Highlights
-
•
Out-of-hospital cardiac arrest (OHCA) treatment and outcomes vary significantly by municipality in Connecticut.
-
•
Municipality population size greater than 100,000 and predominantly non-English-speaking communities were associated with lower rates of bystander CPR.
-
•
Non-English-speaking, low per capita income and Hispanic communities were associated with lower rates of bystander AED use.
-
•
High population size, low English language use, low per capita income and increased Hispanic community make-up were associated with decreased survival with favorable neurological function.
-
•
Statewide and community OHCA outcomes in Connecticut might be improved by campaigns targeting urban population centers and Hispanic communities with culturally sensitive, low or no-cost CPR and AED educational programs using instructional languages other than English.
Keywords: Out-of-hospital cardiac arrest, Cardiopulmonary resuscitation, Bystander intervention, Community health, Health disparities, Social determinants of health
Abstract
Background
Prior reports have demonstrated underutilization of bystander cardiopulmonary resuscitation (CPR) and automated external defibrillator (AED) use in patients with witnessed out-of-hospital cardiac arrest (OHCA) in Connecticut. This study aimed to identify community-level risk factors that contribute to low rates of bystander intervention to improve statewide OHCA outcomes.
Methods
We analyzed 2,789 adult patients with witnessed, non-traumatic OHCA submitted to the Connecticut Cardiac Arrest Registry to Enhance Survival (CARES) between 2013–2022. Patients were grouped by zip code, and associated municipal characteristics were acquired from 2022 United States Census Bureau data. Use of bystander CPR, attempted bystander AED defibrillation, and patient survival with favorable neurological function were determined for 19 of the 20 most populous cities and towns. Pearson correlation tests and linear regression were used to determine associations between OHCA treatment and outcomes with population size, racial/ethnic demographics, language use, income, and educational level.
Results
Bystander CPR was lower in municipalities with population size > 100,000 and in communities where > 40% of residents are non-English-speaking. AED use was also lower in these municipalities, as well as those with per capita incomes < $40,000 or > 1/3 Hispanic residents. Communities with populations > 100,000, > 40% non-English-speaking, per capita income < $40,000, and > 1/3 Hispanic residents were all associated with lower survival rates.
Conclusions
OHCA pre-hospital treatment and outcomes vary significantly by municipality in Connecticut. Community outcomes might be improved by specifically targeting urban population centers and Hispanic communities with culturally sensitive, low, or no-cost CPR and AED educational programs, using instructional languages other than English.
Introduction
Out-of-hospital cardiac arrest (OHCA) occurs in approximately 350,000 patients each year in the United States and is associated with a high rate of morbidity and mortality.1 Data from the Cardiac Arrest Registry to Enhance Survival (CARES) [https://mycares.net] reveals that approximately 9% of patients with OHCA who receive care by emergency medical services (EMS) will survive to hospital discharge in the United States and fewer will survive with good neurological function. Bystander administration of cardiopulmonary resuscitation (CPR) and bystander use of automatic external defibrillators (AEDs) are interventions associated with improved survival and neurological outcomes for patients who have witnessed OHCA.2 However, these pre-hospital interventions, components of the American Heart Association chain of survival, are not consistently used across communities in the United States.3, 4, 5
In Connecticut, statistics for use of bystander CPR, public AED use and OHCA survival trail 2022 national norms published by CARES.6 As a state with a diverse population with over 20% of residents identifying as non-White, our group has additionally published data demonstrating that Black and Hispanic OHCA victims received less bystander CPR and early attempted defibrillation, with lower overall survival and worse neurological outcomes.7 Of note, statewide census tract data further demonstrated that minority bystander CPR rates were lower in affluent and integrated communities.7
To design actionable strategies that might improve statewide OHCA outcomes, it is important to understand and address potential causes for community-level variation in pre-hospital treatment and outcomes for witnessed OHCA. We established a state-wide data sharing collaboration for EMS and hospital system contributors with the Connecticut CARES registry that enabled identification of the zip code for witnessed OHCA between 2013 and 2022. We hypothesized that socioeconomic indices previously reported to be associated with bystander intervention, such as population size, race/ethnicity, primary spoken language, income and education level,4, 5, 8, 9, 10, 11, 12 would be associated with successful bystander resuscitation and overall patient survival in a given municipality. We further hypothesized that future community-specific strategies to address individual municipality deficiencies in OHCA care might contribute to overall improved performance on a statewide level.
Methods
Study design
This retrospective, observational study was approved by the Hartford Hospital Institutional Review Board, which waived the requirement for informed consent.
Data acquisition
Out-of-hospital cardiac arrest data was acquired through CARES for Connecticut residents from 2013 to 2022. Inclusion criteria included witnessed non-traumatic cardiac arrests in adult patients where resuscitation was attempted. All OHCA events were witnessed either by bystanders or non-EMS 9-1-1 responders. Data were grouped by zip code and then by municipality. Municipal characteristics were acquired through United States Census Bureau QuickFacts for 2022 [https://census.gov/quickfacts]. These include data on population size, race/ethnicity (White, Black, Hispanic), primary language, median household and per capita income, poverty levels, and education levels (high school graduate or higher, bachelor’s degree or higher).
Study population
CARES is a prospective and multicenter national registry of OHCA that uses standardized Utstein reporting. This study used statewide data from this registry, which was obtained from a variety of EMS systems. Telephone CPR is a statewide standard of care.
