Abstract
Torsion and rupture are life-threatening emergencies in rudimentary horn pregnancy, an extremely rare type of ectopic pregnancy. This case report aims to share the diagnosis and treatment of a patient, with torsion and ruptured horn pregnancy in a setting, with limited resources. It highlights the challenges faced and the strategies employed to ensure appropriate care. A 38-year-old woman, gravida 2, para 1, presented to the Obstetric and Gynaecology (OBGYN Department of Hiwot Fana University Hospital with a diagnosis of uterine rupture after she presented with a complaint of pushing down pain of 1 h, decreased fetal movement of 1-day duration, and with sudden and severe lower abdominal pain and distension. Conservative management was chosen, but deteriorating symptoms necessitated an emergency laparotomy, confirming a ruptured rudimentary horn pregnancy and surgically excising the horn. Ruptured rudimentary horn pregnancy with torsion is an extremely uncommon and perilous obstetric emergency that necessitates swift diagnosis and surgical intervention. For advanced primitive horn pregnancy, laparotomy combined with horn removal continues to be the gold standard of therapy. Healthcare providers can improve patient outcomes and alleviate the burden of life-threatening conditions by promoting multidisciplinary collaboration and embracing innovative, technologically advanced techniques.
Keywords: Rudimentary horn pregnancy, ectopic pregnancy, torsion, rupture, low-resource setting
Introduction
A rudimentary horn pregnancy occurs when a fertilized egg implants and develops in an undeveloped area of the uterus. 1 This underdeveloped part of the uterus is called the rudimentary horn of a unicornuate uterus. An incidence of 1 in 75,000–150,000 pregnancies has been observed for rudimentary horn pregnancy, which is an extremely rare kind of ectopic pregnancy. 2 Torsion and rupture of a horn pregnancy are extremely uncommon and can be severe and life-threatening emergencies. This case report aims to share the diagnosis and treatment of a patient, with torsion and ruptured horn pregnancy in a setting, with limited resources. It highlights the challenges faced and the strategies employed to ensure appropriate care.
Case presentation
A 38-year-old woman, gravida 2, para 1, presented to the OBGYN Department of Hiwot Fana University Hospital with sudden and severe lower abdominal pain and distension. Her last menstrual period was on December 24, 2022 making her GA = 32 weeks + 1 day. She presented to our hospital with a referral paper from Gursum Hospital (a nearby hospital) with a diagnosis of uterine rupture after she presented with a complaint of pushing down pain of 1 h and decreased fetal movement of 1-day duration. The patient had no history of pelvic surgeries but reported irregular menstrual cycles. She has a history of vaginal bleeding one episode (at the referral site). On general appearance, she was acutely sick-looking, and on physical examination, the patient was in significant distress, with marked tenderness and guarding in the lower abdomen. Her vital sign results are as follows: pulse rate = 138 beats/min, respiration rate = 26/min, and oxygen saturation rate in off oxygen = 89% which revealed tachycardia and hypotension, but she was not in a shocking state. So, these results suggest she was in a critical state.
After observing the symptoms and suspecting uterine rupture, a prompt ultrasound was conducted. The results of the ultrasound showed the presence of fluid in the peritoneal cavity, 32 weeks (by Femur Length [FL]) sized Right (Rt)cornual pregnancy, Fetal Heart Beat (FHB −VE was seen, uterus was observed and empty. Unfortunately, due to resources, we were unable to use imaging techniques. Nevertheless, based on the ultrasound findings, it strongly indicated right cornual pregnancy to R/O uterine rupture, which required immediate exploration.
