SUMMARY
Earthquakes are unpredictable natural disasters accompanied by material damage and many victims. In the case of a person remaining trapped under the collapsed material, the development of crush syndrome can occur. Crush syndrome is the result of traumatic rhabdomyolysis and is present in 2%-15% of all injured persons in an earthquake. It is not easy to recognize, and proper treatment is challenging. Persons who have a clear crush injury and/or have been immobilized for more than four hours should be considered potential victims of crush syndrome. Therefore, knowledge about crush syndrome must be comprehensive and accessible to all parties involved. In this paper, the management of crush syndrome victims, which includes the principles of triage, and medical and logistic principles as well, is presented. Triage principles are presented at the level of triage priorities, places, and diagnoses. Medical principles, crucial for crush syndrome, are presented regarding the duration of compression and time before or after extraction of the patient. Logistic principles provide an overview of the priorities and modes of transport in relation to distance of health institutions, and the importance of management and education associated with crush syndrome. Each country with recognized disasters (natural or man-made) in which crush-related victims are expected, will benefit if the knowledge about triage, medical and logistic principles for crush syndrome is incorporated in their educational programs and regularly updated.
Key words: Crush syndrome, Earthquakes, Emergencies, Risk management, Triage
Introduction
Earthquakes are unpredictable natural disasters followed by significant material damage and potentially a large number of deaths and injuries (1). The earthquake consequences lead to reduced access to health care due to damaged health facilities, roads, and bridges (later causing transport problems) (2). Earthquake morbidity and mortality depend on several factors including the magnitude and intensity of the earthquake, distance of the epicenter from urban centers, preparedness of emergency medical service providers in disaster situations, and good disaster management protocols (3).
In the event of an earthquake, instant death occurs because of extensive injuries including injuries to the brain and spinal cord. The second wave of injuries often includes injuries to the internal organs such as the liver, spleen, subdural hematoma, and pelvic fractures. Subsequent mortality occurs within the first few hours of the event and, according to previous experience, rapid response and treatment can significantly reduce mortality. Additionally, the third wave of mortality follows later, these are the patients who die in the hospital a few days to a week after the event. These are usually due to sepsis, disseminated intravascular coagulation, and multiorgan failure. The earthquake is also accompanied by specific health conditions, crush syndrome being one of them when a person remains trapped under the collapsed material. To triage and treat all these patients, adequate knowledge of proper medical care is needed (4).
First aid in crisis situations is immediate aid provided to any minor or severely injured or sick person. It includes activities to save lives, prevention of worsening the condition or improving recovery, and also psychosocial support for injured and first responders (5, 6).
First aid saves lives before arrival of the professional emergency help; reduces harmful consequences of the crisis event; helps affected individuals save lives; and prevents further incidents. First aid can be provided by well-trained laymen, including other well-trained professionals, e.g., firefighters, police officers and soldiers, members of the Red Cross (5, 7).
Knowledge of first aid in crisis situations includes assessment of injuries and diseases, stopping bleeding by using the method of digital compression, use of compression bandage and ligation (for heavy bleeding in the extremities and in amputating injuries), and placement of immobilization by improvisational or standard means, as well as cardiopulmonary resuscitation (CPR) and/or use of an automatic external defibrillator and emergency oxygen application (7-9).
The most important resuscitation procedures are divided according to priority. Without prior examination, and a visible need for resuscitation, the patient should not be resuscitated. If the patient is unconscious, the severity of her/his condition is determined by the degree of threat to her/his vital functions (7). Resuscitative procedures of emergency include airway management, rapid sequence intubation, needle decompression, tube thoracostomy, central venous catheter placement, intraosseous line placement, pericardiocentesis, emergency department thoracotomy, defibrillator, and transcutaneous pacing. High-quality cardiopulmonary resuscitation (CPR) is the most important lifesaving technique in any kind of emergency and could be performed by trained people. However, untrained people can also perform CPR but they should have some basic knowledge of how to perform it (10). Trained people and professionals should perform CPR according to guidelines for resuscitation of the European Council on Resuscitation from 2015 (11).
The emergency medical service provides first-line medical care to disaster victims and people who require urgent medical care in any other kind of emergency (12).
The most effective approach in disaster risk management is preparedness and improvement of disaster protocol.
