Abstract
Introduction
This study provides an in‐depth analysis of the immediate postoperative outcomes and implications or robotic‐assisted total knee arthroplasty (RA‐TKA) compared with conventional TKA (C‐TKA), particularly with regard to mortality, complications, hospital stay and costs, drawing from a comprehensive nationwide data set.
Methods
The Nationwide Inpatient Sample (NIS) database, the largest all‐payer inpatient healthcare database in the United States, was used to identify all patients who underwent RA‐TKA or C‐TKA from 2016 to 2019. A total of 527,376 cases, representing 2,638,679 patients who underwent elective TKA were identified, of which 88,415 had RA‐TKA. To mitigate potential variations and selection bias in baseline characteristics between the two groups, a propensity score‐matched analysis was employed to further balance and refine our data set, resulting in 176,830 patients evenly distributed between the groups. Analysis was performed according to demographics, immediate post‐operative complications, and economic data, including payor class, length of stay and total charges.
Results
There was a marked shift towards RA‐TKA, from an initial 0.70% in 2016 to a notable 7.30% by 2019. Patients who underwent RA‐TKA were slightly younger (66.2 ± SD years), compared to the C‐TKA group (66.7 ± SD years). Hospital stay was 1.89 days and 2.29 days for RA‐TKA and C‐TKA, respectively. Charges metrics revealed slightly higher charges for RA‐TKA. Less postoperative complications were found in the RA‐TKA group, such as blood loss, anaemia, acute kidney injury, venous thromboembolism, pulmonary embolism, pneumonia and surgical wound complication. Even following the propensity score matching, these findings remained consistent and statistically significant.
Conclusions
RA‐TKA use in the United States has grown substantially in the last few years and has been associated with significantly reduced immediate post‐operative complications and length of hospital stay compared to C‐TKA, offering safer surgical management for TKA patients. Further studies on the short‐ and long‐term outcomes of RA‐TKA would improve the understanding of the full potential of this technology.
Levels of Evidence
Level III.
Keywords: national inpatient sample, post‐operative complications, robotic knee surgery, total knee arthroplasty
Abbreviations
- C‐TKA
conventional total knee arthroplasty
- HCUP
Healthcare Cost and Utilization Project
- ICD‐10
International Classification of Diseases, 10th Revision
- KSS
Knee Society Score
- LOS
length of stay
- NIS
Nationwide Inpatient Sample
- RA‐TKA
robotic‐assisted total knee arthroplasty
- SPSS
Statistical Package for the Social Sciences
- SSI
surgical site infection
- TKA
total knee arthroplasty
- WOMAC
Western Ontario and McMaster Universities Osteoarthritis Index
INTRODUCTION
Robotic‐assisted total knee arthroplasty (RA‐TKA) has been increasingly used in orthopaedic surgery worldwide. Studies indicate potential long‐term advantages, such as faster recovery and enhanced knee mobility, due to the higher precision of alignment achieved with RA‐TKA [10, 13, 15, 22, 32, 33]. A systematic review reported superior clinical outcomes based on WOMAC and KSS in favour of RA‐TKA, though these results are based on a small number of studies [39]. Despite these promising outcomes, the need for RA‐TKA and its full benefits continue to be discussed.
Assessing RA‐TKA requires evaluating not only clinical outcomes but also immediate, short‐term benefits like postoperative complications, hospital costs, and length of stay. In 2011, knee arthroplasty accounted for 718,000 hospitalizations and 4.6% of all operating room procedures in the United States alone, highlighting its significant financial burden, particularly regarding the perioperative period [26, 37]. Thus, the assessment of early post‐operative complications remains an important aspect of TKA.
The number of TKAs has increased constantly throughout the last decades and it will likely continue to do so as life expectancy continues to increase. It has been suggested that by 2030, the demand for TKA will increase to 3.48 million surgeries annually in the United States [7]. Despite numerous advancements in TKA reflected by implant design, materials, recovery programs, pain management, reduction in blood loss, and thromboembolic and antibiotic prophylaxis, up to 20% of patients remain dissatisfied following TKA [1, 18, 28].
The latest evolutions in TKA have focused on advancements in surgical technique by improving accuracy in surgery and respecting patients' anatomy better. Given that surgeon‐controlled variables such as implant positioning, balanced flexion‐extension gaps, ligament tensioning and soft tissue preservation, alongside implant stability and survivorship, are pivotal for clinical outcomes, technological advancements facilitating the precise and reproducible achievement of these technical objectives may significantly enhance TKA outcomes [8, 9, 13, 24, 38].
It is hypothesized that achieving higher precision in planning and executing TKA surgery could lead to a less traumatic procedure. This, in turn, may result in fewer immediate post‐operative complications, shorter hospital stays and ultimately, reduced costs.
