Abstract
Background
Research on Qi Gong (QG) supports promising health benefits. Both interest and use of QG in U.S. adults has increased over the past decade. Shared Medical Appointments (SMAs) are a novel, cost-effective, and time efficient health care delivery approach associated with patient and clinician satisfaction.
Objectives
A telehealth delivered QG SMA was pilot tested among a diverse demographic population within an integrative medicine practice at an academic medical center to assess feasibility and acceptability.
Methods
This was a feasibility/acceptability pilot study conducted at a large New York City academic medical center’s Integrative Health and Wellness center from January to July 2023. A QG instructor-acupuncturist and an integrative medicine physician-acupuncturist co-led 3 separate series (5 Element QG, Eight-Section Brocade, and Joint-Mobilizing/Sinew Strengthening exercises) of weekly 30-45-minute sessions of QG SMA on a weekday afternoon via telemedicine. The first session included an overview of QG and Traditional Chinese Medicine (TCM) research while follow-up sessions included a check-in, didactic demonstration followed by QG practice, and a debrief to answer questions. Video links were provided for home practice. Surveys assessing satisfaction were sent pre/post series.
Results
18 sessions of QG SMA were offered over a 6-month period. A total of 40 unique participants from diverse demographics (gender, race/ethnicity, primary residence) attended, for a total of 197 virtual visits. A total of 20 participants enrolled in Series 1 (8 weeks), 23 enrolled in Series 2 (7 weeks), and 16 enrolled in Series 3 (3cweeks). For each session, group attendance ranged from 8-16 with an average of 11 participants. Attendance was high with participants attending an average of 72% of the sessions. Participants attended 88% of the first 8-week series, 54% of the second 7-week series, and 60% of the third series. Participant interest persisted over time with 35% of the 40 participants attending more than 1 series, and 12.5% attending all 3 series. Participants’ diagnoses and health symptoms included pain (62.5%), cancer (45%) anxiety/depression (40%), cardiovascular disease (CVD) or metabolic conditions (32.5%), gastrointestinal (GI) symptoms/diagnoses (27.5%), stress (22.5%), osteopenia/osteoporosis (17.5%), and insomnia (17.5%). Pre-series [n = 27] participants endorsed symptoms including sleep disturbances, fatigue, pain, stress, weakness, GI symptoms, psychological symptoms, hot flashes, and brain fog. Post-program survey results [n = 11] suggested QG program addressed common symptoms including fatigue, insomnia, anxiety, stress, pain, weakness, and gastrointestinal symptoms. Participants reported incorporating QG, breathing techniques, and meditation into their daily routine. All participants reported their goals were met and that they would recommend the program to others. Regarding delivery preferences, 73% preferred telehealth, 27% hybrid, and none preferred in-person. Participants appreciated the format, new skills, community, and instructors.
Conclusion
While the Virtual QG SMA series provided to diverse demographic population with mixed diagnoses is feasible, acceptable, and shows promising positive impact in this pilot, caution in interpreting the data is advised due to the low response rate of the post-program survey. Robust studies with longer follow-ups are recommended.
Keywords: Qi Gong, shared medical appointment, group medical visit, telehealth, remote delivery, integrative medicine, mindful movement, traditional Chinese medicine, pain, anxiety, depression, cancer, cardiovascular, fatigue, stress, neuropathy, balance
Background
Between 2007 and 2017, Tai Chi/Qi Gong (TCQG) use in U.S. adults increased by 64%. The greatest increases in TCQG use (in 2017) were among vulnerable subgroups 1 (older adults, lower income, female, delayed access to health care, physically inactive).
Positive trends have been observed for improving anxiety, stress, depressive symptoms, fatigue, sleep quality, and quality of life among cancer patients who participate in Qi Gong (QG) and Baduanjin.2-5 QG, particularly Baduanjin (a popular QG set), improved sleep quality in adult populations with and without chronic conditions (fatigue, fibromyalgia, cancer, Parkinson disease, chronic low back pain, and stroke) and those with a chronic condition reported significantly greater sleep improvements after Health QG training. 6 QG is an effective and safe exercise with potential benefits in reducing severity and frequency of migraines 7 and hot flashes, 8 improving perimenopausal sleep quality, 8 and improving post-menopausal sleep (quality, latency, duration, efficiency). 9 It is also associated with physical, mental, and relational improvements in well-being. 10 Research on the use of QG to improve musculoskeletal pain, Parkinson’s, blood pressure, cancer, chronic obstructive pulmonary disease (COPD), chronic heart failure, maternal health, diabetes, and aging are promising.11-15
Shared medical appointments (SMA), also called group medical visits, have increased in popularity over the past 50 years as an innovative approach to improve health education and social support, access to care, and clinician well-being without increasing the cost of care.16-20 SMAs are a group health care model where patients with similar medical conditions participate in a collective appointment with health care providers. More recently, Integrative SMAs21-24 add complementary and integrative health (CIH) care education and services to existing SMA models 25 and may increase patient access to CIH services such as acupuncture, mindfulness, and yoga that are often inaccessible due to limited insurance coverage 26 and high out-of-pocket costs. They may also advance health equity by serving patient populations that have been historically negatively impacted by health and health care disparities.27-29
SMAs, including virtual ones, have been found to be feasible, cost-effective, time-efficient, and beneficial for both patients and clinicians. These appointments have also garnered interest and satisfaction among stakeholders.19,25,30-34 Virtual SMAs were successfully piloted in 2020-2022 at the Integrative Health Center of an academic tertiary care center in New York City among patients with various health concerns (oncology, women’s health) or modality interests (lifestyle change, yoga, acupuncture). Although telehealth visits became routine during the pandemic and improved access to care for underserved patients with chronic conditions,35-39 few studies have assessed the feasibility and impact of virtual QG group visits on both patients and clinicians. 40
Given the interest in mind-body SMAs, yoga, acupuncture, and Traditional Chinese Medicine (TCM), a telehealth delivered QG SMA among a mixed diagnosis population was piloted to assess feasibility and acceptability. Specifically, this study aimed to assess feasibility and acceptability of Virtual Qi Gong Shared Medical Appointment (VQGSMA) offered via telehealth among a diverse demographic population with mixed diagnoses within an integrative medicine practice at an urban tertiary care academic medical center and describe its potential impact on patient goals, clinician satisfaction, and institutional financial efficiency.
Methods
This was a feasibility/acceptability pilot 41 study at a large academic medical center’s Integrative Health and Wellness Center in New York City from January 2023 to July 2023.
