Take Home Message
Among patients with spinal cord injury, the incidence rate for urinary stones is 16.6%. Male sex, complete spinal-cord injury, and catheter use are key risk factors. Our results offers insights for urinary stone prevention and management in this population.
Keywords: Spinal cord injury, Urinary stones, Incidence, Risk factors, Systematic review
Abstract
Background and objective
Urinary stones are a significant and common complication among patients with spinal cord injury (SCI), but epidemiological data are scarce and the evidence regarding risk factors remains unclear. Our aim was to investigate the incidence of and risk factors for urinary stones in SCI patients to provide evidence for better prevention and treatment strategies.
Methods
Relevant studies were identified from the PubMed, Web of Science, Cochrane, Embase, and Scopus databases. Literature screening, information extraction, and quality evaluation were conducted in accordance with established standards. Data analysis was performed using the metaprop and metan commands in Stata 16.0.
Key findings and limitations
A total of 65 studies involving 64 059 patients were included in the analysis. Meta-analysis using a random-effects model revealed that the overall incidence of urinary stones after SCI was 16.6% (95% confidence interval 14.1–19.3%). Over time, the incidence rate has stabilized between 15% and 20%, although annual rates varied significantly, ranging from 2.2% to 68.7%. The highest incidence was observed for bladder stones, with lower incidence rates for kidney and ureteral stones. Among the 13 factors assessed, male sex, a complete injury, and the use of intermittent, indwelling, and condom catheters were identified as independent risk factors for urinary stones.
Conclusions and clinical implications
The incidence of urinary stones after SCI is high, with a number of risk factors identified. However, further high-quality research is needed to explore additional potential risk factors.
Patient summary
We reviewed the results of previous studies on urinary stones in patients with a spinal cord injury. We found a high rate of urinary stones of about 17% for this patient group. Males are more prone to urinary stones and use of a catheter is a risk factor. More research is needed to identify other risk factors.
1. Introduction
Spinal cord injury (SCI) is a severely disabling neurological condition typically caused by incidents such as motor vehicle collisions (46%), falls (22%), violence (16%), and sports injuries (12%) [1], [2]. Currently, there are more than 27 million SCI patients worldwide, with an additional 900 000 cases occurring each year [3], [4]. SCI patients experience sensory and motor dysfunction at and below the injury site, leading to numerous complications, including secondary lung infections, deep venous thrombosis, urinary retention, urinary stones, pressure sores, pain, and psychological issues [1]. These complications are major contributors to morbidity and mortality, resulting in higher rates of hospitalization, higher health care costs, and diminished quality of life [5], [6].
Among the many complications of SCI, urinary stones are particularly common and harmful. Symptoms of urinary stones include severe pain, hematuria, nausea, and vomiting, with potential complications such as urinary tract infection (UTI) and obstruction in severe cases [7]. For SCI patients, the risk of urinary stone formation is heightened because of urinary system dysfunction, recurrent infections, and urinary retention. The partial or complete loss of sensory function in SCI patients means they often do not report discomfort caused by stones, and urinary stones are not routinely screened for in these patients [8], [9]. Consequently, the detection rate for urinary stones among SCI patients is low, which poses significant risks. Surgical management of urinary stones is more challenging in SCI patients than in the general population. Limb spasms and spinal deformities complicate surgical localization and increase anesthetic risks [10]. These factors lead to poorer stone clearance and a higher risk of postoperative complications.
Early identification and intervention for urinary stones can reduce the disease burden for SCI patients. However, the exact mechanisms and risk factors for urinary stone formation remain unclear [11]. Existing studies typically involve small case numbers and lack clear research methodologies. No targeted research has explored the incidence of and risk factors for urinary stones in the SCI population. Consequently, there is a significant gap in epidemiological data on this issue. This motivated us to perform a systematic review of related studies to explore the incidence of and risk factors for urinary stones in SCI patients to provide crucial evidence for disease prevention.
2. Methods
2.1. Research guidelines
We adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 statement and the review was prospectively registered on PROSPERO (CRD42022385360).
2.2. Inclusion and exclusion criteria
According to the PICOS (Population, Intervention, Comparator, Outcome, Study type) framework, the population was patients with SCI and the outcome was the incidence of and risk factors for urinary stones. Observational and experimental studies were eligible for the review. The intervention and comparator domains are not applicable.
