Abstract
Objective
To carry out a systematic literature review to identify the Value Based Digital Health elements.
Methods
The search for records was carried out for the period 2012 to January 2024, in two main databases, EMBASE and Scopus. Records were limited to studies published since 2012. Studies presented either a conceptual framework on the concept of Value-Based Digital Health (VBDH), or results from an empirical work to generate evidence on the value of digital health, or a combination of both. The characteristics of the study, the type of digital health and measures and/or their value elements included, are synthesized and interpreted. To synthetize information, the patient journey phases are used as themes, where the identified value elements are allocated. This is analyzed by type of agent (of the general healthcare framework).
Results
The search yielded a total of 606 abstracts for screening. In the end, 67 studies were finally included for data extraction. VBDH elements are presented by phases of the patient journey and by agent. Despite the high heterogeneity of patients, theoretical and empirical works converge in elements such as the value of patient-centered care, education (health literacy) in the use of new digital health technologies, mechanisms to increase patient confidence and their participation in the health decision-making processes, or the importance of collecting patients’ reported outcomes and experiences, among other elements. The review also found empty areas among theoretical and empirical studies, where no VBDH elements were identified.
Conclusion
This systematic review identified the theoretical and empirical elements to measure the value of digital health and provides a framework of VBDH elements. Some of the theoretical elements are actually used in practice. Others, however, despite being relevant from a theoretical point of view, do not seem to be measured empirically. This work provides researchers of a source, for consultation, of value based digital health elements. This is helpful for improving the measurement of the value of digital health.
Keywords: Systematic literature review, digital health, value-based digital health, value based health care, eHealth, strategic framework
Introduction
There are multiple definitions of Digital Health in the literature. Digital Health (DH) primarily focuses on healthcare in the digital world, bridging the evolution of advances in informatics and technology in medicine, health and all aspects of health care with the application of these developments in clinical practice, the patient experience, and their social, political and economic implications. The common element to all definitions of Digital Health is a digital intervention that examines the provision of healthcare and not only the use of the technology itself. 1 When referring to value of health tools, generically, in the literature this has been defined as the outcomes that are important to patients, relative to the costs required to achieve those outcomes. 2 In this study, the value of digital health will be explored, including not only looking for the value-based elements of health technologies, but any digital health resource used for the provision of health services. This is what this work understands by the concept of Value-Based Digital Health (VBDH).
The concept of Value-Based HealthCare (VBHC) was introduced by Michael Porter about fifteen years ago. 3 VBHC is currently being used as a guide for the healthcare practice towards those activities that generate the best possible health results or outcomes for each monetary unit of expenditure. The VBHC approach, thus, emphasizes the overall result of the health care process, that might be carried out on people or patients, considering the partial or complete recovery of the health state and the sustainability of that recovered health in relation to the efforts made. It has been argued, however, that the use of technology only leads to better health outcomes if the related cultural challenges are acknowledged and the new needs of patients are, actually, met. 4
Health systems are currently undergoing a digital transformation process that affects all areas of the health care process. The VBHC paradigm is evolving to a VBDH approach in many leading healthcare systems worldwide. VBHC and VBDH are closely related, both in the search for more effective and value-focused healthcare for patients. Paul Sonnier defined Digital Health as “that discipline where the digital and genomic revolutions converge with health and healthcare.” 5 However, defining the concept of VBDH and its implications is a work still in progress, but necessary, to give strength to this emerging concept, in order to help on this transformation process, by improving its quality, resilience, sustainability and innovative capacity. VBDH is, in the end, understood as the use of digital tools, solutions, strategies, and ecosystems to contribute to the generation of value in health. 6 Investigating the concept of VBDH is, thus, crucial because it optimizes healthcare and improves the efficiency of the healthcare system by focusing on outcomes that matter to patients and maximizing the use of resources.7,8
Some literature reviews have attempted to identify how VBDH is conceptualized in the literature, but these were in very specific settings,9,10 with the focus only on the economic value, and not on the effectiveness of VBDH, 11 or was done for the perspective of health professionals only. 12 No systematic literature review has, yet, approached, the concept of VBDH including all perspectives and all identifiable settings. Efforts have been also made trying to identify the degree of maturity of healthcare professionals on the use of digital health tools and technologies. Specifically, there is evidence of negative experiences due to the fact that the transformation process on this new digital changes the way some health services are provided. 2
The aim of this study is, thus, to carry out a systematic literature review on the identification of the VBDH elements.
The nature and extent of published evidence, that has linked both concepts, theoretically and empirically, is summarized into a conceptual framework of use in research and in the clinical practice.
Methods
Review design
A systematic literature review on the identification of value elements of digital health, VBDH, is the chosen method for gathering and analyze information regarding the concept of VBDH. Systematic literature reviews follow strict protocols. 13 First, the selection of at least two databases for the search was done and agreed by all authors, leading to the choice of EMBASE and Scopus as the two main databases for consultation for this work. The combination of these two databases led to a good number of records. It was considered that additional databases would need to be consulted if the selection of papers would not lead to an enough number of papers for the data extraction. This was not necessary in the end. The review method is qualitative, and targets the identification of value elements of digital health, and their description, in theoretical and empirical studies. To synthetize information, the patient journey phases (prevention, diagnosis, access to health care services, hospital/home care, specialist care, treatment and valuation/measurement of health outcomes) are used as themes, where the identified value elements will be allocated at the data extraction phase. This will, also, be analyzed by type of agent. Two researchers worked on the screening of abstracts and full texts. The data extraction method was also agreed by all authors, but was conducted by one researcher. A second researcher checked 10% of the screened abstracts, until there was agreement with the final selection and distribution among included and excluded records. This second researcher also checked the data extraction and the quality and bias assessment. The review was not registered in PROSPERO given that the initial idea was to conduct a scoping review (although in the end a full systematic review was conducted), which is a type of review that does not require registration in this system.
Search strategy
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. 14 The PICO/PECO method was applied to structure. 15 The framework of this systematic review according to PICO was: any place where the process has been studied and/or attempted to measure the value of digital transformation in the provision of health services (population); Digital transformation in health (Intervention); the elements identified in the theoretical literature vs. empirical works (comparison); theoretical elements to explain the value of digital health, and value elements of digital transformation in the provision of health services (outcomes).
The keywords of the search algorithm were combined using Boolean terms. The search strategy was conducted in EMBASE and Scopus:
((digital health OR digital healthcare OR digital health care OR digital health intervention* OR digital health technolog* OR telemedicine OR telehealth OR eHealth OR electronic health OR M-health OR mobile health) AND (value-based healthcare OR value-based health care OR value based healthcare OR value based health care)) NOT (Cost-effectiveness OR cost-utility OR cost-benefit)
Inclusion and exclusion criteria
Records were limited to any academic article or grey literature (e.g., reports from official and reliable institutions such as, for example the WHO) published since 2012 and available in full text format, in English or Spanish language, that provided relevant information about the theoretical model of the value of digital health transformation, as well as empirical works that actually measure the value of the said transformation, either for some specific digital technology, or for the set of digital health technologies in general. Articles that offered only a cost-effectiveness/utility analysis without any additional disruptive or novel measure of the value of new digital health technologies were not of interest, and were, thus, excluded.
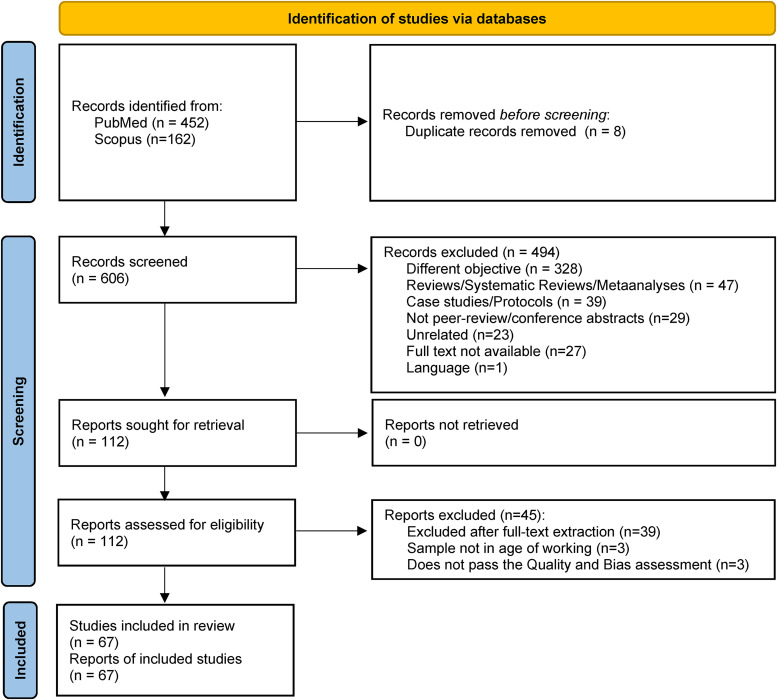
Both purely theoretical and empirical descriptive studies, well designed, or with solid econometric analysis, were admitted. For qualitative studies, it was verified that the source of the information was reliable, or that the interviewed population had knowledge at an expert level. It was not filtered by age groups, but information was extracted in relation to age (when such information was presented in the study) in the full text review phase, in order to ensure including the results of the population in working age. No criteria were set in relation to the country of study. Included papers were classified into areas of application (using the categorization of the patient journey phases). All identified exclusion criteria are detailed in PRISMA flow diagram (Figure 1).
Figure 1.
PRISMA flow diagram result of the systematic literature review.
Data extraction
The identified references were imported into Zotero, the bibliographic software used for the selection and screening of studies. The screening of studies included the exploration of titles and abstracts in a first stage, and full-texts in a second stage. The search and final selection of references were carried out in January 2024 by two researchers, who did the work in parallel and independently. Any doubts or disagreements between the two researchers regarding the selection and exclusion criteria were discussed with a third researcher. The methodology followed for data extraction was reviewed and approved by all authors.
The following information was extracted for every paper:
Paper general information: authors and year of publication, title, journal, objective and country of study.
- Information related with the study methods:
- Type of study: depending on the methods used, such as qualitative study (for studies conducting focus groups, for example), Randomized Controlled Trials, Observational studies…
- Area of study: depending on the type of patients or population involved in the study (e.g., chronicity, ophthalmology, infectious diseases…).
- Target population description.
- Randomization methods description (when applicable).
- Data information: time horizon analyzed, number of participants, % female, age information, digital health technology analyzed and its description (and same for the comparator, if there is one).
- Application or phase of the patient journey: Access to health care services, prevention, diagnosis, Hospital/clinical/home care, specialist care, Treatment, Valuing and measuring outcomes, behavioral health, and reimbursement decisions.
- Primary outcomes: here the focus was on any outcomes related with the value of digital health technologies or interventions, including (but not just) Patient Reported Outcome Measures and Patient Reported Experience Measures (PROMs and PREMs). Also, when PROMs and PREMs were evaluated, such as instruments for the measurement of Health-Related Quality of Life or satisfaction instruments, an indicator of the instrument validity was also provided.
- Methods for analysis: to make sure of the methods being appropriate for the results obtained, and make sure to keep only papers which methods are strong and analysis of enough (moderate or high) quality.
- Information regarding the study results, discussion and conclusions:
- Main results of the paper, with the focus on value elements of digital health technologies or interventions.
- Discussion of the paper: relevant aspects of the discussion, explaining the contribution of the paper.
- Paper strengths and limitations, as a complementary measure of the paper quality.
- Conclusion: summary of the main results, as a complementary field that will help to make the interpretation of what are the main or the most important findings, and, sometimes, what is suggested for further research.
A supplementary file with the data extraction is available as supplementary material.
Analysis
Papers were classified and analyzed in three categories:
Theoretical or conceptual frameworks: papers presenting a theoretical framework, discussion or commentary papers.
Empirical works: for papers making some kind of evaluation of a novel Digital Health Technology.
Theoretical and Empirical works: papers mixing theoretical and empirical methods.
Having extracted the information described above, the results regarding the value elements identified in the paper were classified, again, in three categories:
Facilitators: elements that have demonstrated positive value.
Barriers: elements that have demonstrated negative effect / value.