The Connecticut CARES dataset contained 10,486 persons with OHCA between January 1, 2013, and December 31, 2022. We excluded 6,019 unwitnessed arrests, 200 pediatric arrests, and 1 person with a zip code that was not reported. Data analyses were performed on Connecticut municipalities that ranked within the top 20 largest cities and towns by population size. One municipality which did not participate in CARES was excluded. The final study cohort consisted of 2,789 witnessed OHCA patients, representing 19 of the 20 largest municipalities in Connecticut.
Study outcomes
The primary outcomes included: 1) bystander CPR; 2) attempted bystander electrical defibrillation with an AED; 3) achievement of sustained Return of Spontaneous Circulation (ROSC); and 4) survival to hospital discharge with favorable neurological outcome. Bystander CPR was defined as CPR initiated by a family member or other person who was not a 911 responder and where the OHCA location was not a healthcare facility or nursing home and OHCA was not witnessed by a 911 responder. Attempted bystander electrical defibrillation was defined as AED application and delivery of at least one shock by a bystander. Favorable neurological outcome was defined by a discharge Cerebral Performance Category Score of 1 or 2 out of 5, where 1 denotes “no to mild neurological disability” and 2 denotes “moderate disability”.3, 13
Statistical analysis
Continuous variables were expressed as mean ± SD or median (interquartile range) and categorical variables were expressed as percentages. D'Agostino-Pearson omnibus K2 tests revealed normal distribution for the majority of continuous variables, excluding municipal income data as well as single outliers within sustained ROSC and bystander AED data. Multiple regression analysis revealed a relationship between municipal population size and non-English language (p = 0.019), but not per capita income (p = 0.481) or Hispanic ethnicity (p = 0.201).
Hypothesizing that larger, more diverse, and less affluent municipalities face additional challenges influencing study outcomes, 1-tailed Pearson correlation tests were completed between each of the independent municipal variables (population size, non-English primary language, per capita income, median household income, persons in poverty, White race, Black race, Hispanic ethnicity, high school diploma, bachelor’s degree) and the following dependent outcomes from the CARES registry: bystander CPR percentage, bystander AED use with attempted defibrillation percentage, sustained ROSC percentage, and percentage of survival to discharge with favorable neurological outcome. Correlation coefficients (r) and p-values were calculated for all tests.
Variables with statistically significant linear correlations with any of the dependent outcomes were further analyzed to generate pooled odds ratios (OR) with 95% confidence intervals (CI) for each of the following cutoffs. These included population size > 100,000, primary spoken language other than English in > 40% of the community, per capital income < $40,000 and > 1/3 of the community identifying as Hispanic.
Microsoft Excel version 2019, GraphPad Prism 10, and SPSS version 26.0 were used for all analyses, with statistical significance set at p < 0.05.
Results
Correlation of municipal socioeconomic factors with bystander interventions and patient outcomes
Among 19 of the 20 largest Connecticut municipalities, bystander CPR rate ranged from 18.2 to 68.2%, AED use with attempted defibrillation prior to EMS arrival ranged from 1.4 to 29.4%, sustained ROSC ranged from 31.5 to 62.7%, and survival to discharge with favorable neurological function ranged from 6.2 to 25.9%. A Pearson correlation test matrix was constructed to analyze significant associations between municipal census statistics with bystander interventions and patient outcomes (Table 1). Census statistics and cardiac arrest outcomes are presented in quartiles by municipal population size in Table 2.
Table 1.
Pearson correlation test matrix between municipal statistics and four outcome measures from the CARES registry. Top table reports p-values and bottom table reports correlation coefficient (r) of each test. Statistically significant p-values and their associated r values are bolded in red text for emphasis.
| P-Value | Population Size | Per Capita Income | Median Household Income | Persons in Poverty | Non-English Primary Language | White | Black | Hispanic/ Latino |
High School Diploma | Bachelor's Degree |
|---|---|---|---|---|---|---|---|---|---|---|
| Bystander CPR [%] | 0.0428 | 0.1410 | 0.1236 | 0.0777 | 0.2941 | 0.1259 | 0.2079 | 0.2056 | 0.0906 | 0.2446 |
| Bystander AED [%] | 0.4568 | 0.3912 | 0.3511 | 0.2582 | 0.0457 | 0.2099 | 0.3645 | 0.0499 | 0.1246 | 0.1809 |
| Sustained ROSC [%] | 0.1442 | 0.0481 | 0.0801 | 0.1913 | 0.3477 | 0.1860 | 0.0896 | 0.1999 | 0.1234 | 0.0965 |
| Survival (CPC 1–2) [%] | 0.0484 | 0.4555 | 0.4053 | 0.2340 | 0.1171 | 0.1833 | 0.2849 | 0.1083 | 0.0950 | 0.2931 |
| Correlation Coefficient (r) | Population Size | Per Capita Income | Median Household Income | Persons in Poverty | Non-English Primary Language | White | Black | Hispanic/ Latino |
High School Diploma | Bachelor's Degree |
|---|---|---|---|---|---|---|---|---|---|---|
| Bystander CPR [%] | −0.4048 | 0.2602 | 0.2791 | −0.3391 | −0.1327 | 0.2766 | −0.1983 | −0.2002 | 0.3203 | 0.1690 |
| Bystander AED [%] | −0.0267 | 0.0679 | 0.0939 | −0.1587 | −0.3980 | 0.1966 | −0.0851 | −0.3890 | 0.2780 | 0.2217 |
| Sustained ROSC [%] | −0.2568 | 0.3928 | 0.3355 | −0.2124 | −0.0961 | 0.2170 | −0.3218 | −0.2051 | 0.2794 | 0.3123 |
| Survival (CPC 1–2) [%] | −0.3921 | 0.0275 | 0.0589 | −0.1772 | −0.2866 | 0.2194 | −0.1392 | −0.2972 | 0.3143 | 0.1333 |
Table 2.