Crush Syndrome Management in Earthquakes
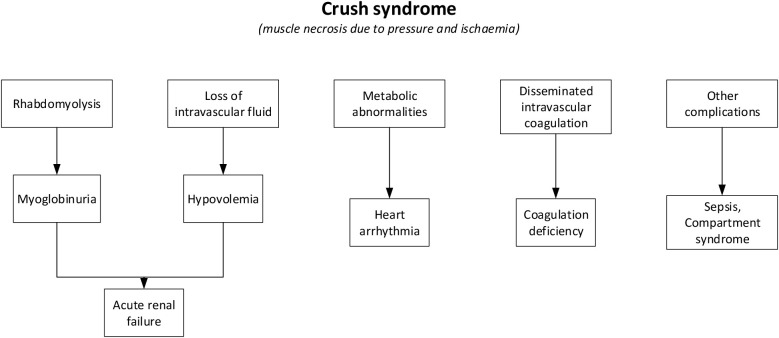
Crush syndrome, one of the most frequent causes of death after earthquakes, is defined as systemic manifestations of muscle crush injury after the direct effect of physical trauma or ischemia reperfusion injury caused by prolonged compression of different parts of the body (13). The major cause of the systemic manifestations is traumatic rhabdomyolysis followed by the release of potentially toxic muscle cell components and electrolytes into the circulatory system (Fig. 1).
Fig. 1.
Pathophysiology of crush syndrome. Source: adapted based on Sever et al. (4) and Nola et al. (7).
Although initially an earthquake victim who has been under the rubble for hours and days may seem stable, he/she can become unstable very soon after being pulled out of the rubble. Once the victim is released from the pressure caused by collapsed material, a reperfusion syndrome may develop as a result of the release of toxic intracellular components from necrotic muscle into the bloodstream. In crush syndrome, early mortality is caused by hypovolemia, cardiac arrhythmia due to metabolic acidosis, and hyperkalemia (18). Further, mortality may occur as a result of renal failure, acute respiratory distress syndrome, disseminated intravascular coagulation, sepsis, and electrolyte disturbances. Thus, understanding the pathophysiology behind the crush syndrome is vital for the appropriate management of injured people (19). The reperfusion syndrome developed after the release of the compressive force is the major cause of rhabdomyolysis. This syndrome is related to swelling in the affected areas and development of muscle necrosis followed by the release of myoglobin and potassium. These processes could lead to kidney damage causing hyperkalemia and possible cardiac arrhythmias. Furthermore, injured muscle cells are taking calcium, which is the cause of hypocalcemia, also contributing to cardiac arrhythmias (20). All these processes are highly dependable on the size of the affected body area and the length of the time the person was trapped (18).
Any victim who has a clear crushing injury and/or has been immobilized for more than four hours should be considered a potential crush syndrome patient (14). According to previous experience, it is estimated that 2%-15% of earthquake victims develop a crush syndrome (15). Although the incidence of crush syndrome has been reported as 2% to 15% in all trauma patients, it can be as high as 30% in earthquake victims (16).
Typically, the most affected areas of the body include lower extremities (74%), upper extremities (10%), and trunk (9%) (17).
If the person is seriously injured, transport to the hospital often arises as the best choice. The order of transport must accord with the urgency status determined in triage. We distinguish the first, second and third order of transport urgency. The first order of urgency of transport refers to persons who are suffocating, and with first aid, suffocation could not be removed; persons who have strong external and internal bleeding, penetrating injuries to the chest, abdomen, and head; and people with crush syndrome and signs of gas gangrene (7).
However, the crush syndrome often represents the most debatable situation since those injuries require specific management but are present only in 2%-5% of all injured people in natural or man-made disasters. Thus, without proper training, they are not easy to recognize, and proper treatment is challenging as well.
How to Choose Proper Approach?
Analyzing records on 19,167 trauma patients in different disasters, researchers found that 84% of the injuries were blunt and 16% were penetrating (21). Their results showed that patients with penetrating trauma had higher odds of mortality if the duration of treatment delivered at the scene exceeded 20 minutes. Otherwise, results showed that longer transport times did not play a role in terms of increased mortality in patients with penetrating trauma. Moreover, the results of the same study showed that patients with blunt trauma had no difference in their survival chances, no matter whether ‘the stay and play or load and go’ decision was made (21).
Still, there are plenty of situations that can go wrong. This is the reason why knowledge about crush syndrome needs to be more comprehensive and available to all involved parties. The required principles of the crush patient management should include the principles of triage, medical principles, and logistics.
