Abstract
Vestibular Incision Subperiosteal Tunnel Access (VISTA) root coverage technique has experienced a surge in popularity in recent times. The methodology employed in this study is characterized by its minimally invasive nature, utilizing a single incision. The primary objective of this systematic review was to assess the effectiveness of the VISTA approach for achieving root coverage. The protocol was registered with PROSPERO and included randomized controlled clinical trials where gingival recessions were managed with VISTA technique or its modifications. Among the total of 416 records, a mere 14 studies were initially deemed eligible for consideration. Ultimately, only eight pieces of research were included in the final analysis. There were six studies that exhibited heterogeneity, while two studies showed homogeneity and were therefore included in the meta-analysis. All of the studies considered in the analysis exhibited a moderate to low risk of bias. The majority of the research included in the analysis focused on selective root coverage outcome indicators, while neglecting to incorporate patient-reported outcome measures and patient experienced outcome measures. The VISTA procedure is commonly acknowledged as the most efficacious approach for managing gingival recession. The current literature provides support for the recommendation of the procedure, with evidence of intermediate certainty. The findings of this systematic review indicates that the available data are restricted due to several methodological limitations observed in the included studies. These limitations include, small sample sizes, selective reporting of outcomes, and very short follow-up periods.
Keywords: Gingival recession, Minimally invasive surgical procedures, Patient reported outcome measures, Systematic review
Introduction
Patients seek oral/dental health consultations that relate to various concerns including sensitivity, gingival bleeding, appearance of teeth and soft tissue aesthetics. According to the American Academy of Periodontology (AAP), gingival recession designates the oral exposure of the root surfaces as a result of displacement of the gingival margin apical to cemento-enamel junction. Over the past decades, significant advancements have been made in surgical techniques for correction of not only isolated recession, but also multiple adjacent gingival recessions. Clinicians around the world have witnessed the development of novel surgical techniques and their progressive modifications, that have evolved ever since the first soft tissue grafting procedures were performed in the early 1950s. It is believed that most of the periodontal plastic surgical procedures are clinically predictable and viable options that are available to varied clinical conditions. One such minimally invasive technique, Vestibular Incision Subperiosteal Tunnel Access (VISTA) technique is an example of a procedure that is performed to treat multiple gingival recessions.1 For the purpose of achieving root coverage, the technique has been modified further by the number and location of incisions placed, in addition to its successful results with collagen membrane/matrix, bone replacement grafts, soft tissue grafts, platelet concentrates, chorion membrane, non-pedicled buccal fat pad and the gold standard ‘connective tissue graft’. However; the predictability and long-term stability of reported outcomes in terms of root coverage, increase in the width of attached gingiva and change in the gingival phenotype with this technique are not systematically reported in any of the published studies. Predominantly, case reports and case series with no long-term follow-up and reports with selective reporting of outcomes have been published. The unfinished research is yet another factor that makes the evidence regarding the aforementioned method less compelling. Therefore, this systematic review is a step towards compiling existing data and bringing out the evidence on the effectiveness of this procedure in terms of root coverage achieved.
Review
A detailed protocol was registered in PROSPERO database (Registration Number CRD42023392044) and the same can be accessed in the following link https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=392044. The protocols were based on the 2020 Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines.2 The purpose of this systematic review was to determine the VISTA as an effective method for the management of multiple adjacent gingival recessions.
Problem/participants/population-interventions-comparisons-outcomes – study design (PICOS):
Population – Patients with multiple adjacent gingival recessions (MAGR).
Intervention – VISTA technique and/ or its modifications.
Control – Any other root coverage technique for MAGR management.
Outcome – Reduction in recession height and gain in clinical attachment level.
Inclusion criteria
-
•
Studies carried out from January 2011 to January 2023.
-
•
Randomized controlled clinical trials (RCTs) with VISTA technique and/or its modification as one of its interventions.
-
•
Studies having minimum two groups with one being intervention group.
-
•
Studies having minimum 6 months post-operative follow-up.
-
•
Studies treating Miller's Class I, II, III or Cairo's RT1 and RT2 type marginal tissue recessions.
Exclusion criteria
-
•
Non-randomized trials, Quasi-experimental studies, Pre- and post comparison clinical trials, Pilot clinical trials, Retrospective studies, Cross-sectional studies, Letters to the editor, Case reports, Conference proceedings/paper/poster/abstract publications, Personal communications and any types of reviews were excluded.
