SUMMARY
The postoperative care unit at the Department of Urology has significantly improved treatment of patients undergoing surgical procedures and reduced admission of urologic patients to the Intensive Care Unit (ICU). We examined the characteristics of urologic patients, time on mechanical ventilation, most common complications, and mortality in the period from January 2017 to March 2022. A total of 84 admissions to ICU were recorded, accounting for 1.5% of all patients having undergone surgical, therapeutic or diagnostic interventions under general or regional anesthesia at the Department of Urology. The most common reasons for admission to ICU were respiratory failure (79 patients), hemodynamic instability, and bleeding. The median time on mechanical ventilation was 9.7 [2.4-58.2] hours in urology patients vs. 6 [3-14.7] hours in the rest of surgical ICU patients (p=0.058). Hypertension and renal failure were more common in urologic than in the rest of surgical ICU patients (p<0.05). The overall mortality of urologic patients was lower than in the rest of surgical ICU patients (10.7% vs. 18.99%, p=0.08) but the difference did not reach statistical significance. Independently of the lower mortality, improvements in the outcome of urologic patients admitted to the ICU are feasible. Early identification of patients at risk of infections, postoperative respiratory failure, cardiovascular incidents, and bleeding may further reduce mortality and improve outcomes.
Key words: Intensive care unit; Urologic surgical procedures; Cardiopulmonary resuscitation; Mechanical ventilation, Critical care outcomes
Introduction
Due to their special characteristics, urologic patients require customized postoperative care. Significant comorbidity that is more common in the elderly urologic population, infections, or intraoperative complications may be the reason for surgical Intensive Care Unit (ICU) admission, and increased mortality (1-3).
The type of surgery influences the frequency of ICU admissions. According to data from the study by Ha et al., the most common admissions of urologic patients to the ICU were recorded after radical cystectomy (4). The ICU admission was recorded in 76% of patients who had postoperative delirium and 54.8% of patients who did not have delirium (4). Admissions to the ICU are less frequent in patients undergoing less invasive surgical procedures. Within 30 days of 104,100 outpatient urethroscopies (URS), all re-admissions to the hospital in patients older than 18 years were recorded in the American commercial database IBM® MarketScan® (5). The study confirmed a frequency of 5.5% of sepsis in URS patients. A total of 35% of septic URS patients were admitted to the ICU, or 1.9% of all patients having undergone URS (6). Patients at special risk were elderly, diabetic, patients having undergone an in-hospital procedure, and those with multiple comorbidities. The mean hospitalization time was 6.7 days (6).
Similar data were obtained in the study by Stone et al. (7). The most common surgical complications requiring return to the operating room were recorded after cystectomy (5.8%) and less frequently after outpatient cystourethroscopy and resection of bladder tumors (7). The most common complications were bleeding, sepsis, and organ system infections. These patients also required prolonged mechanical ventilation (odds ratio [OR] 0.2-0.5, p<0.01) (7).
Patient characteristics such as gender may also influence the frequency of ICU admission and hospital readmission (8). In the study by Down et al., which was conducted on 231 consecutive patients with renal colic, women had a higher risk of infection, more percutaneous nephrostomy insertion and higher frequency of admission to the ICU than men (9.8% vs. 0.7%, p=0.005). In order to examine the frequency of readmissions and their association with patient risk factors, Rambachan et al. analyzed the National Surgical Quality Improvement Program database (9). The authors identified 7,795 patients who were readmitted to the hospital after outpatient urologic surgery (9). Patients with an increased rate of medical and surgical complications were male patients, American Society of Anesthesiologists (ASA) 3 or 4 classifications, and patients with a history of cancer and bleeding disorders (9).
Prostate cancer is the most common newly diagnosed cancer in men, while bladder and kidney cancer are the 4th and 5th most common cancers in adult men in Croatia (10). In women, the incidence of these cancers is somewhat lower, and bladder and kidney cancer are the 9th and 12th most common cancers (10). Given data on the relatively high frequency of these cancers in the adult population, we wanted to examine the frequency of admission of patients from the Department of Urology to the ICU in the Osijek University Hospital Center, Osijek, Croatia. We also wanted to compare their comorbidities, the most common reasons for their admission, time spent on mechanical ventilation, and mortality with those in the overall surgical ICU population.
