Abstract
Background and Aims
Physical performance is a major contributor of mobility and independence during older life. Despite a progressive decline in musculoskeletal function starts from middle age, several factors acting during the life-course can negatively influence musculoskeletal functional capacities. Lifestyle interventions incorporating nutrition and physical exercise can help maximizing the muscle functional capacities in early life as well as preserving them later in life. Among various dietary compounds, omega-3 polyunsaturated fatty acids (PUFAs) are gaining growing attention for their potential effects on muscle membrane composition and muscle function. Indeed, several pathways are enhanced, such as an attenuation of pro-inflammatory oxidative stress, mitochondrial function, activation of the mammalian target of rapamycin (mTOR) signaling and reduction of insulin resistance.
Methods
We performed a narrative review to explore the existing literature on the relationship between omega-3 PUFAs and physical performance across the life-course.
Results
Growing evidence from randomized controlled trials (RCTs) suggests beneficial effects of omega-3 PUFAs on muscle function, including physical performance parameters in mid to later life. On the other hand, despite a direct association in early life is not available in literature, some mechanisms by which omega-3 PUFAs may contribute to improved adult physical performance could be hypothesized.
Conclusion
Omega-3 PUFAs are gaining growing attention for their positive effect on muscle function parameters. The integration of physical function measures in future studies would be of great interest to explore whether omega-3 PUFAs could contribute to improved muscle function, starting from early life and extending throughout the lifespan. However, larger and high-quality RCTs are needed to fully elucidate the beneficial effects of omega-3 PUFAs supplementation on muscle mass and function.
Keywords: aging, nutrition, life course, sarcopenia, omega-3 PUFAs, frailty
Introduction
Advancing age is characterized by a progressive and generalized decline in muscle mass and function, the so-called “sarcopenia.” However, sarcopenia can occur earlier in life (1, 2). The original definition of sarcopenia focused on muscle mass as stand-alone. Subsequently, much more emphasis has been given to muscle function such that it currently comes to the forefront of international guidelines (3, 4). Physical performance, a major contributor of mobility and independence during older life (5), has been defined as “an objectively measured whole-body function related to locomotion” (3, 6). The multidimensional concept of physical performance is not merely limited to skeletal muscle but also involves central and peripheral nervous function including balance (3, 6). Low physical performance has been formerly considered a core component of sarcopenia (3, 7) and has been widely associated with adverse outcomes including frailty, disability and subsequent death (3, 8–14). Consequently, low physical performance is used to identify the severity of sarcopenia (3). There is a large consensus on the key role that physical function, and in particular mobility, plays in the determination of frailty status (15, 16), regardless of the operational definition used (17). At the same time, the relationship between frailty and physical performance may be bi-directional since frailty status can also negatively affect mobility and physical function. In fact, physical performance measures are often used as an outcome measure in most of the trials targeting frailty and sarcopenia. Frailty and sarcopenia can be considered complementary in many aspects. To date, the physical frailty phenotype proposed by Fried et al. (18) shows a remarkable overlap with sarcopenia. The Physical Frailty and Sarcopenia (PF&S) model (15) has been therefore suggested as a possible solution to combine the two entities (i.e., frailty and sarcopenia) into a unique operational definition. Furthermore, the large body of literature about physical function impairment as well as the presence of dedicated measures that are widely accepted (e.g., short physical performance battery, handgrip strength, gait speed), make the PF&S model an easy-to-implement model to capture both frailty and sarcopenia (15). It is indeed largely agreed that the physical function impairment that results from the combination of frailty and sarcopenia acquires completely different connotations toward worst outcomes (19).
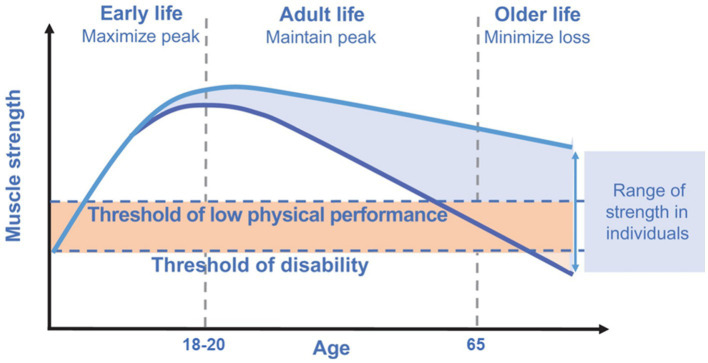
Despite a progressive decline in musculoskeletal function starts from middle age, several factors acting during the life course can influence musculoskeletal functional capacities. Starting from early life, each individual rapidly acquires supporting muscle functions to reach a peak or a plateau nearly at the end of adolescence period. Subsequently, after the fourth decade of life, a progressive decline in muscle mass (i.e., ~1–2% per year) and strength (i.e., ~1.5% per year) is seen (20). Kaymak et al. (3), in a comment to the European Working Group on Sarcopenia in Older People revised consensus (EWGSOP2), suggested that measurement of muscle power (intended as the product of strength and velocity) is more relevant than muscle strength as stand-alone in reflecting physical performance. Accordingly, muscle power has been suggested as the most relevant measure of muscle function, being more strongly correlated with functional performance than strength as stand-alone in older people. An example may be the chair stand test that requires both strength and velocity for its execution (3). In the early phases of muscle decline (i.e., initial decrease in muscle mass and strength), an individual could still have a preserved physical performance and may be very far from the threshold of disability (3) (Figure 1). Hall et al. (5), in the Physical Performance Across the Life-span Study, reported that physical performance is almost stable in the first two decades of adulthood (i.e., from 30 to 50 years of age) with a progressive decline in the middle years (i.e., 50+) and late adulthood. Besides genetic and lifestyle factors operating across the life course, also some pathological conditions can accelerate this degenerative process (with a consequent progression toward functional impairment and disability). Lifestyle interventions incorporating nutrition and physical exercise are able to slow or reverse this process (Figure 1) (3, 21). The rate of decline in muscle mass and function is also reflected by their peaks attained during early life (2). Indeed, it is essential to maximize muscle function in early life as well as maintain this peak during adult life to minimize losses during older life (3).
Figure 1.
Muscle strength across the life course. Modified from Cruz-Jentoft et al. (3), licensed under CC BY-NC 4.0. The rate of decline in muscle strength is reflected by the peak attained during early life. Maximizing the peak of muscle strength in early life as well as maintaining this peak during adult life is pivotal to minimize losses during older life.
Nutritional strategies to counteract muscle mass and function decline are mainly based on protein supplementation combined with adequate calorie intake while there is limited knowledge on other nutritional interventions (22). Furthermore, the efficacy of nutritional interventions is enhanced when combined with physical activity (i.e., resistance training) (23). Inflammation and oxidative stress are considered hallmarks of the aging process (24) influencing the rate of functional decline observed in aging. Therefore, supplementation with individual nutrients sharing antioxidant and anti-inflammatory properties has recently gained attention for potential effects against the age-related functional decline (1, 25, 26). Within the plethora of various dietary supplements, polyunsaturated fatty acids (PUFAs), particularly omega-3 PUFAs and derived long-chain PUFAs (LC-PUFAs), are of particular interest for their potential effects on muscle function and thus on physical performance through various mechanisms. Omega-3 PUFAs may promote muscle anabolism through activation of the mammalian target of rapamycin (mTOR) signaling and reduction of insulin resistance (27, 28). Furthermore, omega-3 PUFAs are widely acknowledged as nutrients with clear anti-inflammatory and antioxidant properties (27, 29, 30).
This narrative review aims to provide an overview of current knowledge about the role of omega-3 PUFAs on physical performance across the lifespan.
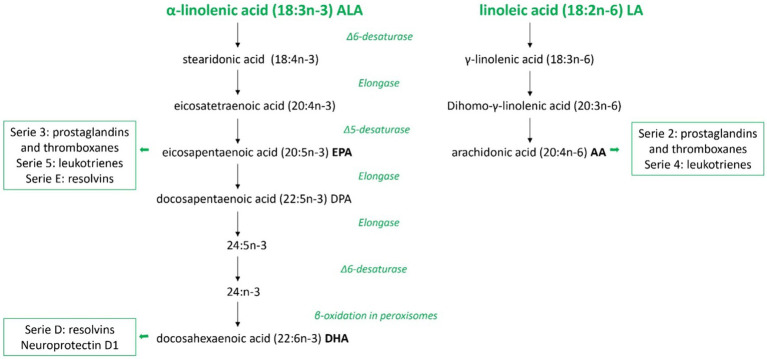
The role of PUFAs in the body
Linoleic acid (LA, 18:2) and α-linolenic acid (ALA, 18:3) are considered essential fatty acids (EFAs) because of the absence of enzymes necessary for their production in humans and other mammals. Instead, they are obtained from plants or other organisms that possess enzymatic pathways for their synthesis. They must be part of the diet and, once introduced into the body, they can be further metabolized in the liver by the enzymes Δ6 and Δ5 desaturases and elongases to generate PUFAs (31) (see Figure 2).
Figure 2.
Overview of polyunsaturated fatty acids metabolism in mammals. Schematic metabolic pathways of the two families of polyunsaturated fatty acids in mammals, omega-3 and omega-6, from the precursors α-linolenic acid and linoleic acid, respectively. In this figure are represented all the consecutive desaturation and elongation steps and the names of major eicosanoids derived. ALA, α-linolenic acid; LA, linoleic acid; EPA, eicosapentaenoic acid; DPA, docosapentaenoic acid; DHA, docosahexaenoic acid; AA, arachidonic acid.
LA is the precursor of the omega-6 PUFA family and arachidonic acid (AA) is its derived compound, while ALA, eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA) belong to the omega-3 PUFA family. These two groups of fatty acids influence in different ways the property of the cell membranes in terms of fluidity and biological effects. DHA, EPA, and AA compete for the sn-2 position on membrane phospholipids. Therefore, their relative abundance in the membrane influences their availability as substrates for the same metabolic pathway enzymes, such as cyclooxygenases and lipoxygenases. Consequently, this balance affects the production of bioactive compounds with antagonistic roles involved in various disease processes (32). Generally, AA-derived metabolites have pro-inflammatory properties, whereas EPA-derived compounds are less inflammatory. DHA-derivates have anti-inflammatory and pro-resolution activities contributing to speeding up the inflammatory response’s physiological resolution (33, 34).
Omega-3 PUFAs such as ALA and DHA and omega-6 PUFAs, such as LA and AA, are important structural components of cell membranes mainly within phospholipids. DHA is necessary for the development of brain functions and retinal functions associated to vision (35, 36). The incorporation of this omega-3 metabolite takes place at uniquely high levels in the central nervous system, where omega-3 PUFA are main determinant of membrane PUFA composition and unsaturation (37). Once high levels of DHA are established in the brain, they tend to be sustained throughout later life. This maintenance likely relies on an optimal dietary supply, particularly considering the potential decrease in efficiency of precursor conversion by the enzymatic pathway among older individuals (35, 38).
The membrane PUFA composition seems to be more responsive to dietary DHA compared to intake of LA and AA, showing a high sensitivity to dietary variations in PUFA-supply (39).
DHA, derived from ALA, has relevant metabolic activities. Besides hypolipidemic properties, reducing blood concentrations of triglycerides, DHA contributes to protect the central nervous system from reactive oxygen species, together with antioxidant properties, capable of shutting down the upstream inflammatory cascade. Furthermore, DHA exhibits immunomodulatory and antiallergic activities, contributing to its overall neuroprotective effects. From intrauterine life through later ages, DHA contributes to the maintenance of cognitive abilities and the prevention of neuropsychiatric and neurodegenerative disorders (40).