Setting
The Integrative Health Center is part of a large urban academic medical center, providing evidence-based, comprehensive, holistic care to prevent disease, promote relaxation, reduce stress and anxiety, and relieve symptoms associated with medical conditions or their treatment. Types of services provided include consultations with physicians, acupuncturists, nutritionists, massage therapists, and mental health clinicians who provide a variety of integrative health therapies including psychoeducation, acupuncture, nutritional counseling, psychotherapy, mind-body therapies, massage therapy, in both 1:1 as well as group visit formats. Our center conducts 12 000 patient visits per year and serves adult and pediatric patients with complex diagnoses from the large urban city and surrounding areas. The center was initiated in 2016 through philanthropic support and is now sustained predominantly through insurance covered visits and hospital funding. The purpose of the center is to make evidence based integrative care accessible and affordable.
Participants
Participants were adult patients (18 years or older) of the academic medical center, English speaking, and had internet access.
Clinicians were employed by the academic medical center’s Integrative Health and were trained in an Integrative Medicine related field such as acupuncture, QG, or integrative medicine.
Invitations to participate were disseminated through flyers, referrals from integrative medicine clinicians, referrals from the institution’s primary care clinicians and specialists, hospital events page, email blasts, 42 word of mouth/patient testimonials, grand rounds presentations, and community outreach programs.
Intervention
Like previously described SMAs in the literature including Integrative Medicine Group Visits developed by Gardiner et al, 2017,43,44 our intervention involved patient groups that focused on health conditions and were led by a medical facilitator. However, what was unique about our intervention was that we taught QG using telehealth in a heterogeneous patient population (ages, gender, race/ethnicity) with mixed diagnoses. The VQGSMA series was initiated as a new service line under Integrative Health and co-led by an integrative medicine physician who is board certified in medical acupuncture and a QG instructor who is a board-certified acupuncturist. No new staff were hired to lead VQGSMA. Each VQGSMA visit combined didactics with experiential QG instruction.
The VQGSMAs were conducted in 3 separate series of weekly 30-45-minute sessions on a weekday afternoon via telehealth using the HIPAA-compliant version of Zoom teleconferencing software. Each visit consisted of a review of the small group confidentiality agreement, distinct didactic content, a QG demonstration followed by an experiential practice, and question/discussion time. During the demonstration and experiential, the QG instructor faced the camera (adjusting foot and body placement to allow viewing of form from multiple angles) while the integrative medicine physician provided technological support (helped participants connect online, monitored the chat box for questions, observed participant’s fidelity of movement, answered medical questions).
Series One
Consisted of 8-weekly sessions on the Five Elements and San Jiao. Five Element QG is a form of QG that harmonizes the Five Elements and Five Organs: Lung-Metal, Kidney-Water, Liver-Wood, Heart-Fire and Spleen-Earth. 45 San Jiao (“triple burner”, or “triple energizer”, or “triple heater”) is a concept in TCM and acupuncture. San Jiao is believed to be a body cavity of some kind which could influence other organs and overall health, mainly through the free movement of Qi. 46
Series Two
Consisted of 7-weekly sessions on Baduanjin (8-Section Brocade). Baduanjin QG (八段錦) is 1 of the most common forms of Chinese QG used as exercise. 47 This contrasts with religious or martial forms of QG. 48
Series Three
Consisted of 3-weekly sessions on myofascial stretches of the whole body. See Appendix 1 for list of exercises.
For the first 2 series, the first session of each series included an overview of QG for health, TCM, and the existing research on the benefits of QG. 11 In response to patient request to focus on the experiential, the overview of QG and description of TCM research was eliminated after series 2 without negative consequence. This information was weaved into the experiential and debriefing time according to participant interest. All sessions after the first session included a check in time (2-3 minutes), breathing (5 minutes), didactic demonstration with experiential practice of QG (20 min), and debriefing time (10 minutes). (The first session had an abbreviated experiential due to the overview). The sequences covered were the same during each session, but the level of difficulty increased with one’s understanding of each movement through repetition. This is because repetition allowed participants to focus on all the nuances of the movement such as timing, shifting of weight, and breath. Over time, the goal was to make the movements smoother, more efficient, and whole-body aligned.
Each series sequentially introduced exercises. Once all the elements were introduced, the instructor would lead participants in performing the entire sequence, culminating in the final session of the series, where participants were observed as a group performing the sequence twice without stopping.
At the beginning of the series, the physician would call each patient prior to the group visit for a brief check-in. In addition, the coordinator and physician would routinely call participants ahead of time to confirm attendance. If any discomfort with or access to technology was detected, technology guidance was provided. During the series, most of the patients saw either the integrative physician who co-led the VQGSMA, another integrative physician in the practice, or 1 of their other specialists (oncologist, pain management physician, etc.) at least once. Electronic health record (EHR) notes were reviewed at each group medical visit for coordination and continuity of care. Generic advice was given during the didactic portion of the group visit, and individualized advice based on diagnosis was provided and documented in the EHR. Following the VQGSMA, digital health resources based on questions from the discussion time and video of the QG instructor demonstrating exercise sequences for home practice were sent to participants through email.
Documentation of the VQGSMA visit along with individual medical management and customized recommendations and treatment plan, was completed by the physician with billing based on decision making complexity. The creation of detailed, customized visit templates (purpose, group interventions utilized, topics discussed) for each session greatly facilitated the electronic charting needed to generate billing information. Unlike “community classes”, our SMA began with a group check-in, ended with a group debriefing, offered safe QG delivery under the synergetic supervision of both an integrative medicine physician and a QG instructor, and provided pre/post-SMA coordination of care and collaboration with an interdisciplinary medical team led by integrative medicine physician (chart review and medication management requests). It focused on coping with and relieving symptoms and provided mental health benefits of group support. Our intervention responded to patient interest for receiving integrative health services in conjunction with their established health care at the academic medical center.
The group visit coordinator communicated with participants through phone, email, and the patient portal. The coordinator verified insurance, set up and disseminated the zoom link, and sent follow up resources. Electronic pre and post Qualtrics surveys were sent to participants at time of enrollment and after each series was completed. Additional qualitative feedback from participating interdisciplinary professionals was also gathered. The academic medical center’s Institutional Review Board (IRB) determined that this activity was not considered research involving human subjects due to its anonymous, program evaluation nature and that further IRB review and approval was not required.