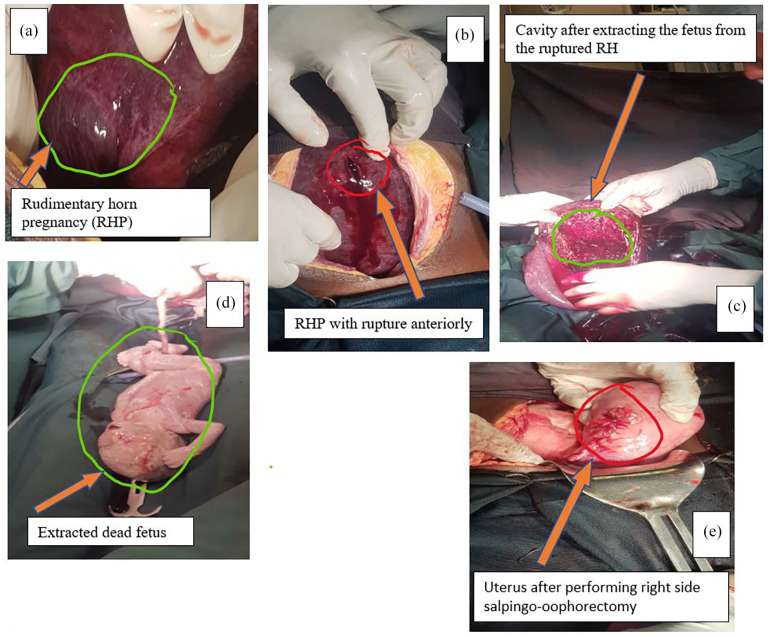
The patient was immediately prepared for emergency laparotomy. Intraoperatively, a right side ruptured rudimentary communicating horn pregnancy was confirmed, with evidence of torsion of the rudimentary horn with 1080° rotated clockwise at the base as well as there were three sites of rupture that is anterior, at the fundus, posterior and the fetus was inside rudimentary horn (Figure 1(a) and (b)). Due to the complexity of the case and limited resources, the surgical team faced challenges during the procedure. A skilled and experienced surgical team performed the excision of a rudimentary horn (Figure 1(c)) and there was a delivery of 1.8 kg freshly dead female (Figure 1(d)), then right-side salpingo-oophorectomy was done (Figure 1(e)), and hemostasis was secured to control the bleeding. Intraoperative blood transfusion was required due to significant blood loss and transfused with 2 units of blood.
Figure 1.
(a) Right rudimentary horn pregnancy with torsion. (b) Rudimentary horn pregnancy with rupture anteriorly. (c) The cavity after extracting the fetus from the ruptured rudimentary horn. (d) 1.8 kg extracted dead fetus. (e) Uterus after performing right-side salpingo-oophorectomy.
Patient follow-up
Postoperatively, the patient was closely monitored in the intensive care unit. She received intravenous antibiotics and analgesics to prevent infection and manage pain. The patient was provided with comprehensive counseling on family planning and contraceptive options. The patient’s recovery, after surgery, showed improvement. She was released from the hospital in stable condition. She was advised to attend regular follow-up appointments to monitor her recovery and reproductive health.
Discussion
Third-trimester rupture of rudimentary horn pregnancy with torsion is an extremely rare and potentially fatal condition, particularly in low-resource settings. 1 Prompt diagnosis and surgical intervention are critical for avoiding serious complications. 3 In managing such complex obstetric emergencies in resource-constrained environments, clinical acumen, timely recognition, and multidisciplinary collaboration are critical. 4
Effective management of ruptured rudimentary horn pregnancies relies heavily on collaboration among various medical specialties. Timely diagnosis and appropriate surgical intervention can be ensured through the early involvement of obstetricians, radiologists, and experienced laparoscopic surgeons. 4
Despite significant advancements in diagnosing and treating ruptured rudimentary horn pregnancies, this condition continues to pose a life-threatening risk, demanding immediate intervention to prevent adverse maternal outcomes. 5 An illustrative case reported by Houmaid and Hilali involving rupture at 16 weeks of gestation emphasizes the severity of this condition and highlights the crucial need for enhanced awareness and education among healthcare providers. 6
Ruptured rudimentary horn pregnancy with torsion is an extremely uncommon and perilous obstetric emergency that necessitates swift diagnosis and surgical intervention. 1 The scarcity of reported cases in the medical literature reflects the difficulties in recognizing this condition and the lack of awareness among healthcare professionals. In resource-limited settings, delays in seeking antenatal care (ANC) and limited access to advanced imaging modalities can exacerbate the challenges in diagnosing this condition. 7
Considering the rarity of this condition, it is imperative to enhance awareness among healthcare practitioners, particularly those working in low-resource settings, to facilitate early identification and appropriate management. 1 Successful outcomes heavily rely on multidisciplinary collaboration between obstetricians, radiologists, and experienced laparoscopic surgeons.
Laparoscopic approaches have emerged as effective and less invasive methods for managing ruptured rudimentary horn pregnancies. 4 These techniques have been shown to minimize postoperative complications and accelerate recovery.8,9 However, the widespread implementation of laparoscopy in resource-constrained environments might be limited due to factors such as the availability of skilled surgeons and advanced equipment.