MATERIALS AND METHODS
Data set acquisition and inclusion criteria
This study utilized a comprehensive data set extracted from the Nationwide Inpatient Sample (NIS) [11], the largest publicly available all‐payer inpatient care database in the United States. Each entry in the data set, referred to as a ‘case’, represented a group of five patients meticulously matched based on general parameters. The resulting data set, extracted from the most recent version of the NIS, comprised 527,376 cases of TKA, encompassing a cohort of 2,638,679 patients. Notably, the NIS discharge weight indicates that each case extrapolates to five patients. Within this cohort, 88,415 patients underwent RA‐TKA, constituting 3.4% of the total patient population.
Study period and data source
Spanning from 1 January 2016, to 31 December 2019, the data set represents the latest available information within the NIS system at the time of this study. The NIS, a core component of the Healthcare Cost and Utilization Project (HCUP) [7], captures 20% of inpatient stays from HCUP‐associated hospitals, amounting to approximately 7 million unweighted enrolments annually.
Patient identification and exclusions
Patients undergoing TKA were identified based on ICD‐10 coding related to total knee replacement, with a comprehensive list of included codes available in the appendix. Exclusions comprised patients with non‐elective admissions or those who underwent surgery before admission.
Statistical analyses and propensity score matching
Statistical analyses, including crosstabs and independent sample t tests, were conducted using SPSS 26 and MATLAB 2018 to compare RA‐TKA with C‐TKA. A significance level of p < 0.05 was applied. To address potential variations and selection bias, a propensity score‐matched analysis was performed using MATLAB 2018. The refined data set included 34,206 cases (representing 176,830 patients) with comparable characteristics undergoing either RA‐TKA or C‐TKA. Matching was based on various factors, including hospital size, patient location (urban‐rural code), median household income, region of the hospital and the total number of discharges from the hospital in the NIS data set.
Comorbidity identification and data analysis
Comorbidities were identified through a review of patient‐specific ICD‐10 codes, with cases reporting hospital costs of $0 excluded. Analytical studies were conducted using SPSS 26 and Microsoft Excel to visualize annual cases, discern trends, and derive key statistical insights.
Outcome measures and procedure identification
RA‐TKA procedures were delineated using specific ICD‐10‐PCS codes provided in the appendix. Clinical outcomes, including in‐hospital mortality, length of stay, complications and overall hospitalization costs, were analysed using established methodologies.
RESULTS
Within the extensive NIS data set of 527,376 cases, representing 2,638,679 patients, a remarkable increase in RA‐TKA was noticed. A total of 88,415 patients underwent RA‐TKA, comprising 3.4% of the total number of procedures. In 2016, RA‐TKA procedures were performed in only 5330 cases (0.7%) of all TKAs and increased to 39,495 cases (7.3%) by 2019 (Figure 1).
Figure 1.
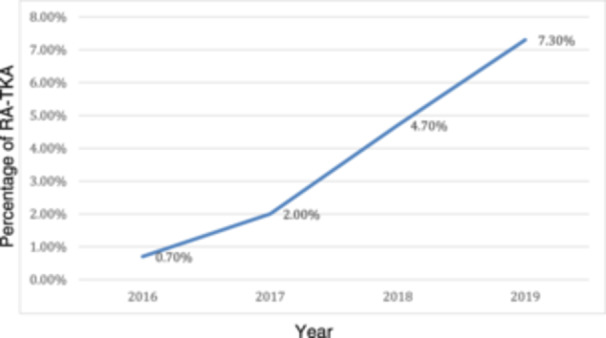
Percentage of robotic‐assisted total knee arthroplasty (RA‐TKA) based on the total number of TKA procedures (2016–2019). This figure illustrates the percentage of RA‐TKA procedures relative to the total number of TKA procedures performed annually between 2016 and 2019.
A comparative analysis of C‐TKA and RA‐TKA across age, payer distribution and gender is presented in Table 1. The average age at the time of surgery was 66.2 ± 9.46 years for the RA‐TKA patients and 66.7 ± 9.48 years for the C‐TKA.
Table 1.
Comparative analysis of conventional total knee arthroplasty (C‐TKA) and robotic‐assisted total knee arthroplasty (RA‐TKA) across age, payer distribution and gender.
| Parameter | RA‐TKA | C‐TKA | Significance |
|---|---|---|---|
| Total surgeries (%) | 3.4 | 96.6 | |
| Average age (years) | 66.23 | 66.7 | p < 0.001 |
| Female (%) | 58.8 | 61.6 | p < 0.001 |
| Payer—Medicare (%) | 54.4 | 57.2 | p < 0.001 |
| Payer—Medicaid (%) | 3.1 | 4.3 | |
| Payer—private (%) | 38.2 | 34.8 | |
| Payer—other (including self‐pay) (%) | 4.2 | 3.7 |
Note: This table provides a comparative analysis of C‐TKA and RA‐TKA across various demographic and healthcare payer parameters.