Data and Outcome Measures
Electronic pre and post surveys using Qualtrics were sent via email from the SMA coordinator to participants at the time of enrollment and immediately after each series was completed.49,50 Responses to the 3-question pre-survey and 10-question post-surveys were optional and completely voluntary. No incentives were available or offered. Surveys were only written in English. All participants in our pilot were comfortable with English, although we did not determine fluency in English as a pre-requisite for participation. See Appendix 2 for surveys.
Sources of data included participant demographics, pre- and post-survey evaluations including responses to open-ended questions, and materials from the program development process. Short debriefing conversations between the integrative medicine physician-acupuncturist and the Qi Gong-acupuncturist occurred after co-led sessions without participants being present. These conversations facilitated an iterative processing of what was working and areas for improvement. Materials were created in the process of developing and implementing the VQGSMA, including e-mails, flyers, and handouts. Descriptive data were collated, and means were calculated in Excel. Responses to open-ended questions on the post-survey were reviewed by the authors. Responses were organized into general themes based on participants’ reported experiences. The center’s executive director performed cost analysis forecasting. The data source was organizational administrative data including elements such as encounters, diagnosis and procedure codes for clinical services, claims, amount billed, and amount reimbursed. Cost analysis methods evaluating efficiency of VQGSMA entailed comparing estimated reimbursement from 1-hour individual consultations for integrative medicine with estimated reimbursement from 1-hour SMAs. Costs for non-revenue generating clinicians and administrative support using hourly rates were factored into the cost/revenue forecasting. Details on the cost-analysis approach can be found in a previous publication. 51
Results
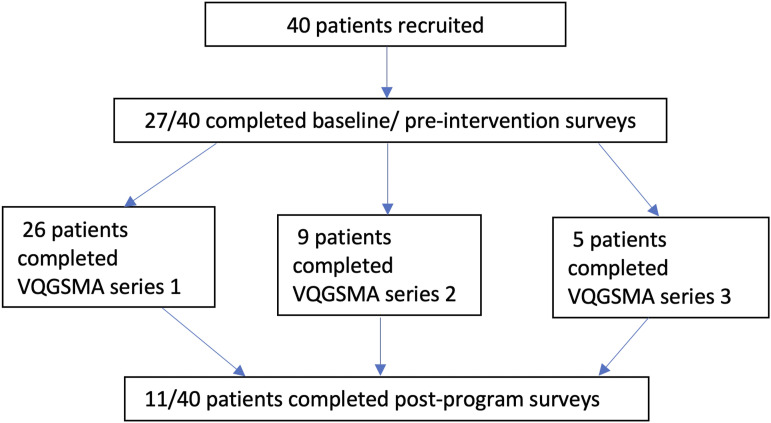
Between January and July 2023, 40 participants were recruited, of whom 27 (68%) completed the optional online pre-program survey and 11 (28%) the optional post-program survey [Figure 1]. A total of 18 sessions of VQGSMA (divided into 3 separate series covering different topics) were offered over a 6-month period. As we did not know how acceptable the VQGSMA would be to participants, only a 8-week series (Series 1) was initially offered. We decided to offer Series 2 (7 weeks) and Series 3 (3 weeks) based on participant feedback requesting more sessions. Over the 18 sessions, we had 59 participants (40 unique individuals) for a total of 197 virtual visits. A total of 20 participants enrolled in Series 1, 23 enrolled in Series 2, and 16 enrolled in Series 3 (Table 1). During each session, group attendance ranged from 8-16 with an average of 11 participants per session. Participation was high as reflected by participants attendance in Series 1 (88% of sessions), Series 2 (54% of sessions), Series 3 (60% of sessions). Participant interest also persisted over time. While the series were meant to be stand alone, some of the participants continued to show interest by choosing to enroll in subsequent series (with different didactic content). 35% of the 40 individuals participated in more than 1 series, and 12.5% attended all 3 series. Participants were not automatically enrolled in the subsequent series and had to contact the VQGSMA coordinator to enroll in subsequent series if desired.
Figure 1.
Participant recruitment and retention in Virtual Qi Gong Shared Medical Appointment (VQGSMAs) Series.
Table 1.
Attendance in Virtual Qi Gong Shared Medical Appointments (VQGSMA) by Series.
| VQGSMA Series # | Length of Series | Number of Participants | % of Sessions Attended by Series |
|---|---|---|---|
| One | 8 weeks | N = 20 | 88% (7/8 sessions) |
| Two | 7 weeks | N = 23 | 57% (4/7 sessions) |
| Three | 3 weeks | N = 16 | 60% (2/3 sessions) |
| Total (1 + 2 + 3) | 18 weeks | 40 a | 72% (13/18) |
aA total of 40 unique patients participated over the 18 weeks, with 19 of them participating in more than 1 session, for a total of 59 participants.
Participant demographics included primarily older (mean age 63 years), white (82%), females (80%) from city center (Manhattan or neighboring suburbs/states). However, nearly a third (30%) of participants lived in underserved areas (Harlem, Bronx, Queens, Brooklyn) and payor mix included 40% Medicare, 60% Commercial insurance (Table 2). Preferred spoken language was English.
Table 2.
Patient Demographic Characteristics, n = 40.
| Characteristic | |
|---|---|
| Mean age in years (range) | 63 (27 – 93) |
| Number (%) | |
| Gender | |
| Female | 32 (80%) |
| Male | 8 (20%) |
| Race | |
| Caucasian | 33 (82%) |
| Asian | 3 (7.5%) |
| African american | 3 (7.5%) |
| Other/Declined | 1 (2.5%) |
| Ethnicity | |
| Hispanic/Latino | 1 (2.5%) |
| Non-Hispanic/Latino | 39 (97.5%) |
| Location of residence | |
| Manhattan | 17 (43%) |
| Manhattan-Harlem | 3 (7.5%) |
| Queens/Brooklyn/Bronx | 9 (22.5%) |
| Westchester/Long Island/Upstate | 6 (15%) |
| Connecticut/New Jersey | 5 (12.5%) |
Quantitative Feedback
Before the program, participants reported a range of diagnoses and health symptoms including pain (62.5%), cancer (45%) anxiety/depression (40%), cardiovascular/metabolic (32.5%), gastrointestinal (27.5%), stress (22.5%), osteopenia/osteoporosis (17.5%), insomnia (17.5%), fatigue (12.5%), asthma/bronchitis (12.5%) grief/Post Traumatic Stress Disorder (PTSD)/Eating Disorder (ED) (7.5%), (7.5%) cognition/memory (7.5%) Neuropathy and breathing issues were most frequently written in the “other” text box.
