Abstract
Introduction
With the introduction of novel treatment options for benign prostatic hyperplasia (BPH), decision making regarding surgical management has become ever more complex. Factors such as clinical exposure, equipment availability, patient characteristics and hospital setting may affect what treatment is offered and an informed patient choice. The aim of this study was to investigate how urologists help patients make decisions regarding BPH management and whether their practice would differ if they were the patient themselves.
Material and methods
A 52-question survey presenting hypothetical clinical scenarios was distributed to European urologists and trainees/residents online and in person. In each scenario, regarding treatment options for BPH, the participant considered themselves firstly as the treating clinician and secondly as the patient themselves. Details regarding the participants’ clinical experience, awareness of treatment options and exposure to these options were obtained.
Results
There were 139 participants; 69.8% of whom were consultants, with 82.1% of participants having practiced urology for more than 5 years. A total of 59.7% of urologists consider themselves BPH specialists. Furthermore, 93.5% of those surveyed had performed transurethral resection of the prostate (TURP), whilst procedures performed the least by participants were minimally invasive surgical therapy (MIST) options. Only 17.3% had seen and 1.4% had performed all of the treatment options. When considering themselves as a patient within standard practice, there was a preference for HoLEP amongst participants.
Conclusions
The majority of urologists surveyed had minimal experience to newer BPH techniques and MIST, suggesting that more exposure is required. A higher rate of HoLEP was chosen as a treatment option for urologists themselves as a patient than what they would choose as an option for their patients.
Keywords: lower urinary tract symptoms, benign prostatic hyperplasia, laser, rezum, urolift, TURP
INTRODUCTION
Benign prostatic hyperplasia (BPH) refers to the non-malignant growth of prostatic tissue that is associated with ageing. Studies suggest that up to 50% of men over the age of 50 and up to 80–90% of men over the age of 70 [1] suffer from BPH. The estimated prevalence of BPH globally increased from 51.1 million in 2000 to 94.0 million in 2019 [2]. As the development of lower urinary tract symptoms (LUTS) secondary to BPH is associated with increasing age, the prevalence of associated LUTS is increasing in our communities.
Whilst conservative management and medical therapies tend to be first-line options for the management of BPH, a number of patients may experience adverse effects or continue to suffer from refractory symptoms, thus selecting surgical intervention. With the increasing number of novel and minimally invasive treatments options (MISTs) for BPH being introduced to our practice, decision making regarding surgical management has become more complex.
The aim of this study was to investigate urologists’ awareness of and experience in different surgical techniques used for managing BPH. Furthermore, we aimed to evaluate the management choices for treatment of BPH when provided with different patient clinical scenarios and to assess whether or not their practice would differ if they were to consider themselves as the patients in the same clinical scenarios.
MATERIAL AND METHODS
A 52-question survey was designed by the research team consisting of both trainee and consultant urologists from the UK and EU. This survey was purposely distributed to potential participants online and in person. It was distributed via several European Association of Urology (EAU) subsections and a large UK Endourology group. The distribution method was via email and in person to the EAU section of Uro-technology (ESUT) group, through WhatsApp endourology group in UK, and EAU groups including European Urology Residents Education Programme (EUREP) and young endourology groups (YAU).
The survey consisted of 4 sections. The 1st Section consisted of questions regarding demographic details of urologists surveyed.
The 2nd Section comprised of questions aimed at assessing the participant’s awareness of, exposure to, and experience in using different treatment options for BPH. Information regarding participants’ routine investigations prior to surgery were obtained in this section; for example, whether they would use urodynamics in their assessment for BPH and LUTS, or whether they would measure prostate volume or prostate-specific antigen (PSA) prior to offering a surgical procedure.
The 3rd Section presented a hypothetical situation to participants, in which they were asked to choose which surgical treatment option for BPH they would perform on a hypothetical scenario of a ‘typical patient’ – a 65-year-old male with symptomatic BPH who has previously tried conservative and medical management. Participants were asked to answer 16 questions as the patient’s treating clinician, with each question presenting a different patient scenario which may alter participants’ choice of treatment option.
The 4th Section asked participants to answer the same hypothetical scenario questions as presented in Section 3, but to consider themselves as the patient in each scenario, rather than as a clinician.
The scenarios presented in Section 3 and 4, whereby the participants act as the treating clinician in Section 3 and as the patient themselves in Section 4 assessed what treatment options participants would choose in the following situations:
Scenarios included in the survey
Their standard BPH Procedure
Prostate volume was between 30 and 80 cc
Prostate volume was over 80 cc
High post-void residual volume (150 ml)
Sexual function was deemed very important
Sexual function not deemed important
Patient had previously had a TURP
Patient had Group 1 prostate cancer on surveillance
Patient had acute urinary retention with indwelling catheter
Patient had chronic urinary retention with indwelling catheter
Patient suffers from recurrent urinary tract infections
Patient takes anticoagulation medication that cannot be stopped
Patient is not fit for general or spinal anaesthesia
Patient has refractory haematuria due to BPH
Patient does not have insurance and can only afford a single self-pay procedure
Patient is insured and not concerned about cost
Treatments included as answer choices in the survey included: monopolar TURP (mTURP), bipolar TURP (bTURP), Holmium laser enucleation of the prostate (HoLEP), other anatomical endoscopic enucleation of the prostate (AEEP), Rezum water therapy (Rezum), prostatic urethral lift (PUL), prostatic artery embolisation (PAE), Greenlight laser photoselective vapourisation of the prostate (GLL PVP), Aquablation and temporarily implanted nitinol device (iTIND).