The payer distribution varies significantly, with a higher percentage of Medicare and Medicaid payers in the C‐TKA group at 57.2% and 4.3%, respectively, compared to 54.4% and 3.1%, respectively, in the RA‐TKA group. The proportion of private payers was higher in the RA‐TKA group) 38.2% (in comparison to the C‐TKA group (34.8%).
The prevalence of various comorbidities in the RA‐TKA and C‐TKA groups is shown in Table 2. C‐TKA demonstrates a higher prevalence of the condition's dyslipidemia, sleep apnoea, chronic anaemia, alcohol abuse, osteoporosis, mental disorders, type 2 diabetes, renal disease and chronic lung disease.
Table 2.
Prevalence of comorbidities in patients undergoing RA‐TKA or C‐TKA.
| RA‐TKA (%) | C‐TKA (%) | Significance | |
|---|---|---|---|
| Hypertension diagnosis | 57.6 | 59.4 | p < 0.0001 |
| Dyslipidemia diagnosis | 44.1 | 46.6 | p < 0.0001 |
| Sleep apnoea diagnosis | 13.8 | 13.2 | p < 0.0001 |
| Chronic anaemia | 4.9 | 5.9 | p < 0.0001 |
| Alcohol abuse | 0.7 | 0.9 | p < 0.0001 |
| Osteoporosis | 3.7 | 4 | p < 0.0001 |
| Mental disorders | 27.9 | 29 | p < 0.0001 |
| Parkinson disease | 0.5 | 0.6 | p = 0.191 |
| Type 2 diabetes | 19.2 | 21.6 | p < 0.0001 |
| Renal disease | 5.5 | 7.1 | p < 0.0001 |
| Congestive heart failure | 1.2 | 1.3 | p = 0.017 |
| Chronic lung disease | 5.0 | 6.0 | p < 0.0001 |
Note: This table displays the prevalence of common comorbidities among patients who underwent either RA‐TKA or C‐TKA.
Abbreviations: C‐TKA, conventional total knee arthroplasty; RA‐TKA, robotic‐assisted total knee arthroplasty.
In order to overcome potential selection bias and baseline differences in terms of existing comorbidities, a propensity score‐matched analysis was performed, ensuring that the two groups compared are statistically equivalent, thus minimizing selection bias. Propensity score‐matched analysis is a statistical method that helps compare two groups in observational studies. It balances participant characteristics by pairing individuals with similar likelihoods of being in either group, making the comparison more reliable and reducing the impact of confounding variables. This approach aims to emulate the random assignment seen in experiments, improving the accuracy of conclusions drawn from non‐randomized studies. It offers insights into demographics, payer details, and the prevalence of various medical conditions, demonstrating the average age, gender distribution, and type of payer, alongside an array of diagnoses, in both the RA‐TKA and C‐TKA groups. The propensity score‐matched analysis data is presented in Table 3. No significant disparities were discerned between the groups in most of the examined parameters, highlighting the homogeneous nature of the two patient cohorts and underlining the effectiveness and reliability of the applied propensity score‐matched analysis.
Table 3.
Comparison of demographic and clinical data in propensity score‐matched cohorts of C‐TKA and RA‐TKA.
| Parameter | RA‐TKA (%) | C‐TKA (%) | Significance |
|---|---|---|---|
| Total surgeries (number) | 88,415 | 88,415 | |
| Average age (years) | 66.23 | 66.34 | p = 0.062 |
| Female (%) | 58.8 | 59.5 | p = 0.147 |
| Payer—Medicare (%) | 54.4 | 55.4 | p = 0.198 |
| Payer—Medicaid (%) | 3.1 | 3.3 | |
| Payer—private (%) | 38.2 | 37.5 | |
| Payer—other (including self‐pay) (%) | 4.2 | 3.8 | |
| Hypertension diagnosis | 57.6 | 58 | p = 0.18 |
| Dyslipidemia diagnosis | 44.1 | 44.6 | p = 0.219 |
| Sleep apnoea diagnosis | 13.8 | 13.4 | p = 0.068 |
| Chronic anaemia | 4.9 | 4.6 | p = 0.211 |
| Alcohol abuse | 0.7 | 0.7 | p = 0.85 |
| Osteoporosis | 3.7 | 3.4 | p = 0.075 |
| Mental disorders | 27.9 | 27.8 | p = 0.923 |
| Parkinson disease | 0.5 | 0.4 | p = 0.19 |
| Type 2 diabetes | 19.2 | 19.2 | p = 0.891 |
| Renal disease | 5.5 | 5.4 | p = 0.702 |
| Chronic heart failure | 1.2 | 1 | p = 0.074 |
| Chronic lung disease | 5 | 4.6 | p = 0.116 |
Note: This table presents a comparison of demographic and clinical data between propensity score‐matched cohorts of patients who underwent C‐TKA and RA‐TKA.