DHA and EPA share anti-inflammatory and inflammation-resolving properties including the partial inhibition of leucocyte chemotaxis, adhesion molecule expression and leukocyte-endothelial adhesive interactions, production of eicosanoids such as prostaglandins and leukotrienes from the AA, as well as the production of pro-inflammatory cytokines (30). These anti-inflammatory and pro-resolving effects show to be relevant to improve clinical outcomes in different therapeutic areas, supporting the protective role of the immune system (41). Omega-3 PUFAs seem to be involved in the activation of cells from both the innate and the adaptive immune system (42). In particular, in the innate immune cells omega-3 PUFAs (1) reduce neutrophil migration and increase their phagocytosis, (2) reduce pro-inflammatory cytokine release, increase phagocytosis and M2 macrophages phenotype that promote tissue repair at macrophage level and (3) reduce presentation at dendritic cells level (42). In the adaptive immune cells, omega-3 PUFAs limit excessive B-cells responses, increase T regulatory cells differentiation and function while reduce T helper 17 differentiation, and limit the release of pro-inflammatory cytokines (42, 43). Consistent with aims of the present review, in older populations growing evidence suggests a role of omega-3 PUFAs in the maintenance of muscle mass and function and in the musculoskeletal health in general (44).
Main mechanisms of omega-3 PUFAs in the muscle
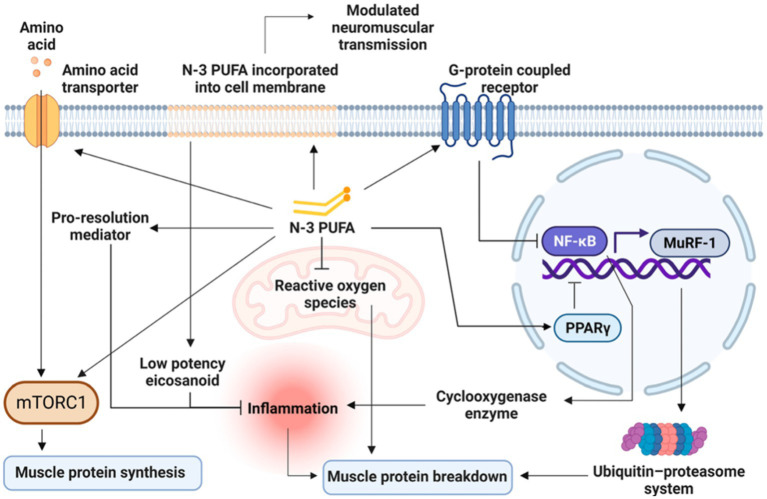
Most studies on omega-3 PUFAs have been primarily focused on cellular and molecular mechanisms underlying muscle protein metabolism (45). Accordingly, the main mechanisms through which omega-3 PUFAs could benefit muscle parameters seem to be (1) both anti-catabolic and anabolic effects on muscle protein synthesis (2) modulation of insulin sensitivity (3) amelioration of mitochondrial functioning, inflammation and muscle fiber contractile properties (4) neuroprotective and motor neuron excitability properties (46). Figure 3 presents an overview on the main mechanisms, which will be discussed in detail by each life stage (e.g., early life, adult and older life) in the following specific sections, by which omega-3 PUFAs can influence muscle parameters.
Figure 3.
Overview of the main mechanisms by which Omega-3 PUFAs can influence muscle parameters. Modified from Therdyothin et al. (47), licensed under CC BY 4.0. Omega-3 PUFAs, incorporated into the cell membrane, modulate neuromuscular transmission and seem to directly stimulate mTORC1, both as stand-alone and synergically with amino acids ingestion thus enhancing muscle protein synthesis. Omega-3 PUFAs also counteract inflammatory processes through less production of inflammatory mediators as well as by the release of pro-resolution mediators and by reducing ROS production at the mitochondrial level, thus decreasing muscle protein breakdown. Omega-3 PUFAs also act as ligands for G-protein coupled receptors (GPCRs) and induce the activation of the peroxisome proliferator-activated receptors (PPARs), with the consequent inhibition of nuclear factor kappa B (NFκB). In turn, the inhibition of NFκB leads to a reduced cyclooxygenase production resulting in a decreased inflammatory response finally reducing muscle protein breakdown. The inhibition of NF-κB also leads to the downregulation of the muscle ring finger-1 (MuRF-1) gene counteracting the ubiquitin-proteasome system and thus reducing muscle protein breakdown. n-3 PUFA, omega-3 polyunsaturated fatty acid; mTORC1, mammalian target of rapamycin complex; NFκB, nuclear factor kappa B; MuRF-1, muscle ring finger-1; PPARs, peroxisome proliferator-activated receptors.
Omega-3 PUFAs EPA and DHA, both as stand-alone and synergically with amino acids ingestion, seem to directly stimulate mTORC1 thus enhancing muscle protein synthesis (Figure 3). However, it should be considered that while the acute activation of mTORC1 could promote muscle protein synthesis (48), the prolonged activation of mTORC1 has been associated with severe muscle atrophy, mainly because of decreased autophagy in the muscle (49). Therefore, it seems that alternating periods of high and low mTORC1 activation, as occurring with a healthy diet incorporating omega-3 PUFAs, is the key for an optimal muscle function (50). Omega-3 PUFAs seem also to improve mitochondrial function, mainly by reducing non-mitochondrial respiration and by augmenting the reserve respiratory capacity and bioenergetics (51). By reducing ROS production at the mitochondrial level, omega-3 PUFAs seem also to reduce muscle protein breakdown (47). Additionally, omega-3 PUFAs seem to counteract insulin resistance by improving mitochondrial function and bioenergetics as well as by modulating phospholipid membranes (52, 53), but also by increasing serum levels of insulin-like growth factor 1 (IGF-1). In turn, IGF-1 stimulates muscle protein synthesis via mTORC1-dependent and independent pathways (47, 54).
Omega-3 PUFAs could inhibit muscle protein breakdown also by acting as ligands for G-protein coupled receptors (GPCRs) and by activating the peroxisome proliferator-activated receptors (PPARs), with the consequent inhibition of nuclear factor kappa B (NFκB). In turn, the inhibition of NFκB leads to a reduced cyclooxygenase production resulting in a decreased inflammatory response (55) (Figure 3). The inhibition of NF-κB also leads to the downregulation of the muscle ring finger-1 (MuRF-1) gene counteracting the ubiquitin-proteasome system and thus reducing muscle protein breakdown (47). Furthermore, PPARs which are transcription factors activated by fatty acids and their derivatives, are involved in development, metabolism, inflammation, and many cellular processes in different tissues including the muscle (56). In particular, there are three different PPAR isotypes: (1) PPARα is highly expressed in tissues, like skeletal muscle, with effective fatty acid catabolism; (2) PPARβ/δ, which is more ubiquitously with a predominance in the skeletal muscle, is implicated in energy metabolism, mitochondrial biogenesis, and fiber-type switching; (3) PPARγ is highly expressed in adipocytes, but it is also involved in fat deposition in the muscle (56). Indeed, beyond NF-κB inhibition, PPARγ activation seems to play a relevant role in the inhibition of myosteatosis (i.e., intramuscular and intermuscular fat infiltration) and muscle fiber type switching (56) which are key features in the age-related sarcopenia (1). In particular, fat deposition in the muscle with its lipotoxic action, can exert detrimental effects on both muscle quality and strength, also negatively affecting mobility function (57–59). These effects are even more magnified when sarcopenia is accompanied by obesity (60). Additionally, PPARγ is a key regulator of glucose homeostasis and insulin sensitivity in the human skeletal muscle (61), with abnormalities in its expression being involved in skeletal muscle insulin resistance, especially in the presence of obesity and/or type II diabetes (62). The effects of omega-3 PUFAs supplementation on PPARγ activity have been demonstrated also in young athletes (e.g., age range of 20 to 30 years) who were supplemented with 2000 mg/day of omega-3 PUFAs (EPA: 360 mg, DHA: 240 mg) or placebo (2000 mg/day edible paraffin) for 3 weeks (63). The authors found that omega-3 PUFAs supplementation was significantly associated with the up-regulation of PPARγ, with an increase in resting energy expenditure and appetite (63). Also a recent meta-analysis of randomized controlled trials (RCTs) (64), involving both young, middle-aged and older people, showed that omega-3 PUFAs supplementation at varying doses (from 2000 mg/day to 7,000 mg/day) and with varying duration (from 3 to 48 weeks) led to a significant up-regulation of PPAR-γ gene expression. Finally, the incorporation of omega-3 PUFAs in the phospholipid bilayers of the cell membrane favors membrane fluidity and modulates neuromuscular transmission (Figure 3) resulting in greater muscle strength (47, 65–67).
Physical performance measures
The assessment of physical performance in older people can be envisioned as a summary marker of functional status as well as of the underlying biology of ageing (8). Tests of physical performance are strongly associated with frailty, disability and death in older people (9–14) and are used to identify the severity of sarcopenia (3). Physical performance measures are thus intended to monitor the evolution of functional status over time or the change after an intervention (68, 69), so such tests are often used as an outcome measure in most trials (3). Much research has been conducted in large, prospective studies of older populations, assessing physical performance in several ways. The main tests of physical performance in older people are summarized in Table 1. Physical performance is usually measured in older people by the Short Physical Performance Battery (SPPB) (11, 72), the 400-meter walk test (400-MWT) (74), gait speed (70, 71), and the Timed-Up and Go (TUG) test (73), as suggested by the EWGSOP2 (3). Shortly, the SPPB test combines the assessment of gait speed, a balance test, and a chair stand test. The SPPB scores range from 0 to 12, with a score of ≤8 points indicating poor physical performance (11, 72). However, the SPPB is frequently used in research rather than in clinical practice because of its length of administration (i.e., at least 10 min) (3). The 400-MWT evaluates both walking ability and endurance and consists of completing 20 laps of 20 m as fast as possible, with up to two rest stops during the test that are allowed. Non-completion or ≥6 min for completion of this test indicates poor physical performance (74). Also in this case, the length of the 400-MWT as well as the need for a corridor at least 20 m long make it difficult to implement in routine clinical practice. However, in the geriatric context, some tests with shorter distances (e.g., 4, 7, and 10 Meter Walk Test) have been proposed as good alternatives showing high test–retest reliability and validity in measuring walking speed (76–78). However, also the 10-meter walk test (10-MWT) requires a corridor 20 m long making it difficult to implement in most clinical settings (79). Indeed, the 4-meter walk test (4-MWT), which is part of the SPPB test, is considered a valid alternative to the 10-MWT in both clinical and research settings (3, 80), with a cut-off ≤0.8 m/s that has been advised to indicate poor physical performance (i.e., severe sarcopenia) (3). Gait speed is instead considered an easy-to-implement highly reliable measure and it is advised, for its convenience, by EWGSOP2 for physical performance assessment (3). Likewise, the TUG test is widely used in the geriatric context for its simplicity and reliability. In particular, the TUG test asks the participant to rise from a chair, walk up to a marker 3 m away, turn around, walk back to the chair and sit down again, with a cut-off of ≥20 s suggested as indicative of poor physical performance (3, 73). To better capture the age-related modifications in functional status, physical performance should be assessed before reaching old age, taking into consideration the determinants that influence it over one’s lifetime (8). In this way, to intervene earlier in life could slow the rate of functional decline associated with aging. There is a gap in understanding early-life factors influencing late-life physical performance (8). Furthermore, there is a paucity of measures for assessing physical performance in young people as well as the fact that physical performance is rarely assessed in young individuals. Until now, tests of physical performance such as the TUG test or the 10-MWT have been used in pediatric populations with specific pathological conditions (e.g., Down Syndrome (81, 82) or neuromuscular disease (83–85)). These tests, typically employed in the geriatric population, could therefore be applied to younger populations (i.e., young adults) to evaluate physical performance despite different cut-offs may be needed.