Each of the four significant census statistics and each of the four outcomes from the CARES registry are presented for each municipality on Connecticut, arranged by quartiles. Municipalities are ordered by descending population. Numbers represent medians plus interquartile ranges.
| Quartile 1 | Quartile 2 | Quartile 3 | Quartile 4 | |
|---|---|---|---|---|
| Population Size | 136,188 (115,016–148,377) | 64,271 (62,871–91,401) | 60,242 (55,004–61,330) | 50,595 (48,729–52,477) |
| Per Capita Income [$] | 29,506 (25,229–60,109) | 67,164 (28,796–122,697) | 40,984 (37,740–43,753) | 45,526 (32,527–59,735) |
| Non-English [%] | 42.1 (33.3–48.4) | 25.2 (14.6–48.7) | 22.3 (18.6–30.6) | 16.5 (12.0–39.1) |
| Hispanic/Latino [%] | 35.9 (29.8–46.1) | 14.1 (4.4–44.3) | 20.3 (13.7–37.1) | 12.3 (7.7–37.3) |
| Bystander CPR [%] | 28.8 (18.2–43.9) | 43.5 (32.9–46.4) | 34.3 (20.0–41.1) | 46.4 (31.1–66.7) |
| Bystander AED [%] | 11.6 (9.9–14.0) | 7.6 (2.7–21.8) | 11.1 (10.7–14.7) | 12.7 (1.4–29.1) |
| Sustained ROSC [%] | 34.8 (32.6–42.5) | 43.3 (34.3–58.0) | 37.0 (35.4–62.7) | 35.3 (31.5–47.3) |
| Survival (CPC 1–2) [%] | 10.5 (6.5–17.4) | 14.3 (13.4–22.4) | 15.4 (2.9–28.4) | 14.7 (12.4–20.0) |
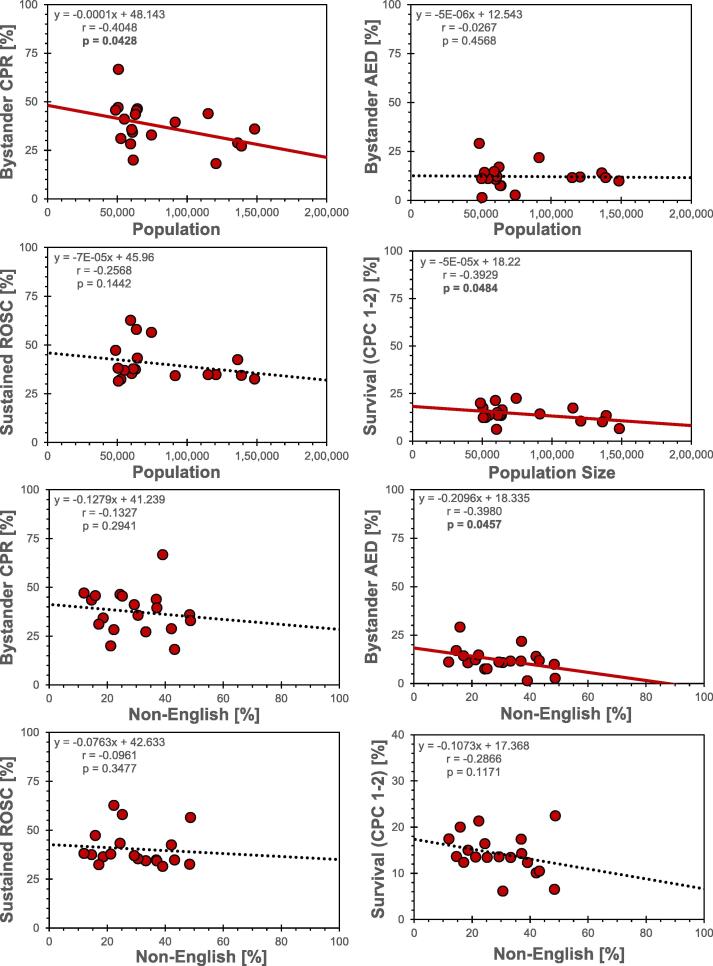
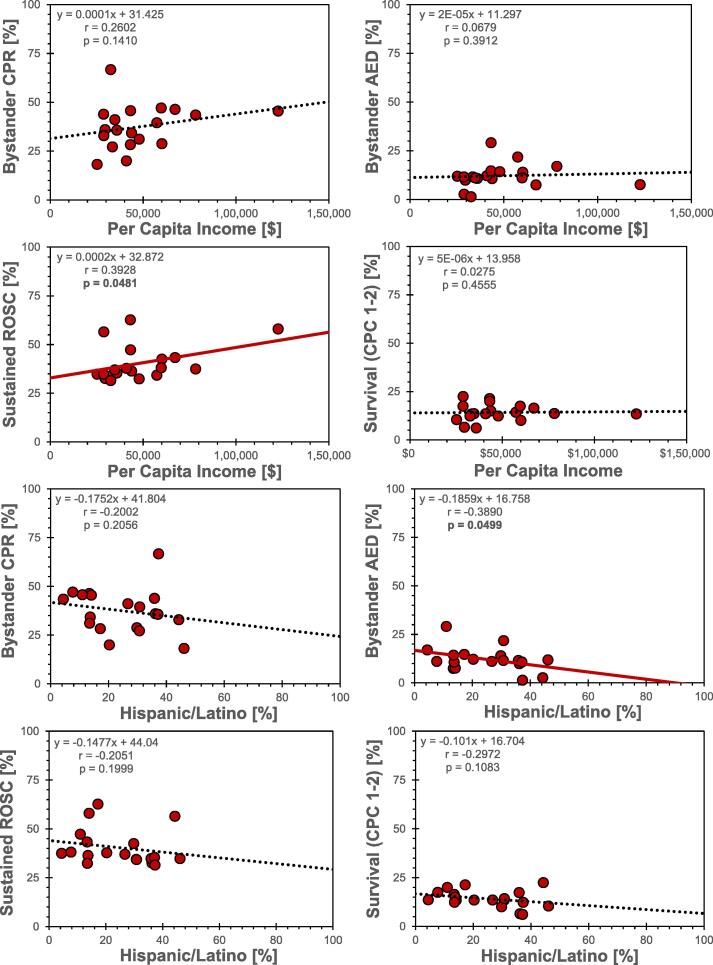
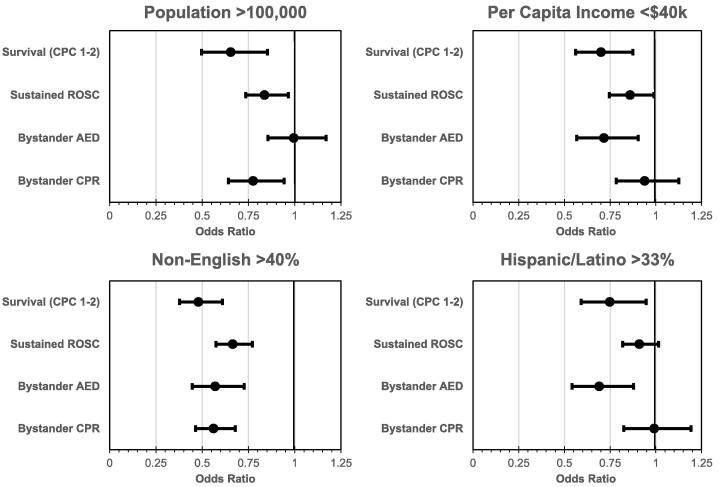
Population size was negatively correlated with bystander CPR (p = 0.0428) and survival to discharge (p = 0.0484; Fig. 1). Primary language other than English was negatively correlated with bystander AED use (p = 0.0457). Per capita income was positively correlated with sustained ROSC (p = 0.0481; Fig. 2). Hispanic ethnicity was negatively correlated with bystander AED use (p = 0.0499).Odds ratios were calculated for municipal characteristics identified in the Pearson matrix. Individuals living in cities with a population of > 100,000 were less likely to receive bystander CPR (OR 0.775, 95% CI 0.646–0.930), achieve sustained ROSC (OR 0.837, 95% CI 0.726–0.964), or survive with good neurological function (OR 0.654, 95% CI 0.521–0.82) (Fig. 3).