Statistical Analysis
Analysis was performed regarding demographics and answers to the two scenarios. Data was collected using Microsoft Excel 2016 (Microsoft, Redmond, WA, USA). Statistical analysis was performed with SPSS version 26 (IBM, Armonk, NY, USA). The independent t-test, Mann–Whitney-U test and Chi-squared test were used, with a p-value of <0.05 as significant.
RESULTS
There were a total of 139 participants. Of these, 97 (69.78%) were consultants, with the remaining 42 (30.22%) being trainees/residents. Demographic information is shown in Table 1. Twenty-five participants (17.99%) had practiced urology for 5 years or less and the majority of participants (71.22%) were working mainly in a University/Teaching Hospital. Of those surveyed, 83 (59.71%) considered themselves to be BPH specialists; with 68.04% of these specialists being consultants. Out of 113 participants for whom this question was applicable; 20 (14.39%) had experienced LUTS secondary to BPH.
Table 1.
Demographic Information on Participants
| Surgical Level Consultant Resident/Trainee |
97 (69.8%) 42 (30.2%) |
| Length of Urology Experience (%) 0–5 Years 6–10 Years 11–15 Years 16–20 Years 21–25 Years 26–30 Years 30+ Years |
25 (18.0%) 30 (21.6%) 31 (22.3%) 24 (17.3%) 17 (12.2%) 8 (5.8%) 4 (2.9%) |
| Institution (%) University/Teaching Hospital Public Hospital Private Hospital |
99 (71.2%) 28 (20.1%) 12 (8.6%) |
| Subspecialty within Urology (%) Andrology & Infertility Endourology – BPH Endourology – Stone Disease Female, Functional & Neuro-Urology Paediatric Urology Reconstructive Urology Transplantation Uro-Oncology General Urology |
15 (10.8%) 83 (59.7%) 87 (62.6%) 15 (10.8%) 12 (8.6%) 13 (9.4%) 8 (5.8%) 62 (44.6%) 78 (56.1%) |
BPH – benign prostatic hyperplasia
Of the treatment options presented; only 88 (63.31%) of participants had heard of all of the treatment choices and only 17.27% of participants had seen all of the treatments performed. The vast majority of participants had both seen mTURP (87.77%) and bTURP (89.21%) as well as performed mTURP (87.77%) and bTURP (92.81%) in their surgical practice. Two (1.44%) participants had performed all of the treatment options in their surgical practice, whilst 3 participants (2.16%) had not performed any. Information regarding participant exposure to and utilisation of treatment options in their surgical practice is shown in Table 2. Significantly lower numbers of participants had seen MIST options or performed them in their surgical practice. Of the MIST options provided; the procedures most commonly seen and performed in surgical practice included Rezum (seen by 58.99% and performed by 35.25%) and GLL PVP (seen by 58.72% and perforned by 35.97%). In comparison, the MIST options least seen and performed in surgical practice were Aquablation (seen by 27.34% and performed by 7.91%) and iTIND (seen by 15.83% and performed by 5.04%)
Table 2.
Information Regarding Participant Exposure to and Utilisation of Treatment Options in Their Surgical Practice
| Treatment Option | Percentage that had seen Treatment Option (%) | Percentage that had performed Treatment Option in Surgical Practice (%) |
|---|---|---|
| mTURP | 87.77% | 87.77% |
| bTURP | 89.21% | 92.81% |
| HoLEP | 71.94% | 53.24% |
| AEEP | 32.37% | 23.02% |
| Rezum | 58.99% | 35.25% |
| PUL | 51.80% | 23.74% |
| PAE | 43.88% | 27.34% |
| GLL PVP | 58.72% | 35.97% |
| Aquablation | 27.34% | 7.91% |
| iTIND | 15.83% | 5.04% |
| All of the above | 17.27% | 1.44% |
| None of the above | 0.00% | 2.16% |
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
The most commonly performed procedures to have been carried out by participants at least once were mTURP (93.53%) and bTURP (93.53%), followed by HoLEP and GLL PVP (54.68% and 44.60%, respectively). Information regarding the number of times participants have performed each of the procedure options is shown in Table 3.
Table 3.
Information Regarding Number of Times Participants have Performed Each Procedure
| Treatment Option | Never Performed (%) | Performed <20 times (%) | Performed 21–50 times (%) | Performed 51–100 times (%) | Performed >100 times (%) |
|---|---|---|---|---|---|
| mTURP | 6.47% | 15.83% | 17.27% | 11.51% | 48.92% |
| bTURP | 6.47% | 10.79% | 16.55% | 14.39% | 51.80% |
| HoLEP | 45.32% | 24.46% | 10.79% | 1.44% | 17.99% |
| AEEP | 69.06% | 10.07% | 5.04% | 1.44% | 14.39% |
| Rezum | 60.43% | 24.46% | 8.63% | 4.32% | 2.16% |
| PUL | 69.78% | 23.74% | 4.32% | 2.16% | 0.00% |
| PAE | 77.70% | 15.11% | 3.60% | 2.16% | 1.44% |
| GLL PVP | 55.40% | 20.86% | 8.63% | 4.32% | 10.79% |
| Aquablation | 90.65% | 5.76% | 0.00% | 0.72% | 2.88% |
| iTIND | 93.53% | 5.04% | 1.44% | 0.00% | 0.00% |
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
When asked which investigations they would carry out routinely prior to operating (Figure 1), a vast majority carried out a flow rate and residual volume (97%), as well as a rectal prostate examination (94%) and a PSA test (89%). However, only 114 participants (82%) would routinely assess prostate volume measurement prior to operating. Compared to 95% of participants assessing International Prostate Symptom Score (IPSS), only 37% would routinely assess International Index of Erectile Function (IIEF-5) Score.