Table 1.
Main measures of physical performance in older people.
| Measure | Description | Cut-off points |
|---|---|---|
| Gait speed (70, 71) | Commonly assessed through a 4-MWT. Other distances (e.g., 7 and 10 meters) have also been proposed | ≤0.8 m/s |
| SPPB (11, 72) | Composite test including assessment of gait speed, a balance test and a chair stand test | ≤8 point score |
| TUG (73) | The person is asked to rise from a standard chair, walk to a marker 3 m away, turn around, walk back and sit down again | ≥20 s |
| 400-MWT (74) | The person is asked to complete 20 laps of 20 m, each lap as fast as possible with up to 2 rest stops during the test | Non-completion or ≥6 min for completion |
| 6-MWT (75) | The test is self-paced, with standardized instructions and encouragement being given as patients walk as far as possible over 6 min through a flat corridor | <400 m |
4-MWT, 4 meter walk test; SPPB, short physical performance battery; TUG, timed up and go; 400-MWT, 400-meter walk test; 6-MWT, 6-min walk test.
Omega-3 PUFAs and physical performance in early life (childhood and adolescence)
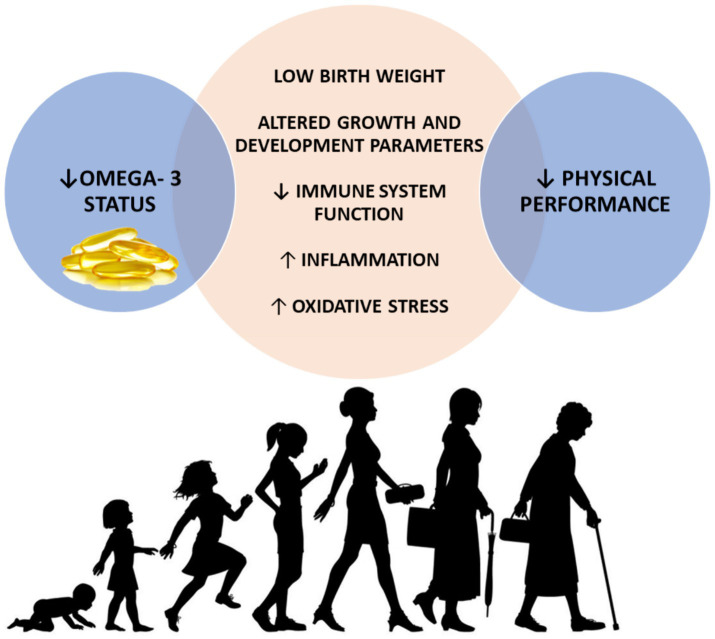
As the global population continues to age, there is a growing need to identify modifiable factors throughout life that influence physical function in later years. These factors may influence the peak of function achieved earlier in life determining the timing and rate of subsequent decline (Figure 1). Literature about the role of omega-3 PUFAs on physical performance in early life is scarce, although beneficial effects of these compounds on sport performance of young athletes have been reported (86, 87). Notwithstanding, some potential mechanisms by which PUFAs could exert beneficial effects on physical performance starting from early life could be argued (Figure 4).
Figure 4.
Possible mechanisms mediating the associations between low omega-3 status during early life and physical performance decline later in life. Decreased omega-3 status has been associated with low birth weight, altered growth and development parameters in early life and decreased immune function, augmented inflammation and oxidative stress across the lifespan. In turn, all these mechanisms have been largely associated with poor physical performance during older life. ↓, decreased; ↑, increased.
The role of the immune system and inflammatory processes throughout the lifespan, including early and in-utero life, has gained growing attention as a driver of a wide spectrum of age-related chronic conditions including metabolic syndrome, type 2 diabetes, cardiovascular disease, osteoporosis and sarcopenia (88). Systemic chronic inflammation, even during childhood and pregnancy, has been reported to influence the inflammatory trajectories in later stages of life (59, 88, 89). Conversely, inflammation, defined as the elevation of pro-inflammatory cytokines (i.e., C-reactive protein, interleukin-6), has been associated with poor physical performance in both older individuals (90, 91) and young adults (i.e., sedentary young adults aged 18–35 years) (92). Inflammation could be regarded as an early determinant of the physical performance decline seen with aging, starting from childhood and even from pregnancy. Starting from pregnancy, the so-called “maternal exposome” (i.e., diet, physical activity, psychological stress and exposure to xenobiotics) influences the immune system programming of the offspring towards a more pro-inflammatory profile in adulthood (88). Poor nutrition during early life (i.e., both undernutrition and overweight and obesity) has been associated with increased levels of inflammatory markers and with consequences during adult life including cardiometabolic disease and sarcopenia (93). The omega-3 PUFAs EPA and DHA are able to partially inhibit many aspects of inflammation, including leukocyte chemotaxis, adhesion molecule expression and leukocyte-endothelial adhesive interactions, production of eicosanoids such as prostaglandins and leukotrienes from the AA, and production of pro-inflammatory cytokines (30). In this context, omega-3 supplementation during pregnancy contributes to increase omega-3 PUFAs status of the offspring (94) and influence immunological outcomes through the modification of offspring cytokine concentrations (95, 96). See et al. (97) reported for the first time that omega-3 PUFAs supplementation during pregnancy was associated with an increase in specialized pro-resolving mediators precursors in the cord blood of the offspring at birth, suggesting a beneficial role in the alleviation of low-grade inflammatory status associated with pregnancy. However, the authors found the effects were not sustained at 12 years of age highlighting that the continuation of supplementation across life course may be also a relevant factor. This is because the effects of omega-3 fatty acid consumption might require a more prolonged and continuous intervention to observe a sustained difference in pro-resolving mediators as the half-life of EPA, DHA and the resolvins is in the hour range (98, 99). The time windows (i.e., at birth and at 12 years of age), used in the study of See et al. (97), have probably been chosen because those life stages can be envisioned as critical and sensitive periods of human development, according to Barker’s ‘developmental origins of health and disease’ hypothesis (100). This theory proposes that factors that modify physiological processes during the critical developmental period in early life may exert a long-term influence on disease in adult life. In particular, early life nutritional exposures, especially during critical or sensitive periods, are significant determinants of both growth and development and later health (100). Specifically, omega-3 PUFAs supplementation during pregnancy seems to increase omega-3 PUFAs status of the newborn (94), influencing immune function by acting on cytokine concentrations (95, 96) and attenuating lipid peroxidation in the newborn (101).Various RCTs involving children and adolescents with specific pathological conditions (i.e., autism spectrum disorder, attention-deficit-hyperactivity disorder, and cystic fibrosis) have demonstrated the role of omega-3 PUFAs in countering pro-inflammatory mediators after birth (102–104).
On the other hand, low birth weight as well as altered physical growth and development parameters (at the age of 1, 7, and 12 years, respectively), have been associated with poor grip strength and physical performance in mid-to-later life (i.e., at the age of 53 and 56 years for mid-life and at the age of 65–70 years for later life) (8, 105–109). Muscle strength is a major determinant of the age-related decline of physical performance (106), as shown in Figure 1. Indeed, incorporating lifestyle modifications to maximize the peak of muscle functional capacities during early life is functional to preserve physical performance in mid-to-later life. Exploring the potential of omega-3 PUFAs to positively affect muscle strength from early life by influencing birth weight and parameters related to growth and development could be of significant interest. In this regard, a longer duration of breastfeeding has been associated with both greater grip strength in older life (110) and increased lower body explosive strength in adolescence (111). The beneficial effects of breastfeeding on grip strength could probably be mediated by breast milk fatty acids content. This is of particular interest since achieving a higher peak in muscle strength starting from early life is directly associated with a lower decline in muscle strength and, consequently, in physical performance being the latter strongly influenced by muscle strength (3, 106). Human milk contains essential dietary fatty acids such as LA and ALA, along with their metabolites AA and DHA, which play a supportive role in the growth and development of breastfed infants (112). The amount of omega-6 and omega-3 fatty acids secreted in the milk is reflective of the maternal dietary intake of PUFAs (112). The hypothesis that omega-3 PUFAs supplementation could prevent preterm birth and low birth weight has originated from studies conducted in the Faroe Islands (113). In these islands, the diet is characterized by a greater intake of marine foods compared with the population of Denmark. This likely accounts for the higher birth weights (approximately 200 g more at term) observed in babies born in this area. Furthermore, birth weights of infants from the Faroe Islands have been found to be higher than those of 33 other countries (113).
From a life course perspective, another factor to be considered is obesity (and in particular adiposity). Maternal obesity has been associated with increased fetal adiposity, especially when accompanied by gestational diabetes (93). Nutritional excess during early childhood (i.e., greater gestational weight gain, higher birth weight, faster postnatal weight gain) is associated with an increased risk of obesity, central adiposity as well as insulin resistance in adult and older life (from 20 till 70 years of age) (93, 114). Subsequently, excess weight gain during childhood and adolescence period is likely to lead to persistent overweight and obesity throughout life (115).
In this context, the role of chronic inflammation should not be overlooked since increased adiposity is characterized by the abnormal secretion of a wide range of pro-inflammatory molecules including adipokines, cytokines and chemokines thus predisposing to adult adverse conditions although inflammation is a necessary biological response to various stimuli, having defense and tissue restructuring functions (88, 116). Inflammatory trajectories across the life course could be thus probably mediated by body composition alterations as both undernutrition and overweight are associated with inflammation (93, 117, 118). In turn, obesity status, either independently or in combination with sarcopenia, has been associated with reduced physical performance in older individuals (119). Based on these considerations, omega-3 PUFAs have been suggested to play a role in the context of overweight/obesity through numerous mechanisms including the modulation of lipid metabolism and inflammation, the regulation of adipokines as well as the promotion of adipogenesis and the alteration of epigenetic mechanisms (120). A reduced red blood cell omega-3 PUFAs status has been reported in children with greater adiposity and has been associated with a suboptimal intake of omega-3 PUFAs (121). In this context, a plausible explanation may be also related to the evolution of the Western diet towards a pro-inflammatory diet rich in refined grains and ultra-processed foods and low in fruits and vegetables, thus poor in vitamins, minerals and with a suboptimal omega-3 content in favor of omega-6 PUFAs (88). However, no significant effects of omega-3 PUFAs supplementation on anthropometric parameters have been reported in children and adolescents living with overweight/obesity (122, 123).
Lower socioeconomic position (SEP) has been associated with lower serum levels of omega-3 PUFAs starting from pregnancy through adulthood (124–129). Robinson et al. (130) in a multi-cohort analysis, reported that a low SEP was independently associated with an unfavorable metabolic profile including low omega-3 status both in children (i.e., aged 7 years), adolescents (i.e., aged 15 and 17 years), adults and older adults (from 31 till 75 years of age). This is probably due to the poor quality of the diet associated with a lower socioeconomic status as reported in ethnic minorities (i.e., Latino immigrants in the U.S.), but also in urban areas of Australia (129, 131) with a reduced consumption of fruits, vegetables, whole grains, fiber, fish and seafood thus reflective of low omega-3 status (132). Additionally it should be considered that low levels and intake of omega-3 may in part be related to the limited accessibility of marine-food sources, especially in certain geographic areas (129). In a systematic review and meta-analysis, Birnie et al. (133) reported an association between lower childhood SEP and reduced physical performance in adulthood and older life (from 18 to 79 years). This connection persisted even after adjustment by adult SEP, despite the presence of heterogeneity among studies. These findings suggest that the accumulation of adverse exposures across the life course may be more predictive of the functional decline observed during aging than models considering only adult factors. It can be assumed that the association between low childhood SEP and reduced physical performance in adult and older life may be mediated, in addition to other adversities, by a poor quality of the diet, including inadequate omega-3 PUFAs intake.
