Abstract
The use of nail–plate constructs has been suggested for treatment of elderly patients with distal femur fractures to facilitate stable fixation and early ambulation. In this article, we describe a technique to link the 2 implants without the use of fluoroscopic “perfect-circle” technique. This technique can be used with implants from different manufacturers.
Keywords: distal femur fracture, nail plate, retrograde nail, distal femur plate
1. Introduction
Distal femur fractures can be challenging to treat because of the presence of osteoporosis, comminution, and the short segment of bone available for fixation. Locked lateral plate mechanical failure rates range from 7% to 22%.1–3
Recently, there have been some reports of use of nail–plate combinations in distal femur fractures.4–7 The use of a nail and a plate would make a mechanically stiffer construct that may be less prone to mechanical failure, especially in osteoporotic bone or medial comminution. Such a construct may also allow for earlier weight bearing.
Occasionally, it may be desirable to link the 2 implants to create a more stable construct or to minimize implant traffic. We describe a simple technique to link a retrograde nail and a distal femur plate that does not rely on the fluoroscopic “perfect-circle” technique.
2. Technique Description
An anterolateral approach to the distal femur is performed for plate fixation, and the fracture is reduced using direct or indirect reduction techniques according to the surgeon's preference. Then, a short incision is performed over the anterior knee for a medial parapatellar or transpatellar approach that will be used for the retrograde nail insertion. The guide wire is inserted, the pilot hole is opened, and then, the canal is reamed. The length of the nail (short or long) depends on the surgeon's preference and presence of any previous implants in the proximal femur. Most of the time, our technique uses a smaller diameter retrograde femoral nail (9 or 10 mm, depending on the implant company).
The retrograde nail is inserted first, with the targeting handle assembled so it is placed medially to avoid interference with the targeting jig of the lateral plate. The depth of insertion is verified with lateral fluoroscopic imaging of the knee. An incision is made medially for the most distal locking hole of the nail. The appropriate drill bit is used, and a hole is drilled from medial to lateral, with the drill bit left in place protruding slightly through the lateral cortex of the distal femur (Fig. 1).
Figure 1.
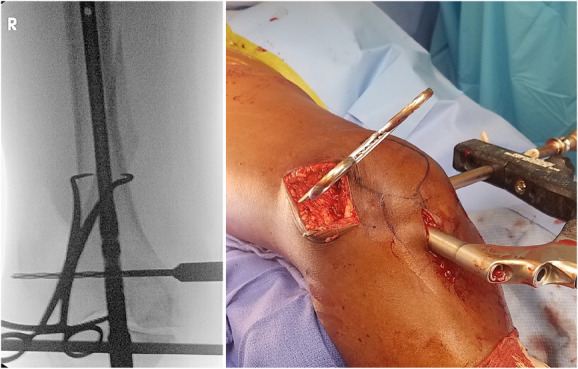
Fluoroscopic and clinical images of a patient with right distal femur fracture. The retrograde nail is inserted, the distal most locking screw is drilled from medial to lateral, and the drill bit is left prominent laterally.
The appropriate length of the distal femur plate (proximal end of the plate at the level of lesser trochanter) is then inserted and advanced submuscularly. The plate is then positioned at the distal femur, so that the protruding drill bit will be passed through one of the holes of the plate that would give the best fit (Fig. 2). This is usually the most distal and anterior plate hole. If a good fit cannot be achieved, then the previously inserted drill bit is retracted, the nail insertion depth is adjusted, or the nail is rotated slightly, and a new drill hole is made from medial to lateral and the plate is positioned over the drill bit. In clinical practice, we have not encountered any incidents where the rotation of the nail made proximal locking unsafe. This is probably due to the small amount of rotation required to properly align the nail screw trajectory with one of the distal plate holes.
Figure 2.
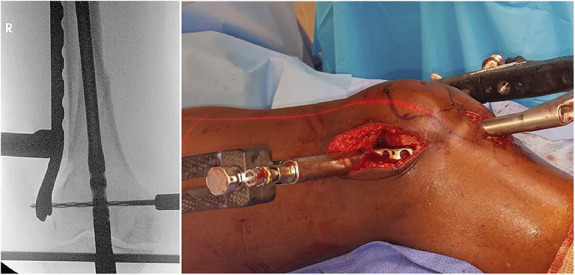
Fluoroscopic and clinical images demonstrating the inserted plate with the most distal anterior plate hole passed through the protruding tip of the drill bit.
