Abstract
Nerve transfer surgery has emerged as a promising approach to restoring function in paralyzed muscles. The trapezius plane block (TPB) blocks the thoracic branches of the posterior primary rami, providing extended analgesia in nerve transfer surgeries. The case report describes the analgesia profiling of a young man who suffered a traumatic pan-brachial plexus injury and underwent a spinal accessory nerve to the suprascapular nerve transfer. TPB was utilized as a part of multimodal analgesia. TPB represents an advancement in regional anesthesia, providing extended analgesia and reducing opioid consumption. TPB can promote patient comfort and facilitate early mobilization.
Keywords: Fascial plane block, nerve transfer surgery, neuromonitoring, trapezius plane block
Introduction
In recent times, nerve transfer surgeries have gained increasing popularity as an effective means of restoring function in paralyzed muscles. Nerve transfer surgery involves implanting a functional peripheral nerve to supply a paralyzed muscle, thereby bypassing the damaged nerve.[1] Transfer of the spinal accessory nerve to the suprascapular nerve is a common procedure performed to reestablish shoulder motion in patients with total brachial plexus palsy and is often performed via a dorsal approach through a suprascapular incision.[2,3] Neuromonitoring with a peripheral nerve stimulator is desired for intraoperative identification of the nerve. Conventional general anesthesia with muscle relaxants can interfere with neuromonitoring. Intraoperative nerve stimulation can also lead to an increased incidence of postoperative pain. Successful outcomes of these surgeries depend upon many factors, such as precise identification of the target nerve to be transferred, adequate perioperative pain control, and implementation of early rehabilitation.[4] Hence, pain management plays a crucial role. Adequate intraoperative analgesia can reduce the requirement for opioid analgesics and reduce the incidence of complications, such as nausea, constipation, and postoperative respiratory depression. Adequate postoperative pain management can optimize patient comfort, promote early recovery, and reduces postoperative complications.[5] It can also decrease the length of hospital stay, thereby reducing the costs of healthcare and enhancing resource utilization. One emerging technique that holds promise in this domain is the trapezius plane block (TPB), a regional anesthetic technique that targets the thoracic branches of the posterior primary rami. It can provide effective pain relief in surgeries involving the trapezius muscle. It involves the deposition of local anesthetic solution into the plane between the superior aspect of the trapezius muscle and the superficial fascia covering the muscle.[6] Initially, it was described in shoulder surgeries and is commonly used for chronic pain interventions. This case report highlights the potential benefit of the use of TPB in perioperative pain management for a dorsal approach to spinal accessory to suprascapular nerve transfer in a patient with a brachial plexus injury.
Informed written consent was obtained from the patient for the use of the patient’s data and images for publication.
Case Description
