Abstract
Background
Various strategies, each with its own set of limitations, are available for managing lumbar spondylolysis. In response, our department has developed an innovative solution: a V-shaped titanium cable integrated with a pedicle screw internal fixation system specifically designed for lumbar spondylolysis in young adults.
Aim
The objective of this study was to thoroughly investigate the long-term efficacy of V-type titanium cable internal fixation for the management of spondylolysis, especially in young adults.
Methods
Twenty-one patients with fifth lumbar spondylolysis were treated using V-shaped titanium cables and pedicle screw internal fixation at the General Hospital Xinjiang Military Command. The duration of low back pain before surgery was 6 ~ 48 (15.85 ± 11.57) months. The Medtronic (S7) navigation system was used during surgery to guide the placement of pedicle screws, aiming to avoid damaging the L4-5 facet joint by positioning the screws lower and further to the side. Intraoperative indices (operative time and intraoperative blood loss) were recorded. The visual analog scale (VAS), Oswestry Disability Index (ODI), pelvic incidence (PI), and intraoperative imaging measurements of screw accuracy were meticulously recorded and assessed in a comprehensive manner. This thorough evaluation was conducted both intraoperatively and throughout the follow-up period, which lasted for at least one year.The Macnab efficacy criteria were used to assess postoperative outcomes during the final follow-up period.
Results
All patients successfully completed the 1-year follow-up on time. Two patients experienced postoperative wound liquefaction and successfully recovered after undergoing dressing changes. The average duration of the surgical procedure was 113.09 ± 6.97 min, and an intraoperative blood loss of 50.47 ± 21.32 millilitres was observed. Significant differences were noted in visual analog scale (VAS) scores before and after surgery at various time intervals, indicating improvement with the progression of rehabilitation exercises. No significant changes were found in the pelvic incidence (PI), and there were no notable differences between the preoperative and postoperative periods. No loosening, breakage, or failure of the internal fixation was found during the long-term follow-up. Furthermore, there were no serious complications, such as infection or vascular or nerve injuries. occurred during the procedure. A patient who presented with a considerable cryptic fissure of sacrum 1 experienced dural injury during the surgical procedure. Intraoperatively, dural sutures were skillfully applied, and the adjacent muscles were fortified. Remarkably, the patient achieved successful healing in a single stage. On the first day postsurgery, a gradual improvement in mobility was noted.
Conclusions
The use of a V-shaped titanium cable in conjunction with a pedicle screw internal fixation system for the management of fifth lumbar spondylolysis in young individuals is characterized by its ease of execution and ability to yield favorable outcomes. This approach relies on the prerequisite that patients with minimal intervertebral disc injury or mild lumbar spondylolisthesis demonstrate high overall success rates but experience low failure rates associated with internal fixation. Most significantly, this technique involves segmental internal fixation, which safeguards the functional spinal unit (FSU).
Keywords: Lumbar, Spondylolysis, Young adult, V-type titanium cable system
Introduction
Spondylolysis is a prevalent condition in spinal surgery [1]. Disruptions or defects in bone structure within the upper and lower articular processes and transverse processes of the lumbar spine are often observed. Anatomical and biomechanical factors play a crucial role in spinal health, with the fifth lumbar vertebra being the most commonly affected. The intricate interplay of anatomical structures and biomechanical forces in this region often leads to specific vulnerabilities and conditions [2]. The presence of isthmus defects or fissures that can lead to spondylolisthesis was initially identified by Robert in 1855. The definition of spondylolysis of the lumbar spine was officially recognized in 1884 when Neugbauer confirmed its congenital origin. Further research has revealed variations in incidence based on race, sex, and physical activity level [3].
Fredrickson et al. [4] reported that the prevalence of spondylolysis at age 6 was 4.4%, which increased to 6% in adults and rose significantly to 15% in adolescents who engaged in repetitive stretching exercises involving the lumbar spine [5].
The management of spondylolysis encompasses conservative approaches, such as rest, analgesia, physiotherapy, and local injection [6]. Surgical intervention may be considered if symptoms persist despite more than 6 months of conservative treatment and if the patient’s quality of life urgently needs improvement [7]. Currently, there are diverse surgical options for treating spondylolysis [8]. However, conventional surgery has inherent limitations and lacks a standardized surgical protocol for managing this condition [9–12].
In 2010, our team developed a modified surgical technique involving pedicle screw spinous process steel-wire fixation after isthmic bone grafting for adolescents who presented with isthmus fissures and prominent symptoms. However, during long-term patient follow-up, we observed instances of failed isthmic healing or wire fracture in some patients. Additionally, postoperative magnetic resonance imaging was not feasible due to the presence of internal wire fixation. To address these limitations and enhance treatment efficacy for young patients with fifth spondylolysis, we implemented a V-type titanium cable internal fixation system. This paper aims to present our modified surgical approach.
