SUMMARY
According to the International Continence Society, stress (static) urinary incontinence is defined as any involuntary loss of urine on effort or physical exertion, due to which intravesical pressure overcomes urethral pressure, with no detrusor activity. Urodynamic testing accurately assesses the function of the bladder and urethra. The urodynamic assessment includes three tests: cystometry, uroflowmetry and profilometry (determination of urethral pressure profile). Prior to urodynamic assessment, it is mandatory to rule out urinary tract infection since it is an invasive test. Urethral profilometry is a technique that measures pressure in the urethra and bladder at rest, during stressful actions, and during the act of miction. Its main purpose is to evaluate the sphincter mechanism. During the examination, a special catheter is used, which is being slowly pulled out from the bladder neck throughout the urethra, with continuous recording of intraurethral pressure. In addition to measuring urethral pressures, stress urinary incontinence is also very successfully proven by the cough test and Bonney test. If, on forced cough, the urine escapes uncontrollably, and continence is restored by finger lifting the neck of the bladder, the diagnosis of static incontinence is confirmed. At our urogynecologic clinic, urodynamic examination is being routinely performed. In the present study, we included patients previously treated for urinary stress incontinence and compared their results of urodynamic assessment to the results of Bonney test. Of the 43 subjects in whom stress incontinence was proven with Bonney test, we recorded an appropriate profilometry result in 13 cases.
Key words: Urodynamic assessment, Stress incontinence, Bonney test
Introduction
According to the International Continence Society (ICS), stress (static) urinary incontinence is defined as any involuntary loss of urine on effort or physical exertion, due to which intravesical pressure overcomes urethral pressure, with no detrusor activity. Urinary incontinence is a common condition that affects millions of people worldwide (1, 3). Urodynamic testing accurately assesses the function of the lower urinary tract (4, 5). Urethral profilometry is a technique that measures pressure in the urethra and bladder at rest, during stressful actions, and during the act of miction. Its main purpose is to evaluate the sphincter mechanism (4, 5). During the examination, a special catheter is used, which is being slowly pulled out from the bladder neck throughout the urethra, with continuous recording of intraurethral pressure. Stress urinary incontinence is also very successfully proven by the cough test and Bonney test (4-6). If, on forced cough, the urine escapes uncontrollably, and continence is restored by finger lifting the neck of the bladder, the diagnosis of static incontinence is confirmed. At our urogynecologic clinic, urodynamic examination is being routinely performed. In this retrospective study, we included patients previously treated for urinary stress incontinence and compared their results of urodynamic assessment to the results of Bonney test. It is important to note that the operational program was greatly reduced during the COVID-19 pandemic period.
Subjects and Material
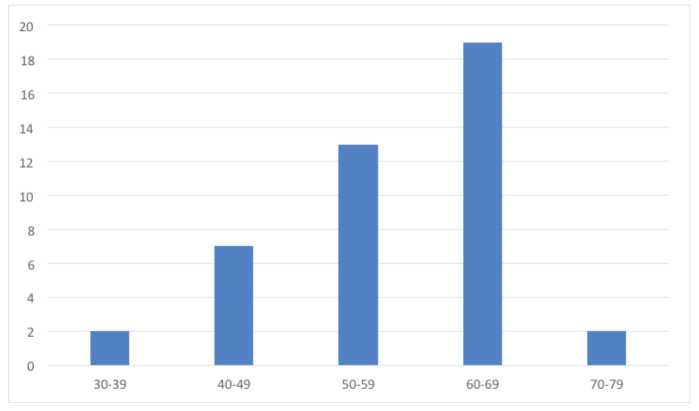
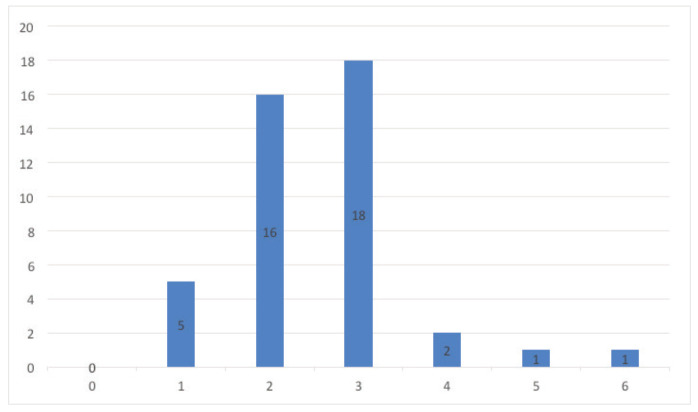
The study included 43 patients treated at our urogynecologic clinic from January 2017 to December 2021. Patients were grouped according to age. The largest proportion of respondents were in the 60-69 age group (n=19, 44.2%), and only two (4.7%) patients were in the 30-39 and 70-79 age groups each (Fig. 1). The youngest and oldest patients were aged 38 and 75 years, respectively. Patient distribution according to parity showed that most patients had three deliveries (n=18, 41.9%), whereas none of the women was nulliparous (Fig. 2) (2).
Fig 1.
Distribution of subjects according to age groups (years).
Fig. 2.