It has been documented that attainment of gross motor development milestones (i.e., standing and walking) during childhood, as well as higher scores on tests measuring cognitive ability and motor coordination, are associated with enhanced physical performance in midlife, independently of other factors (8). In particular, Kuh et al. showed that the age at which an individual first walked was associated with both midlife standing balance and chair stand test, which are two out of three components of the Short Physical Performance Battery (SPPB) (8). The authors reported that better scores on cognitive ability tests at age 8 years and of motor coordination at age 15 years were associated with greater standing balance and chair standing (8). The attainment and maturation of motor and cognitive function during childhood, as well as the age-related motor and cognitive functional decline in older life, are highly integrated (134, 135), indicating that these developmental factors may be envisioned as markers of more complex cortical–subcortical neural circuits connected with higher levels of function later in life (8). This aligns with the findings of Ridler et al., who showed an anatomically related overlap between fronto-cerebellar system related to infant motor development and adult executive function (136). Similarly, Murray et al. reported that early development in the gross motor domain is associated with higher adult executive function (137). In this regard, omega-3 PUFAs are widely acknowledged to play a central role in brain function and contribute to the structure of the neuronal cell membranes (138). They are crucial for myelination and vision development during the perinatal period (139). In particular, DHA represents nearly 90% of total omega-3 PUFAs in the brain and is especially concentrated in the gray matter (140, 141). Early life accumulation of omega-3 PUFAs represents a golden opportunity for their storage in neural tissues (38, 140–142). In this context, it has been demonstrated that omega-3 PUFAs supplementation during pregnancy is associated with earlier achievement of gross motor milestones and improved cognitive development in children (143). The study by Beblo et al. (144) reported that fish oil supplementation enhanced omega-3 PUFAs levels and improved motor skills in children with phenylketonuria. Additionally, Agostoni et al. (145) in a RCT, demonstrated that infants who received DHA supplementation achieved sitting without support in a shorter period. Other studies reported contrasting results. A systematic review by U.S. Departments of Agriculture nutrition evidence reported insufficient evidence to establish a relationship between omega-3 supplementation during pregnancy and lactation with motor and visual development in infants (146). Richardson and Montgomery (147) found that in children with development coordination disorder, PUFAs supplementation (i.e., 2 capsules 3 times/day providing 558 mg of EPA, 174 mg of DHA and 60 mg of LA for 3 months) did not improve motor function, while they improved reading and spelling age and symptoms of attention-deficit/hyperactivity disorder.
In summary, the role of omega-3 PUFAs starting from early life, and even in utero, is intriguing given their long-lasting effects on human health through the various mechanisms discussed (e.g., birth weight, motor development, modulation of inflammation, immune response and oxidative stress) which could probably influence adult physical performance, with potential implications for the prevention of sarcopenia, frailty and disability.
Omega-3 PUFAs and physical performance in mid to later life
Growing clinical evidence supports the positive role of omega-3 PUFAs on physical performance in mid to later life (148–150). Some studies focused on the relationship between omega-3 PUFAs supplementation and muscle strength (27, 151). As shown in Figure 1, with advancing age muscle strength tends to decline earlier and more rapidly than physical performance, especially when a lower peak in muscle strength is reached during early life. According to the latest consensus guidelines of the EWGSOP2, in the early phases of sarcopenia development, a person may result above the threshold of low physical performance despite a reduction in muscle strength (3). The reduction in muscle strength can be considered an early indicator of overt functional decline. This is evidenced by the EWGSOP2 algorithm for sarcopenia case finding where low muscle strength represents the first step in sarcopenia assessment defining probable sarcopenia and low physical performance the last step to quantify sarcopenia severity (3). Muscle strength can be thus considered as the early component, on which acting, to preserve muscle function and thus physical performance during older life. In this regard, a recent meta-analysis showed a beneficial effect of omega-3 PUFAs supplementation on lower body muscle strength while no effects were found on upper body strength (151). Bird et al. (152), in a recent meta-analysis, reported a significant relationship in favor of omega-3 PUFAs supplementation for quadriceps maximal voluntary capacity. Another meta-analysis by Rondanelli et al. (153) found no effects of omega-3 EPA plus DHA supplementation on chair rise test and handgrip strength. On the other hand, a meta-analysis of 9 RCTs showed that omega-3 PUFAs supplementation significantly increased the grip strength (154). In the Hertfordshire cohort study, Robinson et al. found a positive association between fatty fish consumption and grip strength (155). Regarding physical performance, in 2017, Frison et al. (150) reported that higher omega-3 PUFAs plasma levels were associated with lower odds of low gait speed (i.e., <0.63 m/s) in older individuals. In a cross-sectional analysis of the Multidomain Alzheimer Preventive Trial (MAPT), recruiting older adults aged 70 years and older, Fougère et al. (156) found an association between low levels of omega-3 PUFAs in red blood cell membranes and lower physical performance measured through the SPPB. However, in a secondary analysis of the MAPT trial, Rolland et al. (157) reported no significant effects of long-term omega-3 PUFAs supplementation, either alone or in combination with a multidomain lifestyle intervention comprising physical activity counseling, on the walking speed test and SPPB.
In the InCHIANTI study, including 1,273 participants between 22 and 104 years of age living in Tuscany (Italy), Abbatecola et al. (148) found that higher levels of total PUFAs, omega-3 PUFAs, and omega-6 PUFAs were associated with high physical performance (i.e., SPPB score > 9) at baseline, after adjusting for age. However, after adjusting for potential confounders, baseline 7 m walk time was associated with total PUFAs levels. Additionally, the authors found that baseline omega-3 PUFAs levels were inversely associated to the risk of developing a decline in SPPB to scores ≤9, while the omega-6/omega-3 ratio was associated with a higher risk of SPPB decline and with a longer time to walk 7 meters.
Hutchins-Wiese et al. (158), in a RCT recruiting 126 postmenopausal women, demonstrated that omega-3 PUFAs supplementation resulted in greater physical performance, measured by change in walking speed. On contrary, Krzymińska-Siemaszko et al. (159) did not observe an improvement in physical performance after 12 weeks of omega-3 PUFAs supplementation in a sample of older people with low muscle mass. A recent meta-analysis of RCTs in older adults (153), reported that daily omega-3 PUFAs supplementation is associated with a reduction in the time of the TUG test, while no statistically significant effect was found on 4-MWT. These results are in line with another recent meta-analysis (151), focused on people aged 55 years and older, which reported a significant association between omega-3 supplementation and lower TUG but not on walking speed. However, in another systematic review and meta-analysis, it was found that there were minor benefits of omega-3 supplementation for TUG performance, while subgroup analyses showed that omega-3 PUFAs supplements at more than 2 g/day may contribute at improving walking speed, especially if the intervention is carried out for more than 6 months (160).
In summary, evidence from interventional studies and meta-analyses gave controversial results on the beneficial effect of omega-3 PUFAs on physical performance parameters. As outlined by some authors, small study size and heterogeneity in the intervention protocol, including the ratios between EPA and DHA, may have limited the applicability of these results.
Conclusion
Mechanisms through which omega-3 PUFAs could benefit muscle function including physical performance parameters across the life course are intriguing. However, it should be considered that few interventional studies explored the effects of omega-3 PUFAs supplementation on physical performance, with varying duration, dosage and use (i.e., alone or in combination with other interventions). This has led to controversial results reported in literature. However, it seems that omega-3 PUFAs supplementation at high doses (i.e., more than 2 g/day) and for longer periods (i.e., for more than 6 months) may contribute to improving physical performance (e.g., walking speed) in older people. Larger and high-quality RCTs are needed to fully elucidate the beneficial effects of omega-3 PUFAs supplementation on muscle function parameters. Although, a direct association in early life is not available in literature, some mechanisms by which omega-3 PUFAs may contribute to improved physical performance could be hypothesized. The integration of physical function measures in future RCTs would be of great interest to explore whether omega-3 PUFAs could contribute to improved muscle function parameters, starting from early life and extending throughout the lifespan.
Author contributions
DA: Writing – original draft, Writing – review & editing. CB: Writing – original draft, Writing – review & editing. VC: Writing – review & editing. GS: Writing – review & editing. CA: Writing – review & editing. TL: Writing – review & editing. AM: Writing – review & editing.