If the nail's proximal locking options are lateral to medial only, it should be locked proximally before plate fixation to avoid interference between the plate and the screw path. If the nail has anterior-to-posterior proximal locking options, then the proximal locking screw can be placed before or after plate fixation as the plate would not interfere with the perfect-circle technique.
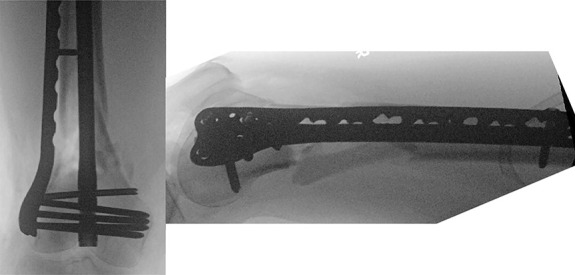
The plate is then provisionally fixed proximally with a wire and compressed against the distal femur with a large periarticular clamp. Then, the appropriate-length screw from the distal femur plate system is inserted from the lateral side as the drill bit is pulled back from the medial side. This way linking of the 2 implants is ensured (Fig. 3).
Figure 3.
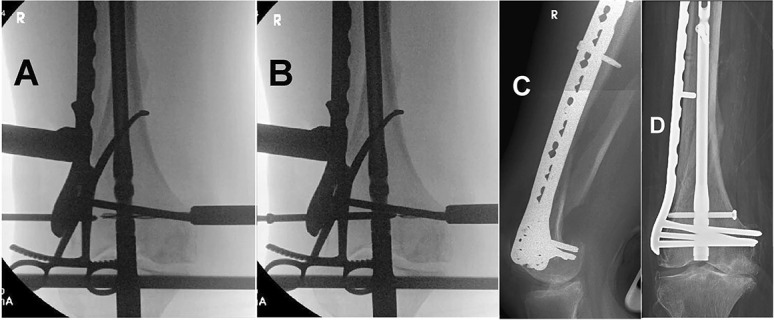
A, The plate is compressed against the distal femur with a large clamp. A (nonlinking) screw has been inserted to hold the position of the plate. B, The drill is pulled back from the medial side as the screw linking the plate to the nail is inserted from the lateral side. C and D, Immediate postoperative radiographs.
An alternative way to link the implants is to remove the drill bit and pass the appropriate guide wire from medial to lateral, followed by insertion of a cannulated screw through the guide wire from lateral to medial (Figs. 4 and 5). We have found that this facilitates the insertion of a second linking screw because cannulation helps to overcome slight imperfections in the alignment between the plate and the nail holes. A limitation to this alternate way of linking is that not all distal femur plate systems have cannulated screws.
Figure 4.
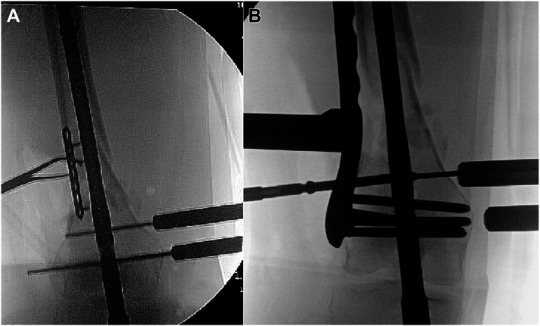
A, A 63-year-old woman with type 3A open distal femur fracture with bone defect. A temporary mini-plate is used to hold reduction. A short retrograde nail is inserted, and both distal locking screws are drilled from medial to lateral. B, The first linking screw has been inserted through the distal-most nail locking hole. Owing to imperfection of the alignment between the plate screw hole and the proximal-most nail locking hole, linking with a second screw is facilitated with the use of a guide wire inserted from medial to lateral, followed by insertion of a cannulated screw from the distal femur plate system from lateral to medial.
Figure 5.
Final fluoroscopic images of the case in Figure 4, demonstrating the 2 linking screws.
We typically use a locking screw to link the 2 implants as the distal femur plate we use has variable angle locking holes (VA LCP condylar plate, DePuy Synthes, West Chester, PA). Alternatively, if this option is not available, a 4.5 cortical screw from the plate system or 5.0 screw from the nail system may be used to link the 2 implants.
The rest of the screws through the plate or through the nail are inserted according to the surgeon's preference. In an attempt to avoid making the construct overly stiff, we use less screws in the plate compared with the number of screws we would have used if the plate was the only implant. Similarly, in the nail, we use less screws than we would have used if the nail was the only implant: 1 screw proximally and 2 screws distally (one or both of them linked with the plate).