Materials and Methods
After obtaining the Ethics Committee approval (R1/6414/2021) for this retrospective study, database of the Department of Intensive Care Medicine in the Osijek University Hospital Center was analyzed. The study included all patients (N=84) admitted from Department of Urology after surgery, endoscopic or diagnostic procedures to the ICU between January 2017 and March 2022. As a control group, 258 consecutive patients admitted to the ICU in 2019 and 2021 were selected. For all patients, age, sex, type of admission (elective or emergency), comorbidity, operations performed, reoperations, Simplified Acute Physiology Score II (SAPS II) on admission and discharge, white blood cell count, C-reactive protein (CRP) and procalcitonin (PCT) were recorded. The length of ICU treatment, the length of mechanical ventilation, and mortality were recorded as indicators of outcome. The length of mechanical ventilation in medical records was recorded in hours.
Comorbidity was counted as a binary variable as present or absent. Diseases for which the patient had been prescribed drug therapy were recorded at the time of admission in medical charts. Conditions arising during hospital treatment such as renal failure or coagulopathy were also recorded. Infections of specific organ systems were recorded as comorbidity, so pneumonia was considered respiratory comorbidity, and urinary tract infection urologic comorbidity. For this analysis, urologic tumors and infections were divided into upper urinary tract and lower urinary tract diseases. Renal tumors and infections were considered renal diseases, and tumors and infections of the prostate, bladder and genital organs were considered lower urinary tract diseases. Sepsis was considered an infection characterized by a positive blood culture with clinical and laboratory indicators of inflammation. Soft tissue infections such as surgical wound infection, retroperitoneal abscesses, cellulitis, or Fournier’s gangrene were classified as soft tissue infections. Chronic alcoholism was classified in the category of psychiatric diseases and liver disease. Cardiopulmonary resuscitation on admission was considered a state of severe hypotension requiring vasoactive drugs and emergency intubation.
Statistical analysis
Statistical analysis was performed using IBM SPSS 20.0 for Windows (IBM, USA) software. Categorical data were presented in absolute and relative frequencies. The normality of distribution of numerical variables was tested by the Kolmogorov-Smirnov test. Differences in categorical variables were tested by the χ2-test or Fisher exact test. Numerical data were described by median and interquartile range (IQR). The correlation of the variables was assessed by Spearman’s correlation coefficient. Differences in continuous variables between the two independent groups were tested by the independent samples median test. All p values were two-sided. The level of significance was set at α=0.05.
Results
In the period between January 2017 and March 2021, a total of 84 admissions were recorded, accounting for 1.4% of all patients who needed general anesthesia, regional anesthesia, or sedation with monitored anesthesia care for operative procedures, therapeutic or diagnostic procedures at the Department of Urology. During the first one-year period observed (January 2017 to January 2018), there were 24 ICU admissions of urology patients. The frequency of admission gradually decreased to 16, 17 and 15 per year. In the period from January 2021 to March 2022, 13 urologic patients were admitted to the ICU. Patient demographic data are shown in Table 1.
Table 1. Characteristics of urologic patients admitted to the ICU between January 2017 and March 2022 and comparison with control group.
