceived benefit, perceived barriers, HIV/AIDS preventive knowledge, and HIV/AIDS preventive attitudes were significantly associated with HIV/AIDS preventive behavior.
In multivariable logistic regression analysis, younger students were three times more likely to have poor HIV/AIDS preventive behaviors as compared with older students (AOR: 3.05; 95 % CI (1.243, 7.496)).
In this multivariable analysis, students who had low perceived susceptibility were 2.12 times more likely to have poor HIV/AIDS preventive behavior compared to those who had high perceived susceptibility (AOR: 2.12; 95 % CI: 1.179–3.809).
Students with low perceived severity were three times higher than those who had poor HIV/AIDS preventive behaviors as compared with those with high perceived severity (AOR: 3.00; 95 % CI (1.636, 5.509)).
Another multivariable analysis on students' perceived barriers towards HIV/AIDS preventive behavior showed that students with high perceived barriers were 2.78 times more likely to have poor preventive behavior than those students with low perceived barriers (AOR: 2.78; 95 % CI (1.487, 5.202)).
Finally, students' HIV/AIDS prevention knowledge was analyzed to assess the effect of preventive knowledge on HIV/AIDS preventive behavior. So, based on the analysis, students who had poor knowledge were 3.87 times more likely to have poor HIV/AIDS preventive behavior compared with students with good HIV/AIDS preventive knowledge (AOR: 3.87; 95 % CI (2.170, 6.919)) with a p-value of ≤0.05 (Table 5).
Table 5.
Bivariate and multivariable analysis of HIV/AIDS preventive behaviour of undergraduate Health Science University students in Northwest Ethiopia, August 3 to May 5, 2022 (n = 284).
| Variables | Category | HIV/AIDS preventive behaviour |
COR (95 % CI) | AOR (95 % CI) | P-value | |
|---|---|---|---|---|---|---|
| Poor | Good | |||||
| Age | 18–24 | 112 | 129 | 3.80 (1.692–8.528) | 3.05 (1.243–7.496) | 0.015 |
| 25–34 | 8 | 35 | 1 | 1 | ||
| Origin of Residence | Urban | 90 | 56 | 1 | 1 | |
| Rural | 74 | 64 | 1.39 (0.867–2.229) | 1.58 (0.868–2.859) | 0.135 | |
| Preparatory school | Governmental | 153 | 99 | 1 | 1 | |
| Nongovernmental | 11 | 21 | 2.95 (1.363–6.385) | 1.83 (0.718–4.681) | 0.205 | |
| Perceived susceptibility | Low | 81 | 84 | 1.98 (1.212–3.227) | 2.12 (1.179–3.809) | 0.012 |
| High | 39 | 80 | 1 | 1 | ||
| Perceived severity | Low | 86 | 71 | 3.31 (2.003–5.479) | 3.00 (1.636–5.509) | 0.000 |
| High | 34 | 93 | 1 | |||
| Perceived benefit | Low | 73 | 65 | 2.37 (1.461–3.830) | 1.32 (0.709–2.447) | 0.383 |
| High | 47 | 99 | 1 | 1 | ||
| Perceived barrier | Low | 110 | 55 | 1 | 1 | |
| High | 54 | 65 | 2.41 (1.483–3.909) | 2.78 (1.487–5.202) | 0.001 | |
| Knowledge | Good | 124 | 48 | 1 | 1 | |
| Poor | 40 | 72 | 4.65 (2.791–7.746) | 3.87 (2.170–6.919) | 0.000 | |
| Attitude | Favorable | 120 | 71 | 1 | 1 | |
| Unfavorable | 44 | 49 | 1.88 (1.140–3.109) | 1.35 (0.733–2.499) | 0.334 | |
Notes: 1 = Reference group.
Abbreviations: CI; Confidence Interval: COR; Crude Odds Ratio: AOR; Adjusted Odds Ratio.
