Abstract
Background: Across the world, health data generation is growing exponentially. The continuous rise of new and diversified technology to obtain and handle health data places health information management and governance under pressure. Lack of data linkage and interoperability between systems undermines best efforts to optimise integrated health information technology solutions. Objective: This research aimed to provide a bibliometric overview of the role of interoperability and linkage in health data management and governance. Method: Data were acquired by entering selected search queries into Google Scholar, PubMed, and Web of Science databases and bibliometric data obtained were then imported to Endnote and checked for duplicates. The refined data were exported to Excel, where several levels of filtration were applied to obtain the final sample. These sample data were analysed using Microsoft Excel (Microsoft Corporation, Washington, USA), WORDSTAT (Provalis Research, Montreal, Canada) and VOSviewer software (Leiden University, Leiden, Netherlands). Results: The literature sample was retrieved from 3799 unique results and consisted of 63 articles, present in 45 different publications, both evaluated by two specific in-house global impact rankings. Through VOSviewer, three main clusters were identified: (i) e-health information stakeholder needs; (ii) e-health information quality assessment; and (iii) e-health information technological governance trends. A residual correlation between interoperability and linkage studies in the sample was also found. Conclusion: Assessing stakeholders’ needs is crucial for establishing an efficient and effective health information system. Further and diversified research is needed to assess the integrated placement of interoperability and linkage in health information management and governance. Implications: This research has provided valuable managerial and theoretical contributions to optimise system interoperability and data linkage within health information research and information technology solutions.
Keywords: health information management, health information interoperability, health information systems, medical informatics, health information exchange, information storage and retrieval, bibliometrics
Keywords: health information governance, data linkage, healthcare stakeholders, system interoperability, e-health, blockchain in healthcare
Introduction
The continuous generation of enormous amounts of health data poses several challenges to its management and governance. Currently, healthcare stakeholders have access to raw health data that must be processed to enable value creation (Arul et al., 2024; Genevieve et al., 2019). Healthcare systems adopt informatics systems that allow the analysis of health data retrieved and provided by different stakeholders (Genevieve et al., 2019). However, there is a lack of linkage and interoperability between these systems (Bates, 2005; Edwards et al., 2010; Genevieve et al., 2019; van Olmen et al., 2020).
As different and complex health informatics systems emerge, the need for integrating and linking data from various datasets also emerges. Data linkage can be defined as “a process of pairing records from two files and trying to select the pairs that belong to the same entity” (Bohensky et al., 2010; Winglee et al., 2005). The Organisation for Economic Co-operation and Development also defined data linkage as “a merging that brings together from two or more sources of data with the object of consolidating facts concerning an individual or an event that are not available in any separate record” (Harron, 2016). In the healthcare sector, data linkage has been applied, for example, to the integration of patient health records and death certificates (Christen, 2019). Other general health-related applications include epidemiological, managerial and service production studies (Holman et al., 2008). Data linkage’s purpose is to enable the integration of different datasets considering the identification and interconnection of records within an organisation with single datasets or multiple ones (Christen, 2019; Green et al., 2015). The multitude of settings and operations within healthcare information systems can threaten the obtainment of optimised linkage between diversified data libraries. For this reason, stakeholders need to continuously address the problem of interconnectivity between healthcare information systems to find facilitators and solutions (Hopf et al., 2014, 2016; March et al., 2020).
With the need for data linkage also comes the need for interoperability between systems. Interoperability is currently one of the top targets of researchers in the field of information technology (Torab-Miandoab et al., 2023). According to the IEEE Standard Computer Dictionary, interoperability is “the ability of two or more systems or components to exchange information and to use the information that has been exchanged” (Lehne et al., 2019). As different hospitals and physicians are increasing their adoption of digital health data records, the lack of interoperability between healthcare informatics systems may pose difficulties regarding communication processes (Lehne et al., 2019; Reisman, 2017). Therefore, healthcare stakeholders must promote research in this field, trying to understand and identify the core variables within different social, political and clinical challenges and contexts, which can be crucial for establishing an interoperable system. Moreover, there is an awareness of the need for a universal interoperability strategy between all healthcare stakeholders (Tiago et al., 2016). Other aspects, such as technology architecture, system governance and core dataset definition, may be crucial for implementing successfully an interoperable system (Azarm et al., 2017). Interoperability standards are also key in any functioning interoperable system (Gowda et al., 2022). Some benefits of interoperable systems include facilitated access to patient health data, more understanding of medical terms, medical bias minimisation, improved health cost management and integration of diversified types of health data (Iroju et al., 2013). However, barriers to interoperability implementation are still present and include the complexity of the healthcare environment, the lack of standardisation, the existence of legacy systems (e.g. an outdated electronic health record system that does not comply with current standards) and semantic compatibilisation issues (e.g. two systems that cannot recognise and interpret each other’s information) and resistance to change to digitalisation processes (Iroju et al., 2013).
Current study
System interoperability and data linkage issues span different types of healthcare environments, leading to difficulties in accessing patient health data generated in different settings. Research made about these concerns needs to be verified to evaluate the state-of-the-art of relevant potential needs and trends. The aim of the current research was to provide an overview of the current and future role of data linkage and system interoperability within the domain of health information management and governance by conducting a bibliometric analysis of relevant published literature.
Method
Search strategy
This bibliometric analysis was based on a search of research articles across three platforms: Google Scholar, PubMed and Web of Science, considered to be the most relevant databases for this analysis. Search terms used for each platform were: “health data management,” “health information governance,” “health information management,” “healthcare data governance,” “healthcare data management,” “healthcare information governance,” “healthcare information management,” associated with the terms “linkage” and “interoperability” (Supplemental material Table S1, online supplement). No year limitations were applied as the objective was to maximise the analysis of the evolution of publishing research articles over time.
Data acquisition
Data were collected from the three search platforms between December 2021 and February 2022. Search results from Google Scholar were first added to the “My Library” feature and then retrieved to an EndNote file using the export function. From the Web of Science search platform (Web of Science Core Collection), data were retrieved directly to an EndNote file. For PubMed, data were obtained using its citation manager, which created a compatible EndNote file. All data were extracted during February 2022. For the citation analysis, the number of citations per article was retrieved manually after completion of the search, and on the same day from Google Scholar.
Data selection process and analysis
All reference files obtained through each search platform were imported to EndNote, followed by a reference update using EndNote’s “Find Reference Updates” feature. With up-to-date references, another automatic EndNote function was used, namely “Find Duplicates,” to eliminate duplicated references. The refined data obtained in EndNote were transferred into Microsoft Excel (Microsoft Corporation, Washington, USA) for further analyses (Figure 1). Using this software, an article’s abstract analysis was performed. The first stage was to verify which results had an abstract and to eliminate the articles without abstracts. At this stage, only articles published by the end of 2021 were considered, as 2022 was an incomplete year and could have provided subsequent erroneous citation calculations and results. In the second stage, selected abstracts were analysed for the inclusion of the term “interoperability” or “linkage.” The results (articles with abstracts that included one or both of these terms) were then analysed according to their average yearly citations. The baseline value of the previous metric was calculated by the average number of citations and article years of the 212 selected articles, to narrow and obtain even more meaningful and impacting results. Research articles with a citation average of less than 4.94 per year were excluded, as this value represented the minimum specific threshold within the scope of the analysis of articles considered impactful (Emmer et al., 2022). Finally, the selected 72 references were screened to verify they met the criteria for the scope of analysis (through screening of articles’ PDF files). Following the earlier selection process, data were evaluated using mainly Microsoft Excel, WORDSTAT v. 9.0.11 and VOSviewer v. 1.6.18 software as schematised in Figure 1. VOSviewer tools (Leiden University, Leiden, Netherlands) were deployed to verify potential relationships between research terms and the strength of these relationships within the abstracts and article titles, and to assess their chronological order.