Post-program survey results suggested VQGSMA program addressed common symptoms including fatigue, insomnia, anxiety, stress, pain, weakness, and gastrointestinal symptoms. Hot flashes were the sole symptom of the 14 pre-program symptoms that was not reported to be addressed for any participants. Balance, which was not reported as a pre-program concern, was reported to be addressed by 55% post program with 27% reporting post-program improvement in balance. Neuropathy as a symptom was not included as an option in the pre-survey but written in by participants as pre-series symptom. Of note, neuropathy (27%) and balance (55%) were cited by participants to have been addressed by the VQGSMA and balance (27%) was cited by participants to have improved post-series. Participants also reported post-program improvements in loneliness/isolation [Table 3].
Table 3.
Patients’ Pre-program Symptoms/Health Concerns, and Whether They Were Addressed and Improved by the Program.
| Symptoms/Health Concerns | Pre-program, n = 27 | Post-program Addressed, n = 11 | Post Program Symptom Improvement, n = 11 |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Fatigue | 19 (70%) | 5 (45%) | 2 (18%) |
| Insomnia/sleep | 19 (70%) | 3 (27%) | 3 (27%) |
| Pain | 18 (67%) | 6 (55%) | 2 (18%) |
| Anxiety/fear | 15 (56%) | 4 (36%) | 3 (27%) |
| Stress/Irritability | 11 (41%) | 7 (64%) | 4 (36%) |
| Weakness | 11 (41%) | 3 (27%) | 1 (9%) |
| Gastrointestinal symptoms a | 10 (37%) | 3 (27%) | 1 (9%) |
| Depression/hopelessness | 8 (27%) | 3 (27%) | 2 (14%) |
| Other | 7 (26%) | 1 (9%) c | 0 (0%) |
| Hot flashes | 6 (22%) | 0 (0%) | 0 (0%) |
| Brain fog | 5 (19%) | 2 (18%) | 0 (0%) |
| Isolation/loneliness | 3 (11%) | 4 (36%) | 1 (9%) |
| Balance | 0 | 6 (55%) | 3 (27%) |
anausea/vomiting/constipation/diarrhea.
bParticipant text: neuropathy (2), issues breathing, overeating, migraine, odd breathing patterns, racing heart.
cParticipant text: Long COVID.
No patients (0%) reported “no symptoms” for pre-program, post-program, or post-program symptom improvement.
Although only VQGSMA was offered, when asked about their preferred mode of program delivery “What did you think about the format?”, 73% preferred remote (zoom), 27% preferred hybrid (remote + in person), none preferred in-person format (0%). All participants felt their goals for attending the series were met and would unequivocally recommend the program to others.
Qualitative Feedback
Pre-VGSMA, when asked “What are you hoping to learn/gain from this Qi Gong Group visit?” participants expressed a wide range of physical (chronic pain, breathing, balance, strength), mental (anxiety, depression, stress), cognitive (focus) and self-efficacy goals (self-knowledge, self-soothing, self-healing) (See Table 4). When asked “What health concerns or life issues are you hoping to address during this Qi Gong Shared Medical Visit series?”, responses included general health (post-surgery and for health maintenance), musculoskeletal (muscle, joint, flexibility), neurologic (migraine, balance, neuropathy, dizziness), pulmonary, gastrointestinal, metabolic, oncologic, and mental health (anxiety, stress, sadness, sleep, focus) (See Table 5)
Table 4.
What are You Hoping to Learn/Gain From This Qi Gong Group Visit?
| Themes | |
|---|---|
| Physical | Gain better functionality breathing |
| How to better deal with chronic illness physically | |
| Practices.to help with sedentary lifestyle doing work on computer all day. To know exercises I could get up and do every 45 minutes or whatever | |
| Less chronic pain overall, improvement in sleep, improvement in migraines, improvement in body aches and improvement in hot flashes | |
| Learn ways to move for healing | |
| Ways in which qigong might improve my physical health | |
| Ways to move subtle without making my pain and balance worse | |
| Relaxation, balance, strength training | |
| Better body movement | |
| Hoping to gain another source of working out to improve my physical well being | |
| This is my first exposure to qi gong. Hoping to learn more about it and how it might be helpful in managing my symptoms | |
| Mental | How to deal with chronic illness mentally |
| Practices I can use as healthy alternative to vices I go to when stressed… | |
| Improvements in anxiety and depression symptoms | |
| Learn ways to meditate | |
| Modalities to promote calmness | |
| To bring a bit of mindfulness to my everyday life | |
| Ways to self soothe | |
| Cognitive | How to stay in the moment, clear my mind, ground myself |
| Focus and better body movement | |
| Social | I enjoy being part of this community of fellow warriors |
| Self-efficacy | I am curious to discover practices I might use in the future |
| I am hoping to learn body movements/techniques that would help in my healing journey | |
| To deepen my practice of Qi Gong | |
| Self knowledge, self healing, and the power of qi |
Table 5.
What Health Concerns or Life Issues are You Hoping to Address During This Qi Gong Shared Medical Visit Series?
| General Health | Be Physically and Mentally Stronger |
| Improve physical strength and energy, balance my systems | |
| General mental/physical wellbeing (3) | |
| After back surgery looking to improve strength | |
| Movement | |
| Pulmonary | Assistance with breathing better |
| Breathing patterns are erratic and contribute to my anxiety and systemic medical issues | |
| Gastrointestinal | IBS issues |
| Musculoskeletal | Muscle and joint tension, core dysfunction, TMJ |
| Pain, aches, stiffness | |
| Gentle movement (range of motion) to help with arthritis | |
| Mechanical flaws from 5th lumbar and hip issues | |
| Improvement of strength and flexibility of spine/back after fusion surgery | |
| Better balance, some muscle innervation | |
| Neurologic | Decrease in dizziness |
| Neuropathy | |
| Balance | |
| Migraine, fatigue | |
| Oncologic | Hot flashes, fatigue from HR +breast cancer treatment |
| Breast cancer after chemo, radiation and surgery. Struggling with joint and muscle pain, osteopenia | |
| General health and wellness during and after treatments for breast cancer | |
| Metabolic | Improved self-awareness and weight reduction |
| Mental health | Chronic and acute stress and anxiety |
| Difficulty falling asleep, overreliance on supplements to sleep | |
| To help my sleep (2 responses) | |
| Mind/body connection for stress and pain | |
| Focus (2 responses) | |
| Stress (2 responses), anxiety (4 responses), sadness |
Post VQGSMA, participants reported incorporating QG into daily practice, exercising more regularly including Tai Chi and yoga, using more mindfulness modalities including QG in their daily routines, enrolling in weekly women’s QG class, adding breathing exercises, and engaging in meditative practices. (See Table 6)
Table 6.