Neutral or uncertain: elements for which value is neutral or still uncertain, but that literature suggests exploring due to its relevance.
The analysis conducted in this study identifies, for each type of study (theoretical papers: papers that offer pure theoretical analysis, empirical studies: studies involving qualitative or quantitative data analysis, or mixed methods: for studies combining theoretical and empirical analysis), the elements for VBDH for each phase of the patient journey (access to health care services, prevention, etc.), by type of digital health technology or intervention, and by agent involved. All agents were considered, as a societal perspective was used, and this includes: health centers, stakeholders, providers, patients, health care systems, researchers and society.
Quality and risk of bias assessment
The scale to assess quality of the studies and their risk of bias was specifically elaborated for this study, similar to previous studies (such as Parmar et al. 16 ) given that there are too many observational studies and none of the existing tools looked suitable formulating the precise questions to evaluate the quality of the different type of studies. This quality and bias assessment tool was developed based on various quality assessment tools for studies of different designs. The creation of adapted tools for quality and bias assessment is considered a valuable resource for evaluating study quality in systematic literature reviews. 17 The adapted tool used here, assesses internal validity (risk of bias), external validity (applicability/variability), and reporting quality based on a set of questions/statements:
Selection bias: The sample is not representative of the population intended to be analyzed
Ecological fallacy: Logical fallacy inherent in making causal inferences from group data to individual behaviors
Confounding bias: The analysis does not account for those confounders that are expected to have an effect on the outcome and that have not been accounted for by the inclusion of other.
Reporting bias: Inappropriate or inaccurate reporting of aspects of the study
Time bias: Bias introduced owing to the timeframe considered
Measurement error in exposure variable: Errors related to the exposure variable.
Measurement error in health outcome: Errors related to the health outcome measurement.
For randomized control trials, selection bias was assessed by analyzing the appropriateness of sampling methods (power, sample size, blind design, and randomization). Those studies that provided information on the value of digital transformation in the most current context of study were considered to be of stronger quality and -at least- lesser temporal bias. The greater the distance (in years) between the time period analyzed and the time of publication, the greater was considered the risk of time bias. A greater measurement risk in our exposure variables (digital health and the value of transformation) was considered for those articles offering theoretical models not tested by empirical work, or for empirical works where the sample is too small (less than 100 for quantitative studies or less than 20 for focus groups and qualitative interviews).
For each publication, each domain of the adapted Parmar et al. scale was studied and given a score of 1 for a low risk of bias, 2 for a moderate risk and 3 for a high risk. The overall rating was calculated as follows: 1 (strong) is given if none of your domains are classified as weak, 2 (moderate) if up to two domains are classified as weak, or 3 (weak) if three or more domains are classified as weak. Records with an overall rating of 3 were finally excluded, leaving only records rated of strong and moderate quality for the final analysis.
Results
The search strategy (across titles and abstracts) identified 614 potential studies from EMBASE (452), Scopus (162). After removing duplicates 606 abstracts remained for review. Four hundred and ninety-four abstracts were excluded as a result of the titles and abstract screening phase and 112 were selected for full text screening. Documents were excluded in the data extraction phase, some because they did not offer results, others because the full text was not available, and others because they were not of enough quality or highly biased. Finally, 67 studies were included from which the detailed information was finally extracted.
A PRIMSA flowchart representing the process of selecting eligible sources for this study is presented in Figure 1. The reasons for exclusion in the screening and eligibility phases are detailed in the PRISMA. Reference lists of primary research reports and previously published systematic reviews with a focus on digital health and/or VBDH were also reviewed in an attempt to identify additional studies. Data extraction and final risk of bias and study quality assessment and scores are available as supplementary material.
Among the 67 studies fully extracted, there were 14 theoretical studies, 40 empirical studies and 13 studies combining theoretical and empirical methods. By agent type, and for each of the phases of the patient journey, the elements of VBDH were identified, and are now summarized. Each paper was allocated to one phase of the patient journey, depending, mainly, on the type of study, on main objective of the paper, and on the study setting. The areas of application identified in the analysis are now done, for each type of agent and by literature category.
Areas of VBDH identified for health care organizations
Only one paper of the theoretical literature identified VBDH elements of access to health care services for health organizations, analyzing the value of Health Information Technologies (HIT). 18
Areas of VBDH identified for stakeholders
One theoretical study found relevant VBDH elements, related to access to health care services, for stakeholders, analyzing the value of eHealth. 19
Two studies, within the mixed methods studies identified, found VBDH elements related to patients’ treatment for stakeholders, analyzing the value of Electronic Medication Adherence products and a disruptive Digital Health Technology.20,21
Areas of VBDH identified for providers
Related with access to health care services, theoretical works found the following VBDH elements. Six studies found specific value elements for providers, related with access to health services, six of them finding elements of positive value. Different technologies were analyzed, including HIT, Emerging digital health care practices, smart nursing, AI and big data, and High Definition Video-to-Video services,18,22–26 one of them finding an element of negative value, related with the burden of health care professionals. 18 Two mixed methods papers found VBDH elements, analyzing digital health communication technologies and Electronic Medical Records.27,28 Related with prevention, one empirical study identified VBDH elements for providers, of analyzing a Quitline-like phone counseling and Telemedicine integrated into Primary Care. 29 Related with diagnosis: One theoretical study analyzing imaging analysis technologies 30 and two empirical studies, on CT, imaging were identified.31,32 Related with hospital/clinical/home care, two theoretical studies identified VBDH elements for providers, analyzing mobile health and smart home devices and the Internet of Medical Things (IoMT).33,34 In addition, one empirical study, studied the value of EHR. 35 Related with specialist care, three empirical studies identified VBDH elements of telemedicine, a theory driven digital intervention, and Digital Health Monitoring Platforms for specialists.36–38 Related with treatment, one empirical study analyzed digital health technologies in general, 39 and one mixed method's paper analyzed the value of Electronic Medication Adherence products. 20 Related with the valuation and measurement of outcomes, twelve studies were found identifying VBDH elements for providers, analyzing very different digital health technologies including a Virtual Reality App, Digital Monitoring Adherence systems, Social media-based health education, AI kit, mobile apps, online telehealth, Imaging related machine learning, teleconsultation, text messaging, Machine learning techniques applied to PROMs and Digital Communication Technologies.40–51 In addition, one study, among the mixed methods included studies, identified negative VBDH elements of Electronic Health Records for this area. 44
Areas of VBDH identified for patients
Related with access to health care services: nine theoretical studies were identified, discussing VBDH elements for different types of DH technologies, including HIT, Emerging Digital health care practices, Smart nursing, AI, High Definition Video-to-Video services and eHealth.18,19,22–26 Among the empirical studies identified within this area of access to health care services, two studies were found, both analyzing VBDH elements of mHealth.52,53
Among the mixed methods studies, three studies were identified: One study, analyzing wearables, 54 a second study, analyzing a cloud-based referral platform 55 and the third study, analyzing an Integrated Digital Patient Education system. 56
Related with prevention, two empirical works identified VBDH elements for patients: one study, analyzing teleophthalmology for screening. 57 The second one, analyzing a Quitline-like phone counselling and Telemedicine integrated into Primary Care. 29
Related with diagnosis, one theoretical work was identified on the VBDH for patients of imaging analysis. 30 Empirically, one study, analyzed Breast Imaging technologies. 58
Related with treatment, three empirical papers were identified. One studied integrated care with telemedicine support. 59 The second paper, studying Digital Health Technologies. 39 The third paper, analyzing an interactive telephone intervention. 60
Related with the valuation and measurement of outcomes, thirteen empirical papers were found, identifying value elements, analyzing: a VR App, 40 telerehabilitation, 61 telehealth education, 62 a digital intervention for online help seekers, 63 a care coordination digital intervention, 64 a Digital Monitoring Adherence system, 41 a mobile phone text messaging self-managing support system,65,66 an evidence-based SDM aid, 67 a computerized intervention, 68 teleconsultation, 48 an open medication system via iPad, 69 and a Digital Communication Technology. 51 One paper among the mixed methods papers, analyzed a eHealth intervention of integrating self-report in Electronic Patient Records (eRAPID). 70
Related with behavioral health, one study, analyzing the use of wearables. 71
Areas of VBDH identified for health care systems
Related with access to health care services, seven theoretical papers identified VBDH elements for health care systems, analyzing: smart nursing, 23 Artificial Intelligence (AI), 26 High Definition Video-to-Video Services,25,72 eHealth in primary care in high and low-resource settings, 19 an electronic mindfulness-based intervention (eMBI). 73 Among mixed methods papers, one paper analyzed a cloud-based referral platform. 55
Related with diagnosis, one study among the mixed methods included studies, analyzed the value of telehealth services. 74
Related with the valuation and measurement of outcomes, one empirical paper was found, analyzing a Digital Communication Technology. 51 In addition, two papers among the mixed methods papers, were found. One, analyzing an eHealth intervention of integrating self-report in Electronic Patient Records (eRAPID), 70 and the second paper, also on Electronic Health Records. 44
Areas of VBDH identified for researchers
Theoretical works identified some positive values in the area of access to health care services for researchers: One study, discussing smart nursing, 23 the second paper, on smart home devices and the Internet of Medical Things, 33 and the third paper, discussing an electronic mindfulness-based intervention (eMBI). 73
Related with treatment, one empirical work studied the value of Digital health Technologies. 39
Areas of VBDH identified for society
Theoretical works identified elements of VBDH for the society related with access to health care services. Technologies analyzed include learning health systems, 75 emerging Digital health care practices, 22 telehealth services 72 and eHealth. 19
Related with the valuation and measurement of outcomes, three empirical papers were found, analyzing a telemedicine outreach system, 76 an mHealth ROADMAP platform, 77 an HPV Cancer Free App. 78
Related with reimbursement decisions, one theoretical analyzed telehealth and the value of digital connectivity. 79
Areas of VBDH identified for patients and providers
Theoretical works found some VBDH elements for both, patients and providers.
For the application area of access to health care services one study was found analyzing emerging digital health. 22 Another study, on Artificial Intelligence. 26 The third paper identified, discussed high definition Video-to-Video services. 25 Finally, the fourth and last identified paper, discussed eHealth. 19
Among empirical studies, some studies were found identifying VBDH elements for patient and providers in the application area of specialist care. These studies include the analysis of telemedicine (virtual visits), 36 a theory driven digital intervention, 37 or Digital Health Monitoring Platforms. 38
One study among the mixed methods studies captured VBDH elements for patients and providers, in the application area of valuation and measurement of outcomes. The study analyzed EHR. 44
Areas of VBDH identified for patients and health care systems
Theoretical works found VBDH elements for patients and health care systems, in the application area of access to health care services. One of the studies analyzed eHealth. 19 Another study, discussed health sensors, smart home devices and the Internet of Medical Things. 33
Related with valuation and measurement of outcomes, theoretical works finding VBDH elements for both, patients and Health Care Systems, were also identified: One discussing an electronic mindfulness-based intervention (eMBI), 73 a second one, analyzing a care coordination intervention, 64 and a third study, analyzing a computerized intervention. 68
Among the mixed methods studies, one paper also found VBDH elements of personal Digital Health Profile (DHP), for patients and health care systems, for the area of prevention. 80 In the area of treatment, a study found VBDH elements for health care systems and researchers analyzing a digital self-management intervention. 81
Elements of VBDH identified by the literature and conceptual framework by literature category
The detailed results and analysis for theoretical studies, empirical studies and mixed methods studies are detailed in Table s1–3, respectively.