Triage principles (adapted based on Haller et al. (22)):
Triage is a process for establishing priorities: for the triage points, for the injured people, and for the transport.
Three triage points – (i) at the scene; (ii) in the treatment resuscitation area; (iii) in the hospital – each of them needs good crush syndrome victims’ management.
Levels of triage – the main principle: “the greatest good for the greatest number” should include well-defined priorities.
Level 1 – occurs at the scene or at the emergency points and must include transport priorities and decisions.
Level 2 – occurs upon arrival at the chosen hospital and could include new decisions on better facilities for specific patients.
At the scene, the most experienced healthcare provider should be responsible for triage management.
Triage categories – to provide a basic algorithm for decision-making in a disaster scenario, based on the International Committee of the Red Cross (23):
-
Category I – Priority for Surgery
Those patients for whom urgent surgery is required and for whom there is a good chance of recovery. In practice, many of these patients will have abdominal injuries.
-
Category II – No Surgery
Those patients who do not require surgery either because their wounds are so slight that they can be managed non-operatively or because their injuries are so severe that they are likely to die or have little chance of survival.
-
Category III – Can Wait for Surgery
Those patients who require surgery but not on an urgent basis.
6. Adequately chosen transport and order of transport based on patient injuries and proximity of health facilities.
Medical principles (adapted based on Sever et al. (19)):
Adequate medical care based on triage categories.
Main medical principle – medical care to all injured people who have a reasonable chance of survival – these are certainly crushed victims.
Recognize crush syndrome – all crush victims should be accepted in the hospital; appropriate fluid compensation may prevent crush-related acute kidney injury (AKI) and prevent the need of dialysis (24).
Start dialysis in crush patients to avoid crush-related AKI, such as developing hyperkalemia – therefore, rapidly increasing serum potassium is the indication(s) for dialysis.
In adult crush victims, intermittent hemodialysis should be the first choice, if medical and logistic assets allow it.
In small children, peritoneal dialysis is the therapy of choice.
-
Efficient clearance of potassium and the possibility of treating several patients on the same machine per day or minimizing/avoiding anticoagulation in bleeding-prone patients will unburden health personnel and/or facilities in risk management and make more chances for patients.
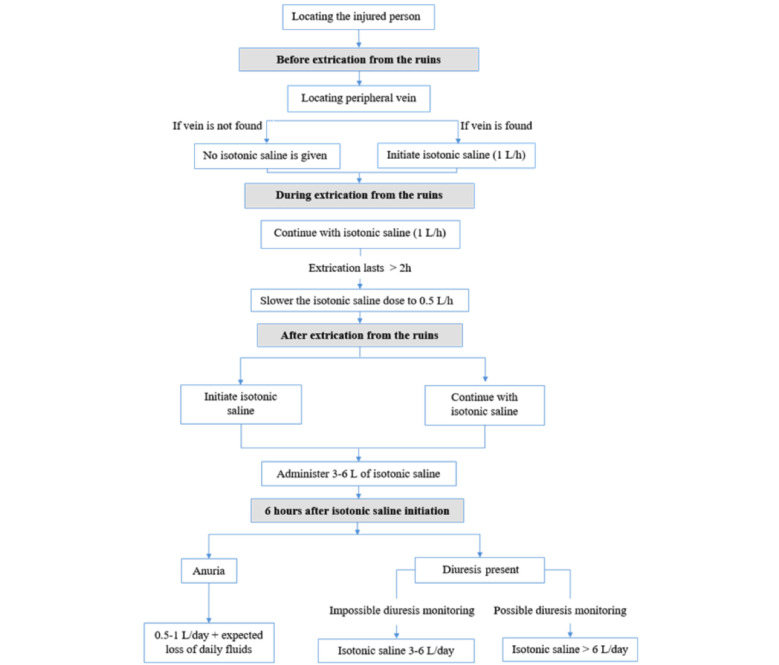
Do not simplify – fluid resuscitation is essential for preventing crush-related AKI, but uniform forceful fluid compensation for all crush victims could be counterproductive (Fig. 2).
Fig. 2.
Algorithm for fluid replacement in adult earthquake casualties before, during and after extrication from the disaster site. Source: adapted based on Sever and Vanholder25 and Nola et al.7.
Several conditions/factors will determine the need of fluid resuscitation, i.e., time of being trapped under the ruins, length of extrication (more than two hours trapped, less than 50% of the initial amount of fluid is needed (25, 26), elderly, children and people with low body mass need less fluid, environmental conditions (low ambient temperature – lower fluid amount), less fluid when hypervolemia and anuria are presented.