-
•
Systematic reviews and meta-analysis.
-
•
Grey literature and unpublished data including thesis/dissertations.
-
•
VISTA for canine disimpaction.
-
•
Duplicate or Redundant publication.
Outcome measures
Primary outcome measures
The primary outcome was to assess the mean reduction in recession height (RH), recession width (RW), pocket probing depth (PPD), clinical attachment level (CAL) gain, mean root coverage (MRC) and complete root coverage (CRC) in both the intervention arm and control arm of included studies using VISTA surgical technique.
Secondary outcome measures
The secondary objective was to report the results in terms of root coverage esthetic (RES) score, complications and patient-reported outcome measures (PROMs).
Search strategy
To identify relevant studies, a thorough electronic search was conducted in the databases viz; Pubmed Central, Pubmed, EMBASE, Google Scholar, Scopus, Medline, Ovidsp, LILACS, HINARI, WoS, EBSCO, Wiley Online, and Cochrane. In addition, manual search in Journal of Periodontology, Journal of Clinical Periodontology and Journal of Periodontal Research was carried out. The MeSH terms used were “VISTA, Gingival Recession and Root Coverage”. The search was conducted on 31 Dec 2022 for the period ranging from January 2011 to December 2022 with the BOOLEAN string VISTA ‘AND’ GINGIVAL RECESSION ‘AND’ ROOT COVERAGE in the Title, Abstract, and Keywords. The duplicates were eliminated from the final search results. The titles and abstracts of the studies were then evaluated independently by two blinded reviewers using the eligibility criteria. The assessment by the third reviewer resolved the conflicts between the two blinded reviewers. The third reviewer contacted the corresponding authors of the articles which were not freely available/accessible via email and requested for the full manuscripts. The full articles of studies included initially were evaluated individually by two reviewers based on inclusion and exclusion criteria and was followed up by the third reviewer. Conflicts arising at the review stage were resolved by a consensus arrived by discussion amongst the three reviewers. Cohen's kappa was used to assess inter-examiner reliability. The appropriate reasons for exclusion of studies at the full article stage were noted. The most comprehensive data for the final studies included was gathered and included.
Data extraction
Two reviewers independently implemented the data assembly and mistyping and erroneous errors were checked for accuracy by the third reviewer. The data extracted from each study included were; second name of first author, year of publication, country, study duration, journal name, trial registration, sample size, gender distribution, number of test sites/control sites, method of sampling, method of randomization, allocation concealment used, blinding/masking, aim and objectives, type of recessions, test and control groups. The outcome measures extracted included; RH, RW, KTW, PPD, CAL, MRC, CRC, RES, incidence of complications and PROMs.
Results
Preliminary screening through database searching identified 416 records and an additional source revealed 19 records. Among 363 records assessed for eligibility, 14 studies were included out of which 06 studies revealed qualitative analysis and 02 studies on quantitative analysis of this review. Fig. 1 shows the flow chart of the reports that were identified, duplicates removed, screened, excluded, assessed for eligibility and included in review as per PRISMA 2020 guidelines.9 The main characteristics of the included studies (Supplementary Table 1) and their parameters were assessed (Supplementary Table 2).
Fig. 1.
Flow chart as per PRISMA 2020 Guidelines.
Data analysis
The software Review Manager (RevMan) Version 5.3 for Windows (The Nordic Cochrane Centre, Copenhagen, Denmark) was utilized for the analysis.6 The mean difference (MD) with a 95% confidence interval (CI) was used to report results for continuous variables. The heterogeneity of studies was evaluated using forest plot, chi-squared homogeneity test and Higgins index (I2). Heterogeneity was regarded as; none (I2 < 25%), low (I2=25% ≥ I2 <50%), moderate (I2=50% ≤ I2 < 75%), or high (I2 ≥ 75%).7 The statistical pooling of data via meta-analysis was only intended for studies deemed sufficiently homogeneous, in terms of methodology and data availability. The risk of bias evaluation and data analysis were carried out by fourth reviewer.