Figure 1.
Data selection process and analysis.
Results
Overview of the data acquisition and selection process
Search results were refined through several processes, which led to the final sample. One of the first meaningful levels of data treatment was the abstract inclusion criterion, which revealed that from the 3977 unique references obtained in EndNote, only 685 (17.22%) had an abstract included in the exported results. After identifying the abstracts that included the terms, “interoperability” and/or “linkage,” the number dropped to 212 references (30.95%; 5.33% from the 3977 unique references). When the last criterion was applied (average citations per year ⩾4.94), only 72 references (33.96%; 1.81% of the 3977 unique references) remained. As to type of publications identified during the sample selection process, most were journal articles (Supplemental material Table S2, online supplement). In terms of chronological evolution (Figure 2), there were few publications on this research topic before 2005. From 2005, the number of publications continued to rise, reaching its peak between 2018 and 2021. In 2019, the number of refined publications (those with an abstract; and those with an abstract that included the selected terms) increased significantly. However, from 2020, these two publication categories began to diverge, as the number of publications with abstracts that included the selected terms continued to drop until the end of 2021.
Figure 2.
Chronological evolution of publications by level of data selection.
Sample overview
According to our research methodology, three search platforms were chosen to provide results on our topic of analysis. Selected articles were searchable heterogeneously throughout each platform. Most articles were available on Google Scholar (63; 100%) and PubMed (58; 92%), while Web of Science results were scarce (14; 22%). As previously noted, 72 articles were selected for the preliminary sample. A detailed analysis of these research articles led to the exclusion of a further nine articles, which did not fit the scope of the present study. The remaining 63 selected articles are described and summarised in Supplemental material Table S3 (online supplement). Of these 63 articles, 51 (80.95%) contained the word “interoperability” in the abstract, followed by the word “linkage” with 11 (17.46%) results, and only 1 (1.59%) article had an abstract containing both “interoperability” and “linkage.” The average number of authors per article was 5, and the maximum and minimum number of authors per article ranged between 15 and 1, respectively. Most articles had between 2 and 5 authors (48 articles; 76.19%). According to Figure 3, 35 countries were associated with at least 1 article. The country with the highest representation was the United States, with 26 associated articles (41.27%), followed by the United Kingdom with 11 articles (17.46%) and Australia with 5 articles (7.94%). Iran and Switzerland were each represented in four articles, and Saudi Arabia in three articles. Six countries (Canada, China, Germany, India, South Korea and Spain) were each represented in 2 research articles, while 23 countries were each represented in only 1 article.
Figure 3.
Geographical distribution of articles according to their authors’ origin.
Article citation analysis
According to the data retrieved and exported to Table 1, the highest number of citations was achieved by Koppel and Lehmann (2015) and the lowest by Ammar et al. (2021). As for the average number of citations per year, Gordon and Catalini (2018) had the highest average and Ammar et al. (2021) the lowest. The average number of citations of all 63 articles was 101.38, while the mean value of the average number of citations per year was 17.19. A reference global impact ranking was also established, which resulted from the multiplication of the average number of citations by the average number of citations per year. The top five publications of this ranking were: (1st) Gordon and Catalini (2018); (2nd) Mandel et al. (2016); (3rd) Koppel and Lehmann (2015); (4th) Kaplan and Harris-Salamone (2009) and (5th) Detmer et al. (2008). The lowest five included the references Genevieve et al. (2019), Ammar et al. (2020), Samra et al. (2020), Arul et al. (2024) and Ammar et al. (2021).
Table 1.
Reference characterisation and global impact ranking.
| References | Publication type | No. of citations (a) | Average citations per year (b) | Global impact ranking (a) × (b) |
|---|---|---|---|---|
| Gordon and Catalini (2018) | Journal Article | 472 | 118 | 1 |
| Mandel et al. (2016) | Journal Article | 475 | 79.17 | 2 |
| Koppel and Lehmann (2015) | Journal Article | 513 | 38.69 | 3 |
| Kaplan and Harris-Salamone (2009) | Journal Article | 503 | 38.69 | 4 |
| Detmer et al. (2008) | Journal Article | 482 | 34.43 | 5 |
| Ford et al. (2009) | Journal Article | 393 | 30.23 | 6 |
| Ahmed et al. (2020) | Journal Article | 142 | 71 | 7 |
| Bahga and Madisetti (2013) | Journal Article | 217 | 24.11 | 8 |
| Bates (2005) | Journal Article | 291 | 17.11 | 9 |
| Hussien et al. (2019) | Journal Article | 103 | 34.33 | 10 |
| Dinh-Le et al. (2019) | Journal Article | 99 | 33 | 11 |
| Jones et al. (2014) | Journal Article | 161 | 20.23 | 12 |
| Huang et al. (2017) | Journal Article | 104 | 20.8 | 13 |
| Furukawa et al. (2013) | Journal Article | 136 | 15.11 | 14 |
| Sittig et al. (2018) | Journal Article | 79 | 19.75 | 15 |
| Hylock and Zeng (2019) | Journal Article | 68 | 22.67 | 16 |
| Johnson et al. (2008) | Journal Article | 117 | 12.64 | 17 |
| Lavin et al. (2015) | Journal Article | 94 | 13.43 | 18 |
| Kalkman et al. (2019) | Journal Article | 54 | 18 | 19 |
| Mohammadzadeh and Safdari (2014) | Journal Article | 88 | 11 | 20 |
| Rezaeibagha et al. (2015) | Journal Article | 82 | 11.71 | 21 |
| Dubovitskaya et al. (2020) | Journal Article | 43 | 21.5 | 22 |
| Witry et al. (2010) | Journal Article | 105 | 8.75 | 23 |
| Krittanawong et al. (2020) | Journal Article | 41 | 20.5 | 24 |
| Jones et al. (2019) | Journal Article | 50 | 16.67 | 25 |
| Lucyk et al. (2017) | Journal Article | 64 | 12.8 | 26 |
| Vazirani et al. (2020) | Journal Article | 39 | 19 | 27 |
| Alonso et al. (2019) | Journal Article | 45 | 15 | 28 |
| Salas-Vega et al. (2015) | Journal Article | 68 | 9.71 | 29 |
| Blasimme et al. (2018) | Journal Article | 50 | 12.5 | 30 |