4. Discussion
HIV/AIDS is a major global public health issue, affecting millions of people annually. It mainly attacks sexually active age groups, such as university students, who are critical to the socio-economic fabric of communities and nations; therefore, protecting them from HIV/AIDS is vital. The preventive behaviors of university students concerning HIV/AIDS are the main concern for economical and social development of society and the country at large.
This study further revealed that 39.4 % of the participants had poor knowledge of HIV/AIDS. Similarly, studies conducted among Dilla and Madawalabu University students in Ethiopia and the young population of Gabon showed that 47.0 %, 48.6 %, and 48.1 % of the participants had poor knowledge of HIV/AIDS, respectively [14,16,17]. This discrepancy might be because previous studies were conducted on participants who had limited information on HIV/AIDS, unlike the current study, which focused on participants for whom health information is expected to be accessed under different conditions, including the curriculum and their clinical exposure.
Furthermore, studies done in China among college students revealed that only 19.2 % of the participants had poor knowledge of HIV/AIDS [18]. This may be due to socioeconomic differences, resulting in good access to information on different alternatives.
The study also examined the attitudes of participants, and it found that 32.7 % of the respondents had unfavorable attitudes toward HIV/AIDS. In line with this, a study conducted at Dilla University, Ethiopia, and Gabon revealed that 42.0 % and 44.3 % of the participants had poor attitudes toward HIV/AIDS, respectively [14,17]. This difference may be due to the study year and population differences in information accessibility. A study conducted in the United States of America among black university students showed that only 12.2 % of respondents had poor attitudes toward HIV/AIDS [19]. This discrepancy might be due to the socioeconomic differences in the study settings.
In this study, 42.3 % (95 % CI; 37.7, 47.8) of the participants had poor HIV/AIDS preventive behavior. This is similar to a study conducted in the southeastern Ethiopian Dima District [12]. This similarity might be because the majority of the participants in both studies were young and sexually active.
This is higher than the study conducted among college students in Gambella town, Southwest Ethiopia [13]. This might be due to the distance of the participants from their family members, which alters the students’ behavior, and the presence of diversified population groups in the current study.
Furthermore, the current study is lower than previous studies conducted in the bench-maji zone of southern Ethiopia [15] and the majang zone of the Gambella region [2]. This discrepancy might be because participants in the current study had better information about the problem since it is part of their curriculum.
In this study, age, perceived susceptibility, perceived severity, perceived barriers, and HIV/AIDS prevention knowledge were significant predictors of HIV/AIDS preventive behaviors.
Younger students were more likely to have poor HIV/AIDS preventive behaviors than older students. This is similar to the study conducted in the Majang zone of the Gambella region, Ethiopia [2], but contradicts the study conducted among college students in Gambella town [13]. The discrepancy between these two studies might be due to sample size differences and the sociodemographic characteristics of the participants.
Those with low perceived susceptibility were more likely to have poor HIV/AIDS preventive behaviors than those with high perceived susceptibility. Similarly, a study conducted among mining workers in southeast Ethiopia revealed that participants with high perceived susceptibility had good preventive behaviors [12]. This might be due to the fact that when individuals perceive that they are susceptible to something, they will take care of themselves from it.
Similarly, students with low perceived severity were more likely to have poor HIV/AIDS preventive behaviors than those with high perceived severity. This is similar to a study conducted among college students in Gambella [13], which revealed that high perceived severity resulted in good preventive behavior. It might be because when students perceive that the problem is severe, they may develop a better behavioral plan for its prevention.
Additionally, in this study, perceived barriers to HIV/AIDS preventive behavior showed that students with high perceived barriers were more positively associated with poor preventive behavior than those with low perceived barriers. Participants with multiple barriers to HIV/AIDS prevention, such as distance from the health institution to seek health care, considering that the test is painful, and being afraid of having an HIV/AIDS test due to fear of bad results, might be barriers to poor prevention behavior.
