Abstract
Background
Lumbar disc herniation (LDH) is a common condition that can be characterized with disabling pain. While most patients recover without surgery, some still require operative intervention. The epidemiology and trends of laminotomy for LDH have not been recently studied, and current practice patterns might be different from historical norms. This study aimed to investigate the trends of inpatient and outpatient laminotomies for LDH and compare complication rates between these two sites of service.
Methods
A large, national database was utilized to identify patients 8 years old who underwent a laminotomy for LDH between 2009 and 2019. Two cohorts were created based on site of surgery: inpatient versus outpatient. The outpatient cohort was defined as patients who had a length of stay less than 1 day without any associated hospitalization. Epidemiologic analyses for these cohorts were performed by demographics. Patients in both groups were then 1:1 propensity-score matched based on age, sex, insurance type, geographic region, and comorbidities. Ninety-day postoperative complications were compared between cohorts utilizing multivariate logistic regressions.
Results
The average incidence of laminotomy for LDH was 13.0 per 10,000 persons-years. Although the national trend in incidence had not changed from 2009 to 2019, the proportion of outpatient laminotomies significantly increased in this time period (p=.02). Outpatient laminotomies were more common among younger and healthier patients. Patients with inpatient laminotomies had significantly higher rates of surgical site infections (odds ratio [OR] 1.61, p<.001), venous thromboembolism (VTE) (OR 1.96, p<.001), hematoma (OR 1.71, p<.001), urinary tract infections (OR 1.41, p<.001), and acute kidney injuries (OR 1.75, p=.001), even when controlling for selected confounders.
Conclusions
Our study demonstrated an increasing trend in the performance of laminotomy for LDH toward the outpatient setting. Even when controlling for certain confounders, patients requiring inpatient procedures had higher rates of postoperative complications. This study highlights the importance of carefully evaluating the advantages and disadvantages of performing these procedures in an outpatient versus inpatient setting.
Keywords: Laminotomy, Lumbar disc herniation, Epidemiology, Postoperative complications, Inpatient surgery, Outpatient surgery, Lumbar spine surgery
Introduction
As the national life expectancy continues to rise, the incidence of degenerative spine disease has also increased [1]. Lumbar disc herniation (LDH) is a common source of back and leg pain among adults, with an incidence ranging from 5 to 20 cases per 1000 adults annually [[2], [3], [4], [5]]. The prevalence of herniated lumbar discs has a male-to-female ratio of 2:1 and is most common between patients 25 to 55 years of age [6,7]. Disc herniation is the displacement of the nucleus pulposus or annulus fibrosis through the intervertebral disc space [8]. Ninety-five percent of disc herniations occur at the L4–L5 or L5–S1 levels [11]. This displacement can cause nerve root compression, leading to radicular pain, numbness, and weakness in the areas supplied by the nerve root [6,9,10].
While most LDHs resolve spontaneously, one surgical intervention that has proven effective for refractory LDH is a laminotomy with discectomy [6,12,13]. The benefits of a laminotomy include short procedure times, minimal blood loss, and a low risk of epidural scarring and cord trauma [12]. However, there have been no recent studies examining national trends in the utilization of laminotomies for LDH nor have there been any recent comparisons by the location of surgery (inpatient versus outpatient).
Recent literature has reported an increased shift to performing various spinal surgeries, including cervical and lumbar fusions, to an outpatient setting [14,17]. This is in large part due to cost reduction and decreased perioperative morbidity relative to inpatient surgery [15]. Clinical practice of surgically managing LDH in the United States (U.S.) might have also changed with the increasing utilization of outpatient surgery. Historical data have primarily focused on laminotomies for LDH in the inpatient setting [16], with relatively few studies examining the incidence and complication rates for these procedures within an outpatient setting [25,36]. Therefore, with the recent shift toward outpatient spinal surgeries, current patterns for laminotomy may have evolved from historical norms.
In order to fill these gaps of knowledge, this study aimed to characterize the national volume of laminotomy for LDH between the inpatient and outpatient settings. We also sought to compare patient demographics and complication rates between inpatient and outpatient laminotomies for LDH. With this study, we hope to better understand current trends in the utilization of laminotomy for LDH in order to provide greater insights toward improving value-based care.
Methods
Data source
As this was a retrospective cohort review of a national, de-identified database, institutional review board (IRB) approval was not necessary. Patients were identified from the IBM MarketScan® Commercial Claims and Encounters and Medicare Supplemental and Coordination of Benefit databases (Ann Arbor, Michigan). The database is a collection of medical insurance claims databases from over 300 employer-sponsored and Medicare supplemental plans, containing more than 240 million de-identified patient records. The database provides information on inpatient admissions, outpatient visits, and pharmaceutical encounters. This database was selected as it is one of the largest administrative claims databases and allows for longitudinal follow-up of continuously enrolled patients.
Patient selection
The database was queried for patients aged > 18 years who underwent a laminotomy between January 1, 2009 and December 31, 2019, as defined by the Current Procedural Terminology (CPT) code "63030" (laminotomy [hemilaminectomy], with decompression of nerve root(s), including partial facetectomy, foraminotomy and/or excision of herniated intervertebral disc; 1 interspace, lumbar). Patients who underwent this procedure were filtered for a diagnosis of lumbar disc herniation as defined by International Classification of Diseases (ICD) diagnostic codes, both the ninth (ICD-9) and tenth (ICD-10) editions. This included the ICD-9 code "72210" (displacement of lumbar intervertebral disc without myelopathy), and ICD-10 codes "M5126" (other intervertebral disc displacement, lumbar region) and "M5127" (other intervertebral disc displacement, lumbosacral region). Patients who had a diagnostic code for cauda equina syndrome at the time of surgery were also excluded from the study (ICD-9 codes "3446," "34460," "34461," and ICD-10 code "G834").
In order to maintain uniformity in the study population, patients who underwent multiple-level laminotomies were excluded from the study. This was done by removing patients that had the CPT code "63035" on the same day (laminotomy [hemilaminectomy], with decompression of nerve root(s), including partial facetectomy, foraminotomy and/or excision of herniated intervertebral disc; each additional interspace, cervical or lumbar). Furthermore, patients who received other concurrent spinal surgical procedures were removed from the study population.
