Abstract
BACKGROUND:
The Band Pull-Apart (BPA) exercise is used to strengthen the periscapular muscles. It was recently stated that the lower extremity and trunk movements should be included in the shoulder rehabilitation programs to optimize an effective energy transfer throughout the kinetic chain.
OBJECTIVE:
The aim of this study is to investigate the effects of kinetic chain based BPA exercise on the muscle activations of the sternocleidomasteideous (SCM) and the trapezius muscles in individuals with and without forward head posture (FHP).
METHODS:
Eighteen individuals with FHP and 18 individuals without FHP were included. Photographic measurements were made to identify individuals with FHP. The muscle activations of SCM, Upper Trapezius (UT), Middle Trapezius (MT), and Lower Trapezius (LT) were measured with surface EMG. BPA exercise was performed in the standing, unipedal standing, squat, unipedal squat, and Bulgarian split squat (BSS).
RESULTS:
There was no Group Exercise interaction for the SCM, UT, MT, LT muscle activations, or for the UT/MT and UT/LT ratios ( 0.05). While there was a difference in the activation of all muscles between individuals with and without FHP ( 0.05), both ratios were similar ( 0.05). There was a statistically significant difference between exercises for SCM, MT, and LT muscle activations ( 0.000 for these muscles), UT/MT ( 0.000) and UT/LT ratios ( 0.004). SCM muscle activation in squat was lower than activation in standing (Mean Difference (MD) 2.5% Maximal Voluntary Isometric Contractions (MVIC); 0.004) and in unipedal standing (MD 2.1% MVIC; 0.002). MT muscle activation in squat was higher than activation in standing (MD 9.7% MVIC), unipedal standing (MD 7.8% MVIC), unipedal squat (MD 6.9% MVIC) and BSS (MD 9.4% MVIC; 0.000 for these positions). LT muscle activation in the squat was higher than activation in the standing (MD 8.5% MVIC) and unipedal squat (MD 8.1% MVIC; 0.004 for these positions). UT/MT ratio in the squat was lower than standing (MD 0.3), unipedal standing (MD 0.2) and BSS (MD 0.3; 0.000 for these positions). UT/LT ratio in squat was lower than unipedal squat (MD 0.5) and BSS (MD 0.6; 0.002; for these positions).
CONCLUSION:
Performing the BPA exercise in the squat position is suggested in cases where lower SCM and UT muscle activation, lower UT/MT, and UT/LT ratios and higher MT and LT muscle activations are needed for individuals with and without FHP.
Keywords: Shoulder, superficial back muscles, electromyography, exercise therapy, posture
1. Introduction
Forward head posture (FHP) is described as the protrusion of the head in the sagittal plane, in positioning the head anterior to the trunk [1], and is considered a common postural deformity regarding musculoskeletal balance abnormalities [2]. Since the shoulder girdle and neck regions share many muscles, changes in head and neck alignment also result in changes in the activation of muscles of the shoulder girdle [3]. It is known that a very small change in the forward position of the head can increase the load on the musculoskeletal system, which in turn increases the activity of the upper extremity muscles [4]. It has been reported that the primary problem in FHP is shortening and hyperactivation of the sternocleideomasteideus (SCM) muscle [5]. It is also stated that the upper trapezius (UT) muscle becomes overactive to overcome the increased tension of the levator scapula due to FHP [6]. Furthermore, it is related to the weakness of the deep cervical flexor muscles and middle thoracic scapular retractor muscles (e.g., middle trapezius (MT), lower trapezius (LT), rhomboids and serratus anterior (SA)) [7]. Therapeutic exercises, including postural training, stretching of tight muscles, and strengthening of weak muscles, are crucial for treating FHP [8]. Elastic Band Pull-Apart (BPA) exercise is frequently used in rehabilitation to strengthen periscapular muscles such as trapezius and rhomboids [9, 10]. Fukunaga et al. found that when performed with a neutral grip, this exercise activated the UT (53%), the MT (55.8%), and LT (39.5%) muscles [9]. In addition, recent guidelines highlight the significance of integrating shoulder girdle exercises into a global functional kinetic chain for multiple reasons [11, 12]. The kinetic chain plays an important role in energy and force transfer from one part of the body to another [13]. Since the upper extremity performance relies not only on a single shoulder joint but also on the sequential activation of the kinetic chain from the bottom to top, clinicians suggest that the kinetic chain should be included in shoulder rehabilitation [14]. Shoulder rehabilitation using the kinetic chain instead of a strengthening exercise focused on a single shoulder joint can be more effective in restoring the normal movement of the scapula without an excessive load on the rotator cuff or periscapular muscles [13]. It is stated in previous studies that scapular muscle activation is altered when the upper body position [14], and lower body position/exercise position are changed [11, 14, 15, 16], or the trunk movements are included [17, 18, 19]. In a systematic review published in 2020 aiming to investigate the effects of the kinetic chain on shoulder rehabilitation, authors stated that integrating the kinetic chain into the shoulder exercises might increase axioscapular muscle recruitment, and leads to lower muscle ratios of the trapezius, and decrease the demand on the rotator cuff muscles [20]. De Mey et al. compared eight different lower extremity conditions and showed that trapezius muscle activity during squat on the contralateral leg was higher than in the traditional sitting position [11]. A challenge to the kinetic chain is often added to complicate the training program in the clinic [16]. With this study, we wanted to evaluate whether adding this difficulty affected the demand of the scapular muscles. Studies have mentioned the importance of the kinetic chain and it has been stated that the change in the demands of the muscles should be investigated when kinetic chain exercises are added to upper extremity exercises commonly used in the clinic. Therefore, this study aimed to determine whether the BPA exercise performed in different lower extremity positions affects the SCM and trapezius muscle activity in individuals with and without FHP. The effect of incorporating the kinetic chain on trapezius muscle activation during the BPA exercise, an exercise frequently used in the clinic, has not been investigated. The use of the lower extremity to encourage scapular movement has been stated to be ideal as it mimics the kinetic chain sequence [21]. We think that understanding the type of activation change that occurs in the scapular muscles with the addition of exercises in different lower extremity positions in individuals with and without FHP will guide us in exercise selection in the clinic. It was hypothesized that when there is a change in the demand of the kinetic chain, there will be a difference in scapular muscle activity during these exercises.