Figure 1.
Investigations that participants would routinely organise for the hypothetical patient.
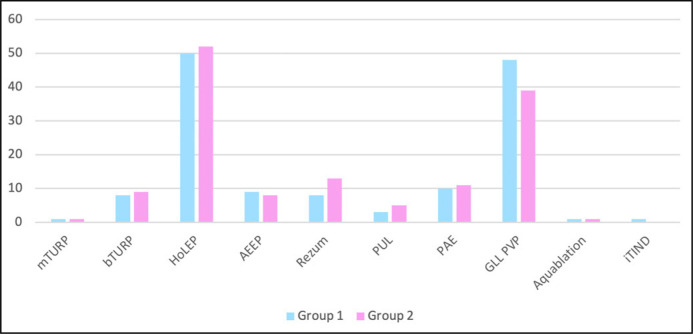
Differences were noted in some of the participants’ preferred treatment selections in the hypothetical situations presented; whereby the participants answered as the treating clinician and as the patient themselves. The overall preferred ‘Standard BPH Procedure’ was bTURP in both situations, when participants considered themselves to be either the clinician or the patient (Figure 2 and Table 4). However, there was a statistically significant increase in preference for HoLEP when participants considered themselves to be the patient (25 vs 40, p = 0.016).
Figure 2.
Q1 – participants standard BPH procedure.
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
Table 4.
Question 1 – Participants’ Standard BPH Procedure Selections
| mTURP | bTURP | HoLEP | AEEP | Rezum | PUL | PAE | GLL PVP | Aquablation | iTIND | |
|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 | 9 | 71 | 25 | 14 | 10 | 2 | 0 | 8 | 0 | 0 |
| Group 2 | 6 | 60 | 40 | 9 | 15 | 3 | 0 | 5 | 1 | 0 |
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
Whilst the majority of participants would have chosen bTURP for their patients if the prostate was between 30 and 80 cc, fewer would have chosen this option for themselves, which was statistically significant (77 vs 60, p = 0.02). More participants were inclined to choose HoLEP and Rezum for themselves (18 as the treating clinician and 27 as patient themselves for both HoLEP and Rezum), however this was not statistically significant (p = 0.07). Results are shown in Figure 3 and Table 5.
Figure 3.
Q2 – participants selection for prostate volume 30–80cc.
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
Table 5.
Question 2 – Participants’ Selections if Prostate Volume Between 30–80 cc
| mTURP | bTURP | HoLEP | AEEP | Rezum | PUL | PAE | GLL PVP | Aquablation | iTIND | |
|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 | 8 | 77 | 18 | 10 | 18 | 1 | 0 | 6 | 1 | 0 |
| Group 2 | 6 | 60 | 27 | 9 | 27 | 3 | 0 | 6 | 1 | 0 |
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
When participants were asked which procedure they would choose if prostate volume was over 80 cc, results were comparable whether the participant was responding as the treating clinician or as patient themselves (Table 6). The most popular choice in both groups was HoLEP (85 as the treating clinician and 91 as patient themselves), with bTURP being the next most common answer; chosen by approximately 15% of the participants.
Table 6.
Question 3 – Participants’ Selections if Prostate Volume >80cc
| mTURP | bTURP | HoLEP | AEEP | Rezum | PUL | PAE | GLL PVP | Aquablation | iTIND | |
|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 | 4 | 22 | 85 | 18 | 2 | 0 | 1 | 7 | 0 | 0 |
| Group 2 | 2 | 21 | 91 | 16 | 3 | 0 | 1 | 5 | 0 | 0 |
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
When asked which options they would choose for a high post-void residual of 150 ml (Table 7 and Figure 4), a statistically significant number of participants would choose HoLEP for themselves rather than for their patients (49 participants responding as the treating clinician vs 70 as the patient themselves, p = 0.005). In keeping with this result, more participants would choose mTURP/bTURP for their patients (combined total of 61 responses) rather than for themselves (combined total of 41 responses) (p = 0.006).
Table 7.
Question 4 – Participants’ Selections if Patient has High Post-Void Residual Volume (150 ml)
| mTURP | bTURP | HoLEP | AEEP | Rezum | PUL | PAE | GLL PVP | Aquablation | iTIND | |
|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 | 7 | 54 | 49 | 15 | 4 | 1 | 0 | 8 | 1 | 0 |
| Group 2 | 3 | 38 | 70 | 14 | 6 | 1 | 0 | 7 | 0 | 0 |
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
Figure 4.
Q4 – participants selection if high PVR (>150 ml).
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
Where sexual function was deemed important (Table 8); the options selected by participants were comparable in both groups with the majority of participants choosing MIST options. Most notably, Rezum was the most commonly chosen option (56 participants as the treating clinician and 52 as patient themselves), followed by PUL. Whilst more participants were likely to choose invasive options for themselves in this scenario rather than for their patient, such as bTURP and HoLEP; this was not statistically significant.
Table 8.
