Abstract
Background
The association between Attention-deficit hyperactivity disorder (ADHD) and suicidality has been subject of growing interest for research in the latest years. Suicidality was generally assessed categorically and without the use of validated instruments, leading to heterogeneous or even conflicting evidence. The prevalence of both suicidal ideation and attempts varies considerably, and the associated risk factors remain unclear. Our study investigated suicidality in ADHD using a dimensional approach and a validated and internationally recognized instrument. Our primary aim was to evaluate the prevalence of suicidal ideation (SI), severe suicidal ideation (SSI), suicidal behavior (SB) and non suicidal self-injury behavior (NSSIB) in a sample of adult patients with ADHD. The second objective was to identify sociodemographic and clinical features associated with increased risk of suicidality in these patients.
Methods
The sample included 74 adult patients with clinical diagnosis of ADHD. Suicidality was assessed by administering the Columbia-Suicide Severity Rating Scale. Logistic regressions were used to examine predictors of SI, SSI, SB and NSSIB.
Results
The lifetime prevalence of SI and SSI were 59.5% and 16.2%, respectively. The 9.5% of patients showed lifetime SB, while NSSIB was found in 10.8% of the subjects. Lifetime SI was associated with severity of inattentive symptoms during adulthood, low self-esteem and impairment in social functioning. Lifetime SSI appeared related to severity of inattentive symptoms during childhood, attentional impulsiveness and number of hospitalizations, while physical activity appeared to be protective. The prevalence of lifetime SB and NSSIB did not appear significantly related to any socio-demographic or clinical feature.
Conclusions
Adults with ADHD should be considered at risk of suicide and it is important to determine which patients are at higher risk, in order to guide preventive interventions. The association between ADHD and suicidal ideation did not appear to be influenced by psychiatric comorbidities, but rather by inattention itself, which represents the core symptom of ADHD.
Keywords: Attention-deficit hyperactivity disorder, Suicidal ideation, Suicidal behavior, Suicide attempts, Risk factors
Introduction
Attention-deficit hyperactivity disorder (ADHD) is a neurodevelopmental condition that begins in childhood and frequently persists into adulthood [1]. ADHD has an estimated prevalence of 4–7% in childhood [2] and of 2.5% in adulthood [3]. ADHD symptoms encompass inattention and hyperactivity, as well as impulsivity and difficulties in emotional regulation [4]. Furthermore, ADHD often co-occurs with other psychiatric disorders such as mood disorders, substance use disorder and personality disorders [5].
Consequently, the link between ADHD and suicidality has garnered significant research interest in recent years. When discussing suicidality, we refer to a complex phenomenon that includes suicidal ideation (SI), severe suicidal ideation (SSI), suicidal behavior (SB) and non suicidal self-injury behavior (NSSIB). According to a recent meta-analysis, lifetime SI and SB prevalences in ADHD adult patients are 40% and 18.9%, respectively [6].
Nevertheless, several limitations have led to heterogeneous or even conflicting findings in the literature. The first methodological limitation lies in the conceptualization and categorical assessment of suicidality, as suicide is a complex and dynamic phenomenon that goes from SI to SB. Thus, specific evaluation tools, like the Columbia-Suicide Severity Rating Scale (C-SSRS), are needed as they enable a dimensional analysis of suicidality 7 [4]. Nonetheless, most research on suicidality in ADHD has employed open-ended questions or questionnaires that were neither specifically designed nor validated for this purpose, or solely relied on diagnostic codes to assess suicidality. We identified only three studies involving adult patients where the C-SSRS or other validated instruments were used [8–10].
Furthermore, while several studies documented the incidence of suicide attempts in ADHD, there is a lack of evidence on other dimensions of suicidality, such as SI, and on clinical or sociodemographic features which may moderate the risk for suicide in ADHD.
Considering the heterogeneous clinical presentation (which, especially in adults, goes far beyond inattention and hyperactivity), the evolving nature of the symptoms, and the high prevalences of psychiatric comorbidities that could complicate or delay the detection of the disease, ADHD diagnosis represents a challenge for clinicians [11, 12]. Furthermore, it is known that certain dimensions of psychiatric disorders (such as specific affective temperaments, coping strategies and defense mechanisms) represent risk factors for suicidality, independently from the disease itself [13, 14]. For these reasons, it should be important to assess ADHD patients following a dimensional approach, as many of dimensions of ADHD could affect the risk of complications [15, 16]. However, most of the studies available not only do not take into account these dimensions, but also do not rely on clinical diagnosis. Indeed, certain studies did not employ clinical or diagnostic interviews, relying exclusively on non-specific screening tools, diagnostic codes, or stimulant prescriptions to identify patients with ADHD [9, 17, 18]. Furthermore, a substantial portion of the research focused solely on male or underage patients, as well as specific populations (such as prison inmates, substance abusers, and individuals with learning disabilities) [19–21].
These methodological limitations and differences in studies design and samples make the results difficult to interpret and compare, besides generating a considerable variability between the results themselves. In literature lifetime SB in adult ADHD patients rates range from 9.1% [21] to 51.5% [22], while lifetime SI rates range from 15.8% [23] to 66.3% [20].
Some researchers have examined risk factors for suicidality in ADHD, with gender being one of the most widely explored factors. The majority of studies have indicated a higher risk of both suicidal ideation (SI) and suicidal behavior (SB), but not of completed suicide, in adult females with ADHD [17, 24–26]. On the other hand, no significant differences were found among underage patients [28, 29].
Few data regarding the potential impact on suicidality of other important dimensions, such as age at diagnosis, symptom severity, ADHD subtype, related symptoms and impulsiveness, is available. Only recently, a meta-analysis underlined ADHD symptoms severity and persistence, family history of ADHD, parental influences and social functioning as risk factors for suicidality in adult patients with ADHD [24].
Concerning the potential influence of psychiatric comorbidities on the relationship between ADHD and suicidality, Septier and colleagues conducted a meta-analysis that highlighted an association largely independent of such variables (including psychiatric comorbidities) [6]. Other studies have suggested a generally significant association even when adjusting for socio-demographic and clinical factors [17, 19, 25]. However, some studies did not replicate these findings [8, 9, 20, 30]. Therefore, the prevalence of suicidality in ADHD and factors related remain unclear, as it remains controversial whether this association is direct or mediated by psychiatric comorbidities.
Our study investigated suicidality in ADHD using a dimensional approach and a validated and internationally recognized instrument. Our primary aim was to evaluate the prevalence of SI, SSI, SB, and NSSIB in a sample of adult patients with ADHD. The second objective was to identify sociodemographic and clinical features associated with increased risk of suicidality in these patients.
To achieve these objectives, we recruited a sample of adult patients with ADHD assessed with a dimensional approach, aiming to overcome, or at least mitigate, the aforementioned methodological limitations. Regarding the sample size, it is important to note that ADHD is a highly specialized topic, and its diagnosis and treatment in Italy can only be carried out by licensed psychiatrists. Therefore, referring patients with ADHD is not as straightforward as with other psychiatric disorders, and this must be taken into account when considering the sample sizes of studies (which is usually smaller than for other disorders).
A better understanding of not only the prevalence of suicidality in ADHD, but also whether it is influenced by other psychiatric disorders or certain clinical dimensions of ADHD, could help identify patients at risk of suicide and, consequently, aid in its prevention.
Materials and methods
Study design and sample
This is a cross-sectional observational study on 74 adults outpatients with a diagnosis of ADHD. The patients were consecutively enrolled at the regional reference center for ADHD in the Psychiatry Unit of San Luigi Gonzaga University Hospital, Orbassano (Turin) from September 2023 to March 2024.