Materials and methods
After the Institutional Review Board’s written approval, a retrospective study was conducted between January 2020 and October 2021. Twenty-one patients with fifth lumbar spondylolysis who underwent surgery involving V-type titanium cable internal fixation at the General Hospital of Xinjiang Military Region were enrolled in the study. The inclusion criteria were as follows: (1) bilateral spondylolysis of the fifth lumbar vertebra was confirmed by X-ray and CT examination, and the diagnosis was confirmed; (2) symptoms were not relieved after conservative treatment for up to 6 months; and (3) Pfirrmann classification was I, II, or III. The following patients were excluded: (1) magnetic resonance imaging (MRI) results indicated prominent protrusion of the intervertebral disc, either with or without associated symptoms of nerve root or cauda equina irritation; (2) previous history of spinal disease; (3) lumbar spondylolisthesis Meyerding grade II or above; and (4) a 1-year follow-up could not be completed within the designated timeframe.
Surgical procedures
The patients were placed in the prone position on a Jackson surgical table, with a support pad positioned in the anterior chest and lumbar region. A C-arm X-ray machine was used to locate and mark the lesion before the operation, and the lesion was cut longitudinally along the fifth lumbar spinous process to avoid injury to the supraspinous and interspinous ligaments. The discontinuous cortices in the isthmus of the fifth lumbar pedicle were exposed. The Medtronic (S7) navigation system was used during surgery to guide the placement of pedicle screws, aiming to avoid damaging the L4-5 facet joint by positioning the screws lower and further to the side, followed by complete removal of local hypertrophic scar tissue and sclerotic bone tissue. A carefully prepared rectangular bone graft bed was created. The posterior superior iliac spine was used as a source for the iliac bone graft, which was then implanted into the isthmus bone graft bed. Additionally, the bone graft was reinforced on the lamina surface. On each side of the fifth lumbar pedicle, a pedicle screw was inserted (the entry point was slightly caudal and lateral), leaving a 4 mm gap for the titanium cable to be threaded through. A specially designed patented cable guide was utilized for traversing pedicle screws to minimize potential soft tissue damage, and a patented cable guide passed through the.
caudal root of the lumbar spinous process (specification: handle length 13.0 cm, semicircular arc straight diameter 2.8 cm, channel straight diameter 0.3 cm) (Fig. 1). The titanium cable was threaded through the base of the spinous process, encircling the root of the screws in both pedicles (Fig. 2). After tightening the titanium cable under pressure, the pedicle screw was further tightened to increase the pressure on the bone graft site. The lytic lesion was covered by the cable wire.All patients underwent surgery performed by a consistent surgical team (Figs 3 and 4).
Fig. 1.

a The titanium cable passes through the base of the junction between the spinous process and the laminae on the left oblique dorsal view of the spine. The pedicle screw entry point was located in the punctular cavity of the left pedicle. b Frontal and posterior views of a spinal model, demonstrating the simulated operation with a miniature cable guide
Fig. 2.

Case example. This pertains to a patient diagnosed with L5 isthmic spondylolysis. Refinement of the intraoperative situation of pedicle screw internal fixation with a V-type titanium cable system
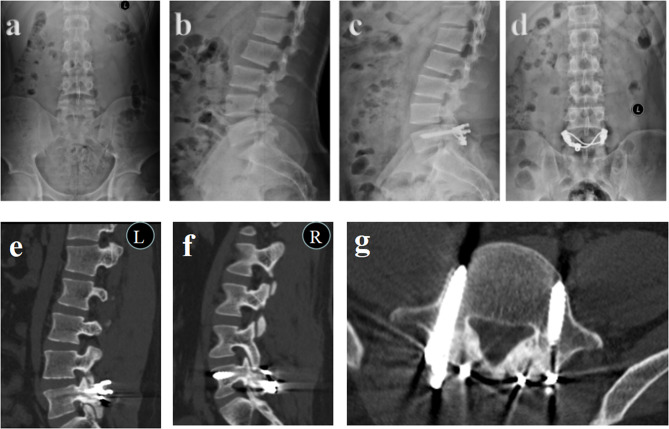
Fig. 3.