The exclusion criteria were as follows: (1) patients with other comorbidities that could lead to urinary stones; (2) studies with a sample size of fewer than 30 patients; (3) studies with vague, incomplete, or non-convertible data; and (4) reviews, conference abstracts, letters, comments, and case reports.
2.3. Database searches and screening
Search terms and free words related to urinary stones, kidney stones, ureteral stones, bladder stones, urethral stones, and SCI were compiled and used to search PubMed, Web of Science, Embase, Scopus, and the Cochrane database. The search was conducted up to November 20, 2023. In addition, the reference lists of the studies included were retrospectively examined to identify any further relevant studies. Detailed retrieval strategies for different databases are provided in Supplementary Table 1. Literature screening involved an initial review of the title and abstract, followed by a full-text review. These processes were conducted independently by two researchers, with a third party resolving any discrepancies.
2.4. Information extraction and quality assessment
Baseline data were extracted from studies meeting the inclusion criteria, including author names, year of publication, country, study type, age, sample size, sex ratio, SCI location and severity, timing of injury, diagnostic methods, and follow-up duration. Data on the incidence of urinary stones (number of individuals affected) and associated risk factors were also collected. The quality of the studies was assessed using the Newcastle-Ottawa Scale (NOS), which evaluates the evidence quality in three areas: selection of the study population, comparability between groups, and outcome measurement [12]. The maximum score is 9, with scores of 1–3, 4–6, and 7–9 indicating low, medium, and high quality, respectively.
2.5. Statistical analysis
The incidence of and risk factors for urinary stones after SCI were calculated using the metaprop and metan commands in STATA 16.0 (StataCorp LLC, College Station, TX, USA), with results expressed as the effect size and corresponding 95% confidence interval (CI). A fixed-effects model was used for data analysis when p > 0.05 and I2 ≤ 50%. Otherwise, a random-effects model was applied, taking into account sources of heterogeneity. Subgroup analyses were conducted according to urinary stone location, and annual incidence rates and cumulative incidence rates over time were calculated according to the publication year. Funnel plots were generated to detect publication bias.
3. Results
3.1. Eligible studies and study characteristics
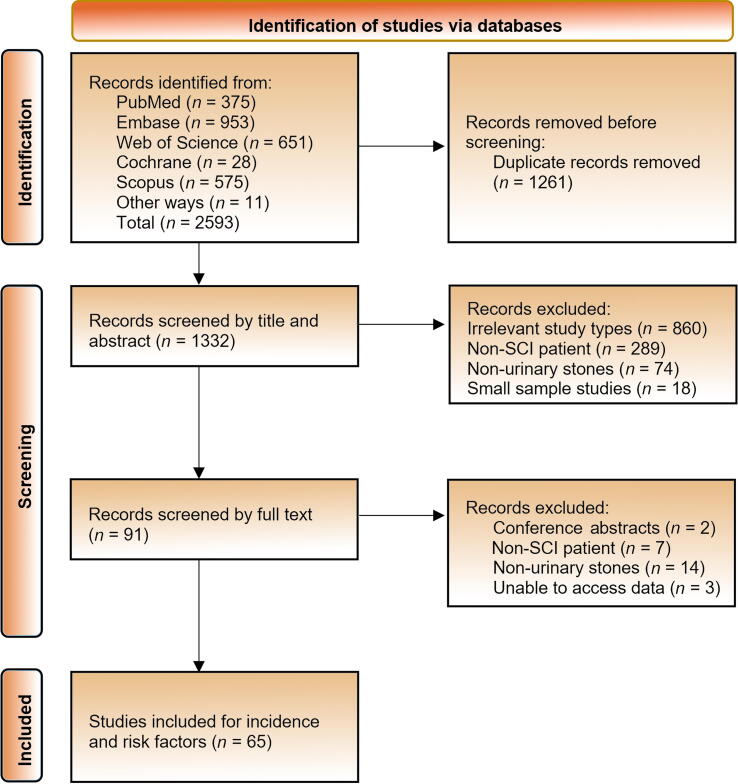
We initially identified 2593 records. After rigorous screening, 65 studies were included: 53 cohort studies, two case-control studies, and ten cross-sectional studies, as detailed in Figure 1. A total of 64 059 patients with SCI were analyzed, comprising 35 594 males and 13 040 females, with 12 studies not reporting gender ratios. The sample size in individual studies ranged from 30 to 8314. None of the studies provided detailed reports on the SCI severity or location. All of the studies included patients with chronic SCI. The diagnostic methods for urinary stones included cystoscopy, pyelography, ultrasound, and X-ray, or combinations of these techniques. Follow-up varied from 3 mo to 27 yr, with 25 studies not reporting follow-up times. Detailed information on the studies included is provided in Supplementary Table 2.