Funding Statement
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This research was partially funded by a contribution from the Italian Ministry of Health (ricerca corrente).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet. (2019) 393:2636–46. doi: 10.1016/S0140-6736(19)31138-9 [DOI] [PubMed] [Google Scholar]
- 2.Sayer AA, Syddall H, Martin H, Patel H, Baylis D, Cooper C. The developmental origins of sarcopenia. J Nutr Health Aging. (2008) 12:427–32. doi: 10.1007/BF02982703, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. (2019) 48:16–31. doi: 10.1093/ageing/afy169, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sayer AA, Cruz-Jentoft A. Sarcopenia definition, diagnosis and treatment: consensus is growing. Age Ageing. (2022) 51:e220. doi: 10.1093/ageing/afac220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hall KS, Cohen HJ, Pieper CF, Fillenbaum GG, Kraus WE, Huffman KM, et al. Physical performance across the adult life span: correlates with age and physical activity. J Gerontol A. (2017) 72:572–8. doi: 10.1093/gerona/glw120129-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beaudart C, Rolland Y, Cruz-Jentoft AJ, Bauer JM, Sieber C, Cooper C, et al. Assessment of muscle function and physical performance in daily clinical practice: a position paper endorsed by the European Society for Clinical and Economic Aspects of osteoporosis, osteoarthritis and musculoskeletal diseases (ESCEO). Calcif Tissue Int. (2019) 105:1–14. doi: 10.1007/s00223-019-00545-w [DOI] [PubMed] [Google Scholar]
- 7.Azzolino D, Alkahtani S, Cesari M. Definitions of sarcopenia across the world. Veronese N, Beaudart C, Sabico S, (Eds.) Sarcopenia: Research and clinical implications. Cham: Springer International Publishing; (2021), 17–26 [Google Scholar]
- 8.Kuh D, Hardy R, Butterworth S, Okell L, Richards M, Wadsworth M, et al. Developmental origins of midlife physical performance: evidence from a British birth cohort. Am J Epidemiol. (2006) 164:110–21. doi: 10.1093/aje/kwj193, PMID: [DOI] [PubMed] [Google Scholar]
- 9.Stel VS, Pluijm SMF, Deeg DJH, Smit JH, Bouter LM, Lips P. Functional limitations and poor physical performance as independent risk factors for self-reported fractures in older persons. Osteoporos Int. (2004) 15:742–50. doi: 10.1007/s00198-004-1604-7, PMID: [DOI] [PubMed] [Google Scholar]
- 10.Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. (2000) 55:M221–31. doi: 10.1093/gerona/55.4.M221, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. (1995) 332:556–62. doi: 10.1056/NEJM199503023320902, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Onder G, Penninx BWJH, Ferrucci L, Fried LP, Guralnik JM, Pahor M. Measures of physical performance and risk for progressive and catastrophic disability: results from the Women’s health and aging study. J Gerontol A Biol Sci Med Sci. (2005) 60:74–9. doi: 10.1093/gerona/60.1.74, PMID: [DOI] [PubMed] [Google Scholar]
- 13.Wolinsky FD, Miller DK, Andresen EM, Malmstrom TK, Miller JP. Further evidence for the importance of subclinical functional limitation and subclinical disability assessment in gerontology and geriatrics. J Gerontol B Psychol Sci Soc Sci. (2005) 60:S146–51. doi: 10.1093/geronb/60.3.S146, PMID: [DOI] [PubMed] [Google Scholar]
- 14.Melzer D, Lan TY, Guralnik JM. The predictive validity for mortality of the index of mobility-related limitation-results from the EPESE study. Age Ageing. (2003) 32:619–25. doi: 10.1093/ageing/afg107, PMID: [DOI] [PubMed] [Google Scholar]
- 15.Cesari M, Landi F, Vellas B, Bernabei R, Marzetti E. Sarcopenia and physical frailty: two sides of the same coin. Front Aging Neurosci. (2014) 6:192. doi: 10.3389/fnagi.2014.00192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abellan van Kan G, Rolland Y, Andrieu S, Bauer J, Beauchet O, Bonnefoy M, et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an international academy on nutrition and aging (IANA) task force. J Nutr Health Aging. (2009) 13:881–9. doi: 10.1007/s12603-009-0246-z, PMID: [DOI] [PubMed] [Google Scholar]
- 17.Theou O, Brothers TD, Peña FG, Mitnitski A, Rockwood K. Identifying common characteristics of frailty across seven scales. J Am Geriatr Soc. (2014) 62:901–6. doi: 10.1111/jgs.12773, PMID: [DOI] [PubMed] [Google Scholar]
- 18.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. (2001) 56:M146–57. doi: 10.1093/gerona/56.3.M146 [DOI] [PubMed] [Google Scholar]
- 19.Daly RM, Iuliano S, Fyfe JJ, Scott D, Kirk B, Thompson MQ, et al. Screening, diagnosis and Management of Sarcopenia and Frailty in hospitalized older adults: recommendations from the Australian and new Zealand Society for Sarcopenia and Frailty Research (ANZSSFR) expert working group. J Nutr Health Aging. (2022) 26:637–51. doi: 10.1007/s12603-022-1801-0 [DOI] [PubMed] [Google Scholar]
- 20.Hughes VA, Frontera WR, Roubenoff R, Evans WJ, Singh MAF. Longitudinal changes in body composition in older men and women: role of body weight change and physical activity. Am J Clin Nutr. (2002) 76:473–81. doi: 10.1093/ajcn/76.2.473, PMID: [DOI] [PubMed] [Google Scholar]
- 21.Bloom I, Shand C, Cooper C, Robinson S, Baird J. Diet quality and sarcopenia in older adults: a systematic review. Nutrients. (2018) 10:308. doi: 10.3390/nu10030308, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dent E, Morley JE, Cruz-Jentoft AJ, Arai H, Kritchevsky SB, Guralnik J, et al. International clinical practice guidelines for sarcopenia (ICFSR): screening, diagnosis and management. J Nutr Health Aging. (2018) 22:1148–61. doi: 10.1007/s12603-018-1139-9, PMID: [DOI] [PubMed] [Google Scholar]
- 23.Damanti S, Azzolino D, Roncaglione C, Arosio B, Rossi P, Cesari M. Efficacy of nutritional interventions as stand-alone or synergistic treatments with exercise for the Management of Sarcopenia. Nutrients. (2019) 11:1991. doi: 10.3390/nu11091991, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G. Hallmarks of aging: an expanding universe. Cell. (2023) 186:243–78. doi: 10.1016/j.cell.2022.11.001, PMID: [DOI] [PubMed] [Google Scholar]
- 25.Ferguson EJ, Seigel JW, McGlory C. Omega-3 fatty acids and human skeletal muscle. Curr Opin Clin Nutr Metab Care. (2021) 24:114–9. doi: 10.1097/MCO.0000000000000723 [DOI] [PubMed] [Google Scholar]
- 26.Zhang Y, Guo H, Liang J, Xiao W, Li Y. Relationship between dietary Omega-3 and Omega-6 polyunsaturated fatty acids level and sarcopenia. A meta-analysis of observational studies. Front Nutr. (2022) 8:738083. doi: 10.3389/fnut.2021.738083, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dupont J, Dedeyne L, Dalle S, Koppo K, Gielen E. The role of omega-3 in the prevention and treatment of sarcopenia. Aging Clin Exp Res. 31:825. doi: 10.1007/s40520-019-01146-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Azzolino D, Coelho-Junior HJ, Proietti M, Manzini VM, Cesari M. Fatigue in older persons: the role of nutrition. Proc Nutr Soc. (2023) 82:39–46. doi: 10.1017/S0029665122002683, PMID: [DOI] [PubMed] [Google Scholar]
- 29.Kiecolt-Glaser JK, Epel ES, Belury MA, Andridge R, Lin J, Glaser R, et al. Omega-3 fatty acids, oxidative stress, and leukocyte telomere length: a randomized controlled trial. Brain Behav Immun. (2013) 28:16–24. doi: 10.1016/j.bbi.2012.09.004, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Calder PC. Omega-3 fatty acids and inflammatory processes: from molecules to man. Biochem Soc Trans. (2017) 45:1105–15. doi: 10.1042/BST20160474, PMID: [DOI] [PubMed] [Google Scholar]
- 31.Calder PC. Mechanisms of action of (n-3) fatty acids. J Nutr. (2012) 142:592S–9S. doi: 10.3945/jn.111.155259 [DOI] [PubMed] [Google Scholar]
- 32.Arterburn LM, Hall EB, Oken H. Distribution, interconversion, and dose response of n-3 fatty acids in humans. Am J Clin Nutr. (2006) 83:1467S–76S. doi: 10.1093/ajcn/83.6.1467S, PMID: [DOI] [PubMed] [Google Scholar]
- 33.Djuricic I, Calder PC. Beneficial outcomes of Omega-6 and Omega-3 polyunsaturated fatty acids on human health: an update for 2021. Nutrients. (2021) 13:2421. doi: 10.3390/nu13072421, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Glaser C, Heinrich J, Koletzko B. Role of FADS1 and FADS2 polymorphisms in polyunsaturated fatty acid metabolism. Metabolism. (2010) 59:993–9. doi: 10.1016/j.metabol.2009.10.022, PMID: [DOI] [PubMed] [Google Scholar]
- 35.Lauritzen L, Brambilla P, Mazzocchi A, Harsløf LBS, Ciappolino V, Agostoni C. DHA effects in brain development and function. Nutrients. (2016) 8:6. doi: 10.3390/nu8010006, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.SanGiovanni JP, Chew EY. The role of omega-3 long-chain polyunsaturated fatty acids in health and disease of the retina. Prog Retin Eye Res. (2005) 24:87–138. doi: 10.1016/j.preteyeres.2004.06.002, PMID: [DOI] [PubMed] [Google Scholar]
- 37.Cetin I, Alvino G, Cardellicchio M. Long chain fatty acids and dietary fats in fetal nutrition. J Physiol. (2009) 587:3441–51. doi: 10.1113/jphysiol.2009.173062, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Carver JD, Benford VJ, Han B, Cantor AB. The relationship between age and the fatty acid composition of cerebral cortex and erythrocytes in human subjects. Brain Res Bull. (2001) 56:79–85. doi: 10.1016/S0361-9230(01)00551-2, PMID: [DOI] [PubMed] [Google Scholar]
- 39.Hulbert AJ, Turner N, Storlien LH, Else PL. Dietary fats and membrane function: implications for metabolism and disease. Biol Rev Camb Philos Soc. (2005) 80:155–69. doi: 10.1017/S1464793104006578 [DOI] [PubMed] [Google Scholar]
- 40.Echeverría F, Valenzuela R, Catalina Hernandez-Rodas M, Valenzuela A. Docosahexaenoic acid (DHA), a fundamental fatty acid for the brain: new dietary sources. Prostaglandins Leukot Essent Fatty Acids. (2017) 124:1–10. doi: 10.1016/j.plefa.2017.08.001, PMID: [DOI] [PubMed] [Google Scholar]
- 41.Troesch B, Eggersdorfer M, Laviano A, Rolland Y, Smith AD, Warnke I, et al. Expert opinion on benefits of long-chain Omega-3 fatty acids (DHA and EPA) in aging and clinical nutrition. Nutrients. (2020) 12:2555. doi: 10.3390/nu12092555, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gutiérrez S, Svahn SL, Johansson ME. Effects of Omega-3 fatty acids on immune cells. Int J Mol Sci. (2019) 20:5028. doi: 10.3390/ijms20205028, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Eggersdorfer M, Berger MM, Calder PC, Gombart AF, Ho E, Laviano A, et al. Perspective: role of micronutrients and Omega-3 long-chain polyunsaturated fatty acids for immune outcomes of relevance to infections in older adults—a narrative review and call for action. Adv Nutr. (2022) 13:1415–30. doi: 10.1093/advances/nmac058, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McGlory C, Calder PC, Nunes EA. The influence of Omega-3 fatty acids on skeletal muscle protein turnover in health, disuse, and disease. Front Nutr. (2019) 6:144. doi: 10.3389/fnut.2019.00144, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Phillips N, Gray SR, Combet E, Witard OC. Long-chain n −3 polyunsaturated fatty acids for the management of age- and disease-related declines in skeletal muscle mass, strength and physical function. Curr Opin Clin Nutr Metab Care. (2024) 27:98–105. doi: 10.1097/MCO.0000000000000986, PMID: [DOI] [PubMed] [Google Scholar]