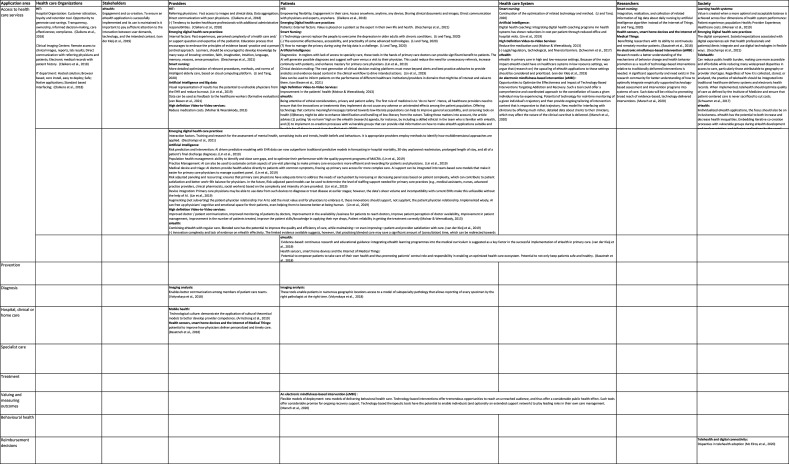
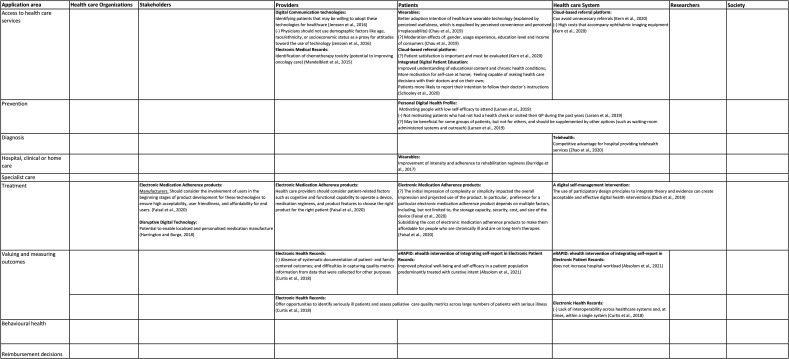
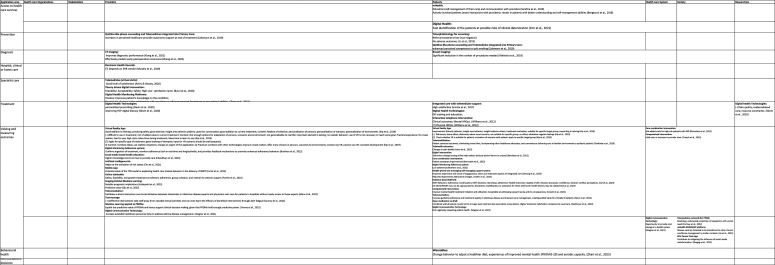
Tables 1–3 have also been of value for generating a conceptual framework, represented by Figures 2–4. The framework provides a list of VBDH elements, by type of agent and application area (phases of the patient journey) according to theoretical literature, empirical and, mixed methods literature, respectively.
Table 1.
Summary of theoretical included papers included: content and main results.
| Authors (year)/country/ type of study | Application/population/therapeutic area | Digital health intervention/description | Objective | Primary outcome/s | Summary of results (value elements by agent type) | ||
|---|---|---|---|---|---|---|---|
| Agents and positive or nonnegative effect/value (facilitators) | Agents and negative effect/value (barriers) | Agents and uncertain effect/value | |||||
| Armstrong et al. (2019) US Recommendation document |
Hospital. Clinical care. Veterans and military Several therapeutic areas |
Mobile health (mHealth) Mobile health as a mechanism for technological culture |
Describe provider- and patient-level cultural issues in the provision of clinical care in the military and veteran populations and how the development of cultural competency in technological culture can improve patient care. | Key factors are addressed when considering the cultural issues involved in the clinical integration of mobile health in the military and veteran populations. | Providers: Technological culture: demonstrate the application of cultural theoretical models to better develop provider competence. | ||
| Basatneh et al. (2018) US Discussion paper |
Home care Patients with Lower Extremity Complications of Diabetes Chronicity |
Health Sensors, Smart Home Devices, and the Internet of Medical Things The IoT covers many areas ranging from enabling technologies and components to several mechanisms that effectively integrate these low-level components. |
To better understand potential opportunities and challenges associated with implementing Internet of Medical Things (IoMT) for management of DFUs. | Discussion regarding future direction for IoMT in the care of the diabetic foot. |
Patients: Potential to empower patients to take care of their own health and thus promoting patients’ central role and responsibility in enabling an optimized health care ecosystem. Potential to not only keep patients safe and healthy. Providers: potential to improve how physicians deliver personalized and timely care. Researchers: Benefitting researchers with its ability to continuously and remotely monitor patients. |
Patients: compliance, Technology issues (e.g., battery life), and security and privacy of patient information | |
| Claikens et al. (2018) Belgium Discussion paper |
Access to health care & health care services delivery Patients using hospital based medical imaging services Several Therapeutic areas |
Health information technology (HIT) The goal of health information technology (HIT) is to improve the well-being of individuals and communities through the use of new technologies and deploying a resilient health information system (HIS), infrastructure and architecture. |
In this article we focus and discuss on the benefits-based analysis of the use of information technology in hospital based medical imaging departments. | Benefits dependency network for an IT/IS investment |
IT benefits of all the stakeholders.
|
Tendency to burden healthcare professionals with additional administrative responsibilities. | |
| Deschamps et al. (2021) UK Commentary |
Access to health care & health care services delivery (Secondary care) Podiatry patients Podiatry |
Emerging digital foot health care practices A framework that helps in portraying and defining drivers of practice, actual practice as well potential barriers for current and future practice. |
The objective of this commentary is to present a conceptual framework, namely the Value Based Digital Foot Care Framework, for use by podiatry students, lecturers, therapists, scientists and policymakers. | The proposed conceptual framework for podiatry practice utilizes the metaphor of an electronic circuit to reflect the vast and complex interconnections between factors that affect practice and professional behaviors. The framework helps in portraying and defining drivers of practice, actual practice as well potential barriers for current and future practice. The circuit emphasis the interconnectedness/interaction of three clusters: 1) internal factors, 2) interaction factors, 3) external factors. |
Providers: Internal factors: Past experiences, perceived complexity of a health care and/ or support question and expertise of the podiatrist. As they learn and develop, student podiatrists are encouraged to embrace the principles of evidence based -practice and a person-centered approach. The term person centered approach is used specifically here in order encourage podiatrists to adopt a patient care perspective that is beyond the condition and tailored to the individual/patients’ wants and needs. In addition, learners, should be encouraged to develop knowledge by many ways of knowing: emotion, faith, imagination, intuition, language, memory, reasons, sense perception). Interaction patients and providers: Interaction factors. Focuses and define the interplay between the podiatrist and the person. this may warrant review of current podiatry education and practice, with training and research into the assessment of mental health, somatising traits and trends, health beliefs and behaviors. It is appropriate podiatrists employ methods to identify how multidimensional approaches are applied, for example use of clinical (red flags) and psychosocial flags (yellow, blue and black flags) that affect outcomes for patients. Patients: External factors. Value is placed on a patient as the expert in their own life and health. Society: The digital component. Societal expectations associated with digital experiences ask that health professionals and patients/clients integrate and use digital technologies in flexible ways. |
||
| Li and Tang (2020) China Theoretical & Discussion paper |
Access to health care & health care services delivery Geriatric patients Geriatric care |
Smart geriatric nursing Smart geriatric nursing is based on the IoT technologies, sensors, big data, artificial intelligence, and many other advanced technologies in information society. |
Basing on the professional knowledge of geriatric nursing, this paper proposes a framework of smart geriatric nursing. | A framework of smart geriatric nursing that consists of three aspects of smart nursing: smart geriatric nursing in physical health using biosensor and advanced devices, smart geriatric nursing in mental health based on user profile, and smart geriatric nursing for daily life based on big data in health. |
Providers: (1) More detailed optimization of relevant procedures, methods, and norms of intelligent elderly care, based on cloud computing platform;. Researchers: (2) integration, realization, and collection of related information of big data about geriatric daily nursing by artificial intelligence algorithm instead of the Internet of Things. Healthcare system: (3) continuation of the optimization of related technology and method. |
Technology cannot replace the people to overcome the depression in older adults with chronic conditions. The economic effectiveness, accessibility, and practicality of some advanced technologies. |
How to manage the privacy during using the big data is a challenge. |
| Lin et al. (2019) US Discussion paper |
Access to health care & health care services delivery (GP/Primary Care) All patients Primary care |
Artificial Intelligence Any technology designed to mimic human cognitive functions—including techniques such as classic machine learning, modern deep learning, natural language processing, and robotics. |
This paper presents a current environmental scan, through the eyes of primary care physicians, of the top ten ways AI will impact primary care and its key stakeholders. We discuss ten distinct problem spaces and the most promising AI innovations in each, estimating potential market sizes and the Quadruple Aims that are most likely to be affected. | Top 10 ways artificial intelligence (AI) will impact primary care. |
|
AI implemented poorly risks pushing humanity to the margins; | |
| Marsch et al. (2020) US Discussion paper |
Valuing outcomes (patients) Patients with addictive behaviors Mental health |
An electronic mindfulness-based intervention (eMBI) ACHESS, a Smartphone-based recovery support system20 that is part of a larger suite of technology-based health systems known as CHESS. This tool is built on evidence-based principles of recovery support: long duration, assertive outreach, monitoring, prompts, action planning, peer and family support, and case management. Recovery support can improve health and reduce health-care use but is rarely used in addiction treatment due to limited resources for this type of care. Among ACHESS’ features focused on personalized monitoring and support to individuals in recovery are a global positioning system for letting individuals know when they are near environments that are historically high-risk areas for them, functionality to monitor one's behavior and risk factors, personal stories of recovery experiences, and links to recovery support groups. |
To describe potential models for implementing technology-based interventions targeting substance use disorders. To discuss opportunities to optimize the effectiveness and impact of technology-based interventions targeting addiction and recovery, along with outstanding research needs. | Synthesis of evidence regarding the benefits of eMBI for society, Healthcare systems, Patients, Providers and Research. |
|
||
| McElroy et al. (2020) US Commentary |
Reimbursment decisions Patients with chronic conditions Chronicity |
Telehealth and digital connectivity Telemedicine will refer to providing medical care at a distance, which includes audio–video care or audio care only. |
In this commentary, we use telehealth as an umbrella term referring to telemedicine and other health-related virtual activities, such as distance continuing medical education, training, and patient portals. Telemedicine will refer to providing medical care at a distance, which includes audio–video care or audio care only. | Telehealth, in person visits and cancelled appointments before and during the pandemic. | Healthcare system: Disparities in telehealth adoption. | ||
| Menear et al. (2019) Canada Discussion paper |
Access to health care & health care services delivery All patients All areas |
Learning health systems Value-creating framework for learning healthcare systems |
This paper presents a conceptual framework that has been developed in Canada to support the implementation of value-creating LHSs. | A conceptual framework for value-creating learning health systems | All agents of healthcare systems: Value is created when a more optimal and acceptable balance is achieved across four dimensions of health system performance: Patient experience; population Health; Provider Experience; Healthcare costs. | ||
| Molnar & Weerakkody (2013) Greece Qualitative (interviews) |
Access to health care & health care services delivery (Secondary care) Glaucoma patients Ophthalmology |
High Definition Video-to-Video Services LiveCity project: Essentially it is an application that manages bandwidth by avoiding interference from unwanted traffic and therefore ensuring that any loss of delivered data and delays are reduced. It therefore creates a virtual path over the public Internet to allow traffic (data, voice and video) to flow freely without losing quality. This ensures that signals are not interrupted by other external Internet traffic when the connection between two points of contact is established, therefore guaranteeing the transmission of high quality live video images between two points of contact. |
This paper examines the process of developing key performance indicators (KPIs) for evaluating the use of high definition video (HD) to video (V2 V) communication for tele-monitoring patients in a healthcare setting. The obtained KPIs are used to analyze the potential of using V2 V services in the context of tele-monitoring glaucoma patients. | In this respect, it is important to find out what criteria are necessary to facilitate a successful adoption of HD V2 V communication as proposed in the LiveCity project in the context of a healthcare setting. |
|
||
| Schwamm et al. (2017) US Policy statement |
Access to health care & health care services delivery (Secondary care) Cardiovascular patients Cardiovascular & Stroke conditions |
Telehealth Telehealth, as defined by Office for the Advancement of Telehealth, comprises the use of telecommunications and information technologies to share information and to provide clinical care, education, public health, and administrative services at a distance. Telehealth is a broad term that encompasses many digital health technologies, including telemedicine, eHealth, connected health, and mHealth. Telehealth is a new method of enabling care delivery that has the potential to help transform the healthcare system, to reduce costs, and to increase quality, patient-centeredness, and patient satisfaction. |
The aim of this policy statement is to provide a comprehensive review of the scientific evidence evaluating the use of telemedicine in cardiovascular and stroke care and to provide consensus policy suggestions. | Summary of evidence regarding the following aspects: 1. Effective telehealth interventions that increase access to or enhance the quality of care for CVD patients; 2. Current barriers to implementation of telehealth interventions; 3. Emerging telehealth technologies; 4. Gaps in evidence and research needs; 5. Strategies to overcome the barriers to broad dissemination of telehealth. |
|
legal/regulatory, technological, and financial barriers. | |
| van Biesen et al. (2021) Not specified Discussion paper |
Access to health care & health care services delivery All patients All areas |
Artificial Intelligence and big data A novel framework of justifiable health care and discussion on how AI and big data can contribute to achieving the goals of this framework |
The current paper presents a novel framework of justifiable health care and explores how the use of artificial intelligence and big data can contribute to achieving the goals of this framework. | A conceptual framework of justifiable healthcare |
Providers: Data can be used as feedback to the healthcare workers (formative evaluation) Patients: Data can be used to inform patients on the performance of different healthcare institutions/providers in domains that might be of interest and value to them. |
||
| van der Kleij et al. (2019) European countries Discussion paper |
Access to health care & health care services delivery (GP/Primary Care) People with complex medical and social needs in primary care. Primary care areas |
eHealth eHealth is not limited to mobile apps that can track a patient's behavior or symptoms. It encompasses communication technology that facilitates the exchange of information between primary and secondary care, or ‘big data’ research that informs the development of risk assessment tools. The first two categories of eHealth technologies, those that provide opportunities to monitor and inform and those that optimize communication, are perhaps most easily linked to the daily practice of primary care providers. However, electronic data collection to enable long-term monitoring, risk detection, and research are also essential to improve primary care. For example, a large data-mining study was able to include over 50 000 primary care patients and verify if the currently used Framingham indicators for heart failure were indeed able to predict eventual heart failure cases, years before diagnosis. |