Use isotonic saline in crush syndrome – potassium-containing fluids should be avoided because fatal hyperkalemia may occur at any moment, even in the absence of renal failure.
Do not prevent crush syndrome by using an arterial tourniquet – it should be applied only for life-threatening bleeding.
Prolonged application of tourniquets may expose the patient to palsy, myonecrosis, thrombosis, rigor, blisters, abrasions, contusions, and pinching lesions, while a massive amount of myoglobin is liberated upon tourniquet release (27).
Amputation should only be done if it is clearly indicated – if so, then guillotine amputation is the choice.
Use guillotine amputation in emergency situations for contaminated wounds or infection as a quick means of removing diseased or damaged tissue (28).
Fasciotomy should only be done if it is clearly indicated.
Clinical signs: absence of distal pulses, a requirement of radical debridement of necrotic muscle or objective compartmental pressure measurements (intracompartmental pressures >30-40 mm Hg, especially without decrease within 6 hours; or differences between compartmental pressure and diastolic blood pressure <30 mm Hg) are present.
Fasciotomy is a clinical diagnosis! (29)
Treat hypocalcemia in crush victims only when symptoms are present.
In crush victims, deposition of calcium into the traumatized skeletal muscles related to rhabdomyolysis-induced acute renal injury might result in hypocalcemia (30), which carries the risk of tetany, seizures, and cardiotoxicity. However, hypercalcemia might develop later during the recovery phase as well, especially in patients who previously received calcium salts. In such cases, the precipitation of calcium in tissue may trigger cell damage and subsequent complications.
Logistic principles (adapted based on Sever et al. (19)):
Main transport principle – right patients at right time to the right medical facility.
Choose well the medical facilities for transport of injured people – severely injured people showed better recovery when treated in remote hospitals not affected by earthquake (31).
Transport logistics should include available routes checked for accessibility.
Hospitals defined based on proximity to the emergency scene are classified as first, second, or third line – for crush syndrome first-line hospitals (those closest to the scene) should be avoided (32).
The first-line hospitals will be overcrowded with people arriving as walking wounded or by private vehicles, and thus triage and registration of patients will suffer.
Second-line hospitals are the main destinations for those in need of emergency treatment, like crush syndrome patients.
-
Third-line hospitals, those far from the emergency scene, are ideal for patients in triage category III (“Those patients who require surgery but not on an urgent basis”).
Educate inhabitants of areas prone to earthquakes – how to act, to behave, to recognize crush victims (and what to do and not to do with them!).
Educate health personnel on crush syndrome and its victims (the emergency medicine specialists can be very helpful in this education (33)) – especially those who will be in charge of the victims discharged to domestic care – they need proper and clear instructions.
Have a very good plan in disaster protocol for such victims based on known guidelines.
Conclusion
To answer the main question, ‘stay and play or load and go’, adequate knowledge of crush syndrome and its victims is needed. Mainly, crush victims will be the load-and-go victims, especially when their parameters show significant urgency or deterioration. Otherwise, proper on-site victim management enables the stay-and-play solution long enough to organize appropriate transport and to choose an ideal health facility. Emergency management related to the crush syndrome should predict those situations and possible victims in their mitigation and preparedness protocols, and especially in response and recovery. Each country with recognized disasters (natural or man-made) in which crush-related victims are expected will benefit if the knowledge about triage, medical and logistic principles for crush syndrome is incorporated in their educational programs and regularly updated.