| Demographic parameter | Urologic patients (N=84) | Control group (N=258) | p |
|---|---|---|---|
| Age (years) | 64.5 [64.5-72] | 65.5 [65.5-72] | 0.973 |
| Sex (male:female, n) | 62:22 (73.9%:26.1%) | 165:93 (64%:36%) | 0.097 |
| Type of admission (elective:emergency, n) | 50:34 (40.4%) | 114:144 (55.8%) | 0.015* |
| Operated patients | 79 (94.1%) | 235 (91.1%) | 0.4 |
| Reoperation | 14 (19.7%) | 40 (17.2%) | 0.993 |
| SAPS II score – admission | 46.5 [46.5-60.5] | 45 [45-58] | 0.687 |
| SAPS II score – discharge | 33 [33-34] | 33 [33-34] | 0.933 |
| White blood cells on ICU admission (x109) | 14.9 [14,9-20.3] | 13.4 [13.4-17.2] | 0.002* |
| C-reactive protein on ICU admission | 121.5 [121.5-242.3] | 72.5 [72.5-173.1] | 0.058 |
| PCT on ICU admission (µg/L) | 1.8 [1.8-17.1] | 1.1 [1.1-6.9] | 0.151 |
| Outcome | |||
| ICU days | 2 [2-4] | 3 [3-6] | 0.056 |
| Mechanical ventilation (hours) | 9.7 [2.4-58.2] | 6 [3-14.7] | 0.058 |
| Mortality rate | 10.7% | 18.9% | 0.08 |
*Statistically significant differences confirmed by median test for continuous variables; χ2-test or Fisher exact were used for categorical data; SAPS II score = Simplified Acute Physiology Score II; ICU = intensive care unit; PCT = procalcitonin
In the group of urologic patients admitted to the ICU, 60% of patients were elective versus only 44% of elective patients in the control group. Surgical procedures that were performed in the patients admitted to the ICU are shown in Figure 1. Thirty-one patients were admitted after nephrectomy (36.9%) and 28 (33.3%) after cystectomy. Reinterventions were performed in 19% of patients admitted to the ICU (Fig. 1).
Fig. 1.
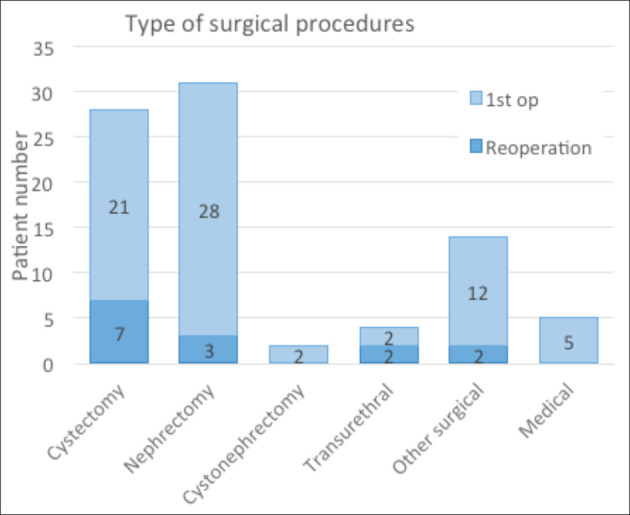
Surgical procedures performed in patients admitted to the Intensive Care Unit: patients admitted after reinterventions are shown for each procedure; patients who were not operated on are presented as medical.
The number of hypertensive patients in this population was higher than in the control group (73% of urologic patients vs. 66% in the control group, p=0.048) (Table 2). In the population of urologic patients, a significantly higher proportion of patients who required cardiopulmonary resuscitation (CPR) on admission were admitted to the ICU as compared with the general population of patients admitted to the ICU (15.4% vs. 4.6%, p<0.001) (Table 2).
Table 2. Comorbidities in urologic patients and comparison with control group of surgical patients admitted to the ICU between January 2017 and March 2022.