Providing insight into the role eHealth could play in primary care, is the aim of a series on eHealth in primary care, which we will publish in the European Journal of General Practice. The series covers seven themes: 1. eHealth for primary care (this paper): concepts, conditions, and challenges 2. eHealth for primary care: addressing the ethical implications 3. Evidence-based eHealth for primary care: inclusive, individualized and blended 4. Implications of eHealth for primary care in medical education and vocational training 5. Implementation of eHealth and integration into primary care routines 6. Developing an eHealth infrastructure: the role of primary care providers 7. Global perspective: eHealth for primary care in low resource settings |
A set of Conditions to develop and implement safe and evidence-based eHealth in primary care. | Making available effective, safe and implementable eHealth applications for primary care:
|
Innovation complexity and lack of evidence on eHealth effectivity. The limited evidence available suggests, however, that practicing blended care may save a significant amount of (consultation) time, which can be redirected towards high-quality face-to-face care for those patients that need it the most. | |
| Volynskaya et al. (2018) Canada Descriptive report |
Diagnosis and Prognosis Patients from anatomic pathology and hematopathology at tertiary-care centers Personalized and Precision medicine |
Imaging analysis Multisite pathology informatics platform to support high-quality surgical pathology and hematopathology using a sophisticated laboratory information system and whole slide imaging for histology and immunohistochemistry, integrated with ancillary tools, including electron microscopy, flow cytometry, cytogenetics, and molecular diagnostics. |
To identify key requirements and establish a systematic approach to providing high-quality pathology in a publicly funded health care system that is responsible for services across a large geographic area that includes a heavily populated urban metropolis, large suburban communities, and remote towns that serve as hubs for large rural areas with scattered populations. |
A model of subspecialty pathology that allows reporting of every specimen by the right pathologist at the right time. |
Patients: 1-These tools enable patients in numerous geographic locations access to a model of subspecialty pathology that allows reporting of every specimen by the right pathologist at the right time; Providers: 2-Enables better communication among members of patient care teams. |
||
Table 3.
Summary of papers mixing theoretical and empirical methods included: content and main results.
| Authors (year)/country/type of study | Application/population/area | Objective | Time horizon of data analyzed | Number of participants/% female/age information | Technology/digital health intervention | Primary Outcome/s | PROMs or PREMs validated measures? | Summary of results (value elements by agent type) | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Positive or nonnegative effect/value (facilitators) | Negative effect/value (barriers) | Uncertain effect/value | ||||||||
| Absolom et al. (2021) UK Prospective, randomized two-arm parallel group study |
Valuing outcomes (patients) Cancer patients Oncology |
Can we control better treatment- and disease-related symptoms during chemotherapy by introducing online monitoring with patient-reported outcome measures, uniquely combined with automated algorithm-driven severity-dependent patient advice? | January 22, 2015-June 11, 2018 | 508 79.9% mean = 56.0 (SD = 11.8) |
eRAPID: eHealth Intervention During Chemotherapy. Immediate integration of the self-reports in electronic patient records (EPRs) facilitated clinical use. | PROMs: Symptom control measured by using the Functional Assessment of Cancer Therapy Scale-General Physical Well-Being subscale (FACT-PWB, scores 0–28, high scores 5 better symptoms) | YES |
Patients: Improved physical well-being and self-efficacy in a patient population predominantly treated with curative intent, Healthcare system: does not increase hospital workload. |
||
| Burridge et al. (2017) UK Overview study |
Home care Upper Limb poststroke spasticity patients Stroke care |
This article addresses the need for cost-effective increased intensity of practice and suggests potential benefits of telehealth (TH) as an innovative model of care in physical therapy. | Not mentioned | Not applicable Not applicable Not applicable |
A web supporting program (LifeCIT): wearable sensors; M-Mark |
Feasibility was assessed by retention and adherence (duration of C-Mitt wear, activities, and use of the Web site). The Wolf Motor Function Test (WFMT) and the Motor Activity Log (MAL) (a self-assessment tool that measures about amount and quality of use of the affected upper limb) PREMs: Views and experience of using the Web site and wearing the CMitt. Safety: measured by documentation of adverse and serious adverse events and reported following standard procedures for each rehabilitation center. The economic impact (use of health and social care) of the LifeCIT intervention compared with usual care was examined using the Client Service Receipt Inventory. |
YES | Patients: Improvement of intensity and adherence to rehabilitation regimens. | ||
| Chau et al. (2019) China Conceptual framework and survey |
Access to health care & health care services delivery Respondents with experience of healthcare wearable technology Unspecified |
To gain knowledge in this area and provide meaningful managerial implications for practitioners and wearable device developers. | October 1st 2018, to January 5th 2019 | 171 45% mean = 26–30 years (ranging from 18 to 65) |
Healthcare wearable devices assisting users to check their health status as well as planning their exercises | Adoption intention of healthcare wearable technology | YES | Patients: better adoption intention of healthcare wearable technology (explained by perceived usefulness, which is expalined by perceived convenience and perceived irreplaceability). | Moderation effects of: gender, usage experience, education level and income of consumers | |
| Curtis et al. (2018) US Narrative review and description |
Valuing outcomes (population-based) Seriously ill patient population Palliative care |
We examine use of the electronic health record (EHR) as a tool to assess quality of serious illness care through narrative review and description of a palliative care quality metrics program in a large healthcare system. | 2010–2015 | 105 43% mean = 65.5 (SD = 15.1) |
Electronic Health Records | A summary of the strengths and weaknesses of the EHR. A discussion of opportunities and challenges. |
NOT ALL | Patients and providers: Offer opportunities to identify seriously ill patients and assess palliative care quality metrics across large numbers of patients with serious illness. |
Healthcare systems: Lack of interoperability across healthcare systems and, at times, within a single system; Providers: absence of systematic documentation of patient- and family-centered outcomes; and difficulties in capturing quality metrics information from data that were collected for other purposes. |
|
| Dack et al. (2019) UK Focus groups and Interview |
Treatment (self-management) Diabetes patients Chronic diseases |
To describe the development process and content of a digital self-management intervention for people with type 2 diabetes (HeLP-Diabetes) that has been found to achieve its target clinical outcome, the reduction of HbA1c, a measure of glycemic control. | 2011–2016 | 20 patients with T2DM and 18 Health care professionals Patients: 40% ; Healthcare professionals: 61.1% Patients: mean age = 56.8 (range 36–77) Healthcare professionals: mean age = 49 (range 32–64) |
A digital self-management intervention (HeLP-Diabetes) | PREMs: Questions regarding patients understanding of the condition, how to self-manage it, where to get information or how to get treatment | YES | Research and Healthcare systems: The use of participatory design principles to integrate theory and evidence can create acceptable and effective digital health interventions. | ||
| Faisal et al. (2020) Canada Mixed-methods approach |
Treatment (adherence) Older adults, caregivers, and health care providers Unspecified |
The aim of this study is to examine user experience with electronic medication adherence products, with particular emphasis on features, usefulness, and preferences. | August-December 2018 | 37 (20 older adults; 5 caregivers; 11 HCP) Older adults: 52%; Caregivers: 20%; HCP: 82% Older adults: mean = 75 (range 65–87); Caregivers: mean = 73 (range 69–79); HCP: not reported |
Electronic medication adherence products | PREMs: Identification of themes regarding users’ experiences with focus on features, usefulness, and preferences |
Providers: Health care providers should consider patient-related factors such as cognitive and functional capability to operate a device, medication regimens, and product features to choose the right product for the right patient. Stakeholders (Manufacturers): should consider the involvement of users in the beginning stages of product development for these technologies to ensure high acceptability, user friendliness, and affordability for end users. Stakeholders (Policy makers): should consider subsidizing the cost of electronic medication adherence products to make them affordable for people who are chronically ill and are on long-term therapies |
Patients: The initial impression of complexity or simplicity impacted the overall impression and projected use of the product. In particular, preference for a particular electronic medication adherence product depends on multiple factors, including, but not limited to, the storage capacity, security, cost, and size of the device. |
||
| Harrington and Burge (2018) UK Mix of literature review and qualitative study (interviews) |
Treatment Patients with chronic conditions Chronicity |
The aim of this paper is to define operating principles and protocols in a variety of healthcare contexts where there is a specific focus on service transformation, enabled by a series of emerging manufacturing paradigms and novel business model concepts. | 2016 | Not mentioned Not mentioned Not mentioned |
Disruptive digital technologies | A Digital value network: conceptual model development based on results from a literature review and interviews. The conceptual model includes:
|
Manufacturers: Potential to enable localized and personalized medication manufacture. | |||
| Jenssen et al. (2016) US National Survey |
Access to health care & health care services delivery Primary care patients Primary care |
We assessed patient attitudes regarding technology use to communicate with their primary care team or to engage with other patients outside typical office settings. | November - December 2012 | 3064 49.8% 18–60 |
Digital Communication technologies | Attitudes on the use of digital technology (email, text messaging, and social media such as Facebook and Twitter) to communicate with primary care teams about health behavior goals and test results. We also assessed attitudes toward the use of digital technologies to engage with other patients in activities such as peer coaching. | YES | Providers: identifying patients that may be willing to adopt these technologies for healthcare |
Providers: Physicians should not use demographic factors like age, race/ethnicity, or socioeconomic status as a proxy for attitudes toward the use of technology |
|
| Kern et al. (2020) UK Retrospective cohort study |
Access to health care & health care services delivery (Secondary care) Patients classified into the HES referral pathway by contributing optometrists have been included into this study. Ophtalmology |
To report the implementation and initial results of a cloud-based referral platform to medical retina HES, which was developed to overcome the increasing demand on scarce ophthalmologist services by improving communication between opticians and ophthalmologists. | April 2018 to January 2019 | 107 53% mean =66.9 (SD = 18, range: 23–95) |
A cloud-based referral platform |
|
Not applicable (does not measure PROMs or PREMs) | Healthcare systems: Can avoid unnecessary referrals |
Health care system: High costs that accompany ophthalmic imaging equipment |
Patients: Patient satisfaction is important and must be evaluated |
| Larsen et al. (2019) Denmark Intervention |
Prevention Chronic patients at primary care Chronicity |
The present paper examines individual characteristics and health-care usage of patients who took up the targeted preventive programs in response to their personal digital health profile. | May 2016 to December 2016. | 2661 56% mean = 45.4 |
Personal digital health profile | Attendance to the preventive programs | YES | Patients and Healthcare systems: Motivating people with low self-efficacy to attend | Patients and healthcare systems: Not motivating patients who had not had a health check or visited their GP during the past years | Patients and Healthcare systems: May be beneficial for some groups of patients, but not for others, and should be supplemented by other options (such as waiting-room administered systems and outreach). |
| Mandelblatt et al. (2015) US Observational study |
Access to health care & health care services delivery (Secondary care) Women with breast cancer Oncology |
We developed and conducted preliminary evaluation of an algorithm to detect grade 3 and 4 toxicities using electronic data from a large integrated managed care organization. | 2006–2009 | 1575 Not mentioned Most participants <65 |
Electronic medical records and administrative data | Having vs not having toxicity | Not applicable (does not measure PROMs or PREMs) | Providers and Patients: Identification of chemotherapy toxicity (potential to improving oncology care). | ||
| Schooley et al. (2020) US Mixed-methods approach (Survey and interviews) |
Access to health care & health care services delivery (Secondary care) Patients who were counseled using a blended digital health education Chronicity |
The goal of this study was to address the need for blended learning strategies combining technical and workflow integration of digital patient education systems for patients with chronic conditions within and across the regular process of care. Studies are needed to evaluate the utility and benefits of these technologies for providers and patients alike. | October 2017 to May 2018 | 178 56.7% Aged 18 years or older |
Integrated Digital Patient Education (mobile devices, interactive media, 3-dimensional images, and multimedia educational content at the bedside.) | Patient understanding, patient motivation for self-care, patient confidence in care decision making, clinician-patient communication, and patient's intention to follow instructions. | YES |
Patients: 1-Improved understanding of educational content and chronic health conditions; 2-More motivation for self-care at home; 3-Feeling capable of making health care decisions with their doctors and on their own; 4-Pastients more likely to report their intention to follow their doctor's instructions. |
||
| Zhao et al. (2020) US Cross-sectional analysis using census data from acute care hospitals |
Hospital/Clinical care Acute care patients Acute care |
The aim of this study was to examine the association between alternative payment models (APMs), market competition, and telehealth provisions in the hospital setting. | 2018 | 4257 (hospitals) Not applicable Not applicable |
Telehealth | Provision rates of Telehealth services | Not applicable (does not measure PROMs or PREMs) | Health care systems: Competitive advantage for hospital providing telehealth services | ||
Figure 2.