| Lee et al. (2020) | Journal Article | 35 | 17.5 | 31 |
| Warner et al. (2016) | Journal Article | 59 | 9.83 | 32 |
| Kharrazi et al. (2017) | Journal Article | 53 | 10.6 | 33 |
| Downs et al. (2019) | Journal Article | 38 | 12.67 | 34 |
| Blazona and Koncar (2007) | Journal Article | 83 | 5.53 | 35 |
| Kasthurirathne et al. (2015) | Journal Article | 56 | 8 | 36 |
| Edwards et al. (2010) | Journal Article | 71 | 5.92 | 37 |
| Masud et al. (2012) | Journal Article | 63 | 6.3 | 38 |
| Vest (2012) | Journal Article | 60 | 6 | 39 |
| Avila et al. (2017) | Journal Article | 42 | 8.4 | 40 |
| Oderkirk et al. (2013) | Journal Article | 56 | 6.22 | 41 |
| Durneva et al. (2020) | Journal Article | 26 | 13 | 42 |
| Sethi and Laurie (2013) | Journal Article | 55 | 6.11 | 43 |
| Wollersheim et al. (2009) | Journal Article | 66 | 5.08 | 44 |
| Ahmadi and Aslani (2018) | Journal Article | 36 | 9 | 45 |
| Abdekhoda et al. (2016) | Journal Article | 42 | 7 | 46 |
| Sinaci et al. (2020) | Journal Article | 24 | 12 | 47 |
| Alkraiji et al. (2013) | Journal Article | 49 | 5.44 | 48 = 49 |
| Tapuria et al. (2013) | Journal Article | 49 | 5.44 | 49 = 48 |
| Joda et al. (2019) | Journal Article | 27 | 9 | 50 |
| Ismail and Materwala (2020) | Journal Article | 22 | 11 | 51 = 52 |
| Shanbehzadeh et al. (2020) | Journal Article | 22 | 11 | 52 = 51 |
| Boyd et al. (2015) | Journal Article | 36 | 5.14 | 53 |
| van Olmen et al. (2020) | Journal Article | 17 | 8.5 | 54 |
| de Quiros et al. (2018) | Journal Article | 23 | 5.75 | 55 = 56 |
| Park et al. (2018) | Journal Article | 23 | 5.75 | 56 = 55 |
| Gamal et al. (2021) | Journal Article | 11 | 11 | 57 |
| de Moura Costa et al. (2020) | Journal Article | 14 | 7 | 58 |
| Genevieve et al. (2019) | Journal Article | 16 | 5.33 | 59 |
| Ammar et al. (2020) | Conference Proceedings | 12 | 6 | 60 = 61 |
| Samra et al. (2020) | Journal Article | 12 | 6 | 61 = 60 |
| Arul et al. (2024) | Journal Article | 6 | 6 | 62 |
| Ammar et al. (2021) | Journal Article | 5 | 5 | 63 |
Note: For references Alkraiji et al. (2013), Tapuria et al. (2013), Ismail and Materwala (2020), Shanbehzadeh et al. (2020), de Quiros et al. (2018), Park et al. (2018), Ammar et al. (2020), Samra et al. (2020): the result of (a) × (b) results in a tie which means they share the same ranking.
Publication analysis
According to Table 2, the 63 references selected for this study were represented across 45 different publications. Almost all of these publications were journals, with only two related to book series. The average number of references in these publications was 1.40. Regarding the citation analysis, the Journal of the American Medical Informatics Association (JAMIA) had the highest number of citations, as well as the highest average number of citations per year. BMC Medical Informatics and Decision-Making registered the highest average number of citations per article. JMIR Formative Research recorded the lowest score in the three previously reported metrics. A publication global impact ranking was also established, which resulted from the multiplication of four metrics: (1) average number of citations per year; (2) average number of citations per article; (3) 2021 CiteScore; (4) 2021 impact factor (Clarivate Analytics). The top five publications of this ranking were (1) Journal of the American Medical Informatics Association (JAMIA); (2) Computational and Structural Biotechnology Journal (CSBJ); (3) Nature Reviews Cardiology; (4) Health Affairs; (5) IEEE Journal of Biomedical and Health Informatics. The lowest five positions of publication global impact raking were (1) JMIR Formative Research; (2) Studies in Health Technology and Informatics; (3) Advances in Health Care Management; (4) Personal and Ubiquitous Computing; (5) Journal of Education and Health Promotion (JEHP).
Table 2.
Publication characteristics and global impact ranking.
| Publication name | ISSN | Publication type | No. of references | Average citations per year (a) | Average citations per article (b) | 2021 CiteScore (c) | Impact factor 2021 Journal Citation Reports (d) | Publication global impact ranking (a) × (b) × (c) a × (d) a |
|---|---|---|---|---|---|---|---|---|
| Journal of the American Medical Informatics Association (JAMIA) | 1527-974X | Journal | 6 | 189.62 | 287 | 9.6 | 7.942 | 1 |
| Computational and Structural Biotechnology Journal (CSBJ) | 2001-0370 | Journal | 1 | 118.00 | 472 | 6 | 6.155 | 2 |
| Nature Reviews Cardiology | 1759-5010 | Journal | 1 | 20.50 | 41 | 31.9 | 49.421 | 3 |
| Health Affairs | 2694-233X | Journal | 3 | 44.72 | 159 | 9.6 | 9.048 | 4 |
| IEEE Journal of Biomedical and Health Informatics | 2168-2208 | Journal | 1 | 24.11 | 217 | 10.9 | 7.021 | 5 |
| Database (Oxford) | 1758-0463 | Journal | 1 | 71.00 | 142 | 6.6 | 4.462 | 6 |
| BMC Medical Informatics and Decision Making | 1472-6947 | Journal | 1 | 34.43 | 482 | 4.6 | 3.298 | 7 |
| Journal of Medical Systems | 1573-689X | Journal | 4 | 62.77 | 63 | 11.5 | 4.92 | 8 |
| Globalisation and Health | 1744-8603 | Journal | 1 | 20.80 | 104 | 8.7 | 10.401 | 9 |
| Journal of Medical Internet Research | 1438-8871 | Journal | 4 | 74.67 | 43 | 8.2 | 7.076 | 10 |
| Journal of Biomedical Informatics (JBI) | 1532-0480 | Journal | 2 | 31.23 | 86 | 8.2 | 8 | 11 |
| npj Digital Medicine | 2398-6352 | Journal | 1 | 19.00 | 39 | 11.8 | 15.357 | 12 |
| JMIR mHealth and uHealth | 2291-5222 | Journal | 1 | 33.00 | 99 | 8.2 | 4.947 | 13 |
| BMC Health Services Research | 1472-6963 | Journal | 3 | 48.17 | 164 | 3.9 | 2.908 | 14 |
| Health Information Management Journal (HIMJ) | 1833-3575 | Journal | 3 | 22.79 | 53 | 5.6 | 3.778 | 15 |
| Health Systems & Reform (HS&R) | 2328-8620 | Journal | 1 | 9.71 | 68 | 4.9 | 6.378 | 16 |
| International Journal of Medical Informatics | 1872-8243 | Journal | 1 | 5.53 | 83 | 8 | 4.73 | 17 |
| Healthcare (Amsterdam, Netherlands) | 2213-0772 | Journal | 1 | 19.75 | 79 | 2.5 | 3.16 | 18 |
| BMC Medical Ethics | 1472-6939 | Journal | 1 | 18.00 | 54 | 3.5 | 2.834 | 19 |
| Sensors | 1424-3210 | Journal | 1 | 8.40 | 42 | 6.4 | 3.847 | 20 |
| Health Policy | 1872-6054 | Journal | 1 | 6.22 | 56 | 5.2 | 3.255 | 21 |
| BMJ Open | 2044-6055 | Journal | 1 | 12.67 | 38 | 3.9 | 3.006 | 22 |
| Applied Clinical Informatics Journal (ACI) | 1869-0327 | Journal | 1 | 7.00 | 42 | 4 | 2.762 | 23 |
| IEEE Access | 2169-3536 | Journal | 1 | 5.75 | 23 | 6.7 | 3.476 | 24 |