Patient 1. A 19-year-old male patient presented with chronic lower back pain that had persisted for 2 years and exacerbated over the past six months. (a) Preoperative coronal and (b) sagittal X-rays. (c) Half-year follow-up postoperative coronal and (d) sagittal X-rays. (e) Left and (f) right CT scans at the 1-year follow-up. (g) CT cross section showing good continuity of the bilateral isthmus cortex in L5
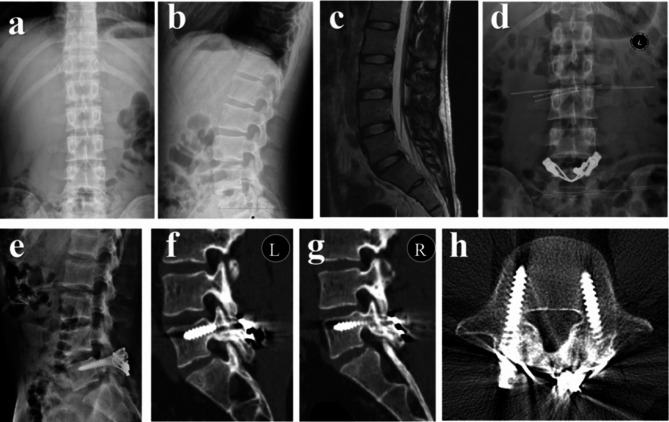
Fig. 4.
Patient 2. A 25-year-old male patient presented with chronic lower back pain that had persisted for 1 year and exacerbated over the past six months. (a) Preoperative coronal and (b) sagittal X-rays. (c) Preoperative lumbar spine MR image. (d) Half-year follow-up postoperative coronal and (e) sagittal X-ray images. (f) Left and (g) right CT scans at the 1-year follow-up. (h) CT cross section showing good continuity of the bolateral isthmus cortex in L5
Postoperative management
Following surgery, the standard procedure for all patients was to receive antibiotics for the initial 24 h. On the second day following surgery, it is recommended to utilize soft lumbar support and gradually initiate downward movement. The patient’s mobility gradually progressed to functional exercises. A rigid girth brace should be worn for a duration of 6 weeks following surgery before it can be removed.
Preoperatively, at 3 and 6 months postsurgery and at the final follow-up, patients were.
assessed via the visual analog scale (VAS) for lumbar and leg pain, as well as the Oswestry Disability Index (ODI). During the final follow-up, the modified MacNab criteria, categorized as excellent, good, fair, or poor, were utilized to evaluate the patients’ satisfaction with the surgical outcomes. The integrity and healing status of the.
internal fixator were assessed through lumbar spine X-rays, CT scans. CT reconstruction was performed to evaluate the status of bone graft fusion.
Statistical analysis
SPSS Statistics software version 26.0 was used for the statistical analysis. All the data were analyzed using a normal distribution test. The mean ± SD was used to represent normally distributed measurement data. Student’s t test was used to compare normally distributed measurement data. Conversely, a nonparametric Mann‒Whitney U test was applied to compare two groups if the data did not display a normal distribution, with the data expressed as medians and interquartile ranges. Repeated measures analysis of variance was used to compare the observed values of each index at different time points. P < 0.05 was considered to indicate statistical significance.
Results
Twenty-one patients who underwent V-type titanium cable internal fixation for young adult fifth lumbar spondylolysis were enrolled in the study. All patients were followed up for more than one year after surgery (Fig. 2). All patients were followed up for 12 ~ 22 (17.04. ±3.01) months (Table 1). Over time, the VAS score decreased gradually, and there was an obvious difference in the VAS score at different time points before and after surgery (P < 0.00). There were no significant differences in the PI or ODI between the various follow-up periods (P > 0.05) (Table 2).
Table 1.
Patient characteristics
| Age (year) |
Pfirrmann classification | Time of illness (months) |
operative time(min) | Blood loss (ml) |
Follow up(months) | Complications | |
|---|---|---|---|---|---|---|---|
| 1 | 23 | Grade I | 12 | 110 | 50 | 12 | N |
| 2 | 26 | Grade II | 48 | 115 | 50 | 14 | N |
| 3 | 19 | Grade I | 24 | 115 | 80 | 16 | N |
| 4 | 22 | Grade I | 24 | 110 | 50 | 20 | N |
| 5 | 27 | Grade II | 6 | 125 | 50 | 22 | Wound delayed union |
| 6 | 23 | Grade I | 17 | 120 | 30 | 14 | N |
| 7 | 23 | Grade III | 6 | 100 | 40 | 12 | N |
| 8 | 21 | Grade I | 6 | 120 | 50 | 22 | N |
| 9 | 19 | Grade I | 12 | 105 | 50 | 20 | N |
| 10 | 22 | Grade II | 8 | 110 | 50 | 16 | N |
| 11 | 20 | Grade I | 12 | 115 | 50 | 12 | N |
| 12 | 23 | Grade I | 12 | 115 | 60 | 18 | Wound delayed union |
| 13 | 20 | Grade I | 12 | 110 | 50 | 22 | N |
| 14 | 23 | Grade I | 9 | 105 | 45 | 20 | N |
| 15 | 20 | Grade I | 36 | 105 | 45 | 19 | N |
| 16 | 24 | Grade III | 17 | 125 | 60 | 17 | NN |
| 17 | 22 | Grade I | 6 | 110 | 50 | 15 | N |
| 18 | 23 | Grade I | 12 | 105 | 60 | 22 | N |
| 19 | 20 | Grade I | 12 | 120 | 50 | 18 | dural injury |
| 20 | 26 | Grade I | 6 | 115 | 50 | 15 | N |
| 21 | 22 | Grade I | 36 | 120 | 50 | 12 | N |
Table 2.