References
- 1.Nola IA. Earthquakes and their environmental, medical and public health impacts. Salud Publica Mex. 2018;60:16. 10.21149/9212 [DOI] [Google Scholar]
- 2.Ceferino L, Mitrani-Reiser J, Kiremidjian A, Deierlein G, Bambarén C. Effective plans for hospital system response to earthquake emergencies. Nat Commun. 2020;11: 10.1038/s41467-020-18072-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Earthquakes [Internet]. WHO. [cited 2022 Apr 28]. Available from: https://www.who.int/health-topics/earthquakes
- 4.Sever MS, Vanholder R, Lameire N. Management of crush-related injuries after disasters. N Engl J Med. 2006. March 9;354(10):1052–63. 10.1056/NEJMra054329 [DOI] [PubMed] [Google Scholar]
- 5.International Federation of Red Cross and Red Crescent Societies (IFRC). First aid policy [Internet]. International Federation of Red Cross and Red Crescent Societies. 2007 [cited 2022 May 2]. Available from: https://oldmedia.ifrc.org/ifrc/what-we-do/health/first-aid-policy/
- 6.Centers for Disease Control and Prevention (CDC). Emergency preparedness and response: taking care of your emotional health [Internet]. Centers for Disease Control and Prevention. 2019 [cited 2022 May 2]. Available from: https://emergency.cdc.gov/coping/selfcare.asp
- 7.Nola IA, Pjevač N, Keranović A, Kuliš T. Upravljanje zdravstvenim rizicima u kriznim situacijama. In: Nola IA, editor. Upravljanje zdravstvenim i javnozdravstvenim rizicima u kriznim situacijama. Priručnik za doktorski studij Biomedicina i zdravstvo Medicinskog fakulteta Sveučilišta u Zagrebu. [Health and public health risks management in crisis situations. Manual for PhD study Biomedicine and health, School of Medicine, University of Zagreb]. Zagreb: Medicinski fakultet, Sveučilište u Zagrebu; 2021, p. 49-79. (in Croatian) [Google Scholar]
- 8.Brouhard R. 10 Basic First Aid Procedures: Getting someone through a medical crisis [Internet]. verywell health. 2022 [cited 2022 May 2]. Available from: https://www.verywellhealth.com/basic-first-aid-procedures-1298578
- 9.The Red Cross Society. Comprehensive Guide for First Aid & CPR [Internet]. Canada: The Red Cross Society; 2017. Available from: https://mediprofirstaid.com/first-aid-and-cpr-guide.html
- 10.Mayo Clinic Staff. Cardiopulmonary resuscitation (CPR): First aid [Internet]. Mayo Clinic. 2022 [cited 2022 May 2]. Available from: https://www.mayoclinic.org/first-aid/first-aid-cpr/basics/art-20056600.
- 11.Monsieurs KG, Nolan JP, Bossaert LL, Greif R, Maconochie IK, Nikolaou NI, et al. European Resuscitation Council Guidelines for Resuscitation 2015. Resuscitation. 2015;95:1–80. 10.1016/j.resuscitation.2015.07.038 [DOI] [PubMed] [Google Scholar]
- 12.Beyramijam M, Khankeh HR, Farrokhi M, Ebadi A, Masoumi G, Aminizadeh M. Disaster preparedness among emergency medical service providers: a systematic review protocol. Emerg Med Int. 2020;2020:6102940. 10.1155/2020/6102940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sever MS, Vanholder R. Management of crush syndrome casualties after disasters. Rambam Maimonides Med J. 2011;2(2):e0039. 10.5041/RMMJ.10039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.EMS1. 4 things EMS providers must know about crush syndrome [Internet]. EMS1 2010 [cited 2022 Apr 27]. Available from: https://www.ems1.com/patient-handling/articles/4-things-ems-providers-must-know-about-crush-syndrome-iGLMvsYAEi0JZael/
- 15.Centers for Disease Control and Prevention (CDC). After an earthquake; management of crush injuries & crush syndrome. Atlanta (USA): Center for Disease Control and Prevention; Jan 14, 2010 [cited 2022 Apr 28]. Available from: https://stacks.cdc.gov/view/cdc/11904
- 16.Li W, Qian J, Liu X, Zhang Q, Wang L, Chen D, et al. Management of severe crush injury in a front-line tent ICU after 2008 Wenchuan earthquake in China: an experience with 32 cases. Crit Care. 2009;13:R178. 10.1186/cc8160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Briggs SM. Earthquakes. Surg Clin North Am. 2006. June;86(3):537–44. 10.1016/j.suc.2006.02.003 [DOI] [PubMed] [Google Scholar]
- 18.Gonzalez D. Crush syndrome. Crit Care Med. 2005. January;33(1) Suppl:S34–41. 10.1097/01.CCM.0000151065.13564.6F [DOI] [PubMed] [Google Scholar]