What Positive Changes Have You Made in Your Life Since Starting the Program?
| I aspire to incorporate Qi Gong into my life and daily practice |
| Doing exercise more regularly including tai chi and yoga |
| Committed to adding qi gong workouts several times a week along with the other workouts that I am currently performing in order to keep my body in the best possible state it can be |
| I’ve incorporated more mindfulness modalities (including a qjgong practice) into my daily routine |
| Enrolled in a weekly women’s qigong class |
| I try to do the exercises daily (but not enough) but I do use the breathing technique a lot |
| I’ve incorporated qi gong, a new mind/body practice into my day. I had been doing meditation. I like how qi gong combines movement with a meditative like practice |
| I don’t know that I actually had anxiety/fear, or that those feelings have been mitigated, but I do feel more grounded, and able to summon that feeling more easily |
Participants appreciated the format of the class, the patience, pace, and teaching style of the instructors, ease of learning new skills, gentle quality of the exercises, ease of practicing at home with no equipment, and “learning a new mindfulness modality in community with people experiencing the same issues as I am.” Feedback and suggestions included interest in a next level class (advanced beginner class), introduction to other forms (sets) of qi gong, primer-type text or handouts with illustrations, access to videos earlier in the series, more full body movement, and longer sessions. The most common patterns from the content analysis of open-ended responses reported was the ease of learning and the quality of the instructor.
Feasibility
Program feasibility was demonstrated through high program participation rates and fidelity to QG exercises was based on observation of participants performing QG at the end of each program series. During the final sessions of each series, participants were observed as a group by the integrative medicine physician via telehealth as they performed the sequences twice without stopping. Participants who had no prior experience with QG reported being helped by the home videos provided by the instructor, practicing on non-VQGSMA days at home, and eventually practiced QG on their own every day. The QG instructor also noted that even those who had previous QG experience appeared to participate in the QG exercises more smoothly and independently by the end of the VQGSMA series.
Telehealth Implementation and Access
While nearly all patients had some type of chronic diagnosis, at least 1/3 were patients who had cancer and had recently undergone or were currently undergoing chemotherapy, radiation or surgery. The flexibility to access care made it easier for these immunocompromised individuals to participate. Those with limiting physical conditions also verbally expressed their appreciation for the ease and safety of “gathering” and building community through the virtual format. All participants were able to join via phone, iPad, computer, or television screen. While most joined from home, several joined from free internet hotspots.
Clinician Feedback
The integrative medicine physician-acupuncturist and QG-acupuncturist were present at every session. Clinicians were part of Integrative Health staff; therefore, no additional hiring of full-time employees was required. Both clinicians reported high levels of satisfaction with VQGSMA and found it to be a sustainable option from the clinician perspective.
Financial Sustainability
For our practice, with a payor mix of 40% Medicare, 60% Commercial insurance and medically complex patients, cost neutrality was attained if groups with 2 providers (MD and QG instructor) enrolled at least 8 participants. Our groups had an average of 11, with a range of 8-16. Physician used the common standard billing method of E/M codes 99212-99214. Of the 197 insurance billable patient visits over the 18 sessions offered over 6-month, there were no SMA specific insurance denials identified based on reports by the center’s executive director and practice manager. See Table 7 for details on revenue/cost forecasting.
Table 7.
Revenue/Cost Forecasting.
| Revenue | Cost | |||
|---|---|---|---|---|
| Estimated reimbursement | $120/patient | Provider cost | ||
| Average number of patients per session | 11 | MD | $240 | |
| Total revenue | $1320 | Qi gong | $60 | |
| Admin | $40 | |||
| Total | $340 |
MDs get 1 h for SMA and 1 h for charting per 5 attendees. Admin cost is $40 or 1 h for every 5 attendees.
Discussion
Despite the increasing popularity of SMAs as a means to improve health education, social support, access to care, and clinician well-being without increasing costs, there remain significant gaps in the literature regarding the integration of Complementary and Integrative Health (CIH) services into these models. While telehealth visits became routine during the pandemic and improved access for underserved patients with chronic conditions, few studies have assessed the feasibility and impact of virtual Qi Gong group visits on both patients and clinicians. This study aimed to assess the feasibility and acceptability of Virtual Qi Gong Shared Medical Appointments (VQGSMA) among a diverse demographic population with mixed diagnoses within an integrative medicine practice at an urban tertiary care academic medical center. Additionally, it sought to describe the potential impact on patient goals, clinician satisfaction, and institutional financial efficiency.
Our pilot study demonstrated that VQGSMA was feasible and acceptable to patients, clinicians, and institutions. The high weekly attendance rate, consistent individual attendance, and repeat attendance in subsequent series underscore the program’s feasibility, participant interest, and acceptability. Participants who completed the program surveys expressed favorable opinions, and clinicians reported high satisfaction. Financial projections indicate the model’s sustainability, with revenue from group visits exceeding that of individual consultations. Participants reported that VQGSMA effectively addressed both physical symptoms (such as fatigue, insomnia, pain, weakness, gastrointestinal symptoms, and neuropathy) and psychoemotional symptoms (such as anxiety, stress, and loneliness). Many participants reported implementing Qi Gong, breathwork, meditative practices, and other exercises into their daily lives, suggesting the potential for long-term behavioral change.
Building up on the literature supporting SMAs, mind-body therapies (predominantly yoga or meditation), and in-person vs remote delivery, this study is innovative by combining 3 factors into 1 intervention: qi gong, group visits, and remote delivery.
A key take-away from this study is the potential for improving clinical care and access while simultaneously improving provider satisfaction and instititutional efficiency. Through these innovative VQGSMAs, patients reported symptom relief and satisfaction with the integrative medicine care they received. At the same time, providers reported satisfaction with leading SMAs. The feasibility and cost-benefit to the institution through these insurance-covered VQGSMAs makes integrative care accessible and affordable, especially to vulnerable immunocompromised patients seeking to reduce exposure. While further research is needed, through the integrative care provided in SMAs, patients and institutions may benefit in the future through potentially lower need for pharmaceutical medications, emergency care utilization, surgeries, and ultimately health care system costs.