Comparison of the VAS score and PI before and after surgery in 21 young adult patients with fifth lumbar spondylolysis
| Preoperation | 3 months | 6 months | 1 year | P | |
|---|---|---|---|---|---|
| VAS | 6.95 ± 1.24 | 3.62 ± 0.92 | 2.28 ± 0.71 | 1.28 ± 0.78 | 0.00 |
| PI | 46.60 ± 1.73 | 46.56 ± 1.80 | 46.64 ± 1.74 | 46.60 ± 1.28 | 0.60 |
| ODI | 32.67 ± 2.87 | 20.47 ± 4.28 | 15.14 ± 3.52 | 10.33 ± 3.29 | 0.00 |
Most fractures were successfully unionized. The rate of fracture healing improved with follow-up time. At the last follow-up, 19 patients had bilateral isthmus union. Unilateral isthmic fusion was achieved in 2 patients. The bilateral healing rate achieved an impressive 90.47%. According to the MacNab criteria, the results were excellent in 16 patients, good in 3 patients, fair in 1 patient, and poor in 1 patient (Table 3).
Table 3.
Evaluation of postoperative effects according to the Macnab efficacy criteria
| Outcome | Numbers/percentage | |||
|---|---|---|---|---|
| Excellent | Good | Fair | Poor | |
| 16 | 3 | 1 | 1 | |
No intraoperative vascular injury complications or neurological cord injury were observed in the study. Two patients experienced postoperative wound liquefaction and successfully recovered after undergoing dressing changes. Moreover, there was no secondary lumbar spondylolisthesis, no obvious ASD, and no breakage or loosening of the internal fixator. A patient who presented with significant sacral cryptorchism experienced unfortunate dural injury during the surgical procedure. Intraoperatively, a skilled dural suture was applied to fortify the adjacent muscle.
Discussion
The etiology of spondylolysis remains largely unclear [13]. In addition to familial inheritance, fatigue fractures and traumatic injuries, long-term intense training can also contribute to the development of lumbar spondyloysis, which is a common cause of low back pain in young athletes [14, 15].A study conducted at the University of Connecticut School of Medicine in the United States suggested that repetitive lumbar extension exercises are responsible for symptomatic spondylolysis or isthmic spondylolisthesis (IS), with approximately 9% of baseball pitchers experiencing lower back pain due to lumbar spondylolysis [16]. Furthermore, Kimberly A et al. [16] confirmed that spondylolysis represents a transition from quadrupedal locomotion to bipedal walking. Spondylolysis is among the most prevalent causes of lower back pain and contibutes significantly to the global disease burden [16–18].It not only impacts human well-bing but also poses an economic burden. When conservative treatment fails for at least six months and there is evidence of disc degeneration, surgical intervention becomes necessary. Direct repair surgery for restoring integrity in patients with spondylolysis is widely considered the preferred treatment option [19–22].
Currently, there are two surgical approaches for the treatment of lumbar spondylolysis. These techniques include intrasegmental isthmus repair and interbody fusion between the affected vertebra and the adjacent lower vertebra. The latter method employs intervertebral bone grafting to facilitate fusion between the implicated and lower vertebral bodies, thereby restoring spinal structural stability and enhancing physiological function. Interbody fusion offers evident advantages in terms of stability and biomechanics compared to traditional surgery; however, it inevitably leads to FSU loss while also increasing the risk of ASD [22, 23].