- 46.Tseng PT, Zeng BY, Zeng BS, Liao YC, Stubbs B, Kuo JS, et al. Omega-3 polyunsaturated fatty acids in sarcopenia management: a network meta-analysis of randomized controlled trials. Ageing Res Rev. (2023) 90:102014. doi: 10.1016/j.arr.2023.102014, PMID: [DOI] [PubMed] [Google Scholar]
- 47.Therdyothin A, Phiphopthatsanee N, Isanejad M. The effect of Omega-3 fatty acids on sarcopenia: mechanism of action and potential efficacy. Mar Drugs. (2023) 21:399. doi: 10.3390/md21070399, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bodine SC, Stitt TN, Gonzalez M, Kline WO, Stover GL, Bauerlein R, et al. Akt/mTOR pathway is a crucial regulator of skeletal muscle hypertrophy and can prevent muscle atrophy in vivo. Nat Cell Biol. (2001) 3:1014–9. doi: 10.1038/ncb1101-1014, PMID: [DOI] [PubMed] [Google Scholar]
- 49.Castets P, Lin S, Rion N, Di Fulvio S, Romanino K, Guridi M, et al. Sustained activation of mTORC1 in skeletal muscle inhibits constitutive and starvation-induced autophagy and causes a severe, late-onset myopathy. Cell Metab. (2013) 17:731–44. doi: 10.1016/j.cmet.2013.03.015, PMID: [DOI] [PubMed] [Google Scholar]
- 50.Saxton RA, Sabatini DM. mTOR signaling in growth, metabolism, and disease. Cell. (2017) 168:960–76. doi: 10.1016/j.cell.2017.02.004, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Borja-Magno AI, Furuzawa-Carballeda J, Guevara-Cruz M, Arias C, Granados J, Bourges H, et al. Supplementation with EPA and DHA omega-3 fatty acids improves peripheral immune cell mitochondrial dysfunction and inflammation in subjects with obesity. J Nutr Biochem. (2023) 120:109415. doi: 10.1016/j.jnutbio.2023.109415 [DOI] [PubMed] [Google Scholar]
- 52.Gao K, Chen L, Yang M, Han L, Yiguang S, Zhao H, et al. Marine n-3 PUFA protects hearts from I/R injury via restoration of mitochondrial function. Scand Cardiovasc J. (2015) 49:264–9. doi: 10.3109/14017431.2015.1071873, PMID: [DOI] [PubMed] [Google Scholar]
- 53.Lepretti M, Martucciello S, Burgos Aceves MA, Putti R, Lionetti L. Omega-3 fatty acids and insulin resistance: focus on the regulation of mitochondria and endoplasmic reticulum stress. Nutrients. (2018) 10:350. doi: 10.3390/nu10030350, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schiaffino S, Mammucari C. Regulation of skeletal muscle growth by the IGF1-Akt/PKB pathway: insights from genetic models. Skelet Muscle. (2011) 1:4. doi: 10.1186/2044-5040-1-4, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Blaauw R, Calder PC, Martindale RG, Berger MM. Combining proteins with n-3 PUFAs (EPA + DHA) and their inflammation pro-resolution mediators for preservation of skeletal muscle mass. Crit Care. (2024) 28:38. doi: 10.1186/s13054-024-04803-8, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Manickam R, Duszka K, Wahli W. PPARs and microbiota in skeletal muscle health and wasting. Int J Mol Sci. (2020) 21:8056. doi: 10.3390/ijms21218056, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Marcus RL, Addison O, Dibble LE, Foreman KB, Morrell G, Lastayo P. Intramuscular adipose tissue, sarcopenia, and mobility function in older individuals. J Aging Res. (2012) 2012:629637: 1–6. doi: 10.1155/2012/629637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Addison O, Marcus RL, Lastayo PC, Ryan AS. Intermuscular fat: a review of the consequences and causes. Int J Endocrinol. (2014) 2014:309570: 1–11. doi: 10.1155/2014/309570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Azzolino D, Spolidoro GCI, Saporiti E, Luchetti C, Agostoni C, Cesari M. Musculoskeletal changes across the lifespan: nutrition and the life-course approach to prevention. Front Med. (2021). doi: 10.3389/fmed.2021.697954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zamboni M, Rubele S, Rossi AP. Sarcopenia and obesity. Curr Opin Clin Nutr Metab Care. (2019) 22:13–9. doi: 10.1097/MCO.0000000000000519 [DOI] [PubMed] [Google Scholar]
- 61.Amin RH, Mathews ST, Camp HS, Ding L, Leff T. Selective activation of PPARgamma in skeletal muscle induces endogenous production of adiponectin and protects mice from diet-induced insulin resistance. Am J Physiol Endocrinol Metab. (2010) 298:E28–37. doi: 10.1152/ajpendo.00446.2009, PMID: [DOI] [PubMed] [Google Scholar]
- 62.Park KS, Ciaraldi TP, Abrams-Carter L, Mudaliar S, Nikoulina SE, Henry RR. PPAR-γ gene expression is elevated in skeletal muscle of obese and type II diabetic subjects. Diabetes. 46:1230. doi: 10.2337/diab.46.7.1230 [DOI] [PubMed] [Google Scholar]
- 63.Moradi S, Alivand M, KhajeBishak Y, AsghariJafarabadi M, Alipour M, Chilibeck PD, et al. The effect of omega3 fatty acid supplementation on PPARγ and UCP2 expressions, resting energy expenditure, and appetite in athletes. BMC Sports Sci Med Rehabil. (2021) 13:48. doi: 10.1186/s13102-021-00266-4, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Heshmati J. Effect of omega-3 fatty acid supplementation on gene expression of inflammation, oxidative stress and cardiometabolic parameters: systematic review and meta-analysis. J Funct Foods. (2021) 85:104619. doi: 10.1016/j.jff.2021.104619 [DOI] [Google Scholar]
- 65.Gerling CJ, Mukai K, Chabowski A, Heigenhauser GJF, Holloway GP, Spriet LL, et al. Incorporation of Omega-3 fatty acids into human skeletal muscle Sarcolemmal and mitochondrial membranes following 12 weeks of fish oil supplementation. Front Physiol. (2019) 10:348. doi: 10.3389/fphys.2019.00348, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Innis SM. Dietary (n-3) fatty acids and brain development. J Nutr. (2007) 137:855–9. doi: 10.1093/jn/137.4.855, PMID: [DOI] [PubMed] [Google Scholar]
- 67.Salem N, Litman B, Kim HY, Gawrisch K. Mechanisms of action of docosahexaenoic acid in the nervous system. Lipids. (2001) 36:945–59. doi: 10.1007/s11745-001-0805-6 [DOI] [PubMed] [Google Scholar]
- 68.Buckinx F, Aubertin-Leheudre M. Physical performance and muscle strength tests: pros and cons. Veronese N, Beaudart C, Sabico S, (Eds.) Sarcopenia: Research and clinical implications. Cham: Springer International Publishing; (2021), 65–99 [Google Scholar]
- 69.Cesari M, Bernabei R, Vellas B, Fielding RA, Rooks D, Azzolino D, et al. Challenges in the development of drugs for sarcopenia and frailty - report from the international conference on frailty and sarcopenia research (ICFSR) task force. J Frailty Aging. (2022) 11:135–42. doi: 10.14283/jfa.2022.30, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European working group on sarcopenia in older people. Age Ageing. (2010) 39:412–23. doi: 10.1093/ageing/afq034, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, et al. Gait speed and survival in older adults. JAMA. (2011) 305:50–8. doi: 10.1001/jama.2010.1923, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Pavasini R, Guralnik J, Brown JC, di Bari M, Cesari M, Landi F, et al. Short physical performance battery and all-cause mortality: systematic review and meta-analysis. BMC Med. (2016) 14:215. doi: 10.1186/s12916-016-0763-7, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bischoff HA, Stähelin HB, Monsch AU, Iversen MD, Weyh A, von Dechend M, et al. Identifying a cut-off point for normal mobility: a comparison of the timed ‘up and go’ test in community-dwelling and institutionalised elderly women. Age Ageing. (2003) 32:315–20. doi: 10.1093/ageing/32.3.315, PMID: [DOI] [PubMed] [Google Scholar]
- 74.Newman AB, Simonsick EM, Naydeck BL, Boudreau RM, Kritchevsky SB, Nevitt MC, et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA. (2006) 295:2018–26. doi: 10.1001/jama.295.17.2018, PMID: [DOI] [PubMed] [Google Scholar]
- 75.Morley JE, Abbatecola AM, Argiles JM, Baracos V, Bauer J, Bhasin S, et al. Sarcopenia with limited mobility: an international consensus. J Am Med Dir Assoc. (2011) 12:403–9. doi: 10.1016/j.jamda.2011.04.014, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Studenski S, Perera S, Wallace D, Chandler JM, Duncan PW, Rooney E, et al. Physical performance measures in the clinical setting. J Am Geriatr Soc. (2003) 51:314–22. doi: 10.1046/j.1532-5415.2003.51104.x [DOI] [PubMed] [Google Scholar]
- 77.Fritz S, Lusardi M. White paper: ‘walking speed: the sixth vital sign’. J Geriatr Phys Ther. (2009) 32:46–9. doi: 10.1519/00139143-200932020-00002, PMID: [DOI] [PubMed] [Google Scholar]
- 78.Peters DM, Fritz SL, Krotish DE. Assessing the reliability and validity of a shorter walk test compared with the 10-meter walk test for measurements of gait speed in healthy, older adults. J Geriatr Phys Ther. (2013) 36:24–30. doi: 10.1519/JPT.0b013e318248e20d, PMID: [DOI] [PubMed] [Google Scholar]
- 79.Nguyen AT, Nguyen HTT, Nguyen TX, Nguyen TN, Nguyen TTH, Nguyen AL, et al. Walking speed assessed by 4-meter walk test in the community-dwelling oldest old population in Vietnam. Int J Environ Res Public Health. (2022) 19:9788. doi: 10.3390/ijerph19169788, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Cabanas-Valdés R, García-Rueda L, Salgueiro C, Pérez-Bellmunt A, Rodríguez-Sanz J, López-de-Celis C. Assessment of the 4-meter walk test test-retest reliability and concurrent validity and its correlation with the five sit-to-stand test in chronic ambulatory stroke survivors. Gait Posture. (2023) 101:8–13. doi: 10.1016/j.gaitpost.2023.01.014, PMID: [DOI] [PubMed] [Google Scholar]
- 81.Sánchez-González JL, Llamas-Ramos I, Llamas-Ramos R, Molina-Rueda F, Carratalá-Tejada M, Cuesta-Gómez A. Reliability and validity of the 10-meter walk test (10MWT) in adolescents and young adults with down syndrome. Children. (2023) 10:655. doi: 10.3390/children10040655, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Nicolini-Panisson RD, Donadio MVF. Normative values for the timed ‘up and go’ test in children and adolescents and validation for individuals with down syndrome. Dev Med Child Neurol. (2014) 56:490–7. doi: 10.1111/dmcn.12290, PMID: [DOI] [PubMed] [Google Scholar]
- 83.de Baptista CRJA, Vicente AM, Souza MA, Cardoso J, Ramalho VM, Mattiello-Sverzut AC. Methods of 10-meter walk test and repercussions for reliability obtained in typically developing children. Rehabil Res Pract. (2020) 2020:4209812. doi: 10.1155/2020/4209812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Graser JV, Letsch C, van Hedel HJA. Reliability of timed walking tests and temporo-spatial gait parameters in youths with neurological gait disorders. BMC Neurol. (2016) 16:15. doi: 10.1186/s12883-016-0538-y, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pirpiris M, Wilkinson AJ, Rodda J, Nguyen TC, Baker RJ, Nattrass GR, et al. Walking speed in children and young adults with neuromuscular disease: comparison between two assessment methods. J Pediatr Orthop. (2003) 23:302–7. doi: 10.1097/01241398-200305000-00006, PMID: [DOI] [PubMed] [Google Scholar]
