Abstract
Sepsis accounts for a significant proportion of preventable deaths worldwide and early treatment has been found to be a mainstay of decreasing mortality. Early identification of sepsis in the first-aid setting is critical as this results in a shorter time to hospital presentation and management with antibiotics and initial resuscitation. Our aim was to explore the existing literature related to either sepsis recognition or awareness of sepsis by first-aid providers who are evaluating an adult suspected of an acute infection.
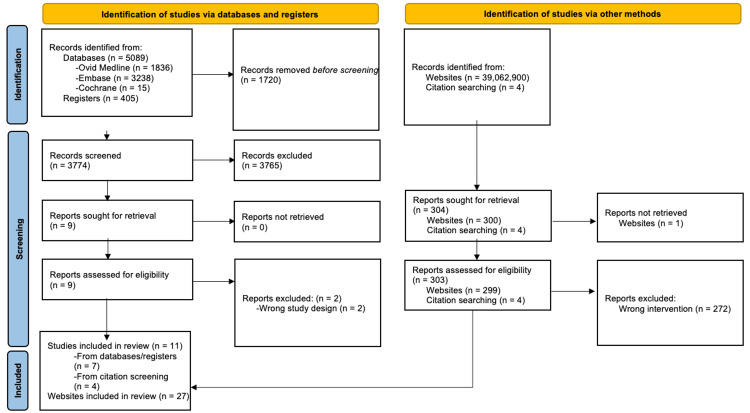
Our scoping review was performed as part of the International Liaison Committee on Resuscitation's (ILCOR) continuous evidence evaluation process to update the 2024 ILCOR Consensus on Science with Treatment Recommendations. We searched Embase, Medline, and Cochrane databases from their inception to January 17, 2023, with updated searches performed on November 21, 2023, and December 2, 2023. The gray literature search was conducted on August 29, 2023. The population included adults presenting with an acute illness exhibiting signs and symptoms of a severe infection. Outcomes included sepsis recognition or awareness of sepsis by a lay first-aid provider.
After reviewing 4380 potential sources, four reviews (three systematic reviews and one scoping review), 11 observational studies, and 27 websites met the inclusion criteria. No study directly addressed our PICOST (Population, Intervention, Comparator, Outcomes, Study Design, and Timeframe) question as none were performed in the first-aid setting. Three systematic reviews and nine observational studies that assessed the ability of early warning scores to detect sepsis and predict adverse outcomes secondary to sepsis had inconsistent results, but many found the screening tools to be useful. One scoping review and one observational study found public knowledge and awareness of sepsis to be variable and dependent upon healthcare employment, location, education level, ethnicity, sex, and age. Signs and symptoms associated with sepsis as listed by gray literature sources fell primarily under nine general categories as a means of educating the public on sepsis recognition.
Although this scoping review did not identify any studies that directly addressed our outcomes, it highlights the need for future research to better understand the recognition of sepsis in first-aid settings.
Keywords: lay provider, first aid, identification, recognition, illness, infection, sepsis
Introduction and background
Sepsis is a critical medical condition characterized by a dysregulated host response to infection, leading to organ dysfunction and potential mortality [1]. With its potential for rapid progression and poor outcomes, frequently requiring admission to the medical wards or an intensive care unit (ICU), sepsis poses a significant burden to healthcare systems worldwide [2]. While the precise global incidence of sepsis is difficult to ascertain, estimates suggest that millions of cases occur annually and it is a major public health issue [3]. Hospital mortality rates have been reported as ranging between 15% and 30% in high-income countries (HICs), increasing to 50% or more in low- to middle-income countries (LMICs) [4,5].
Sepsis presents with a diverse array of signs and symptoms that can vary depending on the underlying infection, the patient's age, and comorbidities. Common clinical manifestations include fever, lethargy, tachycardia, tachypnea, altered mental status, and subjectively feeling unwell, although these may or may not be present. The non-specific nature of these features often results in sepsis mimicking other conditions and diagnostic uncertainty [6].
Prompt recognition and early intervention are paramount in managing sepsis effectively. Early administration of appropriate antibiotics and resuscitative measures have been shown to improve outcomes, including reducing mortality rates [7-9]. Identifying sepsis in its early stages has proven to be challenging, even for healthcare providers with access to advanced testing. Screening tools have been developed to assist with the identification of sepsis, examples of which include vital signs, Systemic Inflammatory Response Syndrome (SIRS) criteria, quick Sequential Organ Failure Score (qSOFA) criteria, or Sequential Organ Failure Assessment (SOFA) criteria, National Early Warning Score (NEWS), NEWS2, Modified Early Warning Score (MEWS), and Phoenix Sepsis Score [10-13]. However, the utility of these scores has been limited to the healthcare setting. A major limitation to these tools is that they cannot be universally applied by those assessing an acutely ill person for possible sepsis, specifically the lay provider who is often the initial contact and lacks the ability to obtain some of the required variables. Consequently, first-aid providers are limited to more basic means of evaluating someone suspected of sepsis, relying solely on subjective and objective signs of infection and hypoperfusion.
Despite the critical importance of early recognition and intervention, there is limited research evaluating a first-aid provider’s ability to identify sepsis. We sought to explore the existing literature that was related to either sepsis recognition or awareness of sepsis by first-aid providers who are evaluating an adult suspected of an acute infection.
Review
This scoping review was developed as part of the International Liaison Committee on Resuscitation's (ILCOR) continuous evidence evaluation process, conducted by the ILCOR First Aid Task Force [14] and was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) [15].
Questions and objectives
We sought to answer the following PICOST (Population, Intervention, Comparator, Outcome, Study Designs and Timeframe) question, which was defined as:
Population: Adults who are being evaluated by a first-aid provider for an acute illness.
Intervention: The identification of any specific signs or symptoms (e.g., pale, blue, or mottled skin, lips or tongue, gums, nails; non-blanching rash; difficulty in breathing or rapid respiratory rates; rigors/shivering; lack of urination in a day; muscle pain; confusion or slurred speech).
Comparator: Fever (≥ 38°C) with signs of infection.
Outcome: 1. Recognition of a seriously ill person requiring hospitalization or evaluation by a physician for sepsis, 2. Increased awareness of sepsis.
Study designs: Randomized controlled trials (RCTs) and non-randomized studies (non-randomized controlled trials, interrupted time series, controlled before-and-after studies, cohort studies) are eligible for inclusion. Gray literature and social media and non-peer reviewed studies, unpublished studies, conference abstracts, and trial protocols are eligible for inclusion. All relevant publications in any language are included as long as there is an English abstract.
Timeframe: All years.
Inclusion and exclusion criteria
Our population included adults (aged 18 years and older) experiencing an acute illness exhibiting signs and symptoms concerning sepsis as suspected in the prehospital setting. We excluded opinions and consensus papers.
Information sources and search strategies
We conducted our search using three separate strategies: (1) published literature through Embase, Medline, and Cochrane databases; (2) hand-searching for relevant articles; and (3) gray literature search using Google.com in an attempt to identify knowledge gaps in this area.
Peer-Reviewed Literature
With the assistance of an information specialist, an initial search strategy was developed and executed in Embase, Medline, and Cochrane Database of Systematic Reviews and Cochrane Central Register of Controlled Trials on January 17, 2023 (Appendix 1). Updated searches were performed on November 21, 2023, and again on December 2, 2023, to comply with protocols outlined by the ILCOR leadership (Appendixes 2, 3).
Gray Literature
In order to supplement the database search and identify the current initiatives geared toward educating the public on sepsis recognition, gray literature searches were performed on August 29, 2023, through Google.com using key terms “Sepsis” and “First Aid” (747,000 results); “Sepsis Recognition” and “Public” (15,900 results); and “Sepsis Recognition” and “Signs and Symptoms” (38,300,000 results) (Appendix 4). The following were criteria for inclusion: (1) primary website from a sepsis awareness campaign, healthcare organization, first-aid training course, or government sepsis program initiative; (2) listed specific signs and symptoms for sepsis identification. The results were excluded if healthcare providers were the targeted audience.
Screening and selection of sources
Peer-Reviewed Literature
The initial search retrieved 5494 results, and after removing duplicates, 3774 unique articles remained for title and abstract screening. Records were downloaded and imported into an EndNote (version 21, Clarivate, Philadelphia, PA, 2013) database to facilitate removal of duplicates and screening. Four independent reviewers (AK, WS, TD, and GF) screened titles and abstracts using Rayyan [16] (www.rayyan.ai), a web-based tool, after which nine articles were identified for full-text review. Four additional articles were identified from a handpicked search. Discrepancies between the reviewers were resolved through discussion after which eleven studies met the final inclusion criteria. A summary of the screening process is shown in the PRISMA diagram (Figure 1). Updated searches performed on November 21, 2023, and December 2, 2023, retrieved 302 results available for screening. Nine articles underwent full-text review, after which four were included.
Figure 1. PRISMA Diagram of Included Studies.
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Gray Literature
One reviewer (AK) screened the first 100 titles of each search for relevance, and after removal for redundancy, a total of 27 were selected for inclusion in the review.
Data extraction and analysis
Data from included data sources were extracted into an extraction matrix that was developed a priori. Data were subjected to simple descriptive analysis and organized into major topic domains and presented narratively. As is permitted in a scoping review, no formal risk of bias assessments were undertaken.