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart. SCI = spinal cord injury.
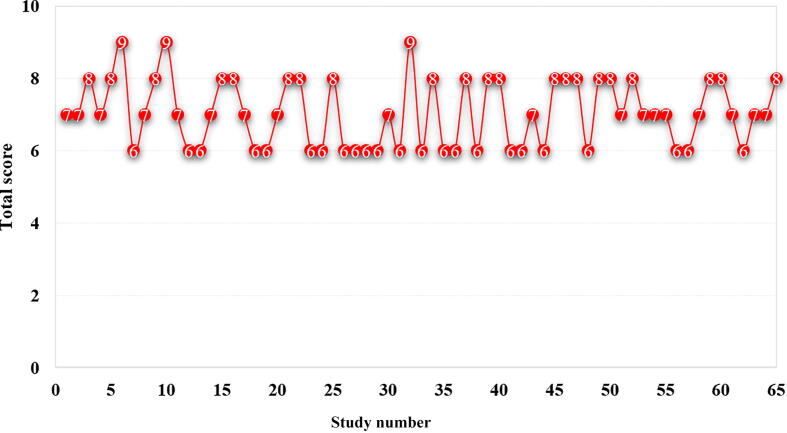
3.2. Quality assessment results
The NOS score for the studies ranged from 6 to 9 points. A total of 42 studies had high research quality, with an NOS score between 7 and 9. The remaining 23 studies had an NOS score of 6, primarily because of insufficient representativeness of the study population, unclear patient selection methods, lack of blinding for outcome assessment, and inadequate follow-up duration, which collectively lowered the evidence quality. Detailed NOS scores for individual studies are presented in Figure 2.
Fig. 2.
Newcastle-Ottawa Scale scores for the studies included in the review (numbers represent the total score for each study).
3.3. Meta-analysis results
3.3.1. Incidence of urinary stones
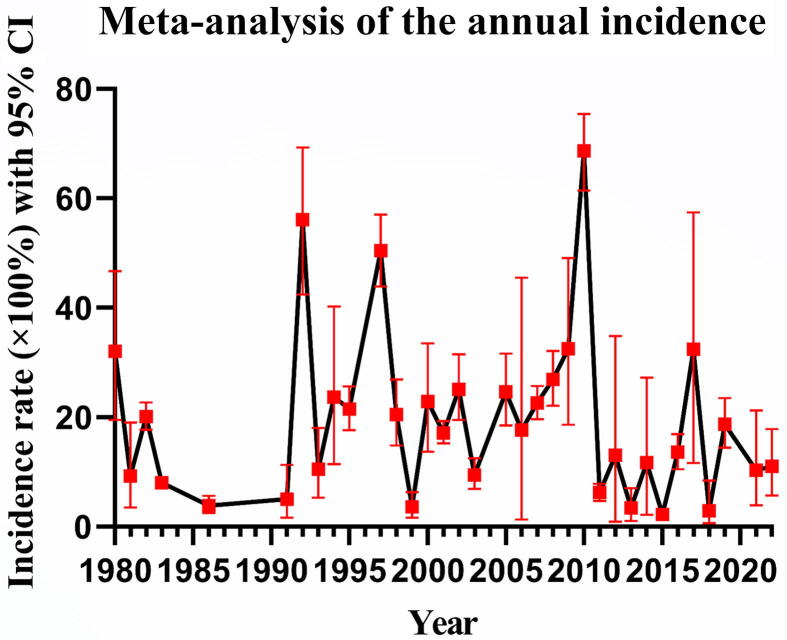
Meta-analysis results according to a random-effects model (I2 = 98.50%) revealed that the incidence of urinary stones after SCI was 16.6% (95% CI 14.1–19.3%). Bladder stones had the highest incidence, followed by ureteral and kidney stones, as detailed in Figure 3. From 1980, the incidence rate of urinary stones after SCI declined up to 1991, followed by a gradual increase, stabilizing between 15% and 20%, as shown in Figure 4. However, the annual incidence rates varied significantly, ranging from 2.2% to 68.7%, as detailed in Figure 5.