Aims and procedures were explained to all the enrolled patients. Inclusion criteria were: ≥ 18 years of age, diagnosis of ADHD according to DSM-5-TR criteria [31], written consent before participation Exclusion criteria were underage and refusal to participation. The study protocol was approved by the local Ethical Committees with number 939.140 The study was conducted in accordance with the Helsinki Declaration, as amended by the 64th WMA General Assembly in Fortaleza, Brazil, in October 2013.
Assessment
Patients were assessed through a semi-structured interview administered upon the patient’s arrival at our clinic, during four outpatient visits (ranging from 3 to 5, depending on the complexity of the clinical picture and the availability of both the patients and their caregivers). Patients were clinically assessed by a trained psychiatrist, with the help of specific and validated tests. In detail, the semi-structured interview explored the following areas:
1) Sociodemographic data: age, sex, marital status, occupational status and education level;
2) Clinical features of ADHD: ADHD subtype; severity of symptoms in childhood and in adulthood (according to the “Diagnostic Interview for ADHD in adults” - DIVA, administered in the presence of a caregiver) [32]; current occurrence of symptoms (measured through ADHD rating scale IV – ADHD-RS IV) [33]; impulsiveness (measured through “Barratt Impulsiveness Scale” – BIS-11) [34]; ADHD related symptoms (such as mood swings, anger outbursts, low self-esteem, low tolerance for frustrations, sleep onset insomnia); areas of functional impairment (according to DIVA Criterion C); age at ADHD diagnosis; age at first ADHD treatment; family history of psychiatric disorders; physical activity, intensity of physical activity (≤ 3 h per week, 3–5 h per week, and ≥ 5 h per week).
3) Psychiatric comorbidities: the Italian version of the Structured Clinical Interview for DSM-5 Axis I Disorders (SCID-5) [35] was administered to assess psychiatric comorbidities, while personality status was evaluated clinically and using the Millon Clinical Multiaxial Inventory (MCMI-III) [36]. DSM-IV-TR Diagnoses were updated to meet the DSM-5-TR criteria [31].
4) Suicidality: the Italian version of the Columbia-Suicide Severity Rating Scale (C-SSRS) Lifetime/Recent version [7] was administrated to all the patients who met the criteria for ADHD diagnosis. C-SSRS consists of four subscales which explore SI severity, SI intensity, SB and lethality. SI severity ranges from 1 (wish to be dead) to 5 (active suicidal ideation with specific plan and intent). The SI intensity subscale explores frequency, duration, controllability, deterrents and reasons for SI. The third subscale includes SB (actual, interrupted and aborted suicide attempts, preparatory behaviors for a suicide attempt) and NSSIB. For our purpose, as other studies previously did [37, 38], lifetime SI was considered a score ≥ 1 on the severity subscale, while lifetime SSI was considered a severity score ≥ 4. This dichotomization relies on the assumption that the intent to act could be a predictive factor for future SB [7], allowing the identification of high-risk patients. Lifetime SB was considered a score ≥ 1 on the behavior subscale, as other studies previously did [7, 37]. This dichotomy was based on the fact that engaging in suicidal acts is associated with an increased risk of subsequent suicide attempts [39]. NSSIB was examined with a specific item on the behavior subscale.
Statistical analysis
The sociodemographic and clinical features of the participants were summarized as mean and SD for continuous variables and as frequency and percentage for categorical variables. We tested the distribution of continuous variables using the Kolmogorov-Smirnov test.
The sample was divided, one at a time, in the following subgroups:
ADHD with SI (score ≥ 1 on the suicidal severity subscale) vs. ADHD without SI (score = 0);
ADHD with SSI (score ≥ 4 on the suicidal severity subscale) vs. ADHD without SSI (score < 4);
ADHD with SB (preparatory acts or aborted/interrupted/actual attempts) vs. ADHD without SB;
ADHD with NSSIB vs. ADHD without NSSIB.
Considering that the distribution was not normal (P < 0.001), comparisons were performed using χ2 tests for categorical variables and Kruskal-Wallis H test for continuous variables.
Binary logistic regression was used to identify explanatory variables related with lifetime SI/SSI/SB/NSSIB, considering the presence of lifetime SI/SSI/SB/NSSIB as the dependent variable. Significant variables were selected using a forward stepwise procedure. To be included in the equation, a probability of 0.05 was required. The group comparison results were presented as two-sided p-values rounded to three decimal places. The criterion for statistical significance in all comparison was a p value < 0.05.
All statistical analyses were performed by SPSS software version 29.0.1.0, IBM Inc., Armonk, New York.
Results
A total of 74 adult patients with a diagnosis of ADHD were enrolled in the study. The sample’s demographic and clinical features are shown in Table 1.
Table 1.
Sociodemographic and clinical characteristics of the total sample (n = 74)
| Sex, n (%) | |
|
Male Female |
50 (67.6) 24 (32.4) |
| Age, mean (SD) | 30.05 (10.8) |
| Marital status, n (%) | |
|
Single Married Separated Widowed |
61 (82.4) 11 (14.9) 2 (2.7) 0 (0) |
| Education (years), mean (SD) | 12.8 (3.4) |
| Paid employment, n (%) | |
|
Yes No |
56 (75.7) 18 (24.3) |
| Family history of psychiatric disorders, n (%) | 30 (41.1) |
| Family history of ADHD, n (%) | |
|
Yes No |
9 (12.2) 65 (87.8) |
| Adult ADHD subtype, n (%) | |
|
Inattentive subtype Combined subtype |
32 (43.2) 42 (56.8) |
| Age at diagnosis (years), mean (SD) | 25.9 (11) |
| Age at first ADHD treatment (years), mean (SD) | 26.1 (10.3) |
| Ongoing ADHD treatment at assessment, n (%) | 22 (29.7) |
| DIVA 2.0, mean (SD) | |
|
Inattentive symptoms in childhood Hyperactivity symptoms in childhood Inattentive symptoms in adulthood Hyperactivity symptoms in adulthood |
7.4 (1.1) 5.2 (2.9) 7.4 (1.2) 5.54 (2.5) |
| ADHD-RS, mean (SD) | 36 (8.6) |
|
BIS-11, mean (SD) Attentional impulsiveness Motor impulsiveness Non-planning impulsiveness |
70.4 (11.6) 20.3 (4) 22.5 (4.7) 27.6 (5.2) |
| Lifetime psychiatric comorbidities, n (%) | |
|
Any comorbid disorder Major depressive disorder Bipolar disorders Substance use disorders Personality disorders Anxiety disorders Autism spectrum disorders |
51 (68.9) 27 (36.5) 3 (4.1) 19 (25.7) 8 (10.8) 6 (8.1) 5 (6.7) |
| Areas of functional impairment, n (%) | |
|
Social functioning Relational functioning Academic functioning Occupational functioning |
45 (60.8) 53 (71.6) 69 (93.2) 53 (71.6) |
| Related symptoms, n (%) | |
|
Mood swings Anger outbursts Low self-esteem Low tolerance for frustrations Sleep onset insomnia |
52 (70.3) 35 (47.3) 55 (74.3) 51 (68.9) 51 (68.9) |
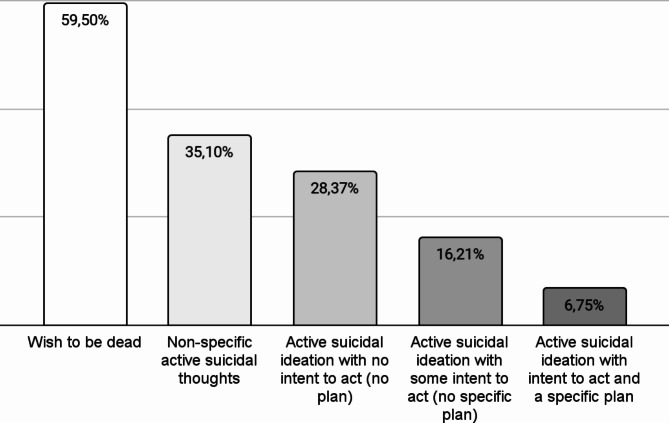
The lifetime prevalence of SI and SSI were 59.5% (n = 44) and 16.2% (n = 12), respectively. The 9.5% of patients (n = 7) showed lifetime SB, while NSSIB was found in 10.8% of the subjects (n = 8).