2. Materials and methods
2.1. Study design
A case-control study design was used to evaluate muscle activation during kinetic chain based exercises in individuals with and without FHP. On the first day of the study, the craniovertebral angle (CVA) values of the participants were evaluated by using photographic posture analysis. After the analysis, participants were divided into two groups according to their CVA values. The BPA exercise was performed in five different lower extremity positions to determine the effects of the kinetic chain based exercises. Muscle activations of the participants during the kinetic chain based exercises were evaluated with surface electromyography (EMG). The 8-channel surface EMG Noraxon MiniDTS, which is a non-invasive method to measure muscle activation, was used to evaluate the activation of the SCM, UT, MT and LT muscles. The EMG data were normalized by using the maximal voluntary isometric contractions (MVIC) measurements for all muscles. EMG activity for each muscle was recorded while the participants were performing the MVIC. MVIC and muscle activations of the participants during exercises were measured on two different evaluation sessions. At the end of the first evaluation, the locations of the electrodes were marked with a permanent pen so that the electrodes could be placed at the same spot in the following evaluations.
2.2. Participants
The study was conducted at Gazi University, Faculty of Health Sciences, Department of Physiotherapy and Rehabilitation, Unit of Athlete Health. The required permission was granted from the Gazi University Ethical Commission (No. E-77082166-302.08.01-419695; Reference No. 2022-935; Date: 22.03.2022). All participants were informed about the study beforehand. All individuals who agreed to participate in the study signed informed consent forms.
Individuals between the ages of 18 and 35 who did not have any surgery, pain in the spine or the upper extremity and the lower extremity, fracture anamnesis of the related body parts, musculoskeletal system pathology in the upper extremity for the past 6 weeks, could perform the exercises properly, and agreed to participate in the study were included [3, 14, 19, 22]. Individuals who suffered from neck, shoulder, and knee pain for the last 6 weeks, had surgery on the related parts, had functional or structural scoliosis, had any neurological, rheumatological, or systemic disorder, had a body mass index (BMI) greater than 30 kg/m2 and participation in any sport activities were excluded [6, 11, 13]. For the non-FHP group, individuals who had a postural deformity regarding the neck and shoulder were also excluded. Undergraduate and graduate students and research assistants of the Gazi University, Physiotherapy and Rehabilitation Department were contacted through social media groups and the inclusion criteria were explained. They were invited to the clinic on the planned day and time to determine their eligibility for inclusion criteria and whether they had FHP. Initially, 62 asymptomatic individuals who agreed to participate were invited to determine their eligibility for inclusion. As a result, the study was performed with 18 participants each in the FHP and non-FHP group. The post hoc power analysis of the study was calculated using G*Power 3.1.9.7 program [23]. As a result of the calculation performed using the research data with a total sample size of 36, the partial eta squared value of the research was calculated as 0.041 (“Group Exercise” interactions for the SCM muscle). The power of the study (1 was calculated as 0.88 with a 5% error ( 0.05) for repeated measures mixed design analysis of variance.
2.2.1. Assessment of forward head posture
Individuals were digitally imaged in the standing position from the lateral side to determine if they had FHP. The photogrammetry is considered the “gold standard” for assessing head position [24], and is reliable and valid compared to radiological measurements [25, 26]. A digital camera (Logitech c922 Pro Stream Webcam) was placed on a stable tripod without any rotation or tilt, at a 1.5-meter distance from the posture chart. The bottom of the camera was adjusted to the shoulder height of the participants [27, 28]. For the FHP evaluation, participants were asked to wear clothes with their neck region exposed to enable palpation of the spinous process of the 7th cervical vertebra and tragus, and two marker bands were placed at these anatomical locations. The marking tapes were placed on the 7th cervical vertebra and tragus following palpation by two experienced physiotherapists. Participants were guided to stand in a relaxed position with their feet shoulder-length apart, ensuring their lower extremities shared their body weight symmetrically [28]. Prior to taking a photo, participants were instructed to perform neck flexion and extension three times before positioning themselves in a resting period. Then, they were again instructed to look straight ahead in their natural relaxed position. Three measurements were performed by the same investigators. After the measurements, photographs were analyzed with the Image-J program [29]. The CVA, described as the angle between the horizontal line passing through the spinous process of the 7th cervical vertebra and the line extending from the tragus of the ear to the 7th vertical vertebra, was measured [27] (Fig. 1). The mean value of the three measurements was recorded as the CVA. A CVA of below 50∘ was considered as a FHP [1].
Figure 1.

Measurement of craniovertebral angle.
2.3. Kinetic chain based exercises
The BPA exercise was performed in; the standing, unipedal standing, squat, unipedal squat and in the Bulgarian split squat (BSS) position to identify the effects of kinetic chain based exercises (Fig. 2). In unipedal positions, the exercise was performed on the dominant leg. The dominant extremity was determined by questioning the leg they used to kick a ball [30]. These positions were chosen because they are the most used exercise positions in the clinic and in studies evaluating the effect of kinetic chain based exercises in the literature. An explanation of the lower extremity positions used during exercises is given in Table 1.
Figure 2.
Kinetic chain based exercises. A: Standing; B: Unipedal standing; C: Squat; D: Unipedal squat; E: Bulgarian split squat.
Table 1.
Descriptions of exercise positions
| Exercise | Descriptions |
|---|---|
| Standing | Participants were asked to stand with their feet shoulder-length apart (Fig. 2A). |
| Unipedal standing | The contralateral knee was placed at a 45∘ while the participants were standing on their dominant leg (Fig. 2B). |
| Squat | Participants were standing with their feet shoulder-length apart. The head and the trunk were aligned vertically. Then, the participants were asked to stay in the squat position with their hips 90∘ flexed and knees 60∘ flexed (Fig. 2C). |
| Unipedal squat | Participants were asked to stand on their dominant leg. Participants were instructed to perform the squat position with their knee 30∘ flexed. The non-dominant knee was 45∘ flexed. Participants were informed that the legs should not touch each other (Fig. 2D). |
| Bulgarian split squat | Participants were asked to stand with their dominant foot forward. The other foot was supported with a step that was equal to the tuberosity of the tibia length of each participant. The distance between the two feet was the same as the leg length that was measured from anterior superior iliac spine to the medial malleolus. Participants were instructed to perform the Bulgarian split squat with their dominant knee flexed at 45∘ and their tibia vertical to the ground (Fig. 2E). |
The feet positions of the participants were marked on the ground with chalk to make sure that the positions stayed the same throughout the trial. The knee angle during the exercises was measured with a goniometer. The angle of knee flexion during the exercises was adjusted with the help of a band placed between two parallel columns.
