SUMMARY
Urolithiasis is a rare urologic complication after kidney transplantation, and its diagnosis and treatment can be challenging for clinicians. In our 52-year-old male patient, graft hydronephrosis was found six months after transplantation. The patient had recurrent urinary tract infections followed by macrohematuria and an increase in creatinine levels. Computerized tomography revealed a 13-mm diameter stone in the ureter of the transplanted kidney as the cause of obstruction. Percutaneous nephrostomy was placed in the graft to solve the obstruction. Initial endoscopic treatment with a retrograde approach failed. An antegrade approach through a previously placed nephrostomy was not successful either. By a repeated retrograde approach, laser lithotripsy was performed successfully. The patient has been monitored for six months and has stable graft function without hydronephrosis or stones. As in our patient’s case, the diagnosis and treatment of urolithiasis in kidney transplant patients is challenging, and minimally invasive procedures are the treatment of choice.
Key words: Kidney transplantation, Ureterolithiasis, Ureteroscopy, Laser lithotripsy
Introduction
Kidney transplantation is the most preferred treatment for patients with end-stage renal disease (1). It has proven to be the most effective method of replacing renal function, as it significantly prolongs survival and improves the quality of life. One of the rare postoperative urologic complications is urolithiasis, and its incidence is less than 1% (2). Due to the lack of specific symptoms resulting from denervation of the kidneys and ureters, urolithiasis in these patients is most often manifested by painless macrohematuria, decreased diuresis, unexplained fever, and elevated creatinine levels (3). Recognition, as well as treatment of graft urolithiasis is a challenge for clinicians, and given that these are immunosuppressed patients, rapid diagnosis and treatment are crucial to prevent transplant loss. This case report presents a male patient with urolithiasis detected six months after kidney transplantation, who was treated with different therapeutic modalities.
Case Report
The patient was a 52-year-old man who had undergone cadaveric kidney transplantation in 2020. He was born with severe bilateral vesicoureteral reflux along with renal impairment. When the patient was two months old, he underwent right-sided nephroureterectomy due to an extremely dilated right ureter and kidney with urosepsis. In the following years, two antireflux operations were performed on the left ureterovesical junction, but both failed, and left-sided ureterocutaneostomy was constructed. In 1972, stoma closure was performed with ureteral reconstruction using large bowel (ureterocolocystoplasty). Over years, there was a gradual decline in renal function, and in 2020, he began hemodialytic treatment. In the same year, he underwent cadaveric kidney transplantation in the right iliac fossa, and his early postoperative clinical course was eventless. Six months post-transplantation, ultrasound revealed mild graft hydronephrosis with an elevated creatinine level of 127 µmol/L (normal range: 64-104 µmol/L). Over the next few months, the patient had recurrent urinary tract infections followed by macrohematuria, and creatinine levels increased to 149 µmol/L. Hydronephrosis was still present on ultrasound, while the urethrocystoscopic finding was normal. Renal scintigraphy revealed dilatation of the renal calyces, renal pelvis and ureter, and a 15% decrease was observed in creatinine clearance. Drainage was significantly worse and was only partially improved by diuretics. The patient underwent anterograde pyeloureterography, and a presumptive diagnosis of stenosis of the ureterovesical anastomosis was established (Fig. 1). The defect of contrast filling was interpreted as an air bubble. However, computerized tomography urography demonstrated a 13-mm diameter stone in the distal part of the ureter of the transplanted kidney as the cause of obstruction (Figs. 2 and 3). Due to the existing obstruction, the patient underwent percutaneous nephrostomy in the graft.
Fig. 1.

Antegrade pyeloureterography demonstrating a visible defect of contrast filling (horizontal arrow) and narrowing in the distal part of the ureter (vertical arrow).
Fig. 2.

Axial computerized tomography of the pelvis demonstrating a stone in the right ureter.
Fig. 3.