| Methods of Information in Medicine | 2511-705X | Journal | 1 | 12.00 | 24 | 4.5 | 1.8 | 25 |
| Medical Archives | 1986-5961 | Journal | 1 | 11.00 | 88 | 1.9 | n.a. | 26 |
| International Journal of Population Data Science (IJPDS) | 2399-4908 | Journal | 1 | 16.67 | 50 | 2.2 | n.a. | 27 |
| PLOS ONE | 1932-6203 | Journal | 1 | 5.33 | 16 | 5.6 | 3.752 | 28 |
| Public Health Genomics | 1662-8063 | Journal | 1 | 9.00 | 27 | 2.9 | 2.132 | 29 |
| Healthcare Informatics Research (HIR) | 2093-369X | Journal | 1 | 5.44 | 49 | 5.1 | n.a. | 30 |
| Online Journal of Issues in Nursing (OJIN) | 1091-3734 | Journal | 1 | 13.43 | 94 | n.a. | n.a. | 31 |
| Symmetry | 2073-8994 | Journal | 1 | 11.00 | 22 | 4.3 | n.a. | 32 |
| Perspectives in Health Information Management | 1559-4122 | Journal | 1 | 8.75 | 105 | 1.1 | n.a. | 33 |
| Acta Informatica Medica | 1986-5988 | Journal | 1 | 9.00 | 36 | 2.7 | n.a. | 34 |
| Wellcome Open Research | 2398-502X | Journal | 1 | 8.50 | 17 | 5.2 | n.a. | 35 |
| Yearbook of Medical Informatics | 2364-0502 | Journal | 1 | 5.75 | 23 | 4.8 | n.a. | 36 |
| Journal of Healthcare Information Management (JHIM) | 1943-734X | Journal | 1 | 5.92 | 71 | n.a. | n.a. | 37 |
| IEEE Transactions on Information Technology in Biomedicine | 1558-0032 | Journal | 1 | 6.30 | 63 | n.a. | n.a. | 38 |
| Health and Technology | 2190-7196 | Journal | 1 | 7.00 | 14 | 3.2 | n.a. | 39 |
| Medical Law International | 2047-9441 | Journal | 1 | 6.11 | 55 | 0.9 | n.a. | 40 |
| Journal of Education and Health Promotion (JEHP) | 2319-6440 | Journal | 1 | 11.00 | 22 | 1.2 | n.a. | 41 |
| Personal and Ubiquitous Computing | 1617-4917 | Journal | 1 | 6.00 | 6 | 6.1 | n.a. | 42 |
| Advances in Health Care Management: Health information technology in the international context | 1474-8231 | Book Series | 1 | 6.00 | 60 | 0.6 | n.a. | 43 |
| Studies in Health Technology and Informatics | 1879-8365 | Book Series | 1 | 6.00 | 12 | 1.4 | n.a. | 44 |
| JMIR Formative Research | 2561-326X | Journal | 1 | 5.00 | 5 | 1.8 | n.a. | 45 |
This part of the formula is not applied if the metric is n.a.
VOSviewer software title and abstract analysis
The database generated in Endnote was exported and evaluated using the VOSviewer software. The analysis was based on the information within the article’s title and abstract. Both abstract and title information are core information vessels within articles, crucial for article search optimisation within databases. Three dimensions were targeted for evaluation as they allowed an integrated analysis: (1) network visualisation, (2) overlay visualisation and (3) density visualisation. The first dimension showed the level of relationship between words, providing information about potential word clusters, and allowing their naming (via word analysis), for better understanding. The overlay visualisation showed which words and clusters were trending. The final dimension complemented the network visualisation by presenting simplified information about each word’s relevance.
The title network visualisation analysis found the existence of three clusters (Supplemental material, Figure S1, online supplement). The first cluster (e-health information future trends) consisted of the terms “blockchain technology,” “challenges,” “future direction” and “systematic review.” The second cluster (e-health information uncertainty) has in its composition the terms “challenge,” “development,” “health care” and “opportunity.” Terms such as “electronic health record,” “evaluation” and “healthcare” formed the final cluster (e-health information quality assessment).
Figure 4.
Theoretical framework to achieve high quality in interoperability and data linkage processes.
When observing the same data display through the overlay visualisation (Supplemental material Figure S2, online supplement), the three clusters appear to have an increasing chronological timeline, as the e-health information future trends cluster appears to have been discussed later in 2020, while the e-health information uncertainty emerged mainly between 2015 and 2018. The oldest cluster was the e-health information quality assessment. The density analysis performed showed that the distribution of occurrences of words in all three clusters was similar. The e-health information quality assessment cluster was the most homogeneous, while the other two clusters were slightly heterogeneous (Supplemental material Figure S3, online supplement).
The abstract analysis (displayed in Figure S4, online supplement) revealed that increasing relationship between words when compared to the title analysis. In accordance with the title evaluation, the network visualisation analysis also presented three clusters. The first cluster (e-health information stakeholder needs) consists of the terms “EHR,” “electronic health record,” “hospital,” “integration,” “interoperability,” “lack,” “patient,” “standard” and “system”; the second cluster (e-health information quality assessment) has in its composition the terms “article,” “challenge,” “data,” “field,” “need,” “quality,” “research” and “researcher”; while the final cluster (e-health information technological governance trends) was related to “blockchain,” “privacy” and “security.”
In terms of timeline analysis (Supplemental material Figure S5, online supplement), the e-health information technological governance trends cluster was the most recent, while the other two clusters appeared to fall within the years 2015 and 2018. When the data were arranged by number of occurrences, the density analysis (Supplemental material Figure S6, online supplement) revealed that the most prominent words in the e-health information stakeholder need cluster were “interoperability” and “system,” with 48 and 44 occurrences, respectively. As for the e-health information quality assessment cluster, terms such as “data” (45 occurrences), “challenge” and “research” (both with 26 occurrences) formed the core of the cluster. “Privacy” (20 occurrences) was the leading word in the e-health information technological governance trends cluster.
An integrated view of the cluster information retrieved through the VOSviewer software was also established (Figure 4). This original view of the title and abstract clusters demonstrated their interconnectivity pattern and relationship with system interoperability and data linkage.