Figures 1 and 2 show the severity of lifetime SI and the different types of lifetime SB in the sample.
Fig. 1.
Cumulative distribution of the severity of suicidal ideation in individuals with ADHD (n = 74)
Fig. 2.
Different types of suicidal behaviors in individuals with ADHD (n = 74)
Tables 2, 3, 4 and 5 show the demographic and clinical features of the subgroups (ADHD with SI vs. ADHD without SI, ADHD with SSI vs. ADHD without SSI, ADHD with SB vs. ADHD without SB, ADHD with NSSIB vs. ADHD without NSSIB), compared according to χ2 tests or Kruskal-Wallis H test. The variables with a statistically significant difference were subjected to binary logistic regression.
Table 2.
Comparison between ADHD with SI vs. ADHD without SI, according to χ2 tests for categorical variables and Kruskal-Wallis H test for continuous variables
| SI group (44) | NO SI group (30) | p-value | |
|---|---|---|---|
| Sex, n (%) | |||
|
Male Female |
27 (61.4) 17 (38.6) |
23 (76.7) 7 (23.3) |
0.167 |
| Age (years), mean (SD) | 27.66 (9.48) | 30.03 (11.13) | 0.328 |
| Age at diagnosis (years), mean (SD) | 25.02 (10.14) | 27.27 (12.33) | 0.395 |
| Age at first ADHD treatment (years), mean (SD) | 25.48 (9.1) | 26.9 (12.06) | 0.569 |
| Ongoing ADHD treatment at assessment, n (%) | 12 (27.3) | 10 (33.3) | 0.391 |
| Family history of psychiatric disorders, n (%) | 23 (53.5) | 7 (23.3) | 0.010 |
| Family history of ADHD, n (%) | 7 (15.9) | 1 (3.3) | 0.08 |
| Adult ADHD subtype, n (%) | |||
|
Inattentive subtype Combined subtype |
19 (43.2) 25 (56.8) |
13 (43.3) 17 (56.7) |
0.99 |
| Childhood ADHD subtype, n (%) | |||
|
Inattentive subtype Combined subtype |
15 (34.1) 29 (65.9) |
11 (36.7) 19 (63.3) |
0.82 |
| DIVA 2.0, mean (SD) | |||
|
Inattentive symptoms in childhood Hyperactivity symptoms in childhood Inattentive symptoms in adulthood Hyperactivity symptoms in adulthood |
7.55 (0.92) 5.16 (3.28) 7.84 (1.18) 5.87 (2.64) |
7.11 (1.41) 5.21 (2.53) 6.68 (1.1) 5 (2.08) |
0.185 0.956 0.001 0.228 |
| ADHD-RS before treatment, mean (SD) | 35.6 (7.8) | 36.5 (9.72) | 0.705 |
|
BIS-11, mean (SD) Attentional impulsiveness Motor impulsiveness Non-planning impulsiveness |
71.27 (11.58) 20.8 (3.87) 23 (4.89) 27.41 (5,29) |
69.27 (11.71) 19.53 (4.17) 21.73 (4.36) 28 (5.28) |
0.469 0.187 0.258 0.638 |
| Lifetime psychiatric comorbidities, n (%) | |||
|
Any comorbid disorder Major depressive disorder Bipolar disorders Substance use disorders Personality disorders Anxiety disorders Autism spectrum disorders |
31 (70.4) 17 (38.6) 3 (6.8) 11 (25) 7 (15.9) 3 (6.8) 3 (6.8) |
20 (66.7) 10 (33.3) 0 (0) 8 (26.7) 2 (6.6) 3 (10) 1 (3.3) |
0.619 0.642 0.144 0.872 0.090 0.622 0.515 |
| Areas of functional impairment, n (%) | |||
|
Social functioning Relational functioning Academic functioning Occupational functioning |
31 (70.5) 34 (77.3) 42 (95.5) 32 (74.4) |
14 (46.6) 19 (63.3) 27 (90) 21 (70) |
0.044 0.192 0.359 0.721 |
| Related symptoms, n (%) | |||
|
Mood swings Anger outbursts Low self-esteem Low tolerance for frustrations Sleep onset insomnia |
30 (68.2) 22 (50) 37 (84.1) 30 (68.2) 29 (65.9) |
22 (73.3) 13 (43.3) 18 (60) 21 (70) 22 (73.3) |
0.634 0.57 0.02 0.868 0.498 |
Table 3.
Comparison between ADHD with SSI vs. ADHD without SSI, according to χ2 tests for categorical variables and Kruskal-Wallis H test for continuous variables
| SSI group (12) | NO SSI group (62) | p-value | |
|---|---|---|---|
| Sex, n (%) | |||
|
Male Female |
9 (18) 3 (12.5) |
41 (82) 21 (87.5) |
0.548 |
| Age (years), mean (SD) | 30.83 (11.82) | 28.19 (9.88) | 0.415 |
| Age at diagnosis (years), mean (SD) | 26.92 (10.33) | 25.74 (11.26) | 0.739 |
| Age at first ADHD treatment (years), mean (SD) | 28.67 (8.21) | 25.52 (10.67) | 0.339 |
| Ongoing ADHD treatment at assessment, n (%) | 2 (16.6) | 20 (35.5) | 0.129 |
| Physical activity, n (%) | 3 (25) | 35 (56.5) | 0.046 |
| Family history of psychiatric disorders, n (%) | 6 (50) | 24 (39.3) | 0.493 |
| Family history of ADHD, n (%) | 1 (12.5) | 7 (11.5) | 0.750 |
| Number of hospitalizations, mean (SD) | 1.17 (1.64) | 0.24 (0.93) | 0.008 |
| Adult ADHD subtype, n (%) | |||
|
Inattentive subtype Combined subtype |
4 (33.3) 8 (66.7) |
28 (45.2) 34 (54.8) |
0.449 |
| Childhood ADHD subtype, n (%) | |||
|
Inattentive subtype Combined subtype |
4 (33.3) 8 (66.7) |
22 (35.5) 40 (64.5) |
0.886 |
| DIVA 2.0, mean (SD) | |||
|
Inattentive symptoms in childhood Hyperactivity symptoms in childhood Inattentive symptoms in adulthood Hyperactivity symptoms in adulthood |
8.10 (0.74) 5.80 (3.22) 8 (0.94) 6.7 (2.16) |
7.2 (1.16) 5.03 (2.95) 7.25 (1.31) 5.25 (2.46) |
0.024 0.470 0.097 0.096 |
| ADHD-RS before treatment, mean (SD) | 35.9 (9.09) | 36.04 (8.65) | 0.963 |
|
BIS-11, mean (SD) Attentional impulsiveness Motor impulsiveness Non-planning impulsiveness |
79 (7.19) 22.83 (4.01) 25 (3.24) 29.7 (3.9) |
68.81 (11.6) 19.79 (3.86) 22 (4.8) 27.98 (5.24) |
0.005 0.015 0.042 0.08 |
| Lifetime psychiatric comorbidities, n (%) | |||
|
Any comorbid disorder Major depressive disorder Bipolar disorders Substance use disorders Personality disorders Anxiety disorders Autism spectrum disorders |
11 (91.7) 5 (41.7) 1 (33.3) 4 (33.3) 2 (16.7) 0 (0) 1 (8.3) |
40 (65.6) 22 (35.5) 2 (3.2) 15 (24.2) 6 (9.7) 6 (9.7) 3 (4.8) |
0.072 0.684 0.412 0.507 0.475 0.261 0.624 |
| Areas of functional impairment, n (%) | |||
|
Social functioning Relational functioning Academic functioning Occupational functioning |
10 (83.3) 10 (83.3) 10 (83.3) 10 (83.3) |
35 (56.5) 43 (69.4) 59 (95.2) 43 (70.5) |
0.081 0.326 0.135 0.574 |
| Related symptoms, n (%) | |||
|
Mood swings Anger outbursts Low self-esteem Low tolerance for frustrations Sleep onset insomnia |
11 (91.7) 7 (58.3) 10 (83.3) 9 (75) 8 (66.7) |
41 (78.8) 28 (45.2) 45 (72.6) 42 (67.7) 43 (69.4) |
0.076 0.403 0.435 0.619 0.854 |
Table 4.