Another take-way is that billing and reimbursement for VQGSMAs need not be a barrier for implementation. Standard billing methods for physicians can be followed using Evaluation and Management codes (E/M) Current Procedural Terminology (CPT) 99212-99214 depending on medical complexity. These billing code options have been successfully used in other shared medical appointments51-53 (Freeman 2022, Loy, 2023). Institutional billing and coding experts can assist in optimizing reimbursement and sustainability of services.
Our findings are consistent with existing literature on in-person Qi Gong, which has demonstrated improvements in physical4-6 and psychoemotional9,12 symptoms. However, our study extends this knowledge by demonstrating the feasibility and benefits of a mixed-diagnosis population and telehealth delivery. Notably, telehealth delivery was not a deterrent, with all participants reporting their goals were met and none preferring an in-person format for future sessions. This preference for remote or hybrid delivery over in-person sessions aligns with trends observed during the pandemic, where telehealth significantly enhanced access to care.
Several limitations should be considered. The 28% response rate to the post-program survey suggests potential reporting bias, as those with positive experiences may have been more likely to respond. The sample may also overrepresent participants from higher-income households, although a significant number lived outside the city center. The study’s demographic skew towards older women, while consistent with broader trends in integrative medicine usage, limits generalizability to other populations. Furthermore, all participants were fluent in English, highlighting a need for future studies to include non-English speakers54-56 to enhance inclusivity. Technological issues, though not observed in this pilot, could pose potential limitations for future virtual Qi Gong instruction.
This pilot study highlights several avenues for future research. Well-controlled studies, 40 such as randomized controlled trials, comparing VQGSMA to in-person QGSMA are needed. Future research should examine long-term health outcomes, feasibility among more diverse populations, and the provision of other integrative health care modalities via telehealth. Additionally, examining outcomes such as increased knowledge, patient and staff satisfaction, clinical outcomes, financial data, office efficiency, and health care utilization will provide a more comprehensive understanding of the impact of the VQGSMA model. At our institution, our plan is to trial VQGSMA with an Nurse Practitioner and Qi Gong Instructor instructor as well as compare virtual and in-person QGSMA with the same 2 providers. We hope to expand beyond our main hospital to satellite community hospitals with higher minority populations.
In conclusion, VQGSMA was found to be feasible and acceptable among a diverse demographic population with mixed diagnoses within an integrative medicine practice at an urban tertiary care academic medical center. This innovative combination of SMA, telehealth, and Qi Gong offers increased access to integrative care for diverse, health-disparate populations, including patients with physical, immunocompromised, or socioeconomic limitations. Our findings suggest promising impacts on patient goals, clinician satisfaction, and institutional financial efficiency, laying the groundwork for future research and implementation efforts to expand and optimize this model of care.
Conclusion
Using a pre-post design, VQGSMA demonstrated feasibility and acceptability for delivery of QG via telehealth to a mixed demographic and mixed diagnoses population. Patients expressed satisfaction with the modality and the pilot suggested preliminary efficacy with respect to symptoms addressed, symptom improvement, and lifestyle changes. This novel VQGSMA was also acceptable to clinicians/institutions and feasible/sustainable regarding time and cost. VQGSMA among a mixed demographic is feasible, acceptable, sustainable, and cost effective to patients, clinicians, and institutions. Nevertheless, caution in interpreting the data is advised due to the low response rate of the post-program survey. Larger methodologically sound implementation trials within health care systems with more diverse populations and with longer follow-up periods are needed and recommended.
Supplemental Material
Supplemental Material for Exploring the Feasibility and Acceptability of Telehealth Qi Gong Shared Medical Appointments: A Novel Approach to Expand Access by Michelle H. Loy, and Tim Fatato in Global Advances in Integrative Medicine and Health
Acknowledgements
We wish to recognize all the patients who participated in VQGSMA and provided evaluation data for this report. We also wish to acknowledge Mary Acosta for her administrative support and Chiti Parikh MD for her leadership support. We wish to thank Melanie A. Gold, DO, DMQ, DABMA and Kathi J. Kemper, MD, MPH for their substantive reviews of the manuscript.
Author Contributions: Dr L. conceptualized and designed the study, coordinated, and supervised data collection, collected data, conducted the initial analysis, drafted the initial manuscript, reviewed, and revised the manuscript. T.F. provided Qi Gong instruction and reviewed the manuscript. All authors approve the manuscript as submitted and agree to be accountable for all aspects of the work.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Institutional Review Board Statement: The academic medical center’s Institutional Review Board (IRB) determined on 31 January 2023 (#23-01 025 565) that this activity is not considered research involving human subjects due to its anonymous, program evaluation nature and that further IRB review and approval is not required.
Supplemental Material: Supplemental material for this article is available online.
ORCID iD
Michelle H. Loy https://orcid.org/0000-0002-9935-6888
Data Availability Statement
Data used in this program evaluation will be made available upon request.
References
- 1.Wang C, Li K, Gaylord A S. Trends and characteristics of tai chi and qi gong use among U.S. Adults: results from the 2007–2017 national health interview survey. Complement Ther Med. 2022;71:102890. doi: 10.1016/j.ctim.2022.102890 [DOI] [PubMed] [Google Scholar]
- 2.Zeng Y, Xie X, Cheng ASK. Qigong or tai chi in cancer care: an updated systematic review and meta-analysis. Curr Oncol Rep. 2019;21(6):48. doi: 10.1007/s11912-019-0786-2 [DOI] [PubMed] [Google Scholar]
- 3.Gong X, Rong G, Wang Z, Zhang A, Li X, Wang L. Baduanjin exercise for patients with breast cancer: a systematic review and meta-analysis. Complement Ther Med. 2022;71:102886. doi: 10.1016/j.ctim.2022.102886 [DOI] [PubMed] [Google Scholar]
- 4.Wayne PM, Lee MS, Novakowski J, et al. Tai Chi and Qigong for cancer-related symptoms and quality of life: a systematic review and meta-analysis. J Cancer Surviv. 2018;12(2):256-267. doi: 10.1007/s11764-017-0665-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen Z, Meng Z, Milbury K, et al. Qigong improves quality of life in women undergoing radiotherapy for breast cancer: results of a randomized controlled trial. Cancer. 2013;119(9):1690-1698. doi: 10.1002/cncr.27904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ko L-H, Hsieh Y-J, Wang M-Y, Hou W-H, Tsai P-S. Effects of health qigong on sleep quality: a systematic review and meta-analysis of randomized controlled trials. Complement Ther Med. 2022;71:102876. doi: 10.1016/j.ctim.2022.102876 [DOI] [PubMed] [Google Scholar]
- 7.Elinoff V, Lynn SJ, Ochiai H, Hallquist M. The efficacy of Kiko exercises on the prevention of migraine headaches: a pilot study. Am J Chin Med. 2009;37(3):459-470. doi: 10.1142/s0192415x09006977 [DOI] [PubMed] [Google Scholar]
- 8.Yeh SC, Chang MY. The effect of Qigong on menopausal symptoms and quality of sleep for perimenopausal women: a preliminary observational study. J Altern Complement Med. 2012;18(6):567-575. doi: 10.1089/acm.2011.0133 [DOI] [PubMed] [Google Scholar]
- 9.Carcelén-Fraile MDC, Aibar-Almazán A, Martínez-Amat A, et al. Qigong for mental health and sleep quality in postmenopausal women: a randomized controlled trial. Medicine (Baltim). 2022;101(39):e30897. doi: 10.1097/md.0000000000030897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kurt Z, Sice P, Krajewska K, et al. A pilot study on the impacts of lung-strengthening Qigong on wellbeing. Complement Ther Med. 2022;71:102891. doi: 10.1016/j.ctim.2022.102891 [DOI] [PubMed] [Google Scholar]
- 11.Qi Gong NCCIH. What you need to know. https://www.nccih.nih.gov/health/qigong-what-you-need-to-know. Accessed 3/24/23, 2023.