- 19.Sever MS, Vanholder R. Workgroup on Recommendations for the Management of Crush Victims in Mass Disasters. Recommendations for the management of crush victims in mass disasters. Nephrol Dial Transplant. 2012;27 Suppl 1:i1–67. 10.1093/ndt/gfs156 [DOI] [PubMed] [Google Scholar]
- 20.Walters T, Powell D, Penny A, Stewart MI, Chung K, Keenan S, et al. Crush syndrome – prolonged field care (CPG ID: 58) [Internet]. Army.mil. 2016 [cited 2022 Apr 27]. Available from: https://jts.amedd.army.mil/assets/docs/cpgs/Crush_Syndrome_PFC_28_Dec_2016_ID58.pdf [DOI] [PubMed]
- 21.McCoy CE, Menchine M, Sampson S, Anderson C, Kahn C. Emergency medical services out-of-hospital scene and transport times and their association with mortality in trauma patients presenting to an urban level I trauma center. Ann Emerg Med. 2013;61(2):167–74. [Internet] 10.1016/j.annemergmed.2012.08.026 [DOI] [PubMed] [Google Scholar]
- 22.Haller HL, Wurzer P, Peterlik C, Gabriel C, Cancio LC. Burn management in disasters and humanitarian crises. In: Herndon DN, editor. Total Burn Care, 5th edn. Elsevier; 2018. p. 36-49. [Google Scholar]
- 23.Kyazze AB. Walking the walk: Evidence of principles in action from Red Cross and Red Crescent National Societies. Int Rev Red Cross. 2015;97(897-898):211–33. [Internet] 10.1017/S1816383115000582 [DOI] [Google Scholar]
- 24.Zhou XL, Ni SZ, Xiong D, Cheng XQ, Xu P, Zhao Y. Fluid resuscitation with preventive peritoneal dialysis attenuates crush injury-related acute kidney injury and improves survival outcome. Scand J Trauma Resusc Emerg Med. 2019;27(1):68. 10.1186/s13049-019-0644-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sever MS, Vanholder R. Management of crush victims in mass disasters: highlights from recently published recommendations. Clin J Am Soc Nephrol. 2013;8:328–35. 10.2215/CJN.07340712 [DOI] [PubMed] [Google Scholar]
- 26.Vanholder R, Sever MS. Crush-related acute kidney injury [Internet]. UpToDate. 2021 [cited 2022 Apr 27]. Available from: https://www.uptodate.com/contents/crush-related-acute-kidney-injury?search=Crush%20injury&source=search_result&selectedTitle=2~121&usage_type=default&display_rank=2#references
- 27.Kragh JF, Jr, Walters TJ, Baer DG, Fox CJ, Wade CE, Salinas J, et al. Practical use of emergency tourniquets to stop bleeding in major limb trauma. J Trauma. 2008. February;64(2) Suppl:S38–49, discussion S49–50. 10.1097/TA.0b013e31816086b1 [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization (WHO). Best practice guidelines on emergency surgical care in disaster situations [Internet]. World Health Organization; 2007 [cited 2022 Apr 27]. Available from: https://www.who.int/publications/i/item/best-practice-guidelines-on-emergency-surgical-care-in-disaster-situations
- 29.Lee P. Crush syndrome and fasciotomy [Internet]. The Royal College of Surgeons of Edinburgh. 2020 [cited 2022 Apr 27]. Available from: https://www.rcsed.ac.uk/professional-support-development-resources/learning-resources/webinars/rsa-webinar-series-for-medical-undergraduates/crush-syndrome-and-fasciotomy
- 30.Llach F, Felsenfeld AJ, Haussler MR. The pathophysiology of altered calcium metabolism in rhabdomyolysis-induced acute renal failure. Interactions of parathyroid hormone, 25-hydroxycholecalciferol, and 1,25-dihydroxycholecalciferol. N Engl J Med. 1981;305(3):117–23. 10.1056/NEJM198107163050301 [DOI] [PubMed] [Google Scholar]
- 31.McConnell KJ, Newgard CD, Mullins RJ, Arthur M, Hedges JR. Mortality benefit of transfer to level I versus level II trauma centers for head-injured patients. Health Serv Res. 2005;40(2):435–57. 10.1111/j.1475-6773.2005.0u367.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Greaves I, Porter K, Smith J. Consensus statement on crush injury and crush syndrome. Trauma. 2002;4(3):129–34. 10.1191/1460408602ta228oa [DOI] [Google Scholar]
- 33.Sorić M, Špoljar D, Golubić M. Effect of the introduction of emergency medicine specialists on the emergency department performance indicators: a retrospective data analysis. Acta Clin Croat. 2022;61 Suppl 1:9–13. 10.20471/acc.2022.61.s1.01 [DOI] [PMC free article] [PubMed] [Google Scholar]