Comparison between ADHD with SB vs. ADHD without SB, according to χ2 tests for categorical variables and Kruskal-Wallis H test for continuous variables
| SB group (7) | NO SB group (67) | p-value | |
|---|---|---|---|
| Sex, n (%) | |||
|
Male Female |
4 (57.1) 3 (42.9) |
46 (68.7) 21 (31.3) |
0.536 |
| Employment, n (%) | |||
|
Unemployed Employed Student Retired |
5 (71.4) 1 (14.2) 1 (14.2) 0 (0) |
13 (19.5) 32 (47.7) 21 (31.3) 1 (1.5) |
0.048 |
| Age (years), mean (SD) | 33.57 (12.55) | 28.10 (9.86) | 0.178 |
| Age at diagnosis (years), mean (SD) | 26.86 (10.76) | 25.84 (11.16) | 0.818 |
| Age at first ADHD treatment (years), mean (SD) | 27 (7.91) | 25.94 (10.59) | 0.798 |
| Ongoing ADHD treatment at assessment, n (%) | 2 (28.6) | 21 (31.3) | 0.880 |
| Family history of psychiatric disorders, n (%) | 4 (57.1) | 26 (39.4) | 0.364 |
| Family history of ADHD, n (%) | 0 (0) | 8 (12,1) | 0.329 |
| Number of hospitalizations, mean (SD) | 1.86 (1.86) | 0.24 (0.9) | < 0.001 |
| Adult ADHD subtype, n (%) | |||
|
Inattentive subtype Combined subtype |
2 (28.5) 5 (71.5) |
31 (46.3) 36 (53.7) |
0.104 |
| Childhood ADHD subtype, n (%) | |||
|
Inattentive subtype Combined subtype |
2 (28.5) 5 (71.5) |
25 (37.3) 42 (62.7) |
0.225 |
| DIVA 2.0, mean (SD) | |||
|
Inattentive symptoms in childhood Hyperactivity symptoms in childhood Inattentive symptoms in adulthood Hyperactivity symptoms in adulthood |
8.2 (0.84) 6.5 (2.34) 8.1 (1.09) 6.9 (1.92) |
7.29 (1.14) 4.98 (3) 7.31 (1.27) 5.36 (2.46) |
0.090 0.154 0.142 0.112 |
| ADHD-RS before treatment, mean (SD) | 37.2 (8.34) | 35.9 (8.74) | 0.752 |
|
BIS-11, mean (SD) Attentional impulsiveness Motor impulsiveness Non-planning impulsiveness |
79.3 (7.95) 22.71 (4.3) 25.57 (2.82) 30,57 (5,25) |
69.54 (11.57) 20 (3.93) 22.16 (4.75) 27,34 (5,2) |
0.033 0.093 0.050 0,123 |
| Lifetime psychiatric comorbidities, n (%) | |||
|
Any comorbid disorder Major depressive disorder Bipolar disorders Substance use disorders Personality disorders Anxiety disorders Autism spectrum disorders |
7 (100) 3 (42.9) 1 (14.3) 3 (42.9) 2 (28.6) 0 (0) 1 (14.3) |
44 (66.7) 24 (35.8) 3 (4.5) 16 (23.9) 6 (9) 6 (9) 3 (4.5) |
0.068 0.713 0.345 0.274 0.112 0.409 0.275 |
| Areas of functional impairment, n (%) | |||
|
Social functioning Relational functioning Academic functioning Occupational functioning |
6 (85.7) 6 (85.7) 6 (85.7) 6 (85.7) |
39 (58.2) 47 (70.1) 63 (94) 46 (69.7) |
0.156 0.385 0.232 0.404 |
| Related symptoms, n (%) | |||
|
Mood swings Anger outbursts Low self-esteem Low tolerance for frustrations Sleep onset insomnia |
6 (85.7) 4 (57.1) 5 (71.4) 6 (85.7) 5 (71.4) |
46 (68.7) 30 (44.8) 50 (74.6) 45 (67.2) 46 (68.7) |
0.347 0.179 0.854 0.313 0.880 |
Table 5.
Comparison between ADHD with NSSIB vs. ADHD without NSSIB, according to χ2 tests for categorical variables and Kruskal-Wallis H test for continuous variables
| NSSIB group (8) | NO NSSIB group (66) | p-value | |
|---|---|---|---|
| Sex, n (%) | |||
|
Male Female |
3 (37.5) 5 (62.5) |
47 (71.2) 19 (28.8) |
0.06 |
| Age (years), mean (SD) | 29.5 (11.52) | 30.12 (10.83) | 0.79 |
| Age at diagnosis (years), mean (SD) | 25.88 (12.84) | 25.94 (10.93) | 0.988 |
| Age at first ADHD treatment (years), mean (SD) | 25.88 (12.84) | 26.06 (10.09) | 0.962 |
| Ongoing ADHD treatment at assessment, n (%) | 2 (25) | 21 (31.8) | 0,888 |
| Current smoking, n (%) | 5 (62.5) | 17 (25.8) | 0.032 |
| Family history of psychiatric disorders, n (%) | 3 (37.5) | 27 (41.5) | 0.827 |
| Family history of ADHD, n (%) | 1 (12.5) | 7 (10.6) | 0,871 |
| Number of hospitalizations, mean (SD) | 1.38 (1.99) | 0.27 (0.92) | 0.008 |
| Adult ADHD subtype, n (%) | |||
|
Inattentive subtype Combined subtype |
2 (25) 6 (75) |
30 (45.5) 36 (54.5) |
0,270 |
| Childhood ADHD subtype, n (%) | |||
|
Inattentive subtype Combined subtype |
2 (25) 6 (75) |
24 (36.4) 42 (63.6) |
0,525 |
| DIVA 2.0, mean (SD) | |||
|
Inattentive symptoms in childhood Hyperactivity symptoms in childhood Inattentive symptoms in adulthood Hyperactivity symptoms in adulthood |
8.17 (0.75) 6.33 (3.14) 8.17 (0.98) 6.67 (3.32) |
7.27 (1.14) 5.02 (2.97) 7.3 (1.28) 5.39 (2.32) |
0.070 0.320 0.118 0.235 |
| ADHD-RS before treatment, mean (SD) | 37 (9.67) | 35.92 (8.64) | 0.793 |
|
BIS-11, mean (SD) Attentional impulsiveness Motor impulsiveness Non-planning impulsiveness |
74.5 (11.85) 21.13 (4.45) 23.25 (4.89) 30.13 (4.99) |
69.97 (11.56) 20.18 (3.99) 22.39 (4.7) 27.3 (5.24) |
0.300 0.535 0.630 0.160 |
| Lifetime psychiatric comorbidities, n (%) | |||
|
Any comorbid disorder Major depressive disorder Bipolar disorders Substance use disorders Personality disorders Anxiety disorders Autism spectrum disorders |
4 (50) 2 (25) 0 (0) 1 (12.5) 3 (37.5) 0 (0) 0 (0) |
48 (72.7) 25 (37.9) 3 (4.5) 10 (15.2) 5 (7.6) 6 (9.1) 4 (6.1) |
0.184 0.475 0.538 0.842 0.010 0.374 0.474 |
| Areas of functional impairment, n (%) | |||
|
Social functioning Relational functioning Academic functioning Occupational functioning |
5 (62.5) 6 (75) 7 (87.5) 6 (75) |
40 (60.6) 47 (71.2) 62 (93.9) 47 (72.3) |
0.917 0,822 0.493 0.493 |
| Related symptoms, n (%) | |||
|
Mood swings Anger outbursts Low self-esteem Low tolerance for frustrations Sleep onset insomnia |
6 (75) 6 (75) 5 (62.5) 5 (62.5) 5 (62.5) |
46 (69.7) 29 (43.9) 50 (75.8) 46 (69.7) 46 (69.7) |
0.757 0.097 0.418 0.678 0.678 |
The results of the binary logistic regression models are described in Tables 6, 7 and 8, and 9.