Exercises were performed with a resistance band. In order to standardize the resistance of the elastic band used in the exercises, the OMNI perceived exertion scale was used [31]. The instruction of the exercises and the amount of resistance of the elastic band were determined on a different day from the EMG measurement. In addition, all subjects were given time to practice the exercise before the test. The quality of exercise performance was checked and, if necessary, was corrected by an experienced physiotherapist. All subjects were instructed by the same researcher. The instructions were standardized with verbal cues to avoid variability between the instructions given to the subjects. The amount of the resistance was determined only in the standing position and not in other exercise positions separately due to the possibility of the occurrence of fatigue. Yellow, red, green, blue, black, silver, and gold elastic bands (Thera-Band®, Hygenic Corp., Akron, OH, USA) were used in this study. Participants were instructed to repeat the exercise 10 times with the lightest elastic band. Subsequently, they were asked to increase the resistance level of the band until the effort perceived by them was rated between the scores of 6 and 8 (somewhat hard and hard) on a scale of 0 to 10 (0: extremely easy; 10: extremely hard) [32].
2.4. Evaluation of the muscle activation
The 8-channel surface EMG Noraxon MiniDTS system (Noraxon, USA, Inc, Scottsdale, AZ, USA), which is a non-invasive method to measure muscle activation, was used to evaluate the activation of the SCM, UT, MT and LT muscles. The device has a common-mode rejection ratio greater than 100 Db, a differential input impedance greater than 100 Mohm, and a 1500–3000 Hz sampling rate for each channel. Disposable and self-adhesive Ag/AgCl electrodes (3M Red Dot 2271) usable for only surface EMG applications were used to record the EMG signals. It was made sure that the distance between the centers of the two electrodes was not more than 2 cm. A synchronized video shooting at 50 frames per second was made to determine the different phases of the exercises. The skin was shaved, scrubbed with soft sandpaper, and cleaned with 70% isopropyl alcohol to minimize skin impedance. Following the skin preparation, electrodes were placed in a parallel orientation to the determined muscle fibers in accordance with the European Recommendations for Surface Electromyography (SENIAM) [33]. For the SCM; electrodes were located 1/3 on the distance between the sternal notch and the mastoid process [34]; for the UT, electrodes were located midway between the 7th cervical vertebra and the acromion (in the direction of C7 and the acromion); for the MT, electrodes were located midway between the medial border of the scapula and the 3rd thoracic vertebra (in the direction of the acromion and T5) and for the LT, electrodes were located 2/3 on the line from the trigonum spinae to the 8th thoracic vertebra (in the direction of acromion and T8) [35]. After the placement of the electrodes, the skin impedance was measured with an ohmmeter to make sure that it was 5 k. If the skin impedance was higher than 5 k, the skin was re-prepared for the measurement [36].
2.4.1. EMG Measurement during exercise
EMG data were collected from the dominant side of the participants. The dominant upper extremity was determined by questioning the hand they used for writing [37]. Participants performed the BPA exercise first without resistance and then with an elastic band resistance to get familiar with the exercise. The exercise order was assigned by the randomization made on www.randomizer.org. Participants were asked to perform 90∘ shoulder flexion, elbow extension, forearm pronation and to hold the elastic band while sustaining a light resistance. Participants were instructed to perform shoulder horizontal abduction [9, 10]. All exercises were divided into three phases (pull apart phase, stationary phase and return phase) according to the synchronized video recording. Every phase lasted for 3 seconds, and the speed of the phases was standardized by a metronome (60 beats per minute). Every exercise was repeated three times. 30-second resting periods were applied between the repetitions, and 5-minute resting periods were also given between the exercises.
2.4.2. Normalizing EMG data
The EMG data were normalized by using the MVIC measurements for SCM, UT, MT and LT respectively. EMG activity for each muscle was recorded while the participants were performing the MVIC. All MVIC measurements were performed by the same investigator. After the familiarization trials of every MVIC test, three repetitions of the MVIC measurements, each lasting for 5 seconds, were performed. There were 30-second resting periods between every MVIC measurement and 1-minute resting periods between the repetitions [38, 39]. Throughout the measurements, participants were given the same standardized verbal stimulations by the same investigator to ensure that they displayed their maximum effort [39]. The MVIC measurement of the SCM muscle was performed in the supine position. Participants’ necks were flexed [34], and the resistance was applied with a stable belt over the forehead [40]. The MVIC measurements of the UT were performed in a sitting position in which the participants’ shoulders were 125∘ flexed, and the resistance was applied with a stable belt over the elbow. For the MT MVIC measurements, participants were asked to take the prone-T thumbs-up position. Resistance was applied vertically with a stable belt over the elbow joint while the shoulders were 90∘ horizontally abducted, and externally rotated. As for the MVIC measurements of the LT, participants were positioned in prone lying with their dominant arms 140∘ abducted and externally rotated. Resistance was applied over the elbow joint using a stable belt parallel to the LT fibers and against flexion [35].
2.4.3. EMG data analysis
Raw EMG signals were visually checked for the possibility of electrocardiac artifact risk. EMG signals were 20 Hz high-pass and 450 Hz low-pass filtered. Then, the root mean square (RMS) of the signals in a 100-millisecond time period was filtered. The signals recorded during the MVIC measurements were analyzed, and the highest value among the three repetitions was recorded. Synchronized video recordings were watched for analysis, and the pull apart, stationary, and return phases of the exercises were identified. Only the stationary phase data were used for the analysis. Later on, EMG signals in the stationary phase of the exercises were divided by the mean MVIC values for normalization. The data were used as % MVIC for the statistical analysis. To simplify the interpretation of the EMG data, the muscle activations were categorized as low ( 20% MVIC), moderate (20%–50% MVIC), or high ( 50% MVIC) activity [41]. We calculated muscle activity ratios: UT/MT (normalized EMG of UT divided by normalized EMG of MT) and UT/LT (normalized EMG of UT divided by normalized EMG of LT) [42]. Scapular muscle ratios for the trapezius muscle were categorized as moderate (0.8–1), good (0.6–0.8) and excellent ( 0.6) [43].