Patients were then classified into two groups based on the site of surgery: inpatient versus outpatient. The inpatient cohort was defined as patients with an associated admission and length of stay (LOS) recorded in the database >=1 day. The outpatient cohort was defined as patients who had a LOS=0 in the database and did not have an associated admission or hospitalization. Patients who had a laminotomy performed in an ambulatory surgery center or other facilities with unrecorded LOS were grouped into a third cohort titled “other.” This cohort was used in calculating total incidences but was not utilized in comparing complication rates after surgery. Patients who were not continuously enrolled in the database for at least 6 months before surgery and 3 months after surgery were also excluded.
Study variables and outcomes
Patient demographic information was collected from the database. Comorbidity status was captured using the Charlson Comorbidity Index (CCI). The CCI is a comorbidity measurement tool that is widely utilized to measure burden of disease, which includes comorbidities such as myocardial infarction (MI), congestive heart failure (CHF), cerebrovascular disease, chronic pulmonary disease, diabetes, chronic kidney disease (CKD), liver disease, malignancy, etc [35]. Additional comorbidities collected included obesity, smoking history, coronary artery disease (CAD), hypertension (HTN), hyperlipidemia (HLD), chronic alcohol use, depression, anxiety, atrial fibrillation, and chronic hypercoagulable state. A chronic hypercoagulable state was defined as patients with a diagnosis of protein C or S deficiency, Factor V Leiden, antiphospholipid antibody, lupus anticoagulant, or other thrombophilia.
Longitudinal tracking within the database allowed us to identify 90-day postoperative complications including dural tear, superficial surgical site infection (SSI), sepsis, nerve injury, venous thromboembolism (VTE), wound dehiscence, hematoma, urinary tract infection (UTI), acute kidney injury (AKI), atrial fibrillation, and neurogenic urinary retention. The corresponding ICD-9/10 diagnoses used to define these diagnoses can be found in Appendix A and Appendix B. Patients were also queried for 90-day all-cause hospital readmissions after surgery, or if they underwent a revision laminotomy procedure within 90 days. Revision procedures were identified by the CPT code "63042" (laminotomy [hemilaminectomy], with decompression of nerve root(s), including partial facetectomy, foraminotomy and/or excision of herniated intervertebral disc, reexploration, single interspace). Complications that were identified were ensured to be within the 90-day period after the associated surgery date, and any complications captured before surgery or after the 90-day period were not included in the study.
Statistical analyses
Patients in the unmatched inpatient and outpatient laminotomy groups were propensity-score matched in a 1:1 ratio based on age, sex, geographic region of surgery (Northeast, North Central South, West), insurance status, and CCI score. Descriptive statistics were generated based on demographics and comorbidity status between unmatched and matched cohorts. Chi-squared tests were used to determine differences in categorical variables, Student's t-tests were used to analyze differences in continuous variables, and Wilcoxon signed ranked tests were utilized for ordinal variables, as indicated.
Epidemiological analyses were performed utilizing the pre-matched population. Annual incidence rates of laminotomy for the treatment of LDH as well as for the treatment of all indications (including LDH), were separately calculated. Annual incidence rates were also broken down by site of service and trended annually. Linear regression was utilized to analyze changes in incidence over time. Represented as per 10,000 database population, annual incidence was defined as the quotient of procedural volumes and the respective total population of continuously enrolled patients for that calendar year within the database. Subsequently, the proportions of inpatient and outpatient laminotomies for LDH were compared over time. Incidence of laminotomies for LDH was also analyzed by age- and sex- strata (age-strata as defined by the database: 18–34 years, 35–44 years, 45–54 years, 55–64 years, 65+ years).
Finally, utilizing the matched cohort, 90-day complication rates were first compared between inpatient and outpatient laminotomies for LDH utilizing univariate analyses with Student's t-tests. Multivariate logistic regressions were then performed within the matched cohorts, controlling again for age, sex, insurance status, geographic region of surgery, and previously defined comorbidities. Statistical significance was defined as p<.05 for all analyses except for analyses of complications, in which Bonferroni corrections were applied to mitigate type 1 errors. In this case, statistical significance was defined as p<.05/13, in which 13 represented the number of comparisons. All statistical analyses were conducted using R-Studio (PBC, Boston, Massachusetts).
Results
A total of 124,587 patients who underwent single-level laminotomies for LDH were identified from 2009 to 2019, with 82,643 patients in the outpatient cohort and 28,450 patients in the inpatient (Table 1). There were 13,494 patients who were categorized in the “other” site of service cohort. The matched cohort included 37,788 patients who displayed an equal distribution of patients across all general demographics. From the unmatched patient population, those who underwent an inpatient laminotomy for LDH were generally older (p<.001), more likely to be female (p<.001), and more likely to have Medicare insurance (p<.001) as compared to those who underwent an outpatient procedure.
Table 1.
Demographic Comparison of Patients Who Underwent Laminotomy for Lumbar Disc Herniation in Inpatient vs. Outpatient, Unmatched and Matched Data
| Variable | Unmatched |
Matched |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| inpatient n (%) | Outpatient n (%) | p-value | inpatient n (%) | Outpatient n (%) | p-value | |||||
| Total (n) | 28,450 | 100% | 82,643 | 100% | 17,886 | 100% | 19,902 | 100% | ||
| Average age (SD) | 50.09 | 13.83 | 47.90 | 12.81 | <.001 | 47.66 | 12.06 | 47.60 | 12.01 | .60 |
| Age (years) | <.001 | .97 | ||||||||
| 18–34 | 3,897 | 13.70% | 13,188 | 15.96% | 2,684 | 15.01% | 2,998 | 15.06% | ||
| 35–44 | 6,381 | 22.43% | 20,222 | 24.47% | 4,554 | 25.46% | 5,110 | 25.68% | ||
| 45–54 | 7,293 | 25.63% | 22,641 | 27.40% | 5,039 | 28.17% | 5,602 | 28.15% | ||
| 55–64 | 7,047 | 24.77% | 20,272 | 24.53% | 4,550 | 25.44% | 5,041 | 25.33% | ||
| 65+ | 3,832 | 13.47% | 6,320 | 7.65% | 1,059 | 5.92% | 1,151 | 5.78% | ||
| Sex | <.001 | .99 | ||||||||
| Male | 14,972 | 52.63% | 45,009 | 54.46% | 9,695 | 54.20% | 10,775 | 54.14% | ||
| Female | 13,478 | 47.37% | 37,634 | 45.54% | 8,191 | 45.80% | 9,127 | 45.86% | ||
| Insurance status | <.001 | .09 | ||||||||
| Commercial | 24,517 | 86.18% | 76,162 | 92.16% | 16,745 | 93.62% | 18,717 | 94.06% | ||
| Medicare | 3,933 | 13.82% | 6,481 | 7.84% | 1,141 | 6.38% | 1,185 | 5.94% | ||
SD=standard deviation.