Results
Study Characteristics
We identified three systematic reviews [17-19], one scoping review [20], and 11 observational studies [21-31] for inclusion, all of which were conducted in HICs; none were performed in the first-aid setting. No published studies directly addressed a first-aid provider’s recognition of sepsis through the presence of specific signs or symptoms in a seriously ill person with the subsequent need to seek further medical attention. Given the lack of any direct evidence, we included studies that were performed in either the prehospital or in-hospital settings, or by emergency medical service (EMS) providers, and extrapolated the data to suggest relevance to the first-aid setting. Studies evaluating physiologic variables that a lay provider could obtain in a first-aid setting, such as temperature, heart rate, and respiratory rate, either in isolation or when assessing using clinical scoring tools, were selected for inclusion. Seven studies assessed screening score performance in the prehospital or in-hospital setting to identify sepsis [17-19,22-25]. One study explored the clinical signs and field assessments by emergency medical service providers of patients with and without a suspicion of sepsis [29]. Five studies evaluated prehospital and emergency triage screening score prediction for adverse in-hospital outcomes (ICU admission or mortality) [21,26,28,30,31]. Two studies evaluated the awareness and knowledge of sepsis by various members of the population and identified potential contributing factors affecting the results [20,27]. The characteristics of the included studies are provided in Tables 1, 2.
Table 1. Characteristics of and Findings in the Included Review Studies.
Abbreviations: ED, emergency department; EMS, Emergency Medical Services; HR, heart rate; qSOFA, quick Sequential Organ Failure Assessment; SIRS, Systemic Inflammatory Response Syndrome; RR, respiratory rate
| Author, year | Study design | Number of articles identified (n) | Population | Intervention | Key findings | Conclusions |
| De Silva et al. 2023 [17] | Systematic review | (n=18) | People with suspected or confirmed sepsis in the emergency setting | Compared sensitivity and specificity of qSOFA to 31 other screening tools for the diagnosis of sepsis | qSOFA produced high specificity and low sensitivity for emergency diagnosis of sepsis among the included studies. | No single screening tool is recommended at this time for use in the emergency setting. A combination of qSOFA and SIRS can improve the prognostic accuracy of 30-day mortality for ED presentation. |
| Lane et al. 2016 [18] | Systematic review | Total: (n=16); Identification: (n=8); Management: (n=7); Both: (n=1) | Articles describing the accuracy of prehospital sepsis identification and prehospital management of patients with sepsis, severe sepsis, or septic shock by EMS | None | The most common approach to identification involved applying SIRS criteria or a combination of vital signs. Primary vital signs considered in seven studies: Temperature, HR, RR. | EMS providers can identify patients with sepsis with modest sensitivity and specificity. The use of provider impression alone had poor sensitivity. Fluid resuscitation was the most commonly described treatment. |
| Smyth et al., 2016 [19] | Systematic review | Total: (n=9); Development of tool: (n=3); Paramedic diagnosis of sepsis: (n=6) | Articles addressing the identification of sepsis among adult patients managed prehospital by EMS. Studies either addressed paramedic diagnosis of sepsis or the development of prehospital sepsis screening tools | None | Very low quality of evidence addressing recognition of sepsis by EMS using a screening tool. The majority of the screening tools rely on SIRS criteria. Very low quality of evidence addressing the accuracy of EMS diagnosis of sepsis in clinical practice. | The accuracy of sepsis recognition by EMS is variable. Prehospital screening tools need to be validated in clinical practice. |
| Fiest et al. 2022 [20] | Scoping review | Total: (n=80); Patients: (n=13); Public: (n=15); Healthcare professionals: (n=48) | Articles related to sepsis awareness, knowledge, and information-seeking behaviors among patients, public, and healthcare professionals | None | Awareness and knowledge of sepsis is high among healthcare professionals compared to patients/public. Patient/public awareness of sepsis gradually improved over time. Most patients/public get sepsis information from the Internet. | Awareness and knowledge of sepsis among patients, public, and healthcare professionals varied globally. |
Table 2. Characteristics of and Findings in the Included Observational Studies.
Abbreviations: qSOFA, Quick Sequential Organ Failure Assessment; SIRS, Systemic Inflammatory Response Syndrome; ED, emergency department; EMS, emergency medical services; HR, heart rate; RR, respiratory rate; SI, Shock Index; ICU, intensive care unit; OR, odds ratio; CI, confidence interval; PPV, positive predictive value; NEWS2, National Early Warning Score 2; mSOFA, Modified Sequential Organ Failure Assessment; AUC, area under the receiver operating characteristic curve; PRESEP, prehospital early sepsis detection; AMS, altered mental status; SD, standard deviation; tqSOFA, Triage Quick Sequential Organ Failure Assessment; CAP, community-acquired pneumonia; CCS, critical care support; LR, likelihood ratio; MEWS, Modified Early Warning Score
PROGRESS: Place of residence, Race/ethnicity/culture/language, Occupation, Gender/sex, Religion, Education, Socioeconomic status, Social capital
Plus:
1. Personal characteristics associated with discrimination (e.g. age, disability) 2. Features of relationships (e.g. smoking parents, excluded from school 3. Time-dependent relationships (e.g. leaving the hospital, respite care, other instances where a person may be temporarily at a disadvantage)
CURB-65: confusion, uremia, respiratory rate, blood pressure, age>65 years
| Author, year | Type of study | Location, study size (n) | Population | PROGRESS-Plus characteristics | Intervention | Comparison | Outcomes | Key findings | Conclusions |
| Baez et al. 2013 [21] | Cross-sectional descriptive study | United States of America (n=63) | Adults (≥18 years) transported by EMS with the diagnosis of sepsis | N/A | EMS data, including vital signs (temperature, HR, RR, SI, and association to outcomes | None | Primary: 1. Mortality, 2. Admission to ICU; Secondary: 1. Ventilator days, 2. ICU length of stay, 3. Hospital length of stay | Elevated RR was found to predict ICU admissions (OR 4.81 (CI, 1.16-21.01; P = .0116)). No physiologic variables studied were found to predict mortality. | Out-of-hospital shock index and respiratory rate have high predictability for ICU admission. |
| Barbara et al. 2018 [22] | Retrospective chart review | United States of America (n=72) | Adults (≥18 years) transported by EMS and evaluated in ED | 1. Gender (No observed discrepancy relating to gender) | Identification of EMS patients meeting all three qSOFA criteria | None | ED identification of sepsis ((≥2 SIRS criteria or admitting diagnosis of sepsis) | Prehospital qSOFA PPV of 66.7% (95% CI 55.8-77.6). | EMS patients with positive qSOFA more likely to be diagnosed with sepsis in the ED. |
| Goodacre et al. 2023 [23] | Retrospective diagnostic cohort | United Kingdom (n=12,870) | Adults (≥18 years) transported by EMS to the ED | 1. Sex; 2. Ethnicity, 3. Excluded mental health problems | Accuracy of prehospital early warning scores + paramedic diagnostic impression for identifying sepsis. | None | Identification of sepsis requiring urgent treatment | No combination of early warning score + paramedic diagnostic impression provided greater sensitivity than 0.8 and PPV greater than 0.15 for sepsis. NEWS2 + paramedic diagnostic impression of infection or sepsis identified 1/3 to 1/2 of sepsis cases. | NEWS2 had superior accuracy over all other early warning scores. |
| Melero-Guijarro et al. 2023 [24] | Prospective, multicenter cohort study | Spain (n=535) | Adults (≥18 years) with suspected infection transferred by EMS to the ED | 1. Age, 2. Sex, 3. Nursing home residence | Performance of qSOFA, NEWS2, and mSOFA to identify sepsis in prehospital care | None | Primary: In-hospital sepsis diagnosis; Secondary: 1. diagnosis of septic shock, 2. Two-day in-hospital mortality | No statistically significant differences were found for sepsis or septic shock. Only the comparison between scores for mortality outcome presented statistically significant differences. mSOFA outperformed the other two scores (p < 0.001 vs. both scores) in identifying two-day mortality. | The mSOFA score performed consistently better in two-day mortality prediction and diagnosis of septic-shock than NEWS2 and qSOFA. |
| Nualprasert et al. 2024 [25] | Retrospective observational study | Thailand (n=354) | Adults (≥18 years) transported by EMS to the ED | 1. Sex, 2. Age | The ability of PRESEP score and Miami Sepsis Score to predict sepsis in the prehospital setting | None | Final diagnosis of sepsis within 48 hours of admission | AUC for the PRESEP score was 0.83 (95% confidence interval [CI] 0.79–0.88) AUC for Miami Sepsis Score was 0.80 (0.75–0.85). The sepsis group compared to those without sepsis showed a high proportion of patients with worse vital signs. | Due to their relatively high ability to detect sepsis patients, the PRESEP and Miami Sepsis Scores are useful tools to screen septic patients in prehospital settings. |
| Olander et al. 2019 [26] | Retrospective observational study | Sweden (n=327) | Adults (≥18 years) transferred by EMS to the ED and started on antibiotic treatment within 48 hours for suspected sepsis | 1. Gender, 2. Age, 3. Form of housing, 4. Type of housing assistance | Prehospital characteristics of patients with sepsis while transported by EMS | None | Patients with and without adverse in-hospital outcomes (ICU requirement or in -hospital mortality). | 50 patients had adverse outcomes. Prehospital AMS, decreased body temperature, decreased oxygen saturation, and increased serum glucose were associated with an adverse outcome. | Altered mental status, low temperature, low oxygen saturation, and high serum glucose level may be early prehospital characteristics related to poorer prognosis and adverse outcomes in patients with sepsis. |