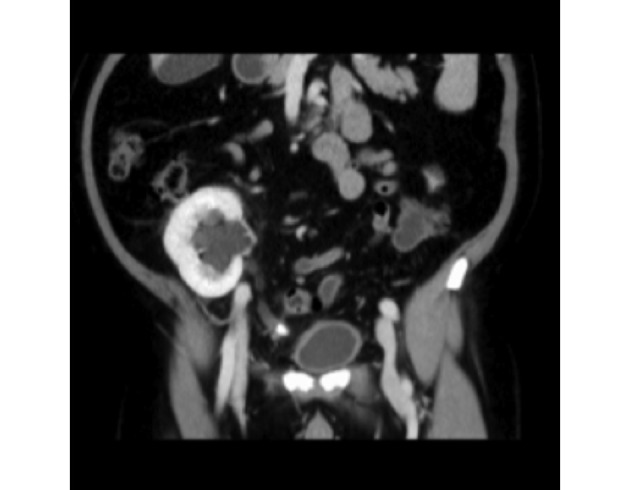
Coronal computerized tomography urography demonstrating a stone in the distal part of the ureter of the transplanted kidney.
Since the stone was in the prevesical position, a retrograde approach was chosen. The ureteral orifice was found only after applying methylene blue through nephrostomy, and the entrance to the ureter was difficult to cannulate because of the unfavorable angle. After entering the ureter, the stone was located and caught in a Dormia wire basket. However, during removal, it was expelled from the basket at the ureterovesical anastomosis and remained in the ureter. Re-entry into the ureteral orifice was no longer possible, primarily due to bleeding and new-onset edema. Approximately one month after the retrograde approach, the antegrade approach was attempted. We used a previously placed nephrostomy for access. A guidewire was placed through it into the renal cavitary system, and after the channel size was expanded, the 12 Ch sheath was inserted, and the renal cavity system was entered with a flexible ureteroscope (antegrade approach). A flexible ureteroscope was used to enter the ureter, but because of anatomic variation of the ureter, it was not possible to reach the stone or place the ureteral double-J stent. Approximately two months later, we managed to enter the ureter again with a retrograde approach. The entering was also challenging but successful, and the stone was located in the distal part of the ureter. The stone was fully disintegrated using holmium-yttrium aluminum garnet (Ho-YAG) laser lithotripsy, after which a double-J stent was placed. Two months after successful lithotripsy, the double-J stent was removed. The patient has been monitored for six months and has stable graft function with no hydronephrosis or urolithiasis.
Discussion
Allograft lithiasis after renal transplantation can either be the result of de novo lithiasis formation or can be donor-gifted (3). Recipients are predisposed to developing graft urolithiasis because of a unique combination of metabolic and urodynamic factors. Secondary vesicoureteral reflux, ureteral stricture or obstruction, and residual foreign bodies (nonabsorbable suture material) promote the development of stones (3). Also, kidney stones were shown to be associated with recurrent urogenital tract infections, especially if they are caused by urease-positive pathogens such as Proteus mirabilis (4). Renal tubular acidosis and tertiary hyperparathyroidism are common findings among kidney transplant recipients and lead to the development of hypercalciuria and hypocitraturia, while the use of calcineurin inhibitors (cyclosporine and tacrolimus) has been associated with the development of hyperuricosuria (5). In addition, increased protein intake, calcium, and vitamin D have potential lithogenic effects (3). Sometimes stones can be detected in a donor before transplantation, during organ assessment. Previously, such candidates were not considered suitable for transplantation due to the potential complications related to the calculus or the treatment procedure (6). Advancement of endourologic techniques, along with expansion of the pre-transplant donor assessment, has relaxed restrictions in this regard (7). Ex vivo treatment (most frequently ureteroscopy [URS] and pyelolithotomy) is performed immediately after nephrectomy and before graft transfer. In 2017, Machen et al. described a series of four patients, recipients of cadaveric kidney transplants, who underwent ex vivo ureteroscopy with successful removal of the calculus (7). According to a systematic analysis conducted by Longo et al., the success rate (stone-free rate [SFR]) of ex vivo surgery was 95.8% (8). Due to the low risk of morbidity and high success rate, ex vivo ureteroscopy is recommended as the first-choice treatment for urolithiasis in kidney grafts from living donors (3). Although calculus was not detected during the donor assessment, we believe that allograft lithiasis in our patient was donor-gifted. Therefore, ex vivo treatment was not an option.