Distribution of subjects according to parity (number of deliveries).
All patients underwent complete evaluation that included standardized history and physical examination, urinalysis and urine culture, and finally urodynamic assessment about a month prior to treatment. During profilometry (4), measurements of functional urethral length (FUL) and pressure transfer during cough were assessed, comparing the pressure recorded at mid-urethral portion and in the bladder. If the bladder pressure exceeds the pressure obtained at the mid-urethral portion, the diagnosis of stress incontinence is confirmed. Finally, with a full bladder, Bonney test (7) was carried out, where the escape of urine from the bladder is observed, which, if stopped by finger lifting the bladder neck, also denotes stress incontinence.
Results and Discussion
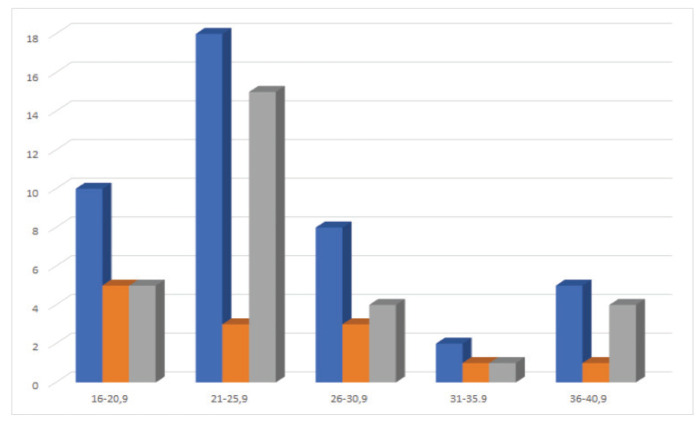
The subjects were divided according to the FUL, continence status according to coughing test in profilometry assessment, and finally, according to the method of treatment and success of the treatment method itself. According to the FUL, the subjects were divided into 5 groups (Fig. 3). Ten (23.2%) subjects had FUL of 16-20.9 mm, 18 (41.9%) were in the range of 21-25.9 mm, eight (18.6%) in the range of 26-30.9 mm, two (4.7%) in the range of 31-35.9 mm, and five (11.6%) in the range of 36-40.9 mm. Stress incontinence confirmed according to profilometry assessment was found in 5, 14, 4, 1 and 4 subjects from the above FUL groups, respectively. In 13 patients with a history of stress incontinence, we recorded normal result of pressure transfer during cough on profilometry, but the same patients also had a positive Bonney test. Looking at the distribution of such cases (normal profilometry result and positive Bonney test) (Fig. 3), the lowest reliability of profilometry versus Bonney test was found in the group of subjects with FUL of 16-20.9 mm, i.e., five out of ten (50%) subjects. It is also important to note that we had two patients with proven stress incontinence on profilometry but negative Bonney test. Due to the history of complaints, both these patients underwent treatment for stress incontinence, one by Burch colposuspension (8), and the other one by paraurethral hyaluronic acid injection (9), and both experienced significant subjective improvement after treatment.
Fig. 3.
Distribution of subjects according to urethral length (mm, blue bars), incontinence on coughing test in profilometry assessment (gray bars) and profilometry/Bonney test discrepant findings (women with normal profilometry results but positive Bonney test, orange bars).
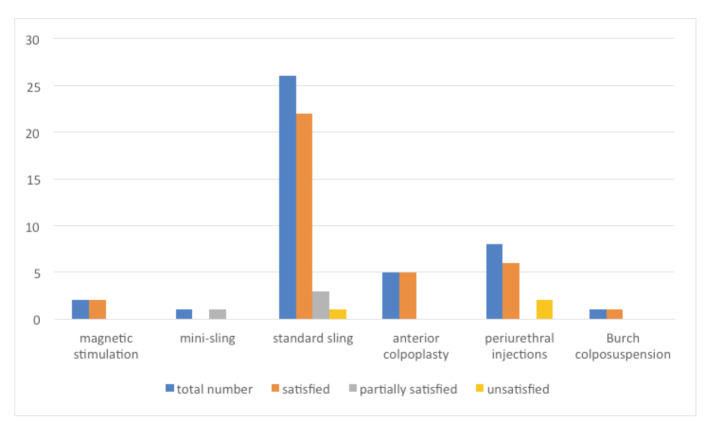
The treatment methods used included functional magnetic stimulation (10), placement of mini (11) or standard (12) suburethral sling, anterior colpoplasty (13), periurethral hyaluronic acid injections (9), and Burch colposuspension (8). The great majority of the 43 study patients (60.5%) were treated with the suburethral sling procedure. Looking at the cure rate, we found that the most successful method was anterior colpoplasty, with all these patients (n=5) reporting continence recovery after surgery. Figure 4 shows cure rate for each method. Study patients were offered to express themselves as follows: fully satisfied, partially satisfied, or dissatisfied with the treatment. In the suburethral sling method group with the largest number of patients, complete satisfaction was recorded in 22 of 26 (84.6%) patients, partial satisfaction in three (11.6%) patients, whereas only one (3%) patient was dissatisfied with the treatment. In two (7.7%) cases, treatment with suburethral sling led to de novo overactive bladder, which is a known postoperative complication, with a previously reported incidence of about 9% (14).