Statistical significance when p-value <.05.
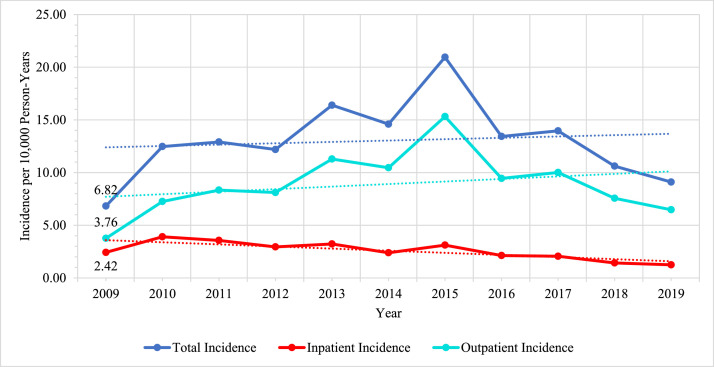
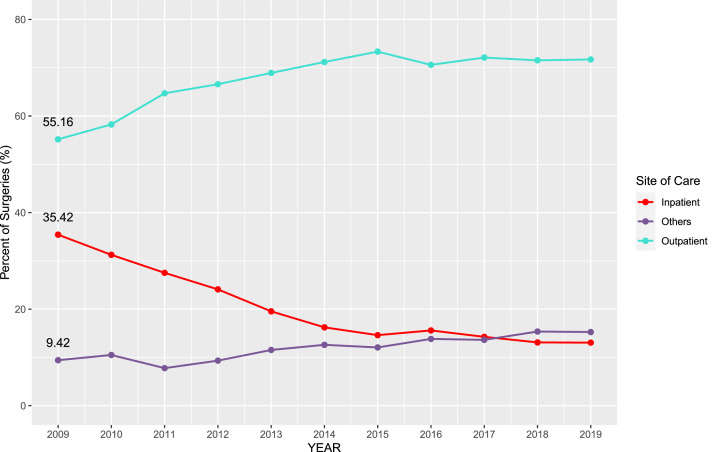
From 2009 to 2019, the average incidence of laminotomy (including all sites of care) for LDH was 13.0 per 10,000 person-years. In 2009, the total incidence of laminotomy for LDH was 6.8 cases per 10,000 person-years while in 2019 the total incidence was 9.1 cases per 10,000 person-years (Fig. 1). This incidence did not significantly change over time (p=.74). While the national volume of laminotomy for LDH did not change from 2009 to 2019, the proportion of laminotomies for LDH in the outpatient setting significantly increased over time (Fig. 2). In 2009, 55.2% of laminotomies were performed in the outpatient setting, which increased to 71.1% in 2019 (R=0.70, p=.02).
Fig. 1.
Annual incidence of laminotomy for lumbar disc herniation from 2009–2019, by Site of Care.
Fig. 2.
Proportion of laminotomy for lumbar disc herniation by Site of Care.
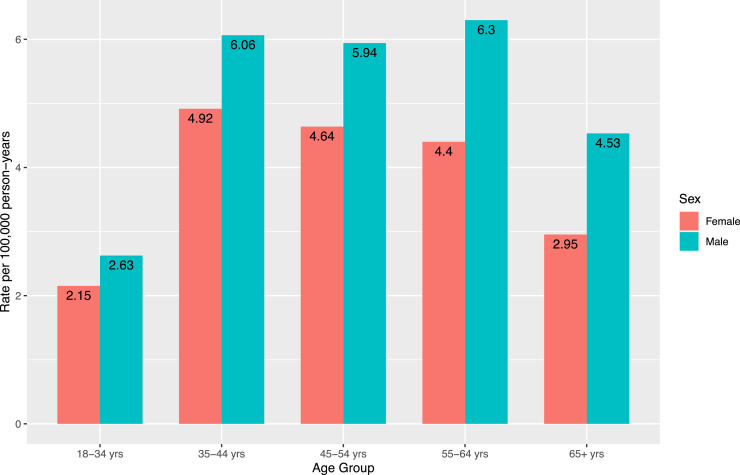
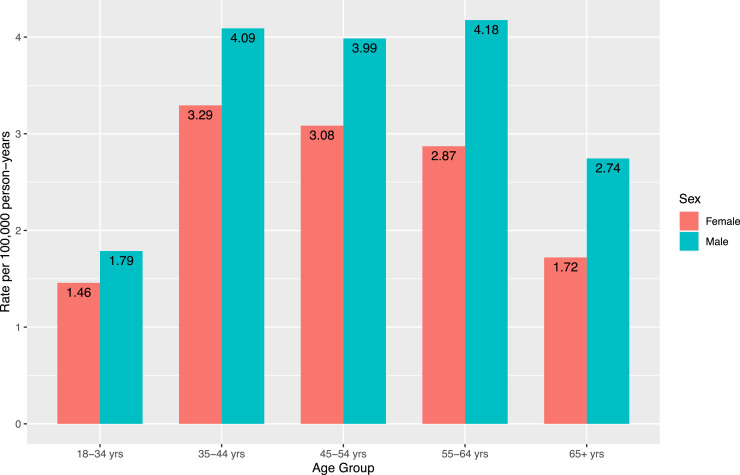
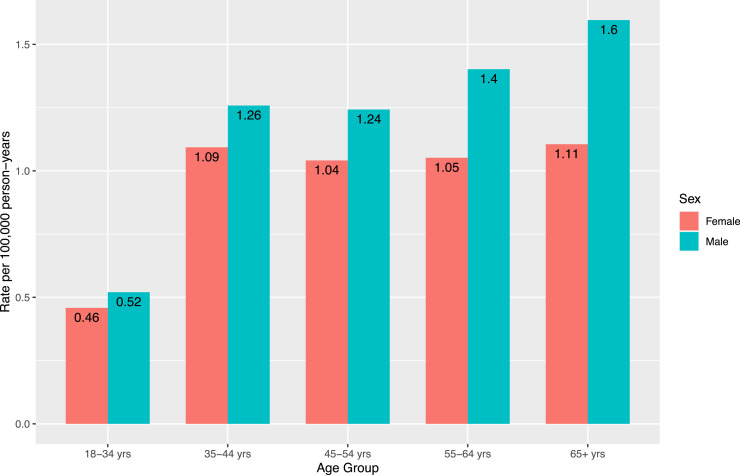
To characterize the distribution of patients undergoing laminotomies for LDH, Fig. 3A–C display the incidences of laminotomies for LDH by age- and sex- strata over the eleven-year period. When looking at all sites of care together, male patients underwent these procedures more than females. The largest cohort of male patients were between ages of 55–64, while the largest cohort of female patients were between 35–44 years old (Fig. 3A). A similar pattern was seen in the incidence of laminotomy for LDH in the outpatient setting (Fig. 3B). In the inpatient setting (Fig. 3C), patients 65+ years of age had the highest incidence for both sexes.