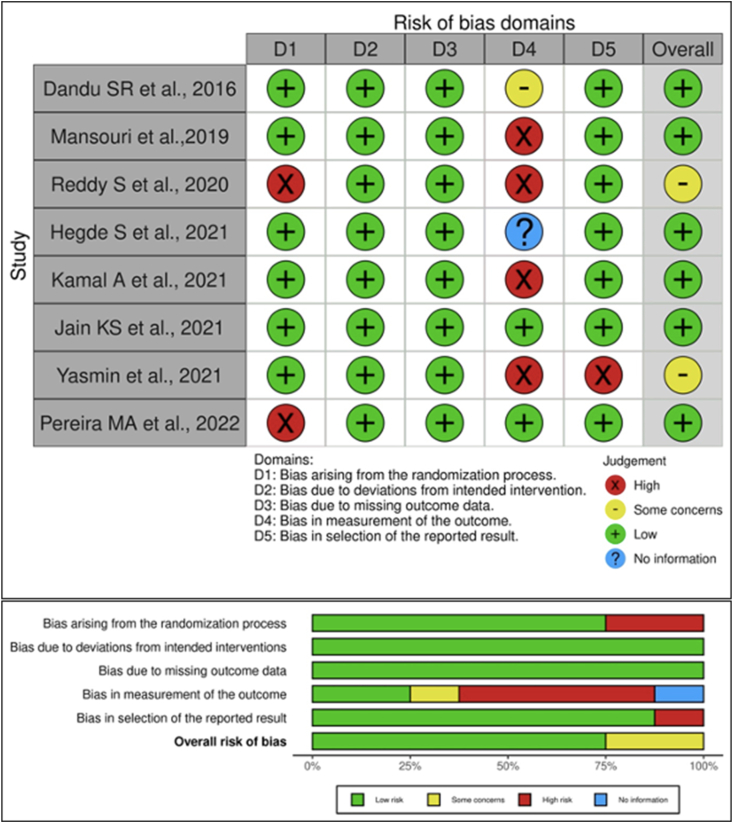
Quality assessment
Two reviewers used Joanna Briggs Institute (JBI) Critical Appraisal Checklist for RCTs to assess the methodological quality of analyzed studies.3 A third reviewer deciphered all the differences in quality assessment. To examine the studies that were included, Cochrane Collaboration's technique was used as guided by the Cochrane Handbook for Systematic Reviews of Interventions (RevMan, version 5.3, The Cochrane Collaboration, Copenhagen, Denmark).4 The risk of bias within studies was estimated using ROBVIS Version 2.0 software as “no information,” “low,” “some concerns” and “high” based on five criteria as; bias arising from the randomization process, bias due to deviation from intended intervention, bias due to missing outcome data, bias in measurement of the outcome, bias in selection of reported result and overall risk assessment.18 The traffic light plot and summary plot were created in accordance with the studies evaluated. The final risk of bias for each study was calculated as follows:
-
•
Low risk of bias: If all the parameters were evaluated to be of “low risk”.
-
•
Moderate risk of bias: If one or more parameters were evaluated to be “unclear or with some concerns”
-
•
High risk of bias: If any of the parameters were evaluated as “high risk”5
Strength of evidence
The “Grading of Recommendations, Assessment, Development, and Evaluation” (GRADE) approach was used to assess the strength of available evidence. The summary of the findings was produced using GRADE online software (Supplementary Table 3) (GRADEpro GTD, Copenhagen, Denmark).8
Risk of bias within included studies
Low risk of bias was observed in one study, unclear risk of bias was observed in four studies and the remaining three studies had a high risk of bias. Among all the included studies, review author's judgments about ‘risk of bias’ was presented (Fig. 2). One study had a low risk of bias10 and four studies had high risk of bias11, 12, 13, 14 for ‘bias in measurement of the outcome’, two studies had high risk of bias arising from the randomization process.12,15 One study had high risk of bias in selection of the reported results.14 Seven studies failed to blind the participants which introduced a high risk of bias. Three studies showed a low risk for selective reporting of outcomes.12,14,16 Only three studies provided details on allocation concealment and blinding was presented only in three studies (single,14 double,11 triple15 each one of them in included studies). Thus, the overall risk of bias was high for the majority of the included studies except for four studies16 which showed an unclear risk of bias and one study showed low risk17 of bias. Only five studies11,13,14,16,17 (5/8) described the random sequence generation and three trials11,14,15 (3/8) described allocation concealment; while detailed information was deficient in other trials. Similarly one trial15 (1/8) provided details relating to blinding of outcome assessment. Only one trial10 (1/8) showed a low risk of bias for incomplete outcome data and selective reporting and majority of the studies11, 12, 13, 14, 15, 16, 17, 18 (7/8) had a low risk of bias. The secondary outcome measures, such as the incidence and management of complications, were not reported in any of included trials. In addition to this, majority of studies did not report the RES, which is one of the most important measures of PROM.