Fig. 1.
Relationships between independent municipal census statistics (population [n] and primary language other than English [%]) and dependent outcomes of bystander CPR percentage, bystander AED percentage, sustained ROSC, or survival to discharge. Red dots represent individual municipalities. Solid red lines indicate significant linear correlations by Pearson test (p < 0.05), black dashed lines indicate insignificant tests (p > 0.05). Linear fit equation, correlation coefficient (r) and p-values presented in upper left of graphs. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 2.
Relationships between independent municipal census statistics (per capita income [$] and Hispanic/Latino race/ethnicity [%]) and dependent outcomes of bystander CPR percentage, bystander AED percentage, sustained ROSC, or survival to discharge. Red dots represent individual municipalities. Solid red lines indicate significant linear correlations by Pearson test (p < 0.05), black dashed lines indicate insignificant tests (p > 0.05). Linear fit equation, correlation coefficient (r) and p-values presented in upper left of graphs. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 3.
Pooled odds ratios (ORs) between municipal risk factors and dependent outcomes. Data points represent ORs plus or minus 95% confidence intervals. Vertical line at 1 represents threshold of no association; values with an upper bound of < 1 represent statistically significant risk factors.
Living in a community in which > 40% of the population speaks a primary language other than English was associated with a risk for lower bystander CPR (OR 0.561, 95% CI 0.464–0.679), lower bystander AED use (OR 0.570, 95% CI 0.447–0.727), decreased sustained ROSC (OR 0.665, 95% CI 0.574–0.770), and decreased survival (OR 0.479, 95% CI 0.378–0.609).
Individuals living in a community with a per capita income of < $40,000 were less likely to receive bystander AED (OR 0.716, 95% CI 0.567–0.904), achieve sustained ROSC (OR 0.859, 95% CI 0.746–0.990), or survive (OR 0.770, 95% CI 0.561–0.875).