- 86.Thielecke F, Blannin A. Omega-3 fatty acids for sport performance—are they equally beneficial for athletes and amateurs? A narrative review. Nutrients. (2020) 12:3712. doi: 10.3390/nu12123712, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tomczyk M, Heileson JL, Babiarz M, Calder PC. Athletes can benefit from increased intake of EPA and DHA—evaluating the evidence. Nutrients. (2023) 15:4925. doi: 10.3390/nu15234925, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Furman D, Campisi J, Verdin E, Carrera-Bastos P, Targ S, Franceschi C, et al. Chronic inflammation in the etiology of disease across the life span. Nat Med. (2019) 25:1822–32. doi: 10.1038/s41591-019-0675-0, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Franceschi C, Bonafè M, Valensin S, Olivieri F, De Luca M, Ottaviani E, et al. Inflamm-aging: an evolutionary perspective on Immunosenescence. Ann N Y Acad Sci. (2000) 908:244–54. doi: 10.1111/j.1749-6632.2000.tb06651.x, PMID: [DOI] [PubMed] [Google Scholar]
- 90.Cesari M, Penninx BWJH, Pahor M, Lauretani F, Corsi AM, Rhys Williams G, et al. Inflammatory markers and physical performance in older persons: the InCHIANTI study. J Gerontol A Biol Sci Med Sci. (2004) 59:242–8. doi: 10.1093/gerona/59.3.M242, PMID: [DOI] [PubMed] [Google Scholar]
- 91.Taaffe DR, Harris TB, Ferrucci L, Rowe J, Seeman TE. Cross-sectional and prospective relationships of interleukin-6 and C-reactive protein with physical performance in elderly persons: MacArthur studies of successful aging. J Gerontol A Biol Sci Med Sci. (2000) 55:M709–15. doi: 10.1093/gerona/55.12.M709, PMID: [DOI] [PubMed] [Google Scholar]
- 92.Calvani R, Marini F, Cesari M, Buford TW, Manini TM, Pahor M, et al. Systemic inflammation, body composition, and physical performance in old community-dwellers. J Cachexia Sarcopenia Muscle. (2017) 8:69–77. doi: 10.1002/jcsm.12134, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wells JC, Sawaya AL, Wibaek R, Mwangome M, Poullas MS, Yajnik CS, et al. The double burden of malnutrition: aetiological pathways and consequences for health. Lancet. (2020) 395:75–88. doi: 10.1016/S0140-6736(19)32472-9, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Dunstan JA, Mori TA, Barden A, Beilin LJ, Holt PG, Calder PC, et al. Effects of n-3 polyunsaturated fatty acid supplementation in pregnancy on maternal and fetal erythrocyte fatty acid composition. Eur J Clin Nutr. (2004) 58:429–37. doi: 10.1038/sj.ejcn.1601825, PMID: [DOI] [PubMed] [Google Scholar]
- 95.Dunstan JA, Mori TA, Barden A, Beilin LJ, Taylor AL, Holt PG, et al. Fish oil supplementation in pregnancy modifies neonatal allergen-specific immune responses and clinical outcomes in infants at high risk of atopy: a randomized, controlled trial. J Allergy Clin Immunol. (2003) 112:1178–84. doi: 10.1016/j.jaci.2003.09.009, PMID: [DOI] [PubMed] [Google Scholar]
- 96.Dunstan JA, Mori TA, Barden A, Beilin LJ, Taylor AL, Holt PG, et al. Maternal fish oil supplementation in pregnancy reduces interleukin-13 levels in cord blood of infants at high risk of atopy. Clin Exp Allergy. (2003) 33:442–8. doi: 10.1046/j.1365-2222.2003.01590.x, PMID: [DOI] [PubMed] [Google Scholar]
- 97.See VHL, Mas E, Prescott SL, Beilin LJ, Burrows S, Barden AE, et al. Effects of prenatal n-3 fatty acid supplementation on offspring resolvins at birth and 12 years of age: a double-blind, randomised controlled clinical trial. Br J Nutr. (2017) 118:971–80. doi: 10.1017/S0007114517002914, PMID: [DOI] [PubMed] [Google Scholar]
- 98.Domenichiello AF, Kitson AP, Bazinet RP. Is docosahexaenoic acid synthesis from α-linolenic acid sufficient to supply the adult brain? Prog Lipid Res. (2015) 59:54–66. doi: 10.1016/j.plipres.2015.04.002, PMID: [DOI] [PubMed] [Google Scholar]
- 99.Kasuga K, Yang R, Porter TF, Agrawal N, Petasis NA, Irimia D, et al. Rapid appearance of resolvin precursors in inflammatory exudates: novel mechanisms in resolution. J Immunol. (2008) 181:8677–87. doi: 10.4049/jimmunol.181.12.8677, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Barker DJP. The developmental origins of adult disease. J Am Coll Nutr. (2004) 23:588S–95S. doi: 10.1080/07315724.2004.10719428 [DOI] [PubMed] [Google Scholar]
- 101.Barden AE, Mori TA, Dunstan JA, Taylor AL, Thornton CA, Croft KD, et al. Fish oil supplementation in pregnancy lowers F2-isoprostanes in neonates at high risk of atopy. Free Radic Res. (2004) 38:233–9. doi: 10.1080/10715760310001656722, PMID: [DOI] [PubMed] [Google Scholar]
- 102.Keim SA, Jude A, Smith K, Khan AQ, Coury DL, Rausch J, et al. Randomized controlled trial of Omega-3 and -6 fatty acid supplementation to reduce inflammatory markers in children with autism Spectrum disorder. J Autism Dev Disord. (2022) 52:5342–55. doi: 10.1007/s10803-021-05396-9, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hariri M, Djazayery A, Djalali M, Saedisomeolia A, Rahimi A, Abdolahian E. Effect of n-3 supplementation on hyperactivity, oxidative stress and inflammatory mediators in children with attention-deficit-hyperactivity disorder. Malays J Nutr. (2012) 18:329–35. PMID: [PubMed] [Google Scholar]
- 104.Sohouli MH, Magalhães Ei Da S, Ghahramani S, Nasresfahani M, Ezoddin N, Sharifi P, et al. Impact of omega-3 supplementation on children and adolescents patients with cystic fibrosis: a systematic review and meta-analysis of randomized-controlled trials. Pediatr Pulmonol. (2023) 58:2219–28. doi: 10.1002/ppul.26491, PMID: [DOI] [PubMed] [Google Scholar]
- 105.Kuh D, Hardy R, Butterworth S, Okell L, Wadsworth M, Cooper C, et al. Developmental origins of midlife grip strength: findings from a birth cohort study. J Gerontol A. (2006) 61:702–6. doi: 10.1093/gerona/61.7.702 [DOI] [PubMed] [Google Scholar]
- 106.Kuh D, Bassey J, Hardy R, Aihie Sayer A, Wadsworth M, Cooper C. Birth weight, childhood size, and muscle strength in adult life: evidence from a birth cohort study. Am J Epidemiol. (2002) 156:627–33. doi: 10.1093/aje/kwf099, PMID: [DOI] [PubMed] [Google Scholar]
- 107.Martin HJ, Syddall HE, Dennison EM, Cooper C, Sayer AA. Physical performance and physical activity in older people: are developmental influences important? Gerontology. (2009) 55:186–93. doi: 10.1159/000174823, PMID: [DOI] [PubMed] [Google Scholar]
- 108.Sayer AA, Cooper C, Evans JR, Rauf A, RPL W, Osmond C, et al. Are rates of ageing determined in utero? Age Ageing. (1998) 27:579–83. doi: 10.1093/ageing/27.5.579 [DOI] [PubMed] [Google Scholar]
- 109.Ylihärsilä H, Kajantie E, Osmond C, Forsén T, Barker DJP, Eriksson JG. Birth size, adult body composition and muscle strength in later life. Int J Obes. (2007) 31:1392–9. doi: 10.1038/sj.ijo.0803612, PMID: [DOI] [PubMed] [Google Scholar]
- 110.Robinson SM, Simmonds SJ, Jameson KA, Syddall HE, Dennison EM, Cooper C, et al. Muscle strength in older community-dwelling men is related to type of milk feeding in infancy. J Gerontol A Biol Sci Med Sci. (2012) 67:990–6. doi: 10.1093/gerona/gls061, PMID: [DOI] [PubMed] [Google Scholar]
- 111.Dodds RM, Roberts HC, Cooper C, Sayer AA. The epidemiology of sarcopenia. J Clin Densitom. (2015) 18:461–6. doi: 10.1016/j.jocd.2015.04.012, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Innis SM. Human milk: maternal dietary lipids and infant development. Proc Nutr Soc. (2007) 66:397–404. doi: 10.1017/S0029665107005666 [DOI] [PubMed] [Google Scholar]
- 113.Olsen SF, Joensen HD. High liveborn birth weights in the Faroes: a comparison between birth weights in the Faroes and in Denmark. J Epidemiol Community Health. (1985) 39:27–32. doi: 10.1136/jech.39.1.27, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Baird J, Fisher D, Lucas P, Kleijnen J, Roberts H, Law C. Being big or growing fast: systematic review of size and growth in infancy and later obesity. BMJ. (2005) 331:929. doi: 10.1136/bmj.38586.411273.E0, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.NCD Risk Factor Collaboration (NCD-RisC) . Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. (2017) 390:2627–42. doi: 10.1016/s0140-6736(17)32129-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Germolec DR, Shipkowski KA, Frawley RP, Evans E. Markers of inflammation. DeWitt JC, Rockwell CE, Bowman CC, (Eds.), Immunotoxicity testing: methods and protocols. New York, NY: Springer; (2018), 57–79. doi: 10.1007/978-1-4939-8549-4_5 [DOI] [PubMed] [Google Scholar]
- 117.Prendergast AJ, Rukobo S, Chasekwa B, Mutasa K, Ntozini R, Mbuya MNN, et al. Stunting is characterized by chronic inflammation in Zimbabwean infants. PLoS One. (2014) 9:e86928. doi: 10.1371/journal.pone.0086928, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Choi J, Joseph L, Pilote L. Obesity and C-reactive protein in various populations: a systematic review and meta-analysis. Obes Rev. (2013) 14:232–44. doi: 10.1111/obr.12003 [DOI] [PubMed] [Google Scholar]
- 119.Chang CI, Huang KC, Chan DC, Wu CH, Lin CC, Hsiung CA, et al. The impacts of sarcopenia and obesity on physical performance in the elderly. Obes Res Clin Pract. (2015) 9:256–65. doi: 10.1016/j.orcp.2014.08.003 [DOI] [PubMed] [Google Scholar]
- 120.Albracht-Schulte K, Kalupahana NS, Ramalingam L, Wang S, Rahman SM, Robert-McComb J, et al. Omega-3 fatty acids in obesity and metabolic syndrome: a mechanistic update. J Nutr Biochem. (2018) 58:1–16. doi: 10.1016/j.jnutbio.2018.02.012, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Mak IL, Cohen TR, Vanstone CA, Weiler HA. Increased adiposity in children with obesity is associated with low red blood cell omega-3 fatty acid status and inadequate polyunsaturated fatty acid dietary intake. Pediatr Obes. (2020) 15:e12689. doi: 10.1111/ijpo.12689, PMID: [DOI] [PubMed] [Google Scholar]
- 122.Curioni CC, Alves NNR, Zago L. Omega-3 supplementation in the treatment of overweight and obese children and adolescents: a systematic review. J Funct Foods. (2019) 52:340–7. doi: 10.1016/j.jff.2018.11.016 [DOI] [Google Scholar]
- 123.Svensson V, Johansson E, Fischer M, Deng SL, Hagströmer M, Danielsson P. Omega-3 fatty acids does not affect physical activity and body weight in primary school children—a double-blind randomized placebo-controlled trial. Sci Rep. (2018) 8:12725. doi: 10.1038/s41598-018-31229-4, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Hergenrader A, VanOrmer M, Thompson M, Slotkowski R, Freeman A, Paetz O, et al. Assessing the impact of socioeconomic status on maternal and cord serum Omega-3 polyunsaturated fatty acid levels. Curr Dev Nutr. (2022) 6:660. doi: 10.1093/cdn/nzac061.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Wilson NA, Mantzioris E, Middleton PF, Muhlhausler BS. Influence of sociodemographic, lifestyle and genetic characteristics on maternal DHA and other polyunsaturated fatty acid status in pregnancy: a systematic review. Prostaglandins Leukot Essent Fat Acids. (2020) 152:102037. doi: 10.1016/j.plefa.2019.102037 [DOI] [PubMed] [Google Scholar]