Fig. 2.
Risk of bias within studies and authors’ judgments about each ‘risk of bias’ item presented as percentages across all included studies. Risk of bias summary for reviewing the authors judgments about each risk of bias item for each included study. Green represents low risk of bias, yellow represents unclear risk of bias and red indicates a high risk of bias and blue indicates no or less information.
Synthesis of the main findings
What is the effect of CTG/PRF combined with VISTA technique ?
Two RCTs contributed to this section.10,14 A randomized controlled clinical trial with parallel arm design by Sery et al.14 compared the application of VISTA technique with CTG and PRF in a total of 24 patients (10 males and 18 females) with 24 sites (n = 12/group) in Miller's Class or Cairo's RT2 recessions. The total follow-up period was six months post-operatively. Another randomized controlled clinical trial by Hegde et al.10 also assessed the same methods in 10 patients with 16 sites and follow-up period of 6 months. The meta-analysis was performed only for these two RCTs. One RCT was in favour of CTG combination with VISTA technique and other one did not report any significant differences between PRF and CTG combined with VISTA technique.
Meta-analyses comparing VISTA with CTG and PRF
Two RCTs were included in the meta-analyses for comparison of effectiveness of combination of VISTA technique with CTG and PRF.
Recession height at baseline
The estimate obtained via the random effect model was not statistically significant (z-test p = 0.06), with a mean difference of 0.34 (95% CI, −0.01 to 0.70). The heterogeneity was low (I2 = 30%, chi-squared p = 0.23) (Fig. 3).
Fig. 3.
- Forest plots comparing the recession height at baseline between VISTA with CTG and PRF.
Width of keratinized tissue at baseline
The estimate obtained via the random effect model was statistically significant (z-test p = 0.0005), with a mean difference of 0.87 (95% CI, 0.38 to 1.37). The heterogeneity was low (I2 = 0%, chi-squared p = 0.33) (Fig. 4).
Fig. 4.
Forest plots comparing the width of keratinized tissue at baseline between VISTA with CTG and PRF.
Post-operative reduction of RH in VISTA with CTG Vs PRF at six months
The estimate obtained via the random effect model was statistically significant (z-test p = 0.008), with a mean difference of 0.46 (95% CI, 0.12 to 0.80). The heterogeneity was low (I2 = 0%, chi-squared p = 0.71) (Fig. 5).
Fig. 5.
Forest plots comparing the recession height at six months post-operatively between VISTA with CTG and PRF.
Post-operative changes in WKT in VISTA with CTG Vs PRF at six months
The estimate obtained via the random effect model was not statistically significant (z-test p = 0.76), with a mean difference of 0.08 (95% CI, −0.41 to 0.57). There was substantial heterogeneity (I2 = 59%, chi-squared p = 0.12) (Fig. 6).
Fig. 6.
Forest plots comparing the width of keratinized tissue at six months post-operatively between VISTA with CTG and PRF.
Can VISTA technique be performed alone or in combination for the management of multiple marginal tissue recessions?
The ‘certainty of evidence’ was considered moderate according to the GRADE criteria for MRC. There was serious inconsistency due to clinical and methodological heterogeneity amongst the included studies. The assessment of certainty of evidence is presented in Supplementary Table 3.