Fig. 3.
A. Incidence of laminotomy for lumbar disc herniation by sex- and age-strata; all sites.
Fig. 3.
B. Incidence of laminotomy for lumbar disc herniation by sex- and age-strata; outpatient only.
Fig. 3.
C. Incidence of laminotomy for lumbar disc herniation by sex- and age-strata; inpatient only.
Furthermore, differences in comorbidities were found between patients who underwent inpatient versus outpatient laminotomies for LDH (Table 2). From the unmatched cohort, patients who underwent inpatient procedures were associated with a greater distribution of CCI scores greater than 0 (p<.001). These patients composed of significantly higher rates of almost all cardiovascular, pulmonary, and neuropsychological comorbidities compared to patients who underwent outpatient laminotomies. After matching, the general distribution of CCI scores was equal between inpatient and outpatient laminotomies. However, the inpatient cohort had higher proportions of patients with history of CHF (p<.001), hemiplegia (p<.001), and CAD (p<.001), while the outpatient cohort had higher proportions of patients with chronic pulmonary disease (p=.02), mild liver disease (p<.001), smoking history (p<.001), and HLD (p<.001).
Table 2.
Comorbidity Comparison of Patients Who Underwent Laminotomy for Lumbar Disc Herniation in Inpatient vs. Outpatient, Unmatched and Matched Data
| Unmatched |
Matched |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable | inpatient n (%) | Outpatient n (%) | p-value | inpatient n (%) | Outpatient n (%) | p-value | ||||
| Charlson index | <.001 | .94 | ||||||||
| 0 | 14,539 | 51.10% | 45,966 | 55.62% | 10,499 | 58.70% | 11,626 | 58.42% | ||
| 1 or 2 | 10,283 | 36.14% | 28,827 | 34.88% | 6,306 | 35.27% | 7,057 | 35.46% | ||
| 3 or 4 | 2,488 | 8.75% | 5,691 | 6.89% | 982 | 5.49% | 1,104 | 5.55% | ||
| 5 or greater | 1,140 | 4.00% | 2,159 | 2.61% | 99 | 0.55% | 115 | 0.58% | ||
| Comorbidities | ||||||||||
| Congestive heart failure | 1,000 | 3.51% | 1,898 | 2.30% | <0.001 | 359 | 2.01% | 304 | 1.53% | <.001 |
| Rheumatic disease | 1,005 | 3.53% | 2,302 | 2.79% | <0.001 | 481 | 2.69% | 498 | 2.50% | .25 |
| Chronic kidney disease | 803 | 2.82% | 1,619 | 1.96% | <0.001 | 202 | 1.13% | 229 | 1.15% | .84 |
| Chronic pulmonary disease | 3,517 | 12.36% | 9,670 | 11.70% | 0.003 | 1,777 | 9.94% | 2,124 | 10.67% | .02 |
| Peripheral vascular disease | 1,124 | 3.95% | 2,417 | 2.92% | <0.001 | 405 | 2.26% | 459 | 2.31% | .79 |
| Cerebral vascular disease | 470 | 1.65% | 989 | 1.20% | <0.001 | 157 | 0.88% | 170 | 0.85% | .81 |
| Myocardial infarction | 639 | 2.24% | 1,422 | 1.72% | <0.001 | 222 | 1.24% | 296 | 1.49% | .05 |
| Dementia | 76 | 0.27% | 140 | 0.17% | 0.004 | 15 | 0.08% | 26 | 0.13% | .16 |
| Peptic ulcer disease | 390 | 1.37% | 997 | 1.21% | 0.03 | 178 | 0.99% | 205 | 1.03% | .74 |
| Mild liver disease | 5,372 | 18.89% | 15,811 | 19.13% | 0.35 | 2,880 | 16.10% | 3,545 | 17.81% | <.001 |
| Diabetes (w/o complication) | 5,016 | 17.63% | 12,076 | 14.61% | <0.001 | 2,384 | 13.33% | 2,586 | 12.99% | .34 |
| Diabetes (with complication) | 1,177 | 4.14% | 2,639 | 3.19% | <0.001 | 308 | 1.72% | 357 | 1.79% | 0.59 |
| Hemiplegia | 724 | 2.54% | 746 | 0.90% | <0.001 | 261 | 1.46% | 126 | 0.63% | <.001 |
| Malignancy | 1,785 | 6.27% | 4,046 | 4.89% | <0.001 | 566 | 3.16% | 678 | 3.41% | .19 |
| Mod/severe liver disease | 38 | 0.13% | 101 | 0.12% | 0.65 | 10 | 0.06% | 4 | 0.02% | .08 |
| Metastatic cancer | 201 | 0.71% | 397 | 0.48% | <0.001 | 6 | 0.03% | 4 | 0.02% | .43 |
| HIV/AIDS | 64 | 0.22% | 144 | 0.17% | 0.11 | 0 | 0.00% | 6 | 0.03% | .99 |
| Obesity | 5,727 | 20.13% | 16,243 | 19.65% | 0.08 | 3,455 | 19.32% | 3,817 | 19.18% | .73 |
| Smoking | 5,415 | 19.03% | 16,422 | 19.87% | 0.002 | 3,353 | 18.75% | 4,046 | 20.33% | <.001 |
| Coronary artery disease | 3,520 | 12.37% | 7,544 | 9.13% | <0.001 | 1,669 | 9.33% | 1,651 | 8.29% | <.001 |
| Hypertension | 13,813 | 48.55% | 36,936 | 44.69% | <0.001 | 7,902 | 44.18% | 8,733 | 43.88% | .56 |
| Hyperlipidemia | 13,394 | 47.08% | 37,052 | 44.83% | <0.001 | 7,636 | 42.69% | 8,900 | 44.72% | <.001 |
| Alcohol | 630 | 2.21% | 1,695 | 2.05% | 0.10 | 355 | 1.98% | 403 | 2.02% | .78 |