- 126.Parmenter BH, Bumrungpert A, Thouas GA. Sociodemographic factors and parental views associated with use of an omega-3 supplement for their children. PharmaNutrition. (2022) 20:100289. doi: 10.1016/j.phanu.2022.100289 [DOI] [Google Scholar]
- 127.Martínez-Martínez MI, Alegre-Martínez A, Cauli O. Omega-3 long-chain polyunsaturated fatty acids intake in children: the role of family-related social determinants. Nutrients. (2020) 12:3455. doi: 10.3390/nu12113455, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Parasannanavar D, Gaddam I, Bukya T, Ibrahim SA, Reddy KS, Banjara SK, et al. Omega-3 polyunsaturated fatty acid intake and plasma fatty acids of school going Indian children—a cross-sectional study. Prostaglandins Leukot Essent Fat Acids. (2021) 170:102294. doi: 10.1016/j.plefa.2021.102294, PMID: [DOI] [PubMed] [Google Scholar]
- 129.Lora KR, Lewis NM, Eskridge KM, Stanek-Krogstrand K, Travnicek DA. Correlation of Omega-3 fatty acids intakes with acculturation and socioeconomic status in Midwestern Latinas. J Immigrant Minority Health. (2011) 13:111–8. doi: 10.1007/s10903-009-9314-z, PMID: [DOI] [PubMed] [Google Scholar]
- 130.Robinson O, Carter AR, Ala-Korpela M, Casas JP, Chaturvedi N, Engmann J, et al. Metabolic profiles of socio-economic position: a multi-cohort analysis. Int J Epidemiol. (2021) 50:768–82. doi: 10.1093/ije/dyaa188, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Inglis V, Ball K, Crawford D. Socioeconomic variations in women’s diets: what is the role of perceptions of the local food environment? J Epidemiol Community Health. (2008) 62:191–7. doi: 10.1136/jech.2006.059253, PMID: [DOI] [PubMed] [Google Scholar]
- 132.Gómez G, Kovalskys I, Leme ACB, Quesada D, Rigotti A, Cortés Sanabria LY, et al. Socioeconomic status impact on diet quality and body mass index in eight Latin American countries: ELANS study results. Nutrients. (2021) 13:2404. doi: 10.3390/nu13072404, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Birnie K, Cooper R, Martin RM, Kuh D, Sayer AA, Alvarado BE, et al. Childhood socioeconomic position and objectively measured physical capability levels in adulthood: a systematic review and meta-analysis. PLoS One. (2011) 6:e15564. doi: 10.1371/journal.pone.0015564, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.MIT Press . (2023). A Dynamic Systems Approach to the Development of Cognition and Action. Available at: https://mitpress.mit.edu/9780262200950/a-dynamic-systems-approach-to-the-development-of-cognition-and-action/ [DOI] [PubMed]
- 135.Kluger A, Gianutsos JG, Golomb J, Ferris SH, George AE, Franssen E, et al. Patterns of motor impairement in normal aging, mild cognitive decline, and early Alzheimer’s disease. J Gerontol B Psychol Sci Soc Sci. (1997) 52B:P28–39. doi: 10.1093/geronb/52B.1.P28, PMID: [DOI] [PubMed] [Google Scholar]
- 136.Ridler K, Veijola JM, Tanskanen P, Miettunen J, Chitnis X, Suckling J, et al. Fronto-cerebellar systems are associated with infant motor and adult executive functions in healthy adults but not in schizophrenia. Proc Natl Acad Sci USA. (2006) 103:15651–6. doi: 10.1073/pnas.0602639103, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Murray GK, Veijola J, Moilanen K, Miettunen J, Glahn DC, Cannon TD, et al. Infant motor development is associated with adult cognitive categorisation in a longitudinal birth cohort study. J Child Psychol Psychiatry. (2006) 47:25–9. doi: 10.1111/j.1469-7610.2005.01450.x, PMID: [DOI] [PubMed] [Google Scholar]
- 138.van Elst K, Bruining H, Birtoli B, Terreaux C, Buitelaar JK, Kas MJ. Food for thought: dietary changes in essential fatty acid ratios and the increase in autism spectrum disorders. Neurosci Biobehav Rev. (2014) 45:369–78. doi: 10.1016/j.neubiorev.2014.07.004, PMID: [DOI] [PubMed] [Google Scholar]
- 139.Nevins JEH, Donovan SM, Snetselaar L, Dewey KG, Novotny R, Stang J, et al. Omega-3 fatty acid dietary supplements consumed during pregnancy and lactation and child neurodevelopment: a systematic review. J Nutr. (2021) 151:3483–94. doi: 10.1093/jn/nxab238, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Brenna JT, Diau GY. The influence of dietary docosahexaenoic acid and arachidonic acid on central nervous system polyunsaturated fatty acid composition. Prostaglandins Leukot Essent Fatty Acids. (2007) 77:247–50. doi: 10.1016/j.plefa.2007.10.016, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Weiser MJ, Butt CM, Mohajeri MH. Docosahexaenoic acid and cognition throughout the lifespan. Nutrients. (2016) 8:99. doi: 10.3390/nu8020099, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Agostoni C, Nobile M, Ciappolino V, Delvecchio G, Tesei A, Turolo S, et al. The role of Omega-3 fatty acids in developmental psychopathology: a systematic review on early psychosis, autism, and ADHD. Int J Mol Sci. (2017) 18:2608. doi: 10.3390/ijms18122608, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Sass L, Bjarnadóttir E, Stokholm J, Chawes B, Vinding RK, Mora-Jensen ARC, et al. Fish oil supplementation in pregnancy and neurodevelopment in childhood-a randomized clinical trial. Child Dev. (2021) 92:1624–35. doi: 10.1111/cdev.13541, PMID: [DOI] [PubMed] [Google Scholar]
- 144.Beblo S, Reinhardt H, Demmelmair H, Muntau AC, Koletzko B. Effect of fish oil supplementation on fatty acid status, coordination, and fine motor skills in children with phenylketonuria. J Pediatr. (2007) 150:479–84. doi: 10.1016/j.jpeds.2006.12.011, PMID: [DOI] [PubMed] [Google Scholar]
- 145.Agostoni C, Zuccotti GV, Radaelli G, Besana R, Podestà A, Sterpa A, et al. Docosahexaenoic acid supplementation and time at achievement of gross motor milestones in healthy infants: a randomized, prospective, double-blind, placebo-controlled trial. Am J Clin Nutr. (2009) 89:64–70. doi: 10.3945/ajcn.2008.26590, PMID: [DOI] [PubMed] [Google Scholar]
- 146.Donovan S, Dewey K, Novotny R, Stang J, Taveras E, Kleinman R, et al. Omega-3 fatty acids from supplements consumed before and during pregnancy and lactation and developmental milestones, including neurocognitive development, in the child: a systematic review [internet]. Alexandria (VA): USDA Nutrition Evidence Systematic Review. (2020). Available at: http://www.ncbi.nlm.nih.gov/books/NBK578641/ [PubMed]
- 147.Richardson AJ, Montgomery P. The Oxford-Durham study: a randomized, controlled trial of dietary supplementation with fatty acids in children with developmental coordination disorder. Pediatrics. (2005) 115:1360–6. doi: 10.1542/peds.2004-2164, PMID: [DOI] [PubMed] [Google Scholar]
- 148.Abbatecola AM, Cherubini A, Guralnik JM, Andres Lacueva C, Ruggiero C, Maggio M, et al. Plasma polyunsaturated fatty acids and age-related physical performance decline. Rejuvenation Res. (2009) 12:25–32. doi: 10.1089/rej.2008.0799, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Reinders I, Murphy RA, Song X, Visser M, Cotch MF, Lang TF, et al. Polyunsaturated fatty acids in relation to incident mobility disability and decline in gait speed; the age, gene/environment susceptibility-Reykjavik study. Eur J Clin Nutr. (2015) 69:489–93. doi: 10.1038/ejcn.2014.277, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Frison E, Boirie Y, Peuchant E, Tabue-Teguo M, Barberger-Gateau P, Féart C. Plasma fatty acid biomarkers are associated with gait speed in community-dwelling older adults: the Three-City-Bordeaux study. Clin Nutr. (2017) 36:416–22. doi: 10.1016/j.clnu.2015.12.008, PMID: [DOI] [PubMed] [Google Scholar]
- 151.Cornish SM, Cordingley DM, Shaw KA, Forbes SC, Leonhardt T, Bristol A, et al. Effects of Omega-3 supplementation alone and combined with resistance exercise on skeletal muscle in older adults: a systematic review and Meta-analysis. Nutrients. (2022) 14:2221. doi: 10.3390/nu14112221, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Bird JK, Troesch B, Warnke I, Calder PC. The effect of long chain omega-3 polyunsaturated fatty acids on muscle mass and function in sarcopenia: a scoping systematic review and meta-analysis. Clinical Nutrition ESPEN. (2021) 46:73–86. doi: 10.1016/j.clnesp.2021.10.011, PMID: [DOI] [PubMed] [Google Scholar]
- 153.Rondanelli M, Perna S, Riva A, Petrangolini G, Di Paolo E, Gasparri C. Effects of n-3 EPA and DHA supplementation on fat free mass and physical performance in elderly. A systematic review and meta-analysis of randomized clinical trial. Mech Ageing Dev. (2021) 196:111476. doi: 10.1016/j.mad.2021.111476, PMID: [DOI] [PubMed] [Google Scholar]
- 154.Ma WJ, Li H, Zhang W, Zhai J, Li J, Liu H, et al. Effect of n-3 polyunsaturated fatty acid supplementation on muscle mass and function with aging: a meta-analysis of randomized controlled trials. Prostaglandins Leukot Essent Fatty Acids. (2021) 165:102249. doi: 10.1016/j.plefa.2021.102249, PMID: [DOI] [PubMed] [Google Scholar]
- 155.Robinson SM, Jameson KA, Batelaan SF, Martin HJ, Syddall HE, Dennison EM, et al. Diet and its relationship with grip strength in community-dwelling older men and women: the Hertfordshire cohort study. J Am Geriatr Soc. (2008) 56:84–90. doi: 10.1111/j.1532-5415.2007.01478.x, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Fougère B, de Souto BP, Goisser S, Soriano G, Guyonnet S, Andrieu S, et al. Red blood cell membrane omega-3 fatty acid levels and physical performance: cross-sectional data from the MAPT study. Clin Nutr. (2018) 37:1141–4. doi: 10.1016/j.clnu.2017.04.005, PMID: [DOI] [PubMed] [Google Scholar]
- 157.Rolland Y, Barreto P de S, Maltais M, Guyonnet S, Cantet C, Andrieu S, et al. Effect of long-term omega 3 polyunsaturated fatty acid supplementation with or without multidomain lifestyle intervention on muscle strength in older adults: secondary analysis of the multidomain Alzheimer preventive trial (MAPT). Nutrients. (2019) 11:1931. doi: 10.3390/nu11081931, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Hutchins-Wiese HL, Kleppinger A, Annis K, Liva E, Lammi-Keefe CJ, Durham HA, et al. The impact of supplemental n-3 long chain polyunsaturated fatty acids and dietary antioxidants on physical performance in postmenopausal women. J Nutr Health Aging. (2013) 17:76–80. doi: 10.1007/s12603-012-0415-3, PMID: [DOI] [PubMed] [Google Scholar]
- 159.Krzymińska-Siemaszko R, Czepulis N, Lewandowicz M, Zasadzka E, Suwalska A, Witowski J, et al. The effect of a 12-week Omega-3 supplementation on body composition, muscle strength and physical performance in elderly individuals with decreased muscle mass. Int J Environ Res Public Health. (2015) 12:10558–74. doi: 10.3390/ijerph120910558, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Huang YH, Chiu WC, Hsu YP, Lo YL, Wang YH. Effects of Omega-3 fatty acids on muscle mass, muscle strength and muscle performance among the elderly: a meta-analysis. Nutrients. (2020) 12:3739. doi: 10.3390/nu12123739, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]