Table 6.
The relationship between potential explanatory variables and lifetime suicidal ideation: results from the binary logistic regression analysis (n = 74)
| B | SE | Wald | p-value | OR | 95%CI | |
|---|---|---|---|---|---|---|
| Severity of inattentive symptoms in adulthood | 0.829 | 0.360 | 5.317 | 0.021 | 2.291 | 0.164–2.884 |
| Family history of psychiatric disorders | 1.029 | 0.588 | 3.068 | 0.080 | 2.800 | -0.161–2.680 |
|
Impairment in social functioning Low self-esteem |
1.075 1.374 |
0.548 0.614 |
3.856 5.013 |
0.049 0.025 |
2.931 3.953 |
0.037–2.672 0.104–3.283 |
| Constant | 2.405 | 0.680 | 12.512 | < 0.001 | 11.080 | - |
Table 7.
The relationship between potential explanatory variables and lifetime severe suicidal ideation: results from the binary logistic regression analysis (n = 74)
| B | SE | Wald | p-value | OR | 95%CI | |
|---|---|---|---|---|---|---|
| Severity of inattentive symptoms in childhood | 1.772 | 0.815 | 4.725 | 0.030 | 5.880 | 0.291–65.893 |
|
Total impulsivity Attentional impulsiveness Motor impulsiveness |
0.185 0.845 -0.311 |
0.193 0.406 0.330 |
0.920 4.327 0.889 |
0.337 0.038 0.346 |
1.203 20.3460.327 |
-5.430–70.744 0.039–2.176 -102.161–3.571 |
| Number of hospitalizations | 0.587 | 0.261 | 5.050 | 0.025 | 1.799 | 0.030-38.569 |
| Physical activity | -2.641 | 1.069 | 6.104 | 0.013 | 0.071 | -80.768- -0.594 |
| Constant | -14.133 | 4.646 | 9.254 | 0.002 | 0.000 | - |
Table 8.
The relationship between potential explanatory variables and lifetime suicidal behavior: results from the binary logistic regression analysis (n = 74)
| B | SE | Wald | p-value | OR | 95%CI | |
|---|---|---|---|---|---|---|
| Employment | -0.398 | 0.374 | 1.132 | 0.287 | 0.672 | -25.777–0.876 |
|
Total impulsivity Motor impulsiveness |
0.118 -0.090 |
0.096 0.213 |
1.503 0.178 |
0.220 0.673 |
1.125 0.914 |
-0.316–0.862 − 1.431–2.980 |
| Number of hospitalizations | 0.593 | 0.265 | 5.001 | 0.080 | 1.810 | -0.013–49.540 |
| Constant | -8.845 | 4.222 | 4.389 | 0.036 | 0.000 | - |
Table 9.
The relationship between potential explanatory variables and lifetime non suicidal self-injury behavior: results from the binary logistic regression analysis (n = 74)
| B | SE | Wald | p-value | OR | 95%CI | |
|---|---|---|---|---|---|---|
| Current smoking | 1.043 | 0.909 | 1.316 | 0.251 | 2.838 | -2.066–19.891 |
| Personality disorders | 1.640 | 0.940 | 3.048 | 0.081 | 5.157 | -18.844–20.923 |
| Number of hospitalizations | 0.299 | 0.274 | 1.186 | 0.276 | 1.348 | -17.326–1.454 |
| Constant | -3.076 | 0.646 | 22.700 | < 0.001 | 0.046 | - |
The incidence of lifetime SI appeared related to severity of inattentive symptoms during adulthood (p = 0.021, OR 2,0.291, 95%CI 0.164–2.884), low self-esteem (p = 0.025, OR 3.953, 95%CI 0.104–3.283) and impairment in social functioning (p = 0.049, OR 2.931, 95%CI 0.037–2.672).
Lifetime SSI was significantly associated to the severity of inattentive symptoms during childhood (p = 0.030, OR 5.880, 95%CI 0.291–65.893), attentional impulsiveness (p = 0.038, OR 2.327, 95%CI 0.039–2.176) and number of hospitalizations (p = 0.025, OR 1,799, 95%CI 0.030-38.569). Physical exercise showed to be related with a significant lower lifetime prevalence of SSI (p = 0.013, OR 0.071, 95%CI − 80.768- -0.594).
No socio-demographic features resulted significantly associated to the occurrence of SI and SSI.
The prevalence of lifetime SB did not appear significantly related to any socio-demographic or clinical feature (including any psychiatric comorbidity), also when stratified in the different types of SB. Similarly, no factor significantly linked with higher prevalence of NSSIB emerged.
Discussion
This observational study aimed to evaluate the prevalence of suicidality (SI, SSI, SB, and NSSIB) in adult patients with ADHD using a dimensional approach and a validated instrument; we also analyzed socio-demographic and clinical factors potentially related to occurrence of SI, SSI, SB, or NSSIB in these patients.
The Columbia-Suicide Severity Rating Scale (C-SSRS) has enabled us to more precisely define and quantify the complex phenomenon of suicidality, which cannot be captured by a single question. As emphasized by Posner and colleagues in the original validation findings of this scale, a general desire to be dead does not pose a comparable risk factor for SB when contrasted with active SI [7]. Additionally, given the high levels of impulsivity in patients with ADHD and the associated risk of acting out, identifying those with active SI could be crucial in preventing suicide.
We identified a high prevalence of suicidality in adult patients with ADHD. Specifically, 59.5% of our sample reported wishing to be dead at least once in their life; moreover, 9.5% of the participants reported at least one lifetime SB. A considerable proportion of individuals with ADHD can be considered at high risk for suicide: 16.2% of our sample scored ≥ 4 on the severity scale of the C-SSRS, presenting lifetime active SI with a specific plan and intent (6.8%) or active SI with some intent to act but no plan (9.4%). Concerning SB, only a minority of our patients had actually attempted suicide (6.8%); many others, however, engaged in some SB, such as interrupted attempts (1.4%), aborted or self-interrupted attempts (2.7%), or in preparatory acts or behaviors (5.4%). Moreover, a considerable part of our sample (10.8%) engaged in NSSIB. Our results are reasonably in line with findings from a recent meta-analysis showing the lifetime prevalence of SI and SB to be 40% and 18.9%, respectively [6].