| Depression | 5,874 | 20.64% | 16,695 | 20.20% | 0.11 | 3,500 | 19.57% | 4,083 | 20.52% | .05 |
| Atrial fibrillation | 867 | 3.05% | 1,756 | 2.12% | <0.001 | 351 | 1.96% | 346 | 1.74% | .11 |
| Hypercoagulable state | 392 | 1.38% | 917 | 1.11% | <0.001 | 202 | 1.13% | 202 | 1.01% | .28 |
| History of DVT/PE | 297 | 1.04% | 694 | 0.84% | 0.003 | 153 | 0.86% | 138 | 0.69% | .07 |
HIV/AIDS=human immunodeficiency virus/acquired immunodeficiency syndrome; DVT/PE=deep vein thrombosis/pulmonary embolism.
Statistical significance when p-value <.05.
Ninety-day complication rates between inpatient and outpatient laminotomies for LDH are shown in Table 3. Both univariate and multivariate analyses demonstrated that inpatient laminotomies were associated with significantly higher risks for SSI (odds ratio [OR] 1.61, p<.001), VTE (OR 1.96, p<.001), hematoma (OR 1.71, p<.001), UTI (OR 1.41, p<.001), AKI (OR 1.75, p=.001), dural tears (OR 1.55, p<.001), neurogenic urinary retention (OR 1.89, p<.001), and all-cause hospital readmissions (OR 1.84, p<.001) compared to outpatient procedures. Interestingly, patients who underwent an inpatient laminotomy were less likely to undergo a revision procedure compared to patients who underwent an outpatient laminotomy (OR 0.67, p<.001).
Table 3.
Univariate and Multivariate Analyses of 90-Day Complication Rates Between Matched Cohort of Inpatient vs. Outpatient Laminotomies for Lumbar Disc Herniation Controlled by Age, Sex, comorbidities, Insurance Type, and Geographic Region
| 90-day complication | Univariate |
Multivariate (Reference group—outpatient) |
||||
|---|---|---|---|---|---|---|
| inpatient % | Outpatient % | p-value | Inpatient odds ratio | 95% CI | p-value | |
| Surgical site infection (SSI) | 2.26% | 1.42% | <.001 | 1.61 | 1.38–1.88 | <.001 |
| Sepsis | 0.33% | 0.29% | .50 | 1.15 | 0.80–1.65 | .46 |
| Nerve injury | 0.02% | 0.03% | .39 | 0.52 | 0.13–2.08 | .35 |
| Venous thromboembolism (VTE) | 1.84% | 0.94% | <.001 | 1.96 | 1.62–2.36 | <.001 |
| Wound dehiscence | 0.83% | 0.58% | .005 | 1.42 | 1.11–1.82 | .005 |
| Hematoma | 1.25% | 0.74% | <.001 | 1.71 | 1.38–2.11 | <.001 |
| Urinary tract infection (UTI) | 3.66% | 2.63% | <.001 | 1.41 | 1.25–1.58 | <.001 |
| Acute kidney injury (AKI) | 0.50% | 0.28% | <.001 | 1.75 | 1.25–2.45 | .001 |
| Atrial fibrillation | 0.97% | 0.77% | .03 | 1.25 | 0.96–1.64 | .10 |
| Dural tear | 0.79% | 0.51% | <.001 | 1.55 | 1.20–2.01 | <.001 |
| Neurogenic urinary retention | 2.26% | 1.20% | <.001 | 1.89 | 1.61–2.22 | <.001 |
| Revision surgery | 1.97% | 2.95% | <.001 | 0.67 | 0.58–0.76 | <.001 |
| Hospital readmission | 7.60% | 4.28% | <.001 | 1.84 | 1.68–2.01 | <.001 |
CI=confidence interval
Statistical significance when p-value <.05/13 based on Bonferroni correction.
Discussion
This study examines recent trends in incidence and complication rates between inpatient versus outpatient laminotomies for LDH. Our findings reveal that, while rates of laminotomies for LDH have not significantly changed from 2009 to 2019, the proportion of laminotomies performed in the outpatient setting has significantly increased in this time period. Laminotomies performed in the inpatient setting were associated with higher rates of 90-day postoperative complications as compared to the outpatient setting, even when controlling for certain comorbidities.
This shift towards outpatient laminotomies for LDH aligns with existing literature reporting increased outpatient utilization for various spinal operations [18,19]. Advances in anesthesia, surgical equipment, and surgical techniques have allowed this to safely be the case. Outpatient surgeries provide a cost-effective option for the healthcare system, which may be a significant driver for the recent changes in practice. Silvers et al. noted that annual health cost savings exceed around $100 million annually with the utilization of day surgeries in the outpatient setting [20]. Purger et al. also demonstrated that overall charges for anterior cervical discectomy and fusion were more than $35,000 cheaper on average per patient when performed in the ambulatory surgery center compared to an inpatient hospital [21].