Finally, living in a community with > 1/3 Hispanic ethnicity was associated with decreased AED use (OR 0.690, 95% CI: 0.537–0.886) and decreased survival (OR 0.748, 95% CI: 0.591–0.947).
2022 correlation of bystander CPR with survival to discharge at the county Level
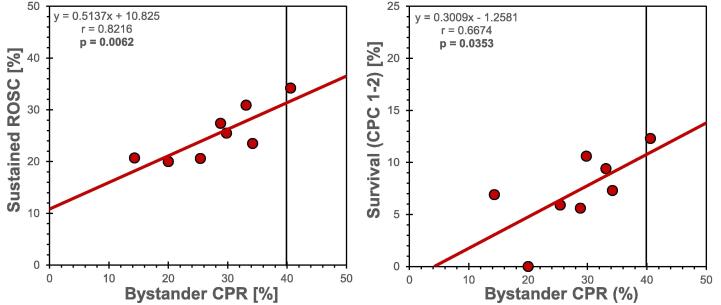
In 2022, bystander CPR participation within the eight counties in Connecticut ranged from 14.3% to 40.6%, averaging 22.8% statewide. A statistically significant linear correlation between bystander CPR and survival to discharge was identified by Pearson correlation test (p = 0.0353, r = 0.6674), revealing the efficacy of bystander CPR at the county level (Fig. 4). A positive correlation was also identified between bystander CPR and sustained ROSC (p = 0.0062, r = 0.8216). Using these linear regressions, a 10% increase in bystander CPR is projected to increase ROSC by approximately 5% and survival to discharge by 3%. Extrapolating from 2022 data, improving statewide bystander CPR from 22.8% to the national average of 40% (Δ = 17.2%) may save 128 lives per year. A linear regression between bystander AED use and survival did not reach statistical significance at the county level.
Fig. 4.
Bystander CPR versus sustained ROSC and survival by county in Connecticut. Red dots represent individual counties. Solid red lines indicate significant linear correlations by Pearson test (p < 0.05). Vertical black line at 40% bystander CPR represents national average. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Discussion
According to 2022 United States OHCA statistics provided by CARES, Connecticut trails the national average with respect to use of bystander CPR, public AED use, and patient survival with favorable neurological function. To better understand and possibly target deficiencies in statewide treatment and outcomes for OHCA, this study has compiled individual municipality data on bystander intervention and survival in the most populous cities and towns in Connecticut. While the study design does not analyze specific community initiatives, correlation of individual community socioeconomic demographics with treatment and survival patterns has led to several important conclusions when taken into context of the existing literature.
First, individual municipality analysis from 2013 to 2022 revealed significant community variation in the use of bystander CPR, AED attempted defibrillation, achievement of sustained ROSC and patient survival to discharge with favorable neurological outcomes. Second, examination of the socioeconomic demographics of municipalities where witnessed OHCA occurred revealed that four community-level characteristics were associated with lower likelihood of bystander administration of at least one component of the pre-hospital cardiac arrest chain of survival and ultimately lower likelihood of survival: 1) population size > 100,000; 2) primary spoken language other than English in > 40% of the community; 3) per capital income < $40,000; and 4) > 1/3 of the community identifying as Hispanic ethnicity. Finally, analysis of 2022 county-specific data demonstrates that bystander CPR use positively correlated with overall patient survival. In the setting of poor bystander CPR use and patient survival compared to other states, there is a clear need to increase the use of this important bystander intervention. Moreover, improvement in bystander intervention at the community level would be expected to improve overall statewide performance.
Our finding of worse witnessed OHCA outcomes coupled with lower community rates of bystander CPR and bystander AED use in lower income communities, in racial/ethnic minority communities, and in communities where English is not the primary spoken language are consistent with prior reports in Texas, North Carolina, and the United States.3, 4, 5 These findings build on results from a prior CARES study in Connecticut by our group that identified racial and ethnic disparities in pre-hospital treatment and outcomes for witnessed OHCA.7 The current study includes additional OHCA data for Connecticut in 2022, and pre-hospital treatment and outcome analyses reflects zip-code level incident location.
Despite proximity to acute-care hospitals and to bystanders who might administer CPR and utilize AEDs, the results of this study suggest that large urban communities in Connecticut are at increased risk for worse cardiac arrest outcomes. A recent report of disparities in bystander interventions for 325,477 adults with OHCA in the CARES registry between 2013 and 2019 found that bystander AED use was similar across the urban–rural spectrum, whereas bystander CPR use occurred most often in rural areas and least often in urban areas.14 This study suggested greater social cohesion, as opposed to a higher likelihood of CPR training, might explain higher likelihood of bystander CPR use in rural communities.14 An implication of this report is that community-centered interventions designed to enhance CPR utilization in urban settings should consider social cohesion among community members.