| Parsons Leigh et al. 2022 [27] | Cross-sectional survey | Canada (n=3200) | Representative sample of English- and French-literature adults (≥18 years) who resided in Canada | 1. Sex, 2. Age, 3. Education, 4. Annual household income, 5. Ethnicity, 6. Region of residence | Examined public awareness and knowledge of sepsis | None | 1. Awareness of sepsis, 2. Knowledge of sepsis, 3. Sepsis information access | Overall 61.4% heard of sepsis. There was significant regional variation in self-reported awareness (p<0.001) and significant association with respondents’ education, ethnicity, sex, and age. Relatively few (9.5%) respondents perceived their level of knowledge as good (7.7%) or very good (1.8%). Respondents who had heard of sepsis scored an average of 44% (mean=44.3% SD 18.9%) on knowledge-based questions. The strongest predictors of sepsis knowledge were previous exposure to sepsis, healthcare employment, female sex, and a college/university education (p < 0.001, all). The top recognized descriptor of sepsis was “the body’s extreme response to infection” (61.3%) and the top recognized sign/symptom of sepsis was fever (55.7%). One-fifth (19.7%) of the respondents who had heard of sepsis (61.8%) actively looked for information and a majority (68.5%) used the Internet. | We found an incomplete awareness and understanding of sepsis among adults. |
| Perman et al. 2020 [28] | Retrospective observational cohort study | United States of America (n=2859) | Adults (≥18 years) transported by EMS, admitted from the ED with severe sepsis present on admission, with treatment initiated in the ED | 1. Age, 2. Gender, 3. Race | Assessed triage qSOFA, maximum qSOFA (derived from worst vitals during ED stay), and first initial serum lactate | Triage SIRS criteria | In-hospital mortality | Mortality for tqSOFA<2 was 11.7% and for tqSOFA≥2 mortality was 26.4%. Mortality for patients with maximum qSOFA<2 was 8.5% and for maximum qSOFA≥2 was 20.6%. Sensitivity of tqSOFA≥ 2 and maximum qSOFA≥ 2 to predict in-hospital mortality were 33% and 69%, respectively. Triage SIRS criteria and the initial lactate > 3 mmol/L had sensitivities of 82% and 65%, respectively. | Triage qSOFA performed poorly at identifying patients at an increased risk of mortality on initial presentation. qSOFA cannot be relied upon to identify sepsis patients at high risk of death. |
| Sjösten et al. 2019 [29] | Retrospective observational study | Sweden (n=353) | Patients transported by EMS and admitted with a final diagnosis related to sepsis | 1. Age, 2. Gender | EMS field assessments of patients with prehospital suspicion of sepsis | EMS field assessments of patients without prehospital suspicion of sepsis | Hospital discharge diagnosis codes corresponding to sepsis | Sepsis symptoms included in research protocol: abdominal pain, dyspnea, diarrhea, nausea/vomiting, rigors/shivering, skin rash/hives, and confusion. Dyspnea, rigors/shivering, and confusion were the most common symptoms, and higher respiratory and heart rate, and temperature abnormalities were most common abnormal vital signs noted in patients with a prehospital suspicion of sepsis. | EMS clinicians identified 36% of patients in the prehospital phase with a final hospital diagnosis of sepsis. |
| Spagnolello et al. 2021 [30] | Retrospective observational study | Italy (n=505) | Adults (≥18 years) evaluated in a single ED with an ED diagnosis of CAP | 1. Age, 2. Gender | Assessed the ability of qSOFA and CURB-65 to predict mortality in the ED | None | 1. Mortality in the ED, 2. CCS requirement, 3. ICU admission | Positive qSOFA (≥ 2) had a LR of 11 for mortality compared to qSOFA negative (0-1) patients in CAP patients. | qSOFA is a valuable score for predicting mortality in the ED and for the prompt identification of patients with CAP requiring CCS. |
| Usul et al. 2021 [31] | Retrospective cohort study | Turkey (n=266) | Adults (≥18 years) transported by EMS, admitted to the hospital with a diagnosis of sepsis | 1. Age, 2. Gender | Assessed qSOFA and MEWS to predict ICU hospitalization and 28-day mortality | None | 1. 28-day mortality, 2. ICU admission | MEWS value > 4 (AUC = 0.641; sensitivity 76.98; specificity 44.88; +LR: 1.4, −LR:0.51; p < 0.001; 95% CI: 0.575–0.708) and qSOFA score > 1 (AUC = 0.651; sensitivity 84.89; specificity 37.8; +LR: 1.36, −LR: 0.4; p < 0.001; 95% CI: 0.585–0.717) were both significant in predicting mortality. MEWS value >5 and qSOFA score >1 were both significant in predicting ICU hospitalization. | MEWS and qSOFA can be used to predict ICU hospitalization and mortality in patients diagnosed with sepsis. |
Screening Score Performance to Identify Sepsis
Three systematic reviews [17-19] and four observational studies [22-25] evaluated the performance of sepsis screening scores to identify adult patients with sepsis in both the prehospital and in-hospital settings and found the accuracy of sepsis recognition by EMS providers to be variable. De Silva et al. identified 18 studies that compared the sensitivity and specificity of qSOFA to 31 other screening tools for the diagnosis of sepsis and determined that qSOFA produced high specificity and low sensitivity for the emergency diagnosis of sepsis among people with suspected or confirmed sepsis in either the prehospital setting or Emergency Department (ED) [17]. Lane et al. described in a narrative review of 17 articles that the accuracy of prehospital sepsis identification of septic patients by EMS using SIRS criteria or a combination of vital signs was heterogeneous [18]. The most common vital signs taken into consideration in seven studies were temperature, heart rate, and respiratory rate. Smyth et al. discussed very low quality of evidence in six studies that addressed the recognition of sepsis by EMS with the majority of screening tools relying on SIRS criteria [19].
One prospective, ambulance-based, cohort study analyzed the performance of qSOFA, NEWS2, and modified SOFA (mSOFA) as sepsis predictors in the prehospital setting among patients with a suspected infection and did not find any statistically significant differences between the scores [24]. Barbara et al. performed a retrospective chart review of patients that met all the three qSOFA criteria by EMS and found a sepsis diagnosis in the ED to have a positive predictive value of 66.67% (95% CI 55.8-77.6) [22]. The ED septic patients demonstrated a statistically significant difference of higher average temperature by >2 °F (>1 °C) (p=0.001), mean maximum heart rate by a difference of >10 beats per minute (p=0.019), and mean maximum respiratory rate of >4 breaths per minute (p=0.0001) compared with the non-septic patients. A retrospective diagnostic cohort study evaluated the accuracy of 21 prehospital early warning scores in combination with parametric diagnostic impression for identifying sepsis and found NEWS2 to be superior to all other scores [23]. A retrospective analysis by Nualprasert et al. evaluated the ability of two early warning scores, Prehospital Early Sepsis Detection (PRESEP) score and Miami Sepsis Score, to detect septic patients in the prehospital setting and found both to be potential screening tool options for EMS given the relatively high sensitivities at the given cutoff values, 0.83 (0.73-0.90) and 0.81 (0.71-0.89), respectively [25].
EMS Use of Clinical Signs and Assessments in Suspected Sepsis
Sjösten et al. performed a retrospective observational analysis of EMS field assessments of patients with a prehospital suspicion of sepsis during which symptoms and vital signs were recorded in the research protocol [29]. Prehospital signs and symptoms that were identified in patients with sepsis included: respiratory difficulties, gastrointestinal symptoms, altered mental status, skin rash, rigors or shivering, temperature abnormalities, and tachycardia. The most common symptoms were dyspnea, rigors or shivering, and confusion, and elevated respiratory and heart rate as well as temperature abnormalities were the most common abnormal vital signs observed in patients with a prehospital suspicion of sepsis.
Prediction of Adverse Outcomes
One systematic review [17] and four observational studies [24,28,30,31] evaluated the prognostic ability of sepsis screening tests performed in the prehospital or emergency setting to predict adverse in-hospital outcomes, such as progression to septic shock, mortality, critical care intervention, or ICU requirement. The qSOFA score was universally evaluated in all the studies but with variable results.
Based on the 18 articles included in the review conducted by De Silva et al., the authors concluded that qSOFA most successfully predicted mortality in at-risk patients compared to 31 other screening tools [17]. A retrospective observational study that evaluated patients presenting to the ED with community-acquired pneumonia also found the qSOFA score to be useful in predicting ED mortality and identifying septic patients requiring critical care support [30]. Usul et al. similarly concluded that a qSOFA score >1 (AUC = 0.651; sensitivity 84.89; specificity 37.8; +LR: 1.36, -LR: 0.4; p<0.001; 95% CI: 0.585-0.717) and MEWS score >4-5 (AUC = 0.641; sensitivity 76.98; specificity 44.88; +LR: 1.4, -LR: 0.51; p<0.001; 95% CI: 0.575-0.708) could be utilized to predict mortality and ICU hospitalization in patients diagnosed with sepsis [31].
A comparison of qSOFA, NEWS2, and mSOFA in a prospective, multicenter cohort study showed that the mSOFA score performed consistently better in two-day mortality prediction and diagnosis of septic shock than both NEWS2 and qSOFA [24]. However, the unique variables of mSOFA differentiating it from NEWS2 and qSOFA are derived from blood work. Perman et al. calculated qSOFA scores obtained at triage and during the ED stay derived from the worst vital signs to predict in-hospital mortality and compared these results with triage SIRS criteria of patients admitted with severe sepsis [28]. Sensitivities for the prediction of in-hospital mortality of triage qSOFA, maximum qSOFA, and triage SIRS were 33%, 69%, and 82%, respectively, suggesting that triage qSOFA is not reliable at identifying septic patients at a high risk of death.