While decreasing costs may be economically beneficial to the healthcare system, these shifts toward outpatient surgeries can only be sustained if clinical outcomes are either at par or superior to those of the inpatient setting. Several studies, including those from Adamson et al. [22], Purger et al. [21], and Cuellar et al. [23], have demonstrated that complication rates from common spinal procedures performed in the outpatient setting were comparable to those performed in the inpatient setting without posing any increased risks. Our current study exemplified that inpatient laminotomies for LDH were associated with higher rates of 90-day postoperative complications, including all-cause hospital readmissions, SSI, hematoma, dural tears, VTE, UTI, AKI, and neurogenic urinary retention. Likewise, An et al. demonstrated that all patients within their study who underwent lumbar laminotomy and discectomy in the outpatient setting reported positive satisfaction after surgery, with only 7% of patients having any postoperative complication [24]. Several other studies have also shown the incidence of complications after various other spinal procedures to be higher in the inpatient cohort as compared to the outpatient [[25], [26], [27]]. These results suggest that outpatient laminotomies for LDH may be a safer alternative, and could also be a driver, alongside the cost reduction, for the recent shifts in practice toward outpatient utilization.
However, the role of patient selection likely impacts these observed results. Our study showed that patients undergoing inpatient procedures in this study tended to be older, with the highest incidence in patients at 65+ years old for both sexes. In the outpatient cohort, the demographics with the highest incidence were male patients between 35–44 and 55–64 years old. These results coincide with the results of prior literature that have shown the incidence of LDH to be most common in middle-aged men with the incidence of inpatient spinal surgery to be higher in elderly patients [6,7,18]. These differences are likely attributed to the fact that patients receiving inpatient procedures have significantly more comorbidities, which aligns with the results shown in this study as well.
Even after propensity-score matching, while the distribution of CCI scores were similar, the individual comorbidities that comprised the CCI score were different. The CCI is a weighed calculator that considers 17 different comorbidities in order to predict 10-year mortality [35], thus while propensity-score matching balanced the distribution of scores, when looking at each individual comorbidity, patients in the inpatient cohort had a higher percentage of CHF, hemiplegia, and CAD while patients in the outpatient cohort had a higher percentage of chronic pulmonary disease, mild liver disease, smoking, and hyperlipidemia. This comorbidity profile in patients undergoing inpatient procedures may potentially contribute to the risk of developing a complication after surgery. Karukonda et al. similarly showed that patients who underwent single or 2-level lumbar laminectomies in the inpatient setting were older and had higher rates of obesity, diabetes, CHF, HTN, and cancer [28]. While comorbidities innately pose a risk for complication, multiple factors related to the site of service also likely affect our findings. Pugely et al. hypothesized that inpatient patients are more likely to be immobilized longer, more likely to have increased rates of urinary catheterization, and more likely to experience exposure to hospital-acquired pathogens [25]. Future prospective work that optimizes patient cohort matching must be done in order to fully understand these effects.
Nevertheless, our results suggest an enhanced risk in performing laminotomies for LDH in the inpatient setting. This then poses the question of which patients, if any, are best suited for receiving a laminotomy in the inpatient setting, which does provide closer monitoring of life-threatening complications including airway compromise, spinal cord compression, or hematoma formation [29,30]. Studies examining inpatient and outpatient surgeries for other spinal operations have postulated that patient selection for surgical site depends on individualized risk stratification to ensure patient safety. For example, patients with American Society of Anesthesiologists (ASA) class 3 or greater, or those with advanced age (>80 years) may not be suitable candidates for outpatient surgeries as they have increased risks for postoperative complications and thus are better candidates for inpatient procedures and closer monitoring [31,32]. Patients with certain independent risk factors such as CCI score 4+, chronic steroid use, higher BMI, chronic obstructive pulmonary disease, history of stroke or transient ischemic attack, or previous cardiac surgical intervention may also benefit from inpatient surgeries [26,33,34]. As a result, surgeons should consider individual risk factors and comorbidities when determining treatment trajectories for patients, weighing the likelihood of complications as a result of the patient risk profile versus the site of surgery itself.
Although inpatient laminotomies and the required hospitalization may pose inherent risks, patients with a severe comorbidity profile may be advised against outpatient surgeries due to the chances of developing serious complications as a result of their comorbidities, thus needing close surveillance. Patients without these high-risk factors would likely benefit from outpatient procedures, as shown in this study, yet these should be educated, joint decisions made between physicians and patients.
Overall, one strength of this study is its evaluation of recent national trends and incidences of laminotomy for LDH. Another strength of our analysis is its utilization of one of the largest national databases, which allows our study to evaluate a heterogenous group of surgical centers and patient populations, making it more generalizable than studies focused on a limited number of centers. Additionally, our study contributes novel information to the spine literature by not only comparing readmission and revision rates of laminotomy for LDH at the 90-day postoperative period as previously done by Mooney et al., but also incorporating a variety of surgical and medical complication rates within the different surgical sites of care [36].
On the other hand, one limitation of this study is its reliance on administrative coding, which may introduce coding errors. For example, one area of inaccuracy may be in defining the patients’ site of surgery, especially for those who may have had an outpatient surgery but were transferred to an inpatient facility due to a postoperative complication or for closer surveillance. Additionally, some patients may have had a multi-level laminotomy but were documented as single level only. While patients with a multi-level laminotomy were excluded using appropriate CPT coding, the database does not provide operative notes to confirm. Similarly, due to the limitations of the database, it is difficult to conclude that all laminotomies in the study population were for LDH and not for other concurrent spinal pathologies. While the study excluded patients with cauda equina syndrome, the study population may still be heterogenous as other spinal pathologies were not excluded. Additionally, ICD codes were only able to be captured on the associated date of surgery rather than prior to the surgery date. Another limitation is that complication rates may have been underestimated in the outpatient group due to possible loss of follow-up, such as patients missing their postoperative appointments or presenting to a different hospital or clinic. While patients without a continuous 90-day enrollment in the database were excluded from the study, this is still a fundamental limitation with the database. Furthermore, although propensity-score matching was employed to mitigate demographic and comorbidity differences, there were still discrepancies between patients who underwent laminotomy for LDH in the inpatient versus outpatient settings. Therefore, it is impossible to directly attribute conclusions about complication risks to the site of service where surgery was performed. Future studies should employ prospective methodologies that control for patient demographics and comorbidities between the two settings. Another limitation is the lack of information in the database on uninsured patients or those on Medicaid payment plans, which may lead to underestimations of the national incidences of laminotomy for LDH. However, previous research has shown the current database to still be reliable and representative of the U.S. population [[29], [30], [31]]. Our results, nevertheless, cannot be generalized to these populations.