A 27-year-old man, weighing 68 kg, sustained a pan right brachial plexus injury following a road traffic accident 10 months back. The patient had motor weakness in the right upper limb with a power of 0/5 in the right shoulder, elbow, wrist, and fingers. The patient was unable to perform shoulder abduction, adduction, and external rotation. The primary goal of the surgery was to restore function in the right shoulder and a nerve transfer of the right spinal accessory nerve to the right suprascapular nerve was planned. The patient did not have any other concomitant injuries, was free from chronic illness, and was categorized under American Society of Anaesthesiology (ASA) physical status 2. He complained of pain over the right upper limb ever since the accident, which was burning in nature, associated with numbness and tingling, which was poorly controlled on over-the-counter analgesics. His pain was 5/10 on the numerical rating scale and the Self-Assessment Leeds Assessment of Neuropathic Symptoms and Signs (S-LANSS) Pain Scale was more than 12. In the operating room, ASA standard monitors and bispectral index (BIS) monitoring were attached. General anesthesia was induced using the following medications: Inj. Glycopyrrolate 0.2 mg intravenous (IV), Inj. Midazolam 1 mg IV, Inj. Fentanyl 70 mcg IV followed by propofol infusion initiated with a target control infusion pump using the Marsh protocol, with a target plasma concentration of 4 mcg/ml. Simultaneously, pre-oxygenation was done with 100% oxygen and following a loss of consciousness and a BIS of 40, Inj. Succinylcholine 100 mg IV was administered, and a cuffed endotracheal tube was placed. The patient was put on a volume-controlled mode of ventilation with tidal volume 420 ml, frequency 12 per minute, and positive end expiratory pressure (PEEP) 4 hPa. The patient was then placed in the prone position. Thereafter, a right-sided trapezius plane block with 0.2% ropivacaine 20 ml and dexamethasone 4 mg was given under ultrasound guidance [Figure 1]. Propofol infusion was continued, and the target plasma concentration was titrated between 3 mcg/ml and 4 mcg/ml based on the hemodynamic parameters and a target BIS of 40 - 60. Intraoperatively, the parameters noted were heart rate, non-invasive blood pressure, SpO2, and BIS. An incision was given for the posterior/dorsal approach to the spinal accessory nerve, as shown in Figure 2a. The suprascapular area was dissected, the supraspinatus ligament was identified [Figure 2b], and the right suprascapular nerve was isolated. Thereafter, a peripheral nerve stimulator was employed for precise identification of the spinal accessory nerve. A current of 3.5 mAmp was delivered to the nerve, and twitches were noted in the trapezius muscle, indicating that the fascial plane block administered did not interfere with the use of the nerve stimulator intraoperatively. The intraoperative course was uneventful, and the hemodynamics remained within 20% of the patient’s baseline [Figure 3]. The total duration of surgery was 3.5 hours, thereafter the patient was weaned from mechanical ventilation and shifted to the post-anesthesia care unit. The Numerical Rating Scale (NRS) score at the 1-hour postoperative period was 1 and at the 6-hour postoperative period was 2. The analgesia plan included intravenous acetaminophen 1 g eight hourly, Tab pregabalin + nortryptomer (75/10 mg) at bedtime, and 50 mg of tramadol IV for breakthrough pain. The time to first rescue analgesia was 14 hours. The cumulative dose of tramadol required in the first 72 hours of surgery was 200 mg. The patient was discharged on the 5th postoperative day and was enrolled in a neurorehabilitation program at our Center and is presently being managed on an outpatient basis.
Figure 1.
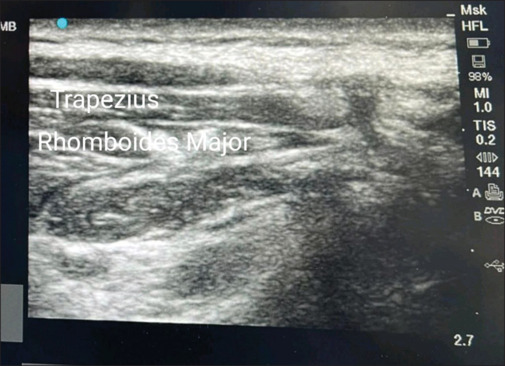
Ultrasound image showing the different layers of tissue for the trapezius plane block
Figure 2.
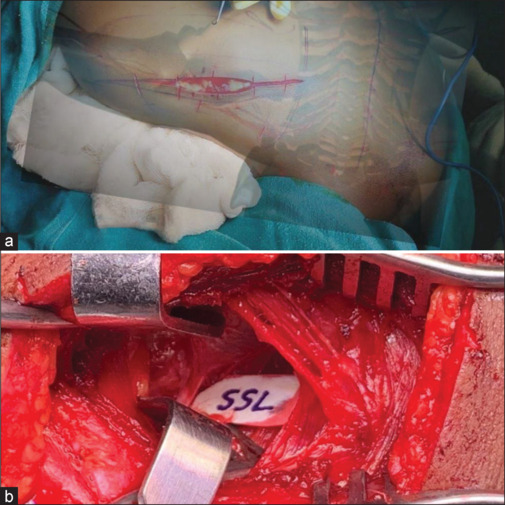
(a) Illustration showing the surgical incision for the dorsal approach for the spinal accessory to suprascapular nerve transfer with the patient in the prone position. The bony landmarks, such as the spine and scapula, have been overlapped onto the surgical image, to add perspective. (b) Image of the surgical field showing the supraspinatus ligament (SSL)
Figure 3.