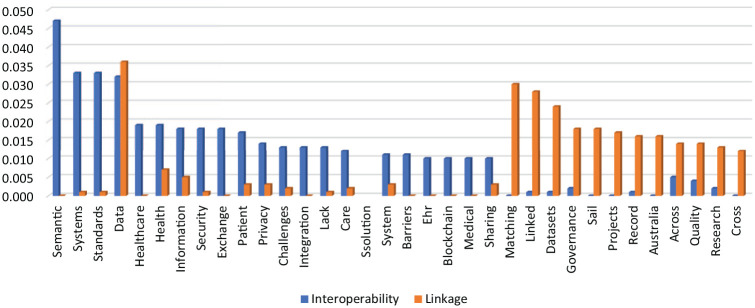
WORDSTAT software proximity of keywords analysis: interoperability versus linkage
A proximity analysis of the selected two keywords by WORDSTAT software (Provalis Research, Montreal, Canada) was performed, and the data retrieved were analysed in Microsoft Excel (Figure 5). According to data retrieved, the terms most associated (association above 0.013) with “interoperability” were (1) semantic, (2) systems, (3) standards, (4) data, (5) healthcare, (6) health, (7) information, (8) security, (9) exchange, (10) patient, (11) privacy, (12) integration and (13) lack. As for the word “linkage,” the following results emerged: (1) data, (2) matching, (3) linked, (4) dataset, (5) governance, (6) sail, (7) projects, (8) record, (9) Australia, (10) across, (11) quality, (12) research. The only word with a similar proximity to the two words in the analysis was “data.”
Figure 5.
Proximity of keywords analysis by WORDSTAT: interoperability vs. linkage.
Discussion
Sample timeline results
The sample’s timeline provided mixed results. While article numbers increased from years 2016 to 2020, they decreased abruptly in 2021. Conversely, global results containing abstracts continued to grow in 2021, suggesting that topics related to the scope of this research may have been redirected into other core subject areas, or that the COVID-19 pandemic may have resulted in quick solutions being incorporated into the marketplace with limited concern for data linkage and systems interoperability.
Journal and article metrics
The reference global impact ranking metric attempts to eliminate the chronological bias that exists when only the number of citations of an article are taken into account. Usually, articles published earlier have an increased probability of achieving a higher number of citations, diminishing the importance of articles published more recently, with less time to accumulate possible citations. As the results of our study have demonstrated, the article citation metric does not correlate with the global impact ranking position; and that the ranking provides a more accurate method to evaluate the impact of research within the overall scope of this (data linkage and systems interoperability within health information management) research domain. The publication global impact ranking in our study produced similar results to the article global impact ranking, meaning the cross-combination of impact metrics and citation metrics did not correlate with standardised impact metrics. These findings suggest that worldwide acceptable metrics are not the best method to evaluate the influence and power of journals within specific disciplinary domains.
Interoperability versus Linkage
In this study, interoperability and linkage concepts appeared distinct. The abstract analysis performed in the sample selection procedure showed that most abstracts contained the word “interoperability” while “linkage” was present in only a few. Only one abstract had both words. This simple analysis showed that researchers were giving more importance to interoperability than to linkage, and they either did not value or they overlooked the potential symbiotic power within the connection between these two disciplines. A further analysis that points to this same finding is the proximity of a keywords analysis performed in WORDSTAT software. The collected data showed that the term “interoperability” had a stronger association with a greater number of words when compared with the word “linkage.” The lack of association between these two words was also apparent, as only a few words achieved a strong association.
VOSviewer cluster findings
The VOSviewer analysis originated three title clusters and three abstract clusters. As these clusters have interconnections, a theoretical framework was established as demonstrated in Figure 4. According to Figure 4, four levels were defined, representing different degrees of broadness. The outer layer is the most wide-ranging, and this complexity diminishes gradually until reaching the core. Interoperability and linkage issues in electronic health information management are uncertain as new trends emerge. To mitigate this uncertainty, governance models and stakeholders’ needs such as those explored by Witry et al. (2010), Alkraiji et al. (2013), Lavin et al. (2015), Abdekhoda et al. (2016) and Ammar et al. (2021) must be assessed so electronic health information possesses the highest degree of quality in which system interoperability and data linkage can achieve their purpose with efficacy and efficiency.
Limitations and advantages
The current study had some limitations. First, in the data-gathering process, results exported from the three search platforms did not generate the same quality of information when imported into Endnote, meaning some crucial data were missing (e.g. some Google Scholar results were without year, abstract and publication information). Second, the criteria applied in the sample selection process, such as the one associated with article citations and selected keywords included in abstracts, may have enhanced the elimination of important articles. Third, sample data extracted from Endnote presented limitations when imported into software such as VOSviewer. However, this study has at least three advantages. To the best of our knowledge, this is the first bibliometric research in which electronic health information has intersected with both interoperability and linkage domains. Second, even with the above limitations, it was still possible to assess the quality and evolution of research about the subject of analysis. Finally, the current research provides insights into the main topics and concerns of the role of interoperability and linkage in health information systems.
Conclusion
Results of this study have outlined theoretical and managerial implications of interoperability and linkage in health information management. One theoretical contribution is based on the need for more literature research about the combined role of interoperability and linkage in health information management, as the existent articles may suggest a lack of interest in the topic area. Also, new metrics and rankings were created to measure the real impact of articles and of journals within the scope of this research, minimising the biases provided by general impact factors and metrics that do not consider research subject specifications. In terms of managerial contributions, this research points to the necessity for the healthcare and information technology sectors to co-develop their solutions, to always consider linkage and interoperability concerns and to put the final consumer as a key player in their discussions. Moreover, these sectors should verify and evaluate stakeholders’ real-world needs so they can introduce their contributions to optimise the architecture of information technology solutions.