In general, there are no differences in the treatment of urolithiasis in native kidneys and transplanted kidneys. However, the endoscopic approach in the treatment of graft ureteral stones is a technically demanding method due to the extra-anatomic position of the transplanted kidney and ectopy of the ureterovesical junction (5). The existence of other comorbidities, such as ureterocolocystoplasty in this patient, may further complicate treatment. According to the guidelines of the European Urological Association, extracorporeal shock wave lithotripsy (ESWL) is considered the first choice for the treatment of stones <15 mm. URS, including the antegrade and retrograde approaches, may be considered for stones <20 mm, while percutaneous nephrolithotomy (PCNL) is most suitable for larger stones (>20 mm) (9). PCNL is used for the treatment of kidney and proximal ureteral stones, and the advantage over open surgery is lower morbidity and mortality with high efficacy (10). In transplant patients, this method is quite simple, considering the location of the graft below the muscles of the anterior abdominal wall and the small distance from the skin to the kidneys (11). According to a study conducted by Duty et al., the success rate (SFR) of stone elimination using this method was 88.5%, with only three reported complications (postoperative sepsis, gastrointestinal bleeding, and herpes esophagitis) (5). An important issue for transplant patients is the extent of kidney damage because standard operative sheaths are 26-32 Ch in diameter. Therefore, the standard PCNL technique has been modified and is currently performed with a miniature endoscope (11-20 Ch) through a small percutaneous tract (11). ESWL is another effective method of treating symptomatic kidney stones, as well as stones in the proximal part of the ureter. The basic preconditions for the implementation of ESWL are determination of morphology and function of the urogenital system and visualization of calculus by diascopy or ultrasonography (12). The graft is placed below the abdominal wall, so ultrasound localization of kidney stones is simpler than with stones in the ureter. Targeting urinary stones, especially those in the distal part of the ureter, can be difficult in a kidney transplant recipient. However, for ureteral stones near the graft, the kidney serves as a good acoustic window, and the dilated ureter simplifies finding stones (13). SFR is between 87% and 100%, but it is often necessary to repeat the procedure until the stones are completely removed. Additionally, close monitoring is mandatory in patients without stents due to the risk of ureteral obstruction during fragment passage (5). In our patient, calculus was not visible on diascopy or ultrasound; therefore, ESWL was not the method of choice.
Ureteroscopy is a minimally invasive method used to diagnose and treat diseases of the ureter and accessible parts of the pelvicalyceal system. It is most often used in the treatment of ureterolithiasis (14, 15). There are two endoscopic approaches to the ureter, antegrade and retrograde (16). When considering the antegrade endoscopic approach, the challenge is the proximity of the bowel located above the transplanted kidney, the arrangement of the hilar structures, and the position of the ureter. In addition to the risk of intestinal perforation or bleeding from adjacent iliac vessels, this technique can be demanding. Fibrous perirenal reactive tissue, formed after transplantation, significantly complicates tract dilatation and nephroscope maneuvering (17). The retrograde approach involves entering the urethra and bladder with a ureteroscope through the ureterovesical orifice into the ureter. Using a natural urinary opening to enter the ureter minimizes the risk of major complications, so a retrograde approach is often the first method of choice. The main difficulties of this endoscopic approach are finding the ureteral orifice and conducting the ureteroscope through the intramural part of the ureter (18). The site of the ureterovesical anastomosis may be on the bladder dome, anterior wall, or high on the posterior bladder wall, and therefore access can be very difficult and often unsuccessful (19). The use of methylene blue, as in our patient, could be helpful in the detection of the ureteral orifice. Furthermore, the absence of natural connective tissue poses a risk of ureteral injury when performing ureteroscopy. This risk can be reduced by inserting a ureteroscope over the guidewire, which provides support for the allograft ureter (20). Regarding the efficiency of the URS in kidney transplant patients, the SFR is 78% (5).