In 1968, Kimura [24] pioneered the concept of direct repair for spondylolysis through intersegmental bone grafting, aiming primarily to restore normal vertebral body anatomy while minimizing interference with neurological and surgical clearance. Patients undergo a two-month bed rest immobilization period and wear a cast until union of the spondylolysis is achieved. Dai [25] enhanced the blending formula and conducted further validation on the feasibility of direct repair. To optimize fusion efficacy, minimize postoperative recovery time, and reduce reliance on stone paste and support, various supplementary internal fixation techniques have been developed. In 1970, Buck conducted a study on internal fixation for lumbar spondylolysis using screws inserted directly through the interarticular area, which yielded favorable outcomes in more than 80% of patients. This technique has since become the most classic form of intersegmental repair due to its advantages of reduced operation time, minimal bleeding, rapid recovery and a high rate of bone healing. The procedure has limited potential for effective bone grafting, posing a significant challenge for surgeons attempting to achieve successful implantation. Nicol and Scott [9] proposed and implemented the wiring technique to address defects, which demonstrated remarkable success in 80% of cases reported in 1987. However, to ensure optimal visualization throughout the procedure [26, 27], Scott’s technique requires extensive tissue removal and excision of the iliolumbar ligament to expose the transverse process. Additionally, it may also lead to fractures of congenitally small transverse processes, resulting in postoperative wire loosening and nonunion at the fracture site, thereby causing persistent chronic lumbago in clinical settings. In 1984, Morscher [28] introduced a laminar hook that was positioned within the defect and applied a compressive force using a spring held against a screw to achieve approximation of the isthmic defect during the articular process. The majority of patients with spondylolysis exhibit congenital malformations, which may lead to potential invasion of the spinal canal. Gillet and Petit [29] proposed a V-shaped titanium rod fixation technique for lumbar spondylolysis, achieving an impressive success rate of approximately 60%. Barakat et al. [30]. further refined the method introduced by Gillet and Petit, utilizing a U-shaped titanium rod fixation approach to treat 25 adolescent patients with lumbar spondylolysis. The results demonstrated that the healing rate of the isthmus bone reached 76% at 6 months, and complete healing (100%) was achieved at 12 months.
Recently, Pedro Berjano [31] introduced a novel technique, the Pedicle Screws, Rod and Polyester Bands technique, which significantly reduced pain and expedited social rehabilitation during a 4-year follow-up period. However, this technique necessitates extensive tissue dissection. The current state of this technique is limited to case reports, and further research with larger sample sizes is necessary to validate the findings. The novel technique presented in this paper for repairing spondylolysis involves the use of a V-type titanium cable and pedicle screw, which represents an advancement over the Scott technique and the Shaped Road technique. This approach combines pedicle screw and titanium cable fixation to create a tension band within the isthmus of the affected vertebra, along with local bone grafting for treating young patients with lumbar spondylolysis, yielding favorable outcomes. Spondylolysis and spina bifida occulta (SBO) often exhibit hereditary tendencies [32] and demonstrate close associations [33, 34]. Compared to traditional procedures, this operation offers enhanced safety and efficacy, along with improved convenience. Our team discovered that pedicle screw and spinous process steel-wire fixation lacked sufficient strength for spondylolysis stabilization. With the advancement of research, V-type titanium cables have replaced spinous process steel wires as a superior alternative. The integration of the titanium cable and pedicle screw forms a V-shaped tension band fixation mode, which effectively prevents severe injury to the quadrate ligament complex of the posterior vertebral body and aligns better with biomechanical requirements. Our team used finite element simulation to evaluate the efficacy of different internal fixation techniques. We compared pedicle screws with laminar hooks, U-shaped rods, and V-shaped titanium cables.The findings showed that the range of motion (ROM) for the vertebral body with the V-shaped titanium cable method (0.39° to 3.67°) was closer to the normal ROM (0.29° to 4.32°). Additionally, this technique achieved joint cartilage stress (6.35 MPa to 18.6 MPa) that more effectively restored normal loading conditions (5.8 MPa to 19.17 MPa), creating a more stable environment for bone grafting.
With this surgical technique, we observed minimal changes in the PI value during subsequent follow-up, indicating that intrasegmental repair did not compromise the integrity of the original anatomical structure. As a crucial parameter for sagittal alignment of the human spine and pelvis, the PI plays a pivotal role in maintaining sagittal balance and is closely associated with the development of IS [35–37]. The patients in this study demonstrated significant improvement in VAS scores and ODI scores with postoperative functional exercises compared to preoperative levels. At the final follow-up, 90.47% of the patients met the Macnab efficacy criteria, indicating that this surgical procedure markedly enhanced quality of life.