Fig. 3.
Incidence of urinary stones by type. CI = confidence interval.
Fig. 4.
Cumulative incidence of urinary stones by year of publication. CI = confidence interval.
Fig. 5.
Annual incidence of urinary stones. CI = confidence interval.
3.3.2. Factors influencing urinary stone formation
Three studies investigated 13 factors associated with urinary stone formation after SCI. Five of these were identified as significant risk factors: male sex, complete injury, intermittent catheter use, indwelling catheter use, and condom catheter use. The remaining eight factors showed no significant correlation with the incidence of urinary stones, as detailed in Supplementary Figure 1.
3.3.3. Publication bias
Publication bias was assessed using a funnel plot, which exhibited a marked asymmetric distribution, indicating a high likelihood of publication bias in the current body of research (Supplementary Fig. 2).
4. Discussion
More than 80% of patients with SCI experience urinary dysfunction, with stones being the most common complication [13], [14]. Urinary stones can lead to obstruction, sepsis, deterioration of renal function, and even loss of kidney function. Stone treatment is particularly challenging in SCI patients because of the complex anatomy of the urinary system [15]. Thus, prevention and early detection of urinary stones are crucial for these patients. However, the epidemiology of urinary stones in the SCI population is currently unclear, necessitating a systematic review of related studies to provide reliable evidence for clinical decision-making.
Despite significant advances in urological treatment for SCI patients, the prevalence of urinary stones has not markedly decreased [16]. Our analysis of data for 64 059 patients indicates that the incidence of urinary stones after SCI is 16.6%. Overall, the incidence declined from 1980 to 1991 but then increased, stabilizing between 15% and 20%. This high incidence rate for SCI patients is concerning and cannot be ignored. In fact, annual incidence rates varied significantly, ranging from 2.2% to 68.7%, and have remained above 10% over the past 5 yr. Our analysis by stone location revealed that bladder stones are the most common, followed by ureteral and kidney stones, with no reported cases of urethral stones. Bladder stones are particularly prevalent because of bladder paralysis and urinary retention, which increase residual urine and intravesical pressure. Long-term use of an indwelling catheter or suprapubic cystostomy further predisposes these patients to bladder stones. A study by Ku et al [17] found that over a period of 17 yr, 15% of SCI patients developed upper urinary tract stones, while 28% developed bladder stones. It is noteworthy that SCI patients may experience atypical renal colic because of neurological impairment, and pre-existing urinary incontinence can mask the symptoms of bladder stones [18], potentially leading to underestimation of their incidence. Therefore, regular screening for urinary stones in SCI patients is essential to reduce their disease burden, with a particular focus on the bladder [9].