Abbreviations: C‐TKA, conventional total knee arthroplasty; RA‐TKA, robotic‐assisted total knee arthroplasty.
The results in hospitalization time, post‐procedure, and comparison are shown in Table 4 between RA‐TKA and C‐TKA. No significant difference was observed in the mortality rate (p = 1.000). However, significant differences were found in both the average length of stay and the mean total charges in favour of RA‐TKA (p < 0.0001).
Table 4.
Comparison of hospitalization outcomes in propensity score‐matched cohorts of C‐TKA and RA‐TKA.
| RA‐TKA (%) | C‐TKA (%) | Significance | |
|---|---|---|---|
| Died during hospitalization | 0.02% | 0.02% | p = 1 |
| Length of stay mean in days | 1.89 (Std. deviation 1.70) | 2.41 (Std. deviation 1.41) | p < 0.0001 |
| Total charges mean in $ | 65,891 (Std. deviation 41,042) | 62,464 (Std. deviation 38,625) | p < 0.0001 |
Note: This table compares hospitalization outcomes between propensity score‐matched cohorts of patients who underwent C‐TKA and RA‐TKA.
Abbreviations: C‐TKA, conventional total knee arthroplasty; RA‐TKA, robotic‐assisted total knee arthroplasty.
Table 5 presents a comparison of postoperative complications between robotic and non‐robotic surgeries after applying propensity score‐matching to ensure a balanced comparison. Noteworthy are the significant differences in various complications, such as anaemia, acute kidney failure, venous thromboembolism, pulmonary embolism, pneumonia and surgical wound complication, which had significantly lower rates in the RA‐TKA group.
Table 5.
Comparison of postoperative complications in propensity score‐matched cohorts of RA‐TKA and C‐TKA.
| RA‐TKA (%) | C‐TKA (%) | Significance | |
|---|---|---|---|
| Anaemia | 11.508 | 17.073 | p < 0.0001 |
| Acute kidney injury | 1.318 | 1.602 | p = 0.016 |
| Heart failure | 0.096 | 0.064 | p = 0.257 |
| Acute coronary artery disease | 0.057 | 0.036 | p = 0.317 |
| Stroke | 0.006 | 0.006 | p = 1 |
| Pulmonary oedema | 0.028 | 0.058 | p = 0.197 |
| Venous thromboembolism | 0.187 | 0.327 | p = 0.010 |
| Pulmonary embolism | 0.074 | 0.228 | p < 0.0001 |
| Pneumonia | 0.085 | 0.181 | p = 0.018 |
| Surgical wound complication | 0.0283 | 0.5672 | p < 0.0001 |
Note: This table presents a comparison of postoperative complications between propensity score‐matched cohorts of patients who underwent RA‐TKA and C‐TKA.
Abbreviations: C‐TKA, conventional total knee arthroplasty; RA‐TKA, robotic‐assisted total knee arthroplasty.
DISCUSSION
The main finding of this study is that RA‐TKA is associated with significantly reduced early post‐operative complications and length of hospital stay compared to C‐TKA, albeit with slightly higher costs. The rapid adoption of RA‐TKA from 2016 to 2019 demonstrates the increasing acceptance of this technology in clinical practice.
The results of this study are consistent with previous research indicating that RA‐TKA improves surgical precision and patient outcomes [2, 10, 25, 29, 30, 31, 32, 35]. The reduced incidence of complications such as anaemia [36], acute kidney injury, venous thromboembolism, pulmonary embolism, pneumonia, and surgical wound complications in the RA‐TKA group highlights the potential benefits of robotic assistance in reducing surgical trauma and improving recovery [23].
The shorter LOS for RA‐TKA patients (1.89 days) compared to C‐TKA patients (2.41 days) is clinically significant, suggesting that RA‐TKA may facilitate faster recovery and support the concept of outpatient TKA surgery, which is gaining popularity [6, 13, 29, 31]. This reduction in hospital stay is particularly important in the context of increasing healthcare costs and the need for efficient resource utilization.
Despite the higher initial costs associated with RA‐TKA [27] ($65,891 vs. $62,464 for C‐TKA), the reduction in post‐operative complications and shorter hospital stays may offset these costs in the long term [5, 16]. The economic benefits of RA‐TKA could be further explored in future studies, considering the potential savings from reduced readmissions and complications.