Discussion
The VISTA technique offers a novel perspective on deciphering the underlying biological principles of root coverage procedures. The guiding principles include a closed approach, minimally invasive procedure, minimal bone exposure, maximum soft tissue preservation, periosteal vascularity, subperiosteal channel for placement of biomaterials and clot stabilization. This is the first-ever systematic review and meta-analysis to summarize the literature on surgical interventions in root coverage of multiple gingival recessions using VISTA or m-VISTA alone or in combination with various biomaterials. Overall, root coverage has been a topic of interest and the number of literature on VISTA has significantly increased in the last two decades. This synthesis does not aim at establishing the efficacy of VISTA technique in root coverage but, (i) at mapping areas of technical development in the surgical procedures using VISTA technique; (ii) identifying critical components of employed surgical interventions in combination with various biomaterials; (iii) to define application of standard procedures; (iv) to define standards for future research. In general, the available data has incomplete description of specific condition being described i.e gingival recession (recession height, recession width, soft tissue phenotype, width of keratinized tissue, pocket probing depth, clinical attachment level, methodology of measurement of recession parameters and their standardization, full description of the type of recession as per Cairo's classification reported in AAP/EFP 2018 Classification of periodontal diseases), the critical characteristics of surgery (number of incisions, type of suturing), biomaterials used in combination with VISTA technique (type and method of CTG harvesting, type and method of PRF preparation, standardization of PRF protocols), the outcome measures (MRC, CRC, RES), complications involved (incidence and type of complications), and PROMs. Missing information of the critical elements reported in trials leads to misinterpretation among students, academicians and researchers. Some studies compared two different techniques which cannot be actually directly compared and related to the obtained results. Although it is a surgical procedure, it is mandatory to provide an accurate description of the intervention as per CONSORT guidelines.19 Out of the total records screened (n = 416), 363 were excluded based on the selection criteria. Within the 14 selected studies considered for inclusion, two retrospective studies,20,21 two non-randomized trials,12,22,23 and one pre and post comparison trial24 were excluded. Surprisingly, one study had redundant publication of the same set of data twice in two different journals.25 The data also showed that most of the trials done with VISTA technique in combination with any biomaterial, did not compare the technique without the biomaterial. This trend significantly complicated the interpretation of the study results, although positive results have been demonstrated when biologics were added during soft tissue surgical procedures.26 On the contrary, the benefit of additional biologics or growth factors over the long-term effects is questionable with the available amount of literature (Supplementary Fig. 1).27
It is definitely important to highlight that the results obtained in the present systematic review are purely based on the included studies, which showed high heterogeneity and did not permit the conduct of meta-analysis. Moreover, the risk of bias was considered moderate to high in some of the included investigations. The main issues of the published studies was the inherent errors in study methodology. They also included method of sampling, randomization, level of blinding, gender distribution, sample size calculation, and description error of patients vs recession sites as individual units of measurements. The inherent errors in reporting the outcomes were; the selective reporting of outcome measures and non-reporting or non-assessment of the PROMs as true measures of outcome assessment. Based on the evidence in this systematic review, the SORT guidelines for recommendation of the strength of this study was Level B – 2 (Supplementary Fig. 1).
Limitations
A preliminary qualitative study on the evaluation of clinical trials revealed censored criticism, obscured research findings, incomplete or even biased evaluations of trial outcomes and a failure to indicate future research directions.28 In this systematic review, there were some common limitations related to the reporting of the original studies. The included studies in this review reported a plethora of types of gingival recession (Miller's Class I, II and III) despite being aware of the limitations of the Miller's classification, in addition to reporting of Cairo's classification which was also introduced in 2011 and was accepted in the classification of periodontal diseases in 2018.29 In addition to missing baseline data in many studies, the included studies in this systematic review did not report the PROMs except one14 as well as unclear description of measurement of post-operative pain and its management. One of the important parameters which was missed in most studies was the soft tissue phenotype in addition to the presence of hard tissue defects; especially osseous dehiscence which cannot be directly visualized with this technique.30 Additionally, some studies mentioned improvement in gingival phenotype without any mention of methodology used. Another important limitation is the short duration of follow-up of cases averaging only six months, which makes it extremely difficult to predict the long-term effectiveness of the technique. The studies also did not mention about the microsurgical approach being used for the technique which has significant benefits in terms of root coverage outcomes.31 There also exists a difference in the root coverage outcomes of maxillary as compared to mandibular sites which was often overlooked in most of the studies on root coverage procedures. The ‘performance bias’ arises due to unequal distribution of females who normally had demonstrated high standards of oral hygiene.32 The end points of root coverage outcomes should be assessed from an operator's point of view, from the patient’s perspective and the same is ill-defined till date in most root coverage studies and are only presented descriptively which needs to be avoided.21 The studies can be compared only if standardized methodologies are being followed universally19 and due to significant heterogeneity, the meta-analysis could be performed only for two studies that included bilaminar VISTA approach using CTG or PRF which is a significant limitation of this review.10,14 However, the bilaminar techniques combining VISTA approach with either CTG or PRF yielded superior outcomes in terms of MRC outcomes. The impact of selective reporting of outcomes and secondary outcome measures including RES and PROMs were not considered. For example, when sensitivity was presented as chief complaint and reduction of the same is mostly not reported.33 The impact of the source of funding on the outcomes was not assessed in this review. The authors also report that VISTA is not very popularly practiced because of its technique sensitivity as a limitation.