| Comorbidities* | Urologic patients (N=84) | Control group (N=258) | p |
|---|---|---|---|
| Cardiac (myocardial infarction, fibrillation, angina pectoris, CABG) | 23 (27.3%) | 93 (36%) | 0.129 |
| Vascular (hypertension, peripheral vascular disease) | 65 (77.3%) | 170 (66.4%) | 0.048* |
| CPR on admission | 13 (15.4%) | 12 (4.6%) | <0.0001* |
| Neurological | 23 (27.3%) | 89 (34.4%) | 0.027 |
| Renal (tumors, infections, renal failure) | 26 (30.9%) | 51 (19.7%) | <0.0001* |
| Bladder and prostate diseases (tumors, infections) | 52 (61.9%) | 24 (9.3%) | <0.0001* |
| Gastrointestinal | 28 (33.3%) | 130 (50.3%) | 0.006* |
| Metabolic | 26 (30.9%) | 47 (18.2%) | 0.024* |
| Endocrine diseases | 14 (16.7) | 70 (37.4) | 0.051 |
| Coagulopathies | 3 (3.5%) | 15 (5.8%) | 0.6 |
| Respiratory | 26 (30.9%) | 104 (40.3%) | 0.125 |
| Hepatobiliary | 14 (16.6%) | 37 (14.3%) | 0.613 |
| Tumors | 67 (79.7%) | 129 (50%) | <0.0001* |
| Sepsis | 14 (16.6%) | 40 (15.5%) | 0.799 |
| Soft tissue infections | 20 (23.8%) | 12 (4.7%) | <0.0001* |
| Trauma | 6 (7.1%) | 39 (15.1%) | 0.060 |
*For each examined comorbidity, the number of patients with the specific comorbid condition is shown, and the percentage within the group of urology or control ICU patients; ICU = intensive care unit; CABG = coronary artery bypass graft; CPR = cardiopulmonary resuscitation
A total of 79 patients required mechanical ventilation due to respiratory failure. The median time of mechanical ventilation was 9.7 [2.4-58.2] hours in urologic and 6 [3-14.7] hours in control patients (p=0.058). The mortality of urologic patients was 10.71%, and of all patients admitted to ICU 18.99% (Table 1).
A correlation analysis confirmed that mortality was in correlation with emergency admission to ICU (Spearman correlation ρ=0.343, p=0.001), sepsis (ρ=0.466, p<0.0001), CPR on admission (ρ=0.385, p=0.0001), higher SAPS II score on admission (ρ=0.343, p=0.001), and infections on admission (ρ=0.372, p<0.0001). Together with sepsis, soft tissue infections, i.e., retroperitoneal abscesses, cellulitis or Fournier’s gangrene as entry diagnosis showed positive correlation with increased mortality (ρ=0.246, p=0.023).
Discussion
Our study confirmed the relatively low frequency of admission of surgical patients from the Department of Urology to the ICU in the Osijek University Hospital Center compared to data published in the literature (1-5). In various studies, the frequency of ICU admission in urologic patients is between 1.9% in patients after URS and 76% in patients who had postoperative delirium after cystectomy. The need of mechanical ventilation and hemodynamic instability were observed as the most common reasons for admission to the ICU in our patients, as also reported in other studies (11). We also confirmed the association of sepsis and soft tissue infections with increased patient mortality (11). In the group of urologic patients who were admitted to the ICU, reinterventions were most frequent after cystectomy (25%), followed by nephrectomy (9.7%), which is in accordance with data reported by other authors (4, 7).
There are several reasons that can be associated with the relatively low frequency of admission of urologic patients to the ICU. These can be appropriate preoperative selection of patients and a series of enhanced recovery after urologic surgery measures, such as less invasive surgical techniques, used of new hemostatic materials, and establishment of a postoperative care unit at the Department of Urology. In addition to the new methods of continuous postoperative monitoring, the education of nursing staff and infection control are important for the quality of care in the postoperative care unit (12, 13). Along with surgical measures, anesthetic procedures have also improved over time. These include more frequent use of regional anesthesia techniques, reduced use of opioids with the aim of reducing postoperative respiratory depression, use of non-opioid analgesics, preoperative optimization in anemic patients, patient-adjusted perioperative monitoring, and other measures (13, 14). Incorporation of all these procedures reduced the number of admissions to the ICU during the observed period.
An important factor that further reduced the frequency of admission of urologic patients to the ICU probably was the COVID-19 pandemic. From March 2021 until the end of the study period, the frequency of ICU admissions decreased significantly. Although there are no accurate data on this aspect, the experiences of numerous institutions confirmed that there was temporary postponement of elective procedures, including operations for malignant diseases and prioritizing of emergency patients during the pandemic (15, 16). The capacities of ICUs were diverted to the treatment of respiratory insufficiency in COVID-19 patients. At the same time, the use of less invasive procedures, day surgery procedures, outpatient procedures and telemedicine consultations in the urology practice have increased (15, 16).