2.5. Statistical analysis
SPSS 22.0 program (IBM Corp., Armonk, NY, USA) was used for the statistical analysis. All outcome variables were normally distributed, as assessed using visual (histograms and probability plots) and analytical methods (Shapiro-Wilk tests). Participants characteristics and descriptive data for EMG were expressed as mean and standard deviation. Independent sample -tests were used to compare demographic variables between with and without FHP. For investigating the interactions between the group and exercise, and the main effects of the exercise or the groups, two-way repeated-measures analyses of variance (ANOVAs) with 1 between-subject factor (group: FHP and non-FHP) and 1 within-subject factor (exercises) were applied. If any significant interaction and/or main effect were observed, the Bonferroni post hoc test was performed. Statistical significance was accepted as 0.05 ( 0.05).
3. Results
Initially, 62 individuals who were informed about the study and agreed to participate were invited to determine their compliance with the inclusion criteria. Four of the participants who underwent photographic measurement did not meet the inclusion criteria. Among the individuals who met the inclusion criteria, those with a CVA lesser than 50∘ were included in the FHP group [1, 44]. According to the results of the photographic evaluation, 18 participants were determined to have a FHP. Eighteen individuals who had similar demographic features (gender, age and BMI) with the participants in the FHP group, met the inclusion criteria and had a CVA greater than 50∘ were included in the non-FHP group. See Fig. 3 for the flowchart of the study.
Figure 3.
Flowchart of the study.
There were no differences between the groups with and without FHP regarding age, height, body weight, and BMI ( 0.05, Table 2). Both groups had similar demographic features.
Table 2.
Comparison of demographic information in individuals with and without FHP
| FHP ( 18) (mean SD) | Non-FHP ( 18) (mean SD) | ||
|---|---|---|---|
| Age (years) | 22.2 2.4 | 21.3 1.6 | 0.227 |
| Weight (kg) | 59.3 9.9 | 59.9 11.0 | 0.862 |
| Height (cm) | 166.9 7.7 | 168.5 9.5 | 0.578 |
| BMI (kg/m2) | 21.2 2.1 | 21.0 2.3 | 0.819 |
| (%) | (%) | ||
| Gender | |||
| Female | 13 (72.2%) | 13 (72.2%) | |
| Male | 5 (27.8%) | 5 (27.8%) | |
| Upper extremity dominance | |||
| Right | 17 (94.4%) | 16 (88.9%) | |
| Left | 1 (5.6%) | 2 (11.1%) | |
| Lower extremity dominance | |||
| Right | 17 (94.4%) | 16 (88.9%) | |
| Left | 1 (5.6%) | 2 (11.1%) |
FHP: Forward Head Posture, SD: Standard Deviation, BMI: Body Mass Index, : Number.
There were no significant “Group Exercise” interactions for the SCM muscle (F(2.917,90.343) 1.319, 0.273, 0.041), UT muscle (F 0.996, 0.395, 0. 0.031), MT muscle (F 1.021, 0.399, 0.032), and LT muscle (F 0.131, 0.913, 0.004).
Although the “Group Exercise” interaction was not significant, group main effect was found to be statistically significant. There was a difference between the groups for SCM muscle (F(1,31) 5.834, 0.022, 0.158), UT muscle (F 7.615, 0.010, 0.197), MT muscle (F 6.669, 0.015, 0.177) and LT muscle (F 4.979, 0.033, 0.138). Muscle activations in individuals with FHP were lower than in individuals without FHP.
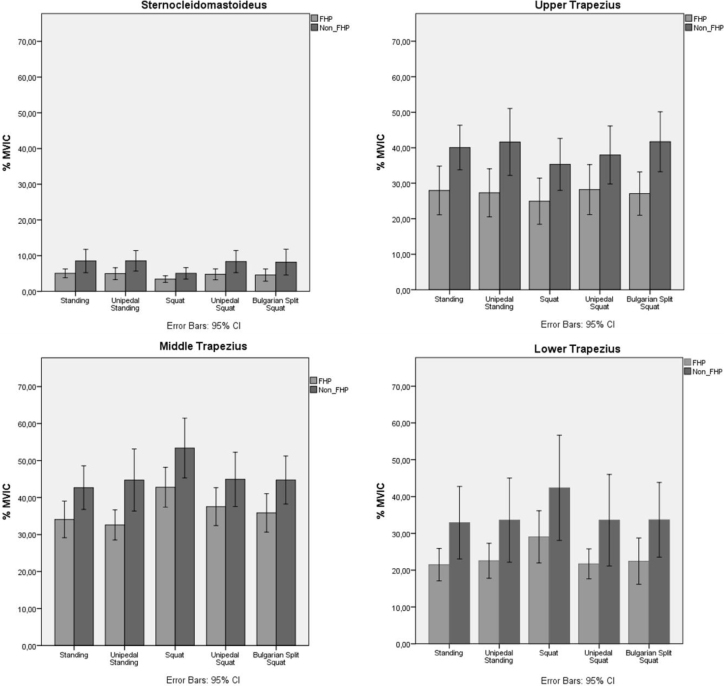
The exercise main effect was found to be statistically significant. There were significant differences observed among the exercises for the SCM muscle (F 8.109, 0.000, 0.207), for the MT muscle (F 18.455, 0.000, 0.373), and for the LT muscle (F 8.182, 0.000, 0.209). However, no statistically significant difference was observed in the UT muscle among the exercises (F 2.664, 0.056, 0.079). Post hoc test results showed that the SCM muscle activation during the BPA exercise in the squat was statistically lower compared to the one in the standing (0.004), and the one in the unipedal standing (0.002). The MT muscle activation during the BPA exercise in the squat was higher compared to the one in the standing, unipedal standing, unipedal squat, and the BSS ( 0.000 for these positions). The LT muscle activation during the BPA exercise in the squat was higher compared to the one in the standing and the unipedal squat ( 0.004 for these positions). The % MVIC values of the SCM, UT, MT, and LT for both groups are shown in Fig. 4.
Figure 4.
Sternocleideomasteideus, upper, middle and lower trapezius muscle activation levels during Band Pull-Apart exercises in individuals with and without FHP. Abbreviations: %MVIC: Percentage of maximum voluntary isometric contraction, FHP: Forward head posture.
No significant “Group Exercise” interactions were observed for the UT/MT (F 0.370, 0.806, 0.012) and UT/LT (F(1.785,55.331) 0.477, 0.602, 0.015) muscle activation ratios. There were also no significant group main effects for the UT/MT (F 1.015, 0.322, 0.032) and UT/LT (F 0.198, 0.660, 0.006). The ratios of the two groups are similar.