According to this study, students who had poor HIV/AIDS prevention knowledge were more likely to have poor HIV/AIDS preventive behavior than students with good HIV/AIDS prevention knowledge. This is in line with studies conducted at selected universities in the Amhara region of Ethiopia with college students in Gambella town, the Majang Zone of Gambella, and southeast Ethiopia [2,12,13,20]. This similarity might be because having good knowledge of HIV/AIDS will encourage individuals to apply different preventive practices because they may understand the consequences of poor preventive practices.
4.1. Limitations of the study
This study was cross-sectional and may not explain the temporal relationship between the outcome and explanatory variables. In addition, the study was not supported by qualitative data and only used a closed-ended questionnaire, which might have limited the participants’ responses. The study might be exposed to social desirability bias since the issue is sensitive in our community context.
5. Conclusion and recommendation
The HIV/AIDS preventive behaviors of the participants in this study were found to be poor. Young age, low perceived susceptibility, low perceived severity, high perceived barriers, and poor HIV/AIDS preventive knowledge were predictors of poor HIV/AIDS preventive behavior. It is better to design strategies and programs by the Ministry of Health, the Ministry of Education, university top managers, and other stakeholders to provide appropriate information and focus on behavioral changes in vulnerable population groups.
Funding statement
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
All the data supporting the study findings are within the manuscript. The additional detailed raw data sets used during this study are available from the corresponding author upon reasonable request.
Additional information
No additional information is available for this paper.
CRediT authorship contribution statement
Adane Birhanu Nigat: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. Moges Wubneh Abate: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. Agimasie Tigabu Demelash: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. Berihun Bantie: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. Nigusie Selomon Tibebu: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. Chalie Marew Tiruneh: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. Tigabu Desie Emiru: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. Mehd Abdu Yimam: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. Getasew Legas: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. Yohannes Shumet Yimer: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2024.e32453.
Contributor Information
Adane Birhanu Nigat, Email: adanebirhanu23@gmail.com.
Moges Wubneh Abate, Email: wmoges7@gmail.com.
Agimasie Tigabu Demelash, Email: ethiomom23@gmail.com.
Berihun Bantie, Email: berihunbante@gmail.com.
Nigusie Selomon Tibebu, Email: nigie1221@gmail.com.
Chalie Marew Tiruneh, Email: marewcha@gmail.com.
Tigabu Desie Emiru, Email: tigabud05@gmail.com.
Mehd Abdu Yimam, Email: mehdabdu@gmail.com.
Getasew Legas, Email: getasewlegas@gmail.com.
Yohannes Shumet Yimer, Email: yohannesdtu@gmail.com.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.UNAIDS . 2018. UNAIDS Data 2018. [Google Scholar]
- 2.Yosef T., Wondimu W., Nigussie T., Asefa A., Qanche Q., Mekonnen B., et al. Factors associated with HIV preventive behavior among adults in majang zone of Gambella region, Southwest Ethiopia. Front. Med. 2022;9(April):1–7. doi: 10.3389/fmed.2022.807730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kayiki S.P., Forste R. HIV/AIDS-related knowledge and perceived risk associated with condom use among adolescents in Uganda. Afr. J. Reprod. Health. 2011;15(1):57–63. [PubMed] [Google Scholar]