Two observational studies [21,26] assessed prehospital characteristics of patients who were admitted to the hospital with diagnosed or suspected sepsis for association with adverse outcomes. One retrospective, cross-sectional descriptive study found that rapid respiratory rate had high predictability for ICU admission (OR 4.81 (CI, 1.16-21.01; P = .0116)) but no physiologic variables were predictive of mortality [21]. Among the 327 patients who were admitted for suspected sepsis and initiation of treatment with antibiotics in a retrospective observational study by Olander et al., it was noted that the presence of prehospital altered mental status and low temperature may be related to poorer prognosis and adverse outcomes with need for ICU level of care and mortality [26].
Awareness and Knowledge of Sepsis
A review of 80 articles related to sepsis awareness and knowledge among healthcare professionals, patients. and the general public found that both knowledge and awareness varied significantly across the groups and geographically [20]. Patients and the public, most of whom obtained information from the Internet, had less awareness and knowledge of sepsis than healthcare professionals. One cross-sectional survey evaluating public awareness and knowledge of sepsis in Canada found significant regional variation in self-reported awareness (p<0.001) and significant association with the respondents’ education, ethnicity, sex, and age [27]. The most recognized sign or symptom of sepsis was “fever” (55.7%) and others being “infection” (52.9%), “feeling extremely ill (like you are going to die)” (39.3%), “extreme shivering or muscle pain” (27.6%), “fast heart rate” (26.4%), “fast breathing/severe breathlessness” (21.2%), “skin blotchy or discolored” (20.7%), “slurred speech or confusion” (12.5%), and “passing no urine all day” (8.0%).
Gray Literature
Of the 27 sources [32-58] that were included from the gray literature, 13 [32-44] were organizations that focused on first-aid training, one [45] was a government-based sepsis public awareness campaign workgroup, and 13 [46-58] were sepsis-focused campaign initiatives, major healthcare institutions, or government-run sepsis- or disease-focused organizations. Each source listed sepsis-associated signs and symptoms as a guide to the public on sepsis recognition as outlined in Table 3.
Table 3. Characteristics of Included Gray Literature Sources.
| Search # | Organization | Website Title | Website | Temperature | Neurology | Musculoskeletal | Urinary | Respiratory | Skin | Subjective | Cardiac | Gastrointestinal | Infectious Disease |
| Search #1 - Sepsis and “First Aid” | St John Ambulance [32] | Sepsis in Adults and Older Children | https://www.sja.org.uk/get-advice/first-aid-advice/sepsis/sepsis-in-adults-and-older-children/ | Slurred speech, confusion, dizziness, or faintness | Extreme shivering or muscle pain | Passing no urine over the past 24 hours | Severe breathlessness or rapid breathing | Skin is mottled, pale, or discolored | "I feel sicker than I ever have before" | ||||
| Search #1 - Sepsis and “First Aid” | Scottish Ambulance Service [33] | Identifying Sepsis | https://www.scottishambulance.com/first-aid-education/identifying-sepsis/ | Very high or low temperature | Confusion | Uncontrolled shivering | Not passing as much urine | Cold or blotchy hands | |||||
| Search #1 - Sepsis and “First Aid” | First Aid for Life [34] | Sepsis – What to Look Out for | https://firstaidforlife.org.uk/sepsis/ | Slurred speech | Muscle pain and shivering | Failure to pass any urine | Breathlessness | Pale, mottled skin | A sense of ‘impending doom’ or a feeling that they might die | ||||
| Search #1 - Sepsis and “First Aid” | CPR First Aid [35] | What Is Septic Shock and How to Prevent It | https://cprfirstaid.com.au/what-is-septic-shock-and-how-to-prevent-it/ | Fever and chills | Confusion or disorientation | Shortness of breath | Sweaty or clammy palms and skin | Elevated heart rate | |||||
| Search #1 - Sepsis and “First Aid” | Andersson First Aid Training [36] | What Is Sepsis? | https://anderssonfirstaidtraining.co.uk/blog/what-is-sepsis/ | Slurred speech or confusion | Extreme shivering or muscle pain | Passing no urine (in a day) | Severe breathlessness | Skin mottled or discolored | It feels like you’re going to die | ||||
| Search #1 - Sepsis and “First Aid” | ANZCOR [37] | Recognition and First Aid Management of the Seriously Ill Person Including Sepsis | https://www.anzcor.org/assets/anzcor-guidelines/guideline-9-2-12-recognition-and-first-aid-management-of-the-seriously-ill-person-including-sepsis-273.pdf | Fever or feeling very cold | Restlessness, agitation, dizziness, decreased level of consciousness, confusion, slurred speech, or disorientation | Shivering or shaking; unexplained muscle pain or discomfort | Passing little or no urine | Rapid breathing; breathlessness or feeling short of breath | New rash or blotchy, pale, or discolored (often described as mottled) skin | The person may say they "don’t feel right" or they might say they feel like they "are going to die" | Rapid heart rate | Nausea and or vomiting | |
| Search #1 - Sepsis and “First Aid” | HTS Training [38] | 6 Clues to Spotting Sepsis | https://hts-training.co.uk/sepsis-symptoms/ | Slurred speech or confusion | Extreme shivering or muscle pain | Passing no urine (in a day) | Severe breathlessness | Skin mottled or discolored | I feel like I might die | ||||
| Search #1 - Sepsis and “First Aid” | SkillBase First Aid [39] | Could It Be Sepsis? | https://www.skillbasefirstaid.com/could-it-be-sepsis/ | A high temperature (fever) or low body temperature | Feeling dizzy or faint; A change in mental state – such as confusion or disorientation; slurred speech; loss of consciousness | Severe muscle pain | Less urine production than normal – for example, not urinating for a day | Severe breathlessness | Cold, clammy, and pale or mottled skin | A fast heartbeat | Diarrhoea; nausea and vomiting | ||
| Search #1 - Sepsis and “First Aid” | First Response [40] | Sepsis Awareness - First Response | https://www.firstresponse.org.uk/medical-training/sepsis | A high temperature (fever) or low body temperature | Feeling dizzy or faint; a change in mental state – such as confusion or disorientation; slurred speech; loss of consciousness | Severe muscle pain | Less urine production than normal – for example, not urinating for a day | Severe breathlessness | Cold, clammy, and pale or mottled skin | A fast heartbeat | Diarrhoea, nausea, and vomiting | ||
| Search #1 - Sepsis and “First Aid” | The Hippocratic Post [41] | Sepsis Signs and Symptoms | https://www.hippocraticpost.com/first-aid/sepsis-signs-and-symptoms/ | Fever | Dislike bright lights; drowsy, difficult to wake; convulsions/seizures; severe headache; confusion and irritability | Stiff neck; severe muscle pain | Pale, blotchy skin; spots/rash; cold hands and feet | Vomiting | |||||
| Search #1 - Sepsis and “First Aid” | NR Medical Training [42] | Understanding Sepsis: Early Detection and Management | https://nrmedical.training/blog/sepsis-spot-it-early | Slurred speech or confusion | Extreme shivering or muscle pain | Passing no urine (in a day) | Severe breathlessness | Skin mottled or discolored | It feels like you’re going to die | ||||
| Search #1 - Sepsis and “First Aid” | End Sepsis [43] | What Is Sepsis? | https://www.endsepsis.org/what-is-sepsis/ | Fever and chills | Confusion or sleepiness | Extreme pain | Rapid breathing | Pale or mottled skin | Feeling the sickest you've ever felt | Fast heartbeat | |||
| Search #1 - Sepsis and “First Aid” | TLCT [44] | Could It Be Sepsis? Local First Aid Training Courses | https://www.tlct.co.uk/could-it-be-sepsis/ | Slurred speech or confusion | Extreme shivering or muscle pain | Passing no urine (in a day) | Severe breathlessness | Skin mottled or discolored | It feels like you’re going to die | ||||
| Search #2 - "Sepsis Recognition" and Public | Maryland Department of Health - Sepsis Public Awareness Campaign Workgroup [45] | Sepsis Public Awareness Campaign Workgroup Meeting #1 Minutes | https://health.maryland.gov/phpa/IDEHASharedDocuments/Minutes%20for%20Sepsis%20Workgroup%20Meeting%201.cc5.pdf | Abnormal temperature | Mental decline | Extreme pain and discomfort | Shortness of breath | Discolored skin | Signs and symptoms of an infection | ||||
| Search #3 - "Sepsis Recognition" and "Signs and Symptoms" | CDC (Centers for Disease Control and Prevention) [46] | Get Ahead of Sepsis | https://www.cdc.gov/sepsis/media/pdfs/Consumer-brochure-its-time-to-talk-about-sepsis-2022-P.pdf | Fever or feeling very cold | Confusion or disorientation | Extreme pain or discomfort; shivering | Shortness of breath | Clammy or sweaty skin | High heart rate or weak pulse | ||||
| Search #3 - "Sepsis Recognition" and "Signs and Symptoms" | Mayo Clinic [47] | Sepsis | https://www.mayoclinic.org/diseases-conditions/sepsis/symptoms-causes/syc-20351214 | Change in mental status Feeling lightheaded | Shivering | Fast, shallow breathing | Sweating for no clear reason | Symptoms specific to the type of infection, such as painful urination from a urinary tract infection or worsening cough from pneumonia | |||||
| Search #3 - "Sepsis Recognition" and "Signs and Symptoms" | Penn Medicine [48] | Sepsis | https://www.pennmedicine.org/for-patients-and-visitors/patient-information/conditions-treated-a-to-z/sepsis | Fever or low body temperature (hypothermia); Chills | Confusion or delirium; lightheadedness due to low blood pressure | Skin rash or mottled skin; warm skin | Rapid heartbeat | ||||||