Question 5 – Participants’ Selections if Sexual Function is Very Important
| mTURP | bTURP | HoLEP | AEEP | Rezum | PUL | PAE | GLL PVP | Aquablation | iTIND | |
|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 | 4 | 8 | 10 | 5 | 56 | 32 | 10 | 6 | 4 | 4 |
| Group 2 | 1 | 14 | 18 | 6 | 52 | 27 | 8 | 4 | 4 | 5 |
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
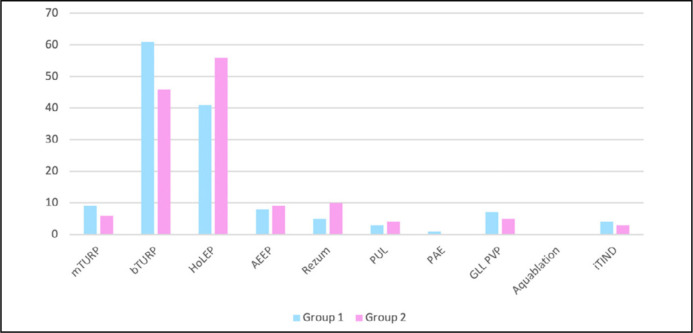
In the scenario whereby sexual function was not deemed important (Table 9 and Figure 5); the most commonly chosen option when participants were acting as the treating clinician was bTURP (52.5%). However, when considering themselves as the patient, the most common answer was HoLEP; 41.7% versus 35.3% who would choose bTURP for themselves. MIST options were less popular with only 8 participants choosing a MIST when responding as the clinician, and 13 choosing a MIST when responding as patient themselves.
Table 9.
Question 6 – Participants’ Selections if Sexual Function is Not Important
| mTURP | bTURP | HoLEP | AEEP | Rezum | PUL | PAE | GLL PVP | Aquablation | iTIND | |
|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 | 11 | 73 | 37 | 10 | 1 | 1 | 0 | 6 | 0 | 0 |
| Group 2 | 7 | 49 | 58 | 12 | 3 | 3 | 0 | 6 | 1 | 0 |
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
Figure 5.
Q6 – participants selections if sexual function was not important.
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
There was a statistically significant difference in those who would choose HoLEP for their patients and those who would choose it for themselves if sexual function was not deemed important (37 vs 58, p = 0.004). Likewise, there was a statistically significant difference in those who would choose bTURP for their patients versus those who would choose it for themselves in this scenario (73 vs 49, p = 0.002).
A high concordance rate for treatment options was noted when participants were asked to choose treatment options if the patient had previously undergone TURP (Table 10) or if the patient was noted to suffer from prostate cancer on surveillance (Table 11). In both scenarios, invasive options were most popular with bTURP being the most common answer followed by HoLEP.
Table 10.
Question 7 – Participants’ Selections if Patient has Previously had a TURP
| mTURP | bTURP | HoLEP | AEEP | Rezum | PUL | PAE | GLL PVP | Aquablation | iTIND | |
|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 | 9 | 63 | 45 | 10 | 2 | 0 | 1 | 7 | 1 | 1 |
| Group 2 | 6 | 60 | 51 | 11 | 3 | 0 | 1 | 7 | 0 | 0 |
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
Table 11.
Question 8 – Participants’ Selections if Patient Suffers from Grade 1 Prostate Cancer on Surveillance
| mTURP | bTURP | HoLEP | AEEP | Rezum | PUL | PAE | GLL PVP | Aquablation | iTIND | |
|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 | 8 | 77 | 39 | 9 | 2 | 1 | 0 | 3 | 0 | 0 |
| Group 2 | 7 | 71 | 39 | 11 | 6 | 1 | 1 | 3 | 0 | 0 |
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
When presented with the scenario whereby the patient had suffered from acute urinary retention and had an indwelling catheter in situ (Table 12); participants were more likely to choose bTURP when responding as the treating clinician (59 responses) and HoLEP when responding as patient themselves (56 responses). In total, only 11 participants (7.9%) would have chosen a MIST for their patients and 10 participants (7.2%) would have chosen a MIST for themselves. The most commonly chosen MIST was Greenlight laser photoselective vapourisation of the prostate (9 as the treating clinician vs 7 as patient themselves).
Table 12.
Question 9 – Participants’ Selections if Acute Urinary Retention with Indwelling Catheter
| mTURP | bTURP | HoLEP | AEEP | Rezum | PUL | PAE | GLL PVP | Aquablation | iTIND | |
|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 | 7 | 59 | 50 | 12 | 1 | 0 | 0 | 9 | 1 | 0 |
| Group 2 | 5 | 51 | 56 | 14 | 3 | 1 | 0 | 7 | 1 | 1 |
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
Similarly, when presented with the scenario whereby the patient had suffered from chronic urinary retention and had an indwelling catheter in situ (Table 13), the same number of participants would choose bTURP or HoLEP (54) for their patients when responding as the clinician, whereas more would choose HoLEP when responding as patient themselves (46 choosing bTURP and 59 choosing HoLEP). Ten participants (7.2%) would choose a MIST as the treating clinician and 12 (8.6%) would choose a MIST when responding as patient themselves.
Table 13.
Question 10 – Participants’ Selections if Chronic Urinary Retention with Indwelling Catheter
| mTURP | bTURP | HoLEP | AEEP | Rezum | PUL | PAE | GLL PVP | Aquablation | iTIND | |
|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 | 8 | 54 | 54 | 13 | 1 | 0 | 0 | 9 | 0 | 0 |
| Group 2 | 7 | 46 | 59 | 15 | 2 | 1 | 1 | 8 | 0 | 0 |
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
Whilst the results were not statistically significant, participants were more inclined to undergo HoLEP themselves if suffering from recurrent urinary tract infections (Table 14) than to provide this option for their patients (42 as the clinician vs 50 as the patient). However, whether responding as the treating clinician or as patient themselves, the most common answer was bTURP with 66 participants choosing this option for their patients as the clinician and 58 choosing this option for themselves as the patient. Only 12 participants (8.6%) responding as the treating clinician and 11 participants (7.9%) responding as the patient would choose a MIST treatment in this scenario.
Table 14.