Future studies
It is important to note that ‘surgical procedure’ and ‘surgical technique’ are not synonymous. Surgical technique focuses more on intraoperative implementation as opposed to peri/postoperative care. Surgical technique is eloquently described as the essential element of surgical craft and art. The lack of completeness, specificity and quality of surgical technique reporting severely hinders the evaluation, dissemination and reproducibility of surgical techniques. The EQUATOR NETWORK thereby provides a focused surgical checklist which is ‘IDEAL’ for all clinical specialties, including periodontal plastic surgery.34 Properly designed RCTs with prospective registration of the trial should be performed with complete and detailed description of the study methodology including intricate details regarding study parameters and assessed outcomes. This is the first systematic review in periodontal plastic surgery to assess the effectiveness of VISTA technique and its modifications alone or in combination of soft tissue grafts, platelet concentrates or with other techniques. The available literature was systematically searched, analyzed and summarized using a template and the distribution of evidence was schematically presented with mind map approach. The guidance of clinical decision-making was not within the aim of this systematic review, for which further high-level evidence is required. Of interest is the finding that descriptive research and case reports/series are increasingly published especially when it comes to root coverage procedures., even though it is well understood that RCTs provide higher level of evidence, when conducted systematically.
Conclusion
Based on moderate certainty level, the VISTA technique and its modifications alone or in combination with various soft tissue grafts, substitutes, platelet concentrates, biologics and growth factors are suggested to be used for the management of multiple gingival recessions. However; essential study information on such studies should be reported in depth and with intricate details. The aim of any research is to allow its replication and bring about translational changes in clinical practice. In light of recent insights into the value of reporting guidelines, which guarantee fullness, openness and a unified comprehension; further RCTs should be conducted carefully evaluating all the necessary parameters. The reporting of all essential outcomes in terms of both operator and patient-related outcome measures thereby will increase the methodological quality.
Disclosure of competing interest
All authors have none to declare.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.mjafi.2024.04.010.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
figs1.
References
- 1.Zadeh H.H. Minimally invasive treatment of maxillary anterior gingival recession defects by vestibular incision subperiosteal tunnel access and platelet-derived growth factor BB. Int J Periodontics Restor Dent. 2011;31(6):653–660. [PubMed] [Google Scholar]
- 2.Page M.J., McKenzie J.E., Bossuyt P.M., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Joanna Briggs Institute. Critical appraisal tools. https://jbi.global/critical-appraisal-tools. Accessed on 15 January 2023.
- 4.Cumpston M.S., McKenzie J.E., Welch V.A., Brennan S.E. Strengthening systematic reviews in public health: guidance in the Cochrane Handbook for systematic reviews of interventions, 2nd edition. J Public Health. 2022;44(4):e588–e592. doi: 10.1093/pubmed/fdac036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McGuinness L.A., Higgins J.P.T. Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. 2021;12(1):55–61. doi: 10.1002/jrsm.1411. [DOI] [PubMed] [Google Scholar]
- 6.Cochrane Training. RevMan 5.3. https://training.cochrane.org/online-learning/core-software/revman/revman-5-download. Accessed on 15 January 2023.