Most patients with lumbar spondylolysis have anatomical variations, such as changes in the lumbar facet joint direction from sagittal to coronal and changes in the facet joint angle on both sides of the lumbar spine, which leads to a decrease in the accuracy of surgical screw placement for lumbar spondylolysis and an increase in complications. The operation not only reconstructs the L5 lumbar vertebral vertebral isthmus but also protects the joint capsule formed by the L4 vertebral subaarticular process and the L5 vertebral supraarticular process, which plays an important role in balancing the stability of the spine and controlling the movement of the spine[. If the lumbar facet joints can be well protected during the operation, the postoperative load of the posterior lumbar spine will not be reduced, which can ensure stable movement of the lumbar spine and prevent excessive torsion of the intervertebral disc from causing injury, which can effectively buffer the forward shear force and prevent the vertebral body from sliding forward.
In addition, the following data were collected from the study: (1) Preoperative three-dimensional printing technology has been used in our department for many years, which is of great help to the planning and development of the operation. (2) The sclerotic area between the isthmus was removed, and the surface of the lamina, the pedicle and the lateral part of the vertebral body were ground to the “fish scale” of cortical bone. (3) The bone graft should be fully and effectively compressed to make the bone graft surface more closely fit and further improve the healing rate. (4) 3D navigation technology is utilized in lumbar interbody fusion surgery to increase the precision of pedicle screw placement and prevent potential damage to the facet joints of the L4 and L5 vertebrae. (5) No intervention is made in the bone graft area, further promoting fracture healing. (6) V-type titanium cables and pedicle screws are simple to use and are suitable for clinical use. (7) The pedicle screw was tensioned, and pressure was applied to the titanium cable and the bone graft area. (8) The indications for this operation should be strictly mastered, and it is not suitable for patients with IS complicated with spinal stenosis. (9) MRI is a valuable technique. If MRI shows obvious degeneration of the intervertebral disc, segmental fusion and internal fixation can be performed.
There are several limitations in this study. First, this was a retrospective study, which has selection bias. Second, this was a single-center study in which only a small number of patients were recruited. More multicenter studies with larger sample sizes are needed to strengthen the conclusions.
Conclusion
The V-shaped titanium cable combined with a pedicle screw fixation system for the treatment of fifth lumbar spondylolysis in young patients is simple and effective. For patients with less disc injury or mild lumbar spondylolysis, the overall excellent and good healing rates of spondylolysis are high, and the failure rate of internal fixation is low. The most important thing is to protect the FSU and reduce the incidence of ASD changes.
Acknowledgements
Not applicable.
Abbreviations
- PI
Pelvic incidence
- VAS
Visual analog scale
- ODI
Oswestry Disability Index
- IS
Isthmic spondylolisthesis
- FSU
Functional spinal unit
- ASD
Adjacent segment disease
- SBO
Spina bifda occulta
- ROM
Range of motion
Author contributions
XH: Conducted the study The data were collected, analyzed, and interpreted. Wrote the manuscript.YT: Designed the study, interpreted the data, and edited the manuscript.RM: Planned the project. Interpreted the data.WA: Interpreted the data.TL: Edited the manuscript and reviewed the manuscript.QL: Edited the manuscript.HX: Planned the project.KY: Manuscript review.All the authors have read and approved the final manuscript.
Funding information
This study was funded by the Natural Science Foundation of Xinjiang Uygur Autonomous Region (2023D01C93) and Regional Collaborative Innovation Project (Science and Technology Assistance to Xinjiang) (2019E0277).
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
This retrospective study was approved by the Ethics Committee of the General Hospital of Xinjiang Military Command and was carried out in accordance with the ethical standards set out in the Helsinki Declaration. Informed consent was obtained from all participants.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Competing interests
The authors declare no competing interests.