Question 11 – Participants’ Selections if Patient Suffers from Recurrent Urinary Tract Infections
| mTURP | bTURP | HoLEP | AEEP | Rezum | PUL | PAE | GLL PVP | Aquablation | iTIND | |
|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 | 6 | 66 | 42 | 14 | 2 | 0 | 0 | 8 | 1 | 0 |
| Group 2 | 7 | 58 | 50 | 13 | 2 | 0 | 2 | 7 | 0 | 0 |
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
When presented with the scenario in which anticoagulation cannot be stopped; more participants were likely to choose a MIST option whether they were responding as the clinician or as the patient (Table 15 and Figure 6). Seventy-one participants (51.1%) would choose a MIST for their patients when responding as the clinician, and 69 participants (49.6%) would choose a MIST for themselves as the patient. Greenlight laser photoselective vapourisation of the prostate was the most popular answer of the MIST options with 48 choosing this for their patients when responding as the clinician (34.5%) and 39 choosing this for themselves as a patient (28.1%). However, the most popular choice by individual treatment option was HoLEP with 50 participants (36.0%) choosing this for their patients and 52 participants (37.4%) choosing this option for themselves.
Table 15.
Question 12 – Participants’ Selections if Patient Takes Anticoagulation Medication that Cannot be Stopped
| mTURP | bTURP | HoLEP | AEEP | Rezum | PUL | PAE | GLL PVP | Aquablation | iTIND | |
|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 | 1 | 8 | 50 | 9 | 8 | 3 | 10 | 48 | 1 | 1 |
| Group 2 | 1 | 9 | 52 | 8 | 13 | 5 | 11 | 39 | 1 | 0 |
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
Figure 6.
Q12 – participant selection if patient took anticoagulation.
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
When the patient was not deemed fit for general or spinal anaesthesia, MIST options were most popular with high concordance in their treatment selections when participants responded as the clinician or as patient themselves (Table 16 and Figure 7). A total of 131 participants (94.2%) chose a MIST as the treating clinician and 130 participants (93%) chose a MIST as patient themselves. Rezum was the most popular choice with 50 participants (36.0%) choosing this treatment as both the clinician and the patient, followed by prostatic urethral lift [39 participants (28.1%) as either the clinician or the patient] and prostate artery embolisation [29 participants (21.0%) as either the clinician or the patient]. Whilst temporarily implanted nitinol device (iTIND) was a very rarely chosen option in other clinical scenarios, having not been chosen by participants responding as either the clinician or the patient in 10 of the 16 scenarios, 12 participants (8.6%) chose this option as the clinician and 10 participants (7.2%) chose this option as the patient.
Table 16.
Question 13 – Participants’ Selections if Patient is Not Fit for General or Spinal Anaesthesia
| mTURP | bTURP | HoLEP | AEEP | Rezum | PUL | PAE | GLL PVP | Aquablation | iTIND | |
|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 | 1 | 1 | 4 | 2 | 50 | 39 | 29 | 1 | 0 | 12 |
| Group 2 | 1 | 2 | 5 | 1 | 50 | 39 | 29 | 1 | 1 | 10 |
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
Figure 7.
Q13 – participants selection if patient is not fit for anaesthesia.
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
When participants were presented with a scenario of refractory haematuria due to BPH, results were comparable when participants responded as either the clinician or the patient (Table 17), with the majority of participants choosing an invasive treatment option rather than a MIST. When providing treatment for their patients; bTURP was marginally more popular than HoLEP (47 vs 44), with PAE being the third most popular option (22 participants). When providing treatment for themselves; HoLEP was more popular than bTURP with 53 choosing HoLEP compared to 40 choosing bTURP. The next most common option when participants responded as the patient was PAE (21 participants).
Table 17.
Question 14 – Participants’ Selections if Patient Suffers from Refractory Haematuria due to BPH
| mTURP | bTURP | HoLEP | AEEP | Rezum | PUL | PAE | GLL PVP | Aquablation | iTIND | |
|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 | 7 | 47 | 44 | 7 | 1 | 0 | 22 | 10 | 1 | 0 |
| Group 2 | 4 | 40 | 53 | 8 | 2 | 0 | 21 | 10 | 1 | 0 |
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
When presented with the scenario in which the patient does not have insurance and can only afford a single self-pay procedure (Table 18 and Figure 8), the majority of participants would choose an invasive procedure (85.6% as the clinician and 84.2% as the patient) instead of a MIST (14.4% as the clinician and 15.8% as patient themselves). Whilst a total of 70 participants would choose mTURP/bTURP for their patients, only 52 would choose this treatment option for themselves (p = 0.014). Similarly, whilst 41 participants would choose HoLEP for their patients; 56 participants would choose HoLEP for themselves (p = 0.029). Half the number of participants would choose Rezum for their patients compared to themselves (5 participants vs 10 participants).
Table 18.
Question 15 – Participants’ Selections if Patient Does Not have Insurance and can Afford a Single Self-Pay Procedure
| mTURP | bTURP | HoLEP | AEEP | Rezum | PUL | PAE | GLL PVP | Aquablation | iTIND | |
|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 | 9 | 61 | 41 | 8 | 5 | 3 | 1 | 7 | 0 | 4 |
| Group 2 | 6 | 46 | 56 | 9 | 10 | 4 | 0 | 5 | 0 | 3 |
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
Figure 8.
Q15 – participants selection if patient does not have insurance and cannot afford to self-pay.
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
When the patient is well insured and cost is not a concern, more participants were inclined to choose HoLEP as their preferred treatment option, followed by bTURP, with more participants choosing HoLEP for themselves than for their patients (62 as the clinician vs 69 as patient themselves) and less choosing bTURP for themselves and more for their patients (41 as the clinician vs 33 as patient themselves) (Table 19). In total, 15.1% of participants would choose a MIST option for their patients and 17.3% would choose a MIST option for themselves.