Fig 4.
Distribution of subjects according to cure by particular methods.
The method of periurethral injection of hyaluronic acid proved to be the least successful procedure with 6 out of 8 (75%) subjects being satisfied with the treatment, whereas the remaining two patients expressed dissatisfaction with the treatment. Those were treated in the second act with suburethral sling placement and eventually became fully satisfied with the treatment (they were not included in the group of those primarily treated with suburethral sling). In one patient treated with the suburethral sling method, intraoperative bladder perforation occurred and mesh repositioning with subsequent satisfaction was eventually achieved (15).
Conclusion
Based on the results obtained in this study, the diagnosis of stress urinary incontinence is more accurately achieved with Bonney test in comparison to the urodynamic method of profilometry. We emphasize that performing Bonney test is much simpler and more affordable in everyday practice compared to a significantly more invasive method of profilometry. In order to confirm the results obtained, further research is needed.
References
- 1.Škegro SN. Konzervativno liječenje statičke inkontinencije mokraće i defekta dna zdjelice. Izabrana poglavlja iz urologije/Selected Chapters in Urology. Medicus. 2015;25(1):25–32. [in Croatian] [Google Scholar]
- 2.Živković K, Živković N, Župić T, Hodžić D, Mandić V, Orešković S. Effect of delivery and episiotomy on the emergence of urinary incontinence in women: review of literature. Acta Clin Croat. 2016;55:615–24. 10.20471/acc.2016.55.04.12 [DOI] [PubMed] [Google Scholar]
- 3.Melville JL, Katon W, Delaney K, Newton K. Urinary incontinence in US women: a population based study. Arch Intern Med. 2005;165:537–42. 10.1001/archinte.165.5.537 [DOI] [PubMed] [Google Scholar]
- 4.Orešković S, Pavić M. Urinarna inkontinencija kod žena i smjernice za liječenje. Izabrana poglavlja iz urologije/Selected Chapters in Urology. Medicus. 2015;25(1):13–23. [in Croatian] [Google Scholar]
- 5.Trošelj M, Rubinić N, Vukelić I, Markić D. Urodinamika i njezina klinička primjena. Med Flum. 2017;53(3):351–8. 10.21860/medflum2017_182974 [DOI] [Google Scholar]
- 6.Chapple CR, MacDiarmid SA. Urodynamics Made Easy. 2nd edn. London: Churchill Livingstone, 2000. [Google Scholar]
- 7.Mozetič V, Sotošek S, Ružić B, Grubišić I. Urološka propedeutika i dijagnostički postupci u urologiji – urodinamika. In: Kvesić A, Paladino J, editors. Kirurgija. Zagreb: Medicinska naklada, 2016; p. 713-4. (in Croatian) [Google Scholar]
- 8.Klutke JJ, Klutke CG, Bergman J, Elia G. Bladder neck suspension for stress urinary incontinence: how does it work? Neurourol Urodyn. 1999;18(6):623–7. [DOI] [PubMed] [Google Scholar]
- 9.Khalef JA, Ibraheem JK, Zghair LF. Urodex injection (urethral bulking agent) outcomes in treatment of stress incontinence, interventional study. IOSR J Pharm Biol Sci. 2018. September-October;13(5):42–5. [Google Scholar]
- 10.Sun K, Zhang D, Wu G, Wang T, Wu J, Ren H, et al. Efficacy of magnetic stimulation for female stress urinary incontinence: a meta-analysis. Ther Adv Urol. 2021. July 13;13:17562872211032485. 10.1177/17562872211032485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Castellier C, Doucède G, Debodinance P. Place of the mini-sling in the treatment of female stress urinary incontinence. J Gynecol Obstet Biol Reprod (Paris). 2013. November;42(7):639–46. Epub 2013 Aug 20. 10.1016/j.jgyn.2013.07.002 [DOI] [PubMed] [Google Scholar]
- 12.Nambiar A, Cody JD, Jeffery ST, Aluko P. Single-incision sling operations for urinary incontinence in women. Cochrane Database Syst Rev. 2017. July 26;7(7):CD008709. 10.1002/14651858.CD008709.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Glazener CM, Cooper K, Mashayekhi A. Anterior vaginal repair for urinary incontinence in women. Cochrane Database Syst Rev. 2017. July 31;7(7):CD001755. 10.1002/14651858.CD001755.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Manodoro S, Barba M, Locatelli L, Palmieri S, Marino G, Frigerio M. Urodynamic predictors of de novo overactive bladder after single-incision sling. Int J Gynaecol Obstet. 2021. June;153(3):412–6. 10.1002/ijgo.13503 [DOI] [PubMed] [Google Scholar]
- 15.Israfil-Bayli F, Bulchandani S, Parsons M, Jackson S, Toozs-Hobson P. Bladder perforation during sling procedures: diagnosis and management of injury. Int Urogynecol J. 2014. May;25(5):691–2. 10.1007/s00192-013-2291-8 [DOI] [PubMed] [Google Scholar]