Framework of value elements by agent type and application area of the patient journey according to theoretical literature.
Figure 4.
Value elements by agent type and application area of the patient journey according to mixed methods literature.
Figure 3.
Framework of value elements by agent type and application area of the patient journey according to empirical literature.
Table 2.
Summary of empirical papers included papers included: content and main results.
| Authors (year)/country/type of study | Application/population/area | Time horizon of data analyzed | Number of participants/% female/age information | Technology/digital health intervention | PROMs or PREMs validated measures? | Summary of results (value elements by agent type) | ||
|---|---|---|---|---|---|---|---|---|
| Positive or nonnegative effect/value (facilitators) | Negative effect/value (barriers) | Uncertain effect/value | ||||||
| Li et al. (2015) US Prospective Randomized Study |
Prevention Population with suspected macular degeneration or stable but nonactive AMD Oftalmology |
November 2011 - November 2012 | 106 61.1% mean age = 81.1 |
Teleoftalmology for screening of age related Macular degeneration | Not mentioned |
Patients: Referral treatment time. No adverse outcomes. |
Healthcare systems and Patients: Monitoring recurrence: increased waiting times. |
|
| Vlahiotis et al. (2018) US Projections |
Diagnosis Adult (aged 18 + years) females who had at least one medical claim for a breast imaging or breast diagnostic procedure Breast procedures |
2011–2015 | 875526 100% mean age = 52.5 |
Breast imaging and diagnostic procedures | Not applicable (does not measure PROMs or PREMs) |
Patients and Healthcare system: Significant reduction in the number of procedures needed. |
||
| Kim et al. (2021) Korea Cohort study |
Access to health care & health care services delivery 1) patients < 65 years with COVID-19, 2) patients without underlying medical comorbidities, and 3) COVID-19 disease severity of mild class. Infectious diseases |
Mar 3, 2020, to Mar 26, 2020 | 290 64.1% median age = 37 |
Digital health (monitoring system): Smartphone app combined with personal health record platform | Not applicable (does not measure PROMs or PREMs) |
Patients and Healthcare systems: Fast identification of the patients at possible risks of clinical deterioration |
||
| Serafica et al. (2019) Hawaii Qualitative: focus groups |
Access to health care & health care services delivery Patients, their family supporters and significant others, and healthcare providers of a clinic that is the only federally qualified health center and safetynet service provider. Nursing and healthcare practice |
Not mentioned | 19 29% mean age = 59.43 (SD = 5.16) |
Mobile health technologies | Not applicable (does not measure PROMs or PREMs) | Patients: Education (self-management of their care) and communication with providers | ||
| Bengtsson et al. (2018) Sweden Qualitative, explorative study |
Access to health care & health care services delivery (GP/Primary Care) Patients being medically treated for hypertension; (2) over 30 years of age and (3) able to understand and read Swedish. Blood diseases |
Not mentioned | 20 55% median = 63.5 (range 43–72) |
Mobile phone self-management support system | YES | Patients: Actively involved patients (more interactions with providers): results in patients with better understanding and self-management abilities | ||
| Ashry & Alsawy (2020) Egypt Clinical data collection & Questionnaire |
Specialist Patients above 18 years and those who agreed to participate in telemedicine visits and patients who experienced a smooth postoperative course in the hospital and not expected to have complications. Neurosurgery |
March-April 2020 | 32 37.5% mean age = 38.8 (range 18–65) |
Telemedicine (virtual) visits | NO |
Patients and Providers: Good level of satisfaction of patients and providers |
||
| Bucci et al. (2018) England Intervention: Implementation and test of efficacy and safety |
Specialist Early psychosis patients. Mental health |
2015–2017 | 36 50% Actissist: mean age = 20.21 (SD = 7.37) ClinTouch: mean age = 18.33 (SD = 7) |
Theory-driven digital intervention: Actissist | YES | Patients: Feasibility; Acceptability; Safety; High user satisfaction level. | ||
| Zhen et al. (2021) US & Canada Survey analysis |
Specialist IBD patients Digestive diseases |
March 1, 2018 to September 30, 2018 | 32 37.5% median = 28.5 (IQR: 22–38) |
Digital Health Monitoring platforms | YES |
Patients: Positive: Improves patient's knowledge on the condition; Neutral: No changes in the relationship with providers or self-management (treatment or prevention) abilities. |
||
| Murphy et al. (2020) US Cross-sectional |
Hospital care Acute care hospitals that attested to participation in the MU program and also participated in the Hospital Value-Based Purchasing Program (HVBP) Acute care |
January 1 to December 31, 2016 | 2362 (hospitals) NA NA |
Electronic health records | YES | Providers: Depends on EHR vendor | ||
| Inoriza et al. (2017) Spain Prospective study of two paralell cohorts |
Treatment (integrated care) Diabetic patients Chronicity |
Julio 2013-Septiembre 2014 | 126 35.70% Cases: mean age = 63.9 (SD = 14.9) Control: mean age = 63.4 (SD = 15.5) |
Integrated care with telemedicine support program | YES |
Patients: High satisfaction obtained by users. |
||
| Slevin et al. (2020) Ireland Qualitative study (interviews) |
Treatment (provision) COPD patients Chronicity |
Not mentioned | 32 (clinicians) Not mentioned Not mentioned |
Digital Health Technologies | NO | Patients: DH training and education; improving HCP digital literacy; Providers: personalized prescribing | Researchers: Data quality; evidence-based care; resource constraints. | |
| Williams et al. (2012) Australia RCT |
Treatment (provision) Type 2 diabetes patients Chronicity |
July 2008 and December 2010 | 120 Not mentioned mean age = 57.4 (SD = 8.3) |
Interactive telephone intervention | YES | Patients: Positive: Clinical outcomes; Mental HRQoL. | Patients: Physical HRQoL | |
| Kip et al. (2019) The Netherlands Semistructured interviews (online questionnaire) |
Valuing outcomes (patients) Mental health patients, therapists and other stakeholders Mental health |
Not mentioned | 146 60.95% Patients: mean age = 41.53 (SD = 7.37) Therapists working in forensic mental health: mean age = 38.79 (SD = 12.51) Other stakeholders: mean age = 43.95 (SD = 14.01) |
Virtual Reality (VR) Application | YES |
Providers: Good addition to therapy; practicing safely; good exercise; insight into behavior patient; cause for conversation; good addition to current treatment; Content: Realism of behavior; personalization of persons; personalization of scenario; personalization of environment; Patients: Improvement (future) behavior; insight own behavior; insight behavior others; treatment motivation; suitable for specific target group; supporting in reliving; |
Providers: difficult to use in treatment; not of added value to current treatment; Content: Not enough options for adaptation of persons, scenarios and environment; not generalizable to real life; important element is lacking; no realistic behavior; use of VR is not necessary to reach same goal. Practical experience: No visual realism; hard to use; high costs; takes time during treatment; takes time to learn to use. Patients: Dishonesty about effect; dishonesty about input scenario; not suitable for specific group; no effect; elicitation negative feelings. |
Providers: Apply for specific type of treatment; good training of therapist; input for VR scenario should be well-prepared; 3) Content: Combine ideas; use realistic situations; change an aspect of the application; 4) Practical: Combine with other technologies; improve visual realism; offer many choices in persons, scenarios & environments; context use VR; posture use VR; constant development Patients: Check whether VR is suitable for patient; cocreation of scenario with patient; apply to specific target group; |
| Tenforde et al. (2020) US Observational |
Valuing outcomes (patients) Patients under telerehabilitation Rehabilitation patients |
During COVID-19 pandemic (time not specified) | 205 53.7% Most participants in age of working, although it also includes children and people >65. |
Telerehabilitation techniques | NO (but survey developed with experts) | Patients: Patient centered outcomes; eliminating travel time, incorporating other healthcare advocates, and convenience delivering care in familiar environment to pediatric patients. | ||
| Liebmann et al. (2019) US RCT |
Prevention Rural smokers Substance abuse disorders |
June, 2009 through June, 2011 | 560 66.9% mean age = 47.51 (SD = 12.96) |
Quitline-like phone counseling (QL) and telemedicine integrated into primary care (ITM) | YES |
Providers: increases in perceived healthcare provider autonomy support at end of treatment Patients: enhanced perceived competence to quit smoking |
||
| Ashar et al. (2022) US RCT |
Valuing outcomes (patients) Patients with chronic conditions Chronicity |
August 2017 to November 2018, with 1-year follow-up completed by November 2019 | 151 54% mean age = 41.1 (SD = 15.6, range 21–70) |
Telehealth education session | YES | Patients: Changes in pain beliefs | ||
| Bendtsen et al. (2022) Sweden RCT |
Valuing outcomes Risky drinkers Substance abuse disorders |
Between 25/04/2019 and 26/11/2020 | 2129 (intervention: 1063, control: 1066) 58% > = 18 |
Digital Intervention | YES | Patients: Behavior change among online help seekers (reduce alcohol harms in society) | ||
| Berinstein et al. (2022) US RCT |
Valuing outcomes (patients) High risk IBD patients Chronicity |
January 2019 to January 2020 | 205 (Intervention: n = 100; usual care: n = 105) 65.85% Usual care group: mean age = 48.35 (SD = 17.76) Care Coordination group: mean age = 46.69 (SD = 17.07) Range 18–90 |
Care coordination intervention: Proactive symptom monitoring and care coordinator-enabled triggered algorithms | YES |
Patients: Patient symptoms improve Healthcare system and society: not added costs for high-risk patients with IBD |
||
| Brothers et al. (2022) US RCT |
Valuing outcomes (Prevention) Young men that have sex with men PrEP |
Not mentioned | 100 3% (transgender) mean age = 21.9 (SD = 2.00, range 16–24) |
Digital monitoring adherence system (Proteus discover) | YES | Providers: Confirms ingestion of treatment, monitors adherence both in real-time and longitudinally, and provides feedback mechanisms to promote enhanced adherence behaviors for YMSM. | Patients: Low adherence | |
| Chaudhary et al. (2023) Nepal RCT |
Valuing outcomes (patients) Pregnant women Postnatal care |
May to August, 2021 | 229 100% mean age = 26.2 (SD = 3.93) |
Digital education: Social media-based health education | YES | Providers: higher knowledge scores on how to provide care | ||
| Cheung et al. (2023) Australia RCT |
Valuing outcomes (patients) Diabetes or Coronoary Heart Disease patients Chronic diseases |
2014–2015 | 902 28.5% mean age = 61.5 (SD = 11.6, >=18) |
Mobile phone text messaging self-management support system | YES | Patients: Improves experience and sense of engagement, which are important aspects of integrated care | ||
| Chu et al. (2021) China Cohort study |
Valuing outcomes (patients) Gastrointestinal stromal tumor patients Oncology |
June 2013–2019 | 292 56.1% mean age = 61 (SD = 12, range 29–90) |
Artificial Intelligence kit | Not applicable (does not measure PROMs or PREMs) | Providers: Helps on the evaluation of risk status | ||
| Col et al. (2023) US RCT |
Valuing outcomes (patients) Multiple sclerosis patients Multiple Sclerosis |
November 11, 2019 and October 23, 2020 | 501 84.6% mean age = 48.4 years (SD = 11, range 19–78) |
Evidence-based SDM aid | YES |
Patients: 1-DMT Behaviors: Adherence, Continuation. 2-DMT decisions: Start/stop, adherence. 3-Health Outcomes: Quality of Life. 4-Decision processes: confidence, decision conflict, perceptions. |