Table 19.
Question 16 – Participants’ Selections if Patient is Well Insured and Not Concerned about Cost
| mTURP | bTURP | HoLEP | AEEP | Rezum | PUL | PAE | GLL PVP | Aquablation | iTIND | |
|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 | 4 | 41 | 62 | 11 | 9 | 2 | 0 | 7 | 3 | 0 |
| Group 2 | 3 | 33 | 69 | 10 | 13 | 2 | 0 | 6 | 3 | 0 |
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
When participants acted as the treating clinician, they were more inclined to choose bTURP for patients who did not have insurance (61 participants) whilst HoLEP was the more popular choice (62 participants) for those who did have insurance (Table 20). When acting as the patient themselves, participants were more inclined to choose HoLEP whether or not they had insurance; 56 participants chose HoLEP with no insurance and 69 participants chose HoLEP with insurance (Table 21 and Figure 9).
Table 20.
Participants’ Selections when acting as the treating clinician when the patient is not insured versus when the patient is insured
| mTURP | bTURP | HoLEP | AEEP | Rezum | PUL | PAE | GLL PVP | Aquablation | iTIND | |
|---|---|---|---|---|---|---|---|---|---|---|
| No insurance | 9 | 61 | 41 | 8 | 5 | 3 | 1 | 7 | 0 | 4 |
| Insurance | 4 | 41 | 62 | 11 | 9 | 2 | 0 | 7 | 3 | 0 |
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
Table 21.
Participants’ Selections when acting as the patient when they are not insured versus when they are insured
| mTURP | bTURP | HoLEP | AEEP | Rezum | PUL | PAE | GLL PVP | Aquablation | iTIND | |
|---|---|---|---|---|---|---|---|---|---|---|
| No Insurance | 6 | 46 | 56 | 9 | 10 | 4 | 0 | 5 | 0 | 3 |
| Insurance | 3 | 33 | 69 | 10 | 13 | 2 | 0 | 6 | 3 | 0 |
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
Figure 9.
Q16 – participants selection if patient insured.
mTURP – monopolar transurethral resection of the prostate; bTURP – bipolar transurethral resection of the prostate; HoLEP – Holmium laser enucleation of the prostate; AEEP – other anatomical endoscopic enucleation of the prostate; Rezum – Rezum water therapy; PUL – prostatic urethral lift; PAE – prostatic artery embolization; GLL PVP – greenlight laser photoselective vapourisation of the prostate; iTIND – temporarily implanted nitinol device
DISCUSSION
An ageing population is inextricably linked with an increase in prevalence of BPH; with Berry et al. estimating 50% prevalence in men between 51 and 60 years old and 80% prevalence in men over 80 years old [3]. Clinical BPH is the manifestation of LUTS, which may become significant enough for patients to seek a medical opinion. Speakman et al. emphasise the negative impact LUTS have on our patients’ quality of life (QoL) [4], with approximately 30% of men over 50 years old suffering from moderate/severe LUTS [5] and Verhamme et al., reporting LUTS due to BPH in 24% of men over 80-years old [6]. There is, therefore, an increasing need for BPH treatment, which has instigated the development of novel surgical and MIST procedures.
Surgical intervention tends to be selected for patients with refractory symptoms despite conservative and lifestyle management or medical treatment. Whilst TURP has remained the most commonly performed surgical treatment for symptomatic BPH, deciding which treatment to choose has become more complex with the introduction of new surgical options. Patients tend to rely upon their doctors to engage in shared decision making so as to obtain knowledge about each treatment and to weigh up the risks and benefits of each option with the aim of achieving optimal patient outcomes [7]. Prior to this study, there have been no studies assessing whether clinicians’ practice would differ in the surgical management of BPH if they were to consider themselves as the patient.
High concordance rates for treatment choices were found in most scenarios, however there was a tendency for clinicians to choose enucleation procedures for themselves over their patients, given the same clinical scenario. Apart from when participants considered the patient to suffer from prostate cancer (in which case the same number of clinicians chose HoLEP for their patients as they would for themselves), more participants chose HoLEP for themselves rather than their patient in each one of the scenarios presented to them. This was statistically significant when choosing their ‘Standard BPH procedure’, choosing options for a high post void residual, if sexual function was not deemed important and if the patient was uninsured.
The reason for clinicians choosing HoLEP for themselves over their patients when presented with the same clinical scenario may be due to the clinicians themselves being personally unable to carry out the procedure or due to the lack of availability and access to HoLEP at their hospitals; therefore, feeling unable to provide this as a viable option to patients. Whilst HoLEP was developed in 1998, it is not yet performed in each hospital, largely due to limited exposure, its steep learning curve and limited mentorship availability [8, 9]; with surgeons on average needing to carry out at least 20 cases to feel confident in the procedure [10, 11]. However, theoretically, a lack of availability in one hospital should not prevent a referral to a centre specialising in HoLEP or with HoLEP mentorship in place, as per National Institute for Health and Care Excellence (NICE) Guidelines [12].
A large number of participants had never performed a number of the MIST options; with only 6.5% of participants having carried out iTIND at least once, and 9.4% having carried out Aquablation at least once. Of the MIST options presented, the most popular treatments to have been carried out at least once by participants were GLL PVP (44.6%) and Rezum (39.6%). No single MIST had been carried out at least once by even half of the participants, indicating that more experience with MISTs is required. The lack of experience with MIST options may be due to poor exposure to and availability of these treatment options to trainees, who therefore do not adopt these methods into their future practice or consider referring patients for them. Whilst there are a number of training simulators for invasive procedures, these do not appear to be as easily accessible for MIST treatments [13]. Each MIST offers its own benefits, risk factors and unique qualities and without sufficient exposure to different MISTs, clinicians will be hard pressed to provide adequate information on treatment options to their patients that are tailored to their patients’ unique clinical scenario in a shared decision-making process [14, 15].