The exercise main effect was found to be statistically significant. It was observed among the exercises that there was a statistically significant difference for UT/MT (F(3.520,109.112) 18.128, 0.000, 0.369), and UT/LT (F 6.661, 0.004, 0.177). Post hoc analysis results showed that the UT/MT muscle activation ratio during the BPA exercise in the squat was lower compared to the one in the standing, unipedal standing and the BSS ( 0.000 for these positions). UT/LT muscle activation ratio during the BPA exercise in the squat was lower compared to the unipedal squat and the BSS ( 0.002 for these positions). UT/MT and UT/LT muscle activation ratios are shown in the Table 3.
Table 3.
The effect of kinetic chain on muscle activation ratios during BPA exercise in individuals with and without FHP
| UT/MT (mean SD) | UT/LT (mean SD) | |||||
|---|---|---|---|---|---|---|
| FHP | Non-FHP | Whole group | FHP | Non-FHP | Whole group | |
| Standing | 0.85 0.4 | 0.98 0.4 | 0.92 0.4 | 1.54 0.9 | 1.88 2.0 | 1.71 1.4 |
| Unipedal standing | 0.86 0.4 | 0.96 0.3 | 0.87 0.4 | 1.44 0.9 | 1.64 1.2 | 1.60 1.1 |
| Squat | 0.60 0.3 | 0.70 0.3 | 0.65 0.3a | 1.05 0.7 | 1.02 0.5 | 1.03 0.6b |
| Unipedal squat | 0.76 0.3 | 0.87 0.4 | 0.82 0.4 | 1.46 0.8 | 1.57 1.4 | 1.51 1.1 |
| Bulgarian split squat | 0.78 0.4 | 0.96 0.3 | 0.91 0.4 | 1.48 0.9 | 1.72 1.8 | 1.54 1.3 |
BPA: Band Pull-Apart; FHP: Forward head posture, SD: Standard deviation, UT: Upper trapezius, MT: Middle trapezius, LT: Lower trapezius. aSignificantly lower UT/MT ratio compared to standing, unipedal standing and Bulgarian split squat. bSignificantly lower UT/LT ratio compared to unipedal squat and Bulgarian split squat.
4. Discussion
The main purpose of this study was to investigate the effects of the kinetic chain during the BPA exercise in individuals with or without FHP. To the best of our knowledge, this study is the first to evaluate the effects of the kinetic chain during the BPA exercise. As a result of this study, SCM, UT, MT and LT muscle activations were found to be lower in the FHP group compared to the non-FHP group. However, UT/MT and UT/LT muscle activation ratios were similar between FHP and non-FHP groups. Considering the kinetic chain effect, it was observed that SCM muscle activation in the squat was lower compared to the activation in the standing and unipedal standing. Although there was no statistically significant difference in the amount of UT muscle activation, the activation during the exercise in the squat was lower compared to the other positions. MT muscle activation in the squat was higher compared to standing, unipedal standing, unipedal squat, and BSS positions. LT muscle activation in the squat was higher than the activation in the standing, and unipedal squat. UT/MT muscle activation ratio in the squat was lower compared to the ratio in the standing, unipedal standing, and BSS. UT/LT muscle activation ratio during the BPA exercise in the squat was lower compared to the one the unipedal squat and the BSS.
FHP alignment places the center of gravity of the head anterior to the vertical axis, thus increasing the load on the posterior neck. These postural changes alter scapular mechanics and muscle activity related to the shoulder complex, resulting in altered force couples and scapular movement [45]. To investigate the effect of FHP on muscle activation, we evaluated muscle activation during BPA exercise. As a result of this study, SCM, UT, MT and LT muscle activations were lower in the FHP group than in the non-FHP group. Similar to our study, Lee et al. stated that the activation of splenii and SCM muscles was found to be reduced in the group with FHP during neck protraction exercise compared to the group without FHP, while OT muscle activation decreased during retraction exercise. The authors also found that UT muscle activation was similar during both protraction and retraction exercises. They stated that the reduced activation was due to changes in muscle length due to FHP and was associated with decreased ability to produce force [46]. In contrast, Khan et al. observed that the EMG activity of the SCM and UT muscles significantly increased in individuals with FHP compared to the group without FHP, both at rest and during shoulder abduction [47]. Kiatkulanusorn et al. investigated the differences in muscle activation while resting in the side lying position in individuals FHP and non-FHP and found that FHP might cause excessive activation in the UT and LT muscles, and that the activations in the SCM and MT were similar in those with FHP and without FHP [48]. When the present study and literature is examined, it is seen that the muscle activations in individuals with FHP are contradictory. The reason for the different results in the studies may be the different exercises used in the studies.
To investigate the effect of the kinetic chain, we evaluated SCM, UT, MT and LT muscle activation during BPA exercise in five different lower extremity positions. The most important finding of this study was that BPA exercise performed in squat position showed decreased SCM, UT and increased MT and LT muscle activation. As a result of the present study, SCM muscle activation in the squat was lower compared to the activation in the standing and the unipedal standing. Although there was no statistically significant difference ( 0.056) in the UT muscle activation, its activation during the exercise in the squat was lower compared to the other positions. The MT muscle produced higher activation in the squat compared to the other all positions. LT muscle activation in the squat was higher than the activation in the standing, and unipedal squat. Myofascial structures that connect the shoulders, trunk, and lower extremities are defined as a potential underlying mechanism to state the effects of the proximal kinetic chain on scapular muscle recruitment. De Mey et al. investigated the effects of the lower extremity positions and movements on the UT and LT muscle activations during scapular retraction variations. The results showed that the trapezius muscle activity during squat position on the contralateral leg was higher than in the traditional sitting position. The authors stated that all exercise variations may be beneficial in the early stages of scapular rehabilitation training because of their favorable trapezius muscle balance activation [11]. Borms et al. investigated the scapular muscle activity during five different kinetic chain variations of the bilateral elevation with external rotation. It was stated that the involvement of the lower extremities only influenced the UT activity, and this led to higher muscle activation. Additionally, it was found that the LT activity decreased when the dynamic unipedal squat was added to the exercise. The authors also stated that including the lower extremity to shoulder rehabilitation can be beneficial for the overhead athlete population relating to the more complex variations of the kinetic chain exercises [14]. Shin et al. investigated the shoulder muscle activation during shoulder external rotation exercises performed with an elastic band in static and dynamic body positions, while the arms of the participants were at their sides or 90∘ abducted. The authors identified that the dynamic squat to standing and trunk rotation positions maintained the efficient control of the scapular motion and lower shoulder muscle activation. They also stated that the kinetic chain exercises which integrate the lower extremity, hips, and trunk to the shoulder exercises might be beneficial for patients with weak periscapular muscles, and decreased LT activations [13]. Borms et al. investigated the scapular muscle activity during the kinetic chain variations of the prone elevation exercise. According to the results, there was no significant difference for the LT and MT muscles among the exercise variations; however, adding rotation to the prone elevation exercise reduced UT activity, while the addition of the trunk extension increased the UT muscle activity. The authors specified that a gradual loading on the functional open chain might be beneficial for scapular rehabilitation [19]. When all these studies are considered, although the different muscles provide different results during various exercises, it is possible that involving the kinetic chain alters the scapular muscle activation. Although many studies indicate that the involvement of the kinetic chain affects the scapular muscle activation, there are conflicting results about the trapezius muscle activations. We believe that the reason for these conflicts is the usage of different exercises in different studies.