Given the high incidence of urinary stones in the SCI population and the common recurrence of stones—30% of patients experience bladder stone recurrence within 1 yr, and 34% have upper urinary tract stone recurrence within 5 yr (compared to 20% in the general population)—prevention is paramount [19], [20], [21]. Identification of risk factors for urinary stone formation after SCI is crucial for effective prevention. There is currently conflicting evidence regarding these risk factors. For instance, some studies suggest that patients with complete SCI have the highest risk of stone formation [6], [22], while others do not support this association [23], [24]. Given the multifactorial nature of urinary stone formation after SCI and the potential for confounding factors, it is not surprising to see contradictory results. Therefore, we only included studies with multivariate analyses that controlled for confounders. Our results show that complete SCI is a significant risk factor for urinary stone formation. Complete SCI leads to paraplegia and quadriplegia, resulting in immobilization and an increase in bone resorption. This causes hypercalciuria, while reduced mobility can lead to urinary retention, which ultimately promotes stone formation [25]. In addition, more than 60% of SCI patients require catheterization [26], which significantly increases the risk of stone formation in comparison to individuals who are catheter-free. Our results indicate that intermittent catheterization, an indwelling catheter, and a condom catheter are all risk factors for urinary stone formation. Moreover, the incidence of urinary stones varied with the type of catheterization. Indwelling catheters were associated with higher stone incidence in comparison to intermittent and condom catheters. Indwelling catheters, which are inserted via the urethra or suprapubic area, remain in the bladder for extended periods (usually 4–6 wk) and can lead to complications such as bladder stones, UTI, and reduced bladder capacity [27]. By contrast, intermittent catheters can be inserted by the patient or caregiver at any location and removed immediately after bladder drainage, reducing the risk of UTI and other complications, thereby improving the patient’s quality of life [28], [29]. Consequently, for SCI patients who cannot avoid catheterization, intermittent catheterization is considered the best option [28]. We also found that male sex is a risk factor for urinary stone formation in the SCI population. This could be because of the disproportionate sex ratio in the studies, as approximately 79% of SCIs occur in males according to the US National Spinal Cord Injury Statistical Center. It could also be related to sex-specific exposure to risk factors. Despite our systematic search for all the relevant studies available, it is surprising that only three studies have explored risk factors for urinary stone formation after SCI, all published before 2006 [16], [17], [30]. This indicates a lack of focus on urinary stone formation in the SCI population. Our meta-analysis identified five significant risk factors for urinary stone formation, while the impact of eight other factors remains unclear. In addition, our analysis of these three studies revealed that the patient age ranged from 15 to 80 yr, and there were differences in sample sizes and sex ratios. Although all three studies focused on chronic SCI, they did not impose any restrictions in terms of SCI severity or location. As a result, the heterogeneity among these studies may compromise the reliability of the meta-analysis results. In conclusion, very few studies have explored urinary stone formation after SCI, and those that exist are of low quality. More high-quality research is needed to investigate additional risk factors.
4.1. Limitations
4.1.1. Heterogeneity
There was significant variability in terms of the study type, follow-up duration, baseline patient characteristics, SCI severity and location, and stone types across the studies included in the review that was not clearly reported, resulting in high heterogeneity.
4.1.2. Quality issues
The studies included in the review had issues related to the representativeness of the study populations, selection of participants, outcome assessment, and follow-up, all of which reduce the quality of the evidence.
4.1.3. Publication bias
The asymmetric funnel plot suggests substantial publication bias, reducing the reliability of the meta-analysis results.
4.1.4. Limited research on risk factors
Very few studies investigated risk factors for stone formation, and those available were outdated and of low methodological quality. Thus, the meta-analysis results are susceptible to inaccuracies because of low study quality and small sample effects.
5. Conclusions
Our systematic review of 65 studies involving 64 059 patients with SCI addresses the lack of epidemiological data on urinary stone formation in this population. The latest evidence indicates that the overall incidence of urinary stones after SCI is relatively high at 16.6% (95% CI 14.1–19.3%), although annual incidence rates vary widely. Bladder stones have the highest incidence. We explored 13 factors related to urinary stone formation, and identified male sex, complete injury, intermittent catheterization, indwelling catheters, and condom catheters as risk factors for urinary stone incidence, with no significant correlation for the remaining eight factors. Despite the high incidence of urinary stones after SCI, there are few studies on risk factors and the quality of the evidence is low. More high-quality research is needed to further investigate the incidence of and risk factors for urinary stone formation after SCI.
Author contributions: Mao Pang had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Pang, Yang.
Acquisition of data: W. Zhang, Shen.
Analysis and interpretation of data: W. Zhang, Shen.
Drafting of the manuscript: Shang.
Critical revision of the manuscript for important intellectual content: Pang.
Statistical analysis: Wang, Yu.
Obtaining funding: Pang.
Administrative, technical, or material support: K. Zhang.
Supervision: Yang.
Other: None.
Financial disclosures: Mao Pang certifies that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (eg, employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending), are the following: None.
Funding/Support and role of the sponsor: This work was supported by the National Natural Science Foundation of China (82102642) and the Guangdong Basic and Applied Basic Research Foundation (2023A1515010313). The sponsors played a role in approval of the manuscript.