Although the type of surgery is associated with increased surgical risks, admission to ICU should only be done in selected cases (17). In the study conducted on a series of 304 patients undergoing cystectomy, Chang et al. confirmed that only patients at an increased risk of surgical complications have an indication for admission to the ICU. Patients admitted to the ICU had longer operative time, intraoperative hemorrhage and received transfusions, and had higher ASA score (17). Comorbidities such as hypertension and diabetes were common in their patients admitted to the ICU (17), as also observed in our study.
In the study by Isharval et al., hypertension is one of the factors that was significantly correlated with long-term functional stability in patients undergoing partial nephrectomy (18). Furthermore, hypertension affected long-term outcomes in the study conducted by Eisenberg et al. in patients undergoing cystectomy (19). In urologic patients, hypertension with more frequent infections may contribute to a higher frequency of CPR on admission to the ICU, as observed in the urologic patients in our study (19, 20).
In this study, the most common reasons for admission to the ICU from the Department of Urology were respiratory failure, hemodynamic instability, and CPR. Other studies also showed that hemodynamic instability, the frequency of vasopressor use, and admission to the ICU were more common after cardiorespiratory arrest in patients with comorbidities and a history of tumors (9, 21, 22).
A higher mean initial values of CRP and leukocytes, and a higher frequency of soft tissue infections were observed in the population of urologic patients admitted to the ICU as compared to the control ICU group. These higher values could be associated with the type of disease and more frequent urinary tract infections (8, 23), as well as with the risk group of patients, such as the elderly and patients with multiple comorbid conditions. Previous instrumental urologic manipulation, duration of catheterization, and antibiotic use were also associated with infections in patients undergoing urologic surgery (24, 25). Similar results were also obtained in other studies (1, 3, 4, 6, 7, 11).
Sepsis and soft tissue infections, which are common in urologic patients, are significantly associated with mortality (20). Early recognition of deterioration in these patients could reduce their mortality (20). This is possible through targeted administration of antibiotics according to microbiological test results, laboratory analyses, and use of specific monitoring that might indicate the need of intensive treatment earlier (26). In this way, an appropriate treatment may be initiated earlier, and a relatively large number of urologic patients admitted to the ICU after CPR could be reduced (20).
Providing appropriate preoperative assessment using a frailty index, cardiopulmonary exercise testing, and routine microbiological samples in patients undergoing intra-abdominal surgery (including radical cystectomy) may suggest therapeutic interventions to be done before surgery (25). Such interventions are preoperative optimization of iron deficiency and anemia, preoperative exercise interventions, and implementation of targeted and appropriate microbiological therapy according to urine culture findings (5). Based on the new studies, less invasive procedures such as robotic surgery may be suggested to reduce perioperative blood loss and postoperative complications (27). In patients at a special risk, radical procedures may be discouraged, and patients may be subjected to oncologic treatment.
A disadvantage of this study was that data were analyzed retrospectively. In the beginning of the study, PCT as a marker of inflammation was not measured routinely. Consequently, its association with the outcome could not be determined, although it was higher in urologic patients. In addition, data on comorbidities were not recorded systematically because some patients were admitted as emergency patients and data on the history of the disease could not be obtained. A new prospective study involving more demographic data such as frailty scores, and more laboratory data could provide more detailed answers about the relationship between comorbidities and outcomes in urologic patients admitted to ICU.
Conclusion
Although the frequency of ICU admission of urology patients was low in our study, it is likely that it might be further improved. Individualized approach and identification of patients at risk of postoperative respiratory failure, bleeding, and cardiovascular incidents, along with prevention and early detection of infections may lead to reduced mortality and improved outcomes.
Acknowledgment
The authors acknowledge the staff of the Division of Anesthesiology, Department of Urology, Osijek University Hospital Center, for their assistance in writing this paper.