Differences were noted in participants’ decisions when choosing treatment options based on whether the patient was insured or not. Clinicians were more inclined to provide bTURP for their uninsured patients (43.9%), yet only a third would choose bTURP for themselves under the same circumstances. Participants instead chose HoLEP (40.2%) and double the number of participants chose Rezum when considering themselves as the uninsured patient. Comparing participants’ choices when their patient is either insured or uninsured has shown that there was a preference for bTURP when uninsured and HoLEP when insured, which may indicate a belief that HoLEP is a more expensive procedure. However, when choosing for themselves; HoLEP was the most popular choice regardless of insurance status.
It is difficult to evaluate the reason behind participants’ choices without qualitative assessment; for example, whether bTURP was preferentially chosen for uninsured patients because of its lower operative cost. Conversely, HoLEP may have been chosen for uninsured patients because of its fewer perioperative complications, more favourable long-term outcomes, lower reoperation rates and improved quality of life [16, 17, 18, 19, 20], therefore opting for a potentially more expensive procedure at face value but one that will likely not require further intervention in the future. As demonstrated by Schiavina et al.; whilst intraoperative costs were higher for HoLEP compared to TURP in prostates <70 cc, the indirect costs in relation to hospitalisation were fewer for HoLEP, demonstrating the durability of enucleation procedures [21]. Similarly, Fraundorfer et al., determined a 24.5% cost saving when offering HoLEP in comparison to TURP at 12 months post operatively, when taking complications, hospital stay and catheterisation time into consideration [22, 23]. Establishing why ‘uninsured’ participants were less likely to choose TURP for themselves and more likely to choose HoLEP when compared to their patients presents similar difficulties. This may reflect a combination of participants’ individual views on which procedure is more cost-effective and participants’ knowledge on what they would personally be able to afford versus their unfamiliarity with their patients’ financial situation.
The survey was distributed to urologists within the UK and the EU, with participants likely referring to NICE Guidelines and EAU Guidelines in their clinical practice to aid them in their decision making. Whilst the guidelines agree on the use of a number of procedures to treat BPH, the indications for some techniques vary between the guidelines, and recommendations for some procedures in some guidelines are not specific [24]. For example, EAU Guidelines recommend TURP on a prostate volume between 30-80 cc and state that HoLEP is their current standard for large prostates, whilst NICE Guidelines do not specify size for TURP or HoLEP [24]. The Clinical Practice Guidelines used by the participants will likely influence their selections [25–27]. It is unknown whether participants would refer to a specific guideline for their patients based on what they are expected to use when practicing, as opposed to a guideline they would ideally want to use for themselves as a patient.
There are limitations to this study. Whilst clinical scenarios were presented to the participants, further background information regarding the hypothetical patients that may alter a clinician’s treatment choice was not provided. Similarly, participants lacked the presence of a ‘real’ patient. Therefore, making a true comparison of treatment selections between the participants (with knowledge of their own personal and medical background) and the hypothetical patient is challenging. The study lacks qualitative data, for example about insurance and financial status, which may alter or explain participants’ selections. Furthermore, it is unknown which clinical practice guidelines each participant was in favour of using to aid them in their decision making as we did not collect the country of participating urologists or their age, gender or experience. Also, as we wanted to collect their reflections on endoscopic and MIST therapies, data was not collected on simple prostatectomy via open, laparoscopic or robotic approaches.
CONCLUSIONS
The majority of urologists that participated in this study had minimal experience in the newer BPH procedures and MISTs, indicating that more exposure and training is required. Whilst there were high consistency rates for treatment choices in most scenarios, there was a tendency for participants to choose HoLEP when considering themselves to be the patient.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
ACKNOWLEDGEMENT
EAU Section of Uro-Technology (ESUT)
References
- 1.Roehrborn CG. Benign prostatic hyperplasia: an overview. Rev Urol. 2005; 7: S3-S14. [PMC free article] [PubMed] [Google Scholar]
- 2.GBD 2019 Benign Prostatic Hyperplasia Collaborators . The global, regional, and national burden of benign prostatic hyperplasia in 204 countries and territories from 2000 to 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Healthy Longev. 2022; 3: e754-e776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol. 1984; 132: 474-479. [DOI] [PubMed] [Google Scholar]
- 4.Speakman M, Kirby R, Doyle S, Ioannou C. Burden of male lower urinary tract symptoms (LUTS) suggestive of benign prostatic hyperplasia (BPH) - focus on the UK. BJU Int. 2015; 115: 508-519. [DOI] [PubMed] [Google Scholar]