Several recent studies support the findings of this study. For instance, Cheng et al. [3] found that robotic‐assisted TKA is associated with the use of thinner polyethylene liners, potentially improving joint function and longevity. Similarly, Erard et al. [8] reported enhanced soft tissue balance with robotic‐assisted TKA, which may contribute to better clinical outcomes. Lee et al. [17] demonstrated that functional alignment maximizes the advantages of robotic arm‐assisted TKA with better patient‐reported outcomes compared to mechanical alignment. Kayani et al. [14] found that robotic‐arm‐assisted TKA is associated with improved forgotten joint scores at 5‐year follow‐up. These findings align with the observed reduction in complications and improved recovery in this study.
Furthermore, Choi et al. [4] demonstrated that functional alignment with robotic‐arm‐assisted TKA results in better patient‐reported outcomes than mechanical alignment with manual TKA. Turan et al. [34] reported coronal alignment improvement with robotic‐assisted techniques, although without significant clinical differences. McCormick et al. [22] showed that robotic‐assisted technology does not influence functional outcomes amongst obese and morbidly obese TKA patients, while Itou et al. [12] found no increased risk of postoperative deep vein thrombosis with robotic‐assisted TKA.
LIMITATIONS
This study has several limitations. The NIS database provides extensive healthcare data, but it may contain errors due to suboptimal coding and manual entry. Additionally, the NIS only provides data for the in‐hospital period, limiting the ability to assess long‐term outcomes [19, 20, 21]. Future studies should include long‐term follow‐up to better understand the full impact of RA‐TKA on patient outcomes.
Another limitation is the potential selection bias, as the choice of surgical technique may be influenced by patient characteristics and surgeon preferences. Although propensity score matching was used to minimize this bias, unmeasured confounding factors may still affect the results. Further research should explore the impact of these factors on the outcomes of RA‐TKA.
Despite these limitations, the strengths of this study include the use of a large, nationally representative data set and the application of rigorous statistical methods to ensure robust and reliable results. The findings contribute to the growing body of evidence supporting the benefits of RA‐TKA in improving patient outcomes and reducing healthcare costs.
CONCLUSION
RA‐TKA has shown substantial growth in usage and is associated with significantly reduced early post‐operative complications and shorter hospital stays compared to C‐TKA. Despite higher initial costs, RA‐TKA offers safer surgical management for TKA patients. Further studies on the short‐ and long‐term outcomes of RA‐TKA would improve the understanding of the full potential of this technology.
AUTHOR CONTRIBUTIONS
David Maman: Conducted major parts of the work, data analysis and manuscript writing. Lior Laver: Manuscript writing. Roland Becker and Yaniv Yonai: Provided clinical expertise. Assil Mahamid: Contributed to manuscript revisions. Loai Ahmad Takrori: Assisted with data validation and analysis. Binyamin Finkel: Participated in data collection and preliminary analysis. Hadar Gan‐Or: Provided support in statistical analysis and validation. Yaron Berkovich: Conceived the study idea and mentored the project.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
The study was conducted under exempt status granted by the institutional review board, and the requirement for informed consent was waived due to the de‐identified nature of the NIS data set.
Supporting information
Supporting information.
ACKNOWLEDGEMENTS
The funding information is not available.
Maman, D. , Laver, L. , Becker, R. , Takrori, L. A. , Mahamid, A. , Finkel, B. et al. (2024) Trends and epidemiology in robotic‐assisted total knee arthroplasty: reduced complications and shorter hospital stays. Knee Surgery, Sports Traumatology, Arthroscopy, 32, 3281–3288. 10.1002/ksa.12353
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the National Inpatient Sample (NIS). However, restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are available from the authors upon reasonable request and with permission of the NIS.