The identification of a high suicidality risk among adults with ADHD underscores the necessity for focused assessment and careful monitoring within clinical practice. Regular clinical assessments and implementation of psychoeducational interventions, not only for patients but also for their familial and caregiving networks, can be crucial tools in addressing this complex clinical concern. It is essential to assess suicidality in patients with ADHD in a dimensional manner during the initial evaluation, employing both clinical judgment and, where feasible, specific tools such as the Columbia Suicide Severity Rating Scale. For patients exhibiting a heightened risk profile, suicidality should not only be monitored as an ongoing component but also integrated into clinical outcomes and management strategies. This includes considering the use of medications that may have transdiagnostic suicidal effects, such as lithium salts [40], particularly in cases where the risk is deemed elevated.
The severity of inattentive symptoms in adulthood appeared significantly associated with lifetime SI, while the severity of hyperactivity/impulsivity symptoms did not result to have an impact on suicidality (both SI, SSI, SB and NSSIB). This evidence suggests that the association between ADHD and suicidality could be mediated by inattention, which represents the core symptom of ADHD.
In accordance with this hypothesis, the only type of impulsiveness (measured through BIS-11) which resulted associated with suicidality (specifically with SSI) in our sample was attentional impulsiveness. This has been defined as an inability to focus attention or concentrate, and it assesses task-focus, intrusive thoughts, and racing thoughts [41]. Instead, motor impulsiveness (acting without thinking) and non-planning impulsiveness (lack of “futuring” or forethought) did not result to affect both SI and SB, confirming that the risk of suicide in ADHD patients could depend on inattention rather than impulsivity itself.
Furthermore, while lifetime SI appeared related to the severity of inattentive symptoms in adulthood, we found that lifetime SSI was associated with the severity of inattentive symptoms during childhood. This result endorses the potential impact in adulthood of the symptoms during childhood, underlining that the intensity of symptoms during this critical developmental period plays a more crucial role in influencing suicidality risk than the timing of the diagnosis itself. Previous research has identified several predictive factors for suicidality in ADHD, such as early externalizing behaviors, adverse childhood experiences, and negative father-daughter interactions, while not placing emphasis on inattentive symptoms [42]. Therefore, considering SSI as the proper risk factor for suicide, exploring symptoms of attention deficit in childhood should be a target in ADHD patients. However, in clinical practice, identifying this cluster in childhood can be challenging due to the occasional unavailability of caregivers and the less overt presentation of inattention, which is not always the predominant feature of ADHD, particularly in children.
It is important to underline that in our sample SI, SSI, SB and NSSIB did not appear associated with any psychiatric comorbidity, in line with prior research findings from Septier’s et al. meta-analysis [6].
Furthermore, we did not find any clinical or socio-demographic factors significantly associated with SB and NSSIB in adult patients with ADHD, indicating a direct correlation between these phenomena.
Unlike SB and NSSIB, other clinical factors were found to be associated with SI and SSI in addition to the previously mentioned inattentive symptoms and attentional impulsiveness. Patients with SI exhibited significantly more frequent impairments in social functioning, though not in other areas. This finding, consistent with existing literature, supports the notion of a causal link between social isolation and suicide, as well as the protective influence of social support against suicide [43]. Physical activity appeared to be associated with a lower lifetime prevalence of SSI, suggesting that being physically active could reduce suicidal risk. While engaging in physical activity has proven to be a protective factor against SSI, the intensity of the activity did not appear to be correlated with the risk, suggesting that even light-intensity physical activity can be protective. This evidence aligns with a recent meta-analysis conducted on psychiatric patients [44] and is significant considering that there are only a limited number of interventions that have demonstrated effectiveness against suicide, and these are not always accessible within public health systems. Indeed, only a few medications have been shown to clearly reduce suicidal risk, such as lithium, ketamine and clozapine [45, 46]. Meanwhile, interventions like cognitive-behavioral therapy have proven effective but are often not readily available within public health systems [45].
Low self-esteem is a known risk factor for suicide, especially in emerging adulthood [47]. It appeared significantly related with lifetime SI (it was found in 84.1% of the patients with suicidality history), but it is important to underline how frequently it occurs also in patients without an history of SI/SSI/SB/NSSIB (60%), being one of the most associated symptoms in ADHD.
No gender differences emerged regarding both SI, SSI, SB and NSSIB in our sample.
Our study has several strengths, including a well-characterized clinical sample comprised of carefully diagnosed patients with thorough evaluations of their ADHD symptoms and comorbidities, the use of standardized validated assessments, and a dimensional approach. However, our study should be considered in light of some limitations. First, the cross-sectional design does not allow for the inference of causal relationships or the evaluation of etiological factors. Another limitation of our study is the gender ratio of approximately 2:1 (males to females) among the patients, which, although slightly higher than the 1.7:1 ratio reported in the literature [48], is still consistent with the general epidemiology of the disorder. Furthermore, while we addressed various aspects of emotional dysregulation (such as anger control, mood reactivity, and frustration tolerance), we did not comprehensively cover emotional dysregulation in its entirety. The absence of patients with the predominantly hyperactive-impulsive subtype and the high prevalence of single patients represent a potential additional barrier to the generalization of our results, as well as the low prevalence of familial ADHD in our sample limits our ability to generalize the results and precludes us from excluding a potential protective role of familial ADHD in suicidality. Additionally, the sample did not include individuals who had completed suicide, which means we cannot determine if the results apply to suicide deaths. Another significant limitation of this study is the small number of participants, which renders the results regarding potential predictors of SB/NSSIB preliminary. Additionally, the absence of a comparison group from the general population further limits the ability to contextualize these findings. It is, therefore, not possible to rule out the possibility that the risk of SB and NSSIB is mediated by factors such as personality disorders or specific temperaments. These traits are particularly prevalent among adults with ADHD [49], contributing to greater functional impairment and reduced treatment response [50], and have also been associated with suicidality dimensions [8].
Despite these limitations, our findings are noteworthy since they highlight that a significant proportion of patients with ADHD have lifetime SI/SB. Moreover, this association appeared not to be affected by psychiatric comorbidities. Instead, our findings suggest that the risk of suicide in ADHD patients could depend on inattention itself. Interestingly, this dimension may be more closely associated with suicidality severity due to several interrelated psychological and social factors. Specifically, individuals exhibiting higher levels of inattention might experience lower self-esteem, a pervasive sense of hopelessness, limited opportunities for personal and professional development, decreased engagement in social situations, and heightened feelings of isolation. These elements can create a detrimental emotional environment that exacerbates suicidality risk, suggesting a complex interplay between ADHD symptoms and the psychosocial challenges faced by these individuals. In conclusion, adult patients with ADHD can be considered at risk of suicide, and it is important to identify which patients are at higher risk, in order to guide preventive pharmacological or psychological treatments and psychoeducational interventions. Therefore, for adult ADHD patients, alongside pharmacological therapy, the utilization of psychotherapeutic interventions, particularly cognitive-behavioral and psychoeducational approaches, is crucial. These interventions aid patients in gaining a deeper understanding of their condition, enhancing self-esteem, and guiding them towards adopting healthy and protective lifestyles, such as regular physical activity.
Future research should aim to replicate our findings in a larger sample to enhance generalizability and robustness. Additionally, it would be beneficial to integrate cognitive assessments specifically focused on the attentional dimension, as well as other cognitive measures, to further explore their associations with dimensions of suicidality. Furthermore, it would be valuable to examine how previous psychotherapy experiences, as well medications and psychosocial interventions (whether individual or family-based) influence suicidality. Such investigations could provide important insights into effective management strategies for individuals with ADHD.