- 12.Zhang YP, Hu RX, Han M, et al. Evidence base of clinical studies on qi gong: a bibliometric analysis. Complement Ther Med. 2020;50:102392. doi: 10.1016/j.ctim.2020.102392 [DOI] [PubMed] [Google Scholar]
- 13.Li R, Chen H, Feng J, et al. Effectiveness of traditional Chinese exercise for symptoms of knee osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Int J Environ Res Public Health. 2020;17(21):7873. doi: 10.3390/ijerph17217873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li X, Si H, Chen Y, Li S, Yin N, Wang Z. Effects of fitness qigong and tai chi on middle-aged and elderly patients with type 2 diabetes mellitus. PLoS One. 2020;15(12):e0243989. doi: 10.1371/journal.pone.0243989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deuel LM, Seeberger LC. Complementary therapies in Parkinson disease: a review of acupuncture, tai chi, qi gong, yoga, and cannabis. Neurotherapeutics. 2020;17(4):1434-1455. doi: 10.1007/s13311-020-00900-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Janevic MR, McLaughlin SJ, Heapy AA, Thacker C, Piette JD. Racial and socioeconomic disparities in disabling chronic pain: findings from the health and retirement study. J Pain. 2017;18(12):1459-1467. doi: 10.1016/j.jpain.2017.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Osborn R, Squires D, Doty MM, Sarnak DO, Schneider EC. In new survey of eleven countries, US adults still struggle with access to and affordability of health care. Health Aff. 2016;35(12):2327-2336. doi: 10.1377/hlthaff.2016.1088 [DOI] [PubMed] [Google Scholar]
- 18.Olayiwola JN, Willard-Grace R, Dubé K, et al. Higher perceived clinic capacity to address patients' social needs associated with lower burnout in primary care providers. J Health Care Poor Underserved. 2018;29(1):415-429. doi: 10.1353/hpu.2018.0028 [DOI] [PubMed] [Google Scholar]
- 19.Roth I, Thompson-Lastad A, Thomas AU. The quadruple aim as a framework for integrative group medical visits. J Altern Complement Med. 2020;26(4):261-264. doi: 10.1089/acm.2019.0425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bari S, Chineke I, Darwin A, et al. Awareness, use and outlook of complementary and alternative medicine (CAM) options in an underserved, uninsured minority cancer patient population. Integr Cancer Ther. 2021;20:15347354211051622. doi: 10.1177/15347354211051622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nahin RL, Barnes PM, Stussman BJ. Insurance coverage for complementary health approaches among adult users: United States, 2002 and 2012. NCHS Data Brief. 2016;235:1-8. [PubMed] [Google Scholar]
- 22.Sidorsky T, Huang Z, Dinulos JG. A business case for shared medical appointments in dermatology: improving access and the bottom line. Arch Dermatol. 2010;146(4):374-381. doi: 10.1001/archdermatol.2010.32 [DOI] [PubMed] [Google Scholar]
- 23.Thompson-Lastad A, Gardiner P, Chao MT. Integrative group medical visits: a national scoping survey of safety-net clinics. Health equity. 2019;3(1):1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haun JN, Paykel J, Alman AC, Patel N, Melillo C. A complementary and integrative health group-based program pilot demonstrates positive health outcomes with female Veterans. Explore. 2020;16(2):85-89. doi: 10.1016/j.explore.2019.08.001 [DOI] [PubMed] [Google Scholar]
- 25.Thompson-Lastad A, Gardiner P. Group medical visits and clinician wellbeing. Glob Adv Health Med. 2020;9:2164956120973979. doi: 10.1177/2164956120973979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Charlot M, D'Amico S, Luo M, Gemei A, Kathuria H, Gardiner P. Feasibility and acceptability of mindfulness-based group visits for smoking cessation in low-socioeconomic status and minority smokers with cancer. J Altern Complement Med. 2019;25(7):762-769. doi: 10.1089/acm.2019.0016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gareau S, Lòpez-De Fede A, Loudermilk BL, et al. Group prenatal care results in medicaid savings with better outcomes: a propensity score analysis of CenteringPregnancy participation in South Carolina. Matern Child Health J. 2016;20(7):1384-1393. doi: 10.1007/s10995-016-1935-y [DOI] [PubMed] [Google Scholar]
- 28.Wan W, Staab EM, Ham SA, et al. Economic evaluation of group medical visits for adults with diabetes in community health centers. Diabetes. 2018;67(Supplement_1):8. doi: 10.2337/db18-8-OR [DOI] [Google Scholar]
- 29.Hirsch JD, Bounthavong M, Arjmand A, et al. Estimated cost-effectiveness, cost benefit, and risk reduction associated with an endocrinologist-pharmacist diabetes intense medical management “Tune-Up” clinic. J Manag Care Spec Pharm. 2017;23(3):318-326. doi: 10.18553/jmcp.2017.23.3.318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Loy M. Shared medical appointments (SMAs) at an academic institution: an engaging, effective, efficient educational model benefitting patients and clinicians. 2023. [Google Scholar]
- 31.Geller J. Loneliness and how group viists help people heal. Alternative and Complementary Thearpies 2020;26(2):53-56. [Google Scholar]
- 32.Dodds M, Nicholson L, Muse B, 3rd, Osborn LM. Group health supervision visits more effective than individual visits in delivering health care information. Pediatrics. 1993;91(3):668-670. [PubMed] [Google Scholar]
- 33.Bronson DL, Maxwell RA. Shared medical appointments: increasing patient access without increasing physician hours. Cleve Clin J Med. 2004;71(5):369-370. doi: 10.3949/ccjm.71.5.369 [DOI] [PubMed] [Google Scholar]