| Search #3 - "Sepsis Recognition" and "Signs and Symptoms" | World Health Organization [49] | Sepsis | https://www.who.int/news-room/fact-sheets/detail/sepsis | Fever or low temperature | Confusion | Extreme body pain or discomfort; shivering | Low urine output | Difficulty breathing | Clammy and sweaty skin | High heart rate, weak pulse, or low blood pressure | |||
| Search #3 - "Sepsis Recognition" and "Signs and Symptoms" | NHS (UK) [50] | Sepsis | https://www.nhs.uk/conditions/sepsis/ | Acting confused, slurred speech, or not making sense | Difficulty breathing, breathlessness or breathing very fast | Blue, gray, pale or blotchy skin, lips or tongue – on brown or black skin; this may be easier to see on the palms of the hands or soles of the feet; A rash that does not fade when you roll a glass over it, the same as meningitis | |||||||
| Search #3 - "Sepsis Recognition" and "Signs and Symptoms" | Texoma Medical Center [51] | Recognizing Signs of Sepsis | https://www.texomamedicalcenter.net/recognizing-signs-sepsis | Temperature: higher or lower than normal | Mental decline: confused, sleepy, difficult to rouse | Severe pain or discomfort | Extremely Ill: "I feel like I might die" | May have signs or symptoms of an infection | |||||
| Search #3 - "Sepsis Recognition" and "Signs and Symptoms" | Sepsis Alliance [52] | It's about TIME | https://www.sepsis.org/about/its-about-time/ | Temperature: higher or lower than normal | Mental decline: confused, sleepy, difficult to rouse | Extremely Ill: severe pain, discomfort | Shortness of breath | May have signs and symptoms of an infection | |||||
| Search #3 - "Sepsis Recognition" and "Signs and Symptoms" | AARP [53] | 7 Sepsis Symptoms You Should Recognize | https://www.aarp.org/health/conditions-treatments/info-2023/sepsis-symptoms.html | Fever and chills; A very low body temperature | Lethargy or tiredness; confusion or dizziness | Extreme pain or discomfort (often at the infection site); shivering | Fast breathing or breathlessness | Clammy, sweaty or blotchy skin | Fast heart rate | ||||
| Search #3 - "Sepsis Recognition" and "Signs and Symptoms" | The UK Sepsis Trust [54] | About Sepsis | https://sepsistrust.org/about/about-sepsis/ | Slurred speech or confusion | Extreme shivering or muscle pain | Passing no urine (in a day) | Severe breathlessness | Skin mottled or discolored | It feels like you’re going to die | ||||
| Search #3 - "Sepsis Recognition" and "Signs and Symptoms" | Cleveland Clinic [55] | Sepsis | https://my.clevelandclinic.org/health/diseases/12361-sepsis | Fever or hypothermia (very low body temperature) | Confusion or agitation | Low energy/weakness; shaking or chills; extreme pain or discomfort | Urinary issues, such as reduced urination or an urge to urinate | Hyperventilation (rapid breathing) or shortness of breath | Rash makes your skin appear red and discolored; You may see small, dark-red spots on your skin; warm or clammy/sweaty skin | Fast heart rate; low blood pressure | |||
| Search #3 - "Sepsis Recognition" and "Signs and Symptoms" | National Kidney Foundation [56] | Sepsis | https://www.kidney.org/atoz/content/sepsis | Temperature: higher or lower than normal; fever, or feeling very cold | Mental decline: confused, sleepy, difficult to rouse; confusion or disorientation | Severe pain or discomfort; shivering | Extremely Ill: shortness of breath | Clammy or sweaty skin | High heart rate or weak pulse | May have signs or symptoms of an infection | |||
| Search #3 - "Sepsis Recognition" and "Signs and Symptoms" | Australian Commission on Safety and Quality in Health Care [57] | Quality Statement 1 - Could It Be Sepsis? | https://www.safetyandquality.gov.au/standards/clinical-care-standards/sepsis-clinical-care-standard/quality-statements/quality-statement-1-could-it-be-sepsis | Fever and chills; low body temperature | Fatigue, confusion, or sleepiness | A lot of pain | Low or no urine output | Fast breathing or breathlessness | ‘feeling worse than ever’ | Fast heartbeat | Nausea and vomiting; diarrhoea | ||
| Search #3 - "Sepsis Recognition" and "Signs and Symptoms" | Queensland Government [58] | Adult Sepsis | https://clinicalexcellence.qld.gov.au/priority-areas/safety-and-quality/sepsis/adult-sepsis | Fever or hypothermia | New onset confusion or altered consciousness | Extreme pain; weakness or aching muscles | Poor urine output | Rapid breathing | Skin rash or clammy/sweaty skin | Feeling very unwell unexplained or the “worst ever”; feeling "the sickest" they have ever been or feeling "an impending sense of doom'" | Rapid heart rate |
Discussion
This topic was selected by the ILCOR First Aid Task Force as a significant proportion of preventable deaths are caused by sepsis worldwide, and there are known benefits of early detection and treatment. No prior review has been undertaken, and in 2022, the Task Force elected by consensus to undertake a scoping review on the recognition and awareness of sepsis by first-aid providers evaluating adults with an acute illness. There were insufficient studies identified to support a systematic review.
Sepsis initiatives have increasingly focused on early sepsis recognition by the lay provider as a means to decrease time to hospital presentation and management with antibiotics and initial resuscitation. Despite the utilization of early warning scoring tools by trained clinicians in the healthcare setting to assist in the detection of sepsis, sepsis recognition remains a challenge due to the variable reliability of the scoring tools. Based on evidence from the EMS and in-hospital settings, no specific sign or symptom or compilation of signs and symptoms has demonstrated a clear association with sepsis. Therefore, it is unreasonable to expect a lay provider to recognize and subsequently diagnose an acute illness as sepsis using only the signs and symptoms exhibited by an ill person. A more feasible request of a lay provider is to, at a minimum, consider an infection in a person being evaluated with an acute illness.
It was noted that online resources providing education to the public on sepsis recognition listed presenting signs and symptoms of sepsis under nine general categories (Table 4): temperature (fever or hypothermia), neurologic (change in mental state, dizziness, slurred speech), musculoskeletal (severe muscle pain, extreme shivering), urologic (poor urine output), respiratory (rapid breathing or breathlessness), skin (clammy/sweaty, new rash, mottled or discolored), cardiac (elevated heart rate), gastrointestinal (nausea, vomiting, diarrhea), and subjective (feeling very unwell or impending sense of doom). However, it was variable as to which signs or symptoms were highlighted by each campaign or organization. For instance, only five of the 27 websites included from the gray literature search mentioned “infection” when describing presenting signs and symptoms of sepsis. Additionally, the presence of a fever (≥ 38°C) was noted to be inconsistently listed as a sign of sepsis and highlights that an elevated temperature is not a prerequisite for this diagnosis.
Table 4. Categories of Signs and Symptoms from Sepsis Awareness Campaigns.
| Categories | Examples |
| Subjective | Feeling very unwell or impending sense of doom |
| Temperature | Fever or hypothermia |
| Respiratory | Rapid breathing or breathlessness |
| Cardiac | Elevated heart rate |
| Neurologic | Change in mental state, dizziness, slurred speech |
| Gastrointestinal | Nausea, vomiting, diarrhea |
| Musculoskeletal | Severe muscle pain or extreme shivering |
| Urologic | Poor urine output |
| Skin | Clammy/sweaty, new rash, mottled or discolored |
It is noteworthy that no literature originating from LMICs was included in this scoping review. Owing to a greater burden of infectious diseases and delayed presentations due to poor access to healthcare, the LMIC contexts may have much higher incidences of sepsis, resulting in higher mortality [4,5]. It is also unclear to what extent the signs and symptoms reported in the HIC literature are transferable to LMICs, where diarrheal illnesses or vector-borne diseases (such as malaria) predominate. In LMICs that feature developing or do not have emergency care systems and services, the integration of community-based first-aid providers offers a prime opportunity to increase sepsis recognition and initiate healthcare-seeking behavior [59], ultimately resulting in decreased mortality. Given a higher sepsis incidence and the critical role that a first-aid provider might play in such nascent systems, it is necessary that research in LMIC contexts should be advanced.
Limitations
There are several limitations to this review. Although this scoping review has not identified sufficient evidence to prompt a further systematic review, it highlights important gaps in research, specifically in the first-aid setting. Retrospective diagnostic studies are needed to evaluate the accuracy of criteria used in specific sepsis awareness campaigns for lay providers. The effectiveness of sepsis awareness campaigns in helping lay responders identify sepsis should be studied to determine if any one campaign is more helpful than the other. Additionally, none of the included studies were conducted in LMICs where access of the disadvantaged to sepsis care or education may have led to alternative results.