Although antegrade endoscopy is a more successful treatment method than retrograde (21), in our patient, both the retrograde and the antegrade approaches initially did not yield desired results. Endoscopic treatment with the retrograde approach is complicated by the inability to find the ureteral orifice. In addition to ectopy as a consequence of transplantation, finding the ureterovesical orifice in our patient was further complicated by previously performed ureterocolocystoplasty. In transplant patients with urinary diversion or bladder augmentation, the bladder wall is changed and contains mucosal folds, so the passage through the ureterovesical anastomosis becomes a potential problem (22). Additionally, re-entering the ureter, as in our patient, is frequently difficult. The antegrade approach was complicated by the anatomic position of the ureter and the sharp pyeloureteral angle, so extraction of the calculus in this way was not possible. Finally, the stone was successfully extracted only after repeating the retrograde procedure.
Conclusion
Urolithiasis is a rare urologic complication after kidney transplantation. For clinicians, it represents a challenge for diagnosis and treatment, especially due to the extra-anatomic position of the transplanted kidney and the ectopy of the ureterovesical junction. However, minimally invasive endoscopic methods with either antegrade or retrograde approaches combined with lithotripsy can give excellent results.
References
- 1.Orlić L, Jelić Pranjić I. Kidney transplantation in the elderly. Med Flum. 2020;56(4):504–12. [in Croatian] [Google Scholar]
- 2.Rahelić D, Sotošek S, Galić J, Fučkar Ž. Urolitijaza. In: Fučkar Ž, Španjol J, editors. Urologija II. (specijalni dio). 2nd edn. Rijeka: School of Medicine, University of Rijeka, 2013;289-330. (in Croatian) [Google Scholar]
- 3.Sarier M, Yayar O, Yavuz A, Turgut H, Kukul E. Update on the management of urological problems following kidney transplantation. Urol Int. 2021;105(7-8):541–7. 10.1159/000512885 [DOI] [PubMed] [Google Scholar]
- 4.Harraz AM, Kamal AI, Shokeir AA. Urolithiasis in renal transplant donors and recipients: an update. Int J Surg. 2016;36:693–7. 10.1016/j.ijsu.2016.11.032 [DOI] [PubMed] [Google Scholar]
- 5.Duty BD, Conlin MJ, Fuchs EF, Barry JM. The current role of endourologic management of renal transplantation complications. Adv Urol. 2013;2013:246520. 10.1155/2013/246520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Olsburgh J, Thomas K, Wong K, Bultitude M, Glass J, Rottenberg G, et al. Incidental renal stones in potential live kidney donors: prevalence, assessment and donation, including role of ex vivo ureteroscopy. BJU Int. 2013;111(5):784–92. 10.1111/j.1464-410X.2012.11572.x [DOI] [PubMed] [Google Scholar]
- 7.Machen GL, Milburn PA, Lowry PS, Lappin JA, Doherty DK, El Tayeb MM. Ex-vivo ureteroscopy of deceased donor kidneys. Can Urol Assoc J. 2017;11(8):251–3. 10.5489/cuaj.4327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Longo N, Calogero A, Creta M, Celentano G, Napolitano L, Capece M, et al. Outcomes of renal stone surgery performed either as predonation or ex vivo bench procedure in renal grafts from living donors: a systematic review. Biomed Res Int. 2020 27;2020:6625882. DOI: 10.1155/2020/6625882 10.1155/2020/6625882 [DOI] [PMC free article] [PubMed] [Retracted]