In conclusion, our study shows that while the use of laminotomy for LDH has remained stable in the U.S., there has been a shift in practice favoring outpatient utilization for these procedures. This shift may be potentially associated with a reduction in several common postoperative complications compared to inpatient procedures, however, more data is needed to fully understand these trends. Nevertheless, our study provides important data on recent trends of lumbar laminotomies for physicians to understand when considering patients for inpatient versus outpatient laminotomies.
Declarations of competing interests
One or more of the authors declare financial or professional relationships on ICMJE-NASSJ disclosure forms.
Footnotes
FDA device/drug status: Not applicable.
Author disclosures: KYH: Nothing to disclose. JMB: Scientific Advisory Board/Other Office: AAOS Now Editorial Board (none). SK: Nothing to disclose. AK: Nothing to disclose. PVR: Nothing to disclose. LAB: Nothing to disclose. STY: Royalties: Spine Art (none), Alphatec (none); Stock Ownership: Medyssey Spine (none); Consulting: Alphatec (none); Trips/Travel: AOSpine (none), ISSLS (none); Scientific Advisory Board/Other Office: ISSLS (none), AOSpine (none); Grants: AOSpine (none), Empiric Spine (none), National Institutes of Health (none).
IRB statement: The present study utilized a publicly available database with de-identified data; therefore, institutional review board approval was not required.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.xnsj.2024.100328.
Appendix. Supplementary materials
References
- 1.Lee CH, Chung CK, Kim CH, Kwon JW. Health care burden of spinal diseases in the Republic of Korea: analysis of a Nationwide Database from 2012 through 2016. Neurospine. 2018;15(1):66–76. doi: 10.14245/ns.1836038.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lucas JW, Connor EM, Back Bose J. Lower limb, and upper limb pain among U.S. adults, 2019. NCHS Data Brief. 2021;(415):1–8. [PubMed] [Google Scholar]
- 3.Dydyk AM, Ngnitewe Massa R, Mesfin FB. Disc herniation. StatPearls. 2022 [PubMed] [Google Scholar]
- 4.Fjeld OR, Grovle L, Helgeland J, et al. Complications, reoperations, readmissions, and length of hospital stay in 34 639 surgical cases of lumbar disc herniation. Bone Joint J. 2019;101-B(4):470–477. doi: 10.1302/0301-620X.101B4.BJJ-2018-1184.R1. [DOI] [PubMed] [Google Scholar]
- 5.Protzer LA, Glassman SD, Mummaneni PV, et al. Return to work in patients with lumbar disc herniation undergoing fusion. J Orthop Surg Res. 2021;16(1):534. doi: 10.1186/s13018-021-02682-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Balaara A, Xu XF, Huang YH, Dapeng L. Predictors of the outcome of lumbar disc herniation following classical surgery: laminotomy with discectomy. Orthopade. 2017;46(6):530–537. doi: 10.1007/s00132-017-3398-2. [DOI] [PubMed] [Google Scholar]
- 7.Jordan J, Konstantinou K, O’Dowd J. Herniated lumbar disc. BMJ Clin Evid. 2011;2011:1118. [PMC free article] [PubMed] [Google Scholar]
- 8.Jordan J, Konstantinou K, O’Dowd J. Herniated lumbar disc. BMJ Clin Evid. 2009;2009:1118. [PMC free article] [PubMed] [Google Scholar]
- 9.Kim KD, Wang JC, Robertson DP, et al. Reduction of radiculopathy and pain with Oxiplex/SP gel after laminectomy, laminotomy, and discectomy: a pilot clinical study. Spine (Phila Pa 1976) 2003;28(10):1080–1087. doi: 10.1097/01.BRS.0000062354.26905.B8. [DOI] [PubMed] [Google Scholar]
- 10.Lewis PJ, Weir BK, Broad RW, Grace MG. Long-term prospective study of lumbosacral discectomy. J Neurosurg. 1987;67(1):49–53. doi: 10.3171/jns.1987.67.1.0049. [DOI] [PubMed] [Google Scholar]
- 11.Al Qaraghli MI, De Jesus O. Lumbar disc herniation. StatPearls. 2022 [PubMed] [Google Scholar]
- 12.Ruggeri A, Pichierri A, Marotta N, Tarantino R, Delfini R. Laminotomy in adults: technique and results. Eur Spine J. 2012;21(2):364–372. doi: 10.1007/s00586-011-1826-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nie H, Hao J, Peng C, Ou Y, Quan Z, An H. Clinical outcomes of discectomy in octogenarian patients with lumbar disc herniation. J Spinal Disord Tech. 2013;26(2):74–78. doi: 10.1097/BSD.0b013e318236b92d. [DOI] [PubMed] [Google Scholar]
- 14.Chatterjee A, Rbil N, Yancey M, Geiselmann MT, Pesante B, Khormaee S. Increase in surgeons performing outpatient anterior cervical spine surgery leads to a shift in case volumes over time. N Am Spine Soc J. 2022;11 doi: 10.1016/j.xnsj.2022.100132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Crawford DC, Li CS, Sprague S, Bhandari M. Clinical and cost implications of inpatient versus outpatient orthopedic surgeries: a systematic review of the published literature. Orthop Rev (Pavia) 2015;7(4):6177. doi: 10.4081/or.2015.6177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Walcott BP, Hanak BW, Caracci JR, et al. Trends in inpatient setting laminectomy for excision of herniated intervertebral disc: population-based estimates from the US nationwide inpatient sample. Surg Neurol Int. 2011;2:7. doi: 10.4103/2152-7806.76144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Naessig S, Kapadia BH, Ahmad W, et al. Outcomes of same-day orthopedic surgery: are spine patients more likely to have optimal immediate recovery from outpatient procedures? Int J Spine Surg. 2021;15(2):334–340. doi: 10.14444/8043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beschloss A, Ishmael T, Dicindio C, et al. The expanding frontier of outpatient spine surgery. Int J Spine Surg. 2021;15(2):266–273. doi: 10.14444/8036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ahn J, Bohl DD, Tabaraee E, Basques BA, Singh K. Current trends in outpatient spine surgery. Clin Spine Surg. 2016;29(9):384–386. doi: 10.1097/BSD.0000000000000417. [DOI] [PubMed] [Google Scholar]