Data sharing statement: The data sets used and/or analyzed in this review are available from the corresponding authors on reasonable request.
Associate Editor: Silvia Proietti
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.euros.2024.10.003.
Contributor Information
Yang Yang, Email: yangyang3@mail.sysu.edu.cn.
Mao Pang, Email: pangmao6@mail.sysu.edu.cn.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Ge L., Arul K., Ikpeze T., et al. Traumatic and nontraumatic spinal cord injuries. World Neurosurg. 2018;111 doi: 10.1016/j.wneu.2017.12.008. [DOI] [PubMed] [Google Scholar]
- 2.Sweis R., Biller J. Systemic complications of spinal cord injury. Curr Neurol Neurosci Rep. 2017;17:8. doi: 10.1007/s11910-017-0715-4. [DOI] [PubMed] [Google Scholar]
- 3.GBD 2016 Traumatic Brain Injury and Spinal Cord Injury Collaborators. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2019;18:56–87. [DOI] [PMC free article] [PubMed]
- 4.Ding W., Hu S., Wang P., et al. Spinal cord injury: the global incidence, prevalence, and disability from the Global Burden of Disease Study 2019. Spine. 2022;47:1532–1540. doi: 10.1097/BRS.0000000000004417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cardenas D.D., Hoffman J.M., Kirshblum S., et al. Etiology and incidence of rehospitalization after traumatic spinal cord injury: a multicenter analysis. Arch Phys Med Rehabil. 2004;85:1757–1763. doi: 10.1016/j.apmr.2004.03.016. [DOI] [PubMed] [Google Scholar]
- 6.McKinley W.O., Jackson A.B., Cardenas D.D., et al. Long-term medical complications after traumatic spinal cord injury: a regional model systems analysis. Arch Phys Med Rehabil. 1999;80:1402–1410. doi: 10.1016/s0003-9993(99)90251-4. [DOI] [PubMed] [Google Scholar]
- 7.Thongprayoon C., Krambeck A.E., Rule A.D. Determining the true burden of kidney stone disease. Nat Rev Nephrol. 2020;16:736–746. doi: 10.1038/s41581-020-0320-7. [DOI] [PubMed] [Google Scholar]
- 8.Consortium for Spinal Cord Medicine Bladder management for adults with spinal cord injury: a clinical practice guideline for health-care providers. J Spinal Cord Med. 2006;29:527–573. [PMC free article] [PubMed] [Google Scholar]
- 9.Cameron A.P., Rodriguez G.M., Schomer K.G. Systematic review of urological followup after spinal cord injury. J Urol. 2012;187:391–397. doi: 10.1016/j.juro.2011.10.020. [DOI] [PubMed] [Google Scholar]
- 10.Ramsey S., McIlhenny C. Evidence-based management of upper tract urolithiasis in the spinal cord-injured patient. Spinal Cord. 2011;49:948–954. doi: 10.1038/sc.2011.50. [DOI] [PubMed] [Google Scholar]
- 11.Spradling K., Ganesan C., Conti S. Medical treatment and prevention of urinary stone disease. Urol Clin North Am. 2022;49:335–344. doi: 10.1016/j.ucl.2021.12.007. [DOI] [PubMed] [Google Scholar]
- 12.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 13.Center N.S.C.I.S. Spinal cord injury facts and figures at a glance. J Spinal Cord Med. 2013;36:1–2. doi: 10.1179/1079026813Z.000000000136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nabbout P., Slobodov G., Culkin D.J. Surgical management of urolithiasis in spinal cord injury patients. Curr Urol Rep. 2014;15:408. doi: 10.1007/s11934-014-0408-3. [DOI] [PubMed] [Google Scholar]
- 15.Gao Y., Danforth T., Ginsberg D.A. Urologic management and complications in spinal cord injury patients: a 40- to 50-year follow-up study. Urology. 2017;104:52–58. doi: 10.1016/j.urology.2017.03.006. [DOI] [PubMed] [Google Scholar]