Patients: MS-SUPPORT may not be appropriate for all patients; modifications or assistance for those with lower health literacy may be needed | |
| Collier et al. (2024) Sweden RCT |
Valuing outcomes (patients) Swedish adults seeking help online to reduce their alcohol consumption. Substance abuse disorders |
Between 25/04/2019 and 26/11/2020 | 1063 in the intervention group and 475 in the responders group 42% Intervention group: mean age = 45 (range 35–55) Responders group: mean age = 48 (range 40–57) |
Digital Intervention: Text message | YES |
Patients: Reported Experiences. Behavioral changes. |
||
| Creech et al. (2022) US RCT |
Valuing outcomes (patients) Women with histories of sexual assault PTSD |
May, 2017, through April, 2019 | 153 100% mean age = 43.55 (SD = 10.10) |
Computerized Intervention | YES |
Patients: Improve mental health treatment initiation and utilization; Acceptable at addressing sexual trauma and its consequences. Healthcare systems: Little cost or increase in provider time. |
||
| Curtis et al. (2022) US RCT |
Valuing outcomes (health professionals) Health professions SBIRT trainees Substance abuse disorders |
Two 10-week cohorts; one cohort in Fall 2016 and the second in Spring 2017 | 131 Not mentioned Not mentioned |
SBIRT mobile app | YES | Providers: Potential value of the TPB model in explaining health care trainee behavior in the delivery of SBIRT | ||
| Fortier et al. (2022) US RCT |
Valuing outcomes (veterans) Post-9/11 veterans PTSD |
Not specified (but during COVID-19 pandemic). | 74 17.56% mean age = 41.0 (SD = 11.5, range 24–65) |
Online telehealth delivery | YES | Patients: Safety, feasibility, and greater treatment enrollment, adherence, group cohesion, and veteran-to-veteran support | ||
| Fortney et al. (2022) US RCT |
Valuing outcomes (patients) Veterans with a PTSD diagnosis who were receiving care at a CBOC, but not engaged in specialty mental healthcare at the VAMC. PTSD |
April 2016 to July 2019 | 447 9.7% mean age = 51.8 (SD = 15.0) |
Telemedicine Outreach for PTSD | YES | Society: Reaching a substantial proportion of population with unmet need | ||
| Jia et al. (2021) China RCT |
Valuing outcomes (patients) Diabetes patients Chronic diseases |
2017–2019 | 17554 59.8% mean age = 60.5 (SD = 8.4) |
mHealth ROADMAP platform | Not applicable (does not measure PROMs or PREMs) | Society: Disease control; Potential to be transferred to other chronic conditions management in similar contexts. | ||
| Kobayashi et al. (2022) France Cohort study |
Valuing outcomes (patients) STANISLAS cohort Prevention |
2011–2015 | 1705 51.8% mean age = 60.0 (SD = 5.0) |
Cardiovascular Imaging-Related Machine Learning | Not applicable (does not measure PROMs or PREMs) | Providers: a new evidence-driven, integrated classification of individuals in preclinical settings with plausible circulating biomarkers and notable prognostic implications | ||
| Marx et al. (2022) Germany RCT |
Valuing outcomes (patients) Adult Patients in intensive care with infectious diseases or possible infectious presentation Infectious diseases |
February 2017 to January 2020 | 159424 Inpatient group: 53% Outpatient group: 45.3% Inpatient group: mean age = 69; Outpatient group: mean age = 42 |
Expert TeleconsultationsPlus Advanced Training Courses | Not applicable (does not measure PROMs or PREMs) |
Providers: facilitates a direct interaction over broad distances between intensivists or infectious disease experts and physicians who care for patients in hospitals without ready access to these experts. Patients: increase guideline adherence and treatment quality in infectious disease and intensive care management, creating added value for critically ill patients. |
||
| Qiu et al. (2022) China Retrospective cohort study |
Valuing outcomes (patients) Type 2 diabetes patients Chronic diseases |
June 2021-December 2022 | 149 37.5% Training group. Normal bone mass group: mean = 54 (SD = 9.7); Abnormal bone mass group: mean = 65.5 (SD = 9.3); Validation group. Normal bone mass group: mean = 56.2 (SD = 8.6); Abnormal bone mass group: mean = 68.1 (SD = 11.7) |
CT images | Not applicable (does not measure PROMs or PREMs) | Providers: Predictive value | ||
| Sacarny et al. (2022) US RCT |
Valuing outcomes (patients) Patient with prescription of opioids or benzodiazepines Substance abuse disorders |
June 2019 to March 2021 | 2237 57% mean age = 48% (SD = 16) |
Text message | Not applicable (does not measure PROMs or PREMs) | Providers: Ineffective interventions take staff away from valuable clinical activities and can even harm the efficacy of beneficial interventions through alert fatigue | ||
| Shegog et al. (2022) US RCT |
Valuing outcomes (behaviors) Parents of 11–17 year old male and female patients Vaccines |
September 2017 through March 2019 | 57084 50.6% mean age = 13.5 (SD = 2.2) |
HPVcancerFree app (HPVCF) | Not applicable (does not measure PROMs or PREMs) | Society: Contribute to mitigating the influence of social media misinformation. | ||
| Stuhlreyer et al. (2022) Germany RCT |
Valuing outcomes (patients) Total knee Replacement patients Trauma surgery |
October 2015 to March 2019 | 96 58% mean age = 68 (SD = 9) |
APP: Open medication via the iPad app | YES | Patients: Combined with physician rounds led to stronger pain relief and less oxycodone consumption. Higher treatment satisfaction compared to usual care. | ||
| Verma et al. (2022) Denmark and The Netherlands RCT and Observational study |
Valuing outcomes (patients) Nonspecific neck and/or low back pain Neck and Back pain |
dataset 1: 2019–2020 dataset 2: 2012–2019 |
dataset 1: 218 ; dataset 2: 159 Not mentioned Not mentioned |
ML methods applied to PROMs data | YES | Providers: Exploit the predictive value of PROMs and hence support clinical decision making, given that PROMs hold enough predictive power. | ||
| Wagner et al. (2021) US RCT |
Valuing outcomes (patients) Asthma patients Respiratory diseases |
February 2017 and August 2018 | 14978 Not mentioned Not mentioned |
Digital Communication Technology | Not applicable (does not measure PROMs or PREMs) |
Providers: Increase available healthcare personnel time to address asthma disease management. Healthcare systems: Opportunity to provide cost savings in a health system Patients: Not negatively impacting patient health. |
||
| Xiong et al. (2021) China Retrospective study |
Diagnosis Patients evaluated for pulmonary ground-glass nodules Oncology |
November 2012 and June 2018 | 198 60.1% median age = 61 (IQR = 54–66) |
CT images | Not applicable (does not measure PROMs or PREMs) | Providers: Improves diagnostic performance | ||
| Zhart et al. (2023) US RCT |
Behavior and health Community-dwelling adults Healthy individuals |
September 2017 and September 2019 | 162 Not mentioned Not mentioned |
Wearables: Apple Watch (Apple Inc.)/Meta-Mindset Intervention | YES | Patients: Change behavior to adopt a healthier diet; experiences of improved mental health (PROMIS-29) and aerobic capacity. | ||
| Zheng et al. (2023) China RCT |
Diagnosis. (Predictive modeling) Patients diagnosed with combined hepatocellular-cholangiocarcinoma (cHCC-CC). Oncology |
January 1, 2012, to December 31, 2020 | 143 28.6% Not mentioned |
CT images | Not applicable (does not measure PROMs or PREMs) | Providers: Effectively predicts early postoperative recurrence | ||
Discussion
This systematic literature review helped identifying, from the most relevant sources published in recent years, those elements that, according to theory, would be relevant to creating digital health value. Through the extraction of information from the reviewed sources, literature was synthetized in a way that VBDH elements can be identified at different levels (by phases of the patient journey), for different agents (in the society) and by type of digital health technology and intervention.
The review also helped identifying the elements that are actually being used to measure the value of digital health empirically. For example, to generate value in the access phase and provision of health services, theoretical and empirical literature coincide in elements such as research, education, patient-centered care, or trust. While theory proposes as an important element the government's regulatory and acting capacity, the empirical works reviewed do not present any type of measure that correspond to this approach. In relation to the diagnosis phase, for example, only the theoretical literature finds as key elements for this phase of the care process the importance of models by pathologies or pathological subspecialties, and of agile transmission, centered on the patient, 30 something that has not yet been studied empirically. Related with the prevention of diseases, hospital care and treatment phases, this study did not find any elements in the theoretical literature, while empirically the existence of certain elements that serve to demonstrate the value of digital health in these areas is being demonstrated. On the valuation and measurement of health outcomes, theoretical literature suggests the need for restructuring of medical practice, which should tend towards more flexible implementation models, 73 while the empirical literature reviewed does not find anything in this regard. However, coinciding elements in this phase are the importance of research (in this case focused on data collection, especially PROMs and PREMs), the importance of feasibility and confidence in new technologies, and the importance of information systems that allow identifying barriers to optimize the effectiveness of interventions based on new health technologies.
There were some common elements found between several of the different phases of the care cycle, such as the importance of patient-centered care. However, no theoretical article focused on the prevention and treatment phases has been identified, suggesting further research could focus on identifying such VBDH elements. Future research should study this context, as these phases of the patient's care cycle should be given the same importance than any other phase.
The main contribution of this study is to offer the VBDH elements identified in the literature (separately by theoretical and empirical works), by type of agent and for the different phases of a patient journey. Previous publication exists, providing a framework for defining Value-Based Health Care. A paper published recently, offers a strategic framework for VBHC implementation to achieve better patient outcomes. 82 An umbrella review was done for the value of mobile health applications used in patients with mental health problems. 83 However, no framework has been proposed yet to identify specific elements of VBHC in the context of Digital Health. Another paper reviewed how digital transformation can help achieve VBHC, 84 supporting the fact that Determining “value” may require a system-level model and framework to understand better the distributed components that are interrelated by complex processes within a healthcare system. Something that has already been a concern by researchers in the field. 85 Therefore, this systematic review is a novel and useful piece of information for researchers who may want to develop, for example, new instruments of patient reported outcomes or experiences regarding the use of different digital health technologies. The framework proposed, result of the synthesis of information extracted, offered by this review, despite its complexity due to the multiple levels of analysis considered, identifies areas where no VBDH elements are identified, and therefore could also be useful for researchers who may be wondering what areas of application are still in need for further research in this sense. Finally, the data extraction could also be used as a data lake (easy to update) of VBDH interventions, for example, helping in the design of research projects in different areas of application.