3. Clinical Series
From June 2018 to December 2021, 11 patients were treated with a nail–plate construct using the described technique (8 native distal femur fractures and 3 fractures above the femoral component of a total knee arthroplasty). All patients were female, and all had a preoperative diagnosis of osteoporosis and intraoperative findings of poor bone quality. All patients were treated operatively by a single fellowship-trained orthopaedic trauma surgeon using a distal femur plate (VA LCP condylar plate, DePuy Synthes, West Chester, PA) and a retrograde femoral nail. Nail sizes and manufacturers are listed in Table 1.
TABLE 1.
Patient Demographics
| Patient | Age | Sex | Fracture Type and Classification | Nail Size and Manufacturer | Outcome/Follow-up |
| Patient #1 | 81 | Female | Su type 1 | 10 mm × 340 mm (Smith&Nephew) | Well-maintained alignment/fixation, healed fracture |
| Patient #2 | 72 | Female | 33C2 | 10 cm × 160 cm (Synthes) | Well-maintained alignment/fixation, healed fracture |
| Patient #3 | 69 | Female | 33C2 | 9 mm × 240 mm (Stryker) | Well-maintained alignment/fixation, healed fracture |
| Patient #4 | 71 | Female | Su type 3 | 9 mm × 220 mm (Synthes) | Required bone grafting + addition of a medial plate for nonunion |
| Patient #5 | 70 | Female | 33A3 | 12 mm × 240 mm (Synthes) | Well-maintained alignment/fixation, healed fracture |
| Patient #6 | 63 | Female | 33A3, type 3A open | 10 mm × 220 mm (Synthes) | Required planned removal of cement spacer and bone grafting |
| Patient #7 | 76 | Female | 33C3, type 3A open | 9 mm × 220 mm (Synthes) | Well-maintained alignment/fixation, healed fracture |
Institutional review board approval was obtained. The use of patient data was approved by the committee on research ethics in accordance with the Declaration of the World Medical Association and informed consent from patients was obtained as required. Each patient's electronic medical record was reviewed to collect demographic information and intraoperative and postoperative records. Preoperative, intraoperative, and postoperative radiographs were reviewed. Bony union was defined as bridging callus on at least 3 cortices with an absence of pain on clinical history and examination. The postoperative rehabilitation protocol was not standardized and was modified depending on local parameters (intraarticular extension or bone defect); 5 patients were weight bearing as tolerated, 1 patient was 50% weight bearing for 6 weeks, and 1 patient was toe-touch weight bearing for 6 weeks followed by 4 weeks of 50% weight bearing. Patients completed 24 hours of postoperative antibiotics and received deep venous thombosis prophylaxis for 6 weeks.
All patients tolerated their procedure well, and no intraoperative complications were observed. 4 patients had less than 6 months of follow-up and were excluded from the series (1 patient died 2 months postoperatively because of pulmonary embolism and 3 patients were lost to follow-up). Therefore, 7 patients were available for review with a mean follow-up of 10.8 ± 4.3 months. The mean age of the patients was 71.7 ± 5.6 years. No patients had implant loosening or failure. 1 patient with morbid obesity, diabetes, and rheumatoid arthritis developed nonunion and underwent autologous bone grafting and addition of a medial plate at 6 months postoperatively. After this procedure, the fracture healed uneventfully. Another patient with type 3A open distal femur fracture with bone defect underwent planned removal of cement spacer and autologous bone grafting at 2 months postoperatively, with uneventful healing. All other patients went on to demonstrate clinical and radiographic union at 6 months of follow-up (Table 1).
4. Discussion
The concept of linking implants has been previously published.8,9 The combined use of a plate and a nail for the treatment of distal femur fractures has been reported recently, as mechanical failure of plates or nails alone has been ranging from 4% to 22%.3,10 Osteoporosis, obesity, medial cortex comminution, and limited amount of bone for fixation in very distal fractures can contribute to inadequate fixation and failure. The retrograde nail resists the cantilever bending forces at the fracture site that exist with a plate alone. The more stable construct allows full weight bearing immediately postoperatively, which is the current protocol in our institution. Although it is unknown how much stiffness of a construct is optimal, the surgeon may elect to link the 2 implants. Owing to the overlapping of the implants, it is challenging to align the plate and the nail holes with fluoroscopy. The technique described to link the nail with the plate relies on visual feedback and not on fluoroscopic targeting.
There is a theoretical concern of galvanic corrosion when 2 different metals (stainless steel and titanium) are in contact, but in clinical practice, this has not been a problem.11 Alternatively, to avoid this, the surgeon may elect to use a titanium lateral locking plate.