Conclusions
Given the diagnostic challenge faced in the first-aid setting and time-sensitive nature of sepsis, increasing sensitivity for the detection of sepsis can be achieved by screening people with an infection and any correlating signs or symptoms that may fall along the spectrum of a less severe presentation. Although the criteria for sepsis may not be fulfilled, at that time or anytime in the future, they are likely to still benefit from an evaluation by a medical professional. Therefore, a first-aid provider should consider an infection in a person who presents with an acute illness, and if associated with any abnormal signs or symptoms, recommend seeking further medical evaluation.
This scoping review found no studies directly addressing our outcomes. However, we identified studies that evaluated patients in the prehospital and in-hospital settings for potential sepsis, as well as awareness and knowledge of sepsis by various members of the community. The limited literature identified in this scoping review does not support the development of a systematic review but highlights the need for future research to institute measures for the recognition of sepsis in first-aid settings.
Acknowledgments
The authors would like to thank the International Liaison Committee on Resuscitation First Aid Task Force for their insights on this review.
Appendices
Appendix 1
Table 5. Initial Search Query in and Results from Embase and Medline databases (January 17, 2023).
| No. | Search String Query (January 17, 2023) | Results |
| 1 | Emergency Medical Services/ or Emergency Medical Technicians/ or Emergency Services/ or First Aid/ | 180,403 |
| 2 | ("emergency care" or "emergency health service*" or "emergency medical service*" or emergicenter* or "medical emergency service*" or "prehospital emergency care" or emergicentre* or emergi-center* or emergi-centre* or "pre-hospital emergency care" or EMT* or "emergency medical technician*" or "first responder*" or "first aid" or "critical care").ti,ab,kw,kf. | 279,299 |
| 3 | 1 or 2 [FIRST AID] | 418,551 |
| 4 | exp Sepsis/ | 459,583 |
| 5 | sepsis (or sepses or septic or "bloodstream infection*" or pyemi* or pyohemi* or pyaemi* or septicemi* or septicaemi* or "blood poisoning*" or bacteremi* or fungemi* or candidemi*).ti,ab,kw,kf. | 519,778 |
| 6 | 4 or 5 [SEPSIS] | 681,253 |
| 7 | 3 and 6 [FIRST AID + SEPSIS] | 17,089 |
| 8 | (evaluat* or assess*).ti,ab,kw,kf. | 16,348,275 |
| 9 | 7 and 8 [FIRST AID + SEPSIS + EVALUATE] | 7066 |
| 10 | (Animals/ or "Animal Experimentation"/ or "Models, Animal"/ or "Disease Models, Animal"/) not (Humans/ or "Human Experimentation"/) | 8,804,236 |
| 11 | 9 not 10 [ANIMAL STUDIES REMOVED] | 6865 |
| 12 | (comment or editorial or "newspaper article" or news or note or lecture).pt. | 3,322,316 |
| 13 | (letter not (letter and randomized controlled trial)).pt. | 2,452,749 |
| 14 | 11 not (12 or 13) [OPINION PIECES REMOVED] | 6769 |
| 15 | "case reports".pt. | 2,313,061 |
| 16 | 14 not 15 [CASE REPORTS REMOVED] | 6738 |
| 17 | (conference or conference abstract or "conference review" or congresses).pt. | 5,438,450 |
| 18 | 16 not 17 [CONFERENCES REMOVED] | 5076 |
| 19 | limit 18 to english | 4726 |
| 20 | limit 18 to abstracts | 5055 |
| 21 | 19 or 20 | 5074 |
| Embase <1974 to 2023 January 17> | 3238 | |
| Ovid MEDLINE(R) and Epub Ahead of Print, In-Process, In-Data-Review & Other Non-Indexed Citations and Daily <1946 to January 17, 2023> | 1836 | |
| 22 | remove duplicates from 21 | 3554 |
| Embase <1974 to 2023 January 17> | 1722 | |
| Ovid MEDLINE(R) and Epub Ahead of Print, In-Process, In-Data-Review & Other Non-Indexed Citations and Daily <1946 to January 17, 2023> | 1832 |
Table 6. Initial Search Query in and Results from the Cochrane database (January 17, 2023).
| No. | Search String Query (January 17, 2023) | Results |
| #1 | ("emergency care" OR "emergency health service" OR "emergency medical service" OR "medical emergency service" OR "emergency health services" OR "emergency medical services" OR emergicenter* OR "medical emergency service" OR "medical emergency services" OR "prehospital emergency care" OR emergicentre* OR emergi-center* OR emergi-centre* OR "pre-hospital emergency care" OR EMT* OR "emergency medical technician" OR "first responder" OR "emergency medical technicians" OR "first responders" OR "first aid" OR "critical care"):ti,ab,kw | 12,546 |
| #2 | (sepsis OR sepses OR septic OR "bloodstream infection" OR "bloodstream infections" OR pyemi* OR pyohemi* OR pyaemi* OR septicemi* OR septicaemi* OR "blood poisoning" OR "blood poisonings" OR bacteremi* OR fungemi* OR candidemi*):ti,ab,kw | 18,820 |
| #3 | #1 AND #2 | 759 |
| #4 | (evaluat* OR assess*):ti,ab,kw | 961,602 |
| #5 | #3 AND #4 | 489 |
| #6 | ([mh ^Animals] OR [mh ^"Animal Experimentation"] OR [mh ^"Models, Animal"] OR [mh ^"Disease Models, Animal"]) NOT ([mh ^Humans] OR [mh ^"Human Experimentation"]) | 5 |
| #7 | #5 NOT #6 | 489 |
| #8 | (comment OR editorial OR "newspaper article" OR news OR note OR lecture):pt | 13,136 |
| #9 | (letter NOT (letter AND randomized controlled trial)):pt | 13,250 |
| #10 | #7 NOT (#8 OR #9) | 483 |
| #11 | "case reports":pt | 0 |
| #12 | #10 NOT #11 | 483 |
| #13 | (conference OR "conference abstract" OR "conference review" OR congresses):pt | 215,178 |
| #14 | #12 NOT #13 | 420 |
| #15 | #12 NOT #13 in Cochrane Reviews, Trials (15 Cochrane Reviews, 405 Trials) | 420 |
Appendix 2
Table 7. Follow-Up Search Query in and Results from Embase database (November 21, 2023).
| No. | Search String Query (November 21, 2023) | Results |
| #1 | 'emergency treatment'/de OR 'first aid'/de OR 'first responder (person)'/exp | 39,589 |
| #2 | 'emergency care':ti,ab,kw OR 'emergency health service*':ti,ab,kw OR 'emergency medical service*':ti,ab,kw OR emergicenter*:ti,ab,kw OR ' medical emergency service*':ti,ab,kw OR 'prehospital emergency care':ti,ab,kw OR emergicentre*:ti,ab,kw OR 'emergi center*':ti,ab,kw OR 'emergi centre*':ti,ab,kw OR 'pre-hospital emergency care':ti,ab,kw OR emt*:ti,ab,kw OR 'emergency medical technician*':ti,ab,kw OR 'first responder*':ti,ab,kw OR 'first aid':ti,ab,kw OR 'critical care':ti,ab,kw | 181,454 |
| #3 | #1 OR #2 | 60,6221 |
| #4 | 'sepsis'/exp OR 'bloodstream infection'/exp | 388,544 |
| #5 | sepsis:ti,ab,kw OR sepses:ti,ab,kw OR septic:ti,ab,kw OR 'bloodstream infection*':ti,ab,kw OR pyemi*:ti,ab,kw OR pyohemi*:ti,ab,kw OR pyaemi*:ti,ab,kw OR septicemi*:ti,ab,kw OR septicaemi*:ti,ab,kw OR 'blood poisoning*':ti,ab,kw OR bacteremi*:ti,ab,kw OR fungemi*:ti,ab,kw OR candidemi*:ti,ab,kw | 329,119 |
| #6 | #4 OR #5 | 484,918 |
| #7 | #3 AND #6 | 32,335 |
| #8 | #7 AND ('Conference Abstract'/it OR 'Conference Paper'/it OR 'Conference Review'/it OR 'Editorial'/it OR 'Letter'/it OR 'Note'/it) | 12,593 |
| #9 | #7 NOT #8 | 19,742 |
| #10 | evaluat*:ti,ab,kw OR assess*:ti,ab,kw | 10,132,567 |
| #11 | #9 AND #10 | 7047 |
| #12 | #11 NOT ([animals]/lim NOT [humans]/lim) | 6661 |
| #13 | #11 NOT ([animals]/lim NOT [humans]/lim) AND [english]/lim | 6265 |
| #14 | #11 NOT ([animals]/lim NOT [humans]/lim) AND [english]/lim AND [2023-current]/py | 228 |
Table 8. Follow-Up Search Query in and Results from Medline database (November 21, 2023).