Regardless of group, when normalised EMG values during different variations of BPA exercise are investigated, SCM muscle activation produced low activation ( 20% MVIC) during all exercise variations. When low SCM muscle activation is required, BPA exercise can be used with different exercise variations. All trapezius muscles produced moderate activity (20–50% of MVIC). This shows that all activation values in all exercise variations are appropriate for scapular muscle control and strengthening training [19]. In cases where the UT, MT, and LT muscles should be strengthened, the variations of the BPA exercise can be used.
Restoring muscle control and balanced coactivation is challenging for clinicians. Maintaining minimal activity in the overactive muscles, and the selective activation of the weak muscles is important to reduce the imbalance in patients with scapular muscle imbalance. Since the lack of MT, LT and SA muscle activity is considered to be related to the excessive recruitment of the UT, it is especially important to keep the UT/MT, UT/LT, and UT/SA ratios balanced [43]. In a systematic review, the authors stated that integrating the kinetic chain into shoulder exercises may produce lower muscle ratios of trapezius and reduce the demands on the rotator cuff muscles [20]. Considering the kinetic chain effect, UT/MT muscle activation ratio in the squat was lower compared to the ratio in the standing, unipedal standing, and BSS. Regardless of groups, the squat position showed a good UT/OT ratio (0.6–0.8), while the other four positions showed a moderate ratio (0.8–1.0). These findings suggest that performing the BPA exercise in the squat may be more beneficial for rehabilitation regarding the trapezius muscle balance. UT/LT muscle activation ratio during the BPA exercise in the squat was lower compared to the one the unipedal squat and BSS. The ratios in all positions were above 1. However, during BPA exercise performed in squat, the ratio was very close to 1. Since a ratio 1.00 indicates that the UT is more active than other scapular stabilisers, it may be recommended to be performed in squat position in order to reduce the UT/LT ratio to at least moderate levels.
When the kinetic chain was included during BPA exercise, decreased SCM and UT and increased MT and LT muscle activations were observed. Furthermore, the incorporation of the kinetic chain decreased muscle activation ratios. It is recommended to perform BPA exercise in the squat position when lower SCM and UT muscle activation, muscle activation ratios, and higher MT and LT muscle activations are requested in individuals with or without FHP. We think that our findings regarding changes in muscle activation by performing the BPA exercise in the squat position will contribute to the literature. To our knowledge, this is the first study to investigate the effect of the kinetic chain in BPA exercise, which is a frequently used exercise in clinics. It is also important because it is the first study investigating the effectiveness of the kinetic chain in individuals with FHP.
This study has several limitations. Firstly, muscles that are important for scapular control during rehabilitation such as pectoralis minor, rhomboids, levator scapula and SA could not be evaluated due to the impossibility of accessing them with surface EMG. Secondly, surface EMG can cause possible crosstalk between superficial and deeper scapulothoracic muscles (such as UT, MT and LT) and artifacts from movement during the test. However, small size surface electrodes and inter-electrode distance, proposed electrode placement are extensively standardized to ensure the reliability of the tests, so errors were minimized. Thirdly, this study was conducted with young, sedentary individuals who did not have any shoulder pathology. Therefore, the results of our study may not be generalizable to different age groups, individuals with different pathologies, or athletes.
5. Conclusion
To our knowledge, this is the first study to examine the influence of the kinetic chain during the BPA exercise. It is also the first study to investigate the effect of the kinetic chain in individuals with FHP. Understanding the muscle activations during exercises can be useful for clinicians and trainers to choose the appropriate exercises. The influence of the kinetic chain on muscle activation and muscle activation ratios should be considered while giving exercises to individuals with and without FHP. The most important finding of this study is that BPA exercise during squat causes decreased SCM and UT and increased MT and LT activation. Moreover, it was found that the involvement of the kinetic chain contributes to the scapular muscle balance by reducing muscle activation ratios. In shoulder rehabilitation, clinicians should consider using BPA exercise in the squat position if lower SCM and UT muscle activation, lower UT/MT and UT/LT ratios, and higher MT and LT muscle activations are desired in individuals with or without FHP. Future studies are needed to investigate the effect of different exercises on the kinetic chain in different age groups, individuals with different shoulder pathologies, and athletes. It may be also intriguing to investigate the effects of the kinetic chain variations on core muscle activity.
Author contributions
GC: Study Design, Data Collection, Statistical Analysis, Data Interpretation, Manuscript Preparation, Literature Search. NAG: Study Design, Data Interpretation, Reviewing. ZBE: Study Design, Data Collection, Literature Search. MYD: Data Collection, Statistical Analysis, Data Interpretation, Manuscript Preparation.
Data availability
Data is available from the corresponding author upon reasonable request.
Ethical approval
The study was approved by the Gazi University Ethical Commission (No. E-77082166-302.08.01-419695; Reference No. 2022 – 935; Date: 22.03.2022).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Informed consent
Informed consent was obtained from the participants prior to the start of the study.
Acknowledgments
The authors would like to thank Nihan Kafa and İrem Düzgün for their contributions in the thesis committee. They would also like to thank Zeynep Hazar, Çağla Özkul, Gökhan Yazıcı, Melek Volkan Yazıcı and Ebrar Bardakçı for their support throughout the thesis process.