- 7.Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brozek J.L., Akl E.A., Alonso-Coello P., et al. GRADE Working Group Grading quality of evidence and strength of recommendations in clinical practice guidelines. Part 1 of 3. An overview of the GRADE approach and grading quality of evidence about interventions. Allergy. 2009;64(5):669–677. doi: 10.1111/j.1398-9995.2009.01973.x. [DOI] [PubMed] [Google Scholar]
- 9.Page M.J., Moher D., Bossuyt P.M., et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160. doi: 10.1136/bmj.n160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hegde S., Madhurkar J.G., Kashyap R., Kumar M.S.A., Boloor V. Comparative evaluation of vestibular incision subperiosteal tunnel access with platelet-rich fibrin and connective tissue graft in the management of multiple gingival recession defects: a randomized clinical study. J Indian Soc Periodontol. 2021;25(3):228–236. doi: 10.4103/jisp.jisp_291_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mansouri S.S., Moghaddas O., Torabi N., Ghafari K. Vestibular incisional subperiosteal tunnel access versus coronally advanced flap with connective tissue graft for root coverage of Miller's class I and II gingival recession: a randomized clinical trial. J Adv Periodontology Implant Dentistry. 2019;11(1):12–20. doi: 10.15171/japid.2019.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Subbareddy B.V., Gautami P.S., Dwarakanath C.D., Devi P.K., Bhavana P., Radharani K. Vestibular incision subperiosteal tunnel access technique with platelet-rich fibrin compared to subepithelial connective tissue graft for the treatment of multiple gingival recessions: a randomized controlled clinical trial. Contemp Clin Dent. 2020;11(3):249–255. doi: 10.4103/ccd.ccd_405_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kamal A., Abdel Meguid Moustafa A., Abdallah Khalil A. Treatment of gingival recession class II defect using buccal fat pad versus platelet rich fibrin using vestibular incision subperiosteal tunnel access technique. Open Access Maced J Med Sci. 2021;9:126–132. doi: 10.3889/oamjms.2021.6536. 2021. [DOI] [Google Scholar]
- 14.Sery Y., Hegab M., Keraa K., El Barbary A., Darhous M. Platelet-Rich fibrin versus connective tissue graft using vestibular incision subperiosteal tunnel access (VISTA) technique in multiple gingival recessions: randomized controlled trial. Periodontics J. 2022;6(1):12–25. doi: 10.26810/perioj.2022.a2. [DOI] [Google Scholar]
- 15.Pereira M.A., Medikeri R.S., Waingade M. A split-mouth randomised controlled trial comparing the clinical effects of MVISTA with chorion membrane or connective tissue graft in multiple gingival recessions. Saudi Dental J. 2023;35(2):178–184. doi: 10.1016/j.sdentj.2022.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dandu S.R., Murthy K.R. Multiple gingival recession defects treated with coronally advanced flap and either the VISTA technique enhanced with GEM 21S or periosteal pedicle graft: a 9-month clinical study. Int J Periodontics Restor Dent. 2016;36(2):231–237. doi: 10.11607/prd.2533. [DOI] [PubMed] [Google Scholar]
- 17.Jain K.S., Vaish S., Gupta S.J., Sharma N., Khare M., Nair M.M. Minimally invasive treatment of gingival recession by vestibular incision subperiosteal tunnel access technique with collagen membrane and advanced platelet-rich fibrin: a 6-month comparative clinical study. J Indian Soc Periodontol. 2021;25(6):496–503. doi: 10.4103/jisp.jisp_590_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zeng X., Zhang Y., Kwong J.S., et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evidence-based Med. 2015;8(1):2–10. doi: 10.1111/jebm.12141. [DOI] [PubMed] [Google Scholar]
- 19.Dwan K., Altman D.G., Cresswell L., Blundell M., Gamble C.L., Williamson P.R. Comparison of protocols and registry entries to published reports for randomised controlled trials. Cochrane Database Syst Rev. 2011;2011(1):MR000031. doi: 10.1002/14651858.MR000031.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gil A., Bakhshalian N., Min S., Nart J., Zadeh H.H. Three-dimensional volumetric analysis of multiple gingival recession defects treated by the vestibular incision subperiosteal tunnel access (VISTA) procedure. Int J Periodontics Restor Dent. 2019;39(5):687–695. doi: 10.11607/prd.4313. [DOI] [PubMed] [Google Scholar]