Supplemental Material
Supplemental material, sj-docx-1-him-10.1177_18333583241277952 for System interoperability and data linkage in the era of health information management: A bibliometric analysis by Tiago Costa, Teresa Borges-Tiago, Francisco Martins and Flávio Tiago in Health Information Management Journal
Supplemental material, sj-docx-2-him-10.1177_18333583241277952 for System interoperability and data linkage in the era of health information management: A bibliometric analysis by Tiago Costa, Teresa Borges-Tiago, Francisco Martins and Flávio Tiago in Health Information Management Journal
Supplemental material, sj-docx-3-him-10.1177_18333583241277952 for System interoperability and data linkage in the era of health information management: A bibliometric analysis by Tiago Costa, Teresa Borges-Tiago, Francisco Martins and Flávio Tiago in Health Information Management Journal
Supplemental material, sj-docx-4-him-10.1177_18333583241277952 for System interoperability and data linkage in the era of health information management: A bibliometric analysis by Tiago Costa, Teresa Borges-Tiago, Francisco Martins and Flávio Tiago in Health Information Management Journal
Supplemental material, sj-jpg-5-him-10.1177_18333583241277952 for System interoperability and data linkage in the era of health information management: A bibliometric analysis by Tiago Costa, Teresa Borges-Tiago, Francisco Martins and Flávio Tiago in Health Information Management Journal
Supplemental material, sj-jpg-6-him-10.1177_18333583241277952 for System interoperability and data linkage in the era of health information management: A bibliometric analysis by Tiago Costa, Teresa Borges-Tiago, Francisco Martins and Flávio Tiago in Health Information Management Journal
Supplemental material, sj-jpg-7-him-10.1177_18333583241277952 for System interoperability and data linkage in the era of health information management: A bibliometric analysis by Tiago Costa, Teresa Borges-Tiago, Francisco Martins and Flávio Tiago in Health Information Management Journal
Supplemental material, sj-jpg-8-him-10.1177_18333583241277952 for System interoperability and data linkage in the era of health information management: A bibliometric analysis by Tiago Costa, Teresa Borges-Tiago, Francisco Martins and Flávio Tiago in Health Information Management Journal
Supplemental material, sj-jpg-9-him-10.1177_18333583241277952 for System interoperability and data linkage in the era of health information management: A bibliometric analysis by Tiago Costa, Teresa Borges-Tiago, Francisco Martins and Flávio Tiago in Health Information Management Journal
Supplemental material, sj-jpg-10-him-10.1177_18333583241277952 for System interoperability and data linkage in the era of health information management: A bibliometric analysis by Tiago Costa, Teresa Borges-Tiago, Francisco Martins and Flávio Tiago in Health Information Management Journal
Acknowledgments
We gratefully acknowledge the support from FCT – Foundation for Science and Technology (Portugal) through research grants UIDB/00685/2020 of the Centre of Applied Economics Studies of the Atlantic, School of Business and Economics of the University of the Azores, UIDB/04521/2020 of the Advance/CSG, ISEG – Lisbon School of Economics and Management, and UIDB/CEC/00408/2019 LASIGE, Faculty of Sciences of the University of Lisbon.
Footnotes
Author contributions: Tiago Costa (conceptualisation; methodology; formal analysis; investigation; data curation; writing [original draft]; writing [review and editing]; visualisation; project administration; funding acquisition). Teresa Borges-Tiago (conceptualisation; writing [review and editing]; supervision). Francisco Martins (conceptualisation; writing [review and editing]; supervision). Flávio Tiago (conceptualisation; writing [review and editing]; supervision). All authors read and approved the final manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The author(s) disclosed receipt of the financial support for the research of this article provided by the PRO-SCIENTIA programme of the Regional Directorate for Science and Technology (DRCT) of the Regional Government of the Azores through the doctoral research grant with the reference M3.1.E/PROPINAS DE DOUTORAMENTO/004/2022 awarded to the author Tiago Costa.
ORCID iD: Tiago Costa  https://orcid.org/0000-0001-8020-1897
https://orcid.org/0000-0001-8020-1897
Supplemental material: Supplemental material for this article is available online.
References
- Abdekhoda M, Ahmadi M, Dehnad A, et al. (2016) Applying electronic medical records in health care: Physicians’ perspective. Applied Clinical Informatics 7(2): 341–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmadi M, Aslani N. (2018) Capabilities and advantages of cloud computing in the implementation of electronic health record. Acta Informatica Medica 26(1): 24–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed Z, Mohamed K, Zeeshan S, et al. (2020) Artificial intelligence with multi-functional machine learning platform development for better healthcare and precision medicine. Database (Oxford) 2020; 2020: baaa010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alkraiji A, Jackson T, Murray I. (2013) Barriers to the widespread adoption of health data standards: An exploratory qualitative study in tertiary healthcare organizations in Saudi Arabia. Journal of Medical Systems 37(2): 9895. [DOI] [PubMed] [Google Scholar]
- Alonso SG, Arambarri J, Lopez-Coronado M, et al. (2019) Proposing new blockchain challenges in eHealth. Journal of Medical Systems 43(3): 1–7. [DOI] [PubMed] [Google Scholar]
- Ammar N, Bailey JE, Davis RL, et al. (2020) The personal health library: A single point of secure access to patient digital health information. Studies in Health Technology and Informatics 270: 448–452. [DOI] [PubMed] [Google Scholar]
- Ammar N, Bailey JE, Davis RL, et al. (2021) Using a personal health library-enabled mHealth recommender system for self-management of diabetes among underserved populations: Use case for knowledge graphs and linked data. JMIR Formative Research 5(3): e24738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arul R, Al-Otaibi YD, Alnumay WS, et al. (2024) Multi-modal secure healthcare data dissemination framework using blockchain in IoMT. Personal and Ubiquitous Computing 28: 3–15. [Google Scholar]
- Avila K, Sanmartin P, Jabba D, et al. (2017) Applications based on service-oriented architecture (SOA) in the field of home healthcare. Sensors (Basel) 17(8): 1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azarm M, Backman C, Kuziemsky C, et al. (2017) Breaking the healthcare interoperability barrier by empowering and engaging actors in the healthcare system. Procedia Computer Science 113: 326–333. [Google Scholar]
- Bahga A, Madisetti VK. (2013) A cloud-based approach for interoperable electronic health records (EHRs). IEEE Journal of Biomedical and Health Informatics 17(5): 894–906. [DOI] [PubMed] [Google Scholar]
- Bates DW. (2005) Physicians and ambulatory electronic health records. Health Affairs 24(5): 1180–1189. [DOI] [PubMed] [Google Scholar]
- Blasimme A, Fadda M, Schneider M, et al. (2018) Data sharing for precision medicine: Policy lessons and future directions. Health Affairs 37(5): 702–709. [DOI] [PubMed] [Google Scholar]
- Blazona B, Koncar M. (2007) HL7 and DICOM based integration of radiology departments with healthcare enterprise information systems. International Journal of Medical Informatics 76(Suppl 3): S425–S432. [DOI] [PubMed] [Google Scholar]
- Bohensky MA, Jolley D, Sundararajan V, et al. (2010) Data linkage: A powerful research tool with potential problems. BMC Health Serv Res 10: 346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd JH, Randall SM, Ferrante AM, et al. (2015) Accuracy and completeness of patient pathways – The benefits of national data linkage in Australia. BMC Health Services Research 15(1): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christen P. (2019) Data linkage: The big picture. Harvard Data Science Review. Epub ahead of print 1 November 2019. DOI: 10.1162/99608f92.84deb5c4. [DOI] [Google Scholar]
- de Moura Costa HJ, da Costa CA, da Rosa Righi R, et al. (2020) Fog computing in health: A systematic literature review. Health and Technology 10: 1025–1044. [Google Scholar]