REFERENCES
- 1. Ahmed, I. , Salmon, L.J. , Waller, A. , Watanabe, H. , Roe, J.P. & Pinczewski, L.A. (2016) Total knee arthroplasty with an oxidised zirconium femoral component: ten‐year survivorship analysis. The Bone & Joint Journal, 98(1), 58–64. Available from: 10.1302/0301-620X.98B1.36314 [DOI] [PubMed] [Google Scholar]
- 2. Barbash, G.I. & Glied, S.A. (2010) New technology and health care costs—the case of robot‐assisted surgery. New England Journal of Medicine, 363, 701–704. Available from: 10.1056/NEJMp1006602 [DOI] [PubMed] [Google Scholar]
- 3. Cheng, R. , Kim, B. , Taylor, 4th, W.L. , Westrich, G.H. & Shen, T.S. (2024) Robotic‐assisted total knee arthroplasty is associated with the use of thinner polyethylene liners compared to navigation‐guided and manual techniques. Knee Surgery, Sports Traumatology, Arthroscopy, 1–7. Available from: 10.1002/ksa.12228 [DOI] [PubMed] [Google Scholar]
- 4. Choi, B.S. , Kim, S.E. , Yang, M. , Ro, D.H. & Han, H.S. (2023) Functional alignment with robotic‐arm assisted total knee arthroplasty demonstrated better patient‐reported outcomes than mechanical alignment with manual total knee arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy, 31(3), 1072–1080. Available from: 10.1007/s00167-022-07227-5 [DOI] [PubMed] [Google Scholar]
- 5. Cool, C.L. , Jacofsky, D.J. , Seeger, K.A. , Sodhi, N. & Mont, M.A. (2019) A 90‐day episode‐of‐care cost analysis of robotic‐arm assisted total knee arthroplasty. Journal of Comparative Effectiveness Research, 8(5), 327–336. Available from: 10.2217/cer-2018-0136 [DOI] [PubMed] [Google Scholar]
- 6. Desai, S.S. , Kunes, J.A. , Held, M.B. , Ren, M. , deMeireles, A.J. , Geller, J.A. , et al. (2023) A comparison of pin site complications between large and small pin diameters in robotic‐assisted total knee arthroplasty. Journal of Experimental Orthopaedics, 10(1), 22. Available from: 10.1186/s40634-023-00584-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dreyer, H.C. , Strycker, L.A. , Senesac, H.A. , Hocker, A.D. , Smolkowski, K. , Shah, S.N. et al. (2013) Essential amino acid supplementation in patients following total knee arthroplasty. The Journal of Clinical Investigation, 123, 4654–4666. Available from: 10.1172/JCI70160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Erard, J. , Olivier, F. , Kafelov, M. , Servien, E. , Lustig, S. & Batailler, C. (2024) Enhancing soft tissue balance: Evaluating robotic‐assisted functional positioning in varus knees across flexion and extension with quantitative sensor‐guided technology. Knee Surgery, Sports Traumatology, Arthroscopy, 1–10. Available from: 10.1002/ksa.12255 [DOI] [PubMed] [Google Scholar]
- 9. Fontalis, A. , Kayani, B. , Asokan, A. , Haddad, I.C. , Tahmassebi, J. , Konan, S. et al. (2022) Inflammatory response in robotic‐arm‐assisted versus conventional jig‐based TKA and the correlation with early functional outcomes: Results of a prospective randomized controlled trial. Journal of Bone and Joint Surgery, 104(21), 1905–1914. Available from: 10.2106/JBJS.22.00167 [DOI] [PubMed] [Google Scholar]
- 10. Hampp, E. , Chughtai, M. , Scholl, L. , Sodhi, N. , Bhowmik‐Stoker, M. , Jacofsky, D. et al. (2019) Robotic‐arm assisted total knee arthroplasty demonstrated greater accuracy and precision to plan compared with manual techniques. The Journal of Knee Surgery, 32, 239–250. Available from: 10.1055/s-0038-1641729 [DOI] [PubMed] [Google Scholar]
- 11. Healthcare Cost and Utilization Project (HCUP) (2019) HCUP‐US NIS Overview. Available from: https://www.hcup-us.ahrq.gov/nisoverview.jsp. [Accessed 15th August 2019].
