Abstract
Background
Laryngeal mask airway (LMA) has been increasingly used for airway management; however, LMA insertion can be difficult and cause adverse effects. Therefore, the rapid, safe, and effective insertion of LMA is necessary. This study aimed to compare the efficacy of the standard method with that of the 30° curved tongue depressor-aided technique for LMA insertion to determine the superior technique.
Methods
This study included 154 patients aged 18–70 years (American Society of Anesthesiologists class I or II) scheduled for general anesthesia. The patients were randomly assigned to the standard LMA insertion group (Group C, n = 77) or the 30° curved tongue depressor-aided LMA insertion group (Group T, n = 77). The primary outcome evaluated was the first-attempt success rate. The secondary outcomes were the second-attempt success rate, insertion time, fiberoptic position grade, oropharyngeal leak pressure (OPLP), and adverse events.
Results
The first-attempt success rate was significantly higher in Group T than in Group C (97.40% vs. 88.31%, P = 0.029). The second-attempt success rate (P = 0.209), insertion time (P = 0.340), fiberoptic position grade (P = 0.872), and OPLP (P = 0.203) were slightly improved in Group T; however, there was no statistical significance. Bleeding events were reduced in Group T than in Group C (6.49% vs. 14.29%); however, there was no statistical significance. The incidence of sore throat symptoms was significantly reduced in Group T than in Group C (5.19% vs. 15.58%, P = 0.035).
Conclusions
The curved tongue depressor-aided technique significantly improved the first-attempt success rate of LMA insertion and reduced the incidence of sore throat symptoms.
Trial registration
KCT0004964; Registered at https://cris.nih.go.kr on April 27, 2020.
Keywords: Standard technique, Curved tongue depressor, Laryngeal mask airway, LMA insertion, First-attempt success rate
Background
Supraglottic airway devices (SADs) are used to maintain upper airway opening and provide adequate ventilation and oxygenation. These devices can be used for airway maintenance during general anesthesia as well as for primary airway maintenance during emergencies (such as intubation failures). Because SADs are less invasive than endotracheal intubation, their use is associated with lesser hemodynamic changes after insertion and a lower incidence of sore throat symptoms after extubation. In addition, usage of SADs has been increasing due to their ease of use [1].
Laryngeal mask airway (LMA), a type of SAD, has been used successfully for airway management. The index finger insertion technique is considered the standard method of LMA insertion and is the most widely used. In this technique, the patient’s head is tilted back with one hand, and the LMA is held similarly to a pen. Subsequently, with the index finger placed at the junction of the cuff and the airway tube, the LMA is inserted while pressing against the hard palate and posterior pharyngeal wall until resistance is encountered when the mask tip reaches the base of the hypopharynx [2]. The success rate of this technique is approximately 80% [3].
Narrowing of the space between the tongue and the hard palate increases the difficulty of LMA insertion. In particular, in cases wherein an LMA with an airbag is used, attempting insertion of the device with the air removed makes insertion in the desired direction difficult and may result in complications such as overlapping cuffs. Therefore, technical developments to increase the success rate have been studied extensively. Insertion of a suction tube as a guide and rotation of the LMA by 90° or 180° have been reported to be more useful than the standard method; however, these modifications are sometimes insufficient [4–8].
The triple airway maneuver is the most reliable manual method for achieving patency of the native upper airway and provides the most favorable position for maintaining the airway. In this maneuver, the operator tilts the patient’s head back, raises their chin, and opens their mouth. It is considered more efficient than the standard method [9]; however, an assistant’s aid is required during LMA insertion. Therefore, it is necessary to develop an easier and more convenient method for LMA insertion.
Because a simple chin-lifting and tongue-pressing device would aid LMA insertion, we developed a 30° curved tongue depressor device that mimics the shape of a laryngoscope blade and compared the efficacy of the standard method with that of the new technique in terms of successful LMA insertion rates to determine the superior technique.
Methods
This prospective, single-center, randomized controlled trial was performed from May 2020 to March 2021 at the Hanyang University Hospital in Seoul, Republic of Korea.
Fabrication of the 30° curved tongue depressor
LMA designed to maintain a 30° angle at the junction of the mask and tube has been shown to both facilitate visualization of the glottis and enhance the success rate of insertion [10]. Thus, a 30° curved tongue depressor was fabricated by bending the position where the length ratio was 1.0:0.6 from the end of the handle of the Wieder Tongue Depressor to maintain a 30° curve (MH22-4 WIEDER Tongue Depressor, large 36-mm serrated blade, Integra Miltex®, Germany; Fig. 1).
Fig. 1.
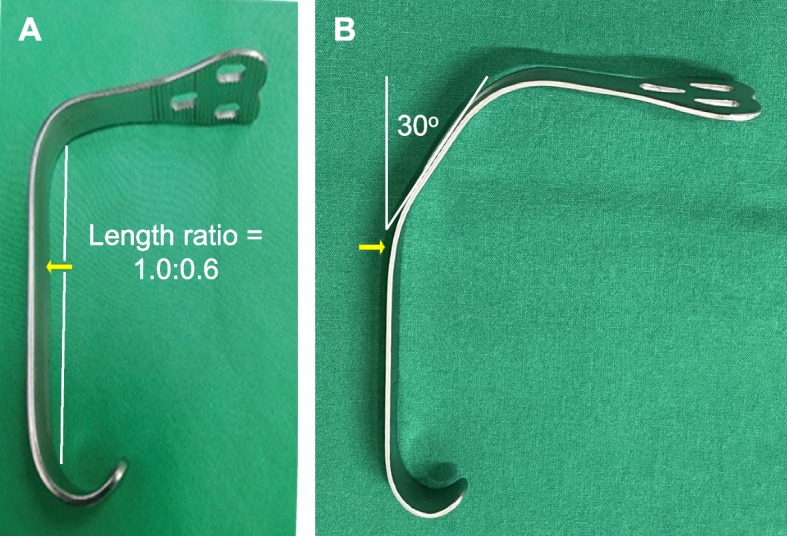
Shapes of the Wieder tongue depressor. A The original shape of the tongue depressor. B the 30° curved tongue depressor, which was reshaped by bending the original tongue depressor into a 30° curve (arrow) at the position with a length ratio of 1.0:0.6 from the end of the handle
Study population
Among the patients scheduled to undergo surgery under general anesthesia, those aged 18–70 years with a Class I or II rating on the American Society of Anesthesiologists (ASA) physical status classification system and a body mass index of < 30 kg/m2 were enrolled in this study. Patients who met any of the following criteria were excluded: (1) unwillingness to participate, (2) mouth opening < 2.5 cm, (3) possible risk of aspiration (such as presence of esophageal hiatal hernia, gastroesophageal reflux disease, and a full stomach), (4) pregnancy, (5) weight < 45 kg or > 100 kg, (6) lung disease, (7) surgery performed in positions other than the supine position, (8) anticipated difficulty in tracheal intubation or positive pressure mask ventilation (i.e., limited jaw protrusion, limited neck extension, Mallampati class III or IV, or patients who had history of snoring or difficult intubation), and (9) anatomical abnormalities in the cervical spine or airway. Prior to anesthesia induction, the patients were assigned to the control group (Group C; standard insertion method performed using the index finger) or the 30° curved tongue depressor-aided group (Group T; proposed insertion method performed using the tongue depressor) at a 1:1 ratio using a random number table generated by a third party. All data were independently collected by blinded investigators who were trained but not directly involved in patient care. All patients tested negative for pre-hospital COVID-19 antigen and PCR tests, and all devices used were disposable.
Anesthesia induction
Monitoring systems with non-invasive blood pressure measurement, pulse oximetry, electrocardiography (CARESCAPE™ B650 Monitor, GE Healthcare, USA), and bispectral index (BIS; BIS™, Medtronic, USA) measurement were applied when the patient entered the operating room. The investigator instructed the patient to breathe deeply with 100% oxygen for 3 min and began anesthesia induction when the oxygen saturation level (SpO2) was > 95%. Intravenous infusion of 1 µg/kg of remifentanil was followed by intravenous administration of 0.5 mg/kg of lidocaine and 1.5 mg/kg of propofol. After confirming the loss of consciousness, 0.6 mg/kg of rocuronium was administered intravenously under peripheral neuromuscular transmission monitoring. Sevoflurane was used to maintain a BIS value between 40 and 60.
LMA insertion (group C vs. Group T)
Following the administration of the induction drugs, the investigator placed a gel pad under the patient’s head in the sniffing position (under neck flexion and head extension), because it is the best position to secure the airway. The LMA (Laryseal blue™, Flexicare Medical Ltd., UK) was prepared with lubrication on the back and a deflated air sac. An LMA of size 3, 4, or 5 was selected if the patient weighed < 50 kg, 50–70 kg, or > 70 kg, respectively. LMA insertion was performed by two investigators with experience of more than 200 LMA insertions.
In Group C, the index finger was placed between the airway tube and the cuff while holding the LMA similarly to a pen. Using the finger as a guide, the investigator gently pushed the LMA along the hard palate to the hypopharynx (Fig. 2A). In Group T, the investigator used the 30° curved tongue depressor (Fig. 1B). The curved tongue depressor was inserted toward the center of the patient’s tongue with one hand and lifted anteriorly. The LMA was held similarly to a pen with the other hand and pushed slowly along the hard palate to the hypopharynx (Fig. 2B).
Fig. 2.
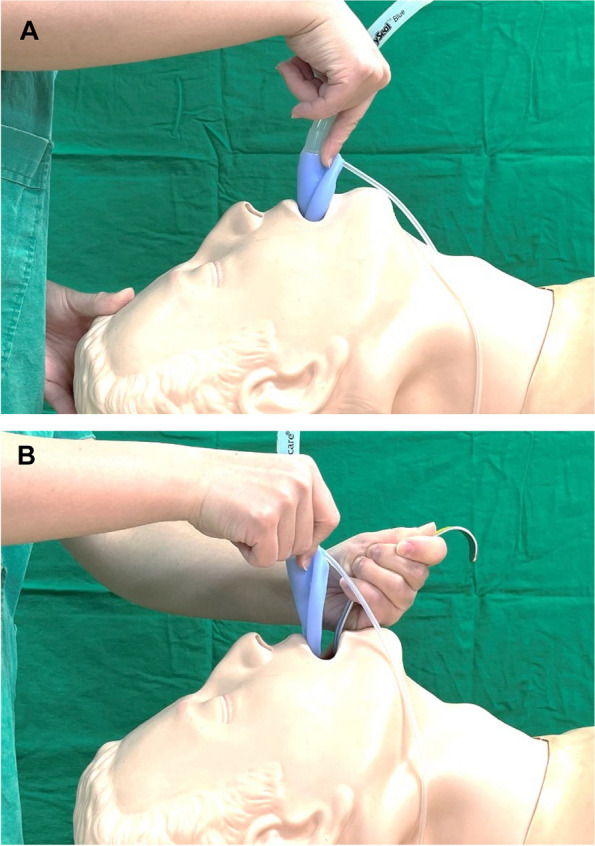
Photographs showing LMA insertion using different methods. A The standard method. B The 30° curved tongue depressor-aided technique
Air was injected into the air sac during LMA insertion, and the ventilator was connected to the LMA. LMA insertion was considered a success if both lung sounds could be heard clearly with no leaking sound around the LMA and if the capnography (EtCO2) curve was normal. A second attempt was made in case of a failure of the first attempt. In case of a failed second attempt, endotracheal intubation was performed for the patient's safety due to a time lapse of approximately 2 min owing to two failed insertions. Cases wherein endotracheal intubation was performed without attempting LMA insertion or the SpO2 fell below 94% after artificial respiration were excluded from this study.
Outcome measurements
The primary outcome evaluated in this study was the first-attempt success rate. The secondary outcomes were the second-attempt success rate, LMA insertion success time, oropharyngeal leak pressure (OPLP), fiberoptic position score, and rates of other complications (blood staining on the LMA device or suction tube, sore throat, dysphagia, and dysphonia). The methods for outcome measurement are detailed below.
1) LMA insertion success time
The time required for successful LMA insertion was recorded as follows. (1) Group C: The duration began when the LMA passed the upper incisors and ended when the first EtCO2 was measured after connecting the ventilator. (2) Group T: The duration began when the tongue depressor passed the upper incisors and ended when the first EtCO2 was measured after connecting the ventilator. Successful insertion on the first attempt was defined as correct placement of the LMA tube with a single insertion within 60 s. If this failed, a second insertion was attempted for an additional 60 s.
2) fiberoptic position score
The fiberoptic position grade was used as determinant of the LMA position as follows [9, 11, 12]: Grade 1, the glottis is completely visible without obscuring the epiglottis; Grade 2, the glottis is slightly obscured by the tip of the epiglottis; Grade 3, more than half of the glottis is obscured by the epiglottis; and Grade 4, the glottis is completely obscured by the epiglottis (complete downfolding). When the fiberoptic position grade was 4, the LMA was removed and reinserted. If the grade at LMA reinsertion was 2 or 3, the surgery proceeded normally; however, if it was 4 again, the surgery was performed after endotracheal intubation.
3) OPLP
At a fresh gas flow of 3 L/min, the exhalation valve was closed to the maximum value, and a stethoscope was placed near the patient’s mouth. As the pressure rose, the sound of air leaking was heard at some point, and the pressure at that time was measured. If no sound was heard even at the maximum pressure (40 cm H2O), the oropharyngeal leakage pressure was recorded as 40 cm H2O.
4) other complications
Bleeding was considered to be present if there was any blood staining on the LMA device or suction tube after extubation. Symptoms of sore throat, dysphagia, and dysphonia were confirmed in the recovery room.
Statistical analysis
The success rate of LMA insertion in adult patients has been reported to be 80.6% [3]. Based on a power of 0.8 for a difference of 15% between the two groups with an alpha of 0.05, we calculated the minimum sample size to be 70 for each group for adequate power. Considering a drop-out rate of 10%, 77 patients were required. Thus, 154 patients were included in this study. The Statistical Package for the Social Sciences software (version 22, IBM Corp., Armonk, NY, USA) was used for all statistical analyses. The statistical analyses were performed suing a Chi-square test, Student’s t-test, or Mann–Whitney U-test between the two groups according to normality. Numerical data are presented as mean ± standard deviation. A P-value of < 0.05 was considered statistically significant. Absolute standardized difference (ASD) was calculated to evaluate the balance of patient characteristics between Group C and T using the stddiff package for R statistical software. The ASD value greater than 0.316 (i.e., 1.96 × = 0.316, where n1 = 77 and n2 = 77) was considered imbalanced.
Results
In total, 154 patients were enrolled in this study. The CONSORT flow diagram is presented in Fig. 3, and the patient characteristics are presented in Table 1. No patient was excluded from the study owing to the exclusion criteria. There were no statistically significant differences between Groups C and T in terms of the patient characteristics. Data regarding the primary and secondary outcomes are presented in Tables 2 and 3, respectively. Table 2 shows that the first-attempt success rate was higher in Group T than in Group C (97.40% vs. 88.31%, n = 77 in each group; P = 0.029); however, no statistically significant differences were observed between the second-attempt success rates of the two groups (Group C vs. T: 93.51% vs. 98.70%; P = 0.209).
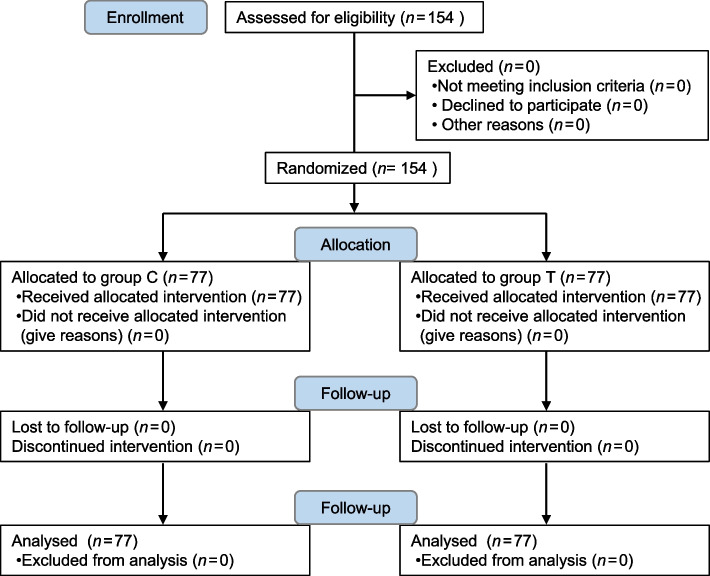
Fig. 3.
CONSORT flow diagram. Diagram shows a comparison between the LMA insertion effect of the standard method (Group C) and that of the curved tongue depressor-aided technique (Group T)
Table 1.
Patient characteristics
| Group C (n = 77) | Group T (n = 77) | P-value | ASDa | |
|---|---|---|---|---|
| Age (yrs) | 46.78 ± 13.16 | 43.43 ± 13.64 | 0.123 | 0.250 |
| Height (cm) | 162.89 ± 8.59 | 164.51 ± 7.38 | 0.134 | 0.203 |
| Weight (kg) | 63.01 ± 10.23 | 62.23 ± 11.56 | 0.659 | 0.071 |
| Sex, M/F (n) | 23/54 | 32/45 | 0.130 | 0.246 |
| ASA Class I/II (n) | 45/32 | 50/27 | 0.407 | 0.134 |
Values are mean ± SD or numbers
ASD Absolute standardized difference
aThe ASD values greater than 0.316 are considered imbalanced between the groups
Table 2.
Primary and secondary attempt success rates
| Group C (n = 77) | Group T (n = 77) | P-value | |
|---|---|---|---|
| First attempt success rate, n (%) | 68 (88.31%) | 75 (97.40%) | 0.029* |
| Second attempt success rate, n (%) | 72(93.51%) | 76 (98.70%) | 0.209 |
Values are mean ± SD or numbers
*, P < 0.05 indicates statistical significance
Table 3.
Secondary variables
| Group C (n = 68) | Group T (n = 75) | P-value | |
|---|---|---|---|
|
Time required for insertion, sec |
23.60 ± 10.16 | 20.97 ± 6.99 | 0.340 |
|
Fiberoptic position score, Grade 1/2/3/4 (n) |
24/25/17/2 | 27/27/20/1 | 0.872 |
|
Oropharyngeal leak pressure, cm H2O (%) |
31.09 ± 8.31 | 32.97 ± 7.34 | 0.203 |
Values are mean ± SD or numbers
Tables 3 present a comparison of the secondary variables between patients from Groups C (n = 68) and T (n = 75) in whom insertion was successful in the first attempt. The time taken for LMA insertion (P = 0.340) and the fiberoptic position score (P = 0.872) did not differ significantly between the two groups; however, an improvement was observed in Group T (Table 3). Similarly, the OPLP did not differ significantly between the two groups (P = 0.203). Table 4 presents the incidence of adverse events. Compared with Group C, Group T exhibited a lower incidence of bleeding (14.29% vs. 6.49%, 0.45-fold) and sore throat symptoms (15.58% vs. 5.19%, 0.33-fold); however, no difference was observed in the incidence of dysphagia between the two groups (1.30% vs. 1.30%). Statistical significance was observed only for the incidence rate of sore throat (P = 0.035) but not for that of bleeding (P = 0.113) or dysphagia (P > 0.999).
Table 4.
Incidence of adverse events
| Group C (n = 77) | Group T (n = 77)) | P-value | |
|---|---|---|---|
| Bleedinga, n (%) | 11 (14.29%) | 5 (6.49%) | 0.113 |
| Sore throat, n (%) | 12 (15.58%) | 4 (5.19%) | 0.035* |
| Dysphagia, n (%) | 1 (1.30%) | 1 (1.30%) | > 0.999 |
| Dysphonia, n (%) | 0 (0.00%) | 0 (0.00%) |
Values are mean ± SD or numbers
aBleeding refers to blood staining on the LMA device or suction tube after extubation
*, P < 0.05 indicates statistical significance
Discussion
Our data demonstrated that the first-attempt success rate was significantly higher and the incidence of sore throat symptoms was significantly lower with the 30° curved tongue depressor-aided technique than with the standard method. These results suggest that compared with the standard method, the curved tongue depressor method can improve the insertion success rate and the incidence of sore throat symptoms without significantly altering the number of adverse events.
LMA insertion failure is not rare but can occur for several reasons, such as downfolding of the epiglottis, lateral double-folding of the epiglottis, excessively deep or shallow insertion of the LMA, folding of the tip of the distal cuff of the LMA, and LMA size being excessively large or small for the patient [13]. Although rare, LMA insertion failure may result in adverse or harmful events and even cause serious complications. Bleeding, sore throat, and dysphagia are common complications, whereas pulmonary aspiration, swelling of the tongue, and lingual ischemia are severe complications [14–19]. Therefore, the rapid, safe, and accurate insertion of an LMA is necessary.
Several techniques have been developed for this purpose, such as laryngoscope- or videolaryngoscope-guided intubation techniques. These techniques have gained popularity due to advantages of rapid insertion and an increased first-attempt success rate of 85 − 98%. Videolaryngoscopy (> 90%) has a slightly higher success rate than that of conventional laryngoscopy (< 90%) [20–23]; however, both scopes have thick blades, which may narrow the oral space and hinder LMA insertion. Compared with the standard method, the 90° rotation technique for LMA insertion has a higher first-attempt success rate (83 − 86% vs. 97 − 100%) in adult patients and is associated with a lower incidence of sore throat symptoms and mucosal bleeding; however, this is not applicable in all cases [5–7, 24–27]. The efficacy of the 180° rotation technique for LMA insertion, including the first-attempt success rate, was similar to or not different from that of the 90° rotation method [7, 27]. Compared with the standard method, the LMA insertion technique with the modified tongue depressor, reformed by bending the inner curved part, improved the first-attempt success rate (82% vs. 98%) and the incidence of bleeding (24% vs. 6%) and sore throat symptoms (28% vs. 8%) [28].
In this study, the curved tongue depressor was designed to have a laryngoscope blade-like curved shape by bending the handle into a 30° curve at a position where the length ratio was 1.0:0.6 from the end of the handle of the original tongue depressor. This device offers several advantages. It facilitates the tip of the LMA to be positioned closer to the tongue base without irritating the epiglottis because its curved handle is longer than the other side (length ratio = 1.0:0.6). In addition, because our curved tongue depressor can be easily lifted upwards and forwards to provide more oral space, it reduces the risk of the epiglottis folding downward or the deflated LMA cuff folding back when the LMA is inserted along the hard palate. Therefore, we found that this device-aided technique is superior to the standard method for LMA insertion in terms of the first-attempt success rate and the incidence of bleeding and sore throat symptoms. Moreover, the efficacy of this technique is equivalent to or better than that of other techniques developed or used clinically [5–7, 20–28]. These results suggest that the curved device facilitates the correct placement and safe insertion of LMA and improves the incidence of complications (such as sore throat symptoms) without affecting other clinical factors or harmful indices.
Nevertheless, this study has some limitations. The first limitation is investigator bias. Although the investigators had performed more than 200 LMA insertions, we could not blind them completely due to the technical differences between the two groups. However, to minimize biased results, other blinded raters evaluated several clinical characteristics in detail, such as the success rate of LMA insertion, vital signs, the fiberoptic position score, and any adverse events. Another limitation was whether the difference in the success rates was applicable to all patients undergoing LMA intubation. Because the patients received general anesthesia and LMA is often used in general clinical practice without muscle relaxants, there may also be partial limitations in interpreting the results of this study. Older adult patients with underlying diseases are at a higher risk of developing respiratory complications and require LMA insertion in an emergency setting in many cases. To facilitate the comparison of the various success rates, this study included participants who were thought to have normal airways, so it is unclear whether the success rate with the curved tongue depressor would be higher in such patients. Additionally, the second success rates of LMA insertion in both groups were not perfect, being 93.5% in Group C (failure in two female patients) and 98.7% in Group T (failure in one female patient). This was attributed to limited mouth opening and neck extension, protruding incisors, and unexpected resistance during LMA insertion (without any other notable limiting characteristics). Therefore, it was difficult to identify the factors involved in LMA insertion failure. In general, the factors that make intubation difficult are the sternomental distance, neck circumference, thyromental distance ratio, and mouth opening of the patient [29, 30]. In this study, factors other than the mouth opening size were not considered. Therefore, further studies are required to compare the relationships between other factors and intubation success.
In our study, all pat.
Conclusions
Compared with the standard method, the curved tongue depressor-aided technique improved the first-attempt success rate for LMA insertion and the incidence of sore throat symptoms without increasing the incidence of other complications. The efficacy of our device for effective LMA intubation is superior to that of the standard method and is equal to or better than that of other improved techniques used in the clinic. Thus, the curved tongue depressor-aided technique may be useful as an acceptable alternative to improve LMA intubation.
Acknowledgements
We thank Dr. Jiyeong Kim in the Department of Pre-Medicine, College of Medicine, and Biostatistics Lab., Medical Research Collaborating Center, Hanyang University, for assistance with statistical counsel.
Abbreviations
- ASD
Absolute standardized difference
- BIS
Bispectral index
- EtCO2
Capnography
- LMA
Laryngeal mask airway
- OPLP,
Oropharyngeal leak pressure
- SADs
Supraglottic airway devices
- SpO2
Oxygen saturation level
Authors’ contributions
C.L.K. Conceptualization, Methodology, Writing original draft. H.L. Formal analysis and investigation. L.K. and J.K. & Y.J. Formal analysis and investigation. M.A.J. Formal analysis and investigation, Writing review and editing. J.Y.K. Conceptualization, Methodology, Writing original draft,Writing review and editing. All authors reviewed the manuscript.
Funding
None.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
This work followed the Consolidated Standards of Reporting Trials (CONSORT) statement and the Declaration of Helsinki. This study was performed from May 2020 to March 2021 after the approval of the Ethics Committee of Hanyang University Hospital in Seoul, Republic of Korea (approval number: HYUH 2020–03-001, date of approval: April 22, 2020). The public trial registration at the Clinical Research Information Service (registration number: KCT0004964, registration date: April 27, 2020) was completed before patient enrolment. Written informed consent was obtained from all participants after they understood the concept of this study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mi Ae Jeong, Email: irisjy00@hanmail.net.
Ji-Yoon Kim, Email: macheong@hanyang.ac.kr.
References
- 1.Sorbello M, Petrini F. Supraglottic airway devices: the search for the best insertion technique or the time to change our point of view? Turk J Anaesthesiol Reanim. 2017;45(2):76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ramachandran SK, Kumar AM. Supraglottic airway devices. Respir Care. 2014;59(6):920–32. [DOI] [PubMed] [Google Scholar]
- 3.Pournajafian A, Alimian M, Rokhtabnak F, Ghodraty M, Mojri M. Success rate of airway devices insertion: laryngeal mask airway versus supraglottic gel device. Anesth Pain Med. 2015;5(2): e22068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yun MJ, Hwang JW, Park SH, Han SH, Park HP, Kim JH, et al. The 90° rotation technique improves the ease of insertion of the ProSeal™ laryngeal mask airway in children. Can J Anaesth. 2011;58(4):379–83. [DOI] [PubMed] [Google Scholar]
- 5.Dhulkhed PV, Khyadi SV, Jamale PB, Dhulkhed VK. A prospective randomised clinical trial for the comparison of two techniques for the insertion of Proseal laryngeal mask airway in adults-index finger insertion technique versus 90° rotation technique. Turk J Anaesthesiol Reanim. 2017;45(2):98–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Koo BW, Oh AY, Hwang JW, Na HS, Min SW. Comparison of standard versus 90° rotation technique for LMA Flexible™ insertion: a randomized controlled trial. BMC Anesthesiol. 2019;19(1):95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shyam T, Selvaraj V. Airway management using LMA-evaluation of three insertional techniques-a prospective randomised study. J Anaesthesiol Clin Pharmacol. 2021;37(1):108–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Micaglio M, Parotto M, Trevisanuto D, Zanardo V, Ori C. Glidescope/gastric-tube guided technique: a back-up approach for ProSeal LMA insertion. Can J Anaesth. 2006;53:1063–4. [DOI] [PubMed] [Google Scholar]
- 9.Aoyama K, Takenaka I, Sata T, Shigematsu A. The triple airway maneuver for insertion of the laryngeal mask airway in paralyzed patients. Can J Anaesth. 1995;42(11):1010–6. [DOI] [PubMed] [Google Scholar]
- 10.Ferneini EM, Bennett JD. Anesthetic considerations in head, neck, and orofacial infections. In: Hupp JR, Ferneini EM, editors. Head, neck, and orofacial infections. St. Louis: Elsevier; 2016. p. 422–37. [Google Scholar]
- 11.Moustafa MA, Abdelhady MM. Fiberoptic assessment of the laryngeal mask airway (Laryseal) position after one hour of positive pressure ventilation: an observational study. J Clin Anesth. 2014;26(6):480–4. [DOI] [PubMed] [Google Scholar]
- 12.Campbell RL, Biddle C, Assudmi N, Campbell JR, Hotchkiss M. Fiberoptic assessment of laryngeal mask airway placement: blind insertion versus direct visual epiglottoscopy. J Oral Maxillofac Surg. 2004;62(9):1108–13. [DOI] [PubMed] [Google Scholar]
- 13.Van Zundert AAJ, Kumar CM, Van Zundert TCR. Malpositioning of supraglottic airway devices: preventive and corrective strategies. Br J Anaesth. 2016;116(5):579–82. [DOI] [PubMed] [Google Scholar]
- 14.McHardy FE, Chung F. Postoperative sore throat: cause, prevention and treatment. Anaesthesia. 1999;54(5):444–53. [DOI] [PubMed] [Google Scholar]
- 15.Parker MRJ, Day CJE. Visible and occult blood contamination of laryngeal mask airways and tracheal tubes used in adult anaesthesia. Anaesthesia. 2000;55(4):388–90. [DOI] [PubMed] [Google Scholar]
- 16.Cros AM, Pitti R, Conil C, Giraud D, Verhulst J. Severe dysphonia after use of a laryngeal mask airway. Anesthesiology. 1997;86(2):498–500. [DOI] [PubMed] [Google Scholar]
- 17.Bernardini A, Natalini G. Risk of pulmonary aspiration with laryngeal mask airway and tracheal tube: analysis on 65 712 procedures with positive pressure ventilation. Anaesthesia. 2009;64(12):1289–94. [DOI] [PubMed] [Google Scholar]
- 18.Twigg S, Brown JM, Williams R. Swelling and cyanosis of the tongue associated with use of a laryngeal mask airway. Anaesth Intensive Care. 2000;28(4):449–50. [DOI] [PubMed] [Google Scholar]
- 19.Gerstein NS, Braude D, Harding JS, Douglas A. Lingual ischemia from prolonged insertion of a Fastrach laryngeal mask airway. West. J Emerg Med. 2011;12(1):124–7. [PMC free article] [PubMed] [Google Scholar]
- 20.Liu DX, Ye Y, Zhu YH, Li J, He HY, Dong L, et al. Intubation of non-difficult airways using video laryngoscope versus direct laryngoscope: a randomized, parallel-group study. BMC Anesthesiol. 2019;19(1):75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schmid B, Eckert D, Meixner A, Pistner P, Malzahn U, Berbeerich M, et al. Conventional versus video-assisted laryngoscopy for perioperative endotracheal intubation (COVALENT) - a randomized, controlled multicenter trial. BMC Anesthesiol. 2023;23(1):128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim GW, Kim JY, Kim SJ, Moon YR, Park EJ, Park SY. Conditions for laryngeal mask airway placement in terms of oropharyngeal leak pressure: a comparison between blind insertion and laryngoscope-guided insertion. BMC Anesthesiol. 2019;19(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kleine-Brueggeney M, Greif R, Schoettker P, Savoldelli GL, Nabecker S, Theiler LG. Evaluation of six videolaryngoscopes in 720 patients with a simulated difficult airway: a multicentre randomized controlled trial. Br J Anaesth. 2016;116(5):670–9. [DOI] [PubMed] [Google Scholar]
- 24.Hwang JW, Park HP, Lim YJ, Do SH, Lee SC, Jeon YT. Comparison of two insertion techniques of ProSeal laryngeal mask airway: standard versus 90-degree rotation. Anesthesiology. 2009;110(4):905–7. [DOI] [PubMed] [Google Scholar]
- 25.Jeon YT, Na HS, Park SH, Oh AY, Park HP, Yun MJ, et al. Insertion of the Proseal laryngeal mask airway is more successful with the 90 degrees rotation technique. Can J Anaesth. 2010;57(3):211–5. [DOI] [PubMed] [Google Scholar]
- 26.Kim HC, Yoo DH, Kim HJ, Jeon YT, Hwang JW, Park HP. A prospective randomised comparison of two insertion methods for i-gel placement in anaesthetised paralysed patients: standard vs. rotational technique. Anaesthesia. 2014;69(7):729–34. [DOI] [PubMed] [Google Scholar]
- 27.Kumar D, Khan M, Ishaq M. Rotational vs. standard smooth laryngeal mask airway insertion in adults. J Coll Physicians Surg Pak. 2012;22(5):275–9. [PubMed] [Google Scholar]
- 28.Liu YC, Cherng CH. A modified tongue depressor facilitates the insertion of Proseal laryngeal mask airway: comparison with digital and introducer techniques. J Chin Med Assoc. 2017;80(9):582–6. [DOI] [PubMed] [Google Scholar]
- 29.Prakash S, Mullick P, Bhandari S, Kumar A, Gogia AR, Singh R. Sternomental distance and sternomental displacement as predictors of difficult laryngoscopy and intubation in adult patients. Saudi J Anaesth. 2017;11(3):273–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim WH, Ahn HJ, Lee CJ, Shin BS, Ko JS, Choi SJ, et al. Neck circumference to thyromental distance ratio: a new predictor of difficult intubation in obese patients. Br J Anaesth. 2011;106(5):743–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.