Acknowledgements
All authors confirm that this manuscript has not been previously published nor is it currently under consideration by any other journal. This research did not received any specific grants from funding agencies in the publica, commercial, or not-for-profit sectors.
Author contributions
All authors have read and approved the final version submitted and take public responsibility for all aspects of the work. Gabriele Di Salvo, Giuseppe Maina and Gianluca Rosso designed the study. Gabriele Di Salvo, Camilla Perotti, Lorenzo Filippo and Camilla Garrone collected the patients’ data. Gabriele Di Salvo and Camilla Perotti managed literature search and Gabriele Di Salvo and Camilla Perotti analyzed the data. Gabriele Di Salvo wrote the draft. Giuseppe Maina and Gianluca Rosso provided substantial comments and helped drafting the manuscript in its final form.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Disclosure
All authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. Gianluca Rosso has been a speaker and/or consultant from Angelini, Lundbeck, Janssen and Otsuka outside of the current work. Giuseppe Maina has been a consultant/speaker and/or has received research grants from Angelini, Boheringer, Innovapharma, Janssen, Fb Health, Otsuka, Lundbeck, Italfarmaco and Sanofi. Gabriele Di Salvo has been a speaker for Lundbeck and Angelini. Nevertheless, all authors report that this did not result in conflicts of interest for the present study.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Leffa DT, Caye A, Rohde LA. ADHD in children and adults: diagnosis and prognosis. Curr Top Behav Neurosci. 2022;57:1–18. [DOI] [PubMed] [Google Scholar]
- 2.Spencer TJ, Biederman J, Mick E. Attention-deficit/hyperactivity disorder: diagnosis, lifespan, comorbidities, and neurobiology. J Pediatr Psychol. 2007;32(6):631–42. 10.1093/jpepsy/jsm005 [DOI] [PubMed] [Google Scholar]
- 3.Simon V, Czobor P, Bálint S, Mészáros A, Bitter I. Prevalence and correlates of adult attention-deficit hyperactivity disorder: meta-analysis. Br J Psychiatry. 2009;194(3):204–11. 10.1192/bjp.bp.107.048827 [DOI] [PubMed] [Google Scholar]
- 4.Weibel S, Menard O, Ionita A, Boumendjel M, Cabelguen C, Kraemer C, et al. Practical considerations for the evaluation and management of attention deficit hyperactivity disorder (ADHD) in adults. Encephale. 2020;46(1):30–40. 10.1016/j.encep.2019.06.005 [DOI] [PubMed] [Google Scholar]
- 5.Katzman MA, Bilkey TS, Chokka PR, Fallu A, Klassen LJ. Adult ADHD and comorbid disorders: clinical implications of a dimensional approach. BMC Psychiatry. 2017;17(1):302. 10.1186/s12888-017-1463-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Septier M, Stordeur C, Zhang J, Delorme R, Cortese S. Association between suicidal spectrum behaviors and Attention-Deficit/Hyperactivity disorder: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2019;103:109–18. 10.1016/j.neubiorev.2019.05.022 [DOI] [PubMed] [Google Scholar]
- 7.Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, et al. The Columbia-suicide severity rating scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168:1266–77. 10.1176/appi.ajp.2011.10111704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Giupponi G, Innamorati M, Rogante E, Sarubbi S, Erbuto D, Maniscalco I, et al. The characteristics of Mood Polarity, temperament, and suicide risk in adult ADHD. Int J Environ Res Public Health. 2020;17(8):2871. 10.3390/ijerph17082871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Olsson P, Wiktorsson S, Strömsten LMJ, Salander Renberg E, Runeson B, et al. Attention deficit hyperactivity disorder in adults who present with self-harm: a comparative 6-month follow-up study. BMC Psychiatry. 2022;22(1):428. 10.1186/s12888-022-04057-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shen Y, Chan BSM, Huang C, Cui X, Liu J, Lu J, et al. Suicidal behaviors and attention deficit hyperactivity disorder (ADHD): a cross-sectional study among Chinese medical college students. BMC Psychiatry. 2021;21(1):258. 10.1186/s12888-021-03247-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Katzman M, Bilkey TS, Chokka PR, Fallu A, Klassen LJ. Adult ADHD and comorbid disorders: clinical implications of a dimensional approach. BMC Psychiatry. 2017;17(1):302. 10.1186/s12888-017-1463-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Salvi V, Ribuoli E, Servasi M, Orsolini L, Volpe U. ADHD and bipolar disorder in Adulthood: clinical and treatment implications. Med (Kaunas). 2021;57(5):466. 10.3390/medicina57050466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pompili M, Rihmer Z, Akiskal HS, Innamorati M, Iliceto P, Akiskal KK, Lester D, Narciso V, Ferracuti S, Tatarelli R, De Pisa E, Girardi P. Temperament and personality dimensions in suicidal and nonsuicidal psychiatric inpatients. Psychopathology. 2008;41(5):313–21. 10.1159/000146069 [DOI] [PubMed] [Google Scholar]
- 14.Orsolini L, Latini R, Pompili M, Serafini G, Volpe U, Vellante F, et al. Understanding the complex of suicide in Depression: from Research to Clinics. Psychiatry Investig. 2020;17(3):207–21. 10.30773/pi.2019.0171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Orsolini L, Longo G, Volgare R, Piergentili S, Servasi M, Perugi G, Volpe U. Cyclothymic affective temperament and low positive attitude coping strategies as predictors of comorbid depressive symptomatology in adult ADHD patients. J Affect Disord. 2024;365:417–26. 10.1016/j.jad.2024.08.083 [DOI] [PubMed] [Google Scholar]
- 16.Heidbreder R. ADHD symptomatology is best conceptualized as a spectrum: a dimensional versus unitary approach to diagnosis. Atten Defic Hyperact Disord. 2015;7(4):249–69. 10.1007/s12402-015-0171-4 [DOI] [PubMed] [Google Scholar]
- 17.Fuller-Thomson E, Rivière RN, Carrique L, Agbeyaka S. The Dark side of ADHD: factors Associated with suicide attempts among those with ADHD in a National Representative Canadian Sample. Arch Suicide Res. 2022;26(3):1122–40. 10.1080/13811118.2020.1856258 [DOI] [PubMed] [Google Scholar]
- 18.Stickley A, Koyanagi A, Ruchkin V, Kamio Y. Attention-deficit/hyperactivity disorder symptoms and suicide ideation and attempts: findings from the Adult Psychiatric Morbidity Survey 2007. J Affect Disord. 2016;189:321–8. 10.1016/j.jad.2015.09.061 [DOI] [PubMed] [Google Scholar]
- 19.Ruchkin V, Koposov RA, Koyanagi A, Stickley A. Suicidal behavior in Juvenile delinquents: the role of ADHD and other Comorbid Psychiatric disorders. Child Psychiatry Hum Dev. 2017;48(5):691–8. 10.1007/s10578-016-0693-9 [DOI] [PubMed] [Google Scholar]
- 20.Arias AJ, Gelernter J, Chan G, Weiss RD, Brady KT, Farrer L, et al. Correlates of co-occurring ADHD in drug-dependent subjects: prevalence and features of substance dependence and psychiatric disorders. Addict Behav. 2008;33(9):1199–207. 10.1016/j.addbeh.2008.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brook U, Boaz M. Attention deficit and hyperactivity disorder/learning disabilities (ADHD/LD): parental characterization and perception. Patient Educ Couns. 2005;57(1):96–100. 10.1016/j.pec.2004.03.018 [DOI] [PubMed] [Google Scholar]