- 12. Itou, J. , Kuwashima, U. , Itoh, M. & Okazaki, K. (2023) Robotic‐assisted total knee arthroplasty is not associated with increased risk of postoperative deep vein thrombosis. Journal of Experimental Orthopaedics, 10(1), 65. Available from: 10.1186/s40634-023-00628-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kayani, B. , Konan, S. , Pietrzak, J.R.T. & Haddad, F.S. (2018) Iatrogenic bone and soft tissue trauma in robotic‐arm assisted total knee arthroplasty compared with conventional jig‐based total knee arthroplasty: a prospective cohort study and validation of a new classification system. The Journal of Arthroplasty, 33, 2496–2501. Available from: 10.1016/j.arth.2018.03.042 [DOI] [PubMed] [Google Scholar]
- 14. Kayani, B. , Fontalis, A. , Haddad, I.C. , Donovan, C. , Rajput, V. & Haddad, F.S. (2023) Robotic‐arm assisted total knee arthroplasty is associated with comparable functional outcomes but improved forgotten joint scores compared with conventional manual total knee arthroplasty at five‐year follow‐up. Knee Surgery, Sports Traumatology, Arthroscopy, 31(12), 5453–5462. Available from: 10.1007/s00167-023-07578-7 [DOI] [PubMed] [Google Scholar]
- 15. Khlopas, A. , Chughtai, M. , Hampp, E.L. , Scholl, L.Y. , Prieto, M. , Chang, T.C. et al. (2017) Robotic‐arm assisted total knee arthroplasty demonstrated soft tissue protection. Surgical Technology International, 30, 441–446. [PubMed] [Google Scholar]
- 16. Khorgami, Z. , Li, W.T. , Jackson, T.N. , Howard, C.A. & Sclabas, G.M. (2019) The cost of robotics: an analysis of the added costs of robotic‐assisted versus laparoscopic surgery using the National inpatient sample. Surgical Endoscopy, 33, 2217–2221. Available from: 10.1007/s00464-018-6507-3 [DOI] [PubMed] [Google Scholar]
- 17. Lee, J.H. , Kwon, S.C. , Hwang, J.H. , Lee, J.K. & Kim, J.I. (2024) Functional alignment maximises advantages of robotic arm‐assisted total knee arthroplasty with better patient‐reported outcomes compared to mechanical alignment. Knee Surgery, Sports Traumatology, Arthroscopy, 32(4), 896–906. Available from: 10.1002/ksa.12120 [DOI] [PubMed] [Google Scholar]
- 18. Luna, I.E. , Kehlet, H. , Peterson, B. , Wede, H.R. , Hoevsgaard, S.J. & Aasvang, E.K. (2017) Early patient‐reported outcomes versus objective function after total hip and knee arthroplasty: a prospective cohort study. The Bone & Joint Journal, 99(9), 1167–1175. Available from: 10.1302/0301-620X.99B9.BJJ-2016-1343.R1 [DOI] [PubMed] [Google Scholar]
- 19. Maman, D. , Laver, L. , Becker, R. , Mahamid, A. & Berkovich, Y. (2024) Robotic‐assisted total knee arthroplasty reduces postoperative complications and length of stay without increased cost compared to navigation-guided techniques: a national analysis. Knee Surgery, Sports Traumatology, Arthroscopy, 1–7. 10.1002/ksa.12348 [DOI] [PubMed] [Google Scholar]
- 20. Maman, D. , Mahamid, A. , Finkel, B. et al. (2024) Comparative evaluation of postoperative outcomes and expenditure between robotic and conventional single-level lumbar fusion surgery: a comprehensive analysis of nationwide inpatient sample data. European Spine Journal. 10.1007/s00586-024-08273-y [DOI] [PubMed] [Google Scholar]
- 21. Maman, D. , Mahamid, A. , Yonai, Y. , Berkovich, Y. (2024) Comparing complication rates, costs, and length of stay between unicompartmental and total knee arthroplasty: insights from a big data analysis using the national inpatient sample dataset. Journal of Clinical Medicine, 13, 3888. 10.3390/jcm13133888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. McCormick, B.P. , Trent, S. , Geng, X. , Lee, J.W. & Boucher, H.R. (2023) Robotic‐assisted technology does not influence functional outcomes among obese and morbidly obese total knee arthroplasty patients. Journal of Experimental Orthopaedics, 10(1), 76. Available from: 10.1186/s40634-023-00634-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nogalo, C. , Meena, A. , Abermann, E. & Fink, C. (2023) Complications and downsides of the robotic total knee arthroplasty: a systematic review. Knee Surgery, Sports Traumatology, Arthroscopy, 31(3), 736–750. Available from: 10.1007/s00167-022-07031-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pando, A. , Hanna, G. & Goldstein, I. (2023) Robotic assistance in lumbar fusion surgery: trends and patterns from 2016–2019. European Spine Journal, 32, 1966–1972. Available from: 10.1007/s00586-023-07663-y [DOI] [PubMed] [Google Scholar]
- 25. Pass, H.I. (2010) Medical registries: continued attempts for robust quality data. Journal of Thoracic Oncology, 5, 198–199. Available from: 10.1097/JTO.0b013e3181dcf957 [DOI] [PubMed] [Google Scholar]
- 26. Pfuntner, A. , Wier, L.M. & Stocks, C. (2013) Most frequent procedures performed in US hospitals, 2010: Statistical Brief# 149. [PubMed]