Image showing the trend of hemodynamics intraoperatively
Discussion
The prognosis of nerve transfer surgeries depends upon many factors. The provision of adequate intraoperative and postoperative analgesia can have a huge positive impact in such cases. Any new technique employed should have the main advantage of non-interference with the use of a peripheral nerve stimulator. Successful administration of trapezius plane block has been shown to decrease the intraoperative requirement of opioid analgesics. The main advantage of this block is its efficacy in nerve transfer surgeries without interference with the use of a peripheral nerve stimulator. The provision of adequate analgesia also maintains hemodynamic stability throughout the surgery. The use of TPB was earlier described in myofascial pain, where administration of local anesthetic in the interfacial plane was shown to reduce the Visual Analog Scale (VAS) score post-injection.[7] The TPB has also been used in superficial surgeries of the posterior hemithorax and has been concluded to have a wider area of analgesia when compared to infiltration of local anesthetic at the surgical site.[6] As the use of TPB in nerve transfer surgeries gains traction, further research is warranted to optimize the technique’s efficacy and determine its long-term benefits. Studies focusing on patients’ postoperative pain outcomes, postoperative rehabilitation, and quality of life measures will help elucidate the full potential of TPB as part of a comprehensive perioperative pain management strategy.
Glossary
TPB – Trapezius Plane Block
ASA - American Society of Anaesthesiology
S-LANSS - Self-Assessment Leeds Assessment of Neuropathic Symptoms and Signs Pain Scale
PEEP – Positive End Expiratory Pressure
BIS – Bispectral Index
IV – Intravenous
NRS – Numerical Rating Scale
VAS – Visual Analog Scale
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Karamanos E. Nerve transfer surgery for penetrating upper extremity injuries. Permanente J. 2018;22:17–156. doi: 10.7812/TPP/17-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tahir H, Osama M, Beg MSA, Ahmed M. Comparison of anterior vs. dorsal approach for spinal accessory to suprascapular nerve transfer in patients with a brachial plexus injury and its outcome on shoulder function. Cureus. 2022;14:e26543. doi: 10.7759/cureus.26543. doi: 10.7759/cureus.26543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bertelli JA, Ghizoni MF. Results of spinal accessory to suprascapular nerve transfer in 110 patients with complete palsy of the brachial plexus. J Neurosurg Spine. 2016;24:990–5. doi: 10.3171/2015.8.SPINE15434. [DOI] [PubMed] [Google Scholar]
- 4.M FG, M M, S H, Khan WS. Peripheral nerve injury: Principles for repair and regeneration. Open Orthopaedics J. 2014;8:199–203. doi: 10.2174/1874325001408010199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chitnis SS, Tang R, Mariano ER. The role of regional analgesia in personalized postoperative pain management. Korean J Anesthesiol. 2020;73:363–71. doi: 10.4097/kja.20323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Del Buono R, Costa F, Pascarella G, Basso V, Doyle JD, Agrò FE. The trapezius plane block. Eur J Anaesthesiol. 2018;35:401–2. doi: 10.1097/EJA.0000000000000721. [DOI] [PubMed] [Google Scholar]
- 7.Domingo T, Blasi J, Casals M, Mayoral V, Ortiz-Sagristá JC, Miguel-Pérez M. Is interfascial block with ultrasound-guided puncture useful in treatment of myofascial pain of the trapezius muscle? Clin J Pain. 2011;27:297–303. doi: 10.1097/AJP.0b013e3182021612. [DOI] [PubMed] [Google Scholar]