Conflict of interest
The authors report no conflict of interest.
References
- [1]. Ruivo RM, Pezarat-Correia P, Carita AI. Cervical and shoulder postural assessment of adolescents between 15 and 17 years old and association with upper quadrant pain. Braz J Phys Ther. 2014; 18: 364-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2]. Lee M-Y, Lee H-Y, Yong M-S. Characteristics of cervical position sense in subjects with forward head posture. J Phys Ther Sci. 2014; 26(11): 1741-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3]. Dehqan B, Delkhoush CT, Mirmohammadkhani M, Ehsani F. Does forward head posture change subacromial space in active or passive arm elevation? J Man Manip Ther. 2021; 29(4): 227-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4]. Kushwah K, Narvey R. EMG Analysis of Head posture at standing and sitting position. IRJET. 2018; 25: 1-188. [Google Scholar]
- [5]. Kim M-S. Neck kinematics and sternocleidomastoid muscle activation during neck rotation in subjects with forward head posture. J Phys Ther Sci. 2015; 27(11): 3425-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6]. Valizadeh A, Rajab R, Rezazadeh F, Mahmoudpour A, Aali S. Comparison of the forward head posture on scapular muscle contributions during shoulder flexion of predominant arm in women with forward head posture. J Res Med Sci. 2014; 16(6): 68-72. [Google Scholar]
- [7]. Harman K, Hubley-Kozey CL, Butler H. Effectiveness of an exercise program to improve forward head posture in normal adults: a randomized, controlled 10-week trial. J Man Manip Ther. 2005; 13(3): 163-76. [Google Scholar]
- [8]. Shih H-S, Chen S-S, Cheng S-C, Chang H-W, Wu P-R, Yang J-S, et al. Effects of Kinesio taping and exercise on forward head posture. J Back Musculoskelet Rehabil. 2017; 30(4): 725-33. [DOI] [PubMed] [Google Scholar]
- [9]. Fukunaga T, Fedge C, Tyler T, Mullaney M, Schmitt B, Orishimo K, et al. Band Pull-Apart Exercise: Effects of Movement Direction and Hand Position on Shoulder Muscle Activity. Int J Sports Phys Ther. 2022; 17(3): 400-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10]. Kushner AM, Brent JL, Schoenfeld BJ, Hugentobler J, Lloyd RS, Vermeil A, et al. The back squat part 2: Targeted training techniques to correct functional deficits and technical factors that limit performance. Strength Cond J. 2015; 37(2): 13-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11]. De Mey K, Danneels L, Cagnie B, Van den Bosch L, Flier J, Cools AM. Kinetic chain influences on upper and lower trapezius muscle activation during eight variations of a scapular retraction exercise in overhead athletes. J Sci Med Sport. 2013; 16(1): 65-70. [DOI] [PubMed] [Google Scholar]
- [12]. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology Part III: The SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy. 2003; 19(6): 641-61. [DOI] [PubMed] [Google Scholar]
- [13]. Shin M-H, Chung S-W, Im J-M, Baek S, Kim T-M, Oh K-S. Changes in Shoulder Muscle Activities Depending on Static and Dynamic Body Positions during Shoulder External Rotation Exercises Using Kinetic Chain Concept. Korean J Sports Med. 2020; 38(4): 199-207. [Google Scholar]
- [14]. Borms D, Maenhout A, Cools AM. Incorporation of the kinetic chain into shoulder-elevation exercises: does it affect scapular muscle activity? J Athl Train. 2020; 55(4): 343-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15]. Maenhout A, Van Praet K, Pizzi L, Van Herzeele M, Cools A. Electromyographic analysis of knee push up plus variations: what is the influence of the kinetic chain on scapular muscle activity? Br J Sports Med. 2010; 44(14): 1010-5. [DOI] [PubMed] [Google Scholar]
- [16]. Werin MB, Maenhout AG, Icket J, Jacxsens N, Kempkes E, Cools AM. Does the Activity in Scapular Muscles During Plyometric Exercises Change When the Kinetic Chain Is Challenged-An? EMG Study. J Strength Cond Res. 2022; 36(7): 1793-800. [DOI] [PubMed] [Google Scholar]
- [17]. Yamauchi T, Hasegawa S, Matsumura A, Nakamura M, Ibuki S, Ichihashi N. The effect of trunk rotation during shoulder exercises on the activity of the scapular muscle and scapular kinematics. J Shoulder Elbow Surg. 2015; 24(6): 955-64. [DOI] [PubMed] [Google Scholar]
- [18]. Nagai K, Tateuchi H, Takashima S, Miyasaka J, Hasegawa S, Arai R, et al. Effects of trunk rotation on scapular kinematics and muscle activity during humeral elevation. J Electromyogr Kinesio. 2013; 23(3): 679-87. [DOI] [PubMed] [Google Scholar]
- [19]. Borms D, Maenhout A, Berckmans K, Spanhove V, Vanderstukken F, Cools A. Scapulothoracic muscle activity during kinetic chain variations of a prone elevation exercise. Braz J Phys Ther. 2022; 26(3): 100420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20]. Richardson E, Lewis JS, Gibson J, Morgan C, Halaki M, Ginn K, et al. Role of the kinetic chain in shoulder rehabilitation: does incorporating the trunk and lower limb into shoulder exercise regimes influence shoulder muscle recruitment patterns? Systematic review of electromyography studies. BMJ Open. 2020; 6(1): e000683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21]. Sciascia A, Cromwell R. Kinetic chain rehabilitation: a theoretical framework. Rehabil Res Pract. 2012; 853037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22]. Maenhout A, Benzoor M, Werin M, Cools A. Scapular muscle activity in a variety of plyometric exercises. J Electromyogr Kinesiol. 2016; 27: 39-45. [DOI] [PubMed] [Google Scholar]
- [23]. Faul F, Erdfelder E, Lang AG, Buchner A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2017; 39(2): 175-191. [DOI] [PubMed] [Google Scholar]