- 9.Guidelines EAU. European Association of Urology – Annual Congress Amsterdam 2022. ISBN 978-94-92671-16-5 [Google Scholar]
- 10.Ahel J, Sotošek S, Rubinić N, Markić D. Mini percutaneous nephrolithotripsy as treatment modality for kidney stones. Med Flum. 2017;53(3):371–5. [in Croatian] 10.21860/medflum2017_182949 [DOI] [Google Scholar]
- 11.Markić D, Krpina K, Ahel J, Gršković A, Španjol J, Rubinić N, et al. Treatment of kidney stone in a kidney-transplanted patient with mini-percutaneous laser lithotripsy: a case report. Case Rep Nephrol Dial. 2016;6(1):26–31. 10.1159/000444251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sotošek S, Ahel J, Rubinić N, Smolić K, Markić D. Extracorporeal shock wave lithotripsy. Med Flum. 2017;53(3):285–91. [in Croatian] 10.21860/medflum2017_182971 [DOI] [Google Scholar]
- 13.Markić D, Valenčić M, Gršković A, Španjol J, Sotošek S, Fučkar Ž, et al. Extracorporeal shockwave lithotripsy of ureteral stone in a patient with en bloc kidney transplantation: a case report. Transplant Proc. 2011;43(5):2110–2. 10.1016/j.transproceed.2011.03.031 [DOI] [PubMed] [Google Scholar]
- 14.Geavlete P, Jecu M, Geavlete B, Multescu R, Nita G, Georgescu D. Ureteroscopy – an essential modern approach in upper urinary tract diagnosis and treatment. J Med Life. 2010;3(2):193–9. [PMC free article] [PubMed] [Google Scholar]
- 15.Yang C, Li S, Cui Y. Comparison of YAG laser lithotripsy and extracorporeal shock wave lithotripsy in treatment of ureteral calculi: a meta-analysis. Urol Int. 2017;98(4):373–81. 10.1159/000452610 [DOI] [PubMed] [Google Scholar]
- 16.Wolf JS, Jr. Treatment selection and outcomes: ureteral calculi. Urol Clin North Am. 2007;34(3):421–30. 10.1016/j.ucl.2007.04.010 [DOI] [PubMed] [Google Scholar]
- 17.O’Kelly J, Quinlan MR, Jack GS, O’Neill DC, McGrath A, Davis NF. Antegrade and retrograde endoscopic approaches for managing obstructing ureteral calculi in renal transplant patients: an illustrative case series. J Endourol Case Rep. 2020;6(4):348–52. 10.1089/cren.2020.0063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Basiri A, Simforoosh N, Nikoobakht M, Hosseini Moghaddam MM. The role of ureteroscopy in the treatment of renal transplantation complications. Urol J. 2004;1(1):27–31. [PubMed] [Google Scholar]
- 19.Sevinc C, Balaban M, Ozkaptan O, Karadeniz T. Flexible ureterorenoscopy and laser lithotripsy for the treatment of allograft kidney lithiasis. Transplant Proc. 2015;47(6):1766–71. 10.1016/j.transproceed.2015.06.020 [DOI] [PubMed] [Google Scholar]
- 20.McAlpine K, Leveridge MJ, Beiko D. Outpatient percutaneous nephrolithotomy in a renal transplant patient: world’s first case. Can Urol Assoc J. 2015;9(5-6):E324–8. 10.5489/cuaj.2414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sfoungaristos S, Mykoniatis I, Isid A, Gofrit ON, Rosenberg S, Hidas G, et al. Retrograde versus antegrade approach for the management of large proximal ureteral stones. BioMed Res Int. 2016;2016:6521461. 10.1155/2016/6521461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schrier BP, Laguna MP, van der Pal F, Isorna S, Witjes JA. Comparison of orthotopic sigmoid and ileal neobladders: continence and urodynamic parameters. Eur Urol. 2005;47(5):679–85. 10.1016/j.eururo.2004.10.018 [DOI] [PubMed] [Google Scholar]