References
- 1.Dahm P, Tuttle-Newhall JE, Yowell CW, Byrne RR, Price DT. Indications for surgical intensive care unit admission of postoperative urologic patients. Urology. 2000;55(3):334–8. 10.1016/S0090-4295(99)00445-8 [DOI] [PubMed] [Google Scholar]
- 2.Cui HW, Turney BW, Griffiths J. The preoperative assessment and optimization of patients undergoing major urological surgery. Curr Urol Rep. 2017;18(7):54. 10.1007/s11934-017-0701-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel HV, Sterling JA, Srivastava A, Ghodoussipour SB, Jang TL, Grandhi MS, et al. The impact of venous thromboembolism on mortality and morbidity during nephrectomy for renal mass. Urology. 2022;168:122–8. 10.1016/j.urology.2022.05.033 [DOI] [PubMed] [Google Scholar]
- 4.Ha A, Krasnow RE, Mossanen M, Nagle R, Hshieh TT, Rudolph JL, et al. A contemporary population-based analysis of the incidence, cost, and outcomes of postoperative delirium following major urologic cancer surgeries. Urol Oncol. 2018;36(7):341.e15–22. 10.1016/j.urolonc.2018.04.012 [DOI] [PubMed] [Google Scholar]
- 5.Baboudjian M, Gondran-Tellier B, Di Bisceglie M, Abdallah R, Michel F, Sichez PC, et al. The prognostic value of serum procalcitonin in acute obstructive pyelonephritis. World J Urol. 2021;39(5):1583–9. 10.1007/s00345-020-03353-2 [DOI] [PubMed] [Google Scholar]
- 6.Bhojani N, Paranjpe R, Cutone B, Rojanasarot S, Chew BH. Predictors and Health Care Utilization of Sepsis Post-Ureteroscopy in a U.S.-Based Population: Results from the Endourological Society TOWER Collaborative. J Endourol. 2022. November;36(11):1411–7. 10.1089/end.2022.0010 [DOI] [PubMed] [Google Scholar]
- 7.Stone BV, Cohn MR, Donin NM, Schulster M, Wysock JS, Makarov DV, et al. Evaluation of unplanned hospital readmissions after major urologic inpatient surgery in the era of accountable care. Urology. 2017;109:94–100. 10.1016/j.urology.2017.07.043 [DOI] [PubMed] [Google Scholar]
- 8.Down C, Malthouse T, Lobo N, Ali A, Symes A, Coker C. Gender differences in acute stone admissions – should we have a lower threshold for treatment in female patients? BJU Int. 2021;128(6):697–701. 10.1111/bju.15363 [DOI] [PubMed] [Google Scholar]
- 9.Rambachan A, Matulewicz RS, Pilecki M, Kim JYS, Kundu SD. Predictors of readmission following outpatient urological surgery. J Urol. 2014;192(1):183–8. 10.1016/j.juro.2013.12.053 [DOI] [PubMed] [Google Scholar]
- 10.Incidencija i mortalitet od raka u EU-27 zemljama za 2020. godinu. Available from: https://www.hzjz.hr/sluzba-epidemiologija-prevencija-nezaraznih-bolesti/incidencija-i-mortalitet-od-raka-u-eu-27-zemljama-za-2020-godinu/ (in Croatian)
- 11.Arrambide-Herrera JG, Robles-Torres JI, Ocaña-Munguía MA, Romero-Mata R, Gutiérrez-González A, Gómez-Guerra LS. Predictive factors for mortality and intensive care unit admission in patients with emphysematous pyelonephritis: 5-year experience in a tertiary care hospital. Actas Urol Esp. 2022;46(2):98–105. 10.1016/j.acuro.2021.01.007 [DOI] [PubMed] [Google Scholar]
- 12.Azhar RA, Bochner B, Catto J, Goh AC, Kelly J, Patel HD, et al. Enhanced recovery after urological surgery: a contemporary systematic review of outcomes, key elements, and research needs. Eur Urol. 2016;70(1):176–87. 10.1016/j.eururo.2016.02.051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhou J, Peng ZF, Song P, Yang LC, Liu ZH, Shi SK, et al. Enhanced recovery after surgery in transurethral surgery for benign prostatic hyperplasia. Asian J Androl. 2023. October 11;23:356–60. 10.4103/aja202267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Darwish OM, Lutnick E, Dalimov Z, Waisanen KM, Wang D, Houjaij A, et al. Neuraxial vs general anesthesia: 30-day mortality outcomes following transurethral resection of prostate. Urology. 2021;157:274–9. 10.1016/j.urology.2021.06.034 [DOI] [PubMed] [Google Scholar]