The results of this investigation are a call to action for initiatives to increase statewide bystander CPR administration and bystander AED use following witnessed OHCA. Prior reports in Denmark have documented the beneficial impact of global efforts to increase bystander intervention.15 A study examining OHCA outcomes in the CARES registry in North Carolina between 2010 and 2013 described state-wide improvement in survival with favorable neurological outcomes from 7.1% to 9.7% following interventions to increase bystander CPR and reduce time to AED use.16 In Sweden, mass CPR training over a 21-year period (1990 to 2011) was associated with an improvement in 30-day survival following witnessed OHCA of 4% to 10.5% when CPR was performed prior to EMS arrival.17 In a separate report from a national registry of sudden cardiac arrest and AED use in United States high schools with CPR-AED programs, there was an overall survival rate of 71% following witnessed OHCA during sports or exercise at high schools, associated with a 96% incidence of bystander CPR.18 In combination, these studies demonstrate the potential to improve survival following witnessed OHCA when there is prompt bystander recognition of cardiac arrest and participation in the chain of survival.
The results of this study also suggest that community-specific efforts may be necessary to improve statewide outcomes for witnessed OHCA. The largest Connecticut municipalities also have the largest percentages of Hispanic populace, inclusive of residents for multiple races and ethnicities for whom English is not the primary language. Bystander hesitancy, particularly in racial and ethnic minority communities, may be associated with the following concerns: 1) non-congruence between the language(s) spoken by bystanders and the language(s) spoken by EMS dispatchers; 2) lack of trust in reporting institutions (e.g., police and health care providers); 3) concerns regarding bystander protection from litigation; 4) concerns regarding the potential to cause harm to arrest victims while attempting resuscitation.3, 12, 19
Dispatcher-directed chest compression-only CPR may be an important approach for encouraging bystanders to feel confident administering CPR to help cardiac arrest victims.20, 21, 22 Future initiatives to increase use of effective dispatcher involvement should consider potential language barriers, particularly in urban and minority communities. Prior studies have highlighted delays in recognition of symptoms by dispatchers and delays in time to first compression with Hispanic or limited English-speaking callers.23, 24 These findings point to the need for increased availability of multi-lingual dispatchers. Evidence also supports the use of scripted questions, which may reduce the total number of questions needed to identify individuals experiencing potential cardiac arrest particularly among callers with limited English proficiency.25
Regarding potential concerns for bystander safety, Connecticut has a Good Samaritan Law (Connecticut General Statutes – 52-557b). Increasing public awareness of this statute may be an important component of public campaigns designed to increase bystander engagement by decreasing concerns for mistrust, potential litigation, and patient harm.
Our data also suggest that additional strategies may be required in low-income communities and minority communities in Connecticut. Financial concerns may be a structural barrier to acquiring CPR and AED training in Connecticut. These concerns may reflect apprehension regarding the time away from work required to obtain CPR/AED training and certification, and direct costs to enroll in CPR/AED training programs. Literacy and internet access may be a concern for self-administered CPR training programs. In addition, for individuals in low-income communities who are CPR/AED trained, there may be concerns related to fear of financial responsibilities for bystanders or arrest victims who interface with emergency medical services.12, 19
Improved public recognition of cardiac arrest may be required to improve OHCA survival. In a review of a 5-year multi-state initiative to improve witnessed OCHA treatment and outcomes (i.e., Heart Recue), it was suggested that the lay public may not understand the difference between a “heart attack” and sudden cardiac arrest.26, 27 In the aftermath of the Covid-19 pandemic, there may be hesitancy to administer CPR to arrest victims due to concerns of bystander safety and self-protection.28 Public service announcements at large public forums (e.g., sport and entertainment events) and in partnership with professional agencies such as the American Heart association and the American Red Cross may be effective approaches for educating the lay public about recognizing cardiac arrest and clarifying that hands-only CPR is an effective approach to resuscitation for victims of cardiac arrest.27
The authors recommend that community-level interventions to enhance CPR and AED training in Connecticut should be culturally sensitive and not cost prohibitive. In addition to intentional efforts to bridge language barriers, there should be efforts to provide low or no-cost CPR/AED training programs and to promote trust between residential communities and institutions that support the emergency medical response systems. To holistically address the needs of local communities, these efforts may require focus groups with community members and community leaders that drive public policy initiatives regarding resource allocation, public policy development, and communication strategies to expand CPR/AED training and AED availability.
Limitations
This study has several limitations. First, as a retrospective observational study, there may have been unregistered confounders and selection bias. We did not have information regarding the level of CPR training of bystanders or the prevalence of CPR training in Connecticut municipalities. This information may help interpret community level disparities in treatment and outcomes.
Second, we acknowledge that this study did not examine EMS or hospital treatment of patients with witnessed OHCA. These factors are part of the chain of survival, and they may have had an impact on survival with good neurological recovery.
Third, we used 2022 United States census Bureau statistics, which corresponds to the last year of data inclusion in our study, and our analyses reflected municipality-level representation of self-identified Black/ African American, White, and non-White Hispanic populations. It is possible that during the period of the investigation there were changes in the socioeconomic demographics of Connecticut municipalities. Our analyses did not account for American Indian, Alaska Native populations, Asian populations, or Native Hawaiian and Pacific Island populations which reflect approximately 0.7%, 5.2%, and 0.1% of the Connecticut population, respectively.
Fourth, our outcome analyses focused on hospital survival with good neurological recovery. It is possible that survival rates would have been different if all patients who survived to hospital discharge were included. Our focus on survival with good neurological outcomes may provide greater insight regarding the effectiveness of bystander resuscitation.
Finally, this report included zip-code level data from 19 of the 20 largest municipalities in Connecticut, excluding one city that did not participate in CARES. We acknowledge that our findings may not be generalizable to all geographic regions in Connecticut.