| No. | Search String Query (November 21, 2023) | Results |
| 1 | Emergency Medical Services/ | 49,123 |
| 2 | Emergency Medical Technicians/ | 6060 |
| 3 | First Aid/ | 8144 |
| 4 | 1 or 2 or 3 | 59,817 |
| 5 | ("emergency care" or "emergency health service*" or "emergency medical service*" or emergicenter* or "medical emergency service*" or "prehospital emergency care" or emergicentre* or emergi-center* or emergi-centre* or "pre-hospital emergency care" or EMT* or "emergency medical technician*" or "first responder*" or "first aid" or "critical care").ti,ab,kw,kf | 120,880 |
| 6 | 4 or 5 | 163,765 |
| 7 | Exp Sepsis/ | 143,368 |
| 8 | (sepsis or sepses or septic or "bloodstream infection*" or pyemi* or pyohemi* or pyaemi* or septicemi* or septicaemi* or "blood poisoning*" or bacteremi* or fungemi* or candidemi*).ti,ab,kw,kf. | 222,148 |
| 9 | 7 or 8 | 273,624 |
| 10 | 6 and 9 | 5229 |
| 11 | (evaluat* or assess*).ti,ab,kw,kf. | 7,258,332 |
| 12 | 10 and 11 | 2125 |
| 13 | (Animals/ or "Animal Experimentation"/ or "Models, Animal"/ or "Disease Models, Animal"/) not (Humans/ or "Human Experimentation"/) | 5,140,014 |
| 14 | 12 not 13 | 2081 |
| 15 | (comment or editorial or "newspaper article" or news or note or lecture).pt. | 1,719,034 |
| 16 | (letter not (letter and randomized controlled trial)).pt. | 1,230,350 |
| 17 | 14 not (15 or 16) | 2038 |
| 18 | "case reports".pt. | 2,369,855 |
| 19 | 17 not 18 | 2006 |
| 20 | (conference or conference abstract or "conference review" or congresses).pt. | 0 |
| 21 | 19 not 20 | 2006 |
| 22 | limit 21 to english language | 1855 |
| 23 | limit 22 to yr="2023 -Current" | 182 |
Appendix 3
Cochrane Follow-Up Search String (November 21, 2023)
("emergency care" OR "emergency health service" OR "emergency medical service" OR "medical emergency service" OR "emergency health services" OR "emergency medical services" OR emergicenter* OR "medical emergency service" OR "medical emergency services" OR "prehospital emergency care" OR emergicentre* OR emergi-center* OR emergi-centre* OR "pre-hospital emergency care" OR EMT* OR "emergency medical technician" OR "first responder" OR "emergency medical technicians" OR "first responders" OR "first aid" OR "critical care") in Title Abstract Keyword AND (sepsis OR sepses OR septic OR "bloodstream infection" OR "bloodstream infections" OR pyemi* OR pyohemi* OR pyaemi* OR septicemi* OR septicaemi* OR "blood poisoning" OR "blood poisonings" OR bacteremi* OR fungemi* OR candidemi*) in Title Abstract Keyword AND (evaluat* OR assess*) in Title Abstract Keyword - (Word variations have been searched).
Appendix 4
Table 9. Literature Search Query in and Results from Google.com (August 29, 2023).
| # | Google.com Search | Results | Results Screened | Total Records Reviewed | Duplicate | Excluded | Included After Review |
| 1 | Sepsis and “First Aid” | 747,000 | 100 | 19 | 2 | 4 | 13 |
| 2 | "Sepsis Recognition" and Public | 15,900 | 100 | 6 | 3 | 2 | 1 |
| 3 | “Sepsis Recognition” and “Signs and Symptoms” | 38,300,000 | 100 | 14 | 0 | 1 | 13 |
| Total: 27 |
Disclosures
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: Amy Kule, Eunice Singletary, Therese Djarv, Willem Stassen, Gustavo E. Flores
Acquisition, analysis, or interpretation of data: Amy Kule, Therese Djarv, Willem Stassen, Gustavo E. Flores
Drafting of the manuscript: Amy Kule, Willem Stassen
Critical review of the manuscript for important intellectual content: Amy Kule, Eunice Singletary, Therese Djarv, Willem Stassen, Gustavo E. Flores
References
- 1.The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) Singer M, Deutschman CS, Seymour CW, et al. JAMA. 2016;315:801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hospital-related costs of sepsis around the world: a systematic review exploring the economic burden of sepsis. van den Berg M, van Beuningen FE, Ter Maaten JC, Bouma HR. J Crit Care. 2022;71:154096. doi: 10.1016/j.jcrc.2022.154096. [DOI] [PubMed] [Google Scholar]
- 3.The global epidemiology of sepsis. Does it matter that we know so little? Finfer S, Machado FR. Am J Respir Crit Care Med. 2016;193:228–230. doi: 10.1164/rccm.201510-1976ED. [DOI] [PubMed] [Google Scholar]
- 4.Assessment of global incidence and mortality of hospital-treated sepsis. Current estimates and limitations. Fleischmann C, Scherag A, Adhikari NK, et al. Am J Respir Crit Care Med. 2016;193:259–272. doi: 10.1164/rccm.201504-0781OC. [DOI] [PubMed] [Google Scholar]
- 5.Reducing the global burden of sepsis. Dugani S, Veillard J, Kissoon N. CMAJ. 2017;189:0–3. doi: 10.1503/cmaj.160798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Assessment of clinical criteria for sepsis: for the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) Seymour CW, Liu VX, Iwashyna TJ, et al. JAMA. 2016;315:762–774. doi: 10.1001/jama.2016.0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Global, regional, and national sepsis incidence and mortality, 1990-2017: analysis for the Global Burden of Disease Study. Rudd KE, Johnson SC, Agesa KM, et al. Lancet. 2020;395:200–211. doi: 10.1016/S0140-6736(19)32989-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Increased time to initial antimicrobial administration is associated with progression to septic shock in severe sepsis patients. Whiles BB, Deis AS, Simpson SQ. Crit Care Med. 2017;45:623–629. doi: 10.1097/CCM.0000000000002262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Surviving Sepsis Campaign bundle: 2018 update. Levy MM, Evans LE, Rhodes A. Intensive Care Med. 2018;44:925–928. doi: 10.1007/s00134-018-5085-0. [DOI] [PubMed] [Google Scholar]
- 10.Implementation of a multicenter performance improvement program for early detection and treatment of severe sepsis in general medical-surgical wards. Schorr C, Odden A, Evans L, Escobar GJ, Gandhi S, Townsend S, Levy M. J Hosp Med. 2016;11:0–9. doi: 10.1002/jhm.2656. [DOI] [PubMed] [Google Scholar]
- 11.Prediction of sepsis patients using machine learning approach: a meta-analysis. Islam MM, Nasrin T, Walther BA, Wu CC, Yang HC, Li YC. Comput Methods Programs Biomed. 2019;170:1–9. doi: 10.1016/j.cmpb.2018.12.027. [DOI] [PubMed] [Google Scholar]
- 12.Development and validation of the phoenix criteria for pediatric sepsis and septic shock. Sanchez-Pinto LN, Bennett TD, DeWitt PE, et al. JAMA. 2024;331:675–686. doi: 10.1001/jama.2024.0196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Evans L, Rhodes A, Alhazzani W, et al. Intensive Care Med. 2021;47:1181–1247. doi: 10.1007/s00134-021-06506-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kule A, Bradley R, Flores-Bauer G, Stassen W, Djarv T on behalf of the International Liaison Committee on Resuscitation First Aid Task Force. Recognition of sepsis in first aid. First Aid Task Force synthesis of a scoping review. [ Jan; 2024 ]. 2024. https://costr.ilcor.org/document/first-aid-recognition-of-sepsis-a-scoping-review https://costr.ilcor.org/document/first-aid-recognition-of-sepsis-a-scoping-review
- 15.PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Tricco AC, Lillie E, Zarin W, et al. Ann Intern Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 16.Rayyan - a web and mobile app for systematic reviews. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Syst Rev. 2016;5:210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Screening tools for sepsis identification in paramedicine and other emergency contexts: a rapid systematic review. De Silva M, Chadwick W, Naidoo N. Scand J Trauma Resusc Emerg Med. 2023;31:74. doi: 10.1186/s13049-023-01111-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Prehospital management and identification of sepsis by emergency medical services: a systematic review. Lane D, Ichelson RI, Drennan IR, Scales DC. Emerg Med J. 2016;33:408–413. doi: 10.1136/emermed-2015-205261. [DOI] [PubMed] [Google Scholar]
- 19.Identification of adults with sepsis in the prehospital environment: a systematic review. Smyth MA, Brace-McDonnell SJ, Perkins GD. BMJ Open. 2016;6:0. doi: 10.1136/bmjopen-2016-011218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patient, public, and healthcare professionals' sepsis awareness, knowledge, and information seeking behaviors: a scoping review. Fiest KM, Krewulak KD, Brundin-Mather R, Leia MP, Fox-Robichaud A, Lamontagne F, Leigh JP. Crit Care Med. 2022;50:1187–1197. doi: 10.1097/CCM.0000000000005564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.The Prehospital Sepsis Project: out-of-hospital physiologic predictors of sepsis outcomes. Baez AA, Hanudel P, Wilcox SR. Prehosp Disaster Med. 2013;28:632–635. doi: 10.1017/S1049023X1300890X. [DOI] [PubMed] [Google Scholar]