- [24]. Gallego-Izquierdo T, Arroba-Díaz E, García-Ascoz G, Val-Cano MdA, Pecos-Martin D, Cano-de-la-Cuerda R. Psychometric proprieties of a mobile application to measure the craniovertebral angle a validation and reliability study. Int J Environ Res Public Health. 2020; 17(18): 6521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25]. Mylonas K, Tsekoura M, Billis E, Aggelopoulos P, Tsepis E, Fousekis K. Reliability and Validity of Non-radiographic Methods of Forward Head Posture Measurement: A Systematic Review. Cureus. 2022; 14(8): e27696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26]. Nam SH, Son SM, Kwon JW, Lee NK. The intra-and inter-rater reliabilities of the forward head posture assessment of normal healthy subjects. J Phys Ther Sci. 2013; 25(6): 737-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27]. Salahzadeh Z, Maroufi N, Ahmadi A, Behtash H, Razmjoo A, Gohari M, et al. Assessment of forward head posture in females: observational and photogrammetry methods. J Back Musculoskelet Rehabil. 2014; 27(2): 131-9. [DOI] [PubMed] [Google Scholar]
- [28]. Ghamkhar L, Kahlaee AH. Is forward head posture relevant to cervical muscles performance and neck pain? A case – control study. Braz J Phys Ther. 2019; 23(4): 346-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29]. Jabbar KM, Gandomi F. The comparison of two corrective exercise approaches for hyperkyphosis and forward head posture: A quasi-experimental study. J Back Musculoskelet Rehabil. 2021; 34(4): 677-87. [DOI] [PubMed] [Google Scholar]
- [30]. Kadri MA, Noé F, Maitre J, Maffulli N, Paillard T. Effects of limb dominance on postural balance in sportsmen practicing symmetric and asymmetric sports: A pilot study. Symmetry. 2021; 13(11): 2199. [Google Scholar]
- [31]. Colado JC, Garcia-Masso X, Triplett NT, Calatayud J, Flandez J, Behm D, et al. Construct and concurrent validation of a new resistance intensity scale for exercise with thera-band elastic bands. J Sports Sci Med. 2014; 13(4): 758-66. [PMC free article] [PubMed] [Google Scholar]
- [32]. Kara D, Harput G, Duzgun I. Trapezius muscle activation levels and ratios during scapular retraction exercises: A comparative study between patients with subacromial impingement syndrome and healthy controls. Clin Biomech. 2019; 67: 119-26. [DOI] [PubMed] [Google Scholar]
- [33]. Hermens HJ, Freriks B, Disselhorst-Klug C, Rau G. Development of recommendations for SEMG sensors and sensor placement procedures. J Electromyogr Kinesiol. 2000; 10(5): 361-74. [DOI] [PubMed] [Google Scholar]
- [34]. Sremakaew M, Treleaven J, Jull G, Vongvaivanichakul P, Uthaikhup S. Altered neuromuscular activity and postural stability during standing balance tasks in persons with non-specific neck pain. J Electromyogr Kinesiol. 2021; 61: 102608. [DOI] [PubMed] [Google Scholar]
- [35]. Uysal Ö, Akoğlu AS, Kara D, Sezik AÇ, Çalık M, Düzgün İ, Theraband applications for improved upper extremity wall slide exercise. J Athl Train. 2022; 57(8): 795-803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36]. Ekstrom RA, Donatelli RA, Soderberg GL. Surface electromyographic analysis of exercises for the trapezius and serratus anterior muscles. J Orthop Sports Phys Ther. 2003; 33(5): 247-58. [DOI] [PubMed] [Google Scholar]
- [37]. Armstrong C, Oldham JA. A comparison of dominant and non-dominant hand strengths. J Hand Surg Br. 1999; 24(4): 421-5. [DOI] [PubMed] [Google Scholar]
- [38]. Castelein B, Cagnie B, Parlevliet T, Cools A. Scapulothoracic muscle activity during elevation exercises measured with surface and fine wire EMG: a comparative study between patients with subacromial impingement syndrome and healthy controls. Man Ther. 2016; 23: 33-9. [DOI] [PubMed] [Google Scholar]
- [39]. Kara D, Harput G, Duzgun I. Shoulder-abduction angle and trapezius muscle activity during scapular-retraction exercise. J Athl Train. 2021; 56(12): 1327-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40]. Falla D, Jull G, Edwards S, Koh K, Rainoldi A. Neuromuscular efficiency of the sternocleidomastoid and anterior scalene muscles in patients with chronic neck pain. Disabil Rehabil., 2004; 26(12): 712-717. [DOI] [PubMed] [Google Scholar]
- [41]. Berckmans K, Castelein B, Borms D, Palmans T, Parlevliet T, Cools A. Analysis of scapular kinematics and muscle activity by use of fine-wire electrodes during shoulder exercises. Am J Sports Med. 2020; 48(5): 1213-9. [DOI] [PubMed] [Google Scholar]
- [42]. Cools A, Declercq G, Cambier D, Mahieu N, Witvrouw E. Trapezius activity and intramuscular balance during isokinetic exercise in overhead athletes with impingement symptoms. Scand J Med Sci Sports. 2007; 17(1): 25-33. [DOI] [PubMed] [Google Scholar]
- [43]. Cools AM, Dewitte V, Lanszweert F, Notebaert D, Roets A, Soetens B, et al. Rehabilitation of scapular muscle balance: which exercises to prescribe? Am J Sports Med. 2007; 35(10): 1744-51. [DOI] [PubMed] [Google Scholar]
- [44]. Moustafa IM, Youssef A, Ahbouch A, Tamim M, Harrison DE. Is forward head posture relevant to autonomic nervous system function and cervical sensorimotor control? Cross sectional study. Gait Posture. 2020; 77: 29-35. [DOI] [PubMed] [Google Scholar]
- [45]. Kim T-H, Hwang B-H. Change of head position and muscle activities of neck during overhead arm lift test in subjects with forward head posture. Phys Ther Korea. 2019; 26(2): 61-8. [Google Scholar]
- [46]. Lee KJ, Han HY, Cheon SH, Park SH, Yong, MS. The effect of forward head posture on muscle activity during neck protraction and retraction. J Phys Ther Sci. 2015; 27(3): 977-979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47]. Khan A, Khan Z, Bhati P, Hussain ME. Influence of forward head posture on cervicocephalic kinesthesia and electromyographic activity of neck musculature in asymptomatic individuals. J Chiropr Med. 2020; 19(4): 230-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48]. Kiatkulanusorn S, Luangpon N, Tudpor K. Increased upper and lower trapezius muscle activities during rest in side-lying position in young adults with forward head posture. Indian J Occup Ther. 2020; 14(2): 266-71. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is available from the corresponding author upon reasonable request.