Conclusions
Witnessed out-of-hospital cardiac arrest pre-treatment and outcomes vary significantly by municipality in the state of Connecticut. Specifically, communities with high non-English speaking populations suffer from a dramatically reduced OR for survival (0.479). Apart from global statewide efforts to increase bystander intervention, individual community approaches to increase bystander CPR and AED use must consider municipal socioeconomic demographics including population size, primary language use, per capita income, and minority population percentage.
CRediT authorship contribution statement
Daniel W. Youngstrom: Writing – review & editing, Writing – original draft, Visualization, Formal analysis, Conceptualization. Trevor S. Sutton: Writing – review & editing, Writing – original draft, Methodology, Formal analysis, Conceptualization. Fleur S. Kabala: Writing – review & editing, Writing – original draft. Isabella C. Rosenzweig: Writing – review & editing, Writing – original draft. Charles W. Johndro: Writing – review & editing, Data curation, Conceptualization. Rabab Al-Araji: Writing – review & editing, Data curation. Carolyn Burke-Martindale: Writing – review & editing, Conceptualization. Jeff F. Mather: Writing – review & editing, Conceptualization. Raymond G. McKay: Writing – review & editing, Writing – original draft, Project administration, Methodology, Formal analysis, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to acknowledge the EMS agencies and hospital systems that participated in a state-wide data sharing collaboration from the CARES registry in Connecticut. The authors also acknowledge the support of CARES, the American Heart Association, and the American Red Cross in supporting the creation of this data sharing collaboration.
Contributor Information
Daniel W. Youngstrom, Email: Daniel.Youngstrom@hhchealth.org.
Trevor S. Sutton, Email: TSutton@uchc.edu.
Fleur S. Kabala, Email: Kabala@uchc.edu.
Isabella C. Rosenzweig, Email: Isabella.Rosenzweig@quinnipiac.edu.
Charles W. Johndro, Email: Charles.Johndro@hhchealth.org.
Rabab Al-Araji, Email: RababCARES@emory.edu.
Carolyn Burke-Martindale, Email: Carolyn.Martindale@hhchealth.org.
Jeff F. Mather, Email: Jeff.Mather@hhchealth.org.
Raymond G. McKay, Email: Raymond.McKay@hhchealth.org.
References
- 1.Martin S.S., Aday A.W., Almarzooq Z.I., et al. 2024 heart disease and stroke statistics: a report of US and global data from the American heart association. Circulation. 2024;149:e347–e913. doi: 10.1161/CIR.0000000000001209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bottiger B.W., Becker L.B., Kern K.B., et al. BIG FIVE strategies for survival following out-of-hospital cardiac arrest. Eur J Anaesthesiol. 2020;37:955–958. doi: 10.1097/EJA.0000000000001247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garcia R.A., Spertus J.A., Girotra S., et al. Racial and ethnic differences in bystander CPR for witnessed cardiac arrest. N Engl J Med. 2022;387:1569–1578. doi: 10.1056/NEJMoa2200798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huebinger R., Vithalani V., Osborn L., et al. Community disparities in out of hospital cardiac arrest care and outcomes in Texas. Resuscitation. 2021;163:101–107. doi: 10.1016/j.resuscitation.2021.03.021. [DOI] [PubMed] [Google Scholar]
- 5.Moeller S., Hansen C.M., Kragholm K., et al. Race differences in interventions and survival after out-of-hospital cardiac arrest in North Carolina, 2010 to 2014. J Am Heart Assoc. 2021;10 doi: 10.1161/JAHA.120.019082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tsao C.W., Aday A.W., Almarzooq Z.I., et al. Heart disease and stroke statistics-2022 update: a report from the American heart association. Circulation. 2022;145:e153–e639. doi: 10.1161/CIR.0000000000001052. [DOI] [PubMed] [Google Scholar]
- 7.Sutton T.S., Bailey D.L., Rizvi A., et al. Racial and ethnic disparities in the treatment and outcomes for witnessed out-of-hospital cardiac arrest in Connecticut. Resuscitation. 2023;188 doi: 10.1016/j.resuscitation.2023.109850. [DOI] [PubMed] [Google Scholar]
- 8.Moller S., Wissenberg M., Starkopf L., et al. Socioeconomic disparities in prehospital factors and survival after out-of-hospital cardiac arrest. Heart. 2021;107:627–634. doi: 10.1136/heartjnl-2020-317761. [DOI] [PubMed] [Google Scholar]
- 9.Chan P.S., McNally B., Vellano K., Tang Y., Spertus J.A. Association of neighborhood race and income with survival after out-of-hospital cardiac arrest. J Am Heart Assoc. 2020;9 doi: 10.1161/JAHA.119.014178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Owen D.D., McGovern S.K., Murray A., et al. Association of race and socioeconomic status with automatic external defibrillator training prevalence in the United States. Resuscitation. 2018;127:100–104. doi: 10.1016/j.resuscitation.2018.03.037. [DOI] [PubMed] [Google Scholar]