- 20.Silvers HR, Lewis PJ, Suddaby LS, Asch HL, Clabeaux DE, Blumenson LE. Day surgery for cervical microdiscectomy: is it safe and effective? J Spinal Disord. 1996;9(4):287–293. [PubMed] [Google Scholar]
- 21.Purger DA, Pendharkar AV, Ho AL, et al. Outpatient vs inpatient anterior cervical discectomy and fusion: a population-level analysis of outcomes and cost. Neurosurgery. 2018;82(4):454–464. doi: 10.1093/neuros/nyx215. [DOI] [PubMed] [Google Scholar]
- 22.Adamson T, Godil SS, Mehrlich M, Mendenhall S, Asher AL, McGirt MJ. Anterior cervical discectomy and fusion in the outpatient ambulatory surgery setting compared with the inpatient hospital setting: analysis of 1000 consecutive cases. J Neurosurg Spine. 2016;24(6):878–884. doi: 10.3171/2015.8.SPINE14284. [DOI] [PubMed] [Google Scholar]
- 23.Cuellar JM, Nomoto E, Saadat E, et al. Outpatient versus inpatient anterior lumbar spine surgery: a multisite, comparative analysis of patient safety measures. Int J Spine Surg. 2021;15(5):937–944. doi: 10.14444/8123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.An HS, Simpson JM, Stein R. Outpatient laminotomy and discectomy. J Spinal Disord. 1999;12(3):192–196. [PubMed] [Google Scholar]
- 25.Pugely AJ, Martin CT, Gao Y, Mendoza-Lattes SA. Outpatient surgery reduces short-term complications in lumbar discectomy: an analysis of 4310 patients from the ACS-NSQIP database. Spine (Phila Pa 1976) 2013;38(3):264–271. doi: 10.1097/BRS.0b013e3182697b57. [DOI] [PubMed] [Google Scholar]
- 26.Fu MC, Gruskay JA, Samuel AM, et al. Outpatient anterior cervical discectomy and fusion is associated with fewer short-term complications in one- and two-level cases: a propensity-adjusted analysis. Spine (Phila Pa 1976) 2017;42(14):1044–1049. doi: 10.1097/BRS.0000000000001988. [DOI] [PubMed] [Google Scholar]
- 27.Khanna R, Kim RB, Lam SK, Cybulski GR, Smith ZA, Dahdaleh NS. Comparing short-term complications of inpatient versus outpatient single-level anterior Cervical discectomy and fusion: an analysis of 6940 patients using the ACS-NSQIP Database. Clin Spine Surg. 2018;31(1):43–47. doi: 10.1097/BSD.0000000000000499. [DOI] [PubMed] [Google Scholar]
- 28.Karukonda TR, Mancini N, Katz A, Cote MP, Moss IL. Lumbar laminectomy in the outpatient setting is associated with lower 30-day complication rates. Global Spine J. 2020;10(4):384–392. doi: 10.1177/2192568219850095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sagi HC, Beutler W, Carroll E, Connolly PJ. Airway complications associated with surgery on the anterior cervical spine. Spine (Phila Pa 1976) 2002;27(9):949–953. doi: 10.1097/00007632-200205010-00013. [DOI] [PubMed] [Google Scholar]
- 30.Bovonratwet P, Fu MC, Tyagi V, et al. Incidence, risk factors, and clinical implications of postoperative hematoma requiring reoperation following anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 2019;44(8):543–549. doi: 10.1097/brs.0000000000002885. [DOI] [PubMed] [Google Scholar]
- 31.Bovonratwet P, Ottesen TD, Gala RJ, et al. Outpatient elective posterior lumbar fusions appear to be safely considered for appropriately selected patients. Spine J. 2018;18(7):1188–1196. doi: 10.1016/j.spinee.2017.11.011. [DOI] [PubMed] [Google Scholar]
- 32.Sher A, Keswani A, Yao DH, Anderson M, Koenig K, Moucha CS. Predictors of same-day discharge in primary total joint arthroplasty patients and risk factors for post-discharge complications. J Arthroplasty. 2017;32(9S):S150–S156.e1. doi: 10.1016/j.arth.2016.12.017. [DOI] [PubMed] [Google Scholar]
- 33.Mathis MR, Naughton NN, Shanks AM, et al. Patient selection for day case-eligible surgery: identifying those at high risk for major complications. Anesthesiology. 2013;119(6):1310–1321. doi: 10.1097/ALN.0000000000000005. [DOI] [PubMed] [Google Scholar]
- 34.Madsen HJ, Henderson WG, Dyas AR, et al. Inpatient versus outpatient surgery: a comparison of postoperative mortality and morbidity in elective operations. World J Surg. 2023;47(3):627–639. doi: 10.1007/s00268-022-06819-z. [DOI] [PubMed] [Google Scholar]
- 35.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 36.Mooney J., Michalopoulos G.D., Zeitouni D., et al. Outpatient versus inpatient lumbar decompression surgery: a matched noninferiority study investigating clinical and patient-reported outcomes. J Neurosurg Spine. 2022;37(4):1–13. doi: 10.3171/2022.3.SPINE211558. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.