- 22.The quick sequential organ failure assessment (qSOFA) identifies septic patients in the out-of-hospital setting. Barbara P, Graziano C, Caputo W, Litvak I, Battinelli D, Hahn B. Am J Emerg Med. 2018;36:1022–1026. doi: 10.1016/j.ajem.2018.01.073. [DOI] [PubMed] [Google Scholar]
- 23.Prehospital early warning scores for adults with suspected sepsis: retrospective diagnostic cohort study. Goodacre S, Sutton L, Thomas B, et al. Emerg Med J. 2023;40:768–776. doi: 10.1136/emermed-2023-213315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Prehospital qSOFA, mSOFA, and NEWS2 performance for sepsis prediction: a prospective, multi-center, cohort study. Melero-Guijarro L, Sanz-García A, Martín-Rodríguez F, et al. Front Med (Lausanne) 2023;10:1149736. doi: 10.3389/fmed.2023.1149736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Evaluation of the PRESEP Score and the Miami Sepsis Score for prehospital sepsis screening. Nualprasert P, Pattanarattanamolee R, Padtalaka P, Nakahara S. Prehosp Emerg Care. 2024;28:369–374. doi: 10.1080/10903127.2023.2166176. [DOI] [PubMed] [Google Scholar]
- 26.Prehospital characteristics among patients with sepsis: a comparison between patients with or without adverse outcome. Olander A, Andersson H, Sundler AJ, Bremer A, Ljungström L, Hagiwara MA. BMC Emerg Med. 2019;19:43. doi: 10.1186/s12873-019-0255-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Public awareness and knowledge of sepsis: a cross-sectional survey of adults in Canada. Parsons Leigh J, Brundin-Mather R, Moss SJ, et al. Crit Care. 2022;26:337. doi: 10.1186/s13054-022-04215-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.The sensitivity of qSOFA calculated at triage and during emergency department treatment to rapidly identify sepsis patients. Perman SM, Mikkelsen ME, Goyal M, et al. Sci Rep. 2020;10:20395. doi: 10.1038/s41598-020-77438-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.The prehospital assessment of patients with a final hospital diagnosis of sepsis: results of an observational study. Sjösten O, Nilsson J, Herlitz J, Axelsson C, Jiménez-Herrera M, Andersson Hagiwara M. Australas Emerg Care. 2019;22:187–192. doi: 10.1016/j.auec.2019.02.002. [DOI] [PubMed] [Google Scholar]
- 30.qSOFA as a new community-acquired pneumonia severity score in the emergency setting. Spagnolello O, Ceccarelli G, Borrazzo C, et al. Emerg Med J. 2021;38:906–912. doi: 10.1136/emermed-2019-208789. [DOI] [PubMed] [Google Scholar]
- 31.The role of the quick sequential organ failure assessment score (qSOFA) and modified early warning score (MEWS) in the pre-hospitalization prediction of sepsis prognosis. Usul E, Korkut S, Kayipmaz AE, Halici A, Kavalci C. Am J Emerg Med. 2021;41:158–162. doi: 10.1016/j.ajem.2020.09.049. [DOI] [PubMed] [Google Scholar]
- 32.Sepsis in adults and older children. [ Aug; 2023 ]. 2019. https://www.sja.org.uk/get-advice/first-aid-advice/sepsis/sepsis-in-adults-and-older-children/ https://www.sja.org.uk/get-advice/first-aid-advice/sepsis/sepsis-in-adults-and-older-children/
- 33.Identifying sepsis. [ Aug; 2023 ]. 2023. https://www.scottishambulance.com/first-aid-education/identifying-sepsis/ https://www.scottishambulance.com/first-aid-education/identifying-sepsis/
- 34.Sepsis - what to look out for. [ Aug; 2023 ]. 2022. https://firstaidforlife.org.uk/sepsis/ https://firstaidforlife.org.uk/sepsis/
- 35.What is septic shock and how to prevent it. [ Aug; 2023 ]. 2022. https://cprfirstaid.com.au/what-is-septic-shock-and-how-to-prevent-it/ https://cprfirstaid.com.au/what-is-septic-shock-and-how-to-prevent-it/
- 36.What is sepsis? [ Aug; 2023 ]. 2023. https://anderssonfirstaidtraining.co.uk/blog/what-is-sepsis/ https://anderssonfirstaidtraining.co.uk/blog/what-is-sepsis/
- 37.Guideline 9.2.12 - Recognition and first aid management of the seriously ill person including sepsis. [ Aug; 2023 ]. 2021. https://www.anzcor.org/assets/anzcor-guidelines/guideline-9-2-12-recognition-and-first-aid-management-of-the-seriously-ill-person-including-sepsis-273.pdf https://www.anzcor.org/assets/anzcor-guidelines/guideline-9-2-12-recognition-and-first-aid-management-of-the-seriously-ill-person-including-sepsis-273.pdf
- 38.6 Clues to spotting sepsis. [ Aug; 2023 ]. 2023. https://hts-training.co.uk/sepsis-symptoms/ https://hts-training.co.uk/sepsis-symptoms/
- 39.Could it be sepsis? [ Aug; 2023 ]. 2017. https://www.skillbasefirstaid.com/could-it-be-sepsis/ https://www.skillbasefirstaid.com/could-it-be-sepsis/
- 40.Sepsis awareness. [ Aug; 2023 ]. 2021. https://www.firstresponse.org.uk/medical-training/sepsis https://www.firstresponse.org.uk/medical-training/sepsis
- 41.Sepsis signs and symptoms. [ Aug; 2023 ]. 2022. https://www.hippocraticpost.com/first-aid/sepsis-signs-and-symptoms/ https://www.hippocraticpost.com/first-aid/sepsis-signs-and-symptoms/
- 42.Understanding sepsis: essential guide for early detection. [ Aug; 2023 ]. 2023. https://nrmedical.training/blog/sepsis-spot-it-early https://nrmedical.training/blog/sepsis-spot-it-early
- 43.What is sepsis? End Sepsis. [ Aug; 2023 ]. 2023. https://www.endsepsis.org/what-is-sepsis/ https://www.endsepsis.org/what-is-sepsis/
- 44.Could it be sepsis? TLCT. [ Aug; 2023 ]. 2023. https://www.tlct.co.uk/could-it-be-sepsis/ https://www.tlct.co.uk/could-it-be-sepsis/
- 45.Sepsis Public Awareness Campaign Workgroup Meeting #1 Minutes. [ Aug; 2023 ]. 2018. https://health.maryland.gov/phpa/IDEHASharedDocuments/Minutes%20for%20Sepsis%20Workgroup%20Meeting%201.cc5.pdf https://health.maryland.gov/phpa/IDEHASharedDocuments/Minutes%20for%20Sepsis%20Workgroup%20Meeting%201.cc5.pdf
- 46.Get ahead of sepsis - know the risks. Spot the signs. Act fast. [ Aug; 2023 ]. 2023. https://www.cdc.gov/patientsafety/features/get-ahead-of-sepsis.html https://www.cdc.gov/patientsafety/features/get-ahead-of-sepsis.html
- 47.Sepsis - symptoms and causes. [ Aug; 2023 ]. 2023. https://www.mayoclinic.org/diseases-conditions/sepsis/symptoms-causes/syc-20351214 https://www.mayoclinic.org/diseases-conditions/sepsis/symptoms-causes/syc-20351214
- 48.Sepsis (septicemia) - symptom and causes. [ Aug; 2023 ]. 2022. https://www.pennmedicine.org/for-patients-and-visitors/patient-information/conditions-treated-a-to-z/sepsis https://www.pennmedicine.org/for-patients-and-visitors/patient-information/conditions-treated-a-to-z/sepsis
- 49.Sepsis. [ Aug; 2023 ]. 2023. https://www.who.int/news-room/fact-sheets/detail/sepsis https://www.who.int/news-room/fact-sheets/detail/sepsis
- 50.Symptoms - sepsis. [ Aug; 2023 ]. 2022. https://www.nhs.uk/conditions/sepsis/ https://www.nhs.uk/conditions/sepsis/
- 51.Recognizing signs of sepsis. [ Aug; 2023 ]. 2023. https://www.texomamedicalcenter.net/recognizing-signs-sepsis https://www.texomamedicalcenter.net/recognizing-signs-sepsis
- 52.It's about TIME. [ Aug; 2023 ]. 2023. https://www.sepsis.org/about/its-about-time/ https://www.sepsis.org/about/its-about-time/
- 53.7 Warning signs of sepsis. [ Aug; 2023 ]. 2023. https://www.aarp.org/health/conditions-treatments/info-2023/sepsis-symptoms.html https://www.aarp.org/health/conditions-treatments/info-2023/sepsis-symptoms.html
- 54.About sepsis. [ Aug; 2023 ]. 2023. https://sepsistrust.org/about/about-sepsis/ https://sepsistrust.org/about/about-sepsis/
- 55.Sepsis: symptoms, causes, treatment and prevention. [ Aug; 2023 ]. 2023. https://my.clevelandclinic.org/health/diseases/12361-sepsis https://my.clevelandclinic.org/health/diseases/12361-sepsis
- 56.Sepsis - symptoms, causes, complications, and treatment. [ Aug; 2024 ]. 2023. https://www.kidney.org/atoz/content/sepsis https://www.kidney.org/atoz/content/sepsis
- 57.Quality statement 1 - could it be sepsis? [ Aug; 2023 ]. 2022. https://www.safetyandquality.gov.au/standards/clinical-care-standards/sepsis-clinical-care-standard/quality-statements/quality-statement-1-could-it-be-sepsis https://www.safetyandquality.gov.au/standards/clinical-care-standards/sepsis-clinical-care-standard/quality-statements/quality-statement-1-could-it-be-sepsis
- 58.Adult sepsis. [ Aug; 2023 ]. 2021. https://clinicalexcellence.qld.gov.au/priority-areas/safety-and-quality/sepsis/adult-sepsis https://clinicalexcellence.qld.gov.au/priority-areas/safety-and-quality/sepsis/adult-sepsis
- 59.Implementation and evaluation of a pilot WHO community first aid responder training in Kinshasa, DR Congo: a mixed method study. Diango K, Mafuta E, Wallis LA, Cunningham C, Hodkinson P. Afr J Emerg Med. 2023;13:258–264. doi: 10.1016/j.afjem.2023.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]