- 34.Heyworth L, Rozenblum R, Burgess JF, Jr., et al. Influence of shared medical appointments on patient satisfaction: a retrospective 3-year study. Ann Fam Med. 2014;12(4):324-330. doi: 10.1370/afm.1660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Patel TA, Johnston CA, Cardenas VJ, Vaughan EM. Utilizing telemedicine for group visit provider encounters: a feasibility and acceptability study. Int J Diabetes Metab Syndr. 2020;1(1):1-6. [PMC free article] [PubMed] [Google Scholar]
- 36.Patel P. Successful use of virtual shared medical appointments for a lifestyle-based diabetes reversal program. Am J Lifestyle Med. 2021;15(5):506-509. doi: 10.1177/15598276211008396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Patel KB, Turner K, Alishahi Tabriz A, et al. Estimated indirect cost savings of using telehealth among nonelderly patients with cancer. JAMA Netw Open. 2023;6(1):e2250211. doi: 10.1001/jamanetworkopen.2022.50211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ernstzen D, Keet J, Louw K-A, et al. “So, you must understand that that group changed everything”: perspectives on a telehealth group intervention for individuals with chronic pain. BMC Musculoskelet Disord. 2022;23(1):538. doi: 10.1186/s12891-022-05467-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.NCI N. NCI telehealth research centers of excellence (TRACE). Accessed 4/2/23, 2023.https://healthcaredelivery.cancer.gov/telehealth/trace.html
- 40.Niles BL, Grossman S, McQuade M, et al. Study protocol for a revised randomized trial: remotely delivered Tai Chi and wellness for Gulf War illness. Contemp Clin Trials. 2023;125:107045. doi: 10.1016/j.cct.2022.107045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Teresi JA, Yu X, Stewart AL, Hays RD. Guidelines for designing and evaluating feasibility pilot studies. Med Care. 2022;60(1):95-103. doi: 10.1097/mlr.0000000000001664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rosenberg M. How Qigong and Tai Chi Benefit the Body and Mind an integrative medicine physician describes the health benefits and explains the difference between these ancient mind-body practices. 2023. https://healthmatters.nyp.org/how-qigong-and-tai-chi-benefit-the-body-and-mind/. Accessed 07/31/23, 2023.
- 43.Gardiner P, Lestoquoy AS, Gergen-Barnett K, et al. Design of the integrative medical group visits randomized control trial for underserved patients with chronic pain and depression. Contemp Clin Trials. 2017;54:25-35. doi: 10.1016/j.cct.2016.12.013 [DOI] [PubMed] [Google Scholar]
- 44.Roth I, Tiedt M, Miller V, et al. Integrative medical group visits for patients with chronic pain: results of a pilot single-site hybrid implementation-effectiveness feasibility study. Front Pain Res (Lausanne). 2023;4:1147588. doi: 10.3389/fpain.2023.1147588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Guo Y, Xu M, Wei Z, et al. Beneficial effects of qigong wuqinxi in the improvement of health condition, prevention, and treatment of chronic diseases: evidence from a systematic review. Evid Based Complement Alternat Med. 2018;2018:3235950. doi: 10.1155/2018/3235950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Avijgan M, Avijgan M. Meraque or triple energizer (san Jiao): actual or virtual organ in traditional medicine - a hypothetical viewpoint. Integr Med Int. 2015;2(1-2):9-20. doi: 10.1159/000433537 [DOI] [Google Scholar]
- 47.Kuei S. Beginning qigong: Chinese secrets for health and longevity. Among the most popular of themThe Eight Brocade Exercises. North Clarendon: Tuttle Publshing; 2011. [Google Scholar]
- 48.Yang J-M. Eight Simple Qigong Exercises for Health: The Eight Pieces of Brocade. Wolfeboro: YMAA Publication Center; 2000. [Google Scholar]
- 49.Berg BL, Lune H. Qualitative Research Methods for the Social Sciences. 8th ed. United States: Pearson Education, Inc.; 2012. [Google Scholar]
- 50.Bengtsson M. How to plan and perform a qualitative study using content analysis. NursingPlus Open. 2016;2:8-14. doi: 10.1016/j.npls.2016.01.001 [DOI] [Google Scholar]
- 51.Loy MH, Prisco L, Parikh C. Implementation of virtual integrative oncology shared medical appointment series (VIOSMAS) within mixed diagnosis population. Integr Cancer Ther. 2024;23:15347354231223969. doi: 10.1177/15347354231223969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Freeman K, Bidwell J. Lifestyle medicine: shared medical appointments. J Fam Pract. 2022;71(Suppl 1 Lifestyle):S62-S65. doi: 10.12788/jfp.0278 [DOI] [PubMed] [Google Scholar]
- 53.Lacagnina S, Tips J, Pauly K, Cara K, Karlsen M. Lifestyle medicine shared medical appointments. Am J Lifestyle Med. 2021;15(1):23-27. doi: 10.1177/1559827620943819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cornelio-Flores O, Lestoquoy AS, Abdallah S, et al. The latino integrative medical group visit as a model for pain reduction in underserved Spanish speakers. J Altern Complement Med. 2018;24(2):125-131. doi: 10.1089/acm.2017.0132 [DOI] [PubMed] [Google Scholar]
- 55.Abbott RB, Hui KK, Hays RD, et al. Medical student attitudes toward complementary, alternative and integrative medicine. Evid Based Complement Alternat Med. 2011;2011:985243. doi: 10.1093/ecam/nep195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Culhane-Pera K, Peterson KA, Crain AL, et al. Group visits for Hmong adults with type 2 diabetes mellitus: a pre-post analysis. J Health Care Poor Underserved. 2005;16(2):315-327. doi: 10.1353/hpu.2005.0030 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Exploring the Feasibility and Acceptability of Telehealth Qi Gong Shared Medical Appointments: A Novel Approach to Expand Access by Michelle H. Loy, and Tim Fatato in Global Advances in Integrative Medicine and Health
Data Availability Statement
Data used in this program evaluation will be made available upon request.