- 22.Westmoreland P, Gunter T, Loveless P, Allen J, Sieleni B, Black DW. Attention deficit hyperactivity disorder in men and women newly committed to prison: clinical characteristics, psychiatric comorbidity, and quality of life. Int J Offender Ther Comp Criminol. 2010;54(3):361–77. 10.1177/0306624X09332313 [DOI] [PubMed] [Google Scholar]
- 23.Haavisto A, Sourander A, Multimäki P, Parkkola K, Santalahti P, Helenius H, et al. Factors associated with ideation and acts of deliberate self-harm among 18-year-old boys. A prospective 10-year follow-up study. Soc Psychiatry Psychiatr Epidemiol. 2005;40(11):912–21. 10.1007/s00127-005-0966-2 [DOI] [PubMed] [Google Scholar]
- 24.Austgulen A, Skram NKG, Haavik J, Lundervold AJ. Risk factors of suicidal spectrum behaviors in adults and adolescents with attention-deficit / hyperactivity disorder - a systematic review. BMC Psychiatry. 2023;23(1):612. 10.1186/s12888-023-05099-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kakuszi B, Bitter I, Czobor P. Suicidal ideation in adult ADHD: gender difference with a specific psychopathological profile. Compr Psychiatry. 2018;85:23–9. 10.1016/j.comppsych.2018.06.003 [DOI] [PubMed] [Google Scholar]
- 26.Babinski DE, Neely KA, Ba DM, Liu G. Depression and suicidal behavior in young adult men and women with ADHD: evidence from claims data. J Clin Psychiatry. 2020;81(6):22578. 10.4088/JCP.19m13130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ljung T, Chen Q, Lichtenstein P, Larsson H. Common etiological factors of attention-deficit/hyperactivity disorder and suicidal behavior. JAMA Psychiat. 2014;71(8):958. 10.1001/jamapsychiatry.2014.363 [DOI] [PubMed] [Google Scholar]
- 28.Mayes SD, Calhoun SL, Baweja R, Feldman L, Syed E, Gorman AA, et al. Suicide ideation and attempts are associated with co-occurring oppositional defiant disorder and sadness in children and adolescents with ADHD. J Psychopathol Behav Assess. 2015;37(2):274–82. 10.1007/s10862-014-9451-0 [Google Scholar]
- 29.Balazs J, Miklósi M, Keresztény A, Dallos G, Gádoros J. Attention-deficit hyperactivity disorder and suicidality in a treatment naïve sample of children and adolescents. J Affect Disord. 2014;152–154:282–7. 10.1016/j.jad.2013.09.026 [DOI] [PubMed] [Google Scholar]
- 30.Park S, Cho MJ, Chang SM, Jeon HJ, Cho SJ, Kim BS, et al. Prevalence, correlates, and comorbidities of adult ADHD symptoms in Korea: results of the Korean epidemiologic catchment area study. Psychiatry Res. 2011;186(2–3):378–83. 10.1016/j.psychres.2010.07.047 [DOI] [PubMed] [Google Scholar]
- 31.American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.).
- 32.Kooij JJS, Francken MH. DIVA 2.0. Diagnostic interview voor ADHD in adults bij volwassenen [DIVA 2.0 diagnostic interview ADHD in adults]. DIVA Foundation; 2010.
- 33.DuPaul P, Anastopoulos R. (1998) ADHD Rating Scale-IV.
- 34.Patton JH, Stanford MS, Barratt ES. (1995). Barratt Impulsiveness Scale-11 (BIS-11).
- 35.First MB, Williams JBW, Karg RS, Spitzer RL. Structured clinical interview for DSM-5 disorders, Clinician Version (SCID-5-CV). Arlington, VA: American Psychiatric Association; 2016. [Google Scholar]
- 36.Millon T. Clinical Multiaxial Inventory (MCMI-III), 1997.
- 37.Conway PM, Erlangsen A, Teasdale TW, Jakobsen IS, Larsen KJ. Predictive validity of the Columbia-suicide severity rating scale for short-term suicidal behavior: a Danish study of adolescents at a high risk of suicide. Arch Suicide Res. 2017;21:455–69. 10.1080/13811118.2016.1222318 [DOI] [PubMed] [Google Scholar]
- 38.Bramante S, Maina G, Borgogno R, Pellegrini L, Rigardetto S, Albert U. Assessing suicide risk in patients with obsessive-compulsive disorder: a dimensional approach. Braz J Psychiatry. 2023;45(1):28–37. 10.47626/1516-4446-2022-2632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Greist JH, Mundt JC, Gwaltney CJ, Jefferson JW, Posner K. Predictive value of Baseline Electronic Columbia-suicide severity rating scale (eC-SSRS) assessments for identifying risk of prospective reports of suicidal behavior during Research Participation. Innov Clin Neurosci. 2014;11(9–10):23–31. [PMC free article] [PubMed] [Google Scholar]
- 40.Nabi Z, Stansfeld J, Plöderl M, Wood L, Moncrieff J. Effects of lithium on suicide and suicidal behaviour: a systematic review and meta-analysis of randomised trials. Epidemiol Psychiatr Sci. 2022;31:e65. 10.1017/S204579602200049X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;51(6):768–74. https://doi.org/10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 42.Meza JI, Owens EB, Hinshaw SP. Childhood predictors and moderators of lifetime risk of self-harm in girls with and without attention-deficit/hyperactivity disorder. Dev Psychopathol. 2021;33(4):1351–67. 10.1017/S0954579420000553 [DOI] [PubMed] [Google Scholar]
- 43.Motillon-Toudic C, Walter M, Séguin M, Carrier JD, Berrouiguet S, Lemey C. Social isolation and suicide risk: literature review and perspectives. Eur Psychiatry. 2022;65(1):e65. 10.1192/j.eurpsy.2022.2320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vancampfort D, Hallgren M, Firth J, Rosenbaum S, Schuch FB, Mugisha J, et al. Physical activity and suicidal ideation: a systematic review and meta-analysis. J Affect Disord. 2018;225:438–48. 10.1016/j.jad.2017.08.070 [DOI] [PubMed] [Google Scholar]
- 45.D’Anci KE, Uhl S, Giradi G, Martin C. Treatments for the Prevention and management of suicide: a systematic review. Ann Intern Med. 2019;171(5):334–42. 10.7326/M19-0869 [DOI] [PubMed] [Google Scholar]
- 46.Masdrakis VG, Baldwin DS. Prevention of suicide by clozapine in mental disorders: systematic review. Eur Neuropsychopharmacol. 2023;69:4–23. 10.1016/j.euroneuro.2022.12.011 [DOI] [PubMed] [Google Scholar]
- 47.Pereira AS, Willhelm AR, Koller SH, Almeida RMM. Risk and protective factors for suicide attempt in emerging adulthood. Cien Saude Colet. 2018;23(11):3767–77. 10.1590/1413-812320182311.29112016 [DOI] [PubMed] [Google Scholar]
- 48.Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163(4):716–23. 10.1176/ajp.2006.163.4.716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Olsen JL, Reimherr FW, Marchant BK, Wender PH, Robison RJ. The effect of personality disorder symptoms on response to treatment with methylphenidate transdermal system in adults with attention-deficit/hyperactivity disorder. Prim Care Companion CNS Disord. 2012;14(5):PCC. 12m01344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gift TE, Reimherr FW, Marchant BK, Steans TA, Wender PH. Personality disorder in adult Attention-Deficit/Hyperactivity disorder: attrition and change during long-term treatment. J Nerv Ment Dis. 2016;204:355–63. 10.1097/NMD.0000000000000470 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.