- de Quiros FGB, Otero C, Luna D. (2018) Terminology services: Standard terminologies to control health vocabulary. Yearbook of Medical Informatics 27(1): 227–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Detmer D, Bloomrosen M, Raymond B, et al. (2008) Integrated personal health records: Transformative tools for consumer-centric care. BMC Medical Informatics and Decision Making 8: 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinh-Le C, Chuang R, Chokshi S, et al. (2019) Wearable health technology and electronic health record integration: Scoping review and future directions. JMIR mHealth and uHealth 7(9): e12861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downs JM, Ford T, Stewart R, et al. (2019) An approach to linking education, social care and electronic health records for children and young people in South London: A linkage study of child and adolescent mental health service data. BMJ Open 9(1): e024355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubovitskaya A, Baig F, Xu Z, et al. (2020) ACTION-EHR: Patient-centric blockchain-based electronic health record data management for cancer care. Journal of Medical Internet Research 22(8): e13598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durneva P, Cousins K, Chen M. (2020) The current state of research, challenges, and future research directions of blockchain technology in patient care: Systematic review. Journal of Medical Internet Research 22(7): e18619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards A, Hollin I, Barry J, et al. (2010) Barriers to cross-institutional health information exchange: A literature review. Journal of Healthcare Information Management 24(3): 22–34. [PubMed] [Google Scholar]
- Emmer A, Allen SK, Carey M, et al. (2022) Progress and challenges in glacial lake outburst flood research (2017–2021): A research community perspective. Natural Hazards and Earth System Sciences 22(9): 3041–3061. [Google Scholar]
- Ford DV, Jones KH, Verplancke JP, et al. (2009) The SAIL databank: Building a national architecture for e-health research and evaluation. BMC Health Services Research 9: 157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furukawa MF, Patel V, Charles D, et al. (2013) Hospital electronic health information exchange grew substantially in 2008–12. Health Affairs 32(8): 1346–1354. [DOI] [PubMed] [Google Scholar]
- Gamal A, Barakat S, Rezk A. (2021) Standardized electronic health record data modeling and persistence: A comparative review. Journal of Biomedical Informatics 114: 103670. [DOI] [PubMed] [Google Scholar]
- Genevieve LD, Martani A, Mallet MC, et al. (2019) Factors influencing harmonized health data collection, sharing and linkage in Denmark and Switzerland: A systematic review. PLoS One 14(12): e0226015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon WJ, Catalini C. (2018) Blockchain technology for healthcare: Facilitating the transition to patient-driven interoperability. Computational and Structural Biotechnology Journal 16: 224–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gowda V, Schulzrinne H, Miller BJ. (2022) The case for medical device interoperability. JAMA Health Forum 3(1): e214313. [DOI] [PubMed] [Google Scholar]
- Green E, Ritchie F, Webber DJ, et al. (2015) Enabling data linkage to maximise the value of public health research data: Full report. Report, UK, Wellcome Trust, March. [Google Scholar]
- Harron K. (2016) A introduction to data linkage. In: Mackey E, Elliot M. (eds.) Better Knowledge Better Society. Colchester: University of Essex, pp. 1–22. [Google Scholar]
- Holman CD, Bass AJ, Rosman DL, et al. (2008) A decade of data linkage in Western Australia: Strategic design, applications and benefits of the WA data linkage system. Australian Health Review 32(4): 766–777. [DOI] [PubMed] [Google Scholar]
- Hopf YM, Bond C, Francis J, et al. (2014) Views of healthcare professionals to linkage of routinely collected healthcare data: A systematic literature review. Journal of the American Medical Informatics Association 21(e1): e6–e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopf YM, Francis J, Helms PJ, et al. (2016) Core requirements for successful data linkage: An example of a triangulation method. BMJ Open 6(10): e011879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang F, Blaschke S, Lucas H. (2017) Beyond pilotitis: Taking digital health interventions to the national level in China and Uganda. Globalization and Health 13(1): 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussien HM, Yasin SM, Udzir SNI, et al. (2019) A systematic review for enabling of develop a blockchain technology in healthcare application: Taxonomy, substantially analysis, motivations, challenges, recommendations and future direction. Journal of Medical Systems 43(10): 320. [DOI] [PubMed] [Google Scholar]
- Hylock RH, Zeng X. (2019) A blockchain framework for patient-centered health records and exchange (HealthChain): Evaluation and proof-of-concept study. Journal of Medical Internet Research 21(8): e13592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iroju O, Soriyan A, Gambo I, et al. (2013) Interoperability in healthcare: Benefits, challenges and resolutions. International Journal of Innovation and Applied Studies 3(1): 262–270. [Google Scholar]
- Ismail L, Materwala H. (2020) Blockchain paradigm for healthcare: Performance evaluation. Symmetry 12(8): 1–19. [Google Scholar]
- Joda T, Waltimo T, Probst-Hensch N, et al. (2019) Health data in dentistry: An attempt to master the digital challenge. Public Health Genomics 22(1–2): 1–7. [DOI] [PubMed] [Google Scholar]
- Johnson SB, Bakken S, Dine D, et al. (2008) An electronic health record based on structured narrative. Journal of the American Medical Informatics Association 15(1): 54–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones KH, Ford DV, Jones C, et al. (2014) A case study of the Secure Anonymous Information Linkage (SAIL) Gateway: A privacy-protecting remote access system for health-related research and evaluation. Journal of Biomedical Informatics 50: 196–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones KH, Ford DV, Thompson S, et al. (2019) A profile of the SAIL databank on the UK secure research platform. International Journal of Population Data Science 4(2): 1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalkman S, Mostert M, Gerlinger C, et al. (2019) Responsible data sharing in international health research: A systematic review of principles and norms. BMC Medical Ethics 20(1): 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan B, Harris-Salamone KD. (2009) Health IT success and failure: Recommendations from literature and an AMIA workshop. Journal of the American Medical Informatics Association 16(3): 291–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasthurirathne SN, Mamlin B, Kumara H, et al. (2015) Enabling better interoperability for healthcare: Lessons in developing a standards based application programing interface for electronic medical record systems. Journal of Medical Systems 39(11): 1–8. [DOI] [PubMed] [Google Scholar]
- Kharrazi H, Lasser EC, Yasnoff WA, et al. (2017) A proposed national research and development agenda for population health informatics: Summary recommendations from a national expert workshop. Journal of the American Medical Informatics Association 24(1): 2–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koppel R, Lehmann CU. (2015) Implications of an emerging EHR monoculture for hospitals and healthcare systems. Journal of the American Medical Informatics Association 22(2): 465–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krittanawong C, Rogers AJ, Aydar M, et al. (2020) Integrating blockchain technology with artificial intelligence for cardiovascular medicine. Nature Reviews Cardiology 17(1): 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavin MA, Harper E, Barr N. (2015) Health information technology, patient safety, and professional nursing care documentation in acute care settings. Online Journal of Issues in Nursing 20(2): 6. [PubMed] [Google Scholar]