- 21.Lee C.T., Lange M., Jureidini A., Bittner N., Schulze-Späte U. Clinical and patient-reported outcomes after recession coverage using modified vestibular incision subperiosteal tunnel access with a volume-stable collagen matrix as compared to a coronally advanced flap with a subepithelial connective tissue graft. J periodontal Implant Sci. 2022;52(6):466–478. doi: 10.5051/jpis.2105760288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mohamed A.D., Marssafy L.H. Comparative clinical study between Tunnel and VISTA approaches for the treatment of multiple gingival recessions with acellular dermal matrix allograft. Egypt Dent J. 2020;66:247–259. doi: 10.21608/edj.2020.77540. [DOI] [Google Scholar]
- 23.Rajeswari S.R., Triveni M.G., Kumar A.B.T., Ravishankar P.L., Rajula M.P.B., Almeida L. Patient-centered comparative outcome analysis of platelet-rich fibrin-reinforced vestibular incision subperiosteal tunnel access technique and Zucchelli's technique. J Indian Soc Periodontol. 2021;25(4):320–329. doi: 10.4103/jisp.jisp_187_2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Iv C., Neichev D., Vicheva D., Atanosov D., Noncheva V. Vista technique and platelet-rich fibrin membrane for treatment of multiple adjacent gingival recessions - 6-month follow-up. IOSR J Dent Med Sci. 2016;15:128–133. doi: 10.9790/0853-15075128133. [DOI] [Google Scholar]
- 25.Kamal A., Abdel Meguid Moustafa A., Abdallah Khalil A. Treatment of gingival recession class II defect using buccal fat pad versus platelet rich fibrin using vestibular incision subperiosteal tunnel access technique. Open Access Macedonian J Med Sci. 2021;9(D):126–132. doi: 10.3889/oamjms.2021.6536. [DOI] [Google Scholar]
- 26.Miron R.J., Fujioka-Kobayashi M., Bishara M., Zhang Y., Hernandez M., Choukroun J. Platelet-Rich fibrin and soft tissue wound healing: a systematic review. Tissue Eng B Rev. 2017;23(1):83–99. doi: 10.1089/ten.TEB.2016.0233. [DOI] [PubMed] [Google Scholar]
- 27.Miron R.J., Moraschini V., Del Fabbro M., et al. Use of platelet-rich fibrin for the treatment of gingival recessions: a systematic review and meta-analysis. Clin Oral Invest. 2020;24(8):2543–2557. doi: 10.1007/s00784-020-03400-7. [DOI] [PubMed] [Google Scholar]
- 28.Horton R. The hidden research paper. JAMA. 2002;287(21):2775–2778. doi: 10.1001/jama.287.21.2775. [DOI] [PubMed] [Google Scholar]
- 29.Pini-Prato G. The Miller classification of gingival recession: limits and drawbacks. J Clin Periodontol. 2011;38(3):243–245. doi: 10.1111/j.1600-051X.2010.01655.x. [DOI] [PubMed] [Google Scholar]
- 30.Kim D.M., Bassir S.H., Nguyen T.T. Effect of gingival phenotype on the maintenance of periodontal health: an American Academy of Periodontology best evidence review. J Periodontol. 2020;91(3):311–338. doi: 10.1002/JPER.19-0337. [DOI] [PubMed] [Google Scholar]
- 31.Burkhardt R., Lang N.P. Coverage of localized gingival recessions: comparison of micro- and macrosurgical techniques. J Clin Periodontol. 2005;32(3):287–293. doi: 10.1111/j.1600-051X.2005.00660.x. [DOI] [PubMed] [Google Scholar]
- 32.Chambrone L., Garcia-Valenzuela F.S., Avila-Ortiz G. Errors and complications in clinical periodontal practice due to methodologic bias and bad interpretation of the evidence. Periodontol. 2023;92(1):373–381. doi: 10.1111/prd.12475. 2000. [DOI] [PubMed] [Google Scholar]
- 33.Souza N.V., Nicolini A.C., Dos Reis I.N.R., Sendyk D.I., Cavagni J., Pannuti C.M. Selective outcome reporting bias is highly prevalent in randomized clinical trials of nonsurgical periodontal therapy. J Periodontal Res. 2023;58(1):1–11. doi: 10.1111/jre.13066. [DOI] [PubMed] [Google Scholar]
- 34.Bilbro N.A., Hirst A., Paez A., et al. IDEAL Collaboration Reporting Guidelines Working Group The IDEAL reporting guidelines: a delphi consensus statement stage specific recommendations for reporting the evaluation of surgical innovation. Ann Surg. 2021;273(1):82–85. doi: 10.1097/SLA.0000000000004180. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.