The technique of linking a lateral distal femur implant and a retrograde nail recently became available through dedicated instrumentation (Locking Attachment Washer—RFN Advanced, Depuy Synthes, West Chester, PA). However, our technique does not rely on specific instruments and is applicable to implants from different companies.
Most retrograde femur nail systems use 5.0-mm distal locking screws, and most distal femur plate systems use screws 4.5–5.0 mm in diameter; thus, placing screws between the 2 implants is feasible.
In some nailing systems, the distal locking holes are threaded. In these cases, the surgeon should be aware that the threads of the screw from the plating system that links the 2 implants may cross-thread in the nail locking hole and this will prevent further advancement of the screw. To avoid this, we use the screw from the nailing system to link the 2 implants.
One more point to discuss is that while some retrograde femoral nail designs allow for medial placement of the aiming arm (Synthes Expert R/AFN, Stryker T2 A/R Femoral Nail) in other systems, the aiming arm extends on both sides of the distal femur (Synthes RFN-Advanced, Stryker T2 Alpha Femur Retrograde Nail, Smith&Nephew Trigen Meta-Nail Retrograde Femoral Nail, Zimmer Biomet Phoenix Retrograde Femoral Nail). This may interfere with the aiming arm of the distal femur plate. To overcome this, the aiming arm can be disconnected from the insertion handle as soon as the drill bit has been inserted from medial to lateral through the most distal nail hole.
In conclusion, we describe a technique for linking a distal femur plate and a retrograde femoral nail that can be used across different implant companies, offers less implant traffic, and does not require fluoroscopic targeting.
Footnotes
This research received no specific grant or funding from any agency, commercial, or nonprofit sectors.
The authors have no conflict of interest related to the contents of this manuscript.
Contributor Information
Ashley Force, Email: force@montefiore.org.
Sandip Tarpada, Email: sptarpada@gmail.com.
Yelena Bogdan, Email: ybogdan@gmail.com.
Milan K. Sen, Email: msenmd@gmail.com.
References
- 1.McDonald TC, Lambert JJ, Hulick RM, et al. Treatment of distal femur fractures with the DePuy-synthes variable angle locking compression plate. J Orthop Trauma. 2019;33:432–437. [DOI] [PubMed] [Google Scholar]
- 2.Ricci WM, Streubel PN, Morshed S, et al. Risk factors for failure of locked plate fixation of distal femur fractures: an analysis of 335 cases. J Orthop Trauma. 2014;28:83–89. [DOI] [PubMed] [Google Scholar]
- 3.Tank JC, Schneider PS, Davis E, et al. Early mechanical failures of the Synthes variable angle locking distal femur plate. J Orthop Trauma. 2016;30:e7–e11. [DOI] [PubMed] [Google Scholar]
- 4.Yoon RS, Patel JN, Liporace FA. Nail and plate combination fixation for periprosthetic and interprosthetic fractures. J Orthop Trauma. 2019;33(suppl 6):S18–S20. [DOI] [PubMed] [Google Scholar]
- 5.Liporace FA, Yoon RS. Nail Plate combination technique for native and periprosthetic distal femur fractures. J Orthop Trauma. 2019;33:e64–e68. [DOI] [PubMed] [Google Scholar]
- 6.Hussain MS, Dailey SK, Avilucea FR. Stable fixation and immediate weight-bearing after combined retrograde intramedullary nailing and open reduction internal fixation of noncomminuted distal interprosthetic femur fractures. J Orthop Trauma. 2018;32:e237–e240. [DOI] [PubMed] [Google Scholar]
- 7.Kanabur P, Sandilands SM, Whitmer KK, et al. Nail and locking plate for periprosthetic fractures. J Orthop Trauma. 2017;31:e425–e431. [DOI] [PubMed] [Google Scholar]
- 8.Venkateswaran B, Smith RM. Extending fixation beyond the working length of an intramedullary nail with a linked intramedullary and extramedullary fixation in complex femoral fractures; a brief series. Injury. 2001;32:719–724. [DOI] [PubMed] [Google Scholar]
- 9.Mast J, Jakob R, Ganz R. Planning and Reduction Technique in Fracture Surgery. Berlin: Springer; 2011. [Google Scholar]
- 10.Herrera DA, Kregor PJ, Cole PA, et al. Treatment of acute distal femur fractures above a total knee arthroplasty: systematic review of 415 cases. Acta Orthop. 2008;79:22–27. [DOI] [PubMed] [Google Scholar]
- 11.Høl PJ, Mølster A, Gjerdet NR. Should the galvanic combination of titanium and stainless-steel surgical implants be avoided? Injury. 2008;39:161–169. [DOI] [PubMed] [Google Scholar]