- 27. Rodrigues Martins, Y.M. , Romanelli de Castro, P. , Drummond Lage, A.P. , Alves Wainstein, A.J. & de Vasconcellos Santos, F.A. (2021) Robotic surgery costs: revealing the real villains. The International Journal of Medical Robotics and Computer Assisted Surgery, 17, e2311. Available from: 10.1002/rcs.2311 [DOI] [PubMed] [Google Scholar]
- 28. Scott, C.E.H. , Turnbull, G.S. , MacDonald, D. & Breusch, S.J. (2017) Activity levels and return to work following total knee arthroplasty in patients under 65 years of age. The Bone & Joint Journal, 99(8), 1037–1046. Available from: 10.1302/0301-620X.99B8.BJJ-2016-1364.R1 [DOI] [PubMed] [Google Scholar]
- 29. Shen, T.S. , Rodriguez, S. , LeBrun, D.G. , Yu, J.S. , Gonzalez Della Valle, A. , Ast, M.P. et al. (2023) Reasons and risk factors for failed same‐day discharge after primary total knee arthroplasty. The Journal of Arthroplasty, 38(4), 668–672. Available from: 10.1016/j.arth.2022.10.044 [DOI] [PubMed] [Google Scholar]
- 30. Skou, S.T. , Roos, E.M. , Laursen, M.B. , Rathleff, M.S. , Arendt‐Nielsen, L. , Simonsen, O. et al. (2015) A randomized, controlled trial of total knee replacement. New England Journal of Medicine, 373(17), 1597–1606. Available from: 10.1056/NEJMoa1505467 [DOI] [PubMed] [Google Scholar]
- 31. Sousa, P.L. , Sculco, P.K. , Mayman, D.J. , Jerabek, S.A. , Ast, M.P. & Chalmers, B.P. (2020) Robots in the operating room during hip and knee arthroplasty. Current Reviews in Musculoskeletal Medicine, 13(3), 309–317. 10.1007/s12178-020-09625-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sultan, A.A. , Samuel, L.T. , Khlopas, A. , Sodhi, N. , Bhowmik‐Stoker, M. , Chen, A. et al. (2019) Robotic‐arm assisted total knee arthroplasty more accurately restored the posterior condylar offset ratio and the Insall‐Salvati index compared to the manual technique: a cohort‐matched study. Surgical Technology International, 34, 409–413. [PubMed] [Google Scholar]
- 33. Thiengwittayaporn, S. , Uthaitas, P. , Senwiruch, C. , Hongku, N. & Tunyasuwanakul, R. (2021) Imageless robotic‐assisted total knee arthroplasty accurately restores the radiological alignment with a short learning curve: a randomized controlled trial. International Orthopaedics, 45(11), 2851–2858. Available from: 10.1007/s00264-021-05179-y [DOI] [PubMed] [Google Scholar]
- 34. Turan, K. , Camurcu, Y. , Kezer, M. , Uysal, Y. , Kizilay, Y.O. , Ucpunar, H. et al. (2023) A comparison of robotic‐assisted and manual techniques in restricted kinematically aligned total knee arthroplasty: coronal alignment improvement with no significant clinical differences. Knee Surgery, Sports Traumatology, Arthroscopy, 31(11), 4673–4679. Available from: 10.1007/s00167-023-07426-8 [DOI] [PubMed] [Google Scholar]
- 35. von Eisenhart‐Rothe, R. , Hinterwimmer, F. , Graichen, H. & Hirschmann, M.T. (2022) Artificial intelligence and robotics in TKA surgery: promising options for improved outcomes. Knee Surgery, Sports Traumatology, Arthroscopy, 30(8), 2535–2537. Available from: 10.1007/s00167-022-07035-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Vandenberk, J. , Mievis, J. , Deferm, J. , Janssen, D. , Bollars, P. & Vandenneucker, H. (2023) NAVIO RATKA shows similar rates of hemoglobin‐drop, adverse events, readmission and early revision vs conventional TKA: a single centre retrospective cohort study. Knee Surgery, Sports Traumatology, Arthroscopy, 31(11), 4798–4808. Available from: 10.1007/s00167-023-07524-7 [DOI] [PubMed] [Google Scholar]
- 37. Weiss, A.J. & Elixhauser, A. (2014) Trends in operating room procedures in US hospitals, 2001–2011: Statistical Brief# 171.
- 38. Young, S.W. , Zeng, N. , Tay, M.L. , Fulker, D. , Esposito, C. , Carter, M. et al. (2022) A prospective randomised controlled trial of mechanical axis with soft tissue release balancing vs functional alignment with bony resection balancing in total knee replacement‐a study using Stryker Mako robotic arm‐assisted technology. Trials, 23(1), 580. Available from: 10.1186/s13063-022-06494-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Zhang, J. , Ndou, W.S. , Ng, N. , Gaston, P. , Simpson, P.M. , Macpherson, G.J. et al. (2022) Robotic‐arm assisted total knee arthroplasty is associated with improved accuracy and patient reported outcomes: a systematic review and meta‐analysis. Knee Surgery, Sports Traumatology, Arthroscopy, 30, 2677–2695. Available from: 10.1007/s00167-021-06464-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Data Availability Statement
The data that support the findings of this study are available from the National Inpatient Sample (NIS). However, restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are available from the authors upon reasonable request and with permission of the NIS.