- 11.Blewer A.L., Ibrahim S.A., Leary M., et al. Cardiopulmonary resuscitation training disparities in the United States. J Am Heart Assoc. 2017;6 doi: 10.1161/JAHA.117.006124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sasson C., Haukoos J.S., Ben-Youssef L., et al. Barriers to calling 911 and learning and performing cardiopulmonary resuscitation for residents of primarily Latino, high-risk neighborhoods in Denver, Colorado. Ann Emerg Med. 2015;65 doi: 10.1016/j.annemergmed.2014.10.028. 545-52 e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Perkins G.D., Jacobs I.G., Nadkarni V.M., et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein resuscitation registry templates for out-of-hospital cardiac arrest: a statement for healthcare professionals from a task force of the International liaison Committee on resuscitation (American heart association, European resuscitation Council, Australian and New Zealand Council on resuscitation, heart and stroke Foundation of Canada, InterAmerican heart Foundation, resuscitation Council of southern Africa, resuscitation Council of Asia); and the American heart association emergency cardiovascular care Committee and the Council on cardiopulmonary, critical care, perioperative and resuscitation. Circulation. 2015;132:1286–1300. doi: 10.1161/CIR.0000000000000144. [DOI] [PubMed] [Google Scholar]
- 14.Grubic N., Peng Y.P., Walker M., Brooks S.C., Group C.S. Bystander-initiated cardiopulmonary resuscitation and automated external defibrillator use after out-of-hospital cardiac arrest: Uncovering disparities in care and survival across the urban-rural spectrum. Resuscitation. 2022;175:150–158. doi: 10.1016/j.resuscitation.2022.04.014. [DOI] [PubMed] [Google Scholar]
- 15.Wissenberg M., Lippert F.K., Folke F., et al. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. JAMA. 2013;310:1377–1384. doi: 10.1001/jama.2013.278483. [DOI] [PubMed] [Google Scholar]
- 16.Hansen C.M., Kragholm K., Granger C.B., et al. The role of bystanders, first responders, and emergency medical service providers in timely defibrillation and related outcomes after out-of-hospital cardiac arrest: Results from a statewide registry. Resuscitation. 2015;96:303–309. doi: 10.1016/j.resuscitation.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 17.Hasselqvist-Ax I., Riva G., Herlitz J., et al. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med. 2015;372:2307–2315. doi: 10.1056/NEJMoa1405796. [DOI] [PubMed] [Google Scholar]
- 18.Drezner J.A., Toresdahl B.G., Rao A.L., Huszti E., Harmon K.G. Outcomes from sudden cardiac arrest in US high schools: a 2-year prospective study from the National Registry for AED Use in Sports. Br J Sports Med. 2013;47:1179–1183. doi: 10.1136/bjsports-2013-092786. [DOI] [PubMed] [Google Scholar]
- 19.Blewer A.L., Bigham B.L., Kaplan S., Del Rios M., Leary M. Gender, socioeconomic status, race, and ethnic disparities in bystander cardiopulmonary resuscitation and education-a scoping review. Healthcare (Basel) 2024;12:456. doi: 10.3390/healthcare12040456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shimamoto T., Iwami T., Kitamura T., et al. Dispatcher instruction of chest compression-only CPR increases actual provision of bystander CPR. Resuscitation. 2015;96:9–15. doi: 10.1016/j.resuscitation.2015.07.009. [DOI] [PubMed] [Google Scholar]
- 21.Tanaka Y., Taniguchi J., Wato Y., Yoshida Y., Inaba H. The continuous quality improvement project for telephone-assisted instruction of cardiopulmonary resuscitation increased the incidence of bystander CPR and improved the outcomes of out-of-hospital cardiac arrests. Resuscitation. 2012;83:1235–1241. doi: 10.1016/j.resuscitation.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 22.Fujie K., Nakata Y., Yasuda S., Mizutani T., Hashimoto K. Do dispatcher instructions facilitate bystander-initiated cardiopulmonary resuscitation and improve outcomes in patients with out-of-hospital cardiac arrest? A comparison of family and non-family bystanders. Resuscitation. 2014;85:315–319. doi: 10.1016/j.resuscitation.2013.11.013. [DOI] [PubMed] [Google Scholar]
- 23.Bradley S.M., Fahrenbruch C.E., Meischke H., Allen J., Bloomingdale M., Rea T.D. Bystander CPR in out-of-hospital cardiac arrest: the role of limited English proficiency. Resuscitation. 2011;82:680–684. doi: 10.1016/j.resuscitation.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 24.Meischke H., Ike B., Painter I., et al. Delivering 9-1-1 CPR instructions to limited English proficient callers: a simulation experiment. J Immigr Minor Health. 2015;17:1049–1054. doi: 10.1007/s10903-014-0017-8. [DOI] [PubMed] [Google Scholar]
- 25.Sanko S., Feng S., Lane C., Eckstein M. Comparison of emergency medical dispatch systems for performance of telecommunicator-assisted cardiopulmonary resuscitation among 9-1-1 callers with limited English proficiency. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.6827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van Diepen S., Girotra S., Abella B.S., et al. Multistate 5-year initiative to improve care for out-of-hospital cardiac arrest: primary results from the heartrescue project. J Am Heart Assoc. 2017;6 doi: 10.1161/JAHA.117.005716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Berger S. Survival from out-of-hospital cardiac arrest: are we beginning to see progress? J Am Heart Assoc. 2017;6 doi: 10.1161/JAHA.117.007469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lim S.L., Toh C., Fook-Chong S., et al. Impact of COVID-19 on barriers to dispatcher-assisted cardiopulmonary resuscitation in adult out-of-hospital cardiac arrests in Singapore. Resuscitation. 2022;181:40–47. doi: 10.1016/j.resuscitation.2022.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]