Disclosure
The authors report no proprietary or commercial interest in any of the products mentioned or concepts discussed in this article.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Aoki Y, Takahashi H, Nakajima A, Kubota G, Watanabe A, Nakajima T, et al. Prevalence of lumbar spondylolysis and spondylolisthesis in patients with degenerative spinal disease. Sci Rep. 2020;10:6739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chung CC, Shimer AL. Lumbosacral Spondylolysis and Spondylolisthesis. Clin Sports Med. 2021;40:471–90. [DOI] [PubMed] [Google Scholar]
- 3.Sakai T, Sairyo K, Suzue N, Kosaka H, Yasui N. Incidence and etiology of lumbar spondylolysis: review of the literature. J Orthop Sci. 2010;15:281–8. [DOI] [PubMed] [Google Scholar]
- 4.Fredrickson BE, Baker D, McHolick WJ, Yuan HA, Lubicky JP. The natural history of spondylolysis and spondylolisthesis. J Bone Joint Surg Am. 1984;66:699–707. [PubMed] [Google Scholar]
- 5.Debnath UK, Freeman BJC, Gregory P, de la Harpe D, Kerslake RW, Webb JK. Clinical outcome and return to sport after the surgical treatment of spondylolysis in young athletes. J Bone Joint Surg Br. 2003;85:244–9. [DOI] [PubMed] [Google Scholar]
- 6.Ying J, Hou L, Teng H. Successful Bony Healing for an adult patient with Isthmic Spondylolysis at Terminal Stage after Conservative Treatment: a Case Report. J Pain Res. 2019;12:3257–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leone A, Cianfoni A, Cerase A, Magarelli N, Bonomo L. Lumbar spondylolysis: a review. Skeletal Radiol. 2011;40:683–700. [DOI] [PubMed] [Google Scholar]
- 8.Bydon M, Alvi MA, Goyal A. Degenerative lumbar spondylolisthesis: definition, natural history, Conservative Management, and Surgical Treatment. Neurosurg Clin N Am. 2019;30:299–304. [DOI] [PubMed] [Google Scholar]
- 9.Buck JE. Direct repair of the defect in spondylolisthesis. Preliminary report. J Bone Joint Surg Br. 1970;52:432–7. [PubMed] [Google Scholar]
- 10.Johnson GV, Thompson AG. The Scott wiring technique for direct repair of lumbar spondylolysis. J Bone Joint Surg Br. 1992;74:426–30. [DOI] [PubMed] [Google Scholar]
- 11.Sales de Gauzy J, Vadier F, Cahuzac JP. Repair of lumbar spondylolysis using Morscher material: 14 children followed for 1–5 years. Acta Orthop Scand. 2000;71:292–6. [DOI] [PubMed] [Google Scholar]
- 12.Patel RD, Rosas HG, Steinmetz MP, Anderson PA. Repair of pars interarticularis defect utilizing a pedicle and laminar screw construct: a new technique based on anatomical and biomechanical analysis. J Neurosurg Spine. 2012;17:61–8. [DOI] [PubMed] [Google Scholar]
- 13.Wu H-H, Brown K, Flores M, Cazzulino A, Swarup I. Diagnosis and management of Spondylolysis and Spondylolisthesis in Children. JBJS Rev. 2022;10. [DOI] [PubMed]
- 14.Tarpada SP, Kim D, Levine NL, Morris MT, Cho W. Comparing Surgical treatments for Spondylolysis: review on current research. Clin Spine Surg. 2021;34:276–85. [DOI] [PubMed] [Google Scholar]
- 15.Yurac R, Bravo JT, Silva Á, Marré B. Spondylolysis Repair using a minimally invasive modified Buck technique with neuronavigation and neuromonitoring in High School and Professional athletes: Technical Notes, Case Series, and Literature Review. World Neurosurg. 2021;155:54–63. [DOI] [PubMed] [Google Scholar]
- 16.Plomp KA, Dobney K, Collard M. Spondylolysis and spinal adaptations for bipedalism: the overshoot hypothesis. Evol Med Public Health. 2020;2020:35–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buchbinder R, Blyth FM, March LM, Brooks P, Woolf AD, Hoy DG. Placing the global burden of low back pain in context. Best Pract Res Clin Rheumatol. 2013;27:575–89. [DOI] [PubMed] [Google Scholar]
- 18.Mohile NV, Kuczmarski AS, Lee D, Warburton C, Rakoczy K, Butler AJ. Spondylolysis and Isthmic spondylolisthesis: a guide to diagnosis and management. J Am Board Fam Med. 2022;35:1204–16. [DOI] [PubMed] [Google Scholar]
- 19.Alqarni AM, Schneiders AG, Cook CE, Hendrick PA. Clinical tests to diagnose lumbar spondylolysis and spondylolisthesis: a systematic review. Phys Ther Sport. 2015;16:268–75. [DOI] [PubMed] [Google Scholar]