This study has limitations. The main limitation is on the subjectivity of the interpretation of results offered by the literature, for example, when allocating the value of a digital technology to a specific phase of the patient journey or for a particular type of agent. However, the interpretation of the results was reviewed by all authors, and the final version has the agreement of all authors of this study. Any other limitations are natural of the methods for conducting any systematic literature review. It may be the case that relevant papers have been excluded in the screening phases of the review, and also it is possible that evaluating the quality and risk of bias of the selected studies, some papers qualified as weak (and thus, excluded) could be relevant papers for the purposes of this study.
Conclusion
This systematic literature review provides a framework composed of the main elements, for each phase of a patient's care cycle, that generate value for digital health technologies and interventions. Furthermore, contrasting the elements identified in theory and empirical work in the context of VBDH, the review shows a list of elements that coincide between both types of literature, as well as some existing gaps in the literature. This work, therefore, offers elements that build up a strategic framework, with empirically observed elements for VBDH, as well as suggests future lines of research that should be priorities for progress in VBDH. It provides researchers of a source, for consultation and development of future research projects, that might be useful for academic researchers as well as a tool to be used by clinicians in the clinical practice or by policy makers in decision making processes in the context of digital health. Conditioned to the existence of instruments to measure the value of these elements, this is a first step for improving the measurement of the value of digital health.
Supplemental Material
Supplemental material, sj-xlsx-1-dhj-10.1177_20552076241277438 for Value-based digital health: A systematic literature review of the value elements of digital health care by Marisa Merino, Jaime del Barrio, Roberto Nuño and María Errea in DIGITAL HEALTH
Supplemental material, sj-docx-2-dhj-10.1177_20552076241277438 for Value-based digital health: A systematic literature review of the value elements of digital health care by Marisa Merino, Jaime del Barrio, Roberto Nuño and María Errea in DIGITAL HEALTH
Footnotes
Conflicting interests: ME has received consulting fees for her working time. Marisa Merino and Jaime del Barrio belong to ASD but their authorship has not biased the results obtained in any way.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by Asociación Salud Digital.
Authors’ Contributions: MM and JdB conceived the study idea. The research question was refined by ME. All authors agreed on the research objectives and study protocol. ME searched the databases for literature and MM and ME screened the abstracts. ME reviewed full texts, supervised by MM and RN. ME wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Guarantor: MM
ORCID iD: María Errea https://orcid.org/0000-0002-2192-0266
Supplemental material: Supplemental material for this article is available online.
References
- 1.Ibrahim MS, Mohamed Yusoff H, Abu Bakar YI, et al. Digital health for quality healthcare: a systematic mapping of review studies. Digital Health 2022; 8: 205520762210858. Available at: http://journals.sagepub.com/doi/10.1177/20552076221085810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nuño-Solinís R, Urizar E, Merino M, et al. Validation study of a value-based digital health questionnaire. Int J Environ Res Public Health 2022; 19: 7034. Available from: https://www.mdpi.com/1660-4601/19/12/7034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Porter ME. What is value in health care? N Engl J Med 2010; 363: 2477–2481. Available at: https://www.nejm.org/doi/10.1056/NEJMp1011024. [DOI] [PubMed] [Google Scholar]
- 4.Meskó B, Drobni Z, Bényei É, et al. Digital health is a cultural transformation of traditional healthcare. Mhealth 2017; 3: 38. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5682364/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sonnier P. The fourth wave: Digital health—a new era of human progress. Independently Published 2017. Available at: https://storyofdigitalhealth.com/book [Google Scholar]
- 6.Asociación Salud Digital. Salud Digital Basada en Valor: ¿Dónde estamos y dónde queremos estar?. 2021. Available at: https://salud-digital.es/wp-content/uploads/2021/07/Informe-SDBV.pdf.
- 7.Porter ME, Lee TH. The strategy that will fix health care. Harv Bus Rev 2013; 91: 50–70. Available at: https://hbr.org/2013/10/the-strategy-that-will-fix-health-care23898735 [Google Scholar]
- 8.Kaplan RS, Porter ME. The big idea: how to solve the cost crisis in health care. Harv Bus Rev 2011; 89: 46–52. Available at: https://hbr.org/2011/09/how-to-solve-the-cost-crisis-in-health-care [PubMed] [Google Scholar]
- 9.van Staalduinen DJ, van den Bekerom P, Groeneveld S, et al. The implementation of value-based healthcare: a scoping review. BMC Health Serv Res 2022; 22: 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buntin MB, Burke MF, Hoaglin MCet al. et al. The benefits of health information technology: a review of the recent literature shows predominantly positive results. Health Aff (Millwood) 2011; 30: 464–471. [DOI] [PubMed] [Google Scholar]
- 11.Zanotto BS, Etges AdS, Marcolino MAZet al. et al. Value-based healthcare initiatives in practice: a systematic review. J Healthc Manag 2021; 66: 340. Available at: https://journals.lww.com/jhmonline/fulltext/2021/10000/value_based_healthcare_initiatives_in_practice__a.5.aspx. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van Engen V, Bonfrer I, Ahaus Ket al. et al. Value-based healthcare from the perspective of the healthcare professional: a systematic literature review. Front Public Health 2022; 9, Available at: https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2021.800702/full. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Charrois TL. Systematic reviews: What do you need to know to get started? Can J Hosp Pharm 2015; 68: 144–148. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4414076/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J 2021: n71. Available at: https://www.bmj.com/content/372/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Higgins JPT, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions. John Wiley & Sons, Ltd., 2019. [Google Scholar]
- 16.Parmar D, Stavropoulou C, Ioannidis JPA. Health outcomes during the 2008 financial crisis in Europe: systematic literature review. Br Med J 2016; 354: i4588. Available at: https://www.bmj.com/content/354/bmj.i4588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Whiting P, Wolff R, Mallett S, et al. A proposed framework for developing quality assessment tools. Syst Rev 2017; 6: 04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Claikens BL. Delivering value from the digital integration in medical imaging centers in healthcare organizations. J Belgian Soc Radiol 2018; 102: 1. Available at: http://jbsr.be/articles/10.5334/jbr-btr.1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van der Kleij RMJJ, Kasteleyn MJ, Meijer E, et al. SERIES: eHealth in primary care. Part 1: Concepts, conditions and challenges. Europ J General Pract 2019; 25: 179–189. doi: 10.1080/13814788.2019.1658190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Faisal S, Ivo J, McDougall Aet al. et al. Stakeholder feedback of electronic medication adherence products: Qualitative analysis. J Med Internet Res 22(12), e18074. 2020. doi: 10.2196/18074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harrington TS, Burge TA. Connecting digital pharma and e-healthcare value networks through product-service design: a conceptual model. Int J Electronic Healthcare 2018; 10: 96–129. [Google Scholar]
- 22.Deschamps K, Brabants A, Nester C, et al. A conceptual framework for contemporary professional foot care practice: ‘The value based digital foot care framework’. J Foot Ankle Res 2021; 14: 22. Available at: https://jfootankleres.biomedcentral.com/articles/10.1186/s13047-021-00465-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li S, Tang Y. A simple framework of smart geriatric nursing considering health big data and user profile. Comput Math Methods Med 2020; 2020: 1–9. Available at: https://www.hindawi.com/journals/cmmm/2020/5013249/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van Biesen W, Van Der Straeten C, Sterckx S, et al. The concept of justifiable healthcare and how big data can help us to achieve it. BMC Med Inform Decis Mak 2021; 21: 87. Available at: https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-021-01444-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Molnar A, Weerakkody V. Defining key performance indicators for evaluating the use of high definition video-to-video services in eHealth. In: Papadopoulos H, Andreou AS, Iliadis L, Maglogiannis I. (eds) Artificial intelligence applications and innovations. Berlin, Heidelberg: Springer Berlin Heidelberg, 2013, pp.452–461. (IFIP Advances in Information and Communication Technology; vol. 412). Available at: http://link.springer.com/10.1007/978-3-642-41142-7_46. [Google Scholar]
- 26.Lin SY, Mahoney MR, Sinsky CA. Ten ways artificial intelligence will transform primary care. J Gen Intern Med 2019; 34: 1626–1630. Available at: http://link.springer.com/10.1007/s11606-019-05035-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jenssen BP, Mitra N, Shah A, et al. Using digital technology to engage and communicate with patients: A survey of patient attitudes. J Gen Intern Med 2016; 31: 85–92. Available at: http://link.springer.com/10.1007/s11606-015-3517-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mandelblatt JS, Huang K, Makgoeng SB, et al. Preliminary development and evaluation of an algorithm to identify breast cancer chemotherapy toxicities using electronic medical records and administrative data. J Oncol Pract 2015; 11: e1–e8. doi: 10.1200/JOP.2013.001288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liebmann EP, Preacher KJ, Richter KP, et al. Identifying pathways to quitting smoking via telemedicine-delivered care. Health Psychol 2019; 38: 638. doi: 10.1037/hea0000740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Volynskaya Z, Chow H, Evans A, et al. Integrated pathology informatics enables high-quality personalized and precision medicine: Digital pathology and beyond. Arch Pathol Lab Med 2018; 142: 369–382. Available at: http://meridian.allenpress.com/aplm/article/142/3/369/103035/Integrated-Pathology-Informatics-Enables. [DOI] [PubMed] [Google Scholar]
- 31.Xiong Z, Jiang Y, Che S, et al. Use of CT radiomics to differentiate minimally invasive adenocarcinomas and invasive adenocarcinomas presenting as pure ground-glass nodules larger than 10 mm. Eur J Radiol 2021; 141: 109772. [DOI] [PubMed] [Google Scholar]
- 32.Zheng C, Gu XT, Huang XL, et al. Nomogram based on clinical and preoperative CT features for predicting the early recurrence of combined hepatocellular-cholangiocarcinoma: A multicenter study. Radiol Med 2023; 128: 1460–1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Basatneh R, Najafi B, Armstrong DG. Health sensors, smart home devices, and the internet of medical things: An opportunity for dramatic improvement in care for the lower extremity complications of diabetes. J Diabetes Sci Technol 2018; 12: 577–586. Available at: http://journals.sagepub.com/doi/10.1177/1932296818768618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Armstrong CM, Ortigo KM, Avery-Leaf SNet al. et al. Cultural considerations in using mobile health in clinical care with military and veteran populations. Psychol Serv 2019; 16: 276. doi: 10.1037/ser0000252 [DOI] [PubMed] [Google Scholar]
- 35.Murphy ZR, Wang J, Boland MV. Association of electronic health record use above meaningful use thresholds with hospital quality and safety outcomes. JAMA Netw Open 2020; 3: e2012529. Available at: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2770283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ashry AH, Alsawy MF. Doctor-patient distancing: An early experience of telemedicine for postoperative neurosurgical care in the time of COVID-19. J Neurol 2020; 56: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bucci S, Barrowclough C, Ainsworth J, et al. Actissist: Proof-of-concept trial of a theory-driven digital intervention for psychosis. Schizophr Bull 2018; 44: 1070–1080. doi: 10.1093/schbul/sby032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhen J, Marshall JK, Nguyen GC, et al. Impact of digital health monitoring in the management of inflammatory bowel disease. J Med Syst 2021; 45: 23. Available at: http://link.springer.com/10.1007/s10916-021-01706-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Slevin P, Kessie T, Cullen J, et al. Exploring the barriers and facilitators for the use of digital health technologies for the management of COPD: A qualitative study of clinician perceptions. QJM 2020; 113: 163–172. [DOI] [PubMed] [Google Scholar]
- 40.Kip H, Kelders SM, Van Gemert-Pijnen LJEWC. Putting the value in VR: how to systematically and iteratively develop a value-based VR application with a Complex target group. In: Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems, Glasgow Scotland, UK, 2019, pp.1–12: ACM. Available at: https://dl.acm.org/doi/10.1145/3290605.3300365 [Google Scholar]