Conclusions
In conclusion, the diagnosis and management of ruptured rudimentary horn pregnancy with torsion pose substantial challenges in both well-equipped healthcare settings and resource-constrained environments.
First-trimester ultrasonography is the only sensitive, noninvasive diagnostic method known for rudimentary horn pregnancy. For advanced primitive horn pregnancy, laparotomy combined with horn removal continues to be the gold standard of therapy. In addition, by fostering multidisciplinary collaboration and embracing innovative, technologically advanced techniques, healthcare providers can enhance patient outcomes and alleviate the burden of this potentially life-threatening condition.
Future research endeavors should prioritize increasing awareness and knowledge of this rare condition among healthcare providers, particularly in regions where access to advanced imaging is restricted. In addition, conducting studies comparing various surgical approaches and their respective outcomes could contribute to refining the management of ruptured rudimentary horn pregnancies.
Timeline
On July 1, 2023, the patient was admitted, and at that time, management and investigations were started. On the day of her admittance, she had an emergency laparotomy, and she received postoperative care for 10 days. It took 3 months to prepare this case report, during which the patient’s agreement was obtained and the case was presented to the ethical committee and the Obstetric Department at Hiwot Fana Specialized Hospital.
Acknowledgments
We are grateful to the Obstetrics Department of Hiwot Fana Specialized Hospital for their assistance. We also thank all teams for their assistance in preparing this scientifically suitable manuscript for publication.
Footnotes
Author contributions: T.S., E.J., K.A., and M.T. are involved in diagnosis and treatment including operation, and A.A. (corresponding author) produced the case report. Each author agreed to take responsibility for all parts of the work, including data analysis, article drafting and revision, and final approval of the version to be published. They also approved or consented to the journal submission.
Data availability statement: Any data related to this review can be provided by the corresponding author at any time on reasonable request.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The health cost was waived by the hospital administration as required by the health policy of the government of Ethiopia. The cost of preparing this manuscript was covered by the authors.
Ethics approval: Our institution does not require ethical approval for reporting individual cases or case series. This case report could be published without the need for institutional approval. The patient has given permission for the case report to be released.
Informed consent: Informed written consent has been obtained from the patient for all case details, images and their anonymized information to be published in this article.
ORCID iD: Astawus Alemayehu  https://orcid.org/0000-0003-1384-7123
https://orcid.org/0000-0003-1384-7123
References
- 1. Yassin A, Munaza S, Mohammed A. Tale of rudimentary horn pregnancy: case reports and literature review. J Matern Fetal Neonatal Med 2019; 32: 671–676. [DOI] [PubMed] [Google Scholar]
- 2. ISUOG. Rudimentary horn pregnancy, https://www.isuog.org/clinical-resources/patient-information-series/patient-information-pregnancy-conditions/early-pregnancy/rudimentary-horn-pregnancy.html (2023, accessed 10 September 2023).
- 3. Tesemma MG. Pregnancy in noncommunicating rudimentary horn of unicornuate uterus: a case report and review of the literature. Case Rep Obstet Gynecol 2019; 2019: 1489751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zhang DD, Gao Y, Lang JH, et al. Diagnosis and treatment of rudimentary horn pregnancy: analysis of eleven cases. Chin Med J (Engl) 2018; 131: 3012–3014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dahab AA, Aburass R, Shawkat W, et al. Full-term extrauterine abdominal pregnancy: a case report. J Med Case Rep 2011; 5: 531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Houmaid H, Hilali A. Rupture of rudimentary horn pregnancy at 16 weeks of gestation. Case Rep Obstet Gynecol 2021; 2021: 8829053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mlandu C, Matsena-Zingoni Z, Musenge E. Trends and determinants of late antenatal care initiation in three East African countries, 2007–2016: A population based cross-sectional analysis. PLOS Glob Public Health 2022; 2: e0000534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sharma D, Usha MG, Gaikwad R, et al. Laparoscopic resection of unruptured rudimentary horn pregnancy. J Gynecol Endosc Surg 2011; 2: 101–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ogbole GI, Adeyomoye AO, Badu-Peprah A, et al. Survey of magnetic resonance imaging availability in West Africa. Pan Afr Med J 2018; 30: 240. [DOI] [PMC free article] [PubMed] [Google Scholar]