- 20.Randall RM, Silverstein M, Goodwin R. Review of Pediatric Spondylolysis and Spondylolisthesis. Sports Med Arthrosc Rev. 2016;24:184–7. [DOI] [PubMed] [Google Scholar]
- 21.Choi JH, Ochoa JK, Lubinus A, Timon S, Lee Y-P, Bhatia NN. Management of lumbar spondylolysis in the adolescent athlete: a review of over 200 cases. Spine J. 2022;22:1628–33. [DOI] [PubMed] [Google Scholar]
- 22.Areias B, Caetano SC, Sousa LC, Parente M, Jorge RN, Sousa H, et al. Numerical simulation of lateral and transforaminal lumbar interbody fusion, two minimally invasive surgical approaches. Comput Methods Biomech Biomed Engin. 2020;23:408–21. [DOI] [PubMed] [Google Scholar]
- 23.Huang Y, Liu J, Guo L, Meng Y, Hao D, Du J. Temporary short segment fixation in treating adolescent lumbar spondylolysis. World Neurosurg. 2019;123:e77–84. [DOI] [PubMed] [Google Scholar]
- 24.Kimura M. [My method of filing the lesion with spongy bone in spondylolysis and spondylolistesis]. Seikei Geka. 1968;19:285–96. [PubMed] [Google Scholar]
- 25.Dai LY, Jia LS, Yuan W, Ni B, Zhu HB. Direct repair of defect in lumbar spondylolysis and mild isthmic spondylolisthesis by bone grafting, with or without facet joint fusion. Eur Spine J. 2001;10:78–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ulibarri JA, Anderson PA, Escarcega T, Mann D, Noonan KJ. Biomechanical and clinical evaluation of a novel technique for surgical repair of spondylolysis in adolescents. Spine (Phila Pa 1976). 2006;31:2067–72. [DOI] [PubMed] [Google Scholar]
- 27.Aihara T, Takahashi K, Yamagata M, Moriya H, Tamaki T. Biomechanical functions of the iliolumbar ligament in L5 spondylolysis. J Orthop Sci. 2000;5:238–42. [DOI] [PubMed] [Google Scholar]
- 28.Morscher E, Gerber B, Fasel J. Surgical treatment of spondylolisthesis by bone grafting and direct stabilization of spondylolysis by means of a hook screw. Arch Orthop Trauma Surg (1978). 1984;103:175–8. [DOI] [PubMed] [Google Scholar]
- 29.Gillet P, Petit M. Direct repair of spondylolysis without spondylolisthesis, using a rod-screw construct and bone grafting of the pars defect. Spine (Phila Pa 1976). 1999;24:1252–6. [DOI] [PubMed] [Google Scholar]
- 30.Barakat AS, Soliman WS, Elgharabawy AF, et al. Repair of spondylolysis using a pedicle screw U-shaped rod construct: a preliminary study of 25 young patients with a mean follow-up of 24 months. J Craniovertebr Junction Spine. 2021 Apr-Jun;12(2):170–7. [DOI] [PMC free article] [PubMed]
- 31.Berjano P, Ristori G, Ismael Aguirre M-F, Langella F, Damilano M, Cecchinato R, et al. A novel technique for Spondylolysis Repair with Pedicle screws, Rod and Polyester Band: Case Report with Technical note and systematic literature review. Spine (Phila Pa 1976). 2020;45:E1682–91. [DOI] [PubMed] [Google Scholar]
- 32.Morimoto M, Sugiura K, Higashino K, Manabe H, Tezuka F, Wada K, et al. Association of spinal anomalies with spondylolysis and spina bifida occulta. Eur Spine J. 2022;31:858–64. [DOI] [PubMed] [Google Scholar]
- 33.Tsukagoshi Y, Kamegaya M, Tatsumura M, Tomaru Y, Kamada H, Morita M, et al. Characteristics and diagnostic factors associated with fresh lumbar spondylolysis in elementary school-aged children. Eur Spine J. 2020;29:2465–9. [DOI] [PubMed] [Google Scholar]
- 34.Aoyagi M, Naito K, Sato Y, Kobayashi A, Sakamoto M, Tumilty S. Identifying acute lumbar spondylolysis in young athletes with low back Pain: retrospective classification and regression tree analysis. Spine (Phila Pa 1976). 2021;46:1026–32. [DOI] [PubMed] [Google Scholar]
- 35.Vazifehdan F, Karantzoulis VG, Igoumenou VG. Acquired spondylolysis and spinopelvic sagittal alignment. Eur J Orthop Surg Traumatol. 2018;28:1033–8. [DOI] [PubMed] [Google Scholar]
- 36.Takeuchi M, Tezuka F, Chikawa T, Hibino N, Takahashi Y, Yamasaki Y, et al. Consecutive double-level lumbar spondylolysis successfully treated with the double smiley face rod method. J Med Invest. 2020;67(12):202–6. [DOI] [PubMed] [Google Scholar]
- 37.Zhou Q-S, Sun MM, Chen X, Xu X, Qian L. B-P, How does sagittal spinopelvic alignment of lumbar multisegmental spondylolysis differ from monosegmental spondylolysis? J Neurosurg Spine. 2020;:1–8. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.