- 4.Shewamene Z., Legesse B., Tsega B., Bhagavathula A.S., Endale A. Consistent condom use in HIV/AIDS patients receiving antiretroviral therapy in northwestern Ethiopia: implication to reduce transmission and multiple infections. HIV AIDS Res. Palliat. Care. 2015;7:119–124. doi: 10.2147/HIV.S79122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ali M.S., Tesfaye Tegegne E., Kassa Tesemma M., Tesfaye Tegegne K. Consistent condom use and associated factors among HIV-positive clients on antiretroviral therapy in north west Ethiopian health center, 2016 GC. AIDS Res Treat. 2019;2019 doi: 10.1155/2019/7134908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Setswe G. Abstinence and faithfulness programmes for the prevention of HIV/AIDS among young people: what are the current debates? South African. Fam. Pract. 2007;49(8):5–10. [Google Scholar]
- 7.Koffi A.K., Kawahara K. Sexual abstinence behaviour among never-married youths in a generalized HIV epidemic country: evidence from the 2005 Cte d'Ivoire AIDS indicator survey. BMC Publ. Health. 2008;8:1–15. doi: 10.1186/1471-2458-8-408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Underhill K., Operario D., Montgomery P. Systematic review of abstinence-plus HIV prevention programs in high-income countries. PLoS Med. 2007;4(9):1471–1485. doi: 10.1371/journal.pmed.0040275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wordofa D., Shiferaw S. Sexual risk behaviors and its associated factors among undergraduate students in Madda Walabu university, southeast Ethiopia : a facility- based cross-sectional study epidemiology. Open Access. 2015;5(4) [Google Scholar]
- 10.Tura G., Alemseged F., Dejene S. Original article risky sexual behavior and predisposing factors among students of jimma university. ETHIOPIA. 2012;22(3):170–180. [PMC free article] [PubMed] [Google Scholar]
- 11.Amante T.D., Oljira L., Assefa N. 2012. Patterns of Sexual Risk Behaviour Among Undergraduate University Students in Ethiopia: a Cross-Sectional Study. June 2014. [PMC free article] [PubMed] [Google Scholar]
- 12.Nigussie T., Mamo Y., Qanche Q., Yosef T., Wondimu W., Asefa A. Research article HIV preventive behaviors and associated factors among gold mining workers in Dima District, Southwest Ethiopia. 2019 : Community-Based Cross-Sectional Study. 2021;2021:1–9. doi: 10.1155/2021/4797590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gizaw A.T., Abreha G.K., Legesse T., Hailesilassie H. Predictors of HIV/AIDS preventive behaviour among college students in Gambella town, Southwest Ethiopia using health belief model. J AIDS HIV Res [Internet] 2018;10(2):13–21. https://academicjournals.org/journal/JAHR/article-abstract/DC7150A55952 Available from: [Google Scholar]
- 14.Gemeda T.T., Gandile A.U., Bikamo D.S. ORIGINAL RESEARCH ARTICLE HIV/AIDS knowledge, attitude university students, Ethiopia and practice among Dilla. Afr. J. Reprod. Health. 2017;21(September):49–61. doi: 10.29063/ajrh2017/v21i3.4. [DOI] [PubMed] [Google Scholar]
- 15.Abdissa H.G., Lemu Y.K., Nigussie D.T. HIV preventive behaviour and associated factors among mining workers in Sali traditional gold mining site bench maji zone, Southwest Ethiopia : a cross-sectional study. 2014:2–9. doi: 10.1186/1471-2458-14-1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kene C. ORIGINAL research HIV/AIDS-related knowledge of university students in southeast Ethiopia : a cross-sectional. Surveyor. 2021:681–690. doi: 10.2147/HIV.S300859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Christane N.A. HIV/AIDS prevalence, knowledge, attitudes and related behaviours among young people in Libreville. Gabon. IOSR J Humanit Soc Sci. 2014;19(1):59–65. [Google Scholar]
- 18.Zhang L., Yu H., Luo H., Rong W., Meng X., Du X., et al. HIV/AIDS-Related knowledge and attitudes among Chinese college students and associated factors: a cross-sectional study. Front. Public Health. 2022;9(January):1–9. doi: 10.3389/fpubh.2021.804626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Andrew P., Bhuiyan A.R., Mawson A., Shahbazi M. Assessment of attitudes toward HIV and AIDS among undergraduate students at a historically black university. J AIDS HIV Treat. 2019;1(2):25–32. [Google Scholar]
- 20.Care P. 2021. Behavioral Response to HIV/AIDS Prevention Messages Among Students in Selected Universities of Amhara Region, Northwest Ethiopia : an Extended Parallel Process Model; pp. 115–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All the data supporting the study findings are within the manuscript. The additional detailed raw data sets used during this study are available from the corresponding author upon reasonable request.