- 16.Chen Y., DeVivo M.J., Roseman J.M. Current trend and risk factors for kidney stones in persons with spinal cord injury: a longitudinal study. Spinal Cord. 2000;38:346–353. doi: 10.1038/sj.sc.3101008. [DOI] [PubMed] [Google Scholar]
- 17.Ku J.H., Jung T.Y., Lee J.K., et al. Risk factors for urinary stone formation in men with spinal cord injury: a 17-year follow-up study. BJU Int. 2006;97:790–793. doi: 10.1111/j.1464-410X.2006.05991.x. [DOI] [PubMed] [Google Scholar]
- 18.Dray E.V., Cameron A.P. Identifying patients with high-risk neurogenic bladder: beyond detrusor leak point pressure. Urol Clin North Am. 2017;44:441–452. doi: 10.1016/j.ucl.2017.04.010. [DOI] [PubMed] [Google Scholar]
- 19.Khan A.A., Mathur S., Feneley R., et al. Developing a strategy to reduce the high morbidity of patients with long-term urinary catheters: the BioMed catheter research clinic. BJU Int. 2007;100:1298–1301. doi: 10.1111/j.1464-410X.2007.07146.x. [DOI] [PubMed] [Google Scholar]
- 20.Chen Y., DeVivo M.J., Stover S.L., et al. Recurrent kidney stone: a 25-year follow-up study in persons with spinal cord injury. Urology. 2002;60:228–232. doi: 10.1016/s0090-4295(02)01734-x. [DOI] [PubMed] [Google Scholar]
- 21.Rule A.D., Lieske J.C., Li X., et al. The ROKS nomogram for predicting a second symptomatic stone episode. J Am Soc Nephrol. 2014;25:2878–2886. doi: 10.1681/ASN.2013091011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DeVivo M.J., Fine P.R. Predicting renal calculus occurrence in spinal cord injury patients. Arch Phys Med Rehabil. 1986;67:722–725. doi: 10.1016/0003-9993(86)90003-1. [DOI] [PubMed] [Google Scholar]
- 23.Ku J.H., Choi W.J., Lee K.Y., et al. Complications of the upper urinary tract in patients with spinal cord injury: a long-term follow-up study. Urol Res. 2005;33:435–439. doi: 10.1007/s00240-005-0504-4. [DOI] [PubMed] [Google Scholar]
- 24.Kohli A., Lamid S. Risk factors for renal stone formation in patients with spinal cord injury. Br J Urol. 1986;58:588–591. doi: 10.1111/j.1464-410x.1986.tb05891.x. [DOI] [PubMed] [Google Scholar]
- 25.Burr R.G., Chem C., Nuseibeh I. Creatinine, calcium, citrate and acid-base in spinal cord injured patients. Paraplegia. 1993;31:742–750. doi: 10.1038/sc.1993.116. [DOI] [PubMed] [Google Scholar]
- 26.Lai E.C., Kao Yang Y.H., Kuo H.C. Complication rate of neurogenic lower urinary tract dysfunction after spinal cord injury in Taiwan. Int Urol Nephrol. 2014;46:1063. doi: 10.1007/s11255-013-0625-6. [DOI] [PubMed] [Google Scholar]
- 27.Linsenmeyer T.A. Catheter-associated urinary tract infections in persons with neurogenic bladders. J Spinal Cord Med. 2018;41:132–141. doi: 10.1080/10790268.2017.1415419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.De Ridder D.J., Everaert K., Fernandez L.G., et al. Intermittent catheterisation with hydrophilic-coated catheters (SpeediCath) reduces the risk of clinical urinary tract infection in spinal cord injured patients: a prospective randomised parallel comparative trial. Eur Urol. 2005;48:991–995. doi: 10.1016/j.eururo.2005.07.018. [DOI] [PubMed] [Google Scholar]
- 29.Hill T.C., Baverstock R., Carlson K.V., et al. Best practices for the treatment and prevention of urinary tract infection in the spinal cord injured population: the Alberta context. Can Urol Assoc J. 2013;7:122–130. doi: 10.5489/cuaj.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen Y., DeVivo M.J., Lloyd L.K. Bladder stone incidence in persons with spinal cord injury: determinants and trends, 1973–1996. Urology. 2001;58:665–670. doi: 10.1016/s0090-4295(01)01374-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.