- 15.Morlacco A, Motterle G, Zattoni F. The multifaceted long-term effects of the COVID-19 pandemic on urology. Nat Rev Urol. 2020;17(7):365–7. 10.1038/s41585-020-0331-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pak JS, Sayegh CI, Smigelski MB, McKiernan JM, Cooper KL. A urology department’s experience at the epicenter of the COVID-19 pandemic. Urology. 2020;144:4–8. 10.1016/j.urology.2020.06.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chang SS, Cookson MS, Hassan JM, Wells N, Smith JA, Jr. Routine postoperative intensive care monitoring is not necessary after radical cystectomy. J Urol. 2002;167(3):1321–4. 10.1016/S0022-5347(05)65291-3 [DOI] [PubMed] [Google Scholar]
- 18.Isharwal S, Ye W, Wang A, Abraham J, Zabell J, Dong W, et al. Impact of comorbidities on functional recovery from partial nephrectomy. J Urol. 2018;199(6):1433–9. 10.1016/j.juro.2017.12.004 [DOI] [PubMed] [Google Scholar]
- 19.Eisenberg MS, Thompson RH, Frank I, Kim SP, Cotter KJ, Tollefson MK, et al. Long-term renal function outcomes after radical cystectomy. J Urol. 2014;191(3):619–25. 10.1016/j.juro.2013.09.011 [DOI] [PubMed] [Google Scholar]
- 20.Galiabovitch E, Hansen D, Retegan C, McCahy P. Urinary tract stone deaths: data from the Australian and New Zealand Audits of Surgical Mortality. BJU Int. 2020;126(5):604–9. 10.1111/bju.15171 [DOI] [PubMed] [Google Scholar]
- 21.Townsend NT, Robinson TN. Surgical risk and comorbidity in older urologic patients. Clin Geriatr Med. 2015;31(4):591–601. 10.1016/j.cger.2015.06.009 [DOI] [PubMed] [Google Scholar]
- 22.Maddineni U, Worrall EF, Baker EA, Earasi M, Mathieu F, Guruli G. Urologic surgery with multisystem comorbidities: a case report. Am J Case Rep. 2018;19:1047–52. 10.12659/AJCR.909554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zeng G, Zhu W, Lam W, Bayramgil A. Treatment of urinary tract infections in the old and fragile. World J Urol. 2020;38(11):2709–20. 10.1007/s00345-020-03159-2 [DOI] [PubMed] [Google Scholar]
- 24.Bouassida K, Jaidane M, Bouallegue O, Tlili G, Naija H, Mosbah AT. Nosocomial urinary tract infections caused by extended-spectrum beta-lactamase uropathogens: prevalence, pathogens, risk factors, and strategies for infection control. Can Urol Assoc J. 2016;10(3-4):E87–93. 10.5489/cuaj.3223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ramos-Castaneda JA, Ruano-Ravina A, Munoz-Price LS, Toro-Bermúdez R, Ruiz-Londoño D, Segura-Cardona AM, et al. Risk of infection in patients undergoing urologic surgery based on the presence of asymptomatic bacteriuria: a prospective study. Am J Infect Control. 2019;47(12):1474–8. 10.1016/j.ajic.2019.06.024 [DOI] [PubMed] [Google Scholar]
- 26.Joean O, Tahedl D, Flintrop M, Winkler T, Sabau R, Welte T, et al. Clinical and microbiological effects of an antimicrobial stewardship program in urology – a single center before-after study. Antibiotics (Basel). 2022;11(3): 10.3390/antibiotics11030372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Flamiatos JF, Chen Y, Lambert WE, Martinez Acevedo A, Becker TM, Bash JC, et al. Open versus robot-assisted radical cystectomy: 30-day perioperative comparison and predictors for cost-to-patient, complication, and readmission. J Robot Surg. 2019;13(1):129–40. 10.1007/s11701-018-0832-3 [DOI] [PubMed] [Google Scholar]