- Lee HA, Kung HH, Udayasankaran JG, et al. (2020) An architecture and management platform for blockchain-based personal health record exchange: Development and usability study. Journal of Medical Internet Research 22(6): e16748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehne M, Sass J, Essenwanger A, et al. (2019) Why digital medicine depends on interoperability. NPJ Digital Medicine 2: 79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucyk K, Tang K, Quan H. (2017) Barriers to data quality resulting from the process of coding health information to administrative data: A qualitative study. BMC Health Services Research 17(1): 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandel JC, Kreda DA, Mandl KD, et al. (2016) SMART on FHIR: A standards-based, interoperable apps platform for electronic health records. Journal of the American Medical Informatics Association 23(5): 899–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- March S, Andrich S, Drepper J, et al. (2020) Good practice data linkage (GPD): A translation of the German version. International Journal of Environmental Research and Public Health 17(21): 7852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masud M, Hossain MS, Alamri A. (2012) Data interoperability and multimedia content management in e-Health systems. IEEE Transactions on Information Technology in Biomedicine 16(6): 1015–1023. [DOI] [PubMed] [Google Scholar]
- Mohammadzadeh N, Safdari R. (2014) Patient monitoring in mobile health: Opportunities and challenges. Medical Archives 68(1): 57–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oderkirk J, Ronchi E, Klazinga N. (2013) International comparisons of health system performance among OECD countries: Opportunities and data privacy protection challenges. Health Policy 112(1–2): 9–18. [DOI] [PubMed] [Google Scholar]
- Park E, Kim JH, Nam HS, et al. (2018) Requirement analysis and implementation of smart emergency medical services. IEEE Access 6: 42022–42029. [Google Scholar]
- Reisman M. (2017) EHRs: The challenge of making electronic data usable and interoperable. P&T 42(9): 572–575. [PMC free article] [PubMed] [Google Scholar]
- Rezaeibagha F, Win KT, Susilo W. (2015) A systematic literature review on security and privacy of electronic health record systems: Technical perspectives. Health Information Management Journal 44(3): 23–38. [DOI] [PubMed] [Google Scholar]
- Salas-Vega S, Haimann A, Mossialos E. (2015) Big data and health care: Challenges and opportunities for coordinated policy development in the EU. Health Systems & Reform 1(4): 285–300. [DOI] [PubMed] [Google Scholar]
- Samra H, Li A, Soh B, et al. (2020) Utilisation of hospital information systems for medical research in Saudi Arabia: A mixed-method exploration of the views of healthcare and IT professionals involved in hospital database management systems. Health Information Management Journal 49(2–3): 117–126. [DOI] [PubMed] [Google Scholar]
- Sethi N, Laurie GT. (2013) Delivering proportionate governance in the era of eHealth: Making linkage and privacy work together. Medical Law International 13(2–3): 168–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanbehzadeh M, Kazemi-Arpanahi H, Mazhab-Jafari K, et al. (2020) Coronavirus disease 2019 (COVID-19) surveillance system: Development of COVID-19 minimum data set and interoperable reporting framework. Journal of Education and Health Promotion 9: 203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinaci AA, Nunez-Benjumea FJ, Gencturk M, et al. (2020) From raw data to FAIR data: The FAIRification workflow for health research. Methods of Information in Medicine 59(S 01): e21–e32. [DOI] [PubMed] [Google Scholar]
- Sittig DF, Belmont E, Singh H. (2018) Improving the safety of health information technology requires shared responsibility: It is time we all step up. Healthcare 6(1): 7–12. [DOI] [PubMed] [Google Scholar]
- Tapuria A, Kalra D, Kobayashi S. (2013) Contribution of clinical archetypes, and the challenges, towards achieving semantic interoperability for EHRs. Healthcare Informatics Research 19(4): 286–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiago M, Tiago F, Amaral F, et al. (2016) Healthy 3.0: Healthcare digital dimensions. In Dwivedi A (ed.) Reshaping medical practice and care with health information systems. Hershey, Pennsylvania: IGI Global, pp. 287–322. [Google Scholar]
- Torab-Miandoab A, Samad-Soltani T, Jodati A, et al. (2023) Interoperability of heterogeneous health information systems: A systematic literature review. BMC Medical Informatics and Decision Making 23(1): 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Olmen J, Erwin E, Garcia-Ulloa AC, et al. (2020) Implementation barriers for mHealth for non-communicable diseases management in low and middle income countries: A scoping review and field-based views from implementers. Wellcome Open Research 5: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vazirani AA, O’Donoghue O, Brindley D, et al. (2020) Blockchain vehicles for efficient medical record management. NPJ Digital Medicine 3: 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vest JR. (2012) Health information exchange: National and international approaches. Advances in Health Care Management 12: 3–24. [DOI] [PubMed] [Google Scholar]
- Warner JL, Rioth MJ, Mandl KD, et al. (2016) SMART precision cancer medicine: A FHIR-based app to provide genomic information at the point of care. Journal of the American Medical Informatics Association 23(4): 701–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winglee M, Valliant R, Scheuren F. (2005) A case study in record linkage. Survey Methodology 31(1): 3–11. [Google Scholar]
- Witry MJ, Doucette WR, Daly JM, et al. (2010) Family physician perceptions of personal health records. Perspectives in Health Information Management 7(Winter): 1d. [PMC free article] [PubMed] [Google Scholar]
- Wollersheim D, Sari A, Rahayu W. (2009) Archetype-based electronic health records: A literature review and evaluation of their applicability to health data interoperability and access. Health Information Management Journal 38(2): 7–17. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-him-10.1177_18333583241277952 for System interoperability and data linkage in the era of health information management: A bibliometric analysis by Tiago Costa, Teresa Borges-Tiago, Francisco Martins and Flávio Tiago in Health Information Management Journal
Supplemental material, sj-docx-2-him-10.1177_18333583241277952 for System interoperability and data linkage in the era of health information management: A bibliometric analysis by Tiago Costa, Teresa Borges-Tiago, Francisco Martins and Flávio Tiago in Health Information Management Journal
Supplemental material, sj-docx-3-him-10.1177_18333583241277952 for System interoperability and data linkage in the era of health information management: A bibliometric analysis by Tiago Costa, Teresa Borges-Tiago, Francisco Martins and Flávio Tiago in Health Information Management Journal
Supplemental material, sj-docx-4-him-10.1177_18333583241277952 for System interoperability and data linkage in the era of health information management: A bibliometric analysis by Tiago Costa, Teresa Borges-Tiago, Francisco Martins and Flávio Tiago in Health Information Management Journal
Supplemental material, sj-jpg-5-him-10.1177_18333583241277952 for System interoperability and data linkage in the era of health information management: A bibliometric analysis by Tiago Costa, Teresa Borges-Tiago, Francisco Martins and Flávio Tiago in Health Information Management Journal
Supplemental material, sj-jpg-6-him-10.1177_18333583241277952 for System interoperability and data linkage in the era of health information management: A bibliometric analysis by Tiago Costa, Teresa Borges-Tiago, Francisco Martins and Flávio Tiago in Health Information Management Journal
Supplemental material, sj-jpg-7-him-10.1177_18333583241277952 for System interoperability and data linkage in the era of health information management: A bibliometric analysis by Tiago Costa, Teresa Borges-Tiago, Francisco Martins and Flávio Tiago in Health Information Management Journal
Supplemental material, sj-jpg-8-him-10.1177_18333583241277952 for System interoperability and data linkage in the era of health information management: A bibliometric analysis by Tiago Costa, Teresa Borges-Tiago, Francisco Martins and Flávio Tiago in Health Information Management Journal
Supplemental material, sj-jpg-9-him-10.1177_18333583241277952 for System interoperability and data linkage in the era of health information management: A bibliometric analysis by Tiago Costa, Teresa Borges-Tiago, Francisco Martins and Flávio Tiago in Health Information Management Journal
Supplemental material, sj-jpg-10-him-10.1177_18333583241277952 for System interoperability and data linkage in the era of health information management: A bibliometric analysis by Tiago Costa, Teresa Borges-Tiago, Francisco Martins and Flávio Tiago in Health Information Management Journal