- 5.Madersbacher S, Haidinger G, Temml C, Schmidbauer CP. Prevalence of lower urinary tract symptoms in Austria as assessed by an open survey of 2,096 men. Eur Urol. 1998; 34: 136-141. [DOI] [PubMed] [Google Scholar]
- 6.Verhamme KM, Dieleman JP, Bleumink GS, et al. Incidence and prevalence of lower urinary tract symptoms suggestive of benign prostatic hyperplasia in primary care--the Triumph project. Eur Urol. 2002; 42: 323-328. [DOI] [PubMed] [Google Scholar]
- 7.Piercy GB, Deber R, Trachtenberg J, et al. Impact of a shared decision-making program on patients with benign prostatic hyperplasia. Urology. 1999; 53: 913-920. [DOI] [PubMed] [Google Scholar]
- 8.Martinez-Salas AJ, Garcia-Rivera OU, Reyna-Blanco I, Jimenez-Garcia AD, Rosas-Hernandez H. Adequate mentorship program for holmium laser enucleation of the prostate (HoLEP) leads to satisfactory short-term outcomes in the early learning curve of young urologists: first-year outcomes of a newly established mentorship training in Mexico. Cureus. 2023; 15: e41756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wright HC, Fedrigon D, De S. Learning From those who learned: A survey of fellowship trained HoLEP Surgeons and their current practice patterns. Urology. 2021; 149: 193-198. [DOI] [PubMed] [Google Scholar]
- 10.Robert G, Cornu JN, Fourmarier M, et al. Multicentre prospective evaluation of the learning curve of holmium laser enucleation of the prostate (HoLEP). BJU Int. 2016; 117: 495-499. [DOI] [PubMed] [Google Scholar]
- 11.Gürlen G, Karkin K. Does Holmium laser enucleation of the prostate (HoLEP) still have a steep learning curve? Our experience of 100 consecutive cases from Turkey. Arch Ital Urol Androl. 2021; 93: 412-417. [DOI] [PubMed] [Google Scholar]
- 12.National Institute for Health and Care Excellence . Lower urinary tract symptoms in men: Management Clinical Guideline [CG97] [Internet]. 23 May 2010, Updated 2 June 2015. Available from: https://www.nice.org.uk/guidance/cg97/chapter/Recommendations [PubMed]
- 13.Luu T, Gonzalez RR. Residency surgical BPH training paradigms from MIST to HoLEP. Curr Urol Rep. 2023; 24: 261-269. [DOI] [PubMed] [Google Scholar]
- 14.Sciacqua LV, Vanzulli A, Di Meo R, et al. Minimally invasive treatment in benign prostatic hyperplasia (BPH). Technol Cancer Res Treat. 2023; 22: 15330338231155000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Franco JV, Jung JH, Imamura M, et al. Minimally invasive treatments for lower urinary tract symptoms in men with benign prostatic hyperplasia: a network meta-analysis. Cochrane Database Syst Rev. 2021; 7: CD013656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gilling PJ, Wilson LC, King CJ, Westenberg AM, Frampton CM, Fraundorfer MR. Long-term results of a randomized trial comparing holmium laser enucleation of the prostate and transurethral resection of the prostate: results at 7 years. BJU Int. 2012; 109: 408-411. [DOI] [PubMed] [Google Scholar]
- 17.Elmansy HM, Kotb A, Elhilali MM. Holmium laser enucleation of the prostate: long-term durability of clinical outcomes and complication rates during 10 years of followup. J Urol. 2011; 186: 1972-1976. [DOI] [PubMed] [Google Scholar]
- 18.Shvero A, Calio B, Humphreys MR, Das AK. HoLEP: the new gold standard for surgical treatment of benign prostatic hyperplasia. Can J Urol. 2021; 28: 6-10. [PubMed] [Google Scholar]
- 19.Das AK, Han TM, Hardacker TJ. Holmium laser enucleation of the prostate (HoLEP): size-independent gold standard for surgical management of benign prostatic hyperplasia. Can J Urol. 2020; 27: 44-50. [PubMed] [Google Scholar]
- 20.Sun F, Sun X, Shi Q, Zhai Y. Transurethral procedures in the treatment of benign prostatic hyperplasia: A systematic review and meta-analysis of effectiveness and complications. Medicine (Baltimore). 2018; 97: e13360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schiavina R, Bianchi L, Giampaoli M, et al. Holmium laser prostatectomy in a tertiary Italian center: A prospective cost analysis in comparison with bipolar TURP and open prostatectomy. Arch Ital Urol Androl. 2020; 92. [DOI] [PubMed] [Google Scholar]
- 22.Fraundorfer MR, Gilling PJ, Kennett KM, Dunton NG. Holmium laser resection of the prostate is more cost effective than transurethral resection of the prostate: results of a randomized prospective study. Urology. 2001; 57: 454-458. [DOI] [PubMed] [Google Scholar]
- 23.Pirola GM, Maggi M, Castellani D, Sciarra A, Rubilotta E, Gubbiotti M. A Cost-Benefit Analysis of Bipolar TURP for the Treatment of Bladder Outflow Obstruction. Res Rep Urol. 2021; 13: 487-494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Enikeev D, Misrai V, Rijo E, et al. EAU, AUA and NICE Guidelines on Surgical and Minimally Invasive Treatment of Benign Prostate Hyperplasia: A Critical Appraisal of the Guidelines Using the AGREE-II Tool. Urol Int. 2022; 106: 1-10. [DOI] [PubMed] [Google Scholar]
- 25.Jones P, Rajkumar GN, Rai BP, et al. Medium-term outcomes of Urolift (minimum 12 months follow-up): evidence from a systematic review. Urology. 2016; 97: 20-24. [DOI] [PubMed] [Google Scholar]
- 26.Maclean D, Harris M, Drake T, et al. Factors predicting a good symptomatic outcome after prostate artery embolization (PAE). Cardiovasc Intervent Radiol. 2018; 41: 1152-1159. [DOI] [PubMed] [Google Scholar]
- 27.Westwood J, Geraghty R, Jones P, et al. Rezum: a new transurethral water. Vapour therapy for benign prostatic hyperplasia. Ther Adv in Urol. 2018; 10: 327-333. [DOI] [PMC free article] [PubMed] [Google Scholar]