- 41.Brothers J, Hosek S, Keckler K, et al. The ATEAM study: Advances in technology to enhance PrEP adherence monitoring (ATEAM) among young men who have sex with men. Clin Transl Sci 2022; 15: 2947–2957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chaudhary K, Nepal J, Shrestha K, et al. Effect of a social media-based health education program on postnatal care (PNC) knowledge among pregnant women using smartphones in Dhulikhel hospital: A randomized controlled trial. PLoS One 2023; 18: e0280622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chu H, Pang P, He J, et al. Value of radiomics model based on enhanced computed tomography in risk grade prediction of gastrointestinal stromal tumors. Sci Rep 2021; 11: 12009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Curtis JR, Sathitratanacheewin S, Starks H, et al. Using electronic health records for quality measurement and accountability in care of the seriously ill: Opportunities and challenges. J Palliat Med 2018; 21: S-52–S-60. Available at: http://www.liebertpub.com/doi/10.1089/jpm.2017.0542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fortier CB, Currao A, Kenna A, et al. Online telehealth delivery of group mental health treatment is safe, feasible, and increases enrollment and attendance in post-9/11 U.S. veterans. Behav Ther 2022; 53: 469–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kobayashi M, Huttin O, Magnusson M, et al. Machine learning-derived echocardiographic phenotypes predict heart failure incidence in asymptomatic individuals. JACC Cardiovasc Imaging 2022; 15: 193–208. [DOI] [PubMed] [Google Scholar]
- 47.Qiu H, Yang H, Yang Z, et al. The value of radiomics to predict abnormal bone mass in type 2 diabetes mellitus patients based on CT imaging for paravertebral muscles. Front Endocrinol (Lausanne 2022; 13: 963246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Marx G, Greiner W, Juhra C, et al. An innovative telemedical network to improve infectious disease management in critically ill patients and outpatients (TELnet@NRW): Stepped-wedge cluster randomized controlled trial. J Med Internet Res 2022; 24: e34098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sacarny A, Safran E, Steffel M, et al. Effect of pharmacist email alerts on concurrent prescribing of opioids and benzodiazepines by prescribers and primary care managers: A randomized clinical trial. JAMA Health Forum 2022; 3: e223378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Verma D, Jansen D, Bach K, et al. Exploratory application of machine learning methods on patient reported data in the development of supervised models for predicting outcomes. BMC Med Inform Decis Mak 2022; 22: 227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wagner NM, Ritzwoller DP, Raebel MA, et al. Can digital communication technology reduce health system personnel time? An evaluation of personnel requirements and costs in a randomized controlled trial. Transl Behav Med 2021; 11: 863–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bengtsson U, Kjellgren K, Hallberg I, et al. Patient contributions during primary care consultations for hypertension after self-reporting via a mobile phone self-management support system. Scand J Prim Health Care 2018; 36: 70–79. doi: 10.1080/02813432.2018.1426144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Serafica R, Inouye J, Lukkahatai N, et al. The use of mobile health to assist self-management and access to services in a rural community. Comput Inform Nurs 2019; 37: 62–72. doi: 10.1097/CIN.0000000000000494 [DOI] [PubMed] [Google Scholar]
- 54.Chau KY, Lam MHS, Cheung ML, et al. Smart technology for healthcare: Exploring the antecedents of adoption intention of healthcare wearable technology. Health Psych Res 2019; 7. Available at: https://www.pagepressjournals.org/index.php/hpr/article/view/8099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kern C, Fu DJ, Kortuem K, et al. Implementation of a cloud-based referral platform in ophthalmology: Making telemedicine services a reality in eye care. Br J Ophthalmol 2020; 104: 312–317. Available at: https://bjo.bmj.com/content/104/3/312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schooley B, Singh A, Hikmet N, et al. Integrated digital patient education at the bedside for patients with chronic conditions: Observational study. JMIR Mhealth Uhealth 2020; 8: e22947. Available at: http://mhealth.jmir.org/2020/12/e22947/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Li B, Powell AM, Hooper PLet al. et al. Prospective evaluation of teleophthalmology in screening and recurrence monitoring of neovascular age-related macular degeneration: A randomized clinical trial. JAMA Ophthalmol 2015; 133: 276. Available at: http://archopht.jamanetwork.com/article.aspx?doi=10.1001/jamaophthalmol.2014.5014. [DOI] [PubMed] [Google Scholar]
- 58.Vlahiotis A, Griffin B, Stavros ATet al. et al. Analysis of utilization patterns and associated costs of the breast imaging and diagnostic procedures after screening mammography. CEOR 2018; 10: 157–167. Available at: https://www.dovepress.com/analysis-of-utilization-patterns-and-associated-costs-of-the-breast-im-peer-reviewed-article-CEOR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Inoriza JM, Ibanez A, Perez-Berruezo X, et al. Effectiveness and economic impact of a program of integrated care with telemedicine support on insulin-treated type 2 diabetic patients (Study GITDIABE). Aten Primaria 2017; 46: 131–139. doi: 10.1016/j.aprim.2016.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Williams ED, Bird D, Forbes AW, et al. Randomised controlled trial of an automated, interactive telephone intervention (TLC diabetes) to improve type 2 diabetes management: Baseline findings and six-month outcomes. BMC Public Health 2012; 12: 602. Available at: http://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-12-602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tenforde AS, Borgstrom H, Polich G, et al. Outpatient physical, occupational, and speech therapy synchronous telemedicine: A survey study of patient satisfaction with virtual visits during the COVID-19 pandemic. J Physic Med 2020; 99: 977–981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ashar YK, Gordon A, Schubiner H, et al. Effect of pain reprocessing therapy vs placebo and usual care for patients with chronic back pain: A randomized clinical trial. JAMA Psychiatry 2022; 79: 13–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bendtsen M, Åsberg K, McCambridge J. Effectiveness of a digital intervention versus alcohol information for online help-seekers in Sweden: A randomised controlled trial. BMC Med 2022; 20: 176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Berinstein JA, Cohen-Mekelburg SA, Greenberg GM, et al. A care coordination intervention improves symptoms but not charges in high-risk patients with inflammatory bowel disease. Clin Gastroenterol Hepatol 2022; 20: 1029–1038.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cheung NW, Redfern J, Thiagalingam A, et al. Effect of mobile phone text messaging self-management support for patients with diabetes or coronary heart disease in a chronic disease management program (SupportMe) on blood pressure: Pragmatic randomized controlled trial. J Med Internet Res 2023; 25: e38275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Collier ES, Blomqvist J, Bendtsen M. Satisfaction with a digital support tool targeting alcohol consumption: Perspectives from participants in a randomized control trial. Alcohol Alcohol 2024; 59: agad070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Col NF, Solomon AJ, Alvarez E, et al. Implementing shared decision-making for multiple sclerosis: The MS-SUPPORT tool. Mult Scler Relat Disord 2023; 80: 105092. [DOI] [PubMed] [Google Scholar]
- 68.Creech SK, Pulverman CS, Kahler CW, et al. Computerized intervention in primary care for women veterans with sexual assault histories and psychosocial health risks: A randomized clinical trial. J Gen Intern Med 2022; 37: 1097–1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Stuhlreyer J, Roder C, Krug F, et al. A digital application and augmented physician rounds reduce postoperative pain and opioid consumption after primary total knee replacement (TKR): A randomized clinical trial. BMC Med 2022; 20: 469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Absolom K, Warrington L, Hudson E, et al. Phase III randomized controlled trial of eRAPID: eHealth intervention during chemotherapy. J Clin Oncol 2021; 39: 734–747. doi: 10.1200/JCO.20.02015 [DOI] [PubMed] [Google Scholar]
- 71.Zahrt OH, Evans K, Murnane E, et al. Effects of wearable fitness trackers and activity adequacy mindsets on affect, behavior, and health: Longitudinal randomized controlled trial. J Med Internet Res 2023; 25: e40529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Schwamm LH, Chumbler N, Brown E, et al. Recommendations for the implementation of telehealth in cardiovascular and stroke care: A policy statement from the American heart association. Circulation 2017; 135: e24–e44. doi: 10.1161/CIR.0000000000000475 [DOI] [PubMed] [Google Scholar]
- 73.Marsch LA. Leveraging technology to enhance addiction treatment and recovery. J Addict Dis 2012; 31: 313–318. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3650640/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zhao M, Hamadi H, Haley DR, et al. Telehealth: Advances in alternative payment models. Telemedicine and e-Health 2020; 26: 1492–1499. Available at: https://www.liebertpub.com/doi/10.1089/tmj.2019.0294. [DOI] [PubMed] [Google Scholar]
- 75.Menear M, Blanchette MA, Demers-Payette Oet al. et al. A framework for value-creating learning health systems. Health Res Policy Sys 2019; 17: 79. Available at: https://health-policy-systems.biomedcentral.com/articles/10.1186/s12961-019-0477-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fortney JC, Rajan S, Reisinger HS, et al. Deploying a telemedicine collaborative care intervention for posttraumatic stress disorder in the U.S. department of veterans affairs: A stepped wedge evaluation of an adaptive implementation strategy. Gen Hosp Psychiatry 2022; 77: 109–117. [DOI] [PubMed] [Google Scholar]
- 77.Jia W, Zhang P, Zhu D, et al. Evaluation of an mHealth-enabled hierarchical diabetes management intervention in primary care in China (ROADMAP): A cluster randomized trial. PLoS Med 2021; 18: e1003754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Shegog R, Savas LS, Healy CM, et al. AVPCancerfree: Impact of a digital behavior change intervention on parental HPV vaccine -related perceptions and behaviors. Hum Vaccin Immunother 2022; 18: 2087430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.McElroy JA, Day TM, Becevic M. The influence of telehealth for better health across communities. Prev Chronic Dis 2020; 17: 200254. Available at: http://www.cdc.gov/pcd/issues/2020/20_0254.htm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Larsen LB, Sondergaard J, Thomsen JI, et al. Step-wise approach to prevention of chronic diseases in the Danish primary care sector with the use of a personal digital health profile and targeted follow-up - an assessment of attendance. BMC Public Health 2019; 19: 1–14. doi: 10.1186/s12889-019-7419-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Dack C, Ross J, Stevenson F, et al. A digital self-management intervention for adults with type 2 diabetes: Combining theory, data and participatory design to develop HeLP-Diabetes. Internet Interv 2019; 17: 100241. doi: 10.1016/j.invent.2019.100241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Teisberg E, Wallace S, O’Hara S. Defining and implementing value-based health care: A strategic framework. Acad Med 2020; 95: 682–685. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7185050/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Koh J, Tng GYQ, Hartanto A. Potential and pitfalls of mobile mental health apps in traditional treatment: An umbrella review. J Pers Med 2022; 12. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9505389/. doi: 10.3390/jpm12091376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rosalia RA, Wahba K, Milevska-Kostova N. How digital transformation can help achieve value-based healthcare: Balkans as a case in point. The Lancet Regional Health – Europe 2021; 4. Available at: https://www.thelancet.com/journals/lanepe/article/PIIS2666-7762(21)00077-6/fulltext. doi: 10.1016/j.lanepe.2021.100100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zeigler B, Traoré M, Zacharewicz Get al. et al. Value-based learning healthcare systems: Integrative modeling and simulation (healthcare technologies). Institution of Engineering and Technology, 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-xlsx-1-dhj-10.1177_20552076241277438 for Value-based digital health: A systematic literature review of the value elements of digital health care by Marisa Merino, Jaime del Barrio, Roberto Nuño and María Errea in DIGITAL HEALTH
Supplemental material, sj-docx-2-dhj-10.1177_20552076241277438 for Value-based digital health: A systematic literature review of the value elements of digital health care by Marisa Merino, Jaime del Barrio, Roberto Nuño